Ocd medicine treatment
International OCD Foundation | Medications for OCD
PLEASE NOTE: The International OCD Foundation has no conflicts of interest or financial relationships related to the content of this web page.The following information refers to OCD medications in adults. For information on medication in children, click here.
Overview
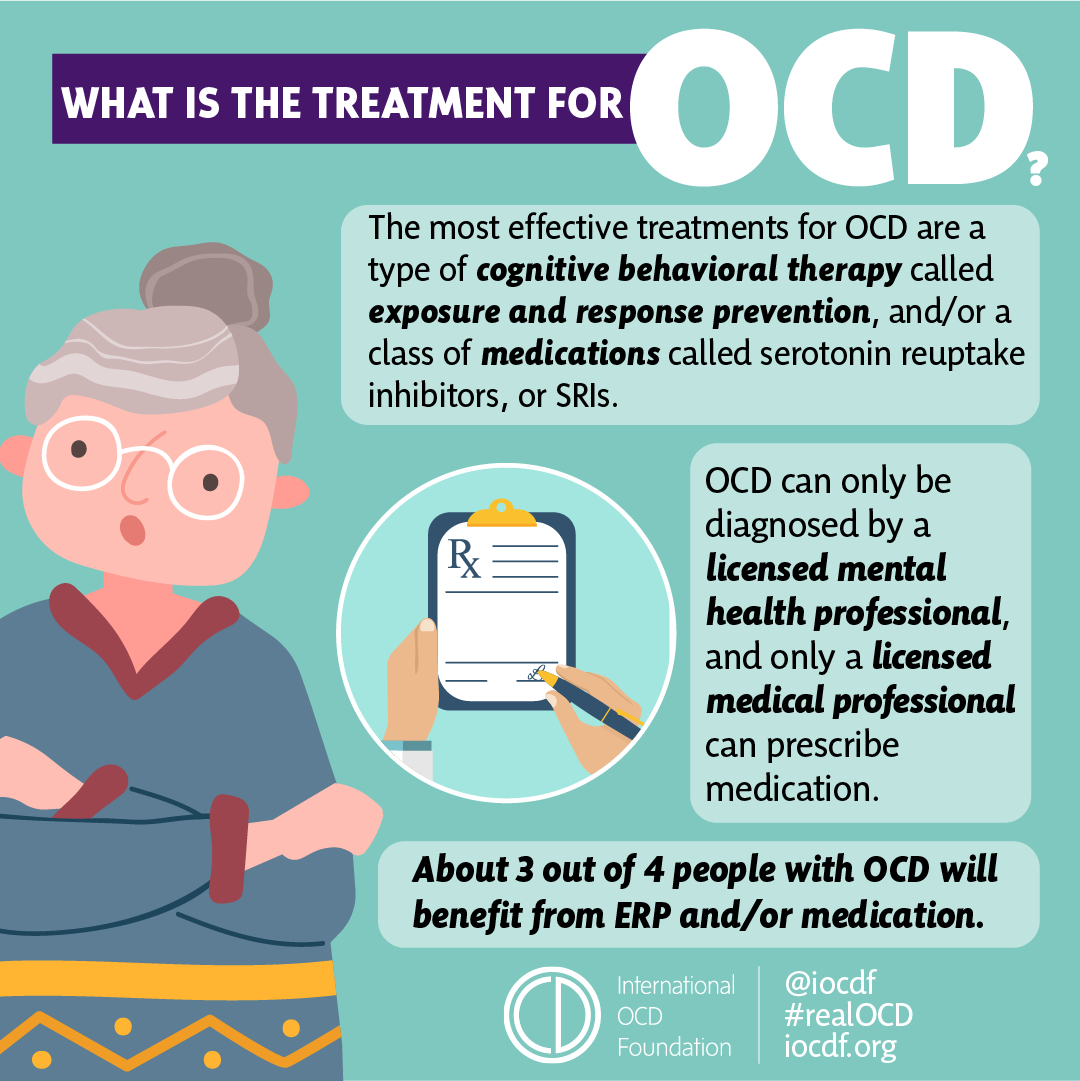
- Medication is an effective treatment for OCD.
- About 7 out of 10 people with OCD will benefit from either medication or Exposure and Response Prevention (ERP). For the people who benefit from medication, they usually see their OCD symptoms reduced by 40-60%.
- For medications to work, they must be taken regularly and as directed by their doctor. About half of OCD patients stop taking their medication due to side effects or for other reasons. If you experience side effects, you should bring this up with your doctor so they can help you address them. They may be able to change your dose or find a different type of SRI that your system better tolerates.
What kinds of medications may help OCD?
The types of medication that research has shown to be most effective for OCD are a type of drug called a Serotonin Reuptake Inhibitor (SRI), which are traditionally used as an antidepressants, but also help to address OCD symptoms. (Note: Depression can sometimes result from OCD, and doctors can treat both the OCD and depression with the same medication.)
Do all antidepressants help OCD symptoms?
No! Some commonly used antidepressants have almost no effect whatsoever on OCD symptoms. Drugs, such as imipramine (Tofranil®) or amitriptyline (Elavil®), that are good antidepressants, rarely improve OCD symptoms.
Which Medications Help OCD?
The following antidepressants have been found to work well for OCD in research studies:
|
|
|
|
|
|
|
|
Have These Drugs Been Tested?
Anafranil has been around the longest and is the best-studied OCD medication.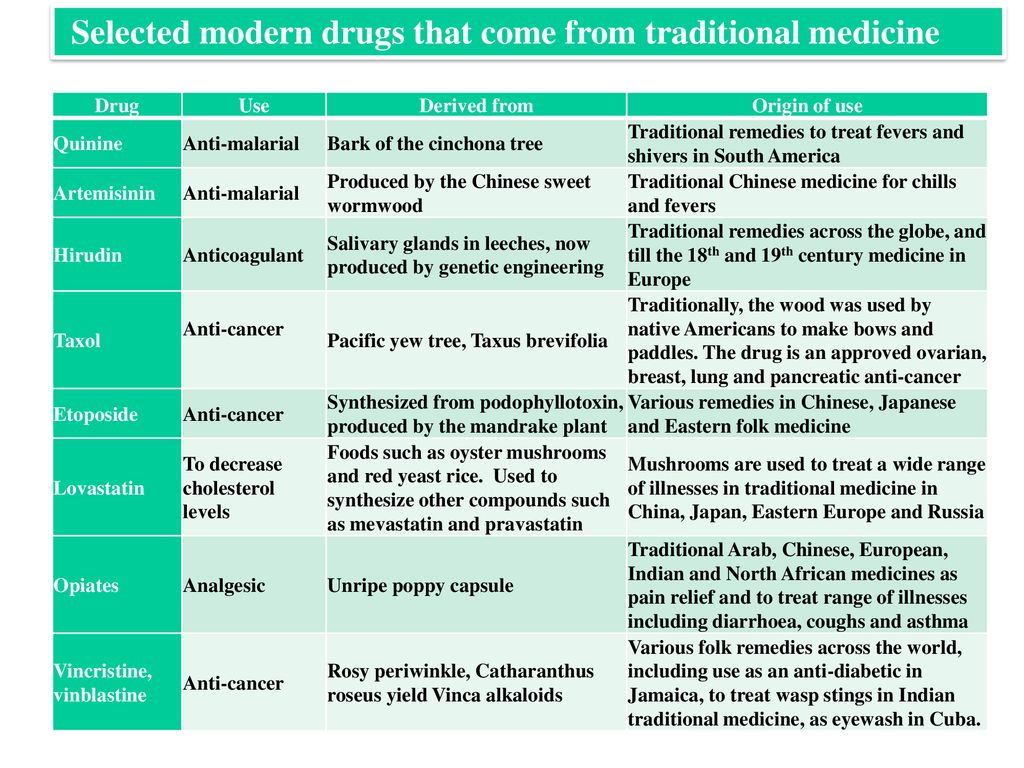 There is growing evidence that the other drugs are as effective. In addition to these carefully studied drugs, there are hundreds of case reports of other drugs being helpful. For example, duloxetine (Cymbalta®) has been reported to help OCD patients who have not responded to these other medications.
There is growing evidence that the other drugs are as effective. In addition to these carefully studied drugs, there are hundreds of case reports of other drugs being helpful. For example, duloxetine (Cymbalta®) has been reported to help OCD patients who have not responded to these other medications.
What Are the Usual Doses for These Drugs?
High doses are often needed for these drugs to work in most people.* Studies suggest that the following doses may be needed:
|
|
|
|
|
|
|
|
Which Drug Should Someone Try First?
