Vitamins for ocd
Nutritional and herbal supplements in the treatment of obsessive compulsive disorder
1. Adam Y, Meinlschmidt G, Gloster AT, et al.. Obsessive–compulsive disorder in the community: 12-month prevalence, comorbidity and impairment. Soc Psychiatry Psychiatr Epidemiol 2012;47:339–49. 10.1007/s00127-010-0337-5 [PubMed] [CrossRef] [Google Scholar]
2. Boileau B. A review of obsessive-compulsive disorder in children and adolescents. Dialogues Clin Neurosci 2011;13:401–11. [PMC free article] [PubMed] [Google Scholar]
3. Goddard AW, Shekhar A, Whiteman AF, et al.. Serotoninergic mechanisms in the treatment of obsessive–compulsive disorder. Drug Discov Today 2008;13:325–32. 10.1016/j.drudis.2007.12.009 [PubMed] [CrossRef] [Google Scholar]
4. Bolton J, Moore GJ, MacMillan S, et al.. Case study: caudate glutamatergic changes with paroxetine persist after medication discontinuation in pediatric OCD. J Am Acad Child Adolesc Psychiatry 2001;40:903–6. 10.1097/00004583-200108000-00011 [PubMed] [CrossRef] [Google Scholar]
5. Chakrabarty K, Bhattacharyya S, Christopher R, et al.. Glutamatergic dysfunction in OCD. Neuropsychopharmacology 2005;30:1735–40. 10.1038/sj.npp.1300733 [PubMed] [CrossRef] [Google Scholar]
6. Arnold P, Rosenberg D, Mundo E, et al.. Association of a glutamate (NMDA) subunit receptor gene (GRIN2B) with obsessive-compulsive disorder: a preliminary study. Psychopharmacology 2004;174:530–8. 10.1007/s00213-004-1847-1 [PubMed] [CrossRef] [Google Scholar]
7. Ougrin D. Efficacy of exposure versus cognitive therapy in anxiety disorders: systematic review and meta-analysis. BMC Psychiatry 2011;11:200 10.1186/1471-244X-11-200 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
8. Dell'Osso B, Nestadt G, Allen A, et al.. Serotonin-Norepinephrine reuptake inhibitors in the treatment of obsessive-compulsive disorder. J Clin Psychiatry 2006;67:600–10. 10.4088/JCP.v67n0411 [PubMed] [CrossRef] [Google Scholar]
9. Fineberg NA, Gale TM. Evidence-Based pharmacotherapy of obsessive–compulsive disorder. Int J Neuropsychopharmacol 1999;8:107–29. 10.1017/S1461145704004675 [PubMed] [CrossRef] [Google Scholar]
Int J Neuropsychopharmacol 1999;8:107–29. 10.1017/S1461145704004675 [PubMed] [CrossRef] [Google Scholar]
10. Cannell JJ, Grant WB. What is the role of vitamin D in autism? Dermatoendocrinol 2013;5:199–204. 10.4161/derm.24356 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
11. Eyles DW, Burne THJ, McGrath JJ. Vitamin D, effects on brain development, adult brain function and the links between low levels of vitamin D and neuropsychiatric disease. Front Neuroendocrinol 2013;34:47–64. 10.1016/j.yfrne.2012.07.001 [PubMed] [CrossRef] [Google Scholar]
12. Holick MF. Vitamin D and brain health: the need for vitamin D supplementation and sensible sun exposure. J Intern Med 2015;277:90–3. 10.1111/joim.12308 [PubMed] [CrossRef] [Google Scholar]
13. Chiang M, Natarajan R, Fan X. Vitamin D in schizophrenia: a clinical review. Evid Based Ment Health 2016;19:6–9. 10.1136/eb-2015-102117 [PubMed] [CrossRef] [Google Scholar]
14. Wang T, Shan L, Du L, et al.. Serum concentration of 25-hydroxyvitamin D in autism spectrum disorder: a systematic review and meta-analysis. Eur Child Adolesc Psychiatry 2016;25:341–50. 10.1007/s00787-015-0786-1 [PubMed] [CrossRef] [Google Scholar]
Eur Child Adolesc Psychiatry 2016;25:341–50. 10.1007/s00787-015-0786-1 [PubMed] [CrossRef] [Google Scholar]
15. Parker GB, Brotchie H, Graham RK. Vitamin D and depression. J Affect Disord 2017;208:56–61. 10.1016/j.jad.2016.08.082 [PubMed] [CrossRef] [Google Scholar]
16. Cui X, Pertile R, Liu P, et al.. Vitamin D regulates tyrosine hydroxylase expression: N-cadherin a possible mediator. Neuroscience 2015;304:90–100. 10.1016/j.neuroscience.2015.07.048 [PubMed] [CrossRef] [Google Scholar]
17. Kaneko I, Sabir MS, Dussik CM, et al.. 1,25-Dihydroxyvitamin D regulates expression of the tryptophan hydroxylase 2 and leptin genes: implication for behavioral influences of vitamin D. Faseb J 2015;29:4023–35. 10.1096/fj.14-269811 [PubMed] [CrossRef] [Google Scholar]
18. Behl A, Swami G, Sircar SS, et al.. Relationship of possible stress-related biochemical markers to Oxidative/Antioxidative status in obsessive-compulsive disorder. Neuropsychobiology 2010;61:210–4. 10.1159/000306591 [PubMed] [CrossRef] [Google Scholar]
19. Garcion E, Sindji L, Montero-Menei C, et al.. Expression of inducible nitric oxide synthase during rat brain inflammation: regulation by 1,25-dihydroxyvitamin D3. Glia 1998;22:282–94. 10.1002/(SICI)1098-1136(199803)22:3<282::AID-GLIA7>3.0.CO;2-7 [PubMed] [CrossRef] [Google Scholar]
Garcion E, Sindji L, Montero-Menei C, et al.. Expression of inducible nitric oxide synthase during rat brain inflammation: regulation by 1,25-dihydroxyvitamin D3. Glia 1998;22:282–94. 10.1002/(SICI)1098-1136(199803)22:3<282::AID-GLIA7>3.0.CO;2-7 [PubMed] [CrossRef] [Google Scholar]
20. Esnafoğlu E, Yaman E. Vitamin B12, folic acid, homocysteine and vitamin D levels in children and adolescents with obsessive compulsive disorder. Psychiatry Res 2017;254:232–7. 10.1016/j.psychres.2017.04.032 [PubMed] [CrossRef] [Google Scholar]
21. Yazici KU, Yazici P, Ustundag B. Vitamin D levels in children and adolescents with obsessive compulsive disorder. Nord J psychiatry 2017:1–6. [PubMed] [Google Scholar]
22. Celik G, Tas D, Tahiroglu A, et al.. Vitamin D deficiency in Obsessive–Compulsive disorder patients with pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections: a case control study. Arch Neuropsychiatr 2016;53:33–7. 10.5152/npa.2015. 8763 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
8763 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
23. Bottiglieri T. Homocysteine and folate metabolism in depression. Prog Neuropsychopharmacol Biol Psychiatry 2005;29:1103–12. 10.1016/j.pnpbp.2005.06.021 [PubMed] [CrossRef] [Google Scholar]
