What is chronic insomnia
Types of Insomnia | Sleep Foundation
Not all cases of insomnia are identical. People can be affected by insomnia in different ways, and distinguishing between forms of the condition can be useful for both health professionals and people with insomnia.
There are two main types of insomnia:
Short-Term Insomnia
Also known as acute insomnia or adjustment insomnia, this is a brief episode of difficulty sleeping. Short-term insomnia is often caused by a stressful life event, such as the loss of a loved one, a disconcerting medical diagnosis, a pandemic, rebounding from cessation of a drug or marijuana, or a major job or relationship change.
Acute insomnia lasts for less than three months, and symptoms may fade on their own as time passes and a person copes with the stressful incident that gave rise to their sleeping problems. However, short-term insomnia can be persistent and become chronic insomnia.
Short-term insomnia can affect both children and adults. It is more common in women than in men, and it can arise during pregnancy as well as menopause.
Chronic Insomnia
Chronic insomnia is a long-term pattern of difficulty sleeping. Insomnia is considered chronic if a person has trouble falling asleep or staying asleep at least three nights per week for three months or longer.
Some people with chronic insomnia have a long history of difficulty sleeping. Inability to get the sleep they need may be persistent or go away and recur with months-long episodes at a time.
Chronic insomnia has many potential causes. Like acute insomnia, it can be tied to stressful situations, but it may also be related to irregular sleep schedules, poor sleep hygiene, persistent nightmares, mental health disorders, underlying physical or neurological problems, medications, a bed partner, and certain other sleep disorders.
Like short-term insomnia, chronic insomnia occurs in people of all ages and has a higher prevalence in women.
Other Ways of Describing Insomnia
While the sleep disorder of insomnia is principally classified as either short-term or chronic, there are other terms that may be used to describe insomnia.
These terms may be used informally or as a way for researchers to better categorize and analyze the different ways that insomnia can be experienced.
Sleep Onset Insomnia
Sleep onset insomnia describes difficulty falling asleep at the beginning of the night, or in the case of shift workers, whenever they attempt to initiate sleep. It is associated with the idea of tossing and turning without actually being able to get to sleep. Most people with sleep onset problems can’t fall asleep even after spending 20-30 minutes in bed.
The inability to fall asleep means that a person with insomnia of this nature has reduced total sleep time and can feel the effects of that lack of sleep the next day.
Sleep Maintenance Insomnia
Sleep maintenance insomnia describes an inability to stay asleep through the night. Most often, this means waking up at least once during the night and struggling to get back to sleep for at least 20-30 minutes.
The fragmented sleep associated with poor sleep maintenance means a decrease in both sleep quantity and quality, creating higher chances of daytime sleepiness or sluggishness.
Early Morning Awakening Insomnia
Early morning awakening insomnia involves waking up well before a person wants or plans to in the morning. Some experts view this as a component of sleep maintenance while others consider it separately.
Inability to get their desired amount of sleep can impair a person’s physical and mental function the next day.
Mixed Insomnia
Though not a formal term, the descriptor mixed insomnia may be applied to people who have a combination of problems related to sleep onset, sleep maintenance, and early morning awakenings.
In general, the broader term insomnia can be thought of as describing mixed insomnia because it is common for people to have overlapping sleeping problems. In addition, people with insomnia often find that their symptoms can shift over time, making it hard to classify insomnia strictly among the subtypes of onset, maintenance, and early morning awakenings.