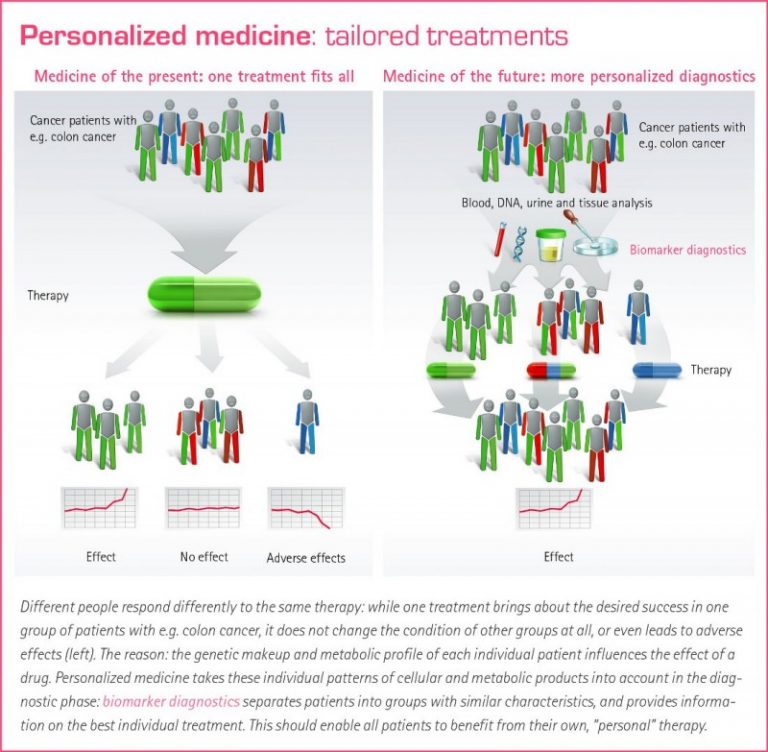
Whenever any of the above drugs have been studied head to head, there seems to be no significant difference in how well they work. However, for any given patient, one drug may be very effective, and the others may not. The only way to tell which drug will be the most helpful with the least side effects is to try each drug for about 3 months. Remember! It is important not to give up after failing one or two drugs. Drugs work very differently for each person.
However, for any given patient, one drug may be very effective, and the others may not. The only way to tell which drug will be the most helpful with the least side effects is to try each drug for about 3 months. Remember! It is important not to give up after failing one or two drugs. Drugs work very differently for each person.
How Do These Medications Work?
It remains unclear as to how these particular drugs help OCD. The good news is that after decades of research, we know how to treat patients, even though we do not know exactly why our treatments work.
We do know that each of these medications affect a chemical in the brain called serotonin. Serotonin is used by the brain as a messenger. If your brain does not have enough serotonin, then your the nerves in your brain might not be communicating right. Adding these medications to your body can help boost your serotonin and get your brain back on track.
Are There Side Effects?- Yes.
 Most patients will experience one or more side effects from all of the medications listed above.
Most patients will experience one or more side effects from all of the medications listed above. - The patient and doctor must weigh the benefits of the drug against the side effects.
- It is important for the patient to be open about problems that may be caused by the medication. Sometimes an adjustment in dose or a switch in the time of day it is taken is all that is needed.
Who Should Not Take These Medications?
- Women who are pregnant or are breastfeeding should weigh the decision to take these drugs with their doctor. If severe OCD cannot be controlled any other way, research has indicated that these medications seem to be safe. Many pregnant women have taken them without difficulty. Some OCD patients choose to use exposure and response prevention (ERP) to minimize medication use during the first or last trimester of pregnancy. Click here to read more about the benefits and risks of using SRIs during pregancy and/or while breastfeeding.
- Very elderly patients should avoid Anafranil as the first drug tried, since it has side effects that can interfere with thinking and can cause or worsen confusion.

- Patients with heart problems should use special caution if taking Anafranil.
What if I cannot take even the smallest pill size of the medication?
Some patients are sensitive to these medications and can’t stand the effects that come with even the lowest dose. However, patients can start at very low doses (for example, 1-2 mg per day) and very slowly increase the dose. For most people, they will eventually be able to handle the medication at its normal dose.
Ask your doctor if you can try a lower dose by breaking pills in half or using a liquid form of medication to slowly increase your doses.
ALWAYS be sure to talk to your doctor before making any changes to the way you take your medications!
The following is one example as told by Dr. Michael Jenike:
“One woman, who was started on Prozac 20 mg/day, complained of bothersome side effects such as increased anxiety, shakiness, and terrible insomnia. She felt it made her OCD worse.
She had horrible side effects from even 12.5 mg of Anafranil, and later with low dosages of Paxil and Zoloft. She requested to start 1-2 mg/day of liquid Prozac, because she heard it was good from other patients that she met from a computer bulletin board. She felt no side effects, and over a period of a few weeks, she got up to 20 mg/day without the previous side effects that she had felt on this dose in the past. Under the supervision of her doctor, she continued to increase the Prozac to 60 mg/day over a couple more months. Her OCD gradually improved quite dramatically.”
Should I Take These Medications Only When I Am Feeling Stressed?
No. This is a common mistake. These medications are meant to be taken every day to keep your serotonin at a constant level. They are not taken like typical anti-anxiety meds, when you feel upset or anxious. It is best not to miss doses if possible. However, if you do miss a dose here or there, it is unlikely that any bad effect on OCD will occur. In fact, sometimes your doctor might tell you to skip doses to help manage troublesome side effects, like sexual problems.
In fact, sometimes your doctor might tell you to skip doses to help manage troublesome side effects, like sexual problems.
What Kind of Doctor Should I Look For to Prescribe These Medications?
Although any licensed physician can legally prescribe these drugs, it is probably best to deal directly with a board-certified psychiatrist who understands OCD. It is important to find a psychiatrist who has special knowledge about the use of drugs to treat mental health disorders. Click here to find a psychiatrist in your area. (Look for therapists with an MD or DO after their name.)
What If I am Afraid to Take My Medication Because I Have an Obsessional Fear About Drugs?
Usually with help from a doctor that you trust, your fears can be overcome. If you have fears about taking medication, ERP can be started first and part of the therapy can focus on these fears of medications.
How Long Does it Take for These Medications to Work?
It is important not to give up on a medication until you have been taking it as prescribed for 10 to 12 weeks.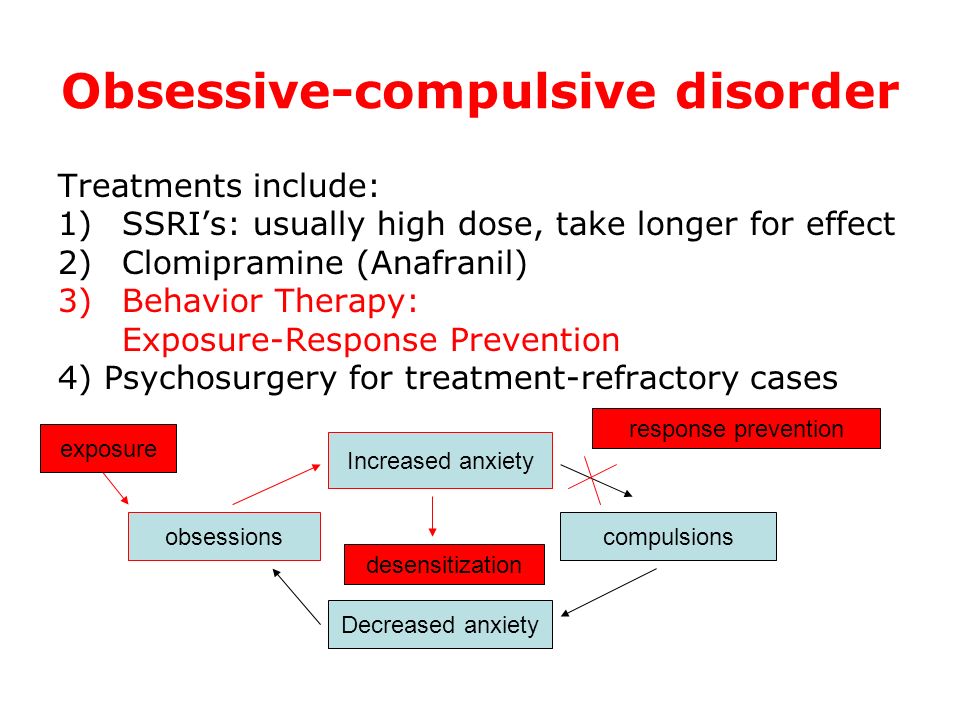 Many patients feel no positive effects for the first few weeks of treatment but then improve greatly.
Many patients feel no positive effects for the first few weeks of treatment but then improve greatly.
Will I Have to Take Medications Forever?
No one knows how long patients should take these medications once they have been effective. Some patients are able to stop their medications after a 6 to 12-month treatment period. It does appear that over half of OCD patients (and maybe many more) will need to be on at least a low dose of medication for years, perhaps even for life. It seems likely that the risk of relapse is lower if patients learn to use behavior therapy techniques while they are doing well on medications. And if medication is tapered slowly (even over several months), the ERP treatment may enable patients to control any symptoms that return when they stop taking the medication.
After medications are stopped, symptoms do not return immediately; they may start to return within a few weeks to a few months. If OCD symptoms return after a medication is stopped, most patients will have a good response if the medication is restarted.
Can I Drink Alcohol While on These Medications?
