Bipolar disorder counseling
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid.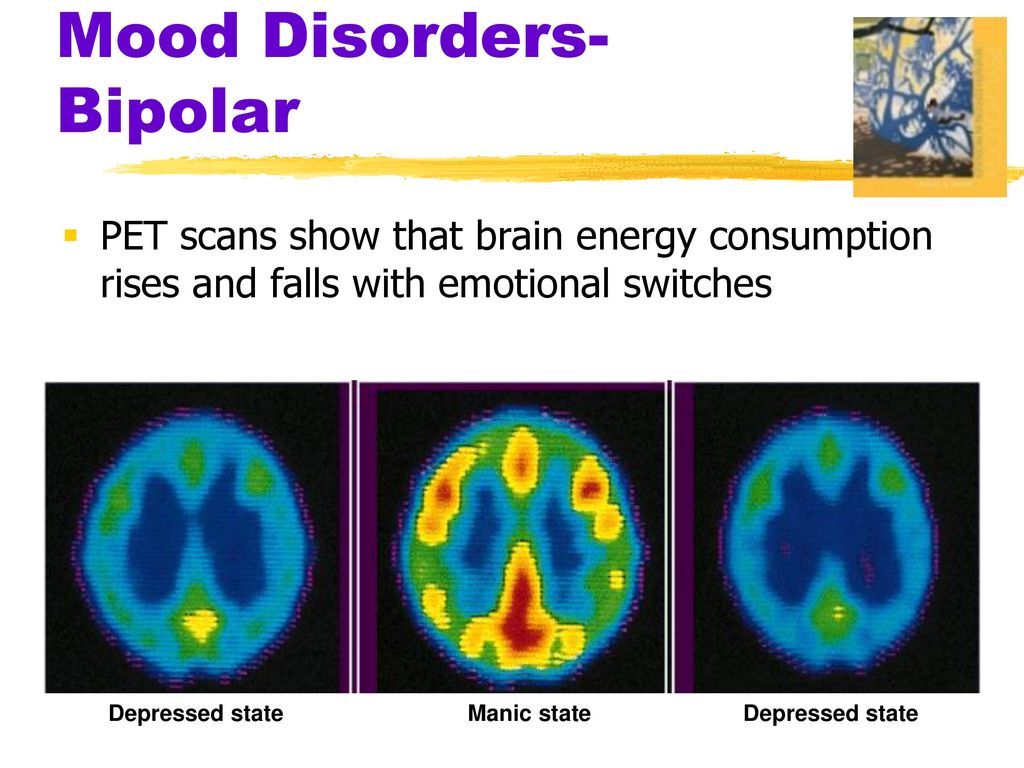 If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.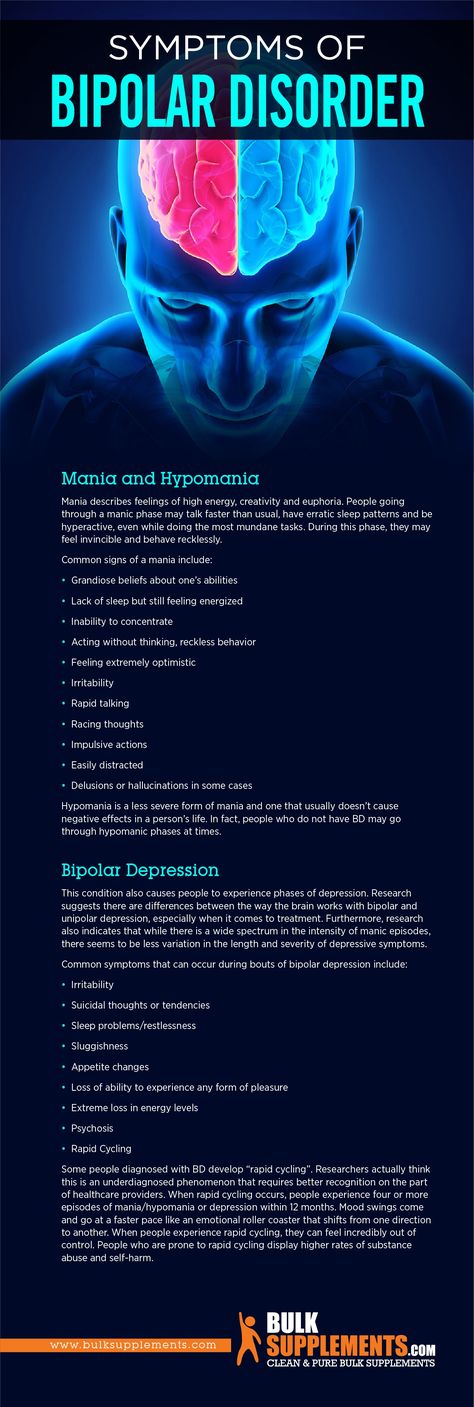
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.

