Natural healing for depression and anxiety
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. SAMHSA’s 2020 National Survey on Drug Use and Health reports that approximately 19.3 million people aged 18 or older had a substance use disorder in the past year.
Alcohol
Data:
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.
 6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- The 2019 National Survey on Drug Use and Health reports that 139.7 million Americans age 12 or older were past month alcohol users, 65.8 million people were binge drinkers in the past month, and 16 million were heavy drinkers in the past month
- About 2.3 million adolescents aged 12 to 17 in 2019 drank alcohol in the past month, and 1.2 million of these adolescents binge drank in that period (2019 NSDUH)
- Approximately 14.5 million people age 12 or older had an alcohol use disorder (2019 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired.
 The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.
 3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Data from the 2019 NSDUH reports that 58.1 million people were current (i.e., past month) tobacco users. Specifically, 45.9 million people aged 12 or older in 2019 were past month cigarette smokers (2019 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey.
 Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018 - E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year.
 Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH) - An estimated 745,000 people had used heroin in the past year, based on 2019 NSDUH data
- In 2019, there were 10.1 million people age 12 or older who misused opioids in the past year. The vast majority of people misused prescription pain relievers (2019 NSDUH)
- An estimated 1.6 million people aged 12 or older had an opioid use disorder based on 2019 NSDUH data
- Opioid use, specifically injection drug use, is a risk factor for contracting HIV, Hepatitis B, and Hepatitis C. The CDC reports that people who inject drugs accounted for 9 percent of HIV diagnoses in the United States in 2016
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.
 5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH) - 2019 NSDUH data indicates that 48.2 million Americans aged 12 or older, 17.5 percent of the population, used marijuana in the past year
- Approximately 4.8 million people aged 12 or older in 2019 had a marijuana use disorder in the past year (2019 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 04/27/2022
Depression
Russian Academy of Medical Sciences
SCIENTIFIC CENTER FOR MENTAL HEALTH
DEPRESSION (from hope to certainty).
(INFORMATION FOR PATIENTS AND THEIR FAMILIES)
MOSCOW
2008
Oleichik I. V. - Candidate of Medical Sciences, Leading Researcher of the Department for the Study of Endogenous Mental Disorders and Affective States
V. - Candidate of Medical Sciences, Leading Researcher of the Department for the Study of Endogenous Mental Disorders and Affective States
© 2008, Oleichik I.V.
© 2008, NTsPZ RAMS
The vast experience accumulated by mankind and reflected in many literary works convincingly shows that sadness (sadness, spleen) has always gone side by side with people, being one of the natural human emotions. None of us is immune from failures, illness, breakups, loss of loved ones, financial collapse. Each person can face something inevitable and inevitable, when it seems that life loses its meaning, and despair becomes boundless. However, normally, sadness, sadness and melancholy, as natural reactions to traumatic events, weaken over time and the person's condition returns to normal without special treatment. The situation is different with depressions, which are mental disorders that differ from natural physiological reactions in greater intensity, special severity of experiences and persistence of manifestations. True depression rarely goes away on its own, requiring persistent, sometimes long-term treatment.
True depression rarely goes away on its own, requiring persistent, sometimes long-term treatment.
A depressive state (from the Latin word depressio - suppression, oppression) is a disease that concerns not only an individual specific sick person, but is also a significant burden of modern society, since it is spreading more and more widely in the world, causing enormous damage to the health of the population and the state. economy. And this applies to all countries, regardless of their level of social development. Every year, at least 200 million people in the world fall ill with depression. Perhaps these figures are even higher, since most victims of depression do not seek help because they are not aware of the painfulness of their condition. Scientists have calculated that almost one in five people who have reached adulthood will experience at least one episode of depression during their lifetime.
In the most general sense, a depressive state is one of the possible forms of a person's response to the impact of stress factors. In some cases, depression can be triggered by external negative influences, for example, mental trauma, excessive educational or work overload, infection or other serious somatic disease, traumatic brain injury, changes in the hormonal background, which is especially important for the female body, regular certain medications, such as hormones, blood pressure medications, alcohol or other drug abuse. In other cases, depressive states develop as a manifestation of such mental illnesses, in which the main influence is heredity or characteristics of the nervous system (cyclothymia, dysthymia, manic-depressive psychosis, schizophrenia, etc.). If, based on the description of depressive symptoms set out later in our brochure, you realize that you have indeed developed a depressive state, do not fall into despair, do not “try to control yourself”, remember that depression is not a manifestation of weakness of will or character, on the contrary, weakening of volitional qualities is one of the main symptoms of depression.
In some cases, depression can be triggered by external negative influences, for example, mental trauma, excessive educational or work overload, infection or other serious somatic disease, traumatic brain injury, changes in the hormonal background, which is especially important for the female body, regular certain medications, such as hormones, blood pressure medications, alcohol or other drug abuse. In other cases, depressive states develop as a manifestation of such mental illnesses, in which the main influence is heredity or characteristics of the nervous system (cyclothymia, dysthymia, manic-depressive psychosis, schizophrenia, etc.). If, based on the description of depressive symptoms set out later in our brochure, you realize that you have indeed developed a depressive state, do not fall into despair, do not “try to control yourself”, remember that depression is not a manifestation of weakness of will or character, on the contrary, weakening of volitional qualities is one of the main symptoms of depression.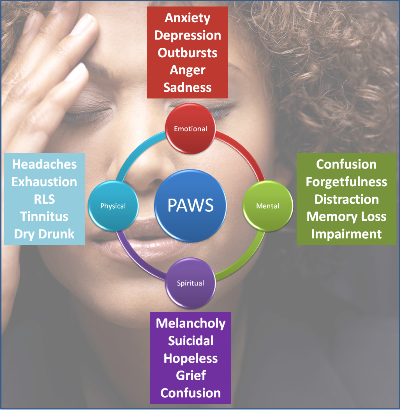 Depression is a disease like rheumatism, arthritis or hypertension, it responds well to treatment, resulting in almost always a full recovery. You should not blame yourself for the occurrence of depression, it does not indicate either your fault, or your weakness, or the possible development of a more severe mental pathology. Below we will tell you about the symptoms of depression, which can be extremely diverse.
Depression is a disease like rheumatism, arthritis or hypertension, it responds well to treatment, resulting in almost always a full recovery. You should not blame yourself for the occurrence of depression, it does not indicate either your fault, or your weakness, or the possible development of a more severe mental pathology. Below we will tell you about the symptoms of depression, which can be extremely diverse.