Many patients drink alcohol while on these medications and handle it well, but be sure to ask your doctor or pharmacist if it is safe. It is important to keep in mind that alcohol may have a greater effect on individuals who are taking these medications; one drink could affect an individual as if it were two drinks. Also, alcohol may limit some of the medications’ benefits, so it may be wise to try not to drink alcohol during the first couple of months after starting any new medication.
Do I Need Other Treatments Too?
Most psychiatrists and therapists believe that combining a type of Cognitive Behavior Therapy (CBT), specifically Exposure and Response Prevention (ERP), and medication is the most effective approach.
What if I Can’t Afford My Medication?
Drug companies give doctors free samples of some medications. Doctors give these samples to patients who cannot afford the cost of the medications.
Most drug companies also have programs that help patients get these and other medications free or at a reduced cost. For more information, visit: www.pparx.org or call 1-888-477-2669.
By Michael Jenike, MD
Chair, International OCD Foundation’s Scientific Advisory Board
Harvard Medical School
* The FDA has issued some warnings on the use of this medication in higher doses. Please check with your physician.
Obsessive-compulsive disorder (OCD) - Diagnosis and treatment
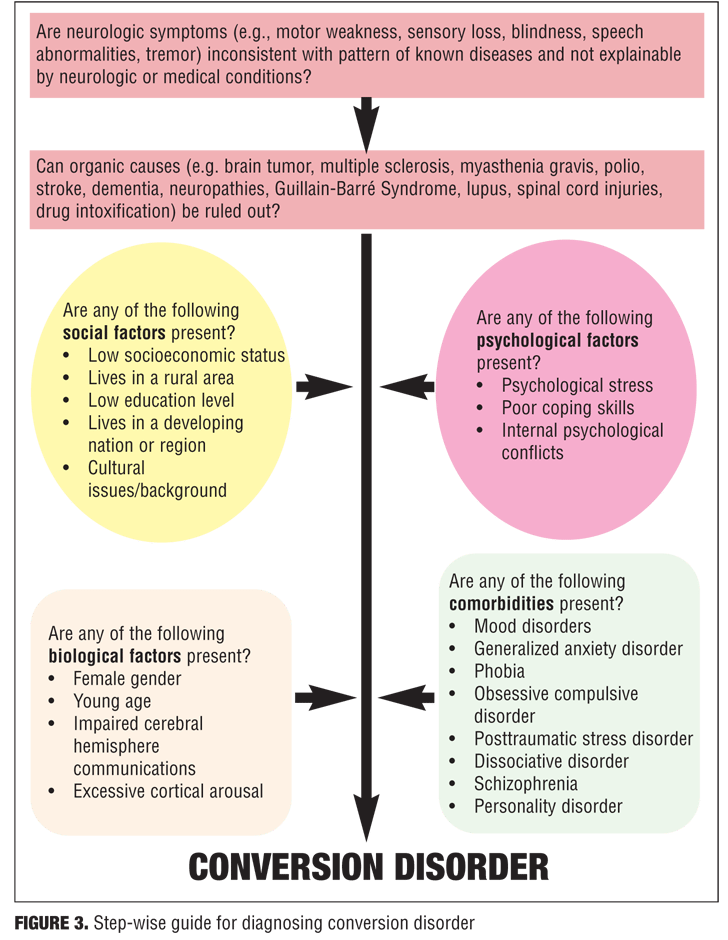
Diagnosis
Steps to help diagnose obsessive-compulsive disorder may include:
- Psychological evaluation. This includes discussing your thoughts, feelings, symptoms and behavior patterns to determine if you have obsessions or compulsive behaviors that interfere with your quality of life. With your permission, this may include talking to your family or friends.
- Diagnostic criteria for OCD.
 Your doctor may use criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
Your doctor may use criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association. - Physical exam. This may be done to help rule out other problems that could be causing your symptoms and to check for any related complications.
Diagnostic challenges
It's sometimes difficult to diagnose OCD because symptoms can be similar to those of obsessive-compulsive personality disorder, anxiety disorders, depression, schizophrenia or other mental health disorders. And it's possible to have both OCD and another mental health disorder. Work with your doctor so that you can get the appropriate diagnosis and treatment.
Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your Obsessive-compulsive disorder (OCD)-related health concerns Start Here
Treatment
Obsessive-compulsive disorder treatment may not result in a cure, but it can help bring symptoms under control so that they don't rule your daily life.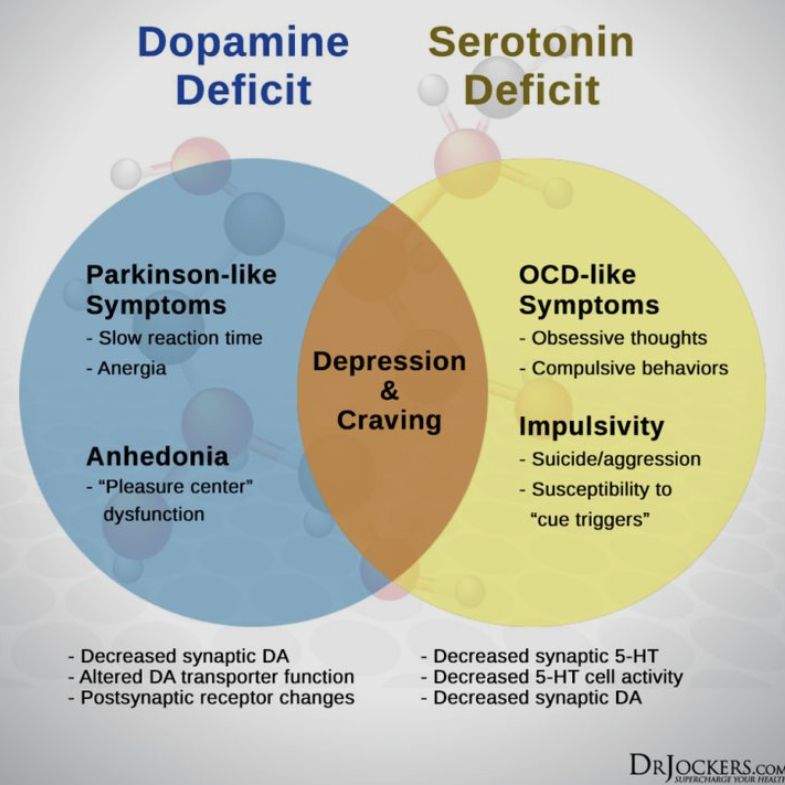 Depending on the severity of OCD, some people may need long-term, ongoing or more intensive treatment.
Depending on the severity of OCD, some people may need long-term, ongoing or more intensive treatment.
The two main treatments for OCD are psychotherapy and medications. Often, treatment is most effective with a combination of these.
Psychotherapy
Cognitive behavioral therapy (CBT), a type of psychotherapy, is effective for many people with OCD. Exposure and response prevention (ERP), a component of CBT therapy, involves gradually exposing you to a feared object or obsession, such as dirt, and having you learn ways to resist the urge to do your compulsive rituals. ERP takes effort and practice, but you may enjoy a better quality of life once you learn to manage your obsessions and compulsions.
Medications
Certain psychiatric medications can help control the obsessions and compulsions of OCD.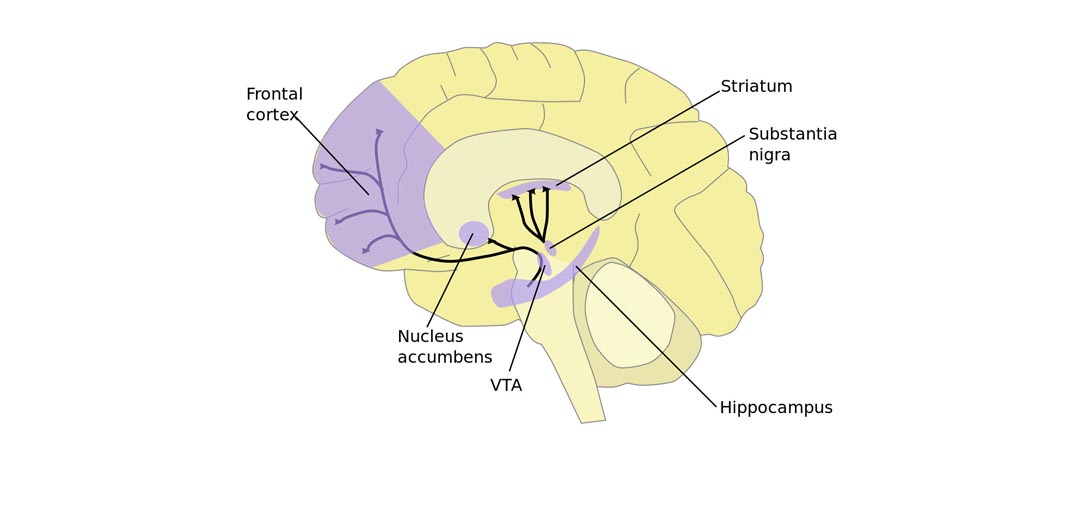 Most commonly, antidepressants are tried first.
Most commonly, antidepressants are tried first.
