Best treatments for eating disorders
Psychological Treatments for Eating Disorders
1. Walsh BT. The enigmatic persistence of anorexia nervosa. Am J Psychiatry. 2013 May 1;170(5):477–484. PubMed PMID: 23429750. [PMC free article] [PubMed] [Google Scholar] This paper presents evidence for a model to elucidate the persistent course of anorexia nervosa.
2. Watson HJ, Bulik CM. Update on the treatment of anorexia nervosa: review of clinical trials, practice guidelines and emerging interventions. Psychol Med. 2012 Dec;10:1–24. PubMed PMID: 23217606. [PubMed] [Google Scholar] This paper reviews treatment research and practice guidelines for anorexia nervosa, with the goal of informing clinical practice for this patient population.
3. Carter FA, Jordan J, McIntosh VV, Luty SE, McKenzie JM, Frampton CM, et al. The long-term efficacy of three psychotherapies for anorexia nervosa: a randomized, controlled trial. Int J Eat Disord. 2011 Nov;44(7):647–654. PubMed PMID: 21997429. [PubMed] [Google Scholar]
4. Schmidt U, Oldershaw A, Jichi F, Sternheim L, Startup H, McIntosh V, et al. Out-patient psychological therapies for adults with anorexia nervosa: randomised controlled trial. Br J Psychiatry. 2012 Nov;201(5):392–399. PubMed PMID: 22995632. Epub 2012/09/22. eng. [PubMed] [Google Scholar]
5. Schmidt U, Renwick B, Lose A, Kenyon M, Dejong H, Broadbent H, et al. The MOSAIC study - comparison of the Maudsley Model of Treatment for Adults with Anorexia Nervosa (MANTRA) with Specialist Supportive Clinical Management (SSCM) in outpatients with anorexia nervosa or eating disorder not otherwise specified, anorexia nervosa type: study protocol for a randomized controlled trial. Trials. 2013 May 30;14(1):160. PubMed PMID: 23721562. [PMC free article] [PubMed] [Google Scholar] This paper outlines the study protocol for the largest trial comparing MANTRA (Maudsley Model of Treatment for Adults with Anorexia Nervosa) to a specialist supportive clinical management intervention, given the lack of evidence-based treatments for anorexia nervosa.
6. Tchanturia K, Lloyd S, Lang K. Cognitive remediation therapy for anorexia nervosa: Current evidence and future research directions. Int J Eat Disord. 2013 Jul;46(5):492–495. PubMed PMID: 23658098. Epub 2013/05/10. eng. [PubMed] [Google Scholar] This paper summarizes current evidence in the literature applying cognitive remediation therapy to anorexia nervosa, and outlines novel directions for this area of treatment research.
7. Davies H, Fox J, Naumann U, Treasure J, Schmidt U, Tchanturia K. Cognitive remediation and emotion skills training for anorexia nervosa: an observational study using neuropsychological outcomes. Eur Eat Disord Rev. 2012 May;20(3):211–217. PubMed PMID: 22431401. [PubMed] [Google Scholar]
8. Abbate-Daga G, Buzzichelli S, Marzola E, Amianto F, Fassino S. Effectiveness of cognitive remediation therapy (CRT) in anorexia nervosa: a case series. J Clin Exp Neuropsychol. 2012 Dec;34(10):1009–1015. PubMed PMID: 22876988. [PubMed] [Google Scholar]
9. Lock J, Agras WS, Fitzpatrick KK, Bryson SW, Jo B, Tchanturia K. Is outpatient cognitive remediation therapy feasible to use in randomized clinical trials for anorexia nervosa? Int J Eat Disord. 2013 Apr;:29. PubMed PMID: 23625628. [PMC free article] [PubMed] [Google Scholar]
Lock J, Agras WS, Fitzpatrick KK, Bryson SW, Jo B, Tchanturia K. Is outpatient cognitive remediation therapy feasible to use in randomized clinical trials for anorexia nervosa? Int J Eat Disord. 2013 Apr;:29. PubMed PMID: 23625628. [PMC free article] [PubMed] [Google Scholar]
10. Touyz S, Le Grange D, Lacey H, Hay P, Smith R, Maguire S, et al. Treating severe and enduring anorexia nervosa: a randomized controlled trial. Psychol Med. 2013 May;3:1–11. PubMed PMID: 23642330. Epub 2013/05/07. Eng. [Google Scholar] This paper demonstrates the promise of psychological treatments with a population of patients with severe and enduring anorexia nervosa, given that illness chronicity is associated with poorer treatment response.
11. Fairburn CG, Jones R, Peveler RC, Hope RA, O'Connor M. Psychotherapy and bulimia nervosa. Longer-term effects of interpersonal psychotherapy, behavior therapy, and cognitive behavior therapy. Arch Gen Psychiatry. 1993 Jun;50(6):419–428. PubMed PMID: 8498876.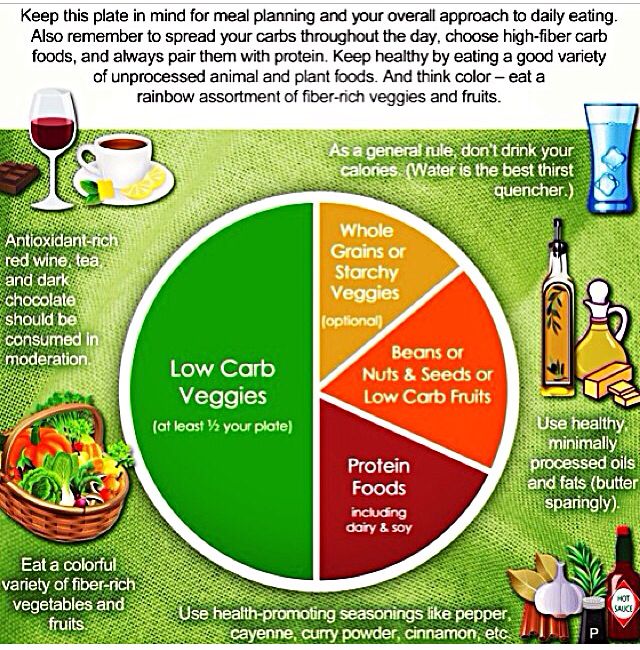 [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
12. Agras WS, Walsh BT, Fairburn CG, Wilson GT, Kraemer HC. A multicenter comparison of cognitive-behavioral therapy and interpersonal psychotherapy for bulimia nervosa. Archives of General Psychiatry. 2000;57(5):459–466. [PubMed] [Google Scholar]
13. Hay P. A systematic review of evidence for psychological treatments in eating disorders: 2005–2012. Int J Eat Disord. 2013 Jul;46(5):462–469. PubMed PMID: 23658093. Epub 2013/05/10. eng. [PubMed] [Google Scholar] This paper provides a comprehensive review and update of eating disorder treatment literature from past seven years adding new evidence for psychotherapies in eating disorders.
14. Brown TA, Keel PK. Current and emerging directions in the treatment of eating disorders. Substance abuse : research and treatment. 2012;6:33–61. PubMed PMID: 22879753. Pubmed Central PMCID: 3411516. [PMC free article] [PubMed] [Google Scholar] This paper provides a comprehensive discussion of current and emerging treatments for eating disorder treatments.