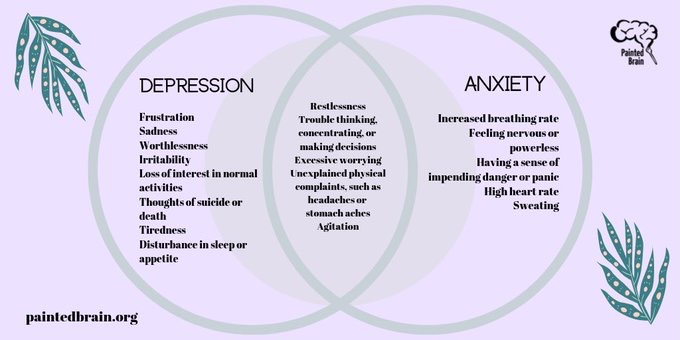
Manifestations of depression
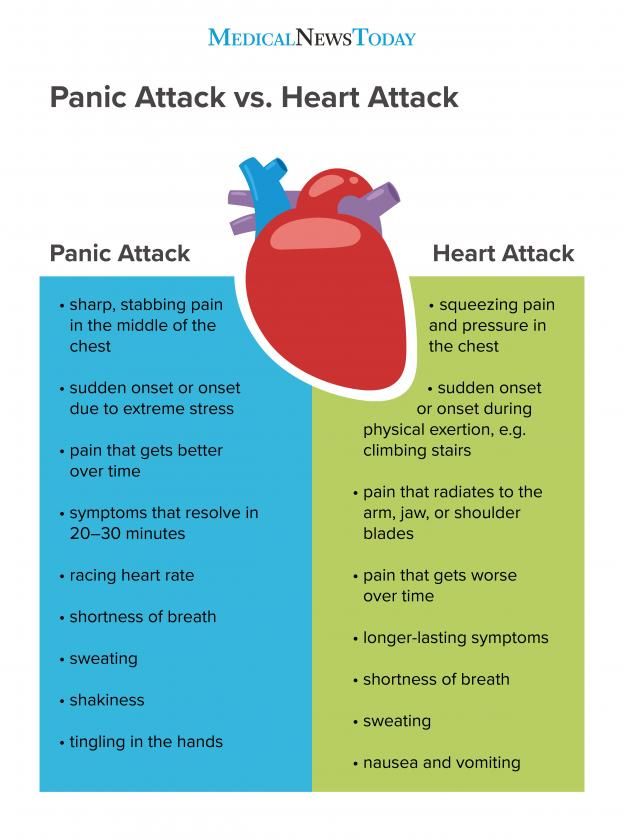
Manifestations of depression can be very different. Depressive states can be manifested by a violation of almost all aspects of mental life: mood, memory, will, activity, which is expressed in the appearance of sadness, sadness, mental and muscle retardation, lasting at least 2 weeks. Depressed mood during depression can manifest itself as mild sadness, sadness, and boundless despair. Often it is accompanied by a feeling of melancholy, unbearable heaviness in the soul, with excruciating pain behind the sternum, a feeling of hopelessness, deep depression, hopelessness, helplessness, despair and uncertainty.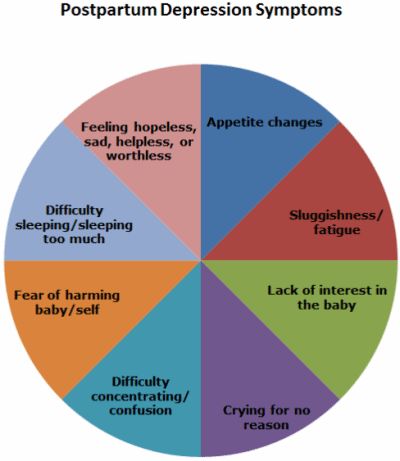 At the same time, the patient is completely immersed in his gloomy experiences, and external events, even the most joyful ones, do not affect him, do not affect his mood, and sometimes even worsen the latter. A constant "companion" of a depressive mood is also anxiety of varying severity: from mild anxiety or tension to violent excitement, riot. Anxiety and bad mood arise at the mere thought of the need to make some kind of decision or change your plans due to suddenly changed circumstances. Anxiety can also manifest itself on the physical (bodily) level in the form of belching, intestinal cramps, loose stools, frequent urination, shortness of breath, palpitations, headaches, increased sweating, etc.
At the same time, the patient is completely immersed in his gloomy experiences, and external events, even the most joyful ones, do not affect him, do not affect his mood, and sometimes even worsen the latter. A constant "companion" of a depressive mood is also anxiety of varying severity: from mild anxiety or tension to violent excitement, riot. Anxiety and bad mood arise at the mere thought of the need to make some kind of decision or change your plans due to suddenly changed circumstances. Anxiety can also manifest itself on the physical (bodily) level in the form of belching, intestinal cramps, loose stools, frequent urination, shortness of breath, palpitations, headaches, increased sweating, etc.
The picture of depression is complemented by the disappearance of desires, interests, a pessimistic assessment of everything around, ideas of one's own low value and self-blame. Deficiency of vital impulses is manifested in patients with a variety of symptoms - from lethargy, physical weakness to a state of weakness, loss of energy and complete impotence. Where an important decision is required, a choice between different options, human activity is sharply hampered. Depressed people are well aware of this: they complain that insignificant everyday tasks, small issues that used to be solved almost automatically, take on the significance of complex, painful, insoluble problems. At the same time, a person feels that he began to think, act and speak slowly, notes the suppression of instincts (including food and sexual instincts), the suppression or loss of the instinct of self-preservation and the lack of the ability to enjoy life up to complete indifference to what used to be liked evoked positive emotions.
Where an important decision is required, a choice between different options, human activity is sharply hampered. Depressed people are well aware of this: they complain that insignificant everyday tasks, small issues that used to be solved almost automatically, take on the significance of complex, painful, insoluble problems. At the same time, a person feels that he began to think, act and speak slowly, notes the suppression of instincts (including food and sexual instincts), the suppression or loss of the instinct of self-preservation and the lack of the ability to enjoy life up to complete indifference to what used to be liked evoked positive emotions.
People suffering from depression often feel "stupid", "mentally retarded", "feeble-minded". Thinking in depression becomes viscous, painful, requires special efforts, one mental image is hardly forced out by the next. The sick person is oppressed by the feeling of his own intellectual insolvency, professional collapse. Depressed patients can hardly describe their painful experiences to the doctor.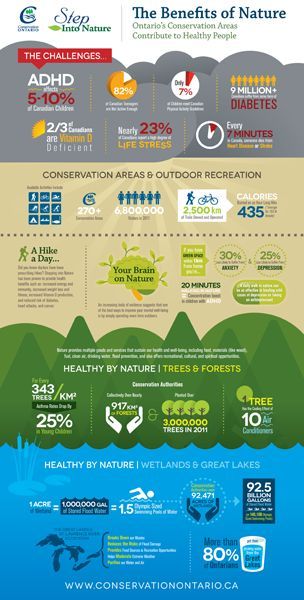 Only after getting out of depression, many of them say that the mood at that moment was lowered, thinking was slow, all undertakings (including treatment) seemed in vain, and the years lived were empty and useless. However, at the time of the first visit to the doctor, they could not explain this because of the almost complete absence of thoughts in their heads, “para-lich of thinking”. With depression, there are also often complaints of memory loss, which is why those suffering from it assume that they have "Alzheimer's disease", "schizophrenia", "senile dementia", which is not true. Especially often these complaints are found in depressions that develop in adolescence.
Only after getting out of depression, many of them say that the mood at that moment was lowered, thinking was slow, all undertakings (including treatment) seemed in vain, and the years lived were empty and useless. However, at the time of the first visit to the doctor, they could not explain this because of the almost complete absence of thoughts in their heads, “para-lich of thinking”. With depression, there are also often complaints of memory loss, which is why those suffering from it assume that they have "Alzheimer's disease", "schizophrenia", "senile dementia", which is not true. Especially often these complaints are found in depressions that develop in adolescence.