Comorbid Insomnia
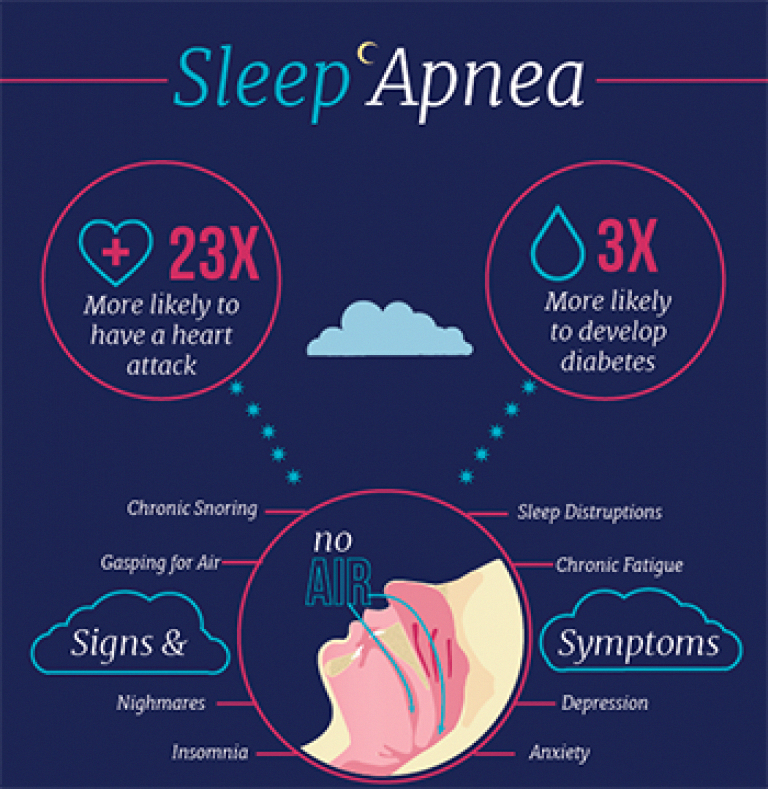
In the past, sleeping problems were sometimes labeled as comorbid insomnia or secondary insomnia.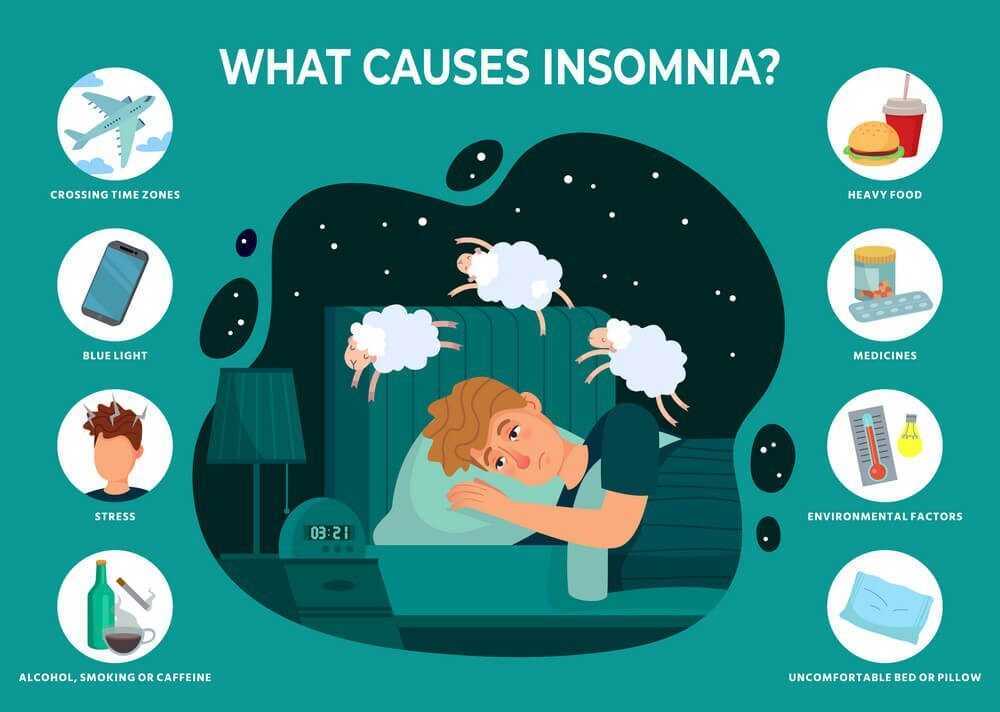 This meant that insomnia was believed to arise as a result of another condition such as anxiety, depression, sleep apnea, gastroesophageal reflux disease (GERD), or physical pain.
This meant that insomnia was believed to arise as a result of another condition such as anxiety, depression, sleep apnea, gastroesophageal reflux disease (GERD), or physical pain.
Contemporary research has generated a deeper understanding of insomnia that recognizes that sleeping problems often have a bidirectional relationship with other health issues. For example, while anxiety may contribute to insomnia, insomnia may trigger or exacerbate anxiety as well. Furthermore, insomnia triggered by another condition does not always go away even after that underlying issue is resolved.
Because of the complexity of these relationships, it becomes difficult to classify insomnia as strictly comorbid or secondary. Similarly, the presence of multiple contributing factors makes identifying a single cause of insomnia challenging for many patients.
For these reasons, insomnia classification systems used in sleep medicine have moved away from this terminology and toward a broader understanding of insomnia.
Future Research About Types of Insomnia
Insomnia can manifest in diverse ways, and researchers are working to further identify how causes, symptoms, health consequences, and treatments may be different among distinct subtypes. For instance, some studies have attempted to connect variations of insomnia to a person’s life and health history and to a host of other individual variables.
In the future, it is possible that continued investigation along these lines may sharpen our understanding of insomnia and expand the ability to optimize treatment for any given patient.
- Was this article helpful?
- YesNo
References
+10 Sources
-
1.
Zhang, B., & Wing, Y. K. (2006). Sex differences in insomnia: a meta-analysis. Sleep, 29(1), 85–93. https://doi.org/10.1093/sleep/29.1.85
-
2.