15. Rieger E, Van Buren DJ, Bishop M, Tanofsky-Kraff M, Welch R, Wilfley DE. An eating disorder-specific model of interpersonal psychotherapy (IPT-ED): causal pathways and treatment implications. Clin Psychol Rev. 2010 Jun;30(4):400–410. PubMed PMID: 20227151. Epub 2010/03/17. eng. [PubMed] [Google Scholar]
16. Arcelus J, Whight D, Langham C, Baggott J, McGrain L, Meadows L, et al. A case series evaluation of a modified version of interpersonal psychotherapy (IPT) for the treatment of bulimic eating disorders: a pilot study. Eur Eat Disord Rev. 2009 Jul;17(4):260–268. PubMed PMID: 19452496. [PubMed] [Google Scholar] This paper introduces a brief, 10-session version of IPT for patients with BN BED, and subclinical EDs with bulimic symptoms.
17. Arcelus J, Whight D, Brewin N, McGrain L. A brief form of interpersonal psychotherapy for adult patients with bulimic disorders: a pilot study. Eur Eat Disord Rev. 2012 Jul;20(4):326–330. PubMed PMID: 22383297. [PubMed] [Google Scholar]
18. Mitchell JE, Agras S, Crow S, Halmi K, Fairburn CG, Bryson S, et al. Stepped care and cognitive-behavioural therapy for bulimia nervosa: randomised trial. The British Journal of Psychiatry. 2011;198(5):391–397. [PMC free article] [PubMed] [Google Scholar]
Mitchell JE, Agras S, Crow S, Halmi K, Fairburn CG, Bryson S, et al. Stepped care and cognitive-behavioural therapy for bulimia nervosa: randomised trial. The British Journal of Psychiatry. 2011;198(5):391–397. [PMC free article] [PubMed] [Google Scholar]
19. Crow SJ, Agras WS, Halmi KA, Fairburn CG, Mitchell JE, Nyman JA. A cost effectiveness analysis of stepped care treatment for bulimia nervosa. Int J Eat Disord. 2013 May;46(4):302–307. PubMed PMID: 23354913. [PMC free article] [PubMed] [Google Scholar]
20. Wonderlich SA, Peterson CB, Crosby RD, Smith TL, Klein MH, Mitchell JE, et al. A randomized controlled comparison of integrative cognitive-affective therapy (ICAT) and enhanced cognitive-behavioral therapy (CBT-E) for bulimia nervosa. Psychol Med. 2013 May;23:1–11. PubMed PMID: 23701891. [PMC free article] [PubMed] [Google Scholar] This paper discusses the first randomized controlled trial to compare a new treatment for BN integrative cognitive-affective therapy (ICAT) and enhanced cognitive behavioral therapy (CBT-E) for bulimia nervosa.
21. Wilson GT, Wilfley DE, Agras WS, Bryson SW. Psychological treatments of binge eating disorder. Arch Gen Psychiatry. 2010 Jan;67(1):94–101. PubMed PMID: 20048227. [PMC free article] [PubMed] [Google Scholar]
22. Tanofsky-Kraff M, Bulik CM, Marcus MD, Striegel RH, Wilfley DE, Wonderlich SA, et al. Binge eating disorder: the next generation of research. Int J Eat Disord. 2013 Apr;46(3):193–207. PubMed PMID: 23354950. Pubmed Central PMCID: 3600071. [PMC free article] [PubMed] [Google Scholar] This paper reviews the state of current knowledge on psychological treatments for binge eating disorder, as well as inclusion of support in the DSM-5, risk factors, comorbidity, Research Domain Criteria, obesity relationships, pharmacological and surgical treatments, military health, and personal costs in relation to binge eating disorder.
23. Hilbert A, Bishop ME, Stein RI, Tanofsky-Kraff M, Swenson AK, Welch RR, et al. Long-term efficacy of psychological treatments for binge eating disorder. Br J Psychiatry. 2012 Mar;200(3):232–237. PubMed PMID: 22282429. Pubmed Central PMCID: 3290797. [PMC free article] [PubMed] [Google Scholar] This paper demonstrates the long-term efficacy of CBT and IPT for treatment of binge eating disorder, highlighting IPT as a viable alternative to CBT.
Br J Psychiatry. 2012 Mar;200(3):232–237. PubMed PMID: 22282429. Pubmed Central PMCID: 3290797. [PMC free article] [PubMed] [Google Scholar] This paper demonstrates the long-term efficacy of CBT and IPT for treatment of binge eating disorder, highlighting IPT as a viable alternative to CBT.
24. Munsch S, Meyer AH, Biedert E. Efficacy and predictors of long-term treatment success for Cognitive-Behavioral Treatment and Behavioral Weight-Loss-Treatment in overweight individuals with binge eating disorder. Behav Res Ther. 2012 Dec;50(12):775–785. PubMed PMID: 23099111. Epub 2012/10/27. eng. [PubMed] [Google Scholar]
25. Grilo CM, Crosby RD, Wilson GT, Masheb RM. 12-month follow-up of fluoxetine and cognitive behavioral therapy for binge eating disorder. J Consult Clin Psychol. 2012 Dec;80(6):1108–1113. PubMed PMID: 22985205. Pubmed Central PMCID: PMC3514647. Epub 2012/09/19. eng. [PMC free article] [PubMed] [Google Scholar] This paper discusses the long-term effects of cognitive behavioral therapy and pharmacotherapy (fluoxetine) in treating binge eating disorder, which demonstrated that cognitive behavioral therapy (alone or with adjunctive pharmacotherapy) was more effective than pharmacotherapy alone.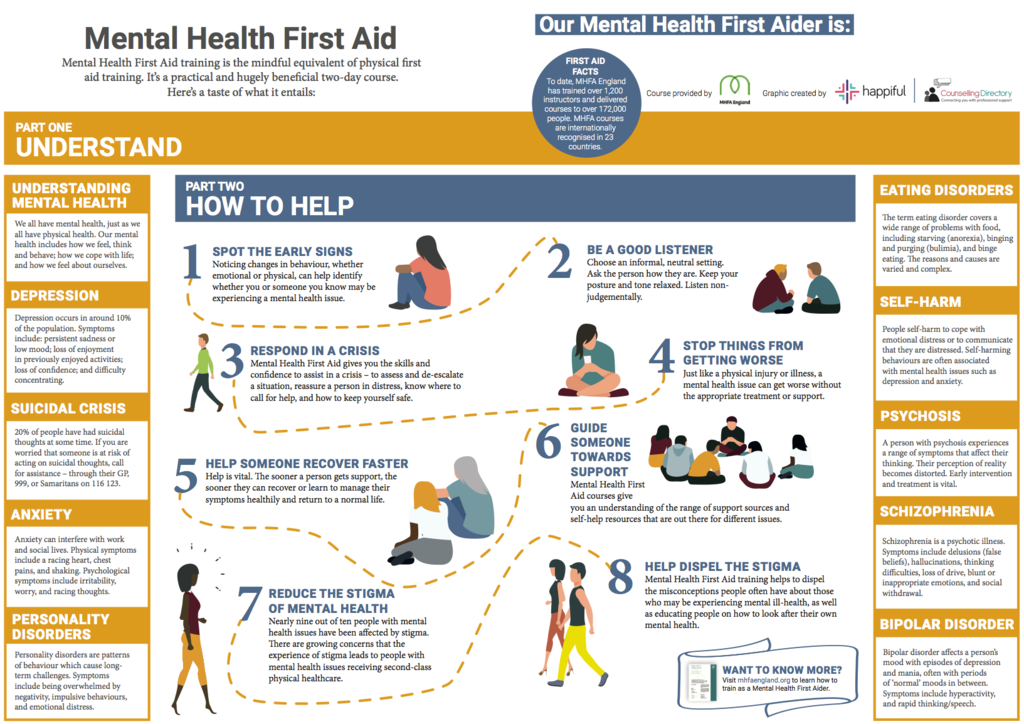
26. Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: a "transdiagnostic" theory and treatment. Behav Res Ther. 2003 May;41(5):509–528. PubMed PMID: 12711261. [PubMed] [Google Scholar]
27. Fairburn CG, Cooper Z, Doll HA, O'Connor ME, Bohn K, Hawker DM, et al. Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: a two-site trial with 60-week follow-up. Am J Psychiatry. 2009 Mar;166(3):311–339. PubMed PMID: 19074978. [PMC free article] [PubMed] [Google Scholar]
28. Byrne SM, Fursland A, Allen KL, Watson H. The effectiveness of enhanced cognitive behavioural therapy for eating disorders: an open trial. Behav Res Ther. 2011 Apr;49(4):219–226. PubMed PMID: 21345418. [PubMed] [Google Scholar]
29. Fairburn CG, Cooper Z, Doll HA, O'Connor ME, Palmer RL, Dalle Grave R. Enhanced cognitive behaviour therapy for adults with anorexia nervosa: a UK-Italy study. Behav Res Ther. 2013 Jan;51(1):R2–R8. PubMed PMID: 23084515. Pubmed Central PMCID: 3662032. [PMC free article] [PubMed] [Google Scholar] This paper provides evidence of the sustained treatment effects of CBT-E among adults with anorexia nervosa, a population for whom no evidence-based treatment is established.