-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly. Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
4 types of psychological counseling (psychotherapy) Bipolar disorder Patients should be familiar with | mental health articles | Emotional & Mental Health center
While medication is still the mainstay of treatment for bipolar disorder, various forms of talk therapy are also becoming an important part of recovery. What should you know?
Bipolar disorder is a lifelong illness characterized by recurrent episodes of hypomania, mania, or depression.
This is also accompanied by an increase in the level of psychosocial disorders. Without a doubt, drug therapy is still the main form of treatment for patients with bipolar disorder, but studies have shown that drug treatment provides only partial relief of symptoms.
Without a doubt, drug therapy is still the main form of treatment for patients with bipolar disorder, but studies have shown that drug treatment provides only partial relief of symptoms.
Some symptoms just can't be taken away with pills, but a well-trained therapist can help with problem solving, coping with skills, and perhaps most importantly, recognizing the triggers and patterns that lead to relapse of bipolar symptoms.
Research has shown that various talk therapies, such as interpersonal social rhythm therapy, cognitive behavioral therapy, psychoeducation, and family-oriented therapy, help prevent relapses, especially when they begin early in the disease. This is because bipolar disorder is characterized by psychosocial impairment, social dysfunction, and low adherence to medication, all of which lend themselves well to psychological counseling.
What types of psychotherapy should all bipolar patients and their families be familiar with?
1. Interpersonal and Social Rhythm Therapy (IPSRT)
There is no single “best treatment for bipolar disorder”, but some studies have shown that Bipolar I and Bipolar II can be effectively controlled with Interpersonal and Social Rhythm Therapy.
It's not about changing a person's beliefs, but rather about helping him understand better what's going on. IPSRT focuses on external action - teaching the patient new methods to reduce the symptoms of mania or depression.
In IPSRT, the goal is to learn how to balance stimulation levels depending on your current mood: patients learn to increase stimulation during depressive episodes and decrease it when they are at risk of hypomania or mania.
Originally planned to be a one-on-one therapy, it can now be done in group sessions. Patients typically start with once-a-week sessions, with therapists gradually reducing it to monthly appointments.
2. Cognitive Behavioral Therapy (CBT)
Unlike IPSRT, which never attempts to change a person's beliefs, CBT is a targeted form of treatment in which the therapist gives insight into people's negative, false, and maladaptive moods and emotions so they can work on changing those patterns. These actions are rarely convenient for the patient. Gradually, a person learns to confront certain situations and develops new and healthier behaviors that improve social functioning.
Gradually, a person learns to confront certain situations and develops new and healthier behaviors that improve social functioning.
Research has shown that CBT can prevent certain manic symptoms from developing into full-blown mania, as well as reduce the duration of a depressive episode.
3. Psychoeducation
Psychoeducation (PE) is the foundation of all psychotherapy programs because it teaches people more about all aspects of their condition. It is known that people who understand what is happening to them are better able to solve these problems and have more strength to fight for their health.
Psychoeducation comes in many forms, but individual and group psychoeducation are the most common. Individual therapy lasts from six to 21 sessions. The therapist provides information about the condition, its causes, treatments, and ways to spot early signs and symptoms of relapse, and teaches patients how to cope with the illness.
4. Family-oriented therapy
Over the past 30 years of research on the benefits of family-oriented therapy for people with bipolar disorder, it has been concluded that FFT - together with mood stabilizers - can speed up recovery from manic and depressive episodes, as well as reduce the frequency as well as the severity of the episodes.
Recent studies show that 12 family education sessions can reduce the likelihood that a person at high risk will develop bipolar disorder, or at least reduce the social impairment associated with the onset of the disease.
It is important that relatives and friends of people diagnosed with bipolar disorder understand what it means and what life with bipolar disorder looks like. This way they can communicate more and view mental health issues not as a taboo but as something that can happen to anyone. Family support also means that a person is more likely to stick to their conversion.
Complementary forms of therapy for bipolar disorder
In addition to psychotherapy, various other forms of treatment have been shown to help reduce the symptoms of bipolar disorder. Some of these include:
- Electroconvulsive therapy (ECT) - due to some serious side effects, it is only recommended for severe cases of bipolar disorder when there is nothing left to lose.

