Personality disorder test nhs
Personality disorders - NHS
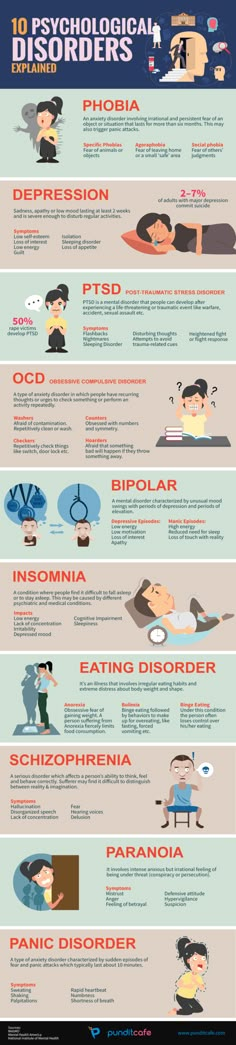
A person with a personality disorder thinks, feels, behaves or relates to others very differently from the average person.
There are several different types of personality disorder.
This page gives some information about personality disorders in general, linking to other sources for more detail.
Symptoms of a personality disorder
Symptoms vary depending on the type of personality disorder.
For example, a person with borderline personality disorder (one of the most common types) tends to have disturbed ways of thinking, impulsive behaviour and problems controlling their emotions.
They may have intense but unstable relationships and worry about people abandoning them.
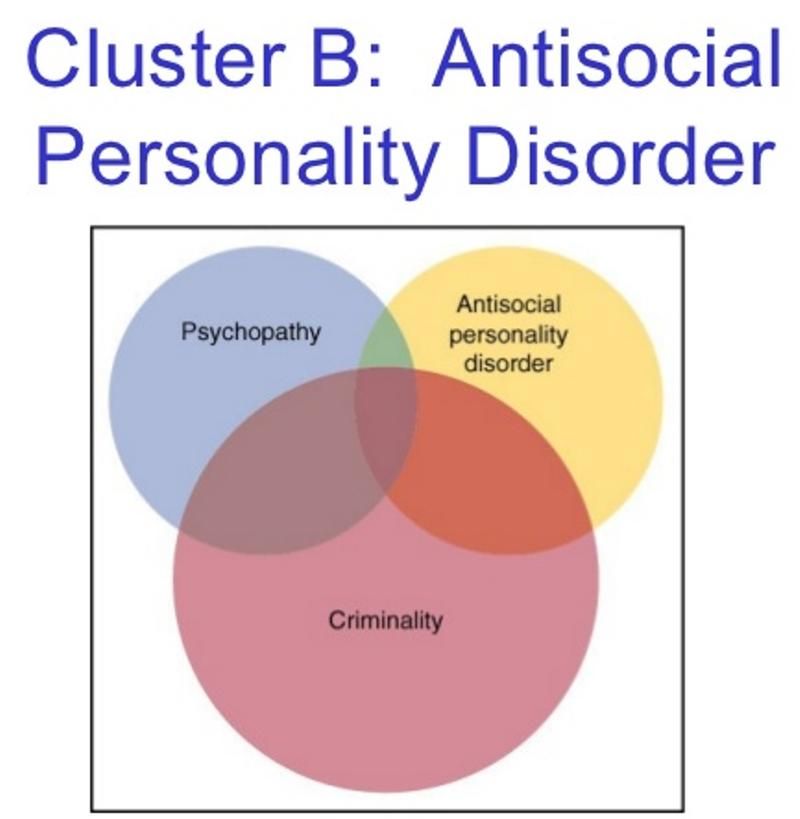
A person with antisocial personality disorder will typically get easily frustrated and have difficulty controlling their anger.
They may blame other people for problems in their life, and be aggressive and violent, upsetting others with their behaviour.
Someone with a personality disorder may also have other mental health problems, such as depression and substance misuse.
Find out more about the different types of personality disorder on the Mind website
Treatment for a personality disorder
Treatment for a personality disorder usually involves a talking therapy. This is where the person talks to a therapist to get a better understanding of their own thoughts, feelings and behaviours.
Treatment can last several months or years, depending on the severity of the condition and other problems the person may have.
As well as listening and discussing important issues with the person, the therapist may identify strategies to resolve problems and, if necessary, help them change their attitudes and behaviour.
Therapeutic communities
Therapeutic communities (TCs) are places where someone visits or stays for an intensive form of group therapy. The experience of having a personality disorder is explored in depth.
The person usually attends for a number of weeks or months.
Medicine
Medicine may be prescribed to treat problems associated with a personality disorder, such as depression, anxiety or psychotic symptoms.
For example, moderate to severe symptoms of depression might be treated with a type of antidepressant called a selective serotonin reuptake inhibitor (SSRI).
Read more about the treatment for borderline personality disorder and antisocial personality disorder.
You can also visit the Royal College of Psychiatrists website, and charity websites Mind and Rethink Mental Illness for their patient information on treatment for other types of personality disorder.
Recovery
Many people with a personality disorder recover over time. Psychological or medical treatment is often helpful, but support is sometimes all that's needed.
There's no single approach that suits everyone – treatment should be tailored to the individual.
Causes
It's not clear exactly what causes personality disorders, but they're thought to result from a combination of the genes a person inherits and early environmental influences – for example, a distressing childhood experience (such as abuse or neglect).