Typical story
Aleksey, 18 years old, 1st year student of a technical university, describes his condition during depression as follows:
“From childhood, I was fond of technology and modeling, I could read special literature for hours, won school and regional olympiads in mathematics and physics. After graduating from school, my dream came true - I brilliantly passed the exams to a prestigious university. Then it seemed to me that the whole world was at my feet, I flew with happiness "as if on wings." In September, I happily began to study. At the beginning, everything worked out well, but after 2 months I began to notice that it was becoming increasingly difficult for me to absorb what I read, I did not remember the simplest text, I could not solve problems that I used to “click like nuts”. Trying to achieve success through many hours of brainstorming or drinking a few cups of coffee led to the fact that I completely stopped thinking about anything. It seemed to me that I was "finally and irreversibly stupid." At night I sobbed, wrapped in a blanket and thought about how best to commit suicide. Luckily, I met a senior in the library and shared my problems with him. My new acquaintance said that he experienced something similar and advised me to contact the psychiatrist of the student clinic. After the examination, I was diagnosed with juvenile depression and sent for treatment to a specialized medical center.
Then it seemed to me that the whole world was at my feet, I flew with happiness "as if on wings." In September, I happily began to study. At the beginning, everything worked out well, but after 2 months I began to notice that it was becoming increasingly difficult for me to absorb what I read, I did not remember the simplest text, I could not solve problems that I used to “click like nuts”. Trying to achieve success through many hours of brainstorming or drinking a few cups of coffee led to the fact that I completely stopped thinking about anything. It seemed to me that I was "finally and irreversibly stupid." At night I sobbed, wrapped in a blanket and thought about how best to commit suicide. Luckily, I met a senior in the library and shared my problems with him. My new acquaintance said that he experienced something similar and advised me to contact the psychiatrist of the student clinic. After the examination, I was diagnosed with juvenile depression and sent for treatment to a specialized medical center. After 2 months, I felt completely healthy, returned to my studies and caught up with my classmates.
After 2 months, I felt completely healthy, returned to my studies and caught up with my classmates.
Depression can also be accompanied by real setbacks: for example, a decrease in academic performance, the quality of work, family conflicts, sexual disorders and their consequences for personal relationships. As a rule, the significance of these failures is exaggerated and as a result there is a false sense of the irreparability of what happened, "the collapse of all hopes."
Another generally recognized danger of depression is the possibility of suicidal thoughts, which often lead to suicide attempts. The condition of a person suffering from depression can suddenly deteriorate sharply, which happens either without clear external causes, or under the influence of traumatic situations, unpleasant news. It is during these hours, and sometimes even minutes, that a fatal decision is made. Factors that increase the risk of suicide in depression are past suicide attempts, the severity and duration of the depressive state, the presence of anxiety in its structure, prolonged insomnia, loneliness or alienation in the family, alcohol and drug abuse, loss of work and a sharp change in lifestyle, as well as relatives commit suicide.
Typical story
Eugene E., 35 years old, leading manager of the company.
Almost all my life, my career went “on the ascending”, the goals set were clear, clear and achievable. The marriage was extremely harmonious, two beloved children grew up. He devoted almost all the time to the affairs of the company, occasionally, once every 1-2 months, he escaped with his family out of town, to the country. He often lacked sleep, stayed late at work, took home assignments, and was deeply worried about the affairs of the company. Gradually, irritability, fatigue, insomnia, difficulty concentrating appeared, more and more often he suffered a “fiasco” in intimate life. Thoughts appeared that life was lived in vain, that it is a "chain of tragic mistakes" that led to a dead end. He began to believe that the choice of work, friends, family was wrong, for which now "retribution has come." Analyzing the past years for a long time, he found more and more evidence and examples of his "duplicity, hypocrisy, insincerity, etc. " I realized that the only way to solve all problems is to voluntarily leave this life. At the same time, he believed that by this act he would free the family from the “burden”, “loser”, “loser”. I decided, having locked myself in the garage, to get poisoned by the exhaust gases of the car. However, by chance, in a semi-conscious state, he was discovered by an employee of a garage cooperative. He explained what happened as an "accident". The thought of leaving life did not leave the patient. I decided to shoot myself with a gas pistol, which I had long ago acquired for self-defense. After a shot in the mouth, in a serious condition, he was taken to the Research Institute. Sklifasovsky, from where he was discharged a week later. The alarmed wife, suspecting something was wrong, decided to consult her husband with a psychiatrist. He was admitted to the clinic. He agreed to this only out of respect for family relations, he himself believed that treatment by psychiatrists was completely useless, because.
" I realized that the only way to solve all problems is to voluntarily leave this life. At the same time, he believed that by this act he would free the family from the “burden”, “loser”, “loser”. I decided, having locked myself in the garage, to get poisoned by the exhaust gases of the car. However, by chance, in a semi-conscious state, he was discovered by an employee of a garage cooperative. He explained what happened as an "accident". The thought of leaving life did not leave the patient. I decided to shoot myself with a gas pistol, which I had long ago acquired for self-defense. After a shot in the mouth, in a serious condition, he was taken to the Research Institute. Sklifasovsky, from where he was discharged a week later. The alarmed wife, suspecting something was wrong, decided to consult her husband with a psychiatrist. He was admitted to the clinic. He agreed to this only out of respect for family relations, he himself believed that treatment by psychiatrists was completely useless, because. his situation is hopeless and no medicines will help here, but will only "stupefy" his psyche. However, after two weeks of taking a modern antidepressant, the patient's point of view changed. Everything began to look not so bleak and hopeless, interest in work and life in general returned, I began to feel more cheerful, more energetic, interest in intimate life appeared. He took work to the clinic, called up colleagues. After two months of treatment, he fully returned to his usual life. With bewilderment, he recalled his thoughts about insolvency, the collapse of life, suicide. He took the drug prophylactically for about six months, then, on the recommendation of a doctor, he gradually reduced the dose and stopped taking it. Over the next two years, the condition remained stable, career growth continued, another child was born.
his situation is hopeless and no medicines will help here, but will only "stupefy" his psyche. However, after two weeks of taking a modern antidepressant, the patient's point of view changed. Everything began to look not so bleak and hopeless, interest in work and life in general returned, I began to feel more cheerful, more energetic, interest in intimate life appeared. He took work to the clinic, called up colleagues. After two months of treatment, he fully returned to his usual life. With bewilderment, he recalled his thoughts about insolvency, the collapse of life, suicide. He took the drug prophylactically for about six months, then, on the recommendation of a doctor, he gradually reduced the dose and stopped taking it. Over the next two years, the condition remained stable, career growth continued, another child was born.
Depression is also characterized by sleep disturbances, occurring in approximately 80% of patients. As a rule, these are early awakenings with the inability to fall asleep, lack of a sense of sleep, difficulty falling asleep. These disorders, as well as restless sleep with unpleasant dreams, are often the very first symptoms of incipient depression.
These disorders, as well as restless sleep with unpleasant dreams, are often the very first symptoms of incipient depression.