24. Folstein M, Liu T, Peter I, et al.. The homocysteine hypothesis of depression. AJP 2007;164:861–7. 10.1176/ajp.2007.164.6.861 [PubMed] [CrossRef] [Google Scholar]
25. COŞAR A, İPÇİOĞLU OM, ÖZCAN Ömer, et al.. Folate and homocysteine metabolisms and their roles in the biochemical basis of neuropsychiatry. Turk J Med Sci 2014;44:1–9. 10.3906/sag-1211-39 [PubMed] [CrossRef] [Google Scholar]
26. Sharma V, Biswas D. Cobalamin deficiency presenting as obsessive compulsive disorder: case report. Gen Hosp Psychiatry 2012;34:578.e7–578.e8. 10.1016/j.genhosppsych.2011.11.006 [PubMed] [CrossRef] [Google Scholar]
27. Valizadeh N, Valizadeh M. Obsessive compulsive disorder as early manifestation of B12 deficiency. Indian J Psychol Med 2011;33:203 10.4103/0253-7176.92051 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Indian J Psychol Med 2011;33:203 10.4103/0253-7176.92051 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
28. Hermesh H, Weizman A, Shahar A, et al.. Vitamin B 12 and folic acid serum levels in obsessive compulsive disorder. Acta Psychiatr Scand 1988;78:8–10. 10.1111/j.1600-0447.1988.tb06294.x [PubMed] [CrossRef] [Google Scholar]
29. Atmaca M, Tezcan E, Kuloglu M, et al.. Serum folate and homocysteine levels in patients with obsessive-compulsive disorder. Psychiatry Clin Neurosci 2005;59:616–20. 10.1111/j.1440-1819.2005.01425.x [PubMed] [CrossRef] [Google Scholar]
30. Türksoy N, Bilici R, Yalçıner A, et al.. Vitamin B12, folate, and homocysteine levels in patients with obsessive–compulsive disorder. Neuropsychiatr Dis Treat 2014;10:1671. [PMC free article] [PubMed] [Google Scholar]
31. Ü T, Çorapçıoğlu A, Ş B, et al.. Double blind controlled study of adding folic acid to fluoxetine in the treatment of OCD. Psychiatr Danub 2019;31:69–77. [PubMed] [Google Scholar]
32. Wołonciej M, Milewska E, Roszkowska-Jakimiec W. Trace elements as an activator of antioxidant enzymes. Postepy Hig Med Dosw 2016;70:1483–98. 10.5604/17322693.1229074 [PubMed] [CrossRef] [Google Scholar]
Wołonciej M, Milewska E, Roszkowska-Jakimiec W. Trace elements as an activator of antioxidant enzymes. Postepy Hig Med Dosw 2016;70:1483–98. 10.5604/17322693.1229074 [PubMed] [CrossRef] [Google Scholar]
33. Ozdemir E, Cetinkaya S, Ersan S, et al.. Serum selenium and plasma malondialdehyde levels and antioxidant enzyme activities in patients with obsessive-compulsive disorder. Prog Neuropsychopharmacol Biol Psychiatry 2009;33:62–5. 10.1016/j.pnpbp.2008.10.004 [PubMed] [CrossRef] [Google Scholar]
34. Shohag H, Ullah A, Qusar S, et al.. Alterations of serum zinc, copper, manganese, iron, calcium, and magnesium concentrations and the complexity of interelement relations in patients with obsessive–compulsive disorder. Biol Trace Elem Res 2012;148:275–80. 10.1007/s12011-012-9371-3 [PubMed] [CrossRef] [Google Scholar]
35. Sayyah mehdi, Andishmand M, Ganji R. Effect of selenium as an adjunctive therapy in patients with treatment-resistant obsessive-compulsive disorder: a pilot randomized double blind placebo-controlled clinical trial. Arch Psych Psych 2018;20:57–65. [Google Scholar]
Arch Psych Psych 2018;20:57–65. [Google Scholar]
36. Takeda A. Movement of zinc and its functional significance in the brain. Brain Res Rev 2000;34:137–48. 10.1016/S0165-0173(00)00044-8 [PubMed] [CrossRef] [Google Scholar]
37. Peters S, Koh J, Choi D. Zinc selectively blocks the action of N-methyl-D-aspartate on cortical neurons. Science 1987;236:589–93. 10.1126/science.2883728 [PubMed] [CrossRef] [Google Scholar]
38. Sayyah M, Olapour A, Saeedabad Yshahhosseini, et al.. Evaluation of oral zinc sulfate effect on obsessive-compulsive disorder: a randomized placebo-controlled clinical trial. Nutrition 2012;28:892–5. 10.1016/j.nut.2011.11.027 [PubMed] [CrossRef] [Google Scholar]
39. Bonanomi L, Toxicology GA. Pharmacokinetics and metabolism of acetylcysteine. Eur J Respir Dis 1980;111:45–51. [PubMed] [Google Scholar]
40. Atkuri KR, Mantovani JJ, Herzenberg LA, et al.. N-Acetylcysteine—a safe antidote for cysteine/glutathione deficiency. Curr Opin Pharmacol 2007;7:355–9. 10.1016/j.coph.2007.04.005 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
10.1016/j.coph.2007.04.005 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
41. Camfield DA, Sarris J, Berk M. Nutraceuticals in the treatment of obsessive compulsive disorder (OCD): a review of mechanistic and clinical evidence. Prog Neuropsychopharmacol Biol Psychiatry 2011;35:887–95. 10.1016/j.pnpbp.2011.02.011 [PubMed] [CrossRef] [Google Scholar]
42. Ng F, Berk M, Dean O, et al.. Oxidative stress in psychiatric disorders: evidence base and therapeutic implications. Int J Neuropsychopharm 2008;11:851–76. 10.1017/S1461145707008401 [PubMed] [CrossRef] [Google Scholar]
43. Lafleur DL, Pittenger C, Kelmendi B, et al.. N-Acetylcysteine augmentation in serotonin reuptake inhibitor refractory obsessive-compulsive disorder. Psychopharmacology 2006;184:254–6. 10.1007/s00213-005-0246-6 [PubMed] [CrossRef] [Google Scholar]
44. Van Ameringen M, Patterson B, Simpson W, et al.. N-Acetylcysteine augmentation in treatment resistant obsessive compulsive disorder: a case series. J Obsessive Compuls Relat Disord 2013;2:48–52. 10.1016/j.jocrd.2012.10.003 [CrossRef] [Google Scholar]
J Obsessive Compuls Relat Disord 2013;2:48–52. 10.1016/j.jocrd.2012.10.003 [CrossRef] [Google Scholar]
45. Afshar H, Roohafza H, Mohammad-Beigi H, et al.. N-Acetylcysteine add-ontreatment in refractory obsessive-compulsive disorder: arandomized, double-blind, placebo-controlled trial. J Clin Psychopharmacol 2012;32:797–803. [PubMed] [Google Scholar]
46. Sarris J, Oliver G, Camfield DA, et al.. N-Acetyl cysteine (NAc) in the treatment of obsessive-compulsive disorder: a 16-Week, double-blind, randomised, placebo-controlled study. CNS Drugs 2015;29:801–9. 10.1007/s40263-015-0272-9 [PubMed] [CrossRef] [Google Scholar]