Silvestri, R., & Aricò, I. (2019). Sleep disorders in pregnancy. Sleep science (Sao Paulo, Brazil), 12(3), 232–239.
 https://doi.org/10.5935/1984-0063.20190098
https://doi.org/10.5935/1984-0063.20190098 -
3.
Bjorøy, I., Jørgensen, V. A., Pallesen, S., & Bjorvatn, B. (2020). The Prevalence of Insomnia Subtypes in Relation to Demographic Characteristics, Anxiety, Depression, Alcohol Consumption and Use of Hypnotics. Frontiers in psychology, 11, 527. https://doi.org/10.3389/fpsyg.2020.00527
-
4.
Hohagen, F., Käppler, C., Schramm, E., Riemann, D., Weyerer, S., & Berger, M. (1994). Sleep onset insomnia, sleep maintaining insomnia and insomnia with early morning awakening--temporal stability of subtypes in a longitudinal study on general practice attenders. Sleep, 17(6), 551–554. https://pubmed.ncbi.nlm.nih.gov/7809569/
-
5.
Finan, P. H., Goodin, B. R., & Smith, M. T. (2013). The association of sleep and pain: an update and a path forward. The journal of pain : official journal of the American Pain Society, 14(12), 1539–1552. https://doi.org/10.1016/j.jpain.2013.08.007
-
6.
Neckelmann, D., Mykletun, A., & Dahl, A. A. (2007). Chronic insomnia as a risk factor for developing anxiety and depression. Sleep, 30(7), 873–880. https://doi.org/10.1093/sleep/30.7.873
-
7.
Sateia M. J. (2014). International classification of sleep disorders-third edition: highlights and modifications. Chest, 146(5), 1387–1394. https://doi.org/10.1378/chest.14-0970
-
8.
Blanken, T. F., Benjamins, J. S., Borsboom, D., Vermunt, J. K., Paquola, C., Ramautar, J., Dekker, K., Stoffers, D., Wassing, R., Wei, Y., & Van Someren, E. (2019). Insomnia disorder subtypes derived from life history and traits of affect and personality. The lancet. Psychiatry, 6(2), 151–163. https://doi.org/10.1016/S2215-0366(18)30464-4
-
9.
Benjamins, J. S., Migliorati, F., Dekker, K., Wassing, R., Moens, S., Blanken, T. F., Te Lindert, B., Sjauw Mook, J., & Van Someren, E. (2017). Insomnia heterogeneity: Characteristics to consider for data-driven multivariate subtyping.
 Sleep medicine reviews, 36, 71–81. https://doi.org/10.1016/j.smrv.2016.10.005
Sleep medicine reviews, 36, 71–81. https://doi.org/10.1016/j.smrv.2016.10.005 -
10.
American Academy of Sleep Medicine. The International Classification of Sleep Disorders – Third Edition (ICSD-3). Darien, IL: American Academy of Sleep Medicine, 2014.
See More
Treatment, Causes, Symptoms, and More
Overview
Insomnia is a common sleep disorder in which you may have trouble falling asleep, staying asleep, or both. A third of Americans report that they don’t get the recommended amount of sleep every night, which is at least seven hours.
Periodically having trouble sleeping, also known as acute insomnia, is common. Acute insomnia lasts for a few days or weeks and often occurs during times of stress or life changes.
Have trouble getting to sleep or staying asleep more than three nights a week for three months or more is considered chronic insomnia. This is also known as chronic insomnia disorder.
There are two main types of chronic insomnia: primary and secondary.
Primary insomnia isn’t due to other medical conditions or medications and is poorly understood by scientists. Specialized MRI scans are being used to study this condition. Primary insomnia may be related to changes in levels of certain brain chemicals, but research is ongoing.
Secondary insomnia is caused by other conditions or situations. This means that it’s a symptom that goes along with some medical issues, such as emotional stress, trauma, and ongoing health problems; certain lifestyle patterns; or taking certain drugs and medications.
Chronic insomnia can cause symptoms at night as well as during the day and can interfere with your ability to go on with your daily tasks.
Symptoms may include:
- trouble falling asleep
- waking up throughout the night
- trouble staying asleep or trouble returning to sleep
- waking up too early
- daytime sleepiness or grogginess
- not feeling rested after a night’s sleep
- irritability
- mood changes, such as feeling depressed
- difficulty concentrating
- problems with memory
- increase in mistakes and accidents
There are many things that can cause chronic insomnia, but it’s often linked to an underlying medical condition. Certain medications and stimulants can cause chronic insomnia, along with lifestyle patterns.
Certain medications and stimulants can cause chronic insomnia, along with lifestyle patterns.