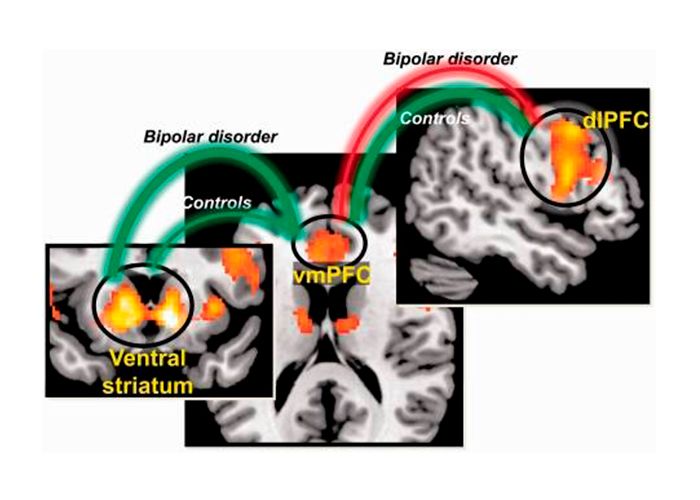
- Transcranial Magnetic Stimulation (TMS) - The scientific community hypothesizes that TMS stimulates the left prefrontal cortex and thus helps relieve symptoms of bipolar disorder, but more research is needed.
- Long-term exposure therapy aims to make patients experience certain traumatic experiences.
Who can provide psychological counseling?
Various professionals trained in mental health care:
- Psychiatrists
- psychologists
- Psychiatric nurses
- Advisors
- Social workers
The experience of the specialist you have chosen as your therapist is certainly important, but it is also important that you feel comfortable with them, as your ability to be completely open with your therapist really matters.
Your therapist is now your partner; both of you are ready to help you feel better, and this is only possible if you openly discuss all your experiences and experiences. What are your goals? Why did you seek treatment? Some people do it to please others, to keep a job or a relationship. Remember that no therapy will work unless you are there for YOU.
What are your goals? Why did you seek treatment? Some people do it to please others, to keep a job or a relationship. Remember that no therapy will work unless you are there for YOU.
Research has shown that Interpersonal Rhythm Therapy, Family-Oriented Therapy, and CBT, when combined with complementary medication, can reduce the duration of both manic and depressive episodes.
Bipolar affective disorder and psychotherapy
10 topics that you will encounter in the process of psychotherapy
It just so happens that I know a lot about bipolar affective disorder and people with this disorder. Once upon a time, this disease ruined my life, followed by many years of treatment and personal psychotherapy. Since 2014, I have been running a website about bipolar disorder, participating in support groups - writing, reading, observing. Readers of the site often send their personal stories, amazing and sad, so different and so similar.
This whole story led me to change my profession, I studied a lot and started working as a psychologist myself.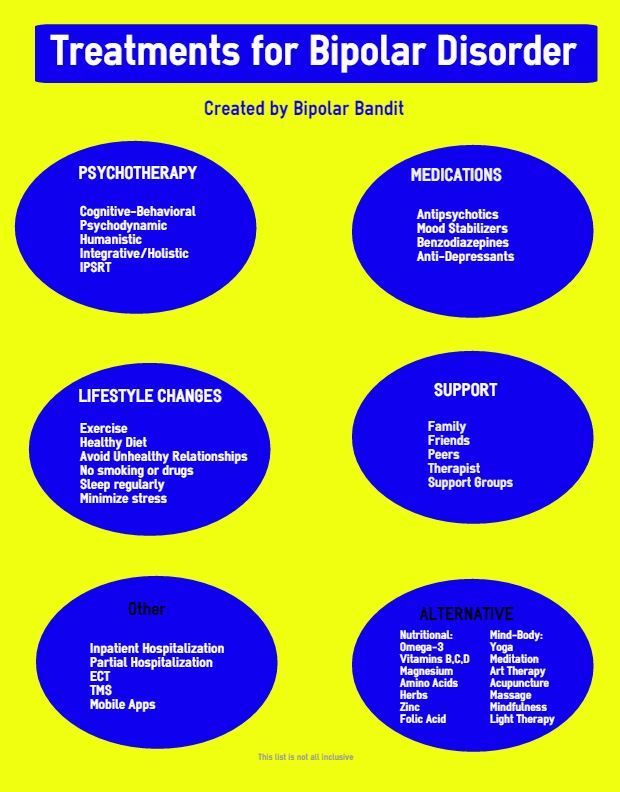 Now the main method in which I work is cognitive-behavioral therapy.