Support for people living with a personality disorder
Having a personality disorder can have a big effect on the person's life, as well as their family and friends, but support is available.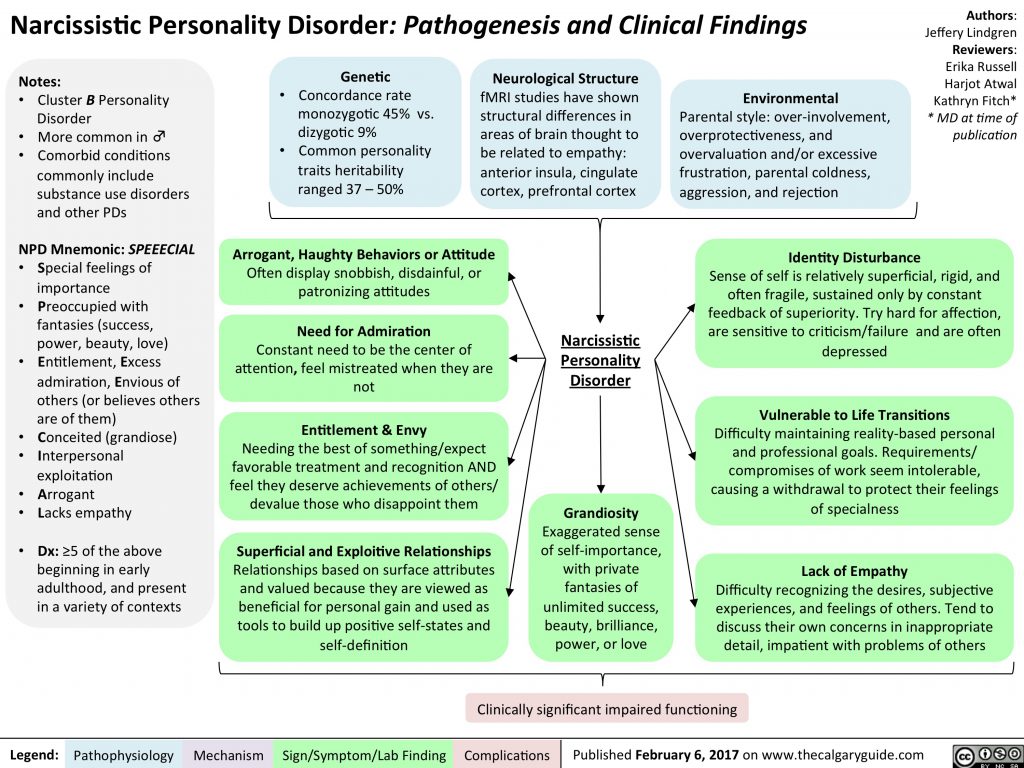
If you'd like support for yourself or someone you know, you may find the following links useful:
- Mind: useful contacts
- Rethink mental illness: personality disorders
- Royal College of Psychiatrists: personality disorder
- Time to Change: personal stories of personality disorders
Ask a GP about support groups for personality disorders near you. Or find out what mental health services exist and how to access them.
Page last reviewed: 12 October 2020
Next review due: 12 October 2023
Borderline Personality Disorder (BPD) Test
Personality DisordersBorderline Personality Disorder (BPD)
Complete the following to get an assessment on the likelihood that you or a loved one is displaying symptoms of borderline personality disorder. All results are completely private.
All results are completely private.
Medical ReviewerRandy Bressler, PsyD
Who Is This Borderline Personality Disorder Quiz For?
The questions below relate to life experiences common among people who have borderline personality disorder. Please read each question carefully, and indicate how often you have experienced the same or similar challenges in the past few weeks.
If you are taking the quiz for someone else such as a husband, wife, boyfriend, girlfriend, parent, or child you should provide answers you think they'd supply. Ideally you'll have the loved one complete the test themselves and take the results to a doctor or licensed professional.
How Accurate Is It?
This quiz is NOT a diagnostic tool. Mental health disorders can only be diagnosed by a licensed mental health professional or doctor.
Psycom believes assessments can be a valuable first step toward getting treatment. All too often people stop short of seeking help out of fear their concerns aren't legitimate or severe enough to warrant professional intervention.
All too often people stop short of seeking help out of fear their concerns aren't legitimate or severe enough to warrant professional intervention.
Your privacy is important to us. All results are completely anonymous.
Alchemer - amazing survey software for business. Please take my survey now
Borderline Personality Disorder
How is borderline personality disorder (BPD) diagnosed?
There is no definitive test to diagnose borderline personality disorder (BPD). It is diagnosed through a clinical interview with a licensed mental health professional, explains Simon A. Rego, PsyD, chief psychologist at Montefiore Medical Center and Associate Professor of Psychiatry and Behavioral Sciences at Albert Einstein College of Medicine, both in New York City.
The mental health professional may ask the person to complete some assessment measures to aid in the diagnosis. They may also talk with the person’s previous health care providers, look at earlier medical evaluations, and conduct interviews with friends and family.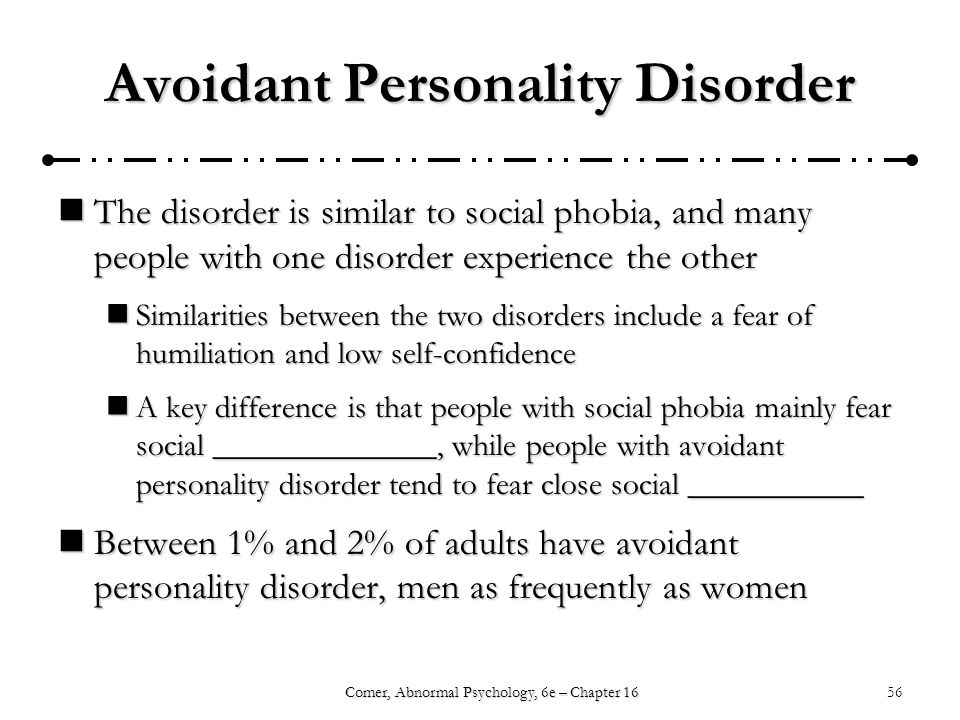 1
1
Who can diagnose borderline personality disorder?
BPD is most often diagnosed by a mental health professional, such as a psychologist, psychiatrist, or social worker, says Simon A. Rego, PsyD, chief psychologist at Montefiore Medical Center and Associate Professor of Psychiatry and Behavioral Sciences at Albert Einstein College of Medicine, both in New York City.
What proportion of people with borderline personality disorder are women?