Medical conditions
Chronic insomnia can be caused by a number of long-term medical conditions, including:
- respiratory conditions, including:
- asthma
- chronic obstructive pulmonary disease (COPD)
- sleep apnea
- congestive heart failure
- diabetes
- acid reflux
- hyperthyroidism
- fibromyalgia
- pain
- restless leg syndrome
- menopause
- urinary incontinence
- stress, both physical and emotional
- anxiety
- depression
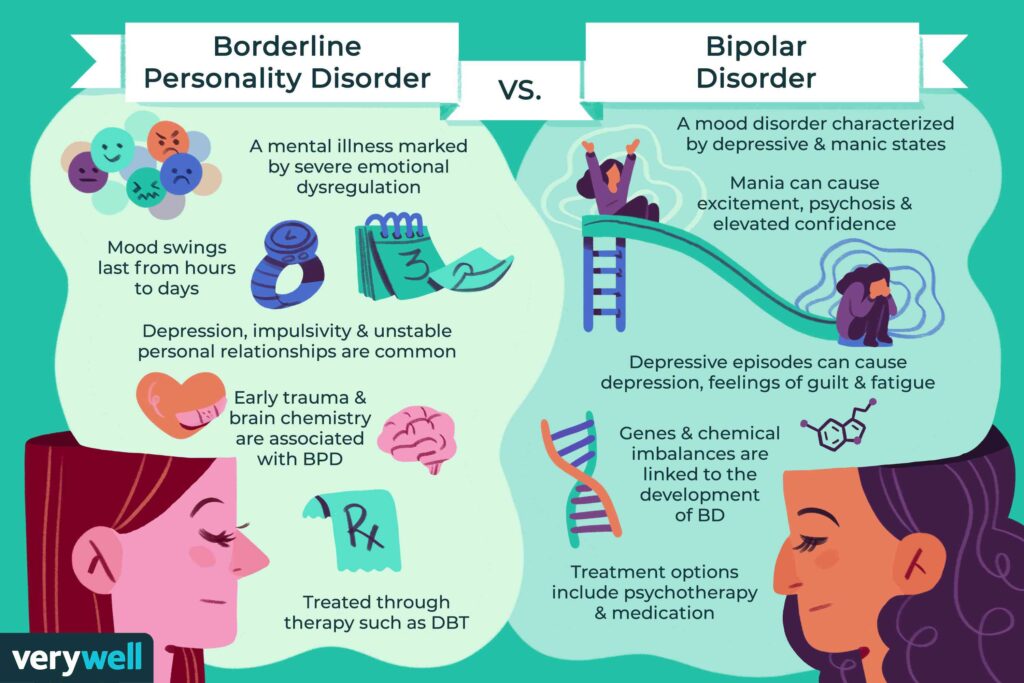
- bipolar disorder
- Alzheimer’s disease
- Parkinson’s disease
Medications and stimulants
For some people, certain medications and stimulants may cause chronic insomnia. These include:
- alcohol
- antidepressants
- beta-blockers
- caffeine
- chemotherapy drugs
- cold and allergy medications containing pseudoephedrine
- diuretics
- illicit drugs, such as cocaine and other stimulants
- nicotine
- stimulant laxatives
Lifestyle patterns
Certain lifestyle patterns may lead to chronic insomnia. These include:
These include:
- rotating shift work
- frequent travel across multiple time zones, leading to jet lag
- physical inactivity
- frequent daytime napping
- lack of routine for waking and sleeping
- poor sleeping environment
A number of at-home and professional treatment options are available for chronic insomnia. Treatment will depend on the cause of your insomnia and may involve medication or therapy to address an underlying condition.
Along with treating any existing conditions, your doctor may recommend one or a combination of treatment options for chronic insomnia.
Cognitive behavioral therapy (CBT)
Research has shown CBT to be as effective, or more effective, than sleep medications in treating chronic insomnia. It involves educating you on sleep and better sleep habits, while teaching you to change the beliefs and behaviors that interfere with your ability to sleep.
Some of the strategies of CBT that are specifically focused on insomnia, known as CBT-I, include the following:
Cognitive techniques
Using journaling to write down worries or concerns before going to bed may help keep a person from actively attempting to work them out while also trying to sleep.
Stimulus control
This entails altering behaviors that condition your mind to fight sleep. Setting a sleep and wake time routine is part this strategy.
Other examples are using your bed only for sleep and sex, and leaving your bedroom if you’re unable to fall asleep within a set number of minutes.
Sleep restriction
This therapy involves limiting the amount of time you spend in bed, including avoiding naps. The goal is to deprive you of enough sleep so that you’re tired at bedtime. Your time in bed is gradually increased as your sleep improves.
Relaxation techniques
Breathing exercises, yoga, guided meditation, and other techniques are used to reduce muscle tension and control your breathing and heart rate so that you’re able to relax.