Now the main method in which I work is cognitive-behavioral therapy.
During this time, I have accumulated some observations that I would like to share.
Why do I need psychotherapy for bipolar disorder?
Bipolar people are the same people as everyone else. They, like everyone else, are interested in relationship problems, career growth, self-confidence, separation from parents, and so on. They also had childhood.
I write this material for the patients themselves and for psychologists.
Often I hear: psychology is for the healthy, psychiatry is for the sick. And let me disagree, people with mental disorders need psychological help even more than others.
People who have had severe depressions and manias behind them lack a sense of stability. Many lost their jobs, some lost their families, most of these people lived for a long time without treatment and did not know what was happening to them. It is almost impossible to plan and predict one's life under such conditions; this gives rise to a constant feeling of anxiety.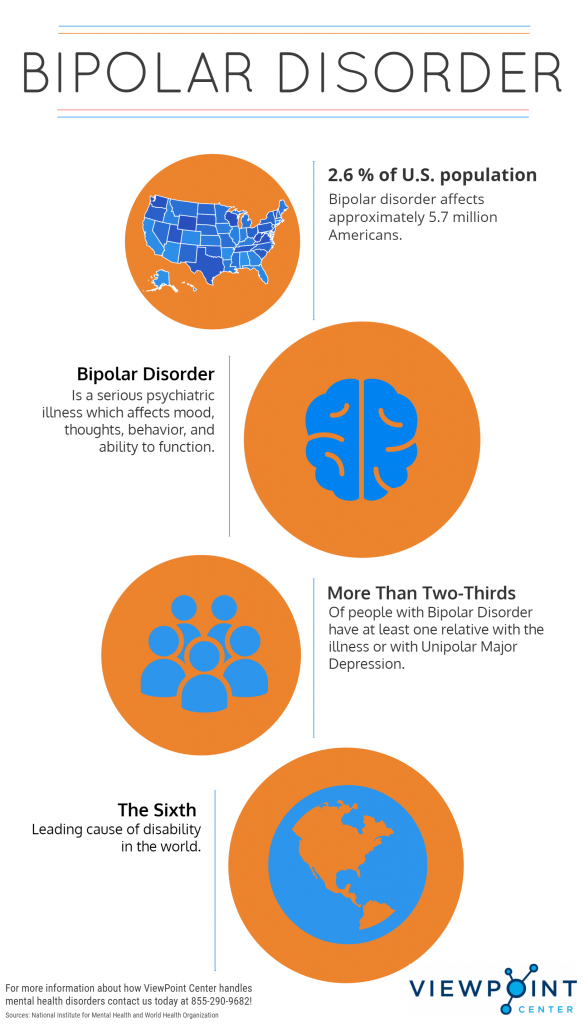 So psychotherapy can be very helpful.
So psychotherapy can be very helpful.
After making a diagnosis, many people breathe a sigh of relief - at last it has become at least a little clear. But this is only the first step and the main work is still ahead.
What to work on in psychotherapy?
First of all, it is awareness of one's responsibility for one's health. How treatment and recovery will take place largely depends on the person himself, on his firmness and determination to improve his condition.
Sometimes people with bipolar disorder lose control of themselves, especially early in the illness. In such cases, you can ask loved ones for help. But in reality, a person can completely lose control only in psychosis. A rapidly unfolding psychotic mania is found in bipolar I disorder, psychotic depression usually unfolds much more slowly and the person has time to realize that he is ill.
In all other cases, it remains possible to take action yourself.
The difficulty here can be hypomania, during which a person controls himself well, but is not completely critical of himself and his illness.
However, psychologists rarely see people in hypomania, more often they have to deal with depression, and in this case, psychotherapy should first of all be aimed at stabilizing the current state. And after getting out of depression, you can move on. During this period, the most important thing is to follow the recommendations of the doctor, and in psychotherapy to support the client and be there.
If a person has depression as part of a bipolar disorder, then it is not worth swinging it, looking for reasons, delving into the past, etc. Crying out tears can be useless, and trying to reach the bottom of depression in order to push yourself away from it (yes, I heard that once!) Can be simply dangerous and push a person to suicide. So it is necessary to wait until the treatment prescribed by the doctor begins to act. It can be only mood stabilizers or their combination with antidepressants and sometimes antipsychotics.
See also: Tests for bipolar disorder
Topics and features you are most likely to encounter in psychotherapy:
often divided into two camps.