Pubmed Central PMCID: 3662032. [PMC free article] [PubMed] [Google Scholar] This paper provides evidence of the sustained treatment effects of CBT-E among adults with anorexia nervosa, a population for whom no evidence-based treatment is established.
30. McIntosh VV, Carter FA, Bulik CM, Frampton CM, Joyce PR. Five-year outcome of cognitive behavioral therapy and exposure with response prevention for bulimia nervosa. Psychol Med. 2011 May;41(5):1061–1071. PubMed PMID: 20810005. [PubMed] [Google Scholar]
31. Steinglass J, Albano AM, Simpson HB, Carpenter K, Schebendach J, Attia E. Fear of food as a treatment target: exposure and response prevention for anorexia nervosa in an open series. Int J Eat Disord. 2012 May;45(4):615–621. PubMed PMID: 21541979. Pubmed Central PMCID: 3151474. [PMC free article] [PubMed] [Google Scholar] This paper presents a novel adaptation of an evidence-based anxiety treatment to an eating disorder population, given the high comorbidity between eating disorders and anxiety.
32. Koskina A, Campbell IC, Schmidt U. Exposure therapy in eating disorders revisited. Neuroscience and biobehavioral reviews. 2013 Feb;37(2):193–208. PubMed PMID: 23201859. Epub 2012/12/04. eng. [PubMed] [Google Scholar] This paper provides a comprehensive review of exposure therapies evaluated with patients with eating disorders and provides novel directions for future research on these treatments.
33. Bankoff SM, Karpel MG, Forbes HE, Pantalone DW. A systematic review of dialectical behavior therapy for the treatment of eating disorders. Eat Disord. 2012 May;20(3):196–215. PubMed PMID: 22519897. [PubMed] [Google Scholar] This study reviews the literature on dialectical behavior therapy for eating disorders, and suggests the need for additional research to evaluate its efficacy.
34. Carter O, Pannekoek L, Fursland A, Allen KL, Lampard AM, Byrne SM. Increased wait-list time predicts dropout from outpatient enhanced cognitive behaviour therapy (CBT-E) for eating disorders. Behav Res Ther. 2012 Aug;50(7–8):487–492. PubMed PMID: 22659158. [PubMed] [Google Scholar]
Behav Res Ther. 2012 Aug;50(7–8):487–492. PubMed PMID: 22659158. [PubMed] [Google Scholar]
35. Knowles L, Anokhina A, Serpell L. Motivational interventions in the eating disorders: what is the evidence? Int J Eat Disord. 2013 Mar;46(2):97–107. PubMed PMID: 23001832. Epub 2012/09/25. eng. [PubMed] [Google Scholar]
36. Dray J, Wade TD. Is the transtheoretical model and motivational interviewing approach applicable to the treatment of eating disorders? A review. Clin Psychol Rev. 2012 Aug;32(6):558–565. PubMed PMID: 22819997. Epub 2012/07/24. eng. [PubMed] [Google Scholar]
37. Waller G. The myths of motivation: time for a fresh look at some received wisdom in the eating disorders? Int J Eat Disord. 2012 Jan;45(1):1–16. PubMed PMID: 22170018. [PubMed] [Google Scholar] This paper counters the commonly-held view that patients’ verbal affirmations of motivation are helpful, and offers behavioral strategies to more effectively address motivation consistently throughout treatment.
38. Wilfley DE, Kolko RP, Kass AE. Cognitive-behavioral therapy for weight management and eating disorders in children and adolescents. Child Adolesc Psychiatr Clin N Am. 2011 Apr;20(2):271–285. PubMed PMID: 21440855. Pubmed Central PMCID: 3065663. Epub 2011/03/29. eng. [PMC free article] [PubMed] [Google Scholar]
39. Stiles-Shields C, Hoste RR, Doyle PM, Le Grange D. A review of family-based treatment for adolescents with eating disorders. Reviews on recent clinical trials. 2012 May;7(2):133–440. PubMed PMID: 22353196. [PubMed] [Google Scholar] This paper provides a comprehensive review of family-based treatment research among adolescents with anorexia nervosa or bulimia nervosa.
40. Couturier J, Kimber M, Szatmari P. Efficacy of family-based treatment for adolescents with eating disorders: a systematic review and meta-analysis. Int J Eat Disord. 2013 Jan;46(1):3–11. PubMed PMID: 22821753. [PubMed] [Google Scholar] This meta-analytic review highlights the efficacy of family-based treatment at long-term follow-up.
41. Lock J. Evaluation of family treatment models for eating disorders. Current opinion in psychiatry. 2011 Jul;24(4):274–279. PubMed PMID: 21519263. [PubMed] [Google Scholar]
42. Sonneville KR, Horton NJ, Micali N, Crosby RD, Swanson SA, Solmi F, et al. Longitudinal associations between binge eating and overeating and adverse outcomes among adolescents and young adults: does loss of control matter? JAMA pediatrics. 2013 Feb;167(2):149–155. PubMed PMID: 23229786. Pubmed Central PMCID: 3654655. [PMC free article] [PubMed] [Google Scholar] This paper highlights the association between binge eating, obesity, and dperession in a large sample of youth.
43. Tanofsky-Kraff M, Wilfley DE, Young JF, Mufson L, Yanovski SZ, Glasofer DR, et al. A pilot study of interpersonal psychotherapy for preventing excess weight gain in adolescent girls at-risk for obesity. Int J Eat Disord. 2010 Dec;43(8):701–706. PubMed PMID: 19882739. Pubmed Central PMCID: 2891416. Epub 2009/11/03. eng. [PMC free article] [PubMed] [Google Scholar]
44. Le Grange D, Lock J, Agras WS, Moye A, Bryson SW, Jo B, et al. Moderators and mediators of remission in family-based treatment and adolescent focused therapy for anorexia nervosa. Behav Res Ther. 2012 Feb;50(2):85–92. PubMed PMID: 22172564. Pubmed Central PMCID: 3260378. [PMC free article] [PubMed] [Google Scholar] This paper discusses moderator analyses of treatment adolescents with anorexia nervosa, which indicated that patients with more severe eating psychopathology performed better in family-based therapy than adolescent focused therapy.