Paradoxical intention
This strategy involves focusing on staying awake in bed instead of expecting to fall asleep. It helps reduce worry and anxiety over being able to fall asleep. It’s most effective in treating learned insomnia.
It’s most effective in treating learned insomnia.
Medications
There are a number of prescription medications and over-the-counter (OTC) sleep aids that may help you get to sleep or remain asleep.
While effective, doctors don’t typically recommend using sleeping pills long term because of the side effects, which can include daytime sleepiness, forgetfulness, sleepwalking, balance problems, and falling. Certain classes of sleeping pills are also habit-forming.
Some of the prescription medications that are approved for treating insomnia include:
- zolpidem (Ambien)
- eszopiclone (Lunesta)
- zaleplon (Sonata)
- doxepin (Silenor)
- ramelteon (Rozerem)
- suvorexant (Belsomra)
- temazepam (Restoril)
OTC sleep aid options may include:
- diphenhydramine (Benadryl)
- doxylamine succinate (Unisom SleepTabs)
- melatonin
- valerian root
- chamomile tea
Always speak to your doctor before taking an OTC sleep aid, including natural remedies, such as melatonin and valerian root.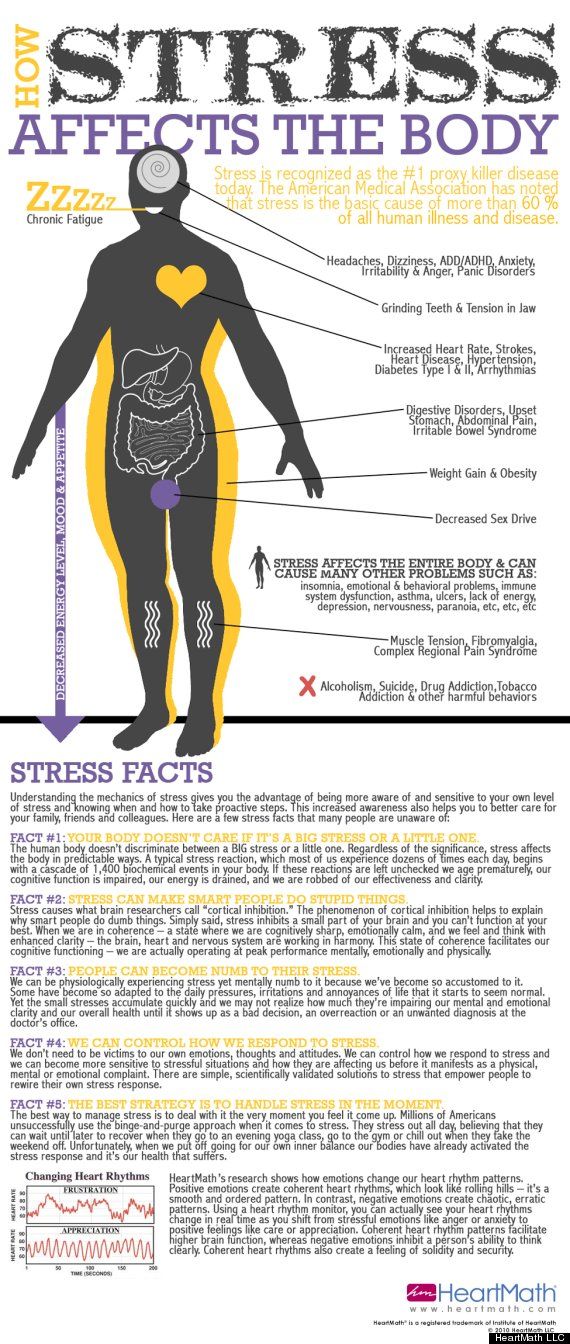 Just like prescription drugs, OTC and natural sleep aids can cause unwanted side effects and interfere with other medications.
Just like prescription drugs, OTC and natural sleep aids can cause unwanted side effects and interfere with other medications.
If your chronic insomnia is caused by an underlying medical condition, such as acid reflux or pain, treating the condition may cure your insomnia.
Chronic health conditions that cause insomnia can be managed with changes in treatment, in turn managing or preventing insomnia. Talk to your doctor about changing medications or treatment plans if a drug you’re taking is causing insomnia.
There are several things that you can do at home to treat or prevent chronic insomnia. One important option for treatment is known as sleep hygiene. This calls for changes in patterns of behavior to help improve your ability to fall asleep and stay asleep.
Try the following tips:
- Avoid caffeine, especially later in the day.
- Avoid alcohol use and smoking cigarettes before bed.
- Engage in regular physical activity.
- Don’t take naps.
- Don’t eat large meals in the evening.
- Go to bed and get up at the same time every day, even on days off.
- Avoid using computers, smartphones, TV, or other technological devices an hour before bedtime.
- Keep your bedroom dark or use a sleep mask.