If the depression is not deep, it is sometimes difficult to recognize it. This is due to the fact that people are ashamed to tell others about their problems, to admit to "weaknesses". Quite often, especially in Russia, depressive states are masked by alcohol abuse (“vodka heals”). In addition, often patients suffering from depression, in order to "shake themselves up", "throw into all serious", engage in casual sex, are fond of gambling or extreme sports, leave to serve on a contract in "hot spots", lead an idle lifestyle with constant attendance at entertainment events. Surrounding people, relatives who do not have psychiatric knowledge, often accuse them of debauchery, drunkenness, riotous lifestyle, parasitism. Meanwhile, this behavior is a kind of “cry for help”, an attempt to fill the spiritual emptiness brought by depression with new acquaintances and impressions.
Depressive conditions can occur in shallow forms that are easily treatable, but at least a third of depressions are more severe. Such depressions are characterized by:
- ideas of guilt, sometimes reaching the degree of delirium, i.e. unshakable conviction in their sinfulness, low value (patients consider themselves great sinners, believe that because of them all relatives and Mankind will die, that they are “moral freaks” from birth, supposedly deprived of the foundations of morality and a sense of empathy for other people that they have no place on earth They find in their past numerous "confirmations" of what has been said above, they believe that the doctor and other patients are aware of these transgressions and express contempt and indignation with their facial expressions and gestures, but in the words “they hide, deny the obvious.” Both the patients themselves and their relatives must remember this in order to prevent the impending threat in time: remove all firearms, piercing and cutting objects, ropes, potent drugs and poisonous close household fluids, close windows or shutters, do not let the patient go anywhere alone.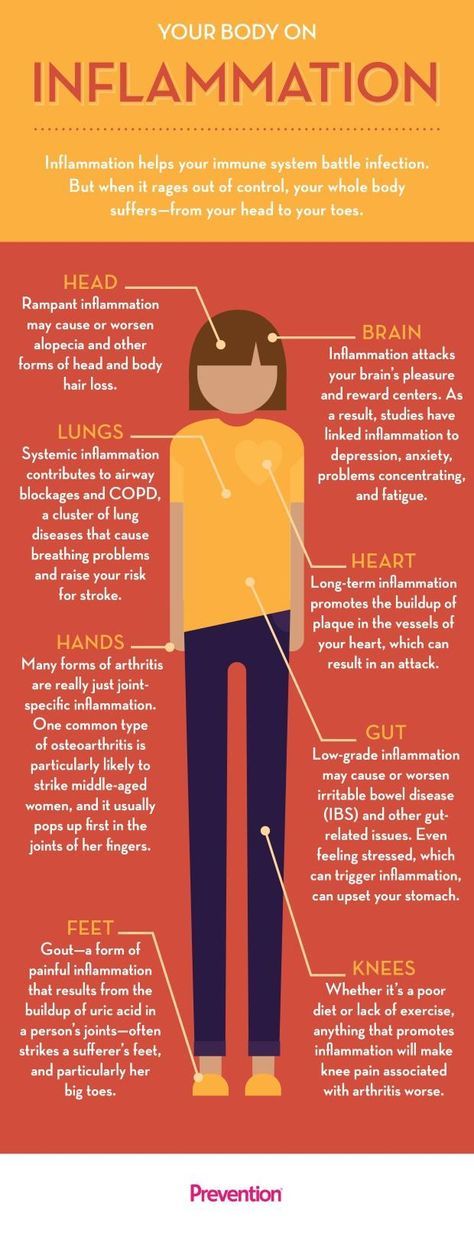 If these ideas become persistent and cannot be dissuaded, it is urgent to seek advice from a psychiatrist. neurological institution or call a psychiatrist at home.
If these ideas become persistent and cannot be dissuaded, it is urgent to seek advice from a psychiatrist. neurological institution or call a psychiatrist at home.
- mood swings during the day: in typical cases, the patient, waking up, immediately feels longing. Sometimes, even before full awakening, through a dream he experiences a painful premonition of a heavy coming morning. In the evening, the state of health improves somewhat.
- the patient may experience a feeling of unmotivated hostility towards relatives, friends, constant internal discontent and irritation, which makes him unbearable for the family.
- in a number of people suffering from depression, constant doubts, fear for the health and well-being of loved ones, obsessive ones, come to the fore. arising against the will, ideas about the misfortunes and troubles of family members.
Typical story
Dmitry Petrovich, 58 years old, teacher.
“After minor troubles at work, I began to feel incomprehensible anxiety and agitation.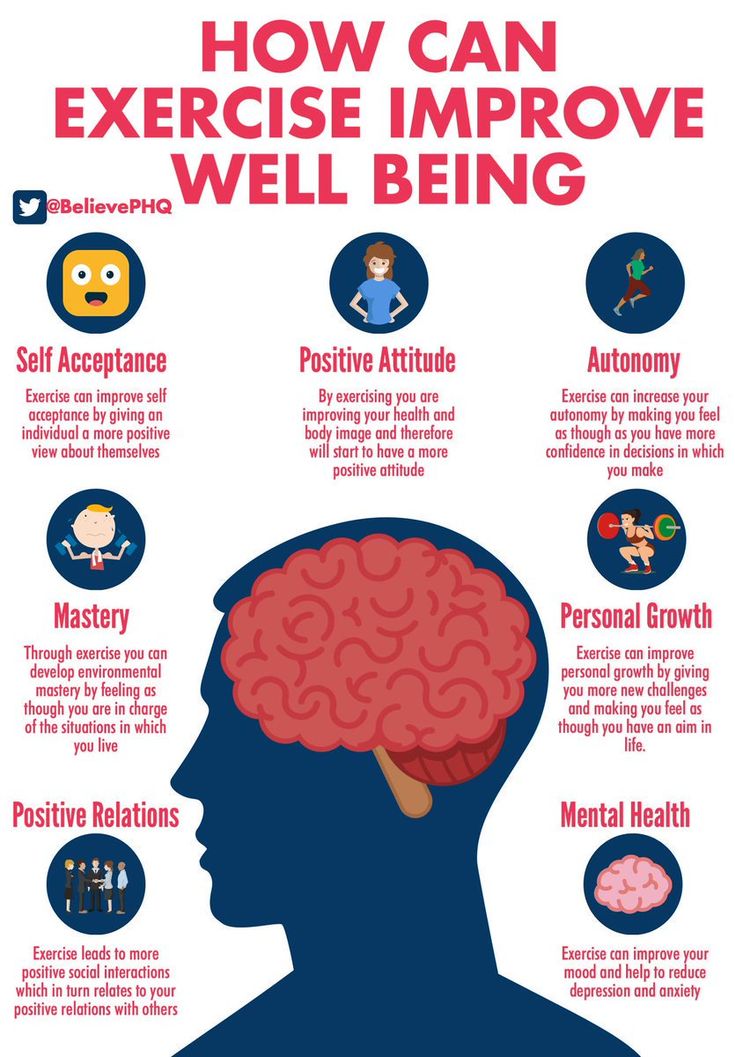 Unpleasant thoughts came into my head that I did something wrong at work, because of which I double-checked everything many times and went home later than everyone else. But even at home, the anxiety did not let go: as soon as the daughter or wife lingered for at least half an hour, terrible pictures of traffic accidents or violence were drawn in the imagination. I fell asleep only in the morning, got up broken and felt sleepy all day. I took Valerian, Corvalol, but it practically did not help. At work, they hinted whether I should take a vacation. Friends advised me to consult a neuropathologist, but he did not find his pathology and sent me to a psychiatrist. I was diagnosed with anxiety depression. After a course of outpatient treatment, I completely recovered.”