Antidepressants approved by the U.S. Food and Drug Administration (FDA) to treat OCD include:
- Clomipramine (Anafranil) for adults and children 10 years and older
- Fluoxetine (Prozac) for adults and children 7 years and older
- Fluvoxamine for adults and children 8 years and older
- Paroxetine (Paxil, Pexeva) for adults only
- Sertraline (Zoloft) for adults and children 6 years and older
However, your doctor may prescribe other antidepressants and psychiatric medications.
Medications: What to consider
Here are some issues to discuss with your doctor about medications for OCD:
- Choosing a medication. In general, the goal is to effectively control symptoms at the lowest possible dosage. It's not unusual to try several drugs before finding one that works well.
 Your doctor might recommend more than one medication to effectively manage your symptoms. It can take weeks to months after starting a medication to notice an improvement in symptoms.
Your doctor might recommend more than one medication to effectively manage your symptoms. It can take weeks to months after starting a medication to notice an improvement in symptoms. - Side effects. All psychiatric medications have potential side effects. Talk to your doctor about possible side effects and about any health monitoring needed while taking psychiatric drugs. And let your doctor know if you experience troubling side effects.
- Suicide risk. Most antidepressants are generally safe, but the FDA requires that all antidepressants carry black box warnings, the strictest warnings for prescriptions. In some cases, children, teenagers and young adults under 25 may have an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed. If suicidal thoughts occur, immediately contact your doctor or get emergency help.
 Keep in mind that antidepressants are more likely to reduce suicide risk in the long run by improving mood.
Keep in mind that antidepressants are more likely to reduce suicide risk in the long run by improving mood. - Interactions with other substances. When taking an antidepressant, tell your doctor about any other prescription or over-the-counter medications, herbs or other supplements you take. Some antidepressants can make some other medications less effective and cause dangerous reactions when combined with certain medications or herbal supplements.
- Stopping antidepressants. Antidepressants aren't considered addictive, but sometimes physical dependence (which is different from addiction) can occur. So stopping treatment abruptly or missing several doses can cause withdrawal-like symptoms, sometimes called discontinuation syndrome. Don't stop taking your medication without talking to your doctor, even if you're feeling better — you may have a relapse of OCD symptoms. Work with your doctor to gradually and safely decrease your dose.
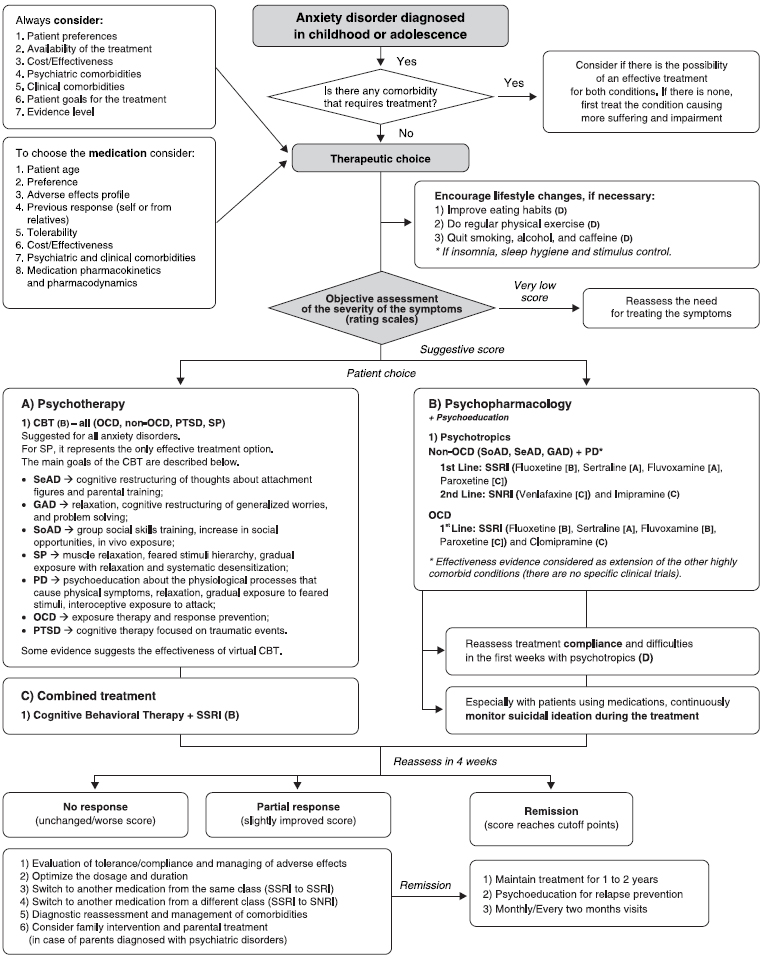
Talk to your doctor about the risks and benefits of using specific medications.
Other treatment
Sometimes, psychotherapy and medications aren't effective enough to control OCD symptoms. In treatment-resistant cases, other options may be offered:
- Intensive outpatient and residential treatment programs. Comprehensive treatment programs that emphasize ERP therapy principles may be helpful for people with OCD who struggle with being able to function because of the severity of their symptoms. These programs typically last several weeks.
- Deep brain stimulation (DBS). DBS is approved by the FDA to treat OCD in adults age 18 years and older who don't respond to traditional treatment approaches.
 DBS involves implanting electrodes within certain areas of your brain. These electrodes produce electrical impulses that may help regulate abnormal impulses.
DBS involves implanting electrodes within certain areas of your brain. These electrodes produce electrical impulses that may help regulate abnormal impulses. - Transcranial magnetic stimulation (TMS). The FDA approved a specific device (BrainsWay Deep Transcranial Magnetic Stimulation) to treat OCD in adults ages 22 to 68 years, when traditional treatment approaches have not been effective. TMS is a noninvasive procedure that uses magnetic fields to stimulate nerve cells in the brain to improve symptoms of OCD. During a TMS session, an electromagnetic coil is placed against your scalp near your forehead. The electromagnet delivers a magnetic pulse that stimulates nerve cells in your brain.

Talk with your doctor to make sure you understand all the pros and cons and possible health risks of DBS and TMS if you're considering one of these procedures.
More Information
- Obsessive-compulsive disorder (OCD) care at Mayo Clinic
- Cognitive behavioral therapy
- Deep brain stimulation
- Electroconvulsive therapy (ECT)
- Psychotherapy
- Transcranial magnetic stimulation
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you.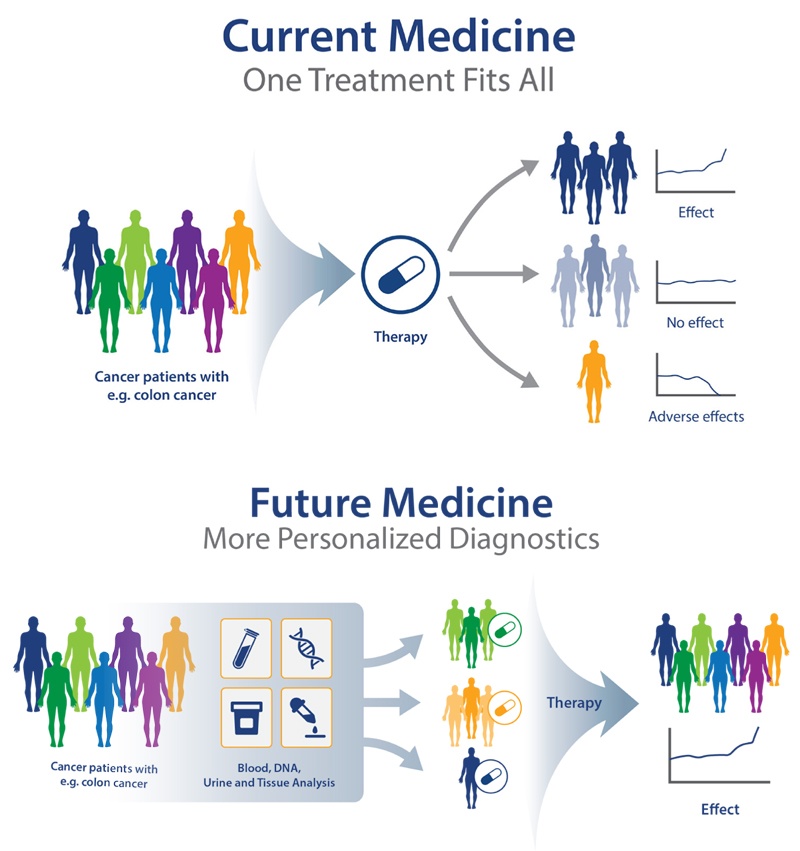 If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Lifestyle and home remedies
Obsessive-compulsive disorder is a chronic condition, which means it may always be part of your life. While OCD warrants treatment by a professional, you can do some things for yourself to build on your treatment plan:
- Practice what you learn. Work with your mental health professional to identify techniques and skills that help manage symptoms, and practice these regularly.

- Take your medications as directed. Even if you're feeling well, resist any temptation to skip your medications. If you stop, OCD symptoms are likely to return.
- Pay attention to warning signs. You and your doctor may have identified issues that can trigger your OCD symptoms. Make a plan so that you know what to do if symptoms return. Contact your doctor or therapist if you notice any changes in symptoms or how you feel.