- Keep your bedroom a comfortable temperature.
- Make sure your sleep surface is comfortable. Want suggestions? Browse our market, filled with editor-trusted and expert-verified mattress recommendations.
Chronic insomnia can be effectively treated using a combination of behavioral therapies and by making a few lifestyle changes to help improve your sleep. If you’re having trouble sleeping and it’s interfering with your quality of life, talk to your doctor.
Ways to cope with insomnia | Memorial Sloan Kettering Cancer Center
Share
Time to read: Approximately 4 min.
This information explains what insomnia is and how you can manage it.
About insomnia
Insomnia is when you can't fall asleep, you can't sleep for a long time, you wake up too early, or you have all of these symptoms at once. People who suffer from insomnia often cannot fall asleep again after they wake up. Insomnia is seen in many people with cancer.
There are 2 types of insomnia:
- Acute insomnia lasts less than 3 months and usually resolves on its own. Sometimes acute insomnia can become chronic.
- Chronic insomnia is a sleep disorder that occurs 3 or more days per week and lasts 3 months or more.
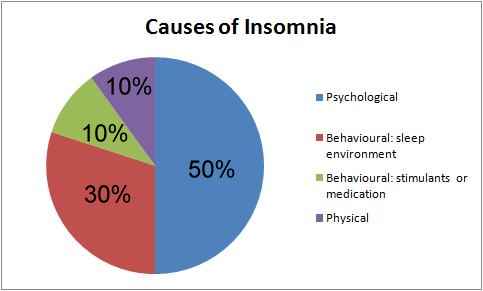
Causes of insomnia
Insomnia can have many causes, a few examples are listed below.
- Anxiety or stress caused by major life events such as a cancer diagnosis or the death of a loved one. For more information on ways to manage anxiety or stress, check out this resource.
- Changes in your environment or work schedule, such as moving to a new location.

- Unhealthy sleep habits, such as watching TV in bed or doing other activities in bed other than sleep or sexual activity.
- Taking certain medications.
- Health problems.
Signs of insomnia
Insomnia may have the following signs:
- you have difficulty falling asleep;
- you often wake up during the night and have difficulty falling asleep again;
- you wake up too early in the morning.
People with insomnia may feel very tired during the day and lack energy. They may also have trouble concentrating, which can affect work or school.
If you have any of these signs, contact your healthcare provider.
back to top of pageHow to deal with insomnia
No matter how long you've had insomnia, there are ways to treat it that can help you. First, talk to your healthcare team. Relevant information materials will be recommended to you.
Below are a few tips that may help.
- Set a regular sleep schedule. A regular schedule with the same bedtime and wakeup time can help you fall asleep and rest well during your sleep.
- Do light exercise at least 2-3 hours before bedtime. Short walks or bike rides may be suitable for you. Being outdoors and in the sun can help your body prepare for a night's sleep.
- Create the perfect sleep environment. Make sure the room you sleep in is cool, dark and quiet. The bed, pillow and blanket should be comfortable for you. If you have pets and they are active at night, don't let them sleep in your bed with you. Take the animals out of the bedroom or put them on their own bed. This way they won't disturb you while you sleep.
- Try to relax and calm down before going to bed. Avoid bright lights and stimulating activities such as strenuous exercise or difficult work-related problems. Try to stick to the same calming and relaxing activities before bed.
 You can take a hot shower or bath before bed, write notes in a diary, read, do some light stretching or yoga.
You can take a hot shower or bath before bed, write notes in a diary, read, do some light stretching or yoga. - Try relaxation techniques. Relaxation techniques such as deep breathing exercises, meditation, and acupressure (pressure on specific areas of the body to relax) can help manage anxiety and improve sleep. For more information, read the resource Integrative Medicine and Cancer Treatment or contact your health care provider. You can also take a free guided meditation course at www.mskcc.org/meditation.
- Stop using devices that emit blue light 2-3 hours before bedtime. Blue light is emitted by electronic devices such as mobile phones, tablets and computers, as well as LED lamps. Many devices come with a blue light filter that you can activate at night. You can also buy blue light blocking goggles and wear them while using electronic devices.
- Talk to your healthcare provider about other options for treating insomnia.
 Many of the integrative medicine methods offered at Memorial Sloan Kettering (MSK) can help with or relieve insomnia. These methods include, for example, cognitive behavioral therapy for insomnia (CBT-I) and acupuncture.
Many of the integrative medicine methods offered at Memorial Sloan Kettering (MSK) can help with or relieve insomnia. These methods include, for example, cognitive behavioral therapy for insomnia (CBT-I) and acupuncture. - CBT-I is a type of therapy talk that helps people change their sleep habits without the use of medication. Such therapy often helps people with chronic insomnia. For more information about CBT-I, read the resource Cognitive Behavioral Therapy for Insomnia.