Le Grange D, Lock J, Agras WS, Moye A, Bryson SW, Jo B, et al. Moderators and mediators of remission in family-based treatment and adolescent focused therapy for anorexia nervosa. Behav Res Ther. 2012 Feb;50(2):85–92. PubMed PMID: 22172564. Pubmed Central PMCID: 3260378. [PMC free article] [PubMed] [Google Scholar] This paper discusses moderator analyses of treatment adolescents with anorexia nervosa, which indicated that patients with more severe eating psychopathology performed better in family-based therapy than adolescent focused therapy.
45. Godart N, Berthoz S, Curt F, Perdereau F, Rein Z, Wallier J, et al. A randomized controlled trial of adjunctive family therapy and treatment as usual following inpatient treatment for anorexia nervosa adolescents. PloS one. 2012;7(1):e28249. PubMed PMID: 22238574. Pubmed Central PMCID: 3251571. [PMC free article] [PubMed] [Google Scholar] This study evaluates the role of family sessions in treatment of adolescents with anorexia nervosa.
46. Dalle Grave R, Calugi S, Doll HA, Fairburn CG. Enhanced cognitive behaviour therapy for adolescents with anorexia nervosa: an alternative to family therapy? Behav Res Ther. 2013 Jan;51(1):R9–R12. PubMed PMID: 23123081. Pubmed Central PMCID: 3662031. [PMC free article] [PubMed] [Google Scholar] This paper discusses the long-term impact of transdiagnostic cognitive behavioral therapy for treatment of eating disorders in adolescents.
47. Pretorius N, Dimmer M, Power E, Eisler I, Simic M, Tchanturia K. Evaluation of a cognitive remediation therapy group for adolescents with anorexia nervosa: pilot study. Eur Eat Disord Rev. 2012 Jul;20(4):321–325. PubMed PMID: 22488792. [PubMed] [Google Scholar] This study evaluates the use of cognitive remediation therapy delivered in a group format for adolescents with anorexia nervosa.
48. Wood L, Al-Khairulla H, Lask B. Group cognitive remediation therapy for adolescents with anorexia nervosa. Clinical child psychology and psychiatry.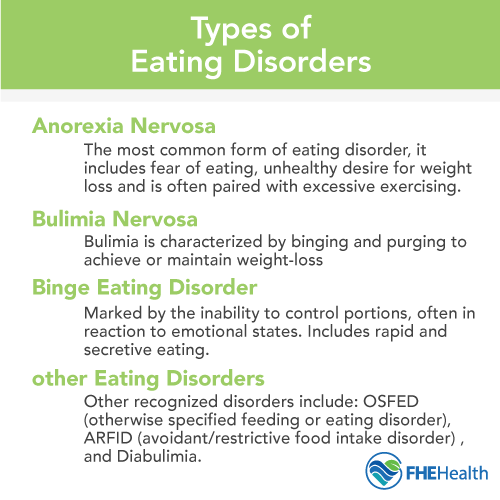 2011 Apr;16(2):225–231. PubMed PMID: 21571765. [PubMed] [Google Scholar]
2011 Apr;16(2):225–231. PubMed PMID: 21571765. [PubMed] [Google Scholar]
49. Debar LL, Wilson GT, Yarborough BJ, Burns B, Oyler B, Hildebrandt T, et al. Cognitive Behavioral Treatment for Recurrent Binge Eating in Adolescent Girls: A Pilot Trial. Cognitive and behavioral practice. 2013 May 1;20(2):147–161. PubMed PMID: 23645978. Pubmed Central PMCID: 3640565. [PMC free article] [PubMed] [Google Scholar] This paper presents results from a small pilot trial of CBT adapted for adolescent girls with recurrent binge eating.
50. Cassidy O, Sbrocco T, Vannucci A, Nelson B, Jackson-Bowen D, Heimdal J, et al. Adapting Interpersonal Psychotherapy for the Prevention of Excessive Weight Gain in Rural African American Girls. J Pediatr Psychol. 2013 May;22 PubMed PMID: 23678135. [PMC free article] [PubMed] [Google Scholar] This paper discusses cultural adaptations and implementation strategies, including incorporation of behavioral as well as parenting components, for delivery of interpersonal psychotherapy for the prevention of excessive weight gain among rural African American girls.
51. Wallace LM, von Ranson KM. Perceptions and use of empirically-supported psychotherapies among eating disorder professionals. Behav Res Ther. 2012 Mar;50(3):215–222. PubMed PMID: 22342168. [PubMed] [Google Scholar] This paper highlights the misperceptions to treatment delivery in routine clinical care and treatments as deployed in controlled treatment trials.
52. Kazdin AE, Blase SL. Rebooting Psychotherapy Research and Practice to Reduce the Burden of Mental Illness. Perspectives on Psychological Science. 2011;6(1):21–37. [PubMed] [Google Scholar]
53. Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010 Jul;167(7):748–751. PubMed PMID: 20595427. [PubMed] [Google Scholar]
54. Tanofsky-Kraff M, Engel S, Yanovski JA, Pine DS, Nelson EE. Pediatric disinhibited eating: Toward a research domain criteria framework. Int J Eat Disord. 2013 Jul;46(5):451–455. PubMed PMID: 23658090. Epub 2013/05/10. eng. [PMC free article] [PubMed] [Google Scholar] This paper describes the potential for adaptation of the novel RDoC framework to the assessment and treatment of binge eating, via assessment of the neurobiological and genetic underpinnings of eating disorders.
2013 Jul;46(5):451–455. PubMed PMID: 23658090. Epub 2013/05/10. eng. [PMC free article] [PubMed] [Google Scholar] This paper describes the potential for adaptation of the novel RDoC framework to the assessment and treatment of binge eating, via assessment of the neurobiological and genetic underpinnings of eating disorders.
55. Van den Eynde F, Guillaume S. Neuromodulation techniques and eating disorders. Int J Eat Disord. 2013 Jul;46(5):447–450. PubMed PMID: 23658089. Epub 2013/05/10. eng. [PubMed] [Google Scholar] This paper reviews the preliminary evidence supporting the efficacy of neuromodulation techniques with eating disorders and addresses the potential impact of this approach, given the need to address the neurobiological changes associated with eating disorders and the efficacy of neuromodulation with other psychiatric illnesses.
56. Lipsman N, Woodside DB, Giacobbe P, Hamani C, Carter JC, Norwood SJ, et al. Subcallosal cingulate deep brain stimulation for treatment-refractory anorexia nervosa: a phase 1 pilot trial. Lancet. 2013 Apr 20;381(9875):1361–1370. PubMed PMID: 23473846. [PubMed] [Google Scholar] This study presents results from the application of deep brain stimulation—an invasive surgical procedure—to the treatment of eating disorder patients, given the potential benefits of neuromodulation techniques for eating disorder treatment.
Lancet. 2013 Apr 20;381(9875):1361–1370. PubMed PMID: 23473846. [PubMed] [Google Scholar] This study presents results from the application of deep brain stimulation—an invasive surgical procedure—to the treatment of eating disorder patients, given the potential benefits of neuromodulation techniques for eating disorder treatment.