Unpleasant thoughts came into my head that I did something wrong at work, because of which I double-checked everything many times and went home later than everyone else. But even at home, the anxiety did not let go: as soon as the daughter or wife lingered for at least half an hour, terrible pictures of traffic accidents or violence were drawn in the imagination. I fell asleep only in the morning, got up broken and felt sleepy all day. I took Valerian, Corvalol, but it practically did not help. At work, they hinted whether I should take a vacation. Friends advised me to consult a neuropathologist, but he did not find his pathology and sent me to a psychiatrist. I was diagnosed with anxiety depression. After a course of outpatient treatment, I completely recovered.”
- in many cases, depression is characterized by unpleasant sensations in the body, disturbances in the activity of internal organs in the absence of objective signs of true somatic, i.e. non-mental illness. At the same time, many patients constantly report pain, internal discomfort.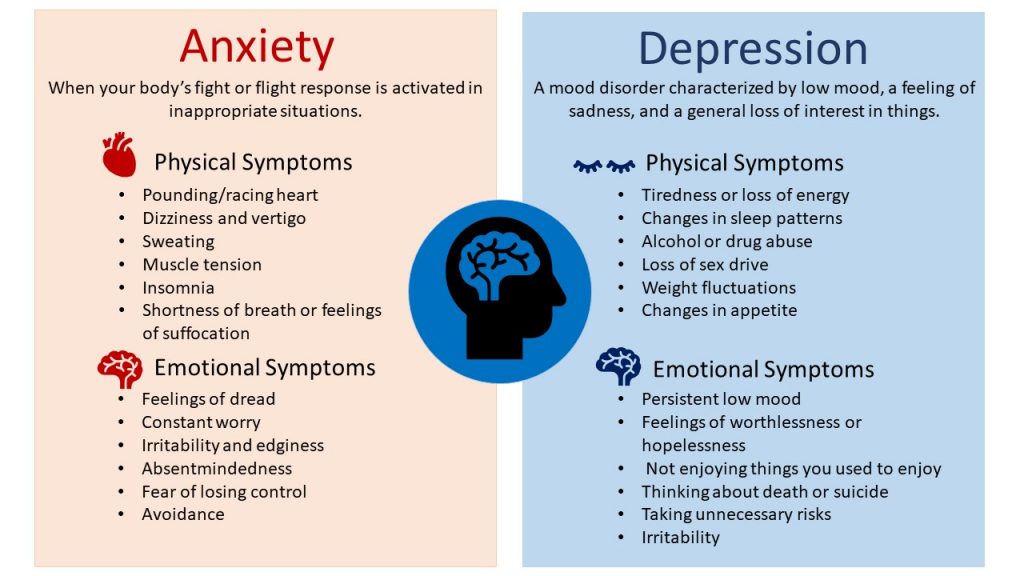 Some complain of headaches, pains in the stomach, joints, lower back, others - of disorders in the intestines: constipation, indigestion, irritation of the colon, others pay attention to a decrease in sexual desire and potency. In women, menstruation often becomes painful and irregular. Approximately 50% of depressed people at the doctor's office complain of such physical ailments, without mentioning the depressed mood or state of mind underlying the depression. Experiencing chronic pain or other unpleasant sensations in the body, patients may not realize that they are suffering from depression, even with severe melancholy, considering the latter a reaction to painful bodily discomfort.
Some complain of headaches, pains in the stomach, joints, lower back, others - of disorders in the intestines: constipation, indigestion, irritation of the colon, others pay attention to a decrease in sexual desire and potency. In women, menstruation often becomes painful and irregular. Approximately 50% of depressed people at the doctor's office complain of such physical ailments, without mentioning the depressed mood or state of mind underlying the depression. Experiencing chronic pain or other unpleasant sensations in the body, patients may not realize that they are suffering from depression, even with severe melancholy, considering the latter a reaction to painful bodily discomfort.
- some patients are convinced that they have some rare and difficult to diagnose disease and insist on numerous examinations in general medical institutions. Doctors call this condition masked (hidden) depression, in which a person may experience pain in the head, in the limbs, behind the sternum, in the abdomen and in any other parts of the body, he may be haunted by anxious fears, he may suffer from insomnia or, on the contrary, too much sleep.
- Patients may experience disturbances in the cardiovascular system, skin itching or lack of appetite. All of these are manifestations of depression.
- the pathological sensations that patients experience during such depressions are quite real, painful, but they are the result of a special mental state, and not an internal disease. It must be remembered that the frequency of latent depressions exceeds the number of explicit ones many times over.
- with such depression, patients, as a rule, also have a changed attitude towards food: they can go without food for a long time and not feel hungry, and sitting down at the table, eat only 1-2 spoons - they have neither strength nor desire for more .
- a sign of depression can serve as a weight loss of more than 5 kg. within a month. In some people, especially women, the appetite for depression, on the contrary, increases, sometimes reaching the level of excruciating hunger, accompanied by severe weakness and pain in the epigastric region. In some cases, food is taken in excess due to an increased craving for sweets or attempts to distract oneself from painful thoughts by frequent eating.
In some cases, food is taken in excess due to an increased craving for sweets or attempts to distract oneself from painful thoughts by frequent eating.
Thus, we see that depression is a disease with many different manifestations that do not go away on their own, requiring special, sometimes long-term, medical intervention. Therefore, when the symptoms described above appear, it is necessary to seek help from a psychiatrist who will prescribe and monitor antidepressant treatment.
TREATMENT OF DEPRESSIVE DISORDERS
To date, it can be argued that the vast majority of cases of depression respond well to treatment. According to modern views, effective treatment of depression consists of a combination of pharmacotherapy, psychotherapy and, if necessary, other types of treatment. At the same time, the main role in therapy, of course, belongs to antidepressants - drugs specially designed for the treatment of various types of depression.