47. Sarris J, Oliver G, Camfield DA, et al.. Participant characteristics as modifiers of response to N-acetyl cysteine (NAc) in obsessive-compulsive disorder. Clin Psychol Sci 2016;4:1104–11. 10.1177/2167702616639864 [CrossRef] [Google Scholar]
48. Costa DLC, Diniz JB, Requena G, et al.. Randomized, Double-Blind, Placebo-Controlled Trial of N-Acetylcysteine Augmentation for Treatment-Resistant Obsessive-Compulsive Disorder. J Clin Psychiatry 2017;78:e766–73. 10.4088/JCP.16m11101 [PubMed] [CrossRef] [Google Scholar]
J Clin Psychiatry 2017;78:e766–73. 10.4088/JCP.16m11101 [PubMed] [CrossRef] [Google Scholar]
49. Paydary K, Akamaloo A, Ahmadipour A, et al.. N-Acetylcysteine augmentation therapy for moderate-to-severe obsessive-compulsive disorder: randomized, double-blind, placebo-controlled trial. J Clin Pharm Ther 2016;41:214–9. 10.1111/jcpt.12370 [PubMed] [CrossRef] [Google Scholar]
50. Ghanizadeh A, Mohammadi MR, Bahraini S, et al.. Efficacy of N-acetylcysteine augmentation on obsessive compulsive disorder: a multicenter randomized double blind placebo controlled clinical trial. Iran J Psychiatry 2017;12:134. [PMC free article] [PubMed] [Google Scholar]
51. Singer HS, Morris C, Grados M. Glutamatergic modulatory therapy for Tourette syndrome. Med Hypotheses 2010;74:862–7. 10.1016/j.mehy.2009.11.028 [PubMed] [CrossRef] [Google Scholar]
52. Cleveland WL, DeLaPaz RL, Fawwaz RA, et al.. High-Dose glycine treatment of refractory obsessive–compulsive disorder and body dysmorphic disorder in a 5-year period. Neural Plast 2009;768398. [PMC free article] [PubMed] [Google Scholar]
Neural Plast 2009;768398. [PMC free article] [PubMed] [Google Scholar]
53. Greenberg WM, Benedict MM, Doerfer J, et al.. Adjunctive glycine in the treatment of obsessive-compulsive disorder in adults. J Psychiatr Res 2009;43:664–70. 10.1016/j.jpsychires.2008.10.007 [PubMed] [CrossRef] [Google Scholar]
54. Kim H, McGrath BM, Silverstone PH. A review of the possible relevance of inositol and the phosphatidylinositol second messenger system (PI-cycle) to psychiatric disorders—focus on magnetic resonance spectroscopy (MRS) studies. Hum Psychopharmacol 2005;20:309–26. 10.1002/hup.693 [PubMed] [CrossRef] [Google Scholar]
55. Harvey BH, Brink CB, Seedat S, et al.. Defining the neuromolecular action of myo-inositol: application to obsessive-com- pulsive disorder. Prog NeuroPsychopharmacol Biol Psychiatry 2002;26:21–32. [PubMed] [Google Scholar]
56. Fux M, Levine J, Aviv A, et al.. Inositol treatment of obsessive-compulsive disorder. Am J Psychiatry 1996;153:1219–21. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
57. Carey PD, Warwick J, Harvey BH, et al.. Single photon emission computed tomography (SPECT) in Obsessive–Compulsive disorder before and after treatment with inositol. Metab Brain Dis 2004;19:125–34. 10.1023/B:MEBR.0000027423.34733.12 [PubMed] [CrossRef] [Google Scholar]
58. Fux M, Benjamin J, Belmaker RH. Inositol versus placebo augmentation of serotonin reuptake inhibitors in the treatment of obsessive–compulsive disorder: a double-blind cross-over study. Int J Neuropsychopharm 1999;2:193–5. 10.1017/S1461145799001546 [PubMed] [CrossRef] [Google Scholar]
59. Seedat S, Stein DJ. Inositol augmentation of serotonin reuptake inhibitors in treatment-refractory obsessive ??? compulsive disorder: an open trial. Int Clin Psychopharmacol 1999;14:353–6. 10.1097/00004850-199911000-00005 [PubMed] [CrossRef] [Google Scholar]
60. Rahimi R, Nikfar S, Abdollahi M. Efficacy and tolerability of Hypericum perforatum in major depressive disorder in comparison with selective serotonin reuptake inhibitors: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry 2009;33:118–27. 10.1016/j.pnpbp.2008.10.018 [PubMed] [CrossRef] [Google Scholar]
Prog Neuropsychopharmacol Biol Psychiatry 2009;33:118–27. 10.1016/j.pnpbp.2008.10.018 [PubMed] [CrossRef] [Google Scholar]
61. Sarris J, Kavanagh DJ, Kava KDJ. Kava and St. John's wort: current evidence for use in mood and anxiety disorders. J Altern Complement Med 2009;15:827–36. 10.1089/acm.2009.0066 [PubMed] [CrossRef] [Google Scholar]
62. Taylor LH, Kobak KA. An open-label trial of St. John's wort (Hypericum perforatum) in obsessive-compulsive disorder. J Clin Psychiatry 2000;61:575–8. 10.4088/JCP.v61n0806 [PubMed] [CrossRef] [Google Scholar]
63. Kobak KA, Taylor LVH, Bystritsky A, et al.. St John??s wort versus placebo in obsessive???compulsive disorder: results from a double-blind study. Int Clin Psychopharmacol 2005;20:299–304. 10.1097/00004850-200511000-00003 [PubMed] [CrossRef] [Google Scholar]
64. Sayyah M, Boostani H, Pakseresht S, et al.. Comparison of Silybum marianum (L.) Gaertn. with fluoxetine in the treatment of obsessive-compulsive disorder. Prog Neuropsychopharmacol Biol Psychiatry 2010;34:362–5. 10.1016/j.pnpbp.2009.12.016 [PubMed] [CrossRef] [Google Scholar]
Prog Neuropsychopharmacol Biol Psychiatry 2010;34:362–5. 10.1016/j.pnpbp.2009.12.016 [PubMed] [CrossRef] [Google Scholar]
65. Katiyar SK. Silymarin and skin cancer prevention: anti-inflammatory, antioxidant and immunomodulatory effects (review). Int J Oncol 2005;26:169–76. 10.3892/ijo.26.1.169 [PubMed] [CrossRef] [Google Scholar]
66. Mazzio E, Harris N, Soliman K. Food constituents attenuate monoamine oxidase activity and peroxide levels in C6 astrocyte cells. Planta Med 1998;64:603–6. 10.1055/s-2006-957530 [PubMed] [CrossRef] [Google Scholar]
67. Khom S, Baburin I, Timin E, et al.. Valerenic acid potentiates and inhibits GABAA receptors: molecular mechanism and subunit specificity. Neuropharmacology 2007;53:178–87. 10.1016/j.neuropharm.2007.04.018 [PubMed] [CrossRef] [Google Scholar]
68. Andreatini R, Sartori VA, Seabra MLV, et al.. Effect of valepotriates (valerian extract) in generalized anxiety disorder: a randomized placebo-controlled pilot study. Phytother Res 2002;16:650–4. 10.1002/ptr.1027 [PubMed] [CrossRef] [Google Scholar]