57. Treasure J, Schmidt U. DBS for treatment-refractory anorexia nervosa. Lancet. 2013 Apr 20;381(9875):1338–1339. PubMed PMID: 23473848. Epub 2013/03/12. eng. [PubMed] [Google Scholar]
58. Patel V, Kieling C, Maulik PK, Divan G. Improving access to care for children with mental disorders: a global perspective. Arch Dis Child. 2013;98(5):323–327. PubMed PMID: 23476001. Pubmed Central PMCID: 3672840. [PMC free article] [PubMed] [Google Scholar] This paper describes barriers regarding access to care and identifies strategies for improved training efforts.
59. Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011 Mar;38(2):65–76. PubMed PMID: 20957426. Pubmed Central PMCID: 3068522. Epub 2010/10/20. eng. [PMC free article] [PubMed] [Google Scholar]
Adm Policy Ment Health. 2011 Mar;38(2):65–76. PubMed PMID: 20957426. Pubmed Central PMCID: 3068522. Epub 2010/10/20. eng. [PMC free article] [PubMed] [Google Scholar]
60. Ravitz P, Cooke RG, Mitchell S, Reeves S, Teshima J, Lokuge B, et al. Continuing education to go: capacity building in psychotherapies for front-line mental health workers in underserviced communities. Canadian journal of psychiatry Revue canadienne de psychiatrie. 2013 Jun;58(6):335–343. PubMed PMID: 23768261. [PubMed] [Google Scholar]
61. Zandberg LJ, Wilson GT. Train-the-trainer: implementation of cognitive behavioural guided self-help for recurrent binge eating in a naturalistic setting. Eur Eat Disord Rev. 2013 May;21(3):230–237. PubMed PMID: 23109361. [PubMed] [Google Scholar] This demonstration project provides proof-of-concept data for the"train-the-trainer” implementation strategy, which has the potential to significantly increase the number of therapists trained to deliver evidence-based treatments and thus address a critical gap in care delivery.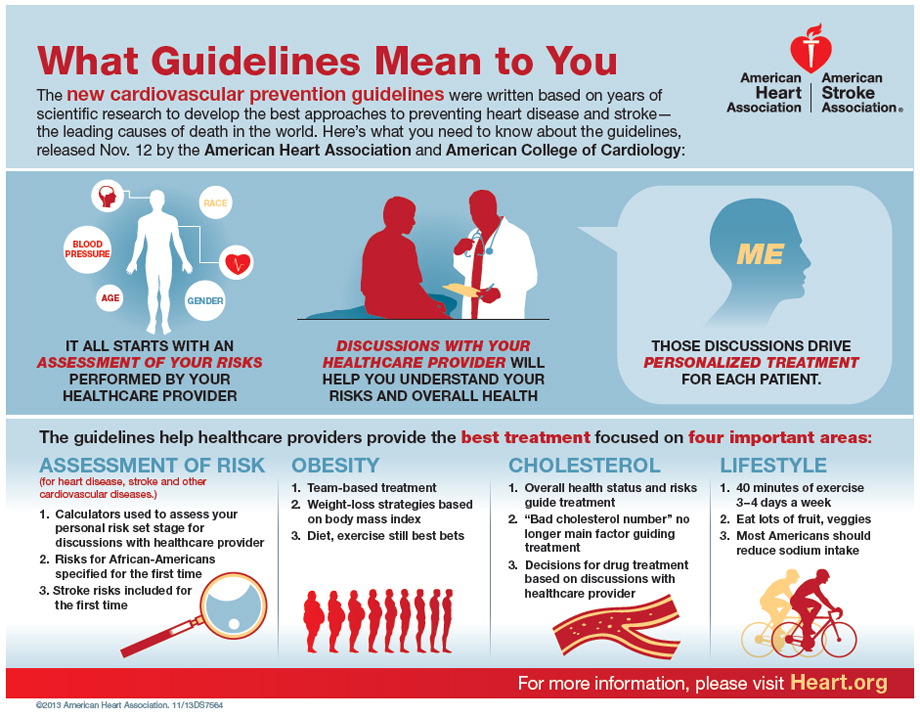
62. Fairburn CG, Cooper Z. Therapist competence, therapy quality, and therapist training. Behav Res Ther. 2011 Jun;49(6–7):373–378. PubMed PMID: 21492829. Pubmed Central PMCID: 3112491. Epub 2011/04/16. eng. [PMC free article] [PubMed] [Google Scholar]
63. Wilson GT, Zandberg LJ. Cognitive–behavioral guided self-help for eating disorders: Effectiveness and scalability. Clinical psychology review. 2012;32(4):343–357. [PubMed] [Google Scholar] This review highlights the efficacy of deploying guided self-help cognitive-behavioral interventions for patients with eating disorders, which is important given the need to conserve person-based resources for those in need of more intensive services.
64. Bauer S, Moessner M. Harnessing the power of technology for the treatment and prevention of eating disorders. Int J Eat Disord. 2013 Jul;46(5):508–515. PubMed PMID: 23658102. Epub 2013/05/10. eng. [PubMed] [Google Scholar] This review is highly important, as it outlines the use of technology for the prevention and treatment of eating disorders. Technology offers an exciting avenue through which to scale evidence-based interventions or augment existing treatment approaches, thereby increasing the potency of the treatment.
Technology offers an exciting avenue through which to scale evidence-based interventions or augment existing treatment approaches, thereby increasing the potency of the treatment.
65. Aardoom JJ, Dingemans AE, Spinhoven P, Van Furth EF. Treating eating disorders over the internet: A systematic review and future research directions. Int J Eat Disord. 2013 May;:15. PubMed PMID: 23674367. Epub 2013/05/16. Eng. [PubMed] [Google Scholar]
66. Shingleton RM, Richards LK, Thompson-Brenner H. Using Technology Within the Treatment of Eating Disorders: A Clinical Practice Review. Psychotherapy (Chicago, Ill) 2013 Mar;:25. PubMed PMID: 23527906. Epub 2013/03/27. Eng. [PMC free article] [PubMed] [Google Scholar] This review provides a clinical guide to the use of technology within eating disorder treatment delivery.
67. Wilfley DE, Agras WS, Taylor CB. Reducing the burden of eating disorders: A model for population-based prevention and treatment for university and college campuses. Int J Eat Disord. 2013 Jul;46(5):529–532. PubMed PMID: 23658106. Epub 2013/05/10. eng. [PMC free article] [PubMed] [Google Scholar] This paper outlines a novel, comprehensive approach to population-based eating disorder identification and intervention on a college campus, using internet-based tools to conserve person-based resources. The authors discuss its potential impact and offer next steps to further this important work.
Int J Eat Disord. 2013 Jul;46(5):529–532. PubMed PMID: 23658106. Epub 2013/05/10. eng. [PMC free article] [PubMed] [Google Scholar] This paper outlines a novel, comprehensive approach to population-based eating disorder identification and intervention on a college campus, using internet-based tools to conserve person-based resources. The authors discuss its potential impact and offer next steps to further this important work.