About 1.4% of adults in the U.S. have BPD1, and it is estimated that around 75% of those diagnosed with borderline personality disorder are women.2 However, more recent research suggests that BPD may be equally as common in men, but is often misdiagnosed as another disorder, such as post-traumatic stress disorder or depression, says Simon A. Rego, PsyD, chief psychologist at Montefiore Medical Center and Associate Professor of Psychiatry and Behavioral Sciences at Albert Einstein College of Medicine, both in New York City.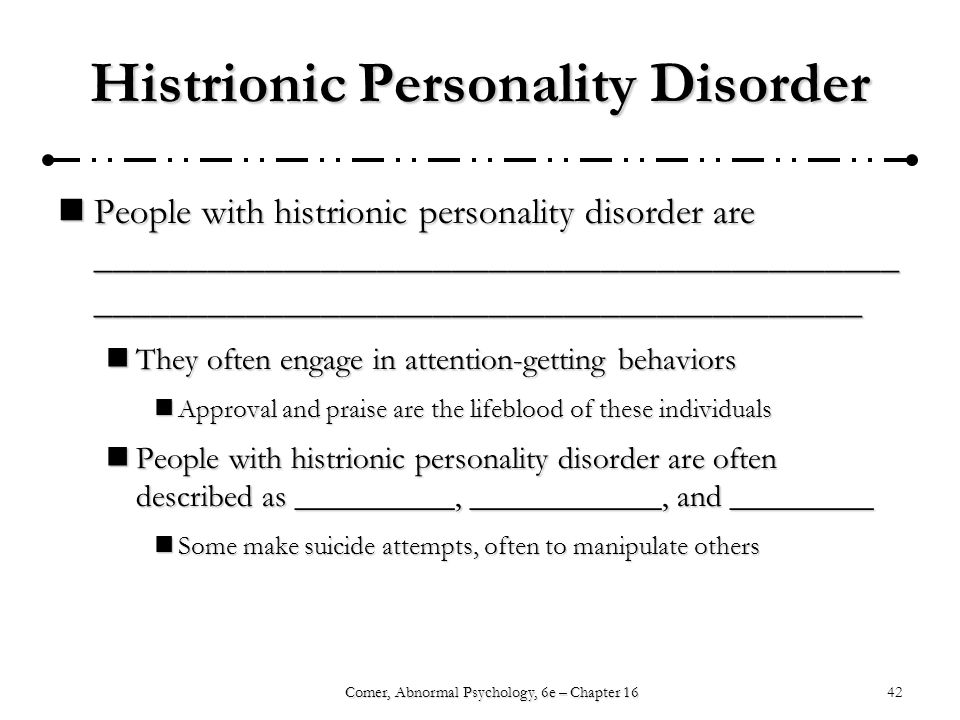
How long does it take to diagnose borderline personality disorder?
Diagnosing BPD typically takes one or two sessions, says Simon A. Rego, PsyD, chief psychologist at Montefiore Medical Center and Associate Professor of Psychiatry and Behavioral Sciences at Albert Einstein College of Medicine, both in New York City. “However, because borderline personality disorder can be confused with other disorders, such as bipolar disorder, unfortunately, getting the correct diagnosis can take some time,” he explains.
For example, a 2009 study found that 74% of the patients who met the criteria for the condition had never been diagnosed with BPD in the past, despite an average of more than 10 years since their first “psychiatric encounter.”3
Why are more women diagnosed with borderline personality disorder?
Some researchers think that there may be biological, psychological, and social/environmental factors that predispose women to BPD, says Simon A.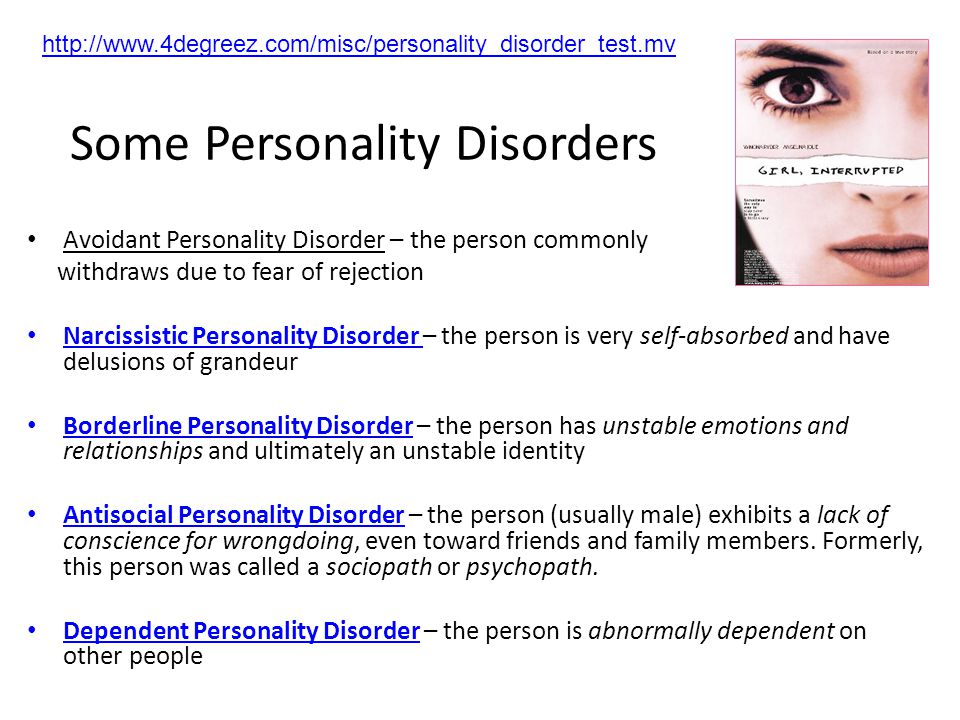 Rego, PsyD, chief psychologist at Montefiore Medical Center and Associate Professor of Psychiatry and Behavioral Sciences at Albert Einstein College of Medicine, both in New York City. However, he explains, evidence also suggests that the difference may be accounted for by a “diagnostic gender bias.”
Rego, PsyD, chief psychologist at Montefiore Medical Center and Associate Professor of Psychiatry and Behavioral Sciences at Albert Einstein College of Medicine, both in New York City. However, he explains, evidence also suggests that the difference may be accounted for by a “diagnostic gender bias.”
A diagnostic gender bias means that if the person is a woman, she is much more likely to receive the diagnosis of BPD than if she were a man reporting the same symptoms, Rego says.
What can borderline personality disorder be mistaken for?
The most common diagnoses that borderline personality disorder is mistaken for are bipolar disorder, depression, anxiety disorders, and eating disorders, says Simon A. Rego, PsyD, chief psychologist at Montefiore Medical Center and Associate Professor of Psychiatry and Behavioral Sciences at Albert Einstein College of Medicine, both in New York City.
What are the criteria for borderline personality disorder?