10.1002/ptr.1027 [PubMed] [CrossRef] [Google Scholar]
69. Pakseresht S, Boostani H, Sayyah M. Extract of valerian root (Valeriana officinalis L.) vs. placebo in treatment of obsessive-compulsive disorder: a randomized double-blind study. J Complement Integr Med 2011;8 10.2202/1553-3840.1465 [PubMed] [CrossRef] [Google Scholar]
70. Daily JW, Yang M, Park S. Efficacy of turmeric extracts and curcumin for alleviating the symptoms of joint arthritis: a systematic review and meta-analysis of randomized clinical trials. J Med Food 2016;19:717–29. 10.1089/jmf.2016.3705 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
71. Lopresti AL, Hood SD, Drummond PD. Multiple antidepressant potential modes of action of curcumin: a review of its anti-inflammatory, monoaminergic, antioxidant, immune-modulating and neuroprotective effects. J Psychopharmacol 2012;26:1512–24. 10.1177/0269881112458732 [PubMed] [CrossRef] [Google Scholar]
72. Chimakurthy J, Murthy TE. Effect of curcumin on quinpirole induced compulsive checking: an approach to determine the predic- tive and construct validity of the model. N Am J Med Sci 2010;2:81–6. [PMC free article] [PubMed] [Google Scholar]
N Am J Med Sci 2010;2:81–6. [PMC free article] [PubMed] [Google Scholar]
73. Sayyah M, Boostani H, Pakseresht S, et al.. Efficacy of aqueous extract of Echium amoenum in treatment of obsessive-compulsive disorder. Prog Neuropsychopharmacol Biol Psychiatry 2009;33:1513–6. 10.1016/j.pnpbp.2009.08.021 [PubMed] [CrossRef] [Google Scholar]
The 22 Best Natural Treatments and Remedies for OCD — Optimal Living Dynamics
Jordan Fallis
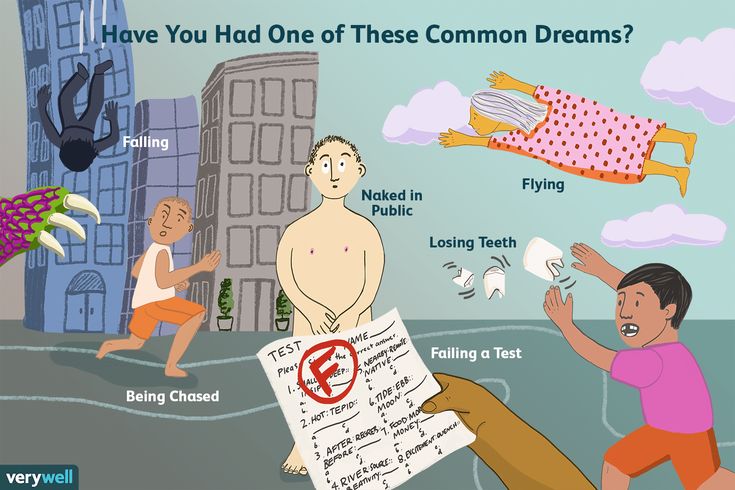
Obsessive-compulsive disorder (OCD) is a chronic mental disorder characterized by obsessions (repetitive thoughts) and compulsions (repetitive actions).
It affects about 3 per cent of adults and 1 per cent of children (79).
It’s clear that both genetic and environmental factors contribute to the development of OCD.
Research shows that OCD is often inherited and passed down within families (89).
But experiencing abuse or trauma as a child also increases the risk of developing the disorder (86-88).
Both children and adults with OCD have high levels of cortisol (a stress hormone) in their blood, and increased glutamate (an excitatory neurotransmitter) in their brain (80-83).
They also have lower levels of GABA and serotonin, which are relaxing neurotransmitters in the brain (84-85).
Antidepressant medication is the standard treatment for OCD.
But many people prefer to manage and treat their OCD without having to rely on drugs.
Researchers have studied many different natural treatments for OCD, and this article explores the most promising ones.
The first section of this article explores the best nutrients, herbs and supplements to naturally treat OCD.
The second section of the article explores the best lifestyle habits, therapies and practices to combat and overcome OCD.
It is important to note that people with OCD often have to try more than one therapy to find one that works well for them.
You shouldn't suddenly change or discontinue your current OCD treatment without consulting with your doctor first.
But read on to learn about some of the best natural remedies and therapies that can help reduce your symptoms of obsessive-compulsive disorder.
1. N-Acetyl CysteineN-Acetyl-Cysteine (NAC) is a modified form of the amino acid cysteine.
It’s also the precursor to glutathione, your body’s master antioxidant.
Nowadays, we’re exposed to so many environmental toxins, which cause oxidative stress in the body and deplete our reserves of cysteine and glutathione.
But supplementing with NAC can increase and normalize your cysteine and glutathione levels.
This can combat and reduce oxidative stress in your brain, which can then help treat several mental illnesses, including OCD.
More than one study has found that NAC can significantly improve OCD symptoms in more than half of OCD patients (44, 46).
And a systematic review determined that NAC is effective at reducing the severity of OCD symptoms with minimal side effects (45).
NAC is included in Optimal Antiox.
Be sure to read this article all about the benefits of NAC.
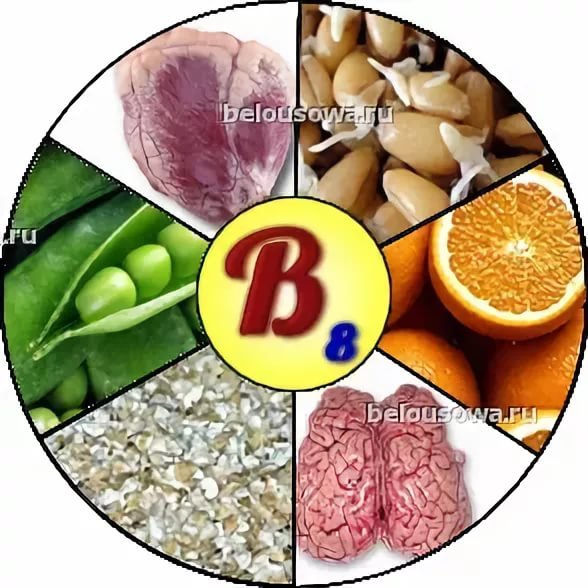
2. InositolInositol is a naturally-occurring molecule found in nearly all plants and animals. It plays a key role in various biological processes.
The brain has the highest concentration of inositol, where it plays an important role making and affecting neurotransmitters, including serotonin (1).
Inositol can be found in many foods, particularly fruit, especially cantaloupe and oranges (2).
It used to be considered a B Vitamin (Vitamin B8). But it currently is no longer considered an essential nutrient because your body can produce inositol from glucose (3).
But it currently is no longer considered an essential nutrient because your body can produce inositol from glucose (3).
However, supplementation with inositol can still help reduce symptoms of OCD.
In one study, patients with OCD took 18 grams of inositol or placebo daily for six weeks.
At the end of the six weeks, the patients who took inositol had significantly lower scores on the Yale-Brown Obsessive Compulsive Scale.
The researchers concluded that inositol can effectively treat obsessive-compulsive disorder (4-5).
It’s important to point out that the research suggests that you need to take high doses (12 to 18 grams daily) if you want to experience the anxiety-reducing benefits of inositol.
I took high doses of this inositol powder when weening off psychiatric medication.
I personally noticed a reduction in my obsessive-compulsive tendencies while supplementing with it.
Check out my full post about inositol to learn more about the benefits.