Treating Eating Disorders - HealthyChildren.org
Log in | Register
Health Issues
Health Issues
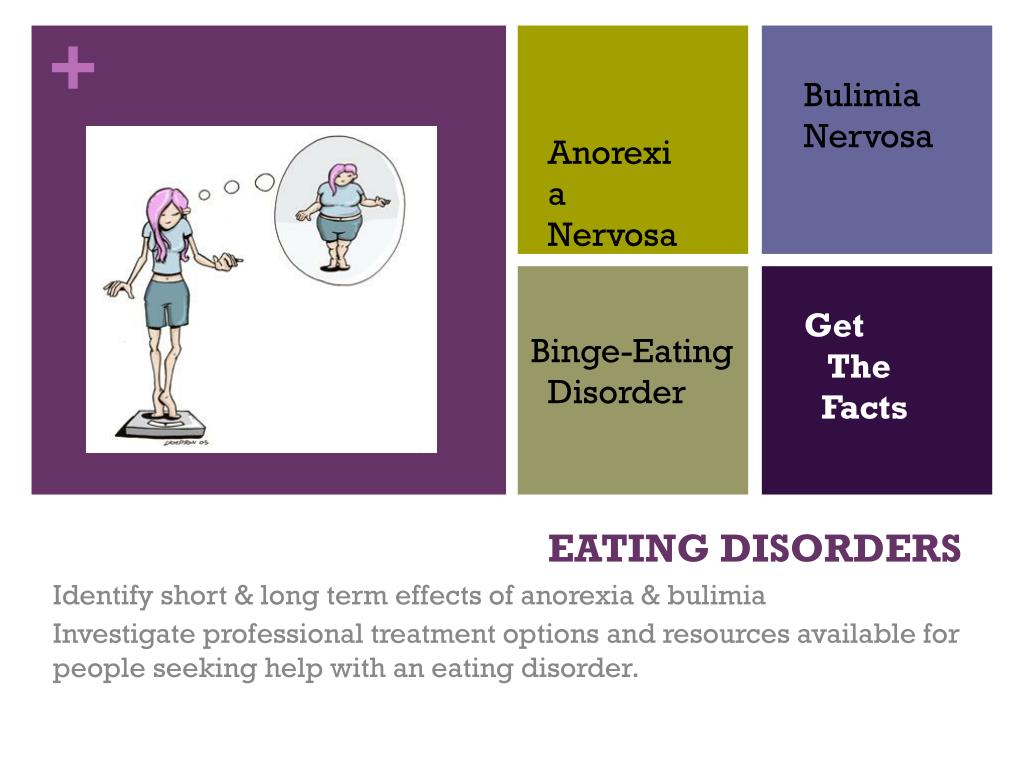
Eating disorders are real, treatable diseases. They frequently coexist with other illnesses such as depression, substance use, or anxiety disorders. Psychological and medicinal treatments are effective for many eating disorders. The earlier eating disorders are diagnosed and treated, the better the chances are for recovery.
How are eating disorders treated?
Typical treatment goals include restoring adequate nutrition, bringing weight to a healthy level, reducing excessive exercise, and stopping binging and purging behaviors. Treatment plans often are tailored to individual needs and may include one or more of the following:
Some patients also may need to be hospitalized to treat problems caused by malnutrition or to ensure they eat enough if they are very underweight. Complete recovery is possible.
About psychotherapies:
Specific forms of psychotherapy, or talk therapy—including a family-based therapy and cognitive behavioral approaches—have been shown to be useful for treating specific eating disorders.
The Maudsley approach, for example, where parents of teens with anorexia nervosa assume responsibility for feeding their child, appears to be very effective in helping teens gain weight and improve eating habits and moods.
Others may undergo cognitive behavioral therapy (CBT) to reduce or eliminate binge-eating and purging behaviors. CBT helps a child learn how to identify distorted or unhelpful thinking patterns and recognize and change inaccurate beliefs.
CBT helps a child learn how to identify distorted or unhelpful thinking patterns and recognize and change inaccurate beliefs.
About medications:
Medications such as antidepressants, antipsychotics, or mood stabilizers approved by the U.S. Food and Drug Administration (FDA) may also be helpful for treating eating disorders and other co-occurring illnesses such as anxiety or depression. Check the FDA website for the latest information on warnings, patient medication guides, or newly approved medications.
What is being done to better understand and treat eating disorders?
Researchers are finding that eating disorders are caused by a complex interaction of genetic, biological, psychological, and social factors. But many questions still need answers. Researchers are studying questions about genetics, brain function, and behavior to better understand and control eating disorders. Neuroimaging and genetic studies may also provide clues for how each person may respond to specific treatments.
Genetics: Mental health researchers are studying the various combinations of genes to determine if any DNA variations are associated with the risk of developing a mental disorder.
Neuroimaging: Magnetic resonance imaging (MRI), for example, may also lead to a better understanding of eating disorders. Neuroimaging already is used to identify abnormal brain activity in patients with schizophrenia, obsessive-compulsive disorder and depression. It may help researchers better understand how people with eating disorders process information, regardless of whether they have recovered or are still in the throes of their illness.
Behavioral or psychological research: Few studies of treatments for eating disorders have been conducted in the past due to the difficulty of this research. New studies currently underway, however, are aiming to remedy the lack of information available about treatment.
Additional Information & Resources:
Identifying and Treating Eating Disorders
How Emotional and Behavioral Disorders are Treated
Eating Disorders: Anorexia
Eating Disorders: Bulimia
Preventing Obesity and Eating Disorders in Adolescents (AAP Clinical Report)
Eating Disorders Clinical Trials (ClinicalTrials.
 gov) - A listing of clinical trials on eating disorders at the National Institutes of Health and across the country.
gov) - A listing of clinical trials on eating disorders at the National Institutes of Health and across the country.
- Last Updated
- 12/21/2020
- Source
- National Institute of Mental Health (NIMH)
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Eating disorders - treatment (therapy) of eating disorders by a psychologist, methods of psychotherapy
Eating disorders - psychologically conditioned behavioral syndromes associated with eating, leading to a deterioration in the quality of life and posing a health hazard.
In contrast to periodic violations of the diet, overeating, passion for a certain product or dish, a short-term diet, disorders are characterized by high frequency, inability to control oneself, unwillingness to see the problem. Eating disorders can cause the development of life-threatening conditions, therefore, if you find dangerous symptoms, do not try to cope with the problem on your own, but consult a doctor in Moscow by visiting the Center for the Study of Eating Disorders.
Eating disorders can cause the development of life-threatening conditions, therefore, if you find dangerous symptoms, do not try to cope with the problem on your own, but consult a doctor in Moscow by visiting the Center for the Study of Eating Disorders.
Article content:
- Types of violations
- Causes of occurrence and development
- Symptoms in disorders
- Troubleshooting
- Treatment approaches
- The main directions of psychotherapy
- What therapy is effective?
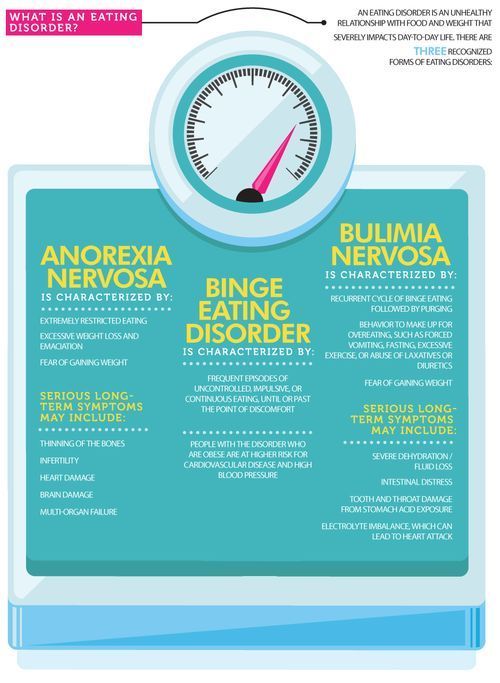
Types of disorders
The following disorders are described in the International Classification of Diseases (ICD-10):
- Anorexia nervosa is a deliberate and physiologically unjustified weight loss through diets, fasting, increased physical activity.