- Check first before taking other medications. Contact the doctor who's treating you for OCD before you take medications prescribed by another doctor or before taking any over-the-counter medications, vitamins, herbal remedies or other supplements to avoid possible interactions.
Coping and support
Coping with obsessive-compulsive disorder can be challenging. Medications can have unwanted side effects, and you may feel embarrassed or angry about having a condition that requires long-term treatment. Here are some ways to help cope with OCD:
Medications can have unwanted side effects, and you may feel embarrassed or angry about having a condition that requires long-term treatment. Here are some ways to help cope with OCD:
- Learn about OCD. Learning about your condition can empower you and motivate you to stick to your treatment plan.
- Stay focused on your goals. Keep your recovery goals in mind and remember that recovery from OCD is an ongoing process.
- Join a support group. Reaching out to others facing similar challenges can provide you with support and help you cope with challenges.
- Find healthy outlets. Explore healthy ways to channel your energy, such as hobbies and recreational activities. Exercise regularly, eat a healthy diet and get adequate sleep.
- Learn relaxation and stress management.
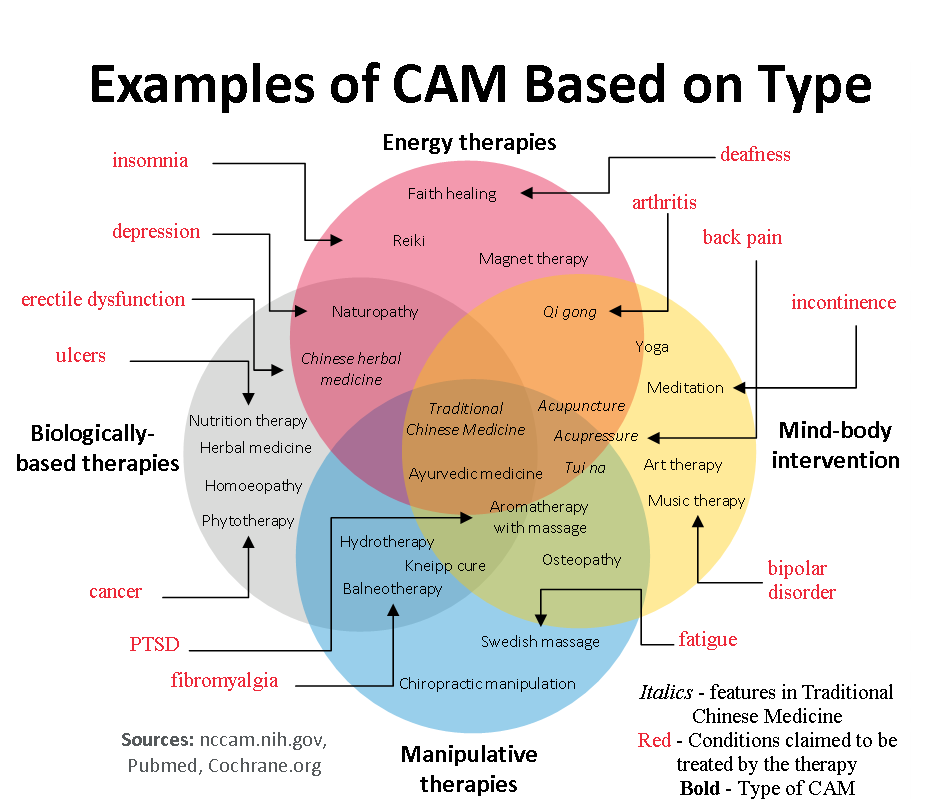
 In addition to professional treatment, stress management techniques such as meditation, visualization, muscle relaxation, massage, deep breathing, yoga or tai chi may help ease stress and anxiety.
In addition to professional treatment, stress management techniques such as meditation, visualization, muscle relaxation, massage, deep breathing, yoga or tai chi may help ease stress and anxiety. - Stick with your regular activities. Try not to avoid meaningful activities. Go to work or school as you usually would. Spend time with family and friends. Don't let OCD get in the way of your life.
Preparing for your appointment
You may start by seeing your primary doctor. Because obsessive-compulsive disorder often requires specialized care, you may be referred to a mental health professional, such as a psychiatrist or psychologist, for evaluation and treatment.
What you can do
To prepare for your appointment, think about your needs and goals for treatment. Make a list of:
- Any symptoms you've noticed, including the types of obsessions and compulsions youꞌve experienced and things that you may be avoiding because of your distress
- Key personal information, including any major stresses, recent life changes and family members with similar symptoms
- All medications, vitamins, herbal remedies or other supplements, as well as the dosages
- Questions to ask your doctor or therapist
Questions to ask might include:
- Do you think I have OCD?
- How do you treat OCD?
- How can treatment help me?
- Are there medications that might help?
- Will exposure and response prevention therapy help?
- How long will treatment take?
- What can I do to help myself?
- Are there any brochures or other printed material that I can have?
- Can you recommend any websites?
Don't hesitate to ask any other questions during your appointment.
What to expect from your doctor
Your doctor is likely to ask you a number of questions, such as:
- Do certain thoughts go through your mind over and over despite your attempts to ignore them?
- Do you have to have things arranged in a certain way?
- Do you have to wash your hands, count things or check things over and over?
- When did your symptoms start?
- Have symptoms been continuous or occasional?
- What, if anything, seems to improve the symptoms?
- What, if anything, appears to worsen the symptoms?
- How do the symptoms affect your daily life? Do you avoid anything because of your symptoms?
- In a typical day, how much time do you spend on obsessive thoughts and compulsive behavior?
- Have any of your relatives had a mental health disorder?
- Have you experienced any trauma or major stress?
Your doctor or mental health professional will ask additional questions based on your responses, symptoms and needs. Preparing and anticipating questions will help you make the most of your appointment time.
Preparing and anticipating questions will help you make the most of your appointment time.
By Mayo Clinic Staff
Related
Associated Procedures
Treatment of obsessive-compulsive disorder
Treatment of obsessive-compulsive disorder. We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
Symptoms of obsessive-compulsive disorder
- Frightening images and drives
- Compulsive acts (rituals)
- Intrusive check of one's own actions
- Fear of trouble, pollution or contamination
- Inexplicable desire to count something
- Excessive organization and pedantry
- Perfectionism in relationships, work and even leisure
- "Stuck", "looping" on one's thoughts
You feel that over time your mood becomes worse: apathy, depression, obsessions increase, and rituals begin to fill all your free time or harm your physical health.
You may have had more than one meeting with psychologists, psychotherapists and psychiatrists.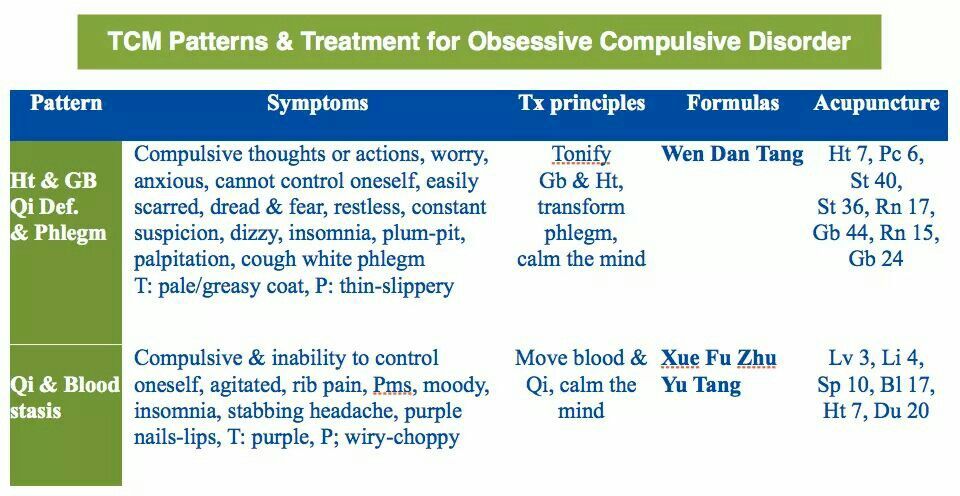 You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
What is obsessive-compulsive disorder?