- Acupuncture is a traditional Chinese medicine treatment. It involves the introduction of very thin needles into certain points of the body. Research shows that acupuncture can help relieve insomnia. To learn more about acupuncture, read the resource About Acupuncture.
- For more information about other Integrative Medicine methods that can help you manage insomnia, read our resource Integrative Medicine and Cancer Treatment .
back to top of page
MSK Resources
Counseling Center
646-888-0200
Many people find that getting counseling helps them better manage their emotions during cancer treatment. Our consultants conduct individual, group and family sessions. They may also prescribe medications to treat anxiety or depression.
Our consultants conduct individual, group and family sessions. They may also prescribe medications to treat anxiety or depression.
Our consultants provide their services in both inpatient and outpatient settings. We are located at 641 Lexington Avenue. The entrance is located at 54 th Street (between Lexington and Third Avenues).
Integrative Medicine Service
www.mskcc.org/integrative-medicine
Our Integrative Medicine Service offers patients a variety of services in addition to conventional medical care. This includes music therapy, mind/body therapy, dance and movement therapy, yoga and touch therapy. To make an appointment for these services, call 646-449-1010.
You can also schedule a consultation with an Integrative Medicine health care provider. Together, you will create a plan to help you maintain a healthy lifestyle and manage side effects. To make an appointment, call 646-608-8550.
Hours of Operation
Monday - Friday: 9:00 am to 8:00 pm
Saturday: 9:00 am to 5:00 pm
Location
Bendheim Integrative Medicine Center0115 205 East 64 th Street (at 64 th Street at Second and Third Avenues)
New York, NY 10065
cancer social work professionals provide emotional support and counseling to patients, as well as their families, friends and caregivers. Among other things, our services include active personal and interactive support groups for patients under treatment and their caregivers. In addition, we help with practical issues such as transportation and financial issues during your treatment.
Among other things, our services include active personal and interactive support groups for patients under treatment and their caregivers. In addition, we help with practical issues such as transportation and financial issues during your treatment.
Cancer social workers are available throughout the inpatient unit at Memorial Hospital and in all of MSK's outpatient facilities, including regional clinics. To speak with a cancer social worker, ask your doctor or nurse/nurse, or call the phone number above.
back to top of pageYou must have JavaScript enabled to use this form.
Share your opinion
Give us your feedback
Your feedback will help us improve the information we provide to patients and caregivers.
Questions
| Questions | Yes | To some extent | No |
|---|---|---|---|
| Was this information easy for you to understand? | Yes | To some extent | No |
What should be explained in more detail?
Date last updated
Chronic insomnia - symptoms, treatment
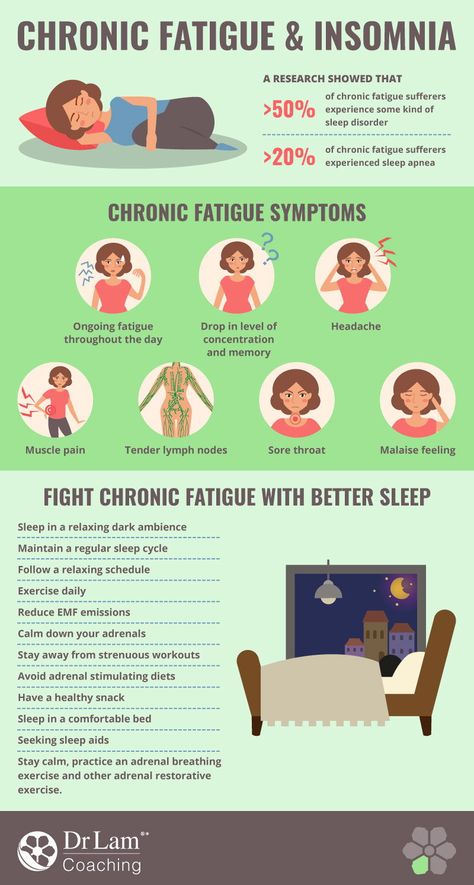
Chronic insomnia or insomnia is the most common sleep disorder. Due to chronic lack of sleep, a person's working capacity, emotional tone and mood decrease. To eliminate the pathology, physiotherapy, psychotherapy and hypnosis are used, in rare cases, drugs are prescribed.
Due to chronic lack of sleep, a person's working capacity, emotional tone and mood decrease. To eliminate the pathology, physiotherapy, psychotherapy and hypnosis are used, in rare cases, drugs are prescribed.
What is chronic insomnia?
Chronic insomnia is a pathological condition in which there is a disorder of daytime sleep and severe daytime sleepiness. It is difficult for a person to fall asleep, his sleep is superficial and intermittent, he often wakes up in the middle of the night and cannot fall asleep again. 30% of people face this problem.