 The first is support. The second ones give advice: you don’t need a doctor, it’s all laziness, doctors will turn you into a vegetable, etc. It can be difficult to maintain such pressure, especially if there are many advisers. It is very important to realize that only the person himself is responsible for his recovery, and the future will depend only on his actions.
The first is support. The second ones give advice: you don’t need a doctor, it’s all laziness, doctors will turn you into a vegetable, etc. It can be difficult to maintain such pressure, especially if there are many advisers. It is very important to realize that only the person himself is responsible for his recovery, and the future will depend only on his actions. 2. Prevention of episodes of depression or mania
Most types of bipolar disorder are seasonal, which can also help control the disease. In some cases, such a connection is not traced, and then, in order to prevent breakdowns, it makes sense to compile a list of the first symptoms of an incipient episode, these are always individual personal calls far from the diagnostic criteria from the textbook.
For example, before the onset of depression, even before the mood changes, a person can communicate less with friends, sleep more, start postponing things for later, play on the computer, and so on, everyone has their own set. During the onset of hypomania and also before the change in mood, a person, on the contrary, may begin to communicate more, write on social networks or go shopping.
During the onset of hypomania and also before the change in mood, a person, on the contrary, may begin to communicate more, write on social networks or go shopping.
If you consult a doctor for any change in the condition, then in most cases you can stop the episode without loss of ability to work. And over time (sometimes it can take several years), the phases of the disease will no longer disturb the usual rhythm.
3. Triggers
As you know, even in endogenous diseases, external factors play an important role - stress, overwork and significant events can put anyone out of action, and for a person with bipolar disorder they can serve as the beginning of depression or mania.
Weather, lunar cycles, solar flares (well, or on Mars), alcohol, chocolate, coffee, lack of sleep, oversleeping, holidays, memorable dates, and so on can affect the condition.
During episodes, even if corrected by medication, the person remains vulnerable to these factors.
Many people with bipolar disorder, even without episodes of the disease, the state and mood remain unstable.
4. Distinguish manifestations of an affective disorder from ordinary human emotions.
At first, it is difficult for a person to separate his usual emotions from the manifestations of depression or mania. It happens that a person is upset or overworked, but then he immediately begins to suspect depression, but it happens the other way around, his depression has been unfolding for a long time and slowly, and he blames everything on fatigue and lack of sleep, gradually gets used to this state and continues to live, plunging into deeper depression.
Manifestations of hypomania can be difficult to distinguish from personality traits, many people with BAD initially have hyperthymic character accentuation.
5. Bipolar Disorder and Personality
When a person is diagnosed with bipolar disorder, they begin to question their whole life. He is frightened that he made many choices in life under the influence of illness. He is lost and wonders: where am I, where are the boundaries of my personality, and where is the disease? Where are my hobbies, achievements and failures, and where did I live completely in the power of the disease? Which of my oddities are related to the disease, and which are not?
He is frightened that he made many choices in life under the influence of illness. He is lost and wonders: where am I, where are the boundaries of my personality, and where is the disease? Where are my hobbies, achievements and failures, and where did I live completely in the power of the disease? Which of my oddities are related to the disease, and which are not?
Fortunately, BAD does not affect the core of the personality, but it has a significant influence on its development. It is important to understand that BAR is not equal to me, and I is not equal to BAR. To open and strengthen other healthy parts of the personality that are not affected by the disease.
6. Self-esteem
Prior to treatment, a person with bipolar disorder's self-esteem jumps from feeling worthless to feeling superhuman.
Once a diagnosis is made and medications are started, everything changes. Fluctuations in self-esteem caused by episodes of the disease are smoothed out. But the diagnosis itself can significantly reduce a person’s self-confidence and their abilities.
Sick, psycho, crazy, mentally ill - all these words can be tried on by people with bipolar disorder.
7. Relationships
In depression, a person avoids contacts, while in hypomania and mania, on the contrary, he is hypersocial. This invariably leads to problems in relationships with loved ones. In hypomania, a person is passionate about himself and his ideas, communicates a lot, spends money, and has difficulty hearing other people. In manias, in some cases, sexual promiscuity, large loans, abrupt moves can join.
8. Feelings of guilt and shame
Many experiences are associated with these feelings. A person may experience shame from being sick, from being treated by a psychiatrist, from being unable to work, from mistreating his children, and so on.
If a person has attempted suicide, then, as a rule, many difficult experiences are also hidden behind them.
In mania, there could be quite a lot of deeds that a person regrets - sex with random people, big loans, carousing, accidents, and so on.