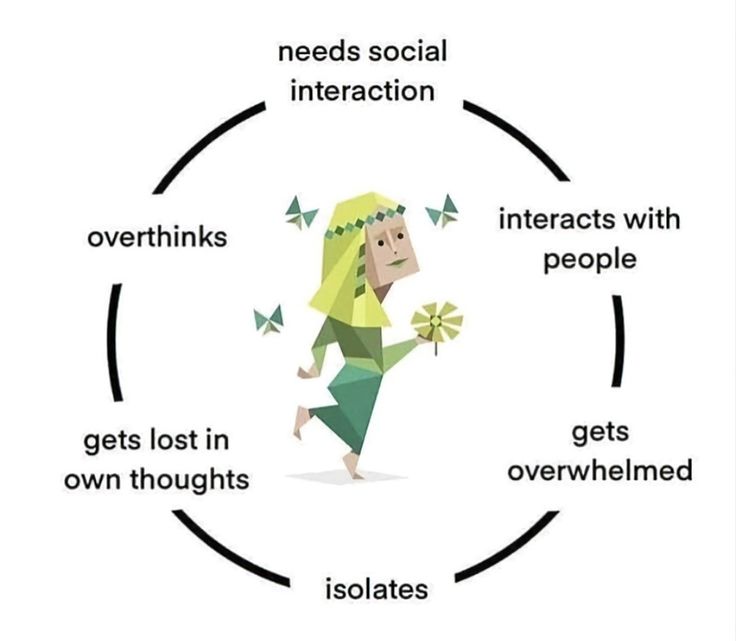
Obsessive-compulsive disorder is a syndrome characterized by the presence of obsessive thoughts (obsessions) to which a person reacts with certain actions (compulsions). The causes of the disorder are rarely superficial. The syndrome is also accompanied by the development of obsessive memories and various pathological phobias. May be chronic, episodic or progressive.
Obsession - obsessive thought, persistent desire for something, uncontrollable and accompanied by anxiety and intense anxiety. In an attempt to cope with such thoughts, a person resorts to committing compulsions.
Compulsion - an irresistible need to perform certain actions (rituals), which can be assessed by the person himself as irrational or meaningless, and the internal need to perform them is forced and is the result of obsessive ideas.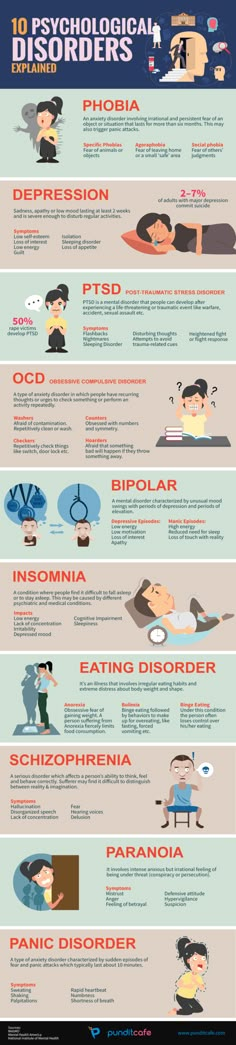
Common examples of OCD manifestations
- An exaggerated sense of danger. Fear of the materiality of thoughts:
- "now I will lose control and hurt my loved ones"
- "something terrible is about to happen, I can feel it"
- "I shouldn't think like that, all this will come true because of me"
- Pathological fear of pollution. Thirst for Purity
- Excessive perfectionism, exaggerated responsibility - "everything must be done perfectly", "everything depends on me, mistakes are unacceptable"
How does this painful algorithm work?
Most people have unwanted or obsessive thoughts quite often, but all sufferers of the disorder greatly exaggerate their importance. Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
As we noted earlier, repetitive avoidance behavior can "get stuck", "loop", that is, have a tendency to repeat. The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
If you periodically experience over the years:
- Constant or fluctuating anxiety
- The need to perform certain ritualized actions
- A persistent decline in the quality of life due to the need to avoid certain thoughts and actions, places and events
And you are also persecuted:
- Significant problems in studies and career
- Failure to establish a serious relationship
- Constant criticism and pressure from relatives
- Many senseless activities
- Excessive involvement in computer games and the Internet, alcohol
- Loneliness and isolation
We strongly recommend that you do not delay seeking help and that you complete a remedial program.
Consultations and psychotherapeutic sessions according to the program are held several times a week, until the relief of severe symptoms, then the frequency of meetings with specialists is reduced to 2–3 per month. Count on the fact that in the end we will deal with your problem together.
Treatment of obsessive-compulsive disorder in Neuro-Psi
Every day, the specialists of the NEURO-PSI clinic analyze the world practice in the field of psychiatry and psychotherapy. The goal is the impartial selection and implementation of those methods of treatment and psychological assistance, the effectiveness of which has been convincingly proven in independent studies.
We are guided by the principles of evidence-based medicine and use as a basic method of treatment a psychotherapeutic paradigm, the effectiveness of which has been widely recognized by the professional community.
1. What is the essence of the obsessive-compulsive disorder treatment program
Since obsessive thoughts, rituals and conditions are only symptoms of mental dysfunction, the root cause must be treated in order to achieve a stable result.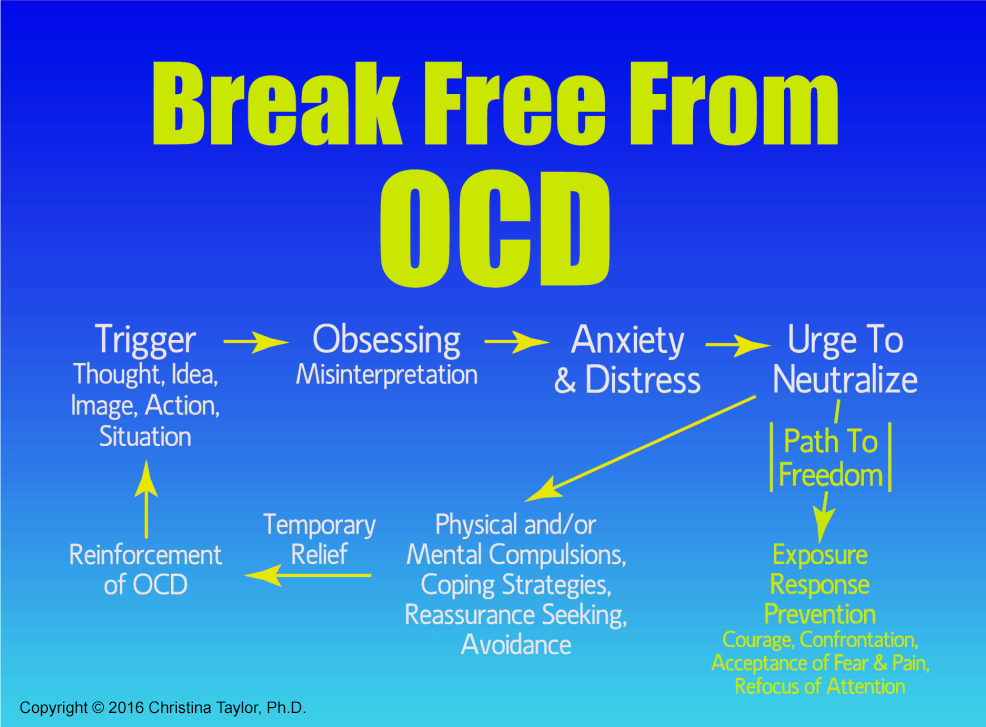 A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
The main emphasis is on teaching the client how to properly respond to his thoughts, emotions, inner feelings and interpretation of external events.
All types of psychotherapeutic and drug treatments serve the same goal: to achieve the best result in the shortest possible time. At the same time, by coordinating the efforts of specialists in various fields, the most complete coverage of all types of mental illnesses, disorders and disorders is possible.
2. What treatments are used
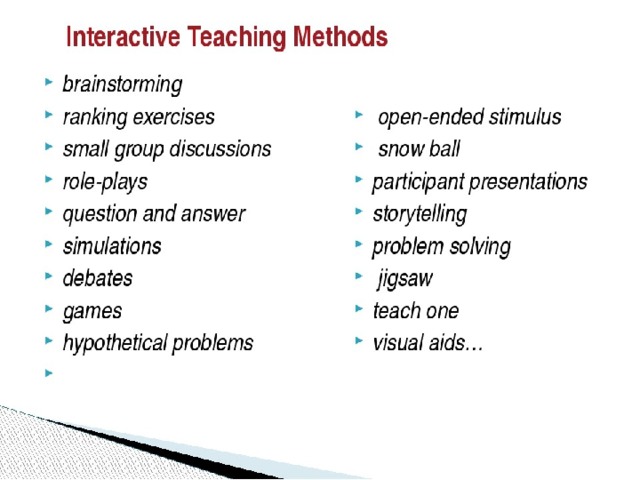
- Priority:
- Cognitive-Behavioral Therapy.
- Schema Therapy.
- Reality Therapy.
- Choice Theory.
- Rational pharmacotherapy.
- Psychopharmacotherapy (if indicated)
- Biofeedback Therapy
- Rational psychocorrection of stress
- Jacobson progressive muscle relaxation.
- Traditional and modern gymnastic systems, relaxation techniques.
- Breathing techniques .
- Stress exposure.
- Self-control training.
- Jacobson progressive muscle relaxation.
- Lifestyle modification
- Work with bad habits.
- Diet correction.
- Professional and social adaptation.
3. How is the treatment under the program
Each treatment program at the NEURO-PSI clinic consists of four stages:
- diagnostics,
- work with disease symptoms,
- work with the causes of the disease,
- consolidation of the achieved results.
Work efficiency is increased by dividing the treatment process into a predetermined number of sessions, at convenient times and without hospitalization. This means that each program is adapted to the problem that the client has addressed.
The treatment method is predictable, time-limited, productive, and most importantly, understandable for the client.
Of course, the treatment takes place in a comfortable mode without interruption from work, study or family. Improvements in well-being and mood (cure) occur in stages: after a decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future.