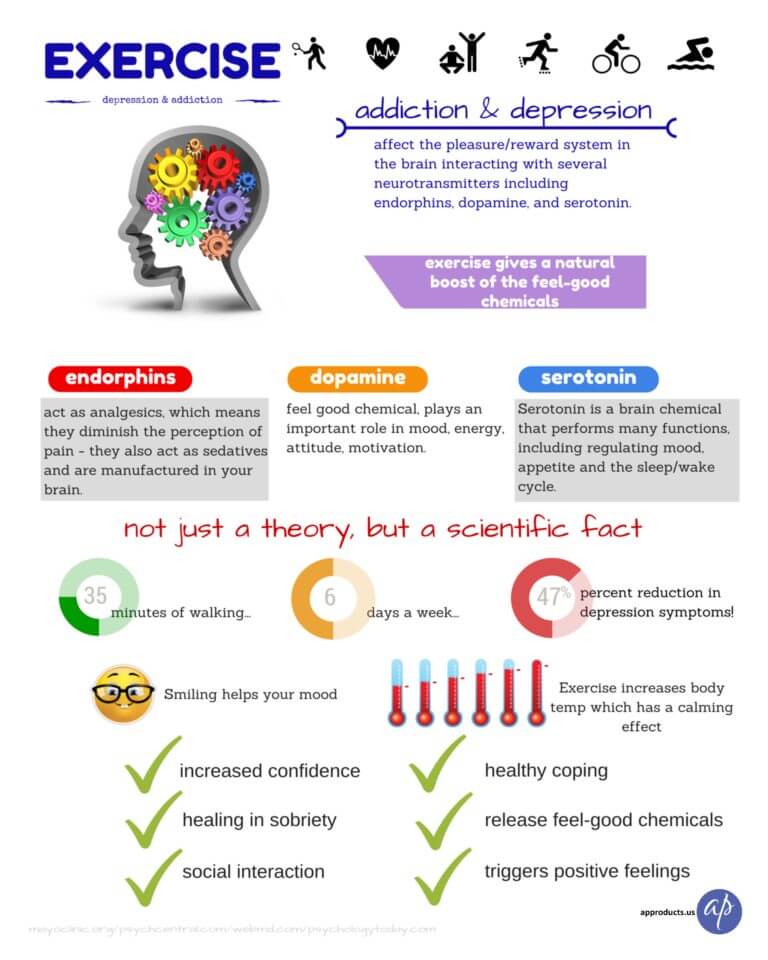
The creation of antidepressants is based on the discovery of scientists that depression develops as a result of a violation of the mechanism of biochemical transmission of nerve impulses in the brain regions responsible for mood, behavior, response to stress, sleep and wakefulness, appetite and some other functions. To ensure the coordination of the work of all these functional divisions, the brain sends special "commands" to them in the form of chemical impulses transmitted from the processes of one nerve cell (neuron) to the processes of another. This transmission is carried out with the help of chemical mediators (neurotransmitters), which, after transmitting a signal, partially return to the original neuron. This process is called neurotransmitter reuptake. Thanks to him, the number of mediators in the microscopic space between the processes of neurons (in the so-called synaptic cleft) decreases, which means that the necessary signals are transmitted worse. Numerous studies have shown that mediators of various structures, in particular, norepinephrine and serotonin, are involved in the transmission of signals that ensure the normal functioning of the nervous system. The first of them has a general activating effect, maintains the level of wakefulness of the body and takes part in the formation of adaptive reactions, and the second has the main antidepressant effect, controls impulsive actions, anxiety, aggressiveness, sexual behavior, falling asleep, feeling of pain, therefore serotonin is called sometimes a "good mood" regulator.
To ensure the coordination of the work of all these functional divisions, the brain sends special "commands" to them in the form of chemical impulses transmitted from the processes of one nerve cell (neuron) to the processes of another. This transmission is carried out with the help of chemical mediators (neurotransmitters), which, after transmitting a signal, partially return to the original neuron. This process is called neurotransmitter reuptake. Thanks to him, the number of mediators in the microscopic space between the processes of neurons (in the so-called synaptic cleft) decreases, which means that the necessary signals are transmitted worse. Numerous studies have shown that mediators of various structures, in particular, norepinephrine and serotonin, are involved in the transmission of signals that ensure the normal functioning of the nervous system. The first of them has a general activating effect, maintains the level of wakefulness of the body and takes part in the formation of adaptive reactions, and the second has the main antidepressant effect, controls impulsive actions, anxiety, aggressiveness, sexual behavior, falling asleep, feeling of pain, therefore serotonin is called sometimes a "good mood" regulator. A decrease in the number of mediators in the synaptic cleft causes symptoms of depression, while an increase, on the contrary, prevents their appearance. The ability of some drugs in one way or another to increase the concentration of mediators in the synaptic cleft allows them to be used as antidepressants.
A decrease in the number of mediators in the synaptic cleft causes symptoms of depression, while an increase, on the contrary, prevents their appearance. The ability of some drugs in one way or another to increase the concentration of mediators in the synaptic cleft allows them to be used as antidepressants.
Now antidepressants are used in Russia, which can be conditionally divided into 4 generations according to the time of creation.
The first antidepressants to find wide clinical use were tricyclic drugs: amitriptyline and imipramine. They have a fairly powerful effect on most depressive states by blocking the reuptake of both norepinephrine and serotonin. However, the real clinical effect of these drugs is significantly offset by their undesirable side effects, which drastically reduce the quality of life of patients during treatment. Side effects of tricyclic antidepressants arise due to the nonspecificity of their effect on receptor structures. Acting in addition to the serotonin and norepinephrine system and other neurotransmitters (acetylcholine, histamine, dopamine), these antidepressants cause side effects such as urinary retention, dry mucous membranes, constipation, palpitations, fluctuations in blood pressure, confusion, tremor, sexual dysfunction. functions, weight gain. In such cases, it is necessary to prescribe other drugs to correct side effects or reduce the therapeutic dose of drugs, which naturally affects the effectiveness of the antidepressant action. It has been observed that up to 50% of patients refuse to take tricyclic antidepressants due to severe side effects. For the same reason, physicians are less likely to prescribe these drugs to patients on an outpatient basis.
functions, weight gain. In such cases, it is necessary to prescribe other drugs to correct side effects or reduce the therapeutic dose of drugs, which naturally affects the effectiveness of the antidepressant action. It has been observed that up to 50% of patients refuse to take tricyclic antidepressants due to severe side effects. For the same reason, physicians are less likely to prescribe these drugs to patients on an outpatient basis.
The situation was somewhat improved by the introduction into practice of drugs of the second generation - tetracyclic antidepressants, which, along with the ability to block the reuptake of norepinephrine and serotonin, could also affect some other receptors. Being analogues of tricyclic compounds, these drugs have antidepressant activity comparable to them, but unlike their predecessors, they are safer, since they cause unwanted side effects much less often. In addition to the antidepressant, mianserin (lerivon) has a clear sedative, anti-anxiety and hypnotic effect. Maprotiline (Ludiamil) has a mild balanced antidepressant effect. In general, these drugs are able to cure mild to moderate depression, but are ineffective in patients with severe depression.
Maprotiline (Ludiamil) has a mild balanced antidepressant effect. In general, these drugs are able to cure mild to moderate depression, but are ineffective in patients with severe depression.
To date, antidepressants of the 3rd generation, such as fluoxetine (Prozac), fluvoxamine (Fevarin), paroxetine (Paxil), sertraline (Zoloft), citalopram (Cipralex) and some other drugs that selectively (selectively) affect the serotonin metabolism system, have received widespread recognition today. , preventing its reuptake in the synaptic cleft. Based on the mechanism of action, these antidepressants are combined into a group of selective serotonin reuptake inhibitors. In addition to treating depression, they are used to correct eating disorders, level panic disorders, so-called social phobias, various obsessive-compulsive disorders and chronic pain symptoms. These drugs have gained popularity due to the possibility of a once-daily intake, concomitant anti-anxiety effect, the presence of a psychostimulant component and a small number of side effects. In addition, they have low toxicity and are well tolerated by elderly patients. However, some researchers note their lack of effectiveness in the treatment of severe forms of depressive states, probably associated with selective activity in relation to only one neurotransmitter - serotonin. It should be noted that in recent years, some American scientists have associated the use of these drugs with an increased risk of suicide, which, however, is not proven.