The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) outlines the criteria for a diagnosis. BPD is diagnosed on the basis of (1) a pervasive pattern of instability of interpersonal relationships, self-image, and affect (the outward display of a person's emotional state, including their speech, body language, and gestures) and (2) marked impulsivity beginning by early adulthood and present in a variety of contexts, as indicated by at least five of the following nine criteria:
BPD is diagnosed on the basis of (1) a pervasive pattern of instability of interpersonal relationships, self-image, and affect (the outward display of a person's emotional state, including their speech, body language, and gestures) and (2) marked impulsivity beginning by early adulthood and present in a variety of contexts, as indicated by at least five of the following nine criteria:
- Frantic efforts to avoid real or imagined abandonment; this does not include suicidal or self-mutilating behavior covered in criterion 5
- A pattern of unstable and intense interpersonal relationships characterized by alternating between extremes of idealization and devaluation
- Markedly and persistently unstable self-image or sense of self
- Impulsivity in at least two areas that are potentially self-damaging (e.g., spending, sex, substance abuse, reckless driving, binge eating). This does not include suicidal or self-mutilating behavior covered in criterion 5.
- Recurrent suicidal behavior, gestures, or threats, or self-mutilating behavior
- Affective instability due to a marked reactivity of mood (e.
 g., intense episodic dysphoria, irritability, or anxiety usually lasting a few hours and only rarely more than a few days)
g., intense episodic dysphoria, irritability, or anxiety usually lasting a few hours and only rarely more than a few days) - Chronic feelings of emptiness
- Inappropriate, intense anger or difficulty controlling anger
- Transient, stress-related paranoid ideation or severe dissociative symptoms
What does it feel like to have borderline personality disorder?
BPD is characterized by intense emotional highs and lows, and can make someone feel very anxious, depressed, and unstable, says Simon A. Rego, PsyD, chief psychologist at Montefiore Medical Center and Associate Professor of Psychiatry and Behavioral Sciences at Albert Einstein College of Medicine, both in New York City.
A person with BPD can have mood swings and unstable relationships. They tend to view things in extremes, as in all good or all bad. Their opinions of other people can change quickly. For instance, they may see a person as a friend one day and an enemy the next. 1
1
Can BPD go away?
While BPD has historically been seen as a lifelong, very disabling mental health condition, recent research is challenging this assumption. Now it appears that there may be a positive trajectory over time, with many of the most troubling symptoms remitting during the first few years. Unfortunately, other symptoms may remain for longer periods.
Even though many psychotherapies have been developed to help people with BPD, long-term recovery in social functioning is still difficult for them, says Simon A. Rego, PsyD, chief psychologist at Montefiore Medical Center and Associate Professor of Psychiatry and Behavioral Sciences at Albert Einstein College of Medicine, both in New York City.
- National Institute of Mental Health. Borderline Personality Disorder. Page Last Revised December 2017. Accessed June 7, 2021.
- National Alliance on Mental Illness. Borderline Personality Disorder. Page Last Reviewed December 2017.
 Accessed June 7, 2021.
Accessed June 7, 2021. - Myerson D et al. Is Borderline Personality Disorder Underdiagnosed? Abstract No. 51 of Scientific and Clinical Reports, American Psychiatric Association 162nd Clinical Meeting, May 2009, San Francisco, California.
Notes: This article was originally published June 27, 2022 and most recently updated June 28, 2022.
8 Bipolar Myths You Shouldn't Believe
October 5, 2021Life
Share
0 Probably everyone has heard jokes about “bipolar”. Usually they are directed towards a person who, for no reason at all, begins to feel sad, angry, or, conversely, rejoice. But the symptoms of bipolar affective disorder (BAD) involve more than just mood swings. Everything is much more complicated. On the eve of World Mental Health Day, which is celebrated on October 10, popular misconceptions about bipolar disorder have been sorted out. We prepared this material together with the pharmaceutical company Gedeon Richter, which has been initiating special projects about the lives of people with schizophrenia and bipolar disorder for several years now.
Myth 1. BAD is a split personality
In fact, these are two different diagnoses. A split personality is officially called a dissociative identity disorder: a person switches from one ego state to another at different intervals. People with this diagnosis may feel that several personalities coexist in their head at once, as if alternately intercepting control. Each of these characters can have their own history, name, age, personality and habits. Other symptoms of dissociative identity disorder include partial memory loss, problems coping with stress and self-identity.
Bipolar disorder in a person with no obvious external causes Bipolar disorder / Mayo Clinic has severe mood swings ranging from depression to mania or hypomania (this condition resembles mania, but with less pronounced manifestations). During a depressive episode, a person experiences an emotional decline, and during a manic episode, a maximum spiritual upsurge. Such instability affects the quality of sleep, behavior, the ability to act and make decisions.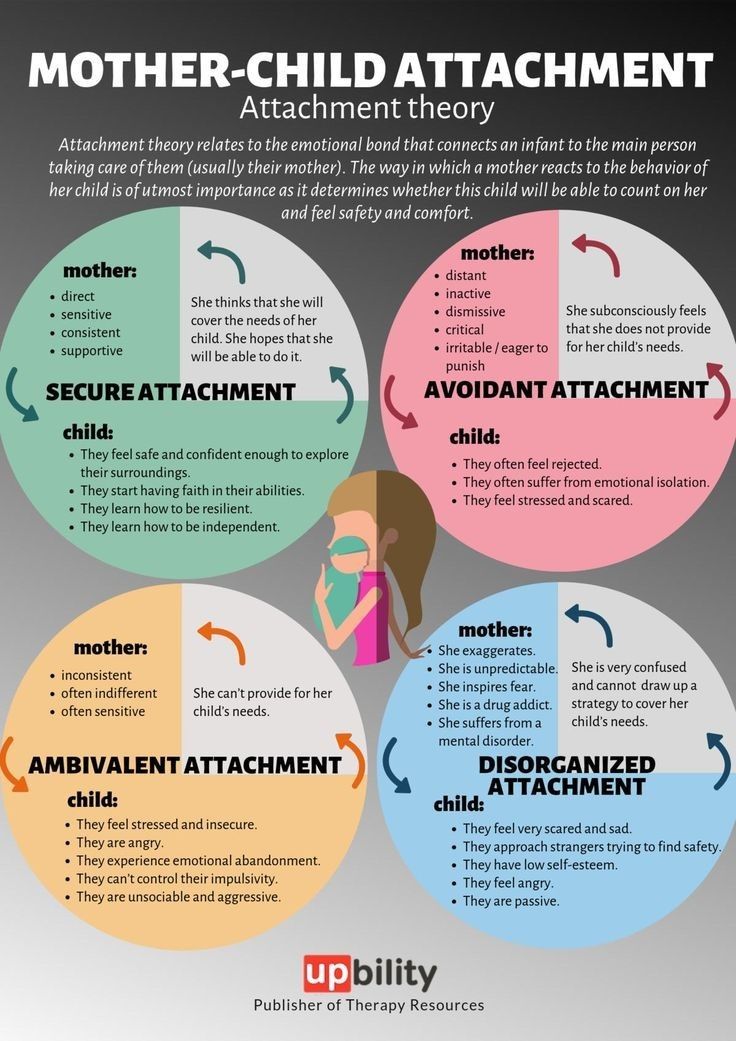
Myth 2. Bipolar disorder is a trendy diagnosis. In fact, his cases are rare
Image: Mary Long / ShutterstockSome form of bipolar disorder is estimated to be experienced from Bipolar disorder statistics 2021 / SingleCare 2.4 to Michael Bauer and Andrea Pfennig. Epidemiology of Bipolar Disorders / Epilepsia 6.5% of the world's population. It is not easy to make such a diagnosis because there is no one simple test or biomarker. The specialist performs a Bipolar disorder / Mayo Clinic multi-stage clinical assessment: collects a mental health history, finds out the severity and duration of symptoms, and also monitors the cyclicity of episodes.