4. What are the results and forecast
Upon completion of the program, you get rid of obsessive thoughts and rituals, fear of pollution, unmotivated fears, panic attacks and multiple vegetative symptoms (sudden jumps in blood pressure, rapid heartbeat, dizziness, nausea).
According to statistics, the effectiveness of the methods used approaches 100% if all recommendations of specialists are followed.
Skills you acquire during the program:
- self-control and self-regulation
- constructive analysis of the state of the body
- understanding one's own mental and emotional sphere
- ability to control one's attention
- ability to act consciously in stressful situations
Significantly improves the emotional and physical condition, gains self-confidence, in the future. Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
Specialists
- Rakhmanov Vladimir Alexandrovich
Psychiatrist, CBT-, ACT- and CFT-psychotherapist.
in the clinic online
Adults (over 18 years old) Elderly (from 60 years old)
Scientific approach. Horizon.
Founder and CEO of the Neuro-Psi network. Psychiatrist and psychotherapist.
As a psychiatrist, Vladimir works strictly in the evidence-based approach (Evidence-based Medicine). As a psychotherapist, he uses modern “rational” methods of psychotherapy (CBT, ACT, CFT, Scheme Therapy)
Vladimir is distinguished by a broad clinical outlook, professional awareness, and a comprehensive understanding of the patient's problem. These qualities are especially important in dealing with complex cases.

Vladimir specializes in working with the following client problems: professional burnout, depressed mood, excessive anxiety, despondency, indecision, regret about missed opportunities, intolerance for uncertainty, loss of meaning and direction in life. Chronic pain, psychosomatic and somatopsychic diseases. Isolation, avoidance of difficulties, loneliness. Does not work with suicidal behavior, addictions of any type, does not conduct outpatient appointments for patients who are hospitalized.
“Difficult tasks, whether it be a health problem or a life catastrophe, require not only perseverance in overcoming. Often a negative course of events changes the intellectual effort - making meaningful decisions based on objective data.
Read more
★9.81 based on 15 reviews
- Chibikova Evgenia Yurievna
Child psychiatrist, adult psychiatrist.
at the clinic online
Children (0-17 years old) Adults (18 to 60 years old)
Concentration.
 Care.
Care. Regularly trains and studies abroad. Thanks to this, he is able to prescribe effective, but at the same time the safest drugs.
Filigree in neurochemistry.
Read more
★9.71 based on 112 reviews
- Kuznetsov Sergey Olegovich
Psychologist. Cognitive behavioral psychotherapist. Family psychotherapist
in the clinic online
Teenagers (16 to 17 years old) Adults (18 to 60 years old)
Clarity. Impartiality.
Outline your problem and steps to fix it. Support on the path of real change. Shows the problem for what it is. Do not embellish and do not add something of their own. Demonstrates an alternative attitude in therapy so that you can live it from your own experience, and not theoretically.
Read more
★9.
 83 based on 52 reviews
83 based on 52 reviews - Dobrovidova Natalya Alexandrovna
Psychologist. Cognitive behavioral psychotherapist. PhD
in the clinic online
Adults (18 to 60 years old) Adolescents (from 14 to 17 years old)
Humanism. Environmental friendliness.
Will teach you how to manage your mental life. She is convinced that "our thoughts are the basis of our mental health and happiness", "and neurosis is a choice." It will help you make a choice in your favor. In fact, it forms a new way of thinking and new habits (which is so difficult to do without help and support). Such changes in the psyche lead to significant changes in life. He believes in every person and considers this the basis of quality therapy.
Read more
★9.64 based on 41 reviews
- Trofimova Marina Ivanovna
Psychologist.
 Sexologist.
Sexologist. in the clinic online
Adults (from 18 to 60 years old)
Non-judgmental. Result.
Can quickly and clearly show the connection between thoughts and emotions that affect life. Teaches you to overestimate the beliefs and attitudes that reduce the quality of life. Helps clients to move towards the goal step by step, respects the choice of the patient, gently and confidently accompanies along the way.
Read more
★9.43 based on 31 reviews
- Vyrikov Artur Igorevich
Clinical psychologist. ACT psychotherapist. Cognitive behavioral psychotherapist
in clinic online
Adults (18 to 55 years old)
Trust. Simplicity.
Creates a friendly atmosphere of understanding and ease, communicates in simple language.
 Easily finds common topics for conversation, tries on situations for himself and asks precise questions "in the case." Helps to quickly understand the essence of the problem and proceed to work on a solution. Works with setting values, finding priorities, and choosing an informed life path.
Easily finds common topics for conversation, tries on situations for himself and asks precise questions "in the case." Helps to quickly understand the essence of the problem and proceed to work on a solution. Works with setting values, finding priorities, and choosing an informed life path. Read more
★9.52 based on 82 reviews
- Yarygin Anton Igorevich
Adult psychiatrist.
in the clinic online
Adults (over 18 years old) Elderly (over 60)
Confidence. Efficiency.
First class and highly organized specialist.
Anton is maximally focused on the healing process. Able to quickly evaluate incoming information, make objective and accurate decisions. Works with full dedication, passionate about the work process.
Competently arranges treatment and brings the case to a positive result.

Read more
★9.27 based on 37 reviews
- Shlyapnikov Sergei Anatolievich
Psychiatrist.
in the clinic online
Adults (18-60) Elderly (from 60 years old) Adolescents (16 to 17 years old)
Perseverance. Result.
Strengths. An incredibly empathetic psychiatrist who works effectively with patients of all ages. He specializes in working with anxiety, panic, depression, obsessions and, in general, working with neurotic disorders.
“I am convinced that psychiatry is one of the most interesting branches of medicine. Seeing the patient feel better is priceless.”
Able to smooth out sharp corners in a humorous way. Sense of humor.
More details
★8.
 23 based on 13 reviews
23 based on 13 reviews
Treatment of obsessive-compulsive disorder
Treatment of obsessive-compulsive disorder. We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
Symptoms of obsessive-compulsive disorder
- Frightening images and drives
- Compulsive acts (rituals)
- Intrusive check of one's own actions
- Fear of trouble, pollution or contamination
- Inexplicable desire to count something
- Excessive organization and pedantry
- Perfectionism in relationships, work and even leisure
- "Stuck", "looping" on one's thoughts
You feel that over time your mood becomes worse: apathy, depression, obsessions increase, and rituals begin to fill all your free time or harm your physical health.
You may have had more than one meeting with psychologists, psychotherapists and psychiatrists. You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless.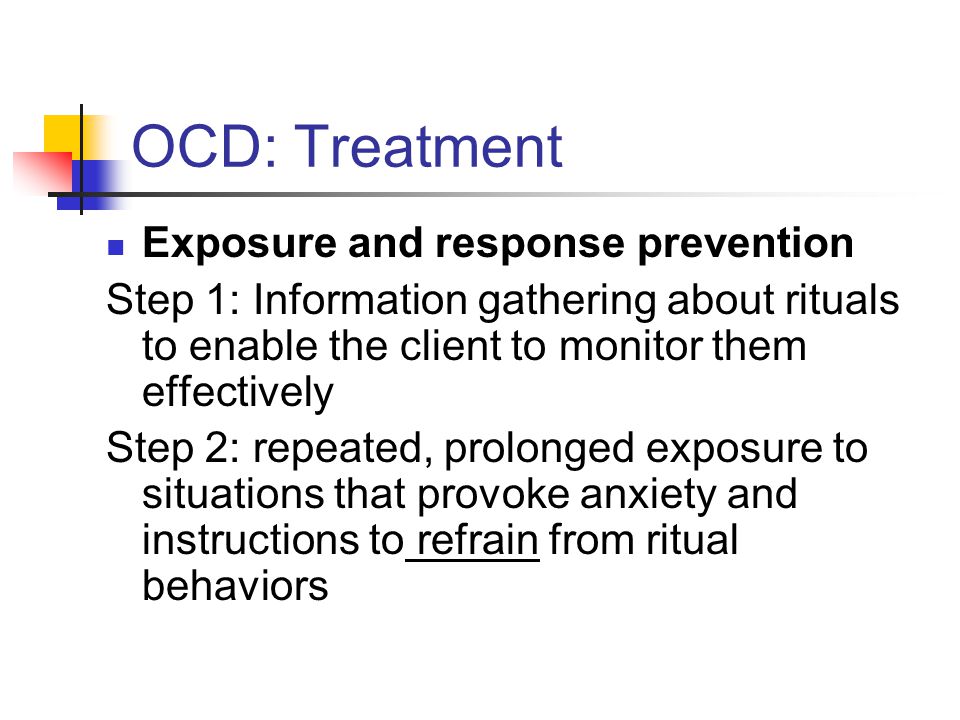 However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder is a syndrome characterized by the presence of obsessive thoughts (obsessions) to which a person reacts with certain actions (compulsions). The causes of the disorder are rarely superficial. The syndrome is also accompanied by the development of obsessive memories and various pathological phobias. May be chronic, episodic or progressive.