In addition, they have low toxicity and are well tolerated by elderly patients. However, some researchers note their lack of effectiveness in the treatment of severe forms of depressive states, probably associated with selective activity in relation to only one neurotransmitter - serotonin. It should be noted that in recent years, some American scientists have associated the use of these drugs with an increased risk of suicide, which, however, is not proven.
Considering the high frequency of side effects in some of the above drugs and the insufficient antidepressant activity in others, psychopharmacologists have taken the path of developing more effective antidepressants - IV generation drugs that selectively block the reuptake of both serotonin and noradrenaline, without affecting other mediators. system and with minor side effects. Currently, 3 drugs meet these requirements: milnacipran (Ixel), duloxetine (Cymbalta) and venlafaxine (Effexor). Their antidepressant activity in the treatment of patients with severe and moderate depression has been confirmed in a number of specially conducted studies, which at the same time showed that these drugs are well tolerated.
It should be noted that antidepressants of plant origin (negrustin, gelarium hypericum, deprim, etc.) can be effective in mild depressive states, but there are no reliable data guaranteeing their effectiveness. The opinion of a number of doctors that all depression can be treated with herbs or, say, acupuncture, should be recognized as unfounded.
For extremely severe depressions that do not improve despite the use of the most powerful antidepressants, electroconvulsive therapy (ECT) can be effective, but this situation is extremely rare and requires careful justification by the commission of doctors and the consent of the patient.
An important additional role in antidepressant therapy, especially with concomitant anxiety, is played by tranquilizers - anti-anxiety drugs, such as Xanax, phenazepam, diazepam, nitrazepam, atarax, etc. Drugs that can, when taken systematically, prevent mood swings in various depressive disorders include so-called mood stabilizers or mood stabilizers - lithium preparations, carbamazepine, valproic acid salts, lamotrigine, topiramate. With their systematic intake in most patients, the clinical manifestations of depression either completely disappear or become rare and mild, requiring no hospitalization and not significantly affecting the ability to work.
With their systematic intake in most patients, the clinical manifestations of depression either completely disappear or become rare and mild, requiring no hospitalization and not significantly affecting the ability to work.
Antipsychotics play a significant role in the treatment of certain forms of depression. These include both traditional drugs - fluanxol, triftazin, eglonil, teralen, neuleptil, sonapax, and atypical antipsychotics that are gaining more and more recognition among doctors: seroquel, solian, zeldox, rispolept, abilify, serdolect and others.
In drug therapy of depressive conditions, an unconventional, strictly individual approach is used, with the obligatory provision of fruitful cooperation between the patient and the doctor. Otherwise, there may be a violation of medical recommendations regarding doses and regimens for taking medications. The patient's faith in the possibility of recovery, the absence of prejudice against the "harm" caused by psychotropic drugs, the systematic observance of the prescriptions prescribed by the doctor largely contribute to the achievement of therapeutic success.
Drug treatment of depression takes time. You should not expect a complete cure already in the first days of taking the drug. It must be remembered that all modern antidepressants begin to act on depressive symptoms no earlier than 1-2 weeks after the start of treatment. Cancellation of an antidepressant, as well as its appointment, should be carried out only by a doctor. Cancellation is usually made no earlier than 6 months from the normalization of the mental state. Even after the complete disappearance of all symptoms of depression, do not rush to stop taking the drug yourself, as there is a risk of an exacerbation of the disease. Therefore, doctors recommend continuing to take the antidepressant for a certain period of time. A common mistake is the premature withdrawal of drugs soon after a significant improvement in the condition or due to "forgetfulness". To avoid this, try to include the drug in the list of daily urgent matters - for example, store it in the bathroom and take it after hygiene procedures. When planning a trip, calculate exactly how many tablets you need for the entire period of absence from home. Breaking therapy is fraught with serious troubles.
When planning a trip, calculate exactly how many tablets you need for the entire period of absence from home. Breaking therapy is fraught with serious troubles.
Conducted along with drug treatment, psychotherapy of patients with depressive states implies various systems of influence, including individual conversations, family and group therapy, etc. An important element of social rehabilitation is participation in the work of mutual support groups for patients who have experienced depression. This allows other patients to feel help in understanding their problems, to realize that they are not alone in their misfortune, to see the possibilities of personal participation in rehabilitation activities and in social life.
How does depression affect how you feel?
Each of us has heard the word "depression". But do we fully understand what it is? Let's try to understand the essence of this disease and how it affects our psychological and physical well-being.
Contents
- What is depression?
- Symptoms of depression: psychological state
- Symptoms of depression: physical condition
- How can a mental disorder cause pain?
- Why does depression occur and who is at risk?
- How to make a diagnosis?
- How to treat?
What is depression?
In many people's minds, the word "depression" is synonymous with bad mood and depression. To some extent this corresponds to the truth, but in reality everything is much more complicated.
To some extent this corresponds to the truth, but in reality everything is much more complicated.
Depression, or major depressive disorder, is an illness that causes persistent feelings of sadness, loss of interest in life, and a host of other symptoms. It affects how a person feels, thinks and behaves and can lead to a variety of both emotional and physical problems. It is important to understand that depression is a serious mental disorder that requires treatment and observation by a specialist, and not to be confused with other problems.
For example, constant fatigue and unwillingness to get out of bed in the morning may indicate a lack of vitamins, iron, magnesium or other trace elements.
Although it is possible to take tests for the level of these substances on your own, you should not do this: it will be better if the necessary checks are prescribed and carried out by a doctor - this will save you unnecessary anxiety and expenses.
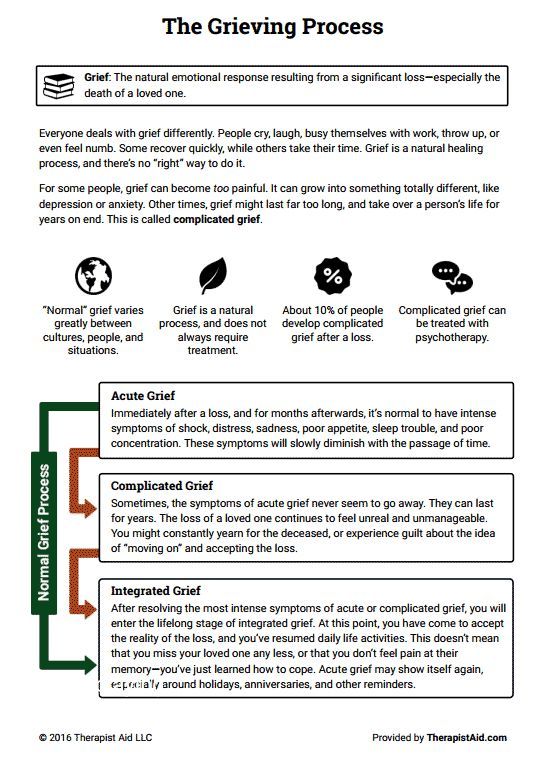
If you feel bad, experience negative emotions and do not find strength for everyday activities, then this is also not a reason to immediately suspect depression. It is likely that the lowering of mood is a reaction to severe stress or bad events that have occurred in your life. Experts point out the following differences between "natural" negative emotions and depression:
It is likely that the lowering of mood is a reaction to severe stress or bad events that have occurred in your life. Experts point out the following differences between "natural" negative emotions and depression:
- If a strong grief has occurred in a person's life (for example, the death of a loved one), then painful feelings come in waves, often mixed with positive memories. With depression, the mood and interest in life are constantly reduced, for two or more weeks.