3. ZincZinc is an essential mineral for mental health, especially if you have chronic anxiety.
Unfortunately, many people are deficient in zinc. In fact, it’s estimated that 2 billion people in the world are deficient. And this often includes people with OCD.
Researchers have found that patients with OCD tend to have much lower levels of zinc that individuals without OCD (49).
And one study showed that zinc supplementation helped reduce obsessions and compulsions without side effects (50).
I created and take the Optimal Zinc supplement to make sure my zinc levels are optimal. I created it because I want to give my clients and readers the very best zinc supplement so that they can experience superior results. I have found that many zinc supplements on the market fall short. Optimal Zinc includes several other nutrients (co-factors) that increase the absorption of zinc.
I have found that many zinc supplements on the market fall short. Optimal Zinc includes several other nutrients (co-factors) that increase the absorption of zinc.
Besides supplementing, you should also eat plenty of healthy, whole foods that contain zinc.
Some of the best foods to optimize your zinc levels include:
Oysters
Grass-fed beef
Pumpkin seeds
Cashews
Mushrooms
Spinach
These foods are included in my Free Grocery Shopping Guide for Optimal Brain and Mental Health.
Check out my previous post all about zinc and anxiety if you want to learn more about how zinc impacts anxiety levels and can contribute to OCD.
Zinc can also stimulate your vagus nerve, which reduces anxiety.
Glycine is an amino acid commonly found in protein-rich foods such as meat, fish, collagen and gelatin.
Glycine is one of three amino acids that your body uses to make glutathione, the master antioxidant in your body.
Supplementing with 60 grams of glycine daily has been shown to reduce OCD symptoms (70).
I personally take this collagen protein powder to make sure I get enough glycine. Or you can supplement with pure glycine powder.
Another option is to take sarcosine.
Sarcosine is a natural supplement that inhibits the uptake of glycine. By doing this, it increases the availability of glycine in the brain.
Researchers have found that sarcosine can lead to quick, profound and sustained improvements in OCD symptoms (71).
I’ve tried sarcosine and I find that it’s much more powerful and effective at improving mental health symptoms than taking glycine or collagen powder. It's very good at reducing anxiety.
You can get sarcosine here or here.
5. CurcuminCurcumin is the most heavily researched compound within turmeric, the spice that gives curry its yellow colour.
It’s one of my favourite natural compounds for optimal health.
Research shows that curcumin can significantly improve obsessive-compulsive symptoms by increasing serotonin (53).
Curcumin is a good option if you struggle with chronic inflammation, depression and OCD.
In my experience, it doesn’t help as much if you only have anxiety.
Since curcumin is a fat soluble, take it with a fatty meal.
Caffeine is a surprising natural remedy for OCD.
It usually increases anxiety and stress in most people.
But research shows that it can improve OCD symptoms.
Two clinical trials found that caffeine significantly reduces the severity of OCD symptoms in people with treatment-resistant OCD (47-48).
I recently cut out coffee completely but I used to drink this coffee.
You can also just take pure caffeine tablets if you want. I sometimes take these tablets before a workout.
Coffee and caffeine can disrupt sleep though, so make sure you don’t drink it in the evening close to bed. Some people like me are really sensitive and have to stop drinking it very early in the day so that it doesn’t disrupt their sleep.
It's also a good idea to try to consume the whole coffee fruit, instead of just coffee or pure caffeine.
Traditionally, the coffee bean is extracted from the coffee fruit for roasting. And the surrounding fruit is discarded.
But that’s a problem because the coffee fruit contains several healthy compounds not found in coffee beans themselves.
And researchers have found that consuming whole coffee fruit concentrate can significantly enhance cognitive functioning.
That’s why I included coffee fruit in the Optimal Brain supplement.
7. MagnesiumMagnesium is the fourth most abundant mineral in the human body, and it’s absolutely essential for optimal mental health.
It’s absolutely essential for the proper functioning of your nervous system and optimal neurotransmitter activity.
Unfortunately, many people don’t get enough of it, even if they eat a healthy diet.
Research shows that low magnesium levels contribute and worsen many neuropsychiatric problems, including OCD.
Patients with OCD have significantly lower levels of magnesium in their blood than people without OCD (54).
So if you have OCD, it’s clearly important to make sure you’re getting enough magnesium so that you don’t have a deficiency.
Since most people are deficient, magnesium is one of the three supplements that I think everyone should be taking every day.
I personally take this supplement every day for energy, and it includes magnesium.
Epsom salt baths are another great way to increase your body’s intake of magnesium.
You should also make sure you’re eating enough magnesium-rich foods on a regular basis, including:
Spinach
Chard
Pumpkin seeds
Almonds
Avocado
Dark chocolate
Bananas
These foods are included in my Free Grocery Shopping Guide for Optimal Mental Health.
Milk thistle is a herb commonly used to improve liver health and protect the liver from alcohol and other drugs.
Silymarin, one of the flavonoids in milk thistle, has been shown to increase serotonin levels in the brains of animals (72).
And one human study found that milk thistle works just as well as a popular SSRI antidepressant at reducing OCD symptoms (73).
9. ProbioticsAs you probably already know, the health of your gut (and the bacteria within it) significantly influence your brain and mental health.
So not surprisingly, probiotics have been shown to be another possible natural remedy for OCD.
Studies also show that the neurotransmitter serotonin is produced in the gut.
By taking a probiotic supplement, you can enhance the diversity of the bacteria in your gut, create a better environment for the synthesis of serotonin, and therefore increase serotonin levels and activity in your brain (18).
Probiotics have also been shown to stimulate the vagus nerve and reduce inflammation, which tends to be elevated in people with OCD.
A systematic review of 38 studies concluded the probiotics can improve psychiatric disorder-related behaviors, including anxiety and OCD (55).
The researchers found that the following probiotics can help with OCD:
Bifidobacterium longum
Bifidobacterium breve
Lactobacillus rhamnosus
All three of these probiotics are included in the Optimal Biotics supplement.
You can also check out this article to learn more about the top 9 psychobiotics that can help reduce your anxiety.
And this article includes 5 ways to increase your good gut bacteria.
10. Borage Oil
Borage OilBorage oil is a natural remedy made from the seeds of the Borago officinalis plant.
The oil is high in gamma linoleic acid (GLA), which is an essential fatty acid that must be obtained from your diet.
It’s commonly used to help reduce the inflammation that is linked to many chronic diseases.
Its anti-inflammatory effects may be why it helps reduce OCD.
Researchers have found that 500 mg of borage oil per day can reduce obsessive and compulsive and anxiety symptoms (75).
Animal research also shows that it can have anti-anxiety effects similar to benzodiazepines (74).
I took this borage oil years ago but no longer feel the need to take it.
11. IronIron is a trace mineral found in every living cell in our bodies.
It carries oxygen to all parts of your body, and low levels can leave you feeling tired, pale, irritable and foggy.
But research also shows that iron is an important cofactor in the synthesis of serotonin, and an iron deficiency can increase the risk of developing an anxiety disorder (6).
Researchers have also found that blood iron levels are significantly lower in patients with mild and moderate OCD (51).
Despite this, I don’t actually recommend supplementing with iron because some research suggests that too much iron can cause health problems and actually increase anxiety (7).
It’s definitely a much better idea to test your iron levels and naturally get your iron from food.
I make sure I get enough simply by taking these grass-fed beef liver capsules.