- Bulimia - bouts of overeating, after which a person carries out cleansing procedures for fear of gaining excess weight.

- Psychogenic overeating - food becomes the main defense against stress, psychological discomfort.
- Psychogenic vomiting - occurs spontaneously in hypochondriacal, dissociative disorders.
- Eating inedible - this diagnosis can be made in adults or adolescents. In children, such actions are caused by other factors and often do not require help, but only careful monitoring.
- Psychogenic loss of appetite.
Obesity is not an ED.
Causes of occurrence and development of disorders
Eating disorders arise due to personal, social, physiological, emotional factors. Often disorders develop under the influence of several causes.
But you should remember that you are not to blame for the problems, but you need help.
Symptoms in violations
Abnormal body weight may be due to eating disorders or indicate the development of other diseases.
If the body weight is within the normal range, one should seek therapy at the CIRP for the following symptoms:
- prolonged loss of appetite;
- eating inedible objects;
- aversion to food;
- recurrent uncontrollable desire to eat - overweight or obesity appears;
- getting rid of food by inducing vomiting or using laxatives;
- a strong feeling of discomfort, depression due to fullness or insufficient body weight, especially if it is not very different from the norm.

Often patients do not recognize deviations in eating behavior, do not see the true problem.
Diagnosis of disorders
Diseases that develop due to eating disorders can be life-threatening, causing damage to internal organs. It is better to diagnose them in the early stages. Treatment of RPP, diagnosis is carried out by several specialists with the appointment of laboratory tests.
The patient is examined by a psychiatrist and, if necessary, referred for a consultation with an endocrinologist, cardiologist, gastroenterologist or other specialists. A psychologist also works with him, and a nutritionist helps to choose a diet.
Approaches to treatment
For each patient, an individual program for the treatment of eating disorders is selected, which depends on the nature and cause of the disorder, the patient's condition at the time of contacting the "CIRP".
Psychiatrist makes a preliminary diagnosis, performs diagnostics.
In some cases (low body mass index, low or high blood pressure, life-threatening disorders of the kidneys, heart, stomach), the patient requires urgent hospitalization and intensive care. As soon as the acute symptoms are relieved by drug treatment, a psychologist can start working with the patient.
When is medication needed?
Depending on the condition of the patient suffering from eating disorders, the psychiatrist prescribes drug therapy.
Short-term use of antidepressants in the early stages of treatment is possible if bouts of overeating provoke depression or anxiety.
The main directions of psychotherapy
The number of diagnosed eating disorders is constantly growing.
New approaches to the treatment of ED are being developed in the EU, Russia, and the USA. CIRP specialists track the achievements of European and American colleagues using effective methods:
- cognitive-behavioral;
- family;
- dialectical behavioral.

The treating psychiatrist determines which type of eating disorder treatment a patient needs. Often several methods are used - simultaneously or alternately. They can offer both individual work, which helps a person to understand himself, increase self-esteem, and group psychotherapy, which will make it possible to realize that other people also face such problems and successfully overcome them.
Cognitive Behavioral Therapy (CBT)
A common method that has been proven to work. It combines the tools of cognitive therapy, which works with thinking errors, and the behavioral method, which allows a person to learn how to change their behavior to solve a problem.
The help of a psychologist allows you to identify errors in thinking, develop a new line of behavior, learn how to eliminate symptoms.
Family Based Therapy (FBT)
It was developed in a British clinic and has shown excellent results in patients suffering from eating disorders. A feature of this method is the work of a psychotherapist with the patient and his family members. The doctor will help the patient, his family to choose a course of action and together overcome the difficult stages of treatment.
A feature of this method is the work of a psychotherapist with the patient and his family members. The doctor will help the patient, his family to choose a course of action and together overcome the difficult stages of treatment.
Both individual sessions of psychotherapy with family members and group sessions are held. They allow you to track the changes that have occurred to a person as a result of an illness, find a way to help him, improve the psychological climate in the family.
Dialectical Behavior Therapy (DBT)
Dialectical Behavior Therapy aims to teach people with eating disorders alternative ways of emotional regulation that do not involve or avoid food.
Psychotherapy for the patient provides an opportunity to gain skills:
- safe emotional self-regulation;
- conscious eating behavior - focus on the feeling of hunger, the body's objective needs for nutrients;
- experiencing crisis situations - after a course of DBT psychotherapy, the likelihood of relapse of the disease decreases under severe stress;
- communication - the ability to build constructive, friendly relationships with people allows you to make a person's life comfortable, learn to cope with stress.
Group therapy
Group therapy for eating disorders develops communication skills. A person gets the opportunity to talk about the problem with other people, to understand that he is not alone in his experiences, and that what is happening to him is not his fault. This allows you to cope with the violation of body perception.
Treatment of disorders will be effective if a person learns to get positive emotions from sports, art, communication. Depending on the characteristics of the individual, interests and preferences of the patient, the "CIRPP" may recommend to him:
- dance and movement therapy;
- art therapy;
- interpersonal psychotherapy;
- body-oriented psychotherapy.
Interpersonal Psychotherapy (IPT)
Patients are advised to undergo interpersonal psychotherapy in order to treat their initial disorders. It allows you to help with the aggravated experience of grief that arose as a result of death or separation from a loved one. This type of psychotherapy is also effective in interpersonal role conflicts.
This type of psychotherapy is also effective in interpersonal role conflicts.
For effective therapy in adolescents, it is often necessary to work out the role transition, which will help to master new social roles, which is necessary at different stages of growing up. The treatment of eating disorders also affects the problem of interpersonal relationship deficit, which interpersonal psychotherapy helps to solve..
Dance movement therapy
Dance movement therapy is effective in the treatment of eating disorders. It allows you to solve the following tasks:
- better understand the body, its capabilities;
- improve self-esteem;
- develop communication skills;
- improve physical condition, provide physical activity with optimal load.
Like other types of therapy, classes are conducted under the guidance of psychotherapists. They help to cope with constraint, to be liberated, to create a benevolent atmosphere in the group.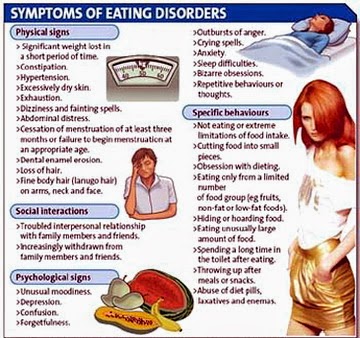
Dance movement therapy does not define the optimal number of sessions. The method is designed for long-term work until the patient feels the benefit, pleasure.
Art Therapy
Art helps a person to express feelings, so it can effectively treat eating disorders.
This method of treatment makes it possible to realize, accept, express feelings, get rid of negativity, get positive emotions. The patient learns to use alternative ways of emotional self-regulation that are not related to food.
Treatment can be carried out both in groups and individually. The psychologist, in agreement with the patient, selects an interesting type of activity: drawing, modeling, crafts from various materials. The effectiveness of treatment is not affected by the patient's creative potential, so you should not refuse art therapy because of the fear of not being able to cope with the tasks.
Which therapy is effective?
The treatment of the disease associated with eating disorders must be dealt with in a complex manner. In order for the treatment to help, CIRP specialists use different methods.
In order for the treatment to help, CIRP specialists use different methods.
Even with the same diagnosis, treatments that are effective for one patient may not be suitable for another. When choosing individual and group classes, you should not rely on the recommendations of friends or other patients.