The sooner the disease is detected, the sooner treatment can begin. With a properly selected scheme, patients can be in stable remission.
Myth 3. Depressive and manic episodes are cyclical
Not everything is so simple. These periods do not have a schedule: some people with bipolar disorder have them all the time, others once or twice a year.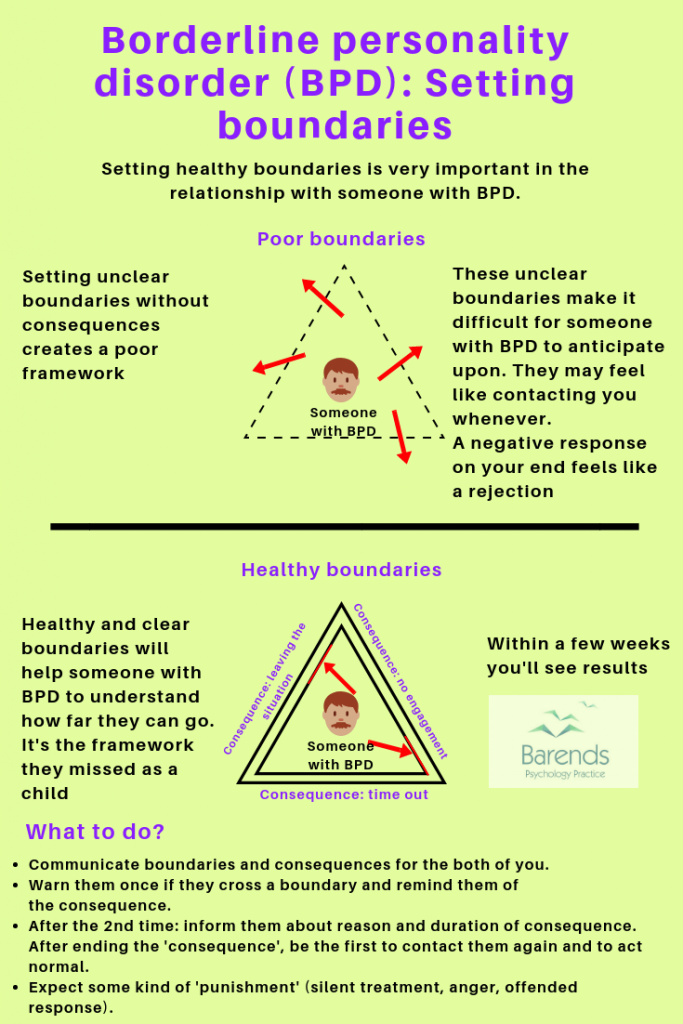 There are intervals in which there are no symptoms at all. A mixed affective state can also be observed with simultaneous experience or rapid alternation of symptoms of both manic and depressive spectrums. For example, sadness and despair, but at the same time a surge of energy.
There are intervals in which there are no symptoms at all. A mixed affective state can also be observed with simultaneous experience or rapid alternation of symptoms of both manic and depressive spectrums. For example, sadness and despair, but at the same time a surge of energy.
There are also several types of bipolar disorder Bipolar Disorder / National Alliance on Mental Illness, which are characterized by different symptoms:
- BAD type I. In this case, manic episodes usually alternate with depressive episodes, but depression is not necessary for a diagnosis. Mania lasts from seven days, and sometimes its symptoms are so pronounced that a person may need to be hospitalized.
- Type II BAR. Here, on the contrary, depressive episodes are usually experienced. There may be a state of hypomania, but there is never a full-fledged mania.
- Cyclothymia. These are chronic state changes. A person for at least two years is constantly in mild depression, then in hypomania.
 Periods of normal mood also occur, but they last no more than eight weeks.
Periods of normal mood also occur, but they last no more than eight weeks.
There are also cases that do not fit the description of either BAD type I or II, or cyclothymia, but are also characterized by periodic bright jumps in the emotional state.
Myth 4. Bipolar disorder is just frequent mood swings
Bipolar disorder is not limited to one alternation of mood ups and downs. It seriously affects various aspects of life - from the ability to concentrate to the quality of sleep. During depressive episodes, suicidal thoughts and feelings of guilt are possible; during manic episodes, frightening self-confidence, nervousness, and a tendency to risky behavior are possible.
In addition, people with type I or II bipolar disorder may experience Bipolar disorder / Mayo Clinic develop comorbid disorders such as melancholia and psychosis.
Myth 5. People with bipolar disorder can't work properly and have relationships
Difficulty finding a job is a common problem people with bipolar disorder face. In fact, they are capable of Managing Bipolar Disorder at Work / WebMD to do the job just as well as others, although in some cases they have to try harder to control their thoughts and moods. In addition, being busy can help such people increase their self-confidence and make their lives more orderly.
In fact, they are capable of Managing Bipolar Disorder at Work / WebMD to do the job just as well as others, although in some cases they have to try harder to control their thoughts and moods. In addition, being busy can help such people increase their self-confidence and make their lives more orderly.
But what kind of work to choose depends on individual preferences, manifestations of episodes and their frequency. For example, it is more convenient for some to deal with projects, for others, constant workload is suitable, for others, a flexible schedule is needed.
People with bipolar disorder can have romantic relationships Bipolar Romantic Relationships: Dating and Marriage / WebMD Moreover, the support of friends and partners helps in treatment. For example, loved ones can make sure that a person regularly takes prescribed medications, remind them of the need to visit a specialist, and notice signs of the onset of a manic or depressive episode in time.