Beef liver is one of the best sources of iron. But I don’t like the taste of cooked beef liver, so I go with the capsules instead.
Some other good sources of iron include:
Spirulina
Dark chocolate
Spinach
Sardines
Pistachios
Raisons
These foods are included in my Free Grocery Shopping Guide for Optimal Brain and Mental Health.
Ashwagandha (Withania sominifera) is a popular Indian herb that has been used for more than 3000 years. It’s sometimes called the “Indian Ginseng”.
It’s known as an “adaptogen”, which is a compound that balances the body and restores normal bodily functioning after chronic stress.
In one study, 30 people with OCD took ashwagandha for 6 weeks, and it notably and significantly reduced their OCD symptoms (52).
Animal research also shows that ashwagandha causes anti-anxiety effects, reduces OCD-like behaviour and improves stress tolerance in rats (8-13).
So it’s a pretty impressive herbal remedy for OCD and anxiety.
But how does it work?
By increasing serotonin and GABA in the brain, and lowering cortisol levels by 25 per cent (14-17).
Ashwagandha is one of the main herbs I took to help myself get off psychiatric medications.
I took this one.
13. SaffronSaffron is a spice derived from the Crocus sativus plant.
It has a number of health benefits due to the medicinal compounds within it.
Saffron is one of the best supplements for reducing depression, anxiety and stress.
Safranal and Crocetin, two of the compounds within saffron, have been shown to stimulate GABA receptors and increase serotonin levels in the brain (19-20).
As a result, researchers have determined that saffron can reduce compulsive behavior (56).
14. ValerianValerian (Valeriana officinalis) is a natural herb, and the root of the herb has traditionally been used to treat insomnia.
But it also can reduce symptoms of OCD.
In one study, supplementing with 750 mg of valerian for eight weeks reduced symptoms by 25% in people diagnosed with OCD (57).
And in an animal study, valerian demonstrated anti-obsessive and anti-compulsive effects and researchers determined it's a good candidate for treating obsessive-compulsive disorder (21).
Scientists have collected a massive amount of research demonstrating that the compounds in valerian naturally reduce symptoms of OCD by:
Partially activating serotonin receptors
Maintaining serotonin levels
Reducing stress hormone levels
Binding to GABA receptors in the amygdala, a brain region associated with fear and anxiety
Increasing GABA levels
Inhibiting the breakdown of GABA in the brain (22-43).
As a result of this, it creates a calming effect similar to anti-anxiety drugs like Xanax and Valium.
This is why valerian is often called “Nature’s Valium”.
Valerian is one of the first herbal remedies I took years ago to manage my anxiety at night and improve my sleep.
It’s included in this anti-anxiety supplement.
Valerian supplements include the roots and stems of the plant.
But you can also take it as a tea or tincture if you want.
15. Cognitive Behavioral TherapyCognitive behavioral therapy (CBT) is one of the first-line treatments for OCD.
It involves challenging and changing unhelpful cognitive distortions and behaviors, improving emotional regulation, and developing personal coping strategies.
A meta-analysis of high-quality studies concluded that CBT is an effective method for treating OCD and reducing OCD symptoms (77-78).
I personally never found CBT helpful for my mental health issues but other people do.
It’s definitely worth trying if you OCD though.
16. NeurofeedbackNeurofeedback is a type of biofeedback that shows you your brain activity in real-time and teaches you how to self-regulate it.
Sensors are placed on your scalp to measure your brain’s activity, and the measurements are displayed using video or sound.
Personally, neurofeedback was the most impactful actions I took to overcome severe anxiety.
It works at a deep subconscious level, breaking the cycle of chronic anxiety.
It allows shifts you into a natural, healthier state of mind.
And research shows that it works for people with OCD.
One study showed that it can normalize brain activity in people with OCD (58).
If you want to try neurofeedback, it’s best to work with a qualified neurofeedback practitioner.
If you’re interested in neurofeedback, I recommend booking a consultation with me to determine the best type of neurofeedback for you and your condition. I have found that some types of neurofeedback are ineffective.
I have found that some types of neurofeedback are ineffective.
I also recommend the Muse headband. It’s a decent substitute to real neurofeedback and gives you real-time feedback in your brainwaves while you meditate.
I previously wrote about the Muse headband here, and you can get it through Amazon or the Muse website.
17. Light TherapyLight therapy is another natural therapy that you may be able to use to manage and treat your OCD.
I came across a case study of a woman who had OCD and it got a lot worse in the winter.
But two hours of light therapy every day for two weeks improved her mood and reduced her symptoms of obsession.
What’s most surprising is that her condition remained stable for 16 months afterwards. She even made it through the next following winter (69).
I personally get sunlight every day during the spring and summer months to support my mental health.
I also use a number of different at-home devices to improve my mood and optimize my brain function.
Throughout the winter, I use a seasonal affective disorder (SAD) light box. I turn it on next to my desk in the morning. I use this lightbox.
I also have a Vitamin D sunlamp for the winter months.
And all year around, I use low-level red-light therapy (LLLT) to improve my mood and cognitive function. I use these three LLLT devices:
Optimal 1000 Brain Photobiomodulation Therapy Light (Combo Red/NIR) - This is a powerful device that shines 660 nm of red light and 850 nm of infrared light. I shine it on my forehead for 5 minutes every day. I also shine it on other parts of my head and on my entire body, including on my thyroid, thymus gland and gut.
 I experience incredible benefits from doing this.
I experience incredible benefits from doing this.Optimal 300 Brain Photobiomodulation Therapy Light (Combo Red/NIR) - This is a smaller and more convenient device that I take with me when I’m travelling. I shine it on my forehead.
Vielight Neuro Duo – This is a transcranial-intranasal headset with 810 nm of near infrared light that I’ve now been using regularly. It penetrates deeper into brain tissue and is absorbed better by the central nervous system. If you decide to get this one, you can use the coupon code JORDANFALLIS for a 10% discount. Some research has shown a 20-fold higher efficiency of light delivery to the deep brain through the nose instead of transcranial application (125). Vielight has several different devices and you can also use the coupon code JORDANFALLIS for 10% off any of them.
You can read more about LLLT here.
I highly recommend all of the above devices if you really want to optimize your mental health and reduce symptoms of OCD.
Meditation is my favourite daily activity to relax and ground myself.
And if you have OCD, you should try to add it into your daily routine as well.
In one study, OCD patients received mindfulness training. They were taught meditative breathing, body-scan, and mindful daily living.
By the end of the study, they witnessed a “significant and large reduction” in their OCD symptoms. It was much easier for them to “let go” (66).
I use the Muse headband to meditate. It gives you real-time feedback while you meditate. That way, you know how well you are meditating. It makes meditation a lot more fun and tolerable.
I previously wrote about the Muse headband here, and you can get it through Amazon or the Muse website.
19. Mindfulness-Based Cognitive TherapyMindfulness-based cognitive therapy (MBCT) is a type of therapy that includes a mix of cognitive behavioral therapy methods and mindfulness meditate practices.
As mentioned before, mindfulness meditation and cognitive behavioral therapy help people with OCD individually.
So it’s not too surprising they also help when used in combination.
In one study, eight weeks of MBCT reduced OCD symptoms.
Two third of the participants reported a decline in symptoms, including an increased ability to let unpleasant emotions surface and to live more consciously in the present (76).