But if you feel like expressing your feelings through dance, yoga, or woodwork, tell your mental health professional. CIRP offers a wide range of treatment methods that are used in clinics in Europe and the USA. Doctors will be able to choose effective therapy. Make an appointment in Moscow by phone +7(499) 703-20-51 or online.
Author: Korshunova Anna Aleksandrovna
Head of the Center for the Study of Eating Disorders,
psychiatrist, psychotherapist.
Effective and absurd treatments for eating disorders. Update 2019
Blog - Effective and absurd treatments for eating disorders.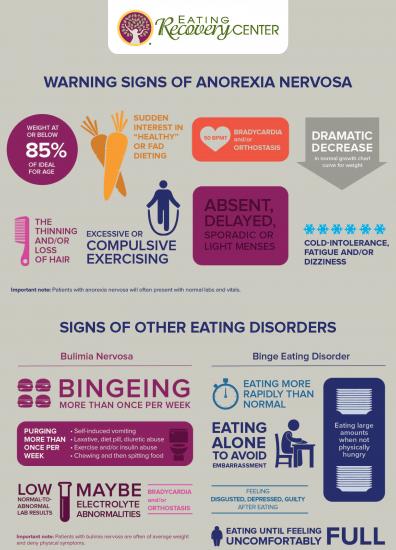 Update 2019
Update 2019
When it comes to treating eating disorders, it's important to note right away that each patient will respond differently to each approach. Even if they all suffer from the same type of disease.
The most popular treatments are listed below. Some of them have proven effective in the treatment of eating disorders in practice, and some have shown their complete ineffectiveness.
Psychotherapy
The psychotherapeutic approach generally addresses the thoughts, emotions, behaviors, thought patterns, motivations, and interpersonal relationships of patients. Treatments such as transactional analysis, cognitive analytic therapy, cognitive behavioral therapy (CBT), and dialectical behavioral psychotherapy (DBT) can be used.
This approach is usually practiced by psychologists. However, other professionals such as psychiatrists, psychotherapists, and counselors may use certain models of psychotherapy to treat eating disorders.
This method shows high efficiency, provided that you have selected a competent specialist.
Family approach
The family approach is most often used in the treatment of adolescents and children suffering from eating disorders. The family approach implies the direct involvement of the patient's family or close environment in the treatment process. The aim of this approach is to, along with the treatment of the patient himself, consult and educate relatives in parallel, so that they can provide him with the right care and support. Separate emphasis can also be placed on strengthening and improving family relationships.
At the Clinic for Eating Disorders A.V. Nazarenko, several specialists take part in family therapy, for example, a child psychologist paired with a specialist in eating disorders. Either the eating disorder specialist works with the teenager and the psychologist works with the parents to work together and work as a team.
Medication
Medication is usually needed if the eating disorder is accompanied by other psychological disorders such as depression, anxiety, insomnia or psychosis.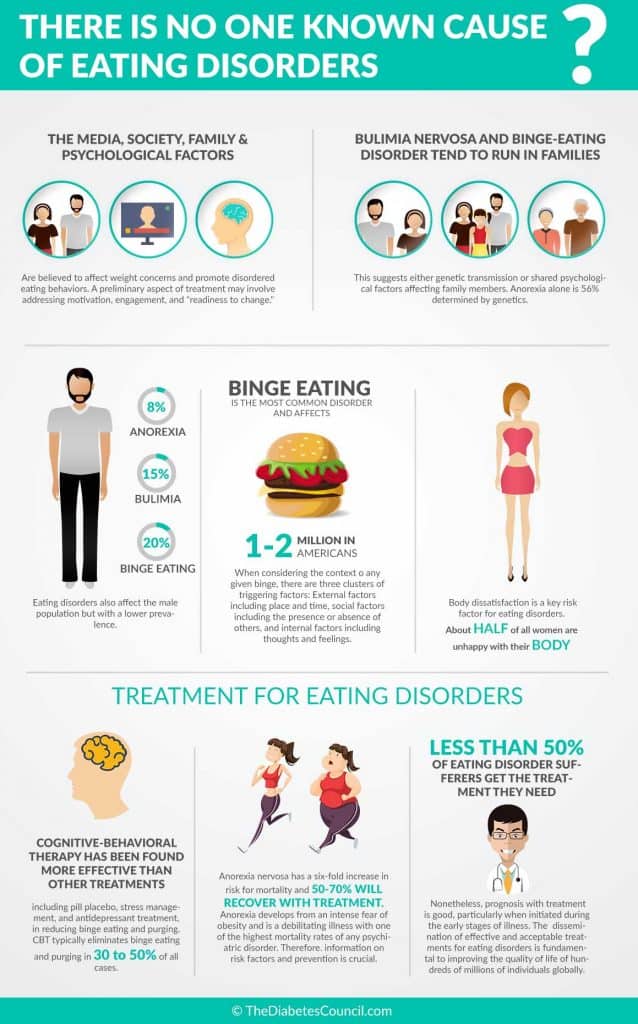 They are usually referred to as a group of so-called. " concomitant » diseases.
They are usually referred to as a group of so-called. " concomitant » diseases.
Medicines may be prescribed by psychiatrists, internists or general practitioners and should only be used in combination with other treatments. Medication alone does not cure an eating disorder.
Diet Therapy
Diet Therapy is commonly practiced by nutritionists and nutritionists. However, a regular therapist can also recommend a diet. Compliance with a certain diet is necessary so that during treatment the patient receives all the necessary vitamins and minerals with food. In addition, due to a properly selected diet, patients form the correct eating habits and change their eating behavior.
However, please note that a nutritionist does not have knowledge or education in the treatment of eating disorders. A nutritionist can only recommend and develop a proper nutrition plan. But practice shows that following diets and another restriction in nutrition in patients with eating disorders most often leads to breakdowns and aggravation of eating disorders.
Therefore, do not consult a nutritionist for the treatment of eating disorders. It's not that food addicts need to eat right, but that they break down on fried potatoes, ice cream, hamburgers. A nutritionist will not help in solving these problems.
Self-treatment
There is not a single food addict who does not try to cure himself. All sorts of books about bulimia, YouTube channels, manuals and courses are in great demand.
According to the statistics of the Russian Association of Eating Disorders, in 92% of cases, self-medication leads to breakdowns and aggravation of the symptoms of the disease. Not a single book or course has yet caused a stable remission for many years: as a result of reading, only a short-term weakening of the symptoms of the disease against the background of an emotional upsurge can occur.
Read more on self-treatment: I'll cure myself with books, absurd and effective ways to self-treat bulimia.
The most effective treatment for bulimia, anorexia, and compulsive overeating is to seek professional help from an eating disorder specialist.
Blog - Effective and absurd treatments for eating disorders. Update 2019
What is RPP? Causes, Symptoms, Signs and Treatments in 2019
Tags:
What is an Eating Disorder? Types of Eating Disorders Causes of Eating Disorders Signs and Symptoms of Eating Disorders Treatment of Eating Disorders Theses on Eating Disorders
7 Reasons Why You Start Gaining Weight By Trying To Lose Weight By Vomiting After Eating
Tags:
Many mistakenly believe that vomiting after eating helps to get rid of excess weight, especially if there is a "cleansing" after each meal. However, this is not always the case. If you want to know the truth about losing weight by inducing vomiting after eating, read this article.
Five irreversible health effects of bulimia
Tags:
Most girls and women are captivated by stereotypes and in pursuit of an ideal appearance and figure are constantly trying to change themselves.