Myth 6. Manic episodes are a period of joy
Image: Mary Long / ShutterstockThis is not always the case. Mania and hypomania can be accompanied by a surge of energy, an increase in mood, and sometimes even euphoria. But these conditions have other, less pleasant manifestations of Bipolar disorder / Mayo Clinic.
Thus, during manic episodes, people with bipolar disorder may become irritable or distracted. The need for rest decreases, which worsens the general condition of the body. The person has difficulty concentrating and making decisions, and may become unusually chatty and agitated.
All this can have a negative impact on working capacity, relationships with friends, family and colleagues. If left unattended, manic episodes can develop into psychosis. When a person with bipolar disorder reports to Psychosis / NHS inform that they are experiencing hallucinations or share strange ideas that are out of touch with reality, a specialist should be consulted urgently.
Myth 7. A person with bipolar disorder will definitely have children with the same diagnosis.
The exact causes of bipolar disorder are unknown. Experts believe that the possibility of hereditary transmission of the disease is not excluded Bipolar Disorder / National Alliance on Mental Illness, but it is impossible to predict whether this will happen or not. A child from a family with a history of bipolar disorder may not experience the disorder themselves.
A more popular version of the occurrence of the disease is an imbalance of Bipolar disorder / NHS neurotransmitters: norepinephrine, serotonin and dopamine. When the level of norepinephrine goes off scale, mania can set in, and when it drops, depression occurs.
BAD can be provoked by periods of acute stress, deep emotional experience, such as the death of a loved one, drug or alcohol addiction, illness, unstable sleep, serious problems in life. But these factors are not the root cause of the disease: just from a couple of sleepless nights or a period of lack of money, bipolar disorder does not develop.
Myth 8. The only way to help people with bipolar disorder is through medication.
Medications, such as antipsychotics and mood stabilizers, can actually Bipolar Disorder / Johns Hopkins Medicine ease the illness so that the person can control mania and depression. For each patient, the specialist selects an individual treatment regimen. Sometimes you need to test several drug combinations to find the right one.
But besides medication, there are Bipolar Disorder / National Institute of Mental Health and other ways to cope with the symptoms of episodes of the disease:
- Psychotherapy. It helps to understand the nature of emotions, thoughts, changes in behavior and learn how to keep them under control.
- Find support from loved ones. Friends, relatives and partners can monitor a person's regimen, offer him various useful activities, and spend time together.
- Lead a healthy lifestyle.
 Proper nutrition, regular exercise and good sleep have a positive effect on overall health and brain function in particular.
Proper nutrition, regular exercise and good sleep have a positive effect on overall health and brain function in particular.
However, none of these methods can guarantee complete relief from the disorder. Bipolar Disorder / National Institute of Mental Health, people with bipolar disorder usually face lifelong manifestations of the disease. But properly selected drug therapy and a combination of different ways to deal with the disorder can help achieve a stable remission. In this state, a person with BAD is able to work calmly, make friends, have romantic relationships, enjoy entertainment - in a word, live a full life.
Tests, Questionnaires and Worksheets - Mental Health Center
1. Which of the following substances have you ever tried in your life? (not prescribed by a doctor)
Nicotine (tobacco, electronic cigarettes)(0) No(1) Yes
Alcoholic products (beer, wine, alcohol)(0) No(1) Yes
Cannabis (marijuana, hashish)(0) No(1 ) Yes
Cocaine (coca, crack)(0) No(1) Yes
Amphetamine-type stimulants (diet pills, speed, ecstasy, etc.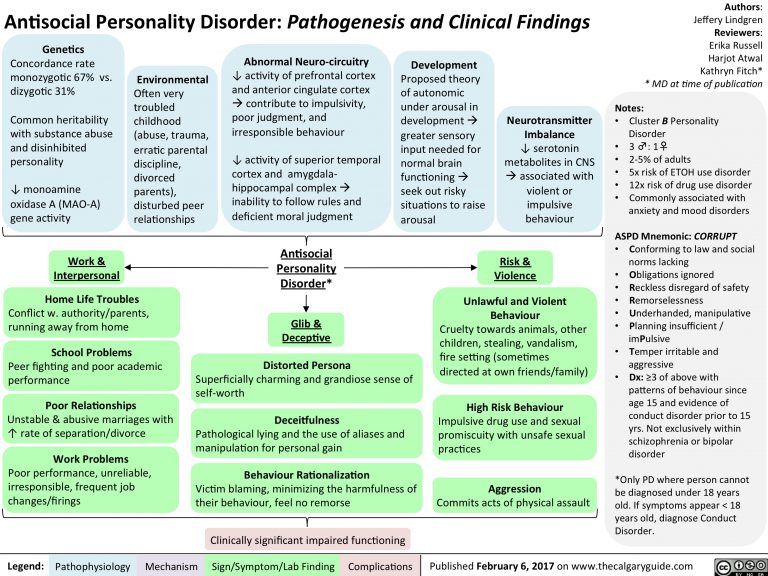 )(0) No(1) Yes
)(0) No(1) Yes
Inhalants (glue, gasoline, thinner)(0) No(1) Yes
Sedatives and hypnotics (Corvalol, Xanax, Relanium phenazepam, etc.)(0) No(1) Yes