20. ExerciseExercise is another natural way to manage and treat OCD.
It’s easily accessible and free, and many doctors and researchers recommend exercise as their number one piece of advice for optimal mental health.
Five different studies have found that aerobic exercise can reduce OCD symptoms (59-63).
After exercising for 12 weeks, study participants reported fewer obsessions and compulsions, and the benefits remain for 6 months (64).
The exercise doesn’t need to be intense though.
Even simply walking can reduce symptoms of OCD (65).
Exercise can be a big chore for a lot of people, so I recommend finding some sort of sport or aerobic activity that you enjoy. That way you won’t get sick of it and you’ll exercise regularly.
21. MusicMusic is actually very healing and can have a calming effect on the brain.
I previously wrote about how music can naturally reduce cortisol, and increase dopamine and oxytocin.
This is probably why it’s been shown to help people with OCD.
In one study, music therapy reduced symptoms of obsession, depression and anxiety in patients with OCD (67).
22. AcupunctureAcupuncture is another natural treatment that has been shown to help people with OCD.
In one study, 19 patients with treatment-resistant OCD received 12 sessions of acupuncture, and it significantly alleviated their OCD symptoms (68).
I’m personally a really big fan of auricular acupuncture. Auricular acupuncture is when needles are inserted into ear. I’d recommend trying to find a health practitioner in your area who provides it, especially if you’re weening off psychiatric medication. It really helped me the first time I came off antidepressants. I was surprised.
At the end of each appointment, my practitioner would secure these small black seeds on my ear.
In my experience, ear acupuncture is more effective than regular acupuncture.
I also lie on this acupuncture mat at home to relax before bed.
References:
(1) https://en.wikipedia.org/wiki/Inositol
(2) https://www.ncbi.nlm.nih.gov/pubmed/7416064
(3) https://en.wikipedia.org/wiki/Inositol
(4) https://www.ncbi. nlm.nih.gov/pubmed/8780431
nlm.nih.gov/pubmed/8780431
(5) https://www.ncbi.nlm.nih.gov/pubmed/9169302
(6) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3680022/
(7) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4253901/
(8) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3252722/
(9) https://www.ncbi.nlm.nih.gov/pubmed/11194174
(10) https://www.ncbi.nlm.nih.gov/pubmed/18476388
(11) https://www.ncbi.nlm.nih.gov/pubmed/22546655
(12) https://www.ncbi.nlm.nih.gov/pubmed/12895672
(13) https://www.ncbi.nlm.nih.gov/pubmed/10075127
(14) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4270108/
(15) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3252722/
(16) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2958355/pdf/IJPsy-42-295.pdf
(17) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3040882/
(18) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5319175/
(19) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4599112/
(20) https://www. ncbi.nlm.nih.gov/pmc/articles/PMC4599118/
ncbi.nlm.nih.gov/pmc/articles/PMC4599118/
(21) https://www.ncbi.nlm.nih.gov/pubmed/22718671
(22) https://www.ncbi.nlm.nih.gov/pubmed/14742369
(22) https://www.ncbi.nlm.nih.gov/pubmed/10411208
(24) https://www.ncbi.nlm.nih.gov/pubmed/17585957
(25) https://www.ncbi.nlm.nih.gov/pubmed/18095218
(26) https://www.ncbi.nlm.nih.gov/books/NBK11084/
(27) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4863311/
(28) https://www.ncbi.nlm.nih.gov/pubmed/14751470
(29) https://www.ncbi.nlm.nih.gov/pubmed/12895671
(30) https://www.ncbi.nlm.nih.gov/pubmed/12662130
(31) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4303399/
(32) https://www.ncbi.nlm.nih.gov/pubmed/20634372
(33) https://www.ncbi.nlm.nih.gov/pubmed/24758222
(34) https://www.ncbi.nlm.nih.gov/pubmed/18160026
(35) https://www.ncbi.nlm.nih.gov/pubmed/18602406
(36) https://www.ncbi.nlm.nih.gov/pubmed/20042323
(37) https://www. ncbi.nlm.nih.gov/pubmed/25495725
ncbi.nlm.nih.gov/pubmed/25495725
(38) https://www.ncbi.nlm.nih.gov/pubmed/26177123
(39) https://www.ncbi.nlm.nih.gov/pubmed/20957125
(40) https://jamanetwork.com/journals/jamapsychiatry/fullarticle/482548
(41) https://www.ncbi.nlm.nih.gov/pubmed/15921820
(42) https://www.ncbi.nlm.nih.gov/pubmed/10622375
(43) https://www.ncbi.nlm.nih.gov/pubmed/24055511
(44) https://www.ncbi.nlm.nih.gov/pubmed/19581567
(45) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4423164/
(46) https://www.ncbi.nlm.nih.gov/pubmed/23131885
(47) https://www.ncbi.nlm.nih.gov/pubmed/19573497
(48) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6559101/
(49) https://www.ncbi.nlm.nih.gov/pubmed/22383079
(50) https://www.ncbi.nlm.nih.gov/pubmed/22465904
(51) https://www.ncbi.nlm.nih.gov/pubmed/22383079
(52) https://www.ncbi.nlm.nih.gov/pubmed/27515872
(53) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3354439/
(54) https://www. ncbi.nlm.nih.gov/pubmed/22383079
ncbi.nlm.nih.gov/pubmed/22383079
(55) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5056568/
(56) https://www.ncbi.nlm.nih.gov/pubmed/22985509
(57) https://www.ncbi.nlm.nih.gov/pubmed/22718671
(58) http://www.yalescientific.org/2016/02/battling-ocd-in-real-time-live-brain-imaging-helps-patients-attack-anxiety-at-the-source/
(59) https://www.ncbi.nlm.nih.gov/pubmed/17568300/
(60) https://www.ncbi.nlm.nih.gov/pubmed/19616916/
(61) https://www.ncbi.nlm.nih.gov/pubmed/25738234
(62) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5726421/
(63) https://www.ncbi.nlm.nih.gov/pubmed/30699885
(64) https://www.ncbi.nlm.nih.gov/pubmed/19616916
(65) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3567313/
(66) https://www.ncbi.nlm.nih.gov/pubmed/18852623
(67) https://www.ncbi.nlm.nih.gov/pubmed/26066780
(68) https://www.ncbi.nlm.nih.gov/pubmed/19684500
(69) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4361980/
(70) https://www. ncbi.nlm.nih.gov/pubmed/19046587
ncbi.nlm.nih.gov/pubmed/19046587
(71) https://www.ncbi.nlm.nih.gov/pubmed/21508860
(72) https://www.tandfonline.com/doi/abs/10.1080/13880200490519712
(73) https://www.ncbi.nlm.nih.gov/pubmed/20035818
(74) https://www.ncbi.nlm.nih.gov/pubmed/15261383
(75) https://www.ncbi.nlm.nih.gov/pubmed/19737592
(76) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3549892/
(77) https://www.ncbi.nlm.nih.gov/pubmed/17849776
(78) https://www.ncbi.nlm.nih.gov/pubmed/22999486
(79) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2797569/
(80) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3613755/
(81) https://www.ncbi.nlm.nih.gov/pubmed/18424906/
(82) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3762604/
(83) https://www.ncbi.nlm.nih.gov/pubmed/12888801/
(84) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3762604/
(85) https://www.ncbi.nlm.nih.gov/pubmed/8201248
(86) https://www.ncbi.nlm.nih.gov/pubmed/22024245
(87) https://www. ncbi.nlm.nih.gov/pmc/articles/PMC3181951/
ncbi.nlm.nih.gov/pmc/articles/PMC3181951/
(88) https://www.ncbi.nlm.nih.gov/pubmed/28549337
(89) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181951/
Terms and Conditions
Privacy Policy
Affiliate Disclosure
Disclaimer
Tags best natural ocd treatments, ocd treatments, natural remedies, ocd remedies, best ocd remedies, supplements, cures, remedies, ocd, OCD, without medication, without drugs, without meds, without medicine, natural medicine, anxiety, diet, ocd diet, ocd foods, foods, ways to reduce ocd, ways to reduce, helps treat ocd, Obsessive-Compulsive Disorder, obsessions, compulsions, disorders, intrusive thoughts, herbs, control ocd, ocd in adults, ocd in children, depression, remedy, cure, symptoms, how to treat ocd, ocd alternatives, ocd food, ocd healing, ocd protocol, vitamins, ocd vitamins, childhood ocd, harm ocd, severe ocd, beat ocd, combat ocd, decrease ocd, heal ocd, improve ocd, manage ocd, overcome ocd, stop ocd, ocd solutions, natural approach to ocd, ocd therapy, inositol, inositol for ocd, treating ocd naturally, paleo for ocd, natural plan for ocd, treat ocd on your own, ocd cleaning, ocd checking, natural ocd relief, herbal remedies, herbal medicine, herbal supplements, holistic, pure ocd, ayurveda, treat ocd yourself, biomedical, chinese medicine ocd, easy, skin picking, functional medicine, ocd list, meditation for ocd, music for ocd, overthinking, orthomolecular medicine, ocd curable, ocd tips
OCD: Supplements to help overcome it
Obsessive Compulsive Disorder (OCD) is exactly what its name suggests.