Obsession - obsessive thought, persistent desire for something, uncontrollable and accompanied by anxiety and intense anxiety. In an attempt to cope with such thoughts, a person resorts to committing compulsions.
Compulsion - an irresistible need to perform certain actions (rituals), which can be assessed by the person himself as irrational or meaningless, and the internal need to perform them is forced and is the result of obsessive ideas.
Common examples of OCD manifestations
- An exaggerated sense of danger. Fear of the materiality of thoughts:
- "now I will lose control and hurt my loved ones"
- "something terrible is about to happen, I can feel it"
- "I shouldn't think like that, all this will come true because of me"
- Pathological fear of pollution. Thirst for Purity
- Excessive perfectionism, exaggerated responsibility - "everything must be done perfectly", "everything depends on me, mistakes are unacceptable"
How does this painful algorithm work?
Most people have unwanted or obsessive thoughts quite often, but all sufferers of the disorder greatly exaggerate their importance. Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
As we noted earlier, repetitive avoidance behavior can "get stuck", "loop", that is, have a tendency to repeat. The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
If you periodically experience over the years:
- Constant or fluctuating anxiety
- The need to perform certain ritualized actions
- A persistent decline in the quality of life due to the need to avoid certain thoughts and actions, places and events
And you are also persecuted:
- Significant problems in studies and career
- Failure to establish a serious relationship
- Constant criticism and pressure from relatives
- Many senseless activities
- Excessive involvement in computer games and the Internet, alcohol
- Loneliness and isolation
We strongly recommend that you do not delay seeking help and that you complete a remedial program.
Consultations and psychotherapeutic sessions according to the program are held several times a week, until the relief of severe symptoms, then the frequency of meetings with specialists is reduced to 2–3 per month. Count on the fact that in the end we will deal with your problem together.
Treatment of obsessive-compulsive disorder in Neuro-Psi
Every day, the specialists of the NEURO-PSI clinic analyze the world practice in the field of psychiatry and psychotherapy. The goal is the impartial selection and implementation of those methods of treatment and psychological assistance, the effectiveness of which has been convincingly proven in independent studies.
We are guided by the principles of evidence-based medicine and use as a basic method of treatment a psychotherapeutic paradigm, the effectiveness of which has been widely recognized by the professional community.
1. What is the essence of the obsessive-compulsive disorder treatment program
Since obsessive thoughts, rituals and conditions are only symptoms of mental dysfunction, the root cause must be treated in order to achieve a stable result. A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
The main emphasis is on teaching the client how to properly respond to his thoughts, emotions, inner feelings and interpretation of external events.
All types of psychotherapeutic and drug treatments serve the same goal: to achieve the best result in the shortest possible time. At the same time, by coordinating the efforts of specialists in various fields, the most complete coverage of all types of mental illnesses, disorders and disorders is possible.
2. What treatments are used
- Priority:
- Cognitive-Behavioral Therapy.
- Schema Therapy.
- Reality Therapy.
- Choice Theory.
- Rational pharmacotherapy.
- Psychopharmacotherapy (if indicated)
- Biofeedback Therapy
- Rational psychocorrection of stress
- Jacobson progressive muscle relaxation.
- Traditional and modern gymnastic systems, relaxation techniques.
- Breathing techniques .
- Stress exposure.
- Self-control training.
- Jacobson progressive muscle relaxation.
- Lifestyle modification
- Work with bad habits.
- Diet correction.
- Professional and social adaptation.
3. How is the treatment under the program
Each treatment program at the NEURO-PSI clinic consists of four stages:
- diagnostics,
- work with disease symptoms,
- work with the causes of the disease,
- consolidation of the achieved results.
Work efficiency is increased by dividing the treatment process into a predetermined number of sessions, at convenient times and without hospitalization. This means that each program is adapted to the problem that the client has addressed.
The treatment method is predictable, time-limited, productive, and most importantly, understandable for the client.
Of course, the treatment takes place in a comfortable mode without interruption from work, study or family. Improvements in well-being and mood (cure) occur in stages: after a decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future.
4. What are the results and forecast
Upon completion of the program, you get rid of obsessive thoughts and rituals, fear of pollution, unmotivated fears, panic attacks and multiple vegetative symptoms (sudden jumps in blood pressure, rapid heartbeat, dizziness, nausea).
According to statistics, the effectiveness of the methods used approaches 100% if all recommendations of specialists are followed.
Skills you acquire during the program:
- self-control and self-regulation
- constructive analysis of the state of the body
- understanding one's own mental and emotional sphere
- ability to control one's attention
- ability to act consciously in stressful situations
Significantly improves the emotional and physical condition, gains self-confidence, in the future. Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
Specialists
- Ruzanov Leonid Timofeevich
Head of the Moscow branch. Cognitive behavioral psychotherapist. Family psychotherapist
in the clinic online
Adults (18 to 55 years old)
Energy. Optimism.
Leading specialist of the clinic. It will help to cope where it seemed impossible. Changes the thinking pattern from self-critical to supportive. It teaches you to treat yourself with deep compassion and sincere sympathy, which gives an experience of acceptance (the absence of which, very often, is the root of the problem). A master of generating insights and understanding in clients.
Read more
★9.79 based on 46 reviews
- Pantsov Oleg Vyacheslavovich
Psychologist.
 Family psychotherapist. Child-parent psychologist. Teenage psychologist. CPT and AST therapist.
Family psychotherapist. Child-parent psychologist. Teenage psychologist. CPT and AST therapist. Online only
Adults (18+) Teenagers (from 14 to 17 years old)
Harmony. Professionalism.
Online reception only.
A holistic specialist who knows the most modern techniques of family therapy. He knows how to look at the situation from different points of view and find the best solution.
Will teach you how to build a dialogue with your partner and with yourself in a new way. Comprehensive approach to overcoming individual and family crises. He adheres to a systematic approach in his work, which combines a clear structure with a careful and attentive attitude.
Read more
★9.76 based on 43 reviews
- Trushkina (Savostina) Anastasia Dmitrievna
Psychologist, Cognitive behavioral therapist, EMDR psychologist.
Online only
Adults (18+) Adolescents (14 to 17 years old)
Flexibility.
 Result.
Result. Online reception only.
Adheres to evidence-based therapies only. It will help to correctly identify the causes of problems and outline a plan for solving them in a short time. Builds partner-equal relationships with clients, accepts and treats each client without judgment. Has her experience of continuous personal therapy for five years.
Read more
★9.89 based on 34 reviews
- Kortunova Irina Alexandrovna
Systemic family psychotherapist, Child-parent psychologist, Emotionally focused therapist, Emdr-psychologist
in clinic online
Adults (18 to 60 years old) Adolescents (11 to 17 years old)
Support. Creation.
Will help to overcome family crises, establish mutual understanding in a couple, cope with naughty children.
 Hear each family member and teach to hear each other. He will give clear recommendations and help you find new working strategies to solve difficult situations.
Hear each family member and teach to hear each other. He will give clear recommendations and help you find new working strategies to solve difficult situations. Believes that each person can do much more than he does, and even more than he thinks. It will help to reveal one's potential, removing fears, fears, anxieties. He knows how to create a warm, trusting atmosphere at the session, he feels the client subtly.
Read more
★9.69 based on 14 reviews
- Strepetova Olesya Vladimirovna
Psychologist, Systemic Family Therapist, Emotionally Focused Therapist, Emdr Psychologist.
in the clinic online
Teenagers (14 to 17 years old) Adults (18 to 50 years old)
Acceptance. Rationality.
Professional and understanding psychologist, sensitive to the individual characteristics of clients, their needs and difficulties.
 He will find a special approach to everyone, he knows various techniques of systemic therapy: short-term strategic therapy, ORCT, EFT, etc., as well as techniques for working with trauma.
He will find a special approach to everyone, he knows various techniques of systemic therapy: short-term strategic therapy, ORCT, EFT, etc., as well as techniques for working with trauma. Will provide support on personal and family issues, help to overcome the crisis in a couple's relationship, cope with difficult situations and get out of them in a resourceful state. I am convinced that the quality of our life directly depends on how we live it “here and now”.
Read more
★9.57 based on 12 reviews
- Sotskaya Gulnara Mizkhatovna
Adolescent Psychologist, Child-Parent Psychologist, Child Psychologist, Neuropsychologist, CBT Therapist.
in the clinic online
Adults (19 to 30 years old) Children (from 2 to 17 years old)
Acceptance.
 Support.
Support. Professional in expert diagnostics and psycho-correctional work with children and adolescents with various disabilities (ADHD, ADHD and ADD), emotional disorders, peer problems and crisis conditions.
Competently solves the problems of child-parent relationships: skillfully selects the "key" to the child and teaches parents to use this "key". Conducts EPI (Experimental Psychological Research).
More
★9.59 based on 7 reviews
- Samarina Olga Evgenievna
Child psychiatrist
Clinic only
Children (0-15 years old)
Peace of mind. Confidence.
Olga is a young and competent child psychiatrist. Like most modern doctors working in a scientific-evidence-based approach, Olga continuously studies foreign sources and literature, knows how to find an approach to each little patient. Olga does not work with adults.
Interested in the profession and has an endless love for children.