Hallucinogens (LSD, acid , mushrooms, ketamine, etc.)(0) No(1) Yes
Opioids (heroin, morphine, methadone, codeine, etc.)(0) No(1) Yes
Other psychoactive substances(0) No(1 ) Yes
2. In the past three months, how often have you used the following types of substances?
Nicotine (tobacco, electronic cigarettes)(0) Never(2) 1-2 times(3) Monthly(4) Weekly(6) Nearly every day
Alcoholic products (beer, wine, alcohol)(0) Never(2) 1-2 times(3) Every month(4) Every week(6) Almost every day
Cannabis (marijuana, hashish)(0) Never(2) 1-2 times(3) Monthly(4) Weekly(6) Almost every day
Cocaine (coca, crack)(0) Never(2) 1-2 times(3) Monthly (4) Every week(6) Almost every day
Amphetamine-type stimulants (speed, diet pills, ecstasy, etc.)(0) Never(2) 1-2 times(3) Every month(4) Every week (6) Almost every day
Inhalants (glue, gasoline, thinner)(0) Never(2) 1-2 times(3) Monthly(4) Weekly(6) Almost every day
Sedatives and hypnotics (Corvalol, Xanax, Relanium phenazepam, etc.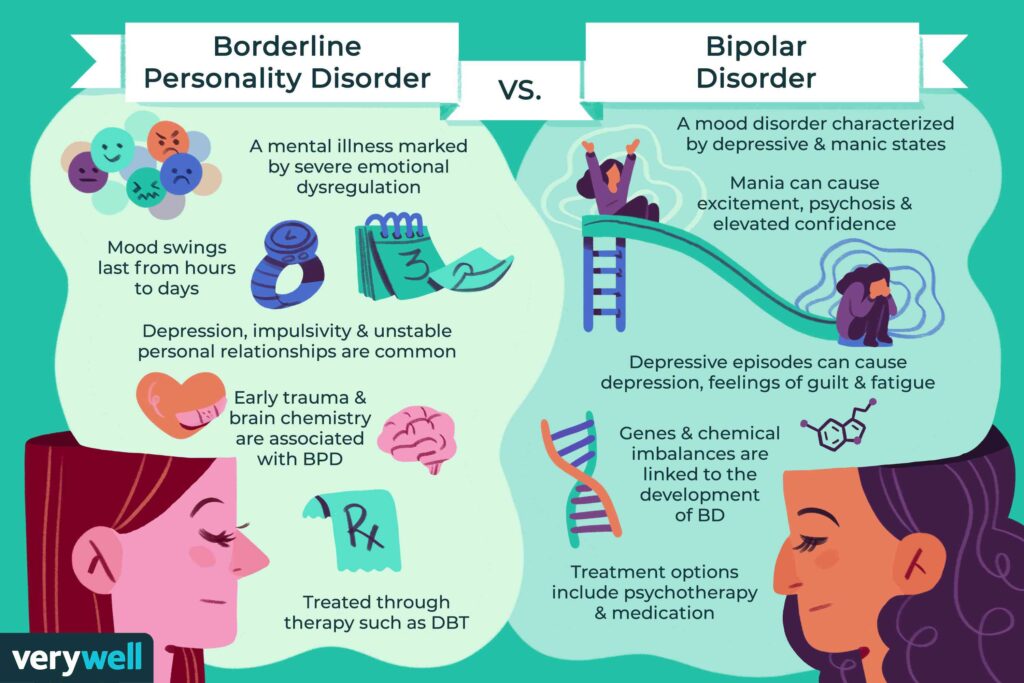 )(0) Never(2) 1-2 times(3) Every month(4) Every week(6) Almost every day
)(0) Never(2) 1-2 times(3) Every month(4) Every week(6) Almost every day
Hallucinogens (LSD, acid, mushrooms, ketamine, etc.)(0 ) Never(2) 1-2 times(3) Monthly(4) Weekly(6) Nearly every day
Opioids (heroin, morphine, methadone, codeine, etc.)(0) Never(2) 1 -2 times(3) Every month(4) Every week(6) Almost every day
Other psychoactive substances(0) Never(2) 1-2 times(3) Monthly(4) Weekly(6) Almost every day
3. In the past three months, how often have you had a strong desire or craving for the following substances?
Nicotine (tobacco, electronic cigarettes)(0) Never(3) 1-2 times(4) Monthly(5) Weekly(6) Almost every day
Alcoholic products (beer, wine, alcohol)(0 ) Never(3) 1-2 times(4) Every month(5) Every week(6) Almost every day
Cannabis (marijuana, hashish)(0) Never(3) 1-2 times(4) Every month(5) Every week(6) Almost every day
Cocaine (coca, crack)(0) Never( 3) 1-2 times(4) Monthly(5) Weekly(6) Almost every day
Amphetamine-type stimulants (speed, diet pills, ecstasy, etc. )(0) Never(3) 1-2 times(4) Monthly(5) Weekly(6) Almost every day
)(0) Never(3) 1-2 times(4) Monthly(5) Weekly(6) Almost every day
Inhalants (glue, gasoline, thinner)(0) Never(3) 1-2 times(4) Monthly(5) Weekly( 6) Almost every day
Sedatives and hypnotics (Corvalol, Xanax, Relanium phenazepam, etc.)(0) Never(3) 1-2 times(4) Monthly(5) Weekly(6) Almost every day
Hallucinogens (LSD , acid, mushrooms, ketamine, etc.)(0) Never(3) 1-2 times(4) Monthly(5) Weekly(6) Nearly every day
Opioids (heroin, morphine, methadone, codeine and etc.)(0) Never(3) 1-2 times(4) Every month(5) Every week(6) Almost every day
Other psychoactive substances(0) Never(3) 1-2 times(4 ) Every month(5) Every week(6) Almost every day
4. During the past three months, how often did the use of the following substances lead to legal, financial, health, or relationship problems?
Nicotine (tobacco, electronic cigarettes)(0) Never(4) 1-2 times(5) Monthly(6) Weekly(7) Almost every day
Alcoholic products (beer, wine, alcohol)(0 ) Never(4) 1-2 times(5) Every month(6) Every week(7) Almost every day
Cannabis (marijuana, hashish)(0) Never(4) 1-2 times(5) Every Monthly(6) Weekly(7) Almost every day
Cocaine (coca, crack)(0) Never(4) 1-2 times(5) Monthly(6) Weekly(7) Almost every day
Amphetamine-type stimulants (speed, diet pills, ecstasy and etc. )(0) Never(4) 1-2 times(5) Every month(6) Every week(7) Almost every day
)(0) Never(4) 1-2 times(5) Every month(6) Every week(7) Almost every day
Inhalants (glue, gasoline, thinner)(0) Never(4) 1 -2 times(5) Every month(6) Every week(7) Almost every day
Sedatives and hypnotics (Corvalol, Xanax, Relanium phenazepam, etc.)(0) Never(4) 1-2 times(5 ) Every month(6) Every week(7) Almost every day
Hallucinogens (LSD, acid, mushrooms, ketamine, etc.)(0) Never(4) 1-2 times(5) Monthly(6) Weekly(7) Almost every day
Opioids (heroin, morphine) , methadone, codeine, etc.)(0) Never(4) 1-2 times(5) Every month(6) Every week(7) Almost every day
Other psychoactive substances(0) Never(4) 1 -2 times(5) Every month(6) Every week(7) Almost every day