Basically, it is a mental condition in which a person experiences intrusive, intrusive and disturbing thoughts that cause feelings of discomfort and/or fear, often leading to obsessive-compulsive behavior.
This can manifest itself in a variety of ways, such as (R):
- Body Dysmorphic Disorder (BDD), in which a person cannot stop thinking about one or more perceived defects or flaws in their appearance. For example, "if I had a smaller forehead or if I was 7 centimeters taller, I would be perfect and everyone would love me."
- Storage disorder.
- Trichotillomania, in which hair is pulled out of the scalp, eyebrows and other parts of the body.
- Excoriation (skin picking) disorder.
- Intrusive/repetitive checks, such as whether you locked the door, etc.
- Hand washing and germ phobia.
- Obsessive thoughts and reflections.
- Ritualized eating behavior characteristic of eating disorders.
- Substance or gambling preoccupation, as seen in substance-related disorders and addictions.

- Preoccupation with illness, as in an anxiety disorder of illness.
- Sexual impulses or fantasies, as in paraphilic disorders.
- Impulses seen in disruptive, impulse control and behavioral disorders.
- Reflections of guilt that arise in major depressive disorder.
- Intrusion or delusional preoccupation, as in the schizophrenic spectrum and other psychotic disorders.
- Repetitive behavior patterns that are characteristic of autism spectrum disorders.
- Fears such as fear of infection, fear of aggression/harm, sexual fears, religious fears and the need to do things "right". Compensatory compulsions for these obsessions include laundry and cleaning, checking, seeking reassurance, repetition, as well as ordering, organizing, etc.
anxiety, depression, autism, fear, etc., so "treatment" can overlap, because what can reduce anxiety, for example, can also reduce OCD.
Let's look at a few mechanisms in the body that potentially contribute to OCD.
HPA axis, glutamate and GABA
HPA (hypothalamus-pituitary-adrenal) axis
The entire stress cascade is elevated in OCD. From the hypothalamus, which secretes the inflammatory corticotropin-releasing hormone (CRH), all the way to the adrenal glands, which secrete cortisol.
Lack of cortisol suppression in the dexamethasone suppression test (DST) is a sign of an abnormal HPA axis in patients with OCD, which may be explained by possible pituitary numbness due to high levels of CRH (CRH) (R). Interestingly, acetylcholine can reduce sensitivity to CRH and lead to increased levels of CRH, ACTH, and cortisol.
Atropine, an anticholinergic drug, activates CRH receptors in the cerebral cortex and shows that excess acetylcholine can contribute to CRH insensitivity and lead to high CRH levels.
High Acetylcholine Syndrome (coming soon)
By taming the HPA axis, we can significantly reduce the symptoms of OCD. And it has been found with many adaptogens such as ashwagandha, valerian, magnesium, etc.
And it has been found with many adaptogens such as ashwagandha, valerian, magnesium, etc.
> Learn more about how to lower cortisol levels here (coming soon)
DHEA-S and GABA
OCD patients also have higher plasma levels of dehydroepiandrosterone sulfate (DHEAS), a neuroactive steroid that has an effect opposite to that of allopregnanolone (R). In this study, the effects of allopregnanolone against obsessive-compulsive disorder were comparable to those of fluoxetine, and the benefits were blocked by finasteride (R).
DHEA-S opposes GABA while allopregnanolone is pro-GABA. Too much DHEA-S can leave you in a state of over-activation, such as ADD, ADHD, anxiety, rumination, depression, etc. GABA is needed to inhibit glutamate, which is chronically elevated in OCD.
Another note about acetylcholine:
Decreasing acetylcholine levels by blocking its receptors or by presynaptically activating mAChR M2/M4 (which act as inhibitory autoreceptors) reduces glutamate release.
Excess glutamate is associated with depression.
...
glutamatergic hyperactivity is associated with obsessive-compulsive disorder, which may be due to the fact that activation of nicotinic receptors releases glutamate (R).
Glutamate
Some studies have shown that the concentration of glutamate is significantly higher in the cerebrospinal fluid of patients with obsessive-compulsive disorder compared to healthy people. Higher glutamate concentrations are associated with excitotoxicity and oxidative stress (glutamate is excitotoxic and neurotoxic) in patients with obsessive-compulsive disorder, and this appears to be correlated with symptom severity (R).
Glutamate acts on a variety of receptors, one of which is NMDA. Quinolic acid is also an agonist at this receptor and can cause neurotoxicity in large amounts. Quinolic acid is formed in the kynurenine pathway, which is activated by inflammation. Reducing inflammation by reducing intake of polyunsaturated fats, reducing excess iron (and other heavy metals) in the body, lowering parathyroid hormone and aldosterone levels, calming gut inflammation, etc. can help reduce excessive inflammation.
can help reduce excessive inflammation.
Turmeric, taurine, glycine, carnosine, niacinamide, magnesium, zinc, selenium, cocoa, vitamin C, E, aspirin, vitamin D, and a host of other herbs and supplements can help reduce inflammation.
GABA keeps glutamate (as well as other neurotransmitters) in check, so when GABA is inhibited, neurotransmitters such as glutamate, CRH, serotonin, acetylcholine, etc. can become too high.
GABAergic supplements are very helpful against OCD. Additives such as:
- Progesterone and its 5-alpha-reduced metabolite, 5-alpha-dihydroprogesterone (5a-DHP)
- Niacinamide (many say that niacin and/or niacinamide did a great job with OCD anxiety)
- Taurine
- Valerian root
- Zinc (anxiety and obsessive thoughts