- In severe sadness or grief, a person's self-esteem is at the same level, and in depression, feelings of worthlessness and self-loathing are common.
- In severe grief, thoughts about one's own death may appear sporadically when a person thinks about "joining" with a deceased loved one. In a depressive disorder, such thoughts arise from a sense of the meaninglessness of one's life or from an inability to cope with problems.
In any case, the symptoms of true depression are not limited to those listed above. They can be divided into psychological and physical.
They can be divided into psychological and physical.
Symptoms of depression: psychological state
Symptoms of depression affecting the psychological state of a person include:
● Feelings of sadness, hopelessness, emptiness.
● Outbursts of anger and irritability even for minor reasons.
● Loss of interest and pleasure in activities that normally bring joy (sports, hobbies, meeting loved ones).
● Attacks of anxiety, agitation, nervousness.
● Feelings of worthlessness or guilt, obsession with past failures.
● Problems with concentration and memory.
● Recurrent thoughts about one's own death, attempts to hurt oneself or otherwise harm oneself.
In children and adolescents, psychological symptoms are generally the same as those listed above, but they may be accompanied by a decrease in school performance, unwillingness to attend classes, avoidance of communication with classmates and friends, tearfulness.
Symptoms of depression: physical condition
Physical manifestations of depressive disorder include the following symptoms:
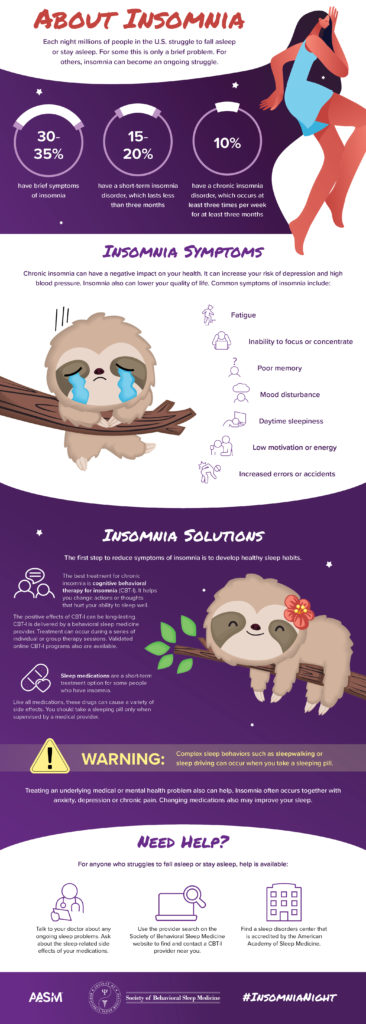
● Sleep disorders: insomnia or drowsiness.
● Constant fatigue and lack of energy, due to which even ordinary daily activities (cleaning, showering) require significant physical effort.
● Disorders of appetite: its decrease or, conversely, its increase. The result is weight loss or gain.
● Pain without apparent cause.
● Convulsions.
● Digestive problems.
How can a mental disorder cause pain?
Experts say that abnormal functioning of the body and pain of unknown origin - that is, arising from no apparent physical cause - are often a symptom of depression. Pain can occur in the joints, in the limbs, in the back and head; in addition, a person may experience problems with the gastrointestinal tract, fatigue, sleep and appetite disorders, changes in psychomotor activity.
Experts say that both types of symptoms are related - the more pain, the more severe the depressive disorder. In addition, pain can be a kind of "indicator" - according to one study, which studied data from more than 1,000 people diagnosed with depression from 14 countries, 69% of patients first came to the doctor because of unclear pain and other physiological problems. This connection between pain and depression can interfere with diagnosis: first, the doctor, of course, will send the patient with a headache or indigestion for further specialized examinations, but if they do not show anything, and the doctor does not have enough knowledge, he may not suspect depression and be in a diagnostic impasse.
In addition, pain can be a kind of "indicator" - according to one study, which studied data from more than 1,000 people diagnosed with depression from 14 countries, 69% of patients first came to the doctor because of unclear pain and other physiological problems. This connection between pain and depression can interfere with diagnosis: first, the doctor, of course, will send the patient with a headache or indigestion for further specialized examinations, but if they do not show anything, and the doctor does not have enough knowledge, he may not suspect depression and be in a diagnostic impasse.
Why is this happening? Physical pain and depression have a deep biological connection. In our body there are biologically active substances called neurotransmitters - they transmit electrochemical impulses from nerve cells and neurons to muscles and other cells of the body. Neurotransmitters that affect both pain and mood include serotonin and norepinephrine.
Changes in the function and effect of these neurotransmitters, and how they interact with neurons and nerve cells involved in maintaining mood stability, may play an important role in the onset of depression.
The reasons why neurotransmitters start to work "wrong" are very complex, and scientists continue to investigate them.
Why does depression occur and who is at risk?
According to experts, women are more prone to depression than men, and the median age of onset is 32 years (this means that half of the people who receive a diagnosis of depression in their lifetime will already have their first depressive episode by this age) . However, this is all - experts cannot give a more detailed portrait of a “typical patient”, because anyone can become a victim of the disease.
However, there are a number of factors that increase the risk of developing a depressive disorder:
- Genetics. Depression can be inherited: studies show that genetics can contribute up to about 40% to the development of depression, and the likelihood that the twin of a person suffering from depression will also receive this diagnosis is about 70%. In 2019, scientists conducted a meta-analysis of data on more than 800 thousand people and found 102 genetic variants associated with the development of depression.

- Environmental factors. If a person has experienced severe stress or psychological trauma in his life (for example, a child had a difficult childhood, he was subjected to violence, lived in conditions of extreme poverty), then the likelihood of developing a depressive disorder increases.
- Personal qualities of a person. People with low self-esteem, easily succumbed to stress, and prone to pessimism are at greater risk.
- Hormonal changes due to pregnancy, postpartum, menopause, and thyroid disorders.
- Other serious health problems: Parkinson's disease, diabetes, heart disease, cancer.
How to make a diagnosis?
Not only the well-being of a person, but also his life can depend on the correct diagnosis and timely treatment. To diagnose a depressive disorder, doctors must conduct a set of studies.
- First of all, a psychiatrist should talk to a person about his state of health, thoughts, behavior. The patient may be asked to fill out a special questionnaire that contains various signs of depression.
 For a diagnosis to be made, the patient must experience a certain amount of these symptoms for two or more weeks over most of the day.
For a diagnosis to be made, the patient must experience a certain amount of these symptoms for two or more weeks over most of the day. - General medical examination to find out if the pains or other disturbances in the functioning of the body - of course, if present - are of a physical nature.
How to treat?
Despite the seriousness of the disease, do not despair when making a diagnosis. Depressive disorder is treated using different methods:
- Antidepressants - these drugs affect the biochemical processes in the brain, the work of neurotransmitters. It is important to know that antidepressants may not have an effect for several weeks after the start of treatment - the patient may not notice improvement within 2-3 months. Sometimes the doctor is not immediately able to choose the right dosage or drug, in addition, antidepressants can have side effects, so they should never be taken on their own, without prescription and constant monitoring by the doctor.
Learn more