5. In the past three months, how often have you given up on planned or regular activities because of your use?
Nicotine (tobacco, electronic cigarettes)(0) Never(5) 1-2 times(6) Monthly(7) Weekly(8) Almost every day
Alcoholic products (beer, wine, alcohol)(0 ) Never(5) 1-2 times(6) Monthly(7) Weekly(8) Almost every day
Cannabis (marijuana, hashish)(0) Never(5) 1-2 times(6) Every Monthly(7) Weekly(8) Almost every day
Cocaine (coca, crack)(0) Never(5) 1-2 times(6) Monthly(7) Weekly(8) Almost every day
Amphetamine-type stimulants (speed, diet pills, ecstasy, etc.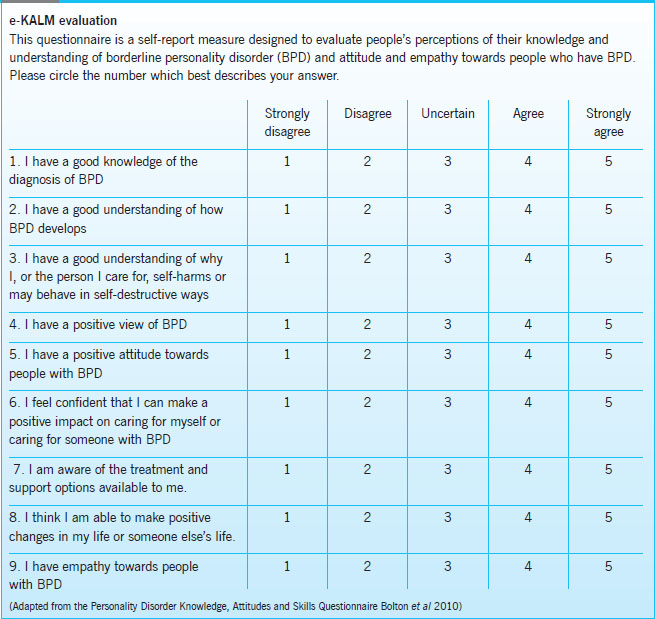 )(0) Never(5) 1-2 times(6) Monthly(7) Weekly(8) Nearly every day
)(0) Never(5) 1-2 times(6) Monthly(7) Weekly(8) Nearly every day
Inhalants (glue, gasoline, thinner)(0) Never(5) 1-2 times(6) Monthly(7) Weekly(8) Almost every day
0) Never(5) 1-2 times(6) Monthly(7) Weekly(8) Almost every day
Hallucinogens (LSD, acid, mushrooms, ketamine, etc.)(0) Never(5) 1-2 times(6) Every month(7) Every week(8) Almost every day
Opioids (heroin, morphine, methadone, codeine, etc.)(0) Never(5) 1-2 times(6) Monthly(7) Weekly(8) Almost every day
Other psychoactive substances(0 ) Never(5) 1-2 times(6) Monthly(7) Weekly(8) Almost every day
6. Has anyone expressed concern to you about what you used?
Nicotine (tobacco, electronic cigarettes)(0) Never(6) Yes, within the last 3 months(3) Yes, but not within the last 3 months
Alcoholic products (beer, wine, spirits)(0) Never(6) Yes, within the last 3 months(3) Yes, but not within the last 3 months
Cannabis (marijuana, hashish)(0) Never( 6) Yes, within the past 3 months(3) Yes, but not within the past 3 months
Cocaine (coca, crack)(0) Never(6) Yes, within the past 3 months(3) Yes, but not within the past 3 months
Amphetamine-type stimulants (speed, diet pills, ecstasy, etc.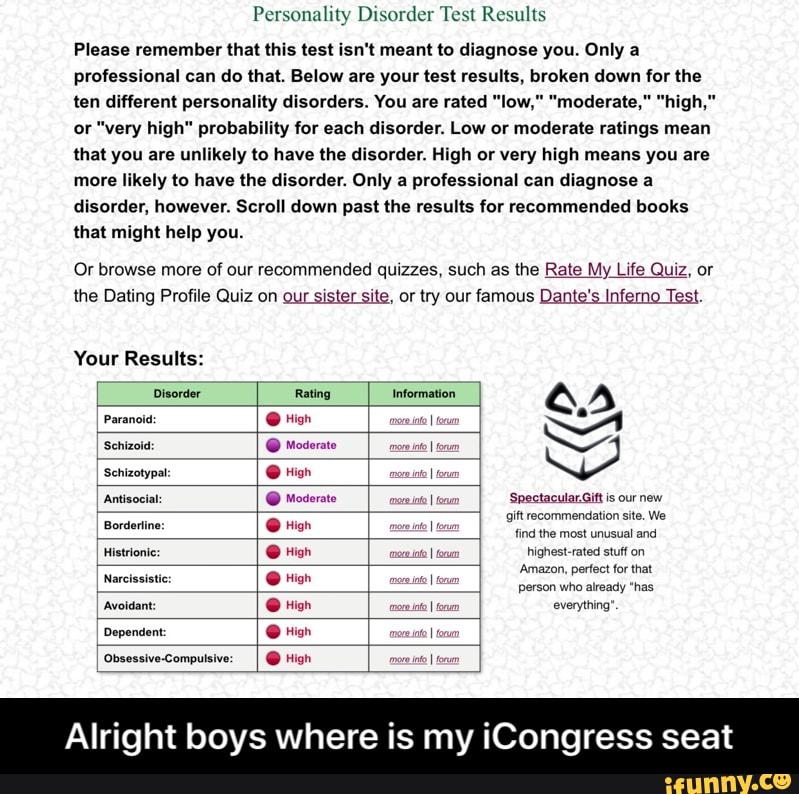 )(0) Never(6) Yes, within the past 3 months(3) Yes, but not within the past 3 months
)(0) Never(6) Yes, within the past 3 months(3) Yes, but not within the past 3 months
Inhalants (glue, gasoline, thinner)(0) Never(6) Yes, within the past 3 months(3) Yes, but not within the past 3 months
Sedatives and hypnotics (Corvalol, Xanax, Relanium etc.)(0) Never(6) Yes, in the last 3 months(3) Yes, but not in the last 3 months
Hallucinogens (LSD, acid, mushrooms, ketamine, etc.)(0) Never(6 ) Yes, within the last 3 months(3) Yes, but not within the last 3 months
Opioids (heroin, morphine, methadone, codeine, etc.)(0) Never(6) Yes, within the last 3 months(3) Yes, but not within the last 3 months
Other psychoactive substances(0) Never( 6) Yes, within the last 3 months(3) Yes, but not within the last 3 months
7. Have you ever tried to control your use and failed?
Nicotine (tobacco, electronic cigarettes)(0) Never(6) Yes, within the last 3 months(3) Yes, but not within the last 3 months
Alcoholic products (beer, wine, spirits)(0) Never(6) Yes, within the last 3 months(3) Yes, but not within the last 3 months
Cannabis (marijuana, hashish)(0) Never( 6) Yes, within the past 3 months(3) Yes, but not within the past 3 months
Cocaine (coca, crack)(0) Never(6) Yes, within the past 3 months(3) Yes, but not within the past 3 months
Amphetamine-type stimulants (speed, diet pills, ecstasy, etc.