Chronic insomnia negatively affects the functioning of the whole organism:
- the functioning of the immune system is disrupted;
- increases the risk of developing diseases of the digestive system;
- develop neurological disorders and psycho-emotional abnormalities;
- memory worsens, concentration of attention decreases;
- develop cardiovascular disease;
- insomnia can lead to infertility, menstrual irregularities, diabetes mellitus, thyroid dysfunction.

People with chronic insomnia are often overweight. This is due to a violation of fat metabolism and metabolism.
Why does chronic insomnia occur?
Chronic insomnia often affects people with increased levels of anxiety and a tendency to panic attacks. The problem can be caused by diseases in which pain, shortness of breath, increased blood pressure, frequent urge to urinate, and respiratory failure disturb at night. The cause may be neurosis, depression, neurasthenia, various phobias.
Triggers:
- shift or night work;
- frequent change of time zones;
- taking psychotropic drugs, narcotic drugs;
- abuse of caffeinated drinks;
- frequent, prolonged stress;
- excessive physical or mental exertion in the evening;
- people spend a lot of time with a tablet or smartphone, in front of a computer monitor,
- smoking.
Insomnia can be caused by an uncomfortable mattress or pillow, an uncomfortable temperature in the bedroom, or the presence of lights or sounds in the room.
Main manifestations
Characteristic signs of chronic insomnia include:
- it takes more than half an hour to fall asleep;
- early awakening, sleep duration less than 6 hours;
- frequent waking at night, unable to get back to sleep;
- sleep disturbance can be provoked by any trifle - dim light, sharp sound;
- in the morning after waking up, the mood is bad, feeling weak and tired, worried about headache, rapid pulse, changes in blood pressure;
- during the day I really want to sleep.
If there are signs of chronic insomnia, you should consult a somnologist. The doctor will conduct a full examination, analysis of complaints. The main diagnostic method is night polysomnography.
Therapy
Chronic insomnia requires a holistic approach.
One of the effective methods of treatment is encephalophony. "Music of the brain" is used to eliminate various neurological pathologies - sleep disturbance, migraine, depressive disorders, stress.
The essence of the technique is that during the session, the patient is given a recording of the electrical activity of the brain. Only its own melody has a healing effect. During listening, nerve cells recognize the sound of the waves as their own voice, which leads to improved functioning.
Other effective treatments for chronic insomnia:
- Inhalation of a mixture of oxygen and xenon. Such inhalations have a positive effect on the composition of cells at the molecular level without any extraneous reactions. Xenon has a tonic, regenerating, healing effect. The gas is non-toxic, completely excreted from the body, there are no negative consequences.
- Light treatment. They use special glasses that create light waves of a certain length. This allows you to normalize the change in the phases of sleep and wakefulness.
- Special relaxation exercises. Gymnastics is based on the alternation of tension and relaxation of certain muscles. Effect - tension disappears, excessive emotionality decreases.
 The patient learns to concentrate on breathing, which helps to relax and fall asleep quickly. Additionally, he masters the technique of self-hypnosis.
The patient learns to concentrate on breathing, which helps to relax and fall asleep quickly. Additionally, he masters the technique of self-hypnosis.
Medications are prescribed to eliminate pathologies that provoked the development of chronic insomnia. These can be benzodiazepines or non-benzodiazepine hypnotics, drugs based on synthetic analogs of melatonin, sedatives with natural ingredients.
Psychotherapy in the treatment of insomnia
Sleep problems are often associated with constant stress, life difficulties. To eliminate these causes, apply the methods of positive therapy. Techniques help to change negative attitudes to positive ones, activate internal reserves to combat the pathological condition. As a result, a person accepts his own uniqueness, realizes that life should be filled with health and vivid impressions.
Cognitive psychotherapy helps to get rid of anxiety. The psychotherapist looks for factors that negatively affect the quality of sleep, then works with them together with the patient.
Ericksonian hypnosis is based on a person's susceptibility to an involuntary hypnotic trance. In this state, the psyche is maximally open to positive changes. During a hypnosis session, the patient does not sleep, he sees, hears, feels everything. But at the same time, the focus of his attention switches to the internal state.
In Ericksonian hypnosis, nothing is suggested to the patient. Hypnosis is necessary to free the subconscious of a person, to find the source of problems, to create new resources.
How to get rid of chronic insomnia - advice from our doctors
To get rid of sleep problems on your own, you need to follow a few simple rules:
- you need to sleep completely in a dark room, the bedroom should be cool;
- clearly observe the daily routine;
- in bed you only need to sleep - you can’t read, deal with work issues;
- take a bath before going to bed, meditate, read;
- in the evening you need to relax without gadgets;
- do not sleep during the day - if it is difficult to do this, you can go for a walk or be distracted by household chores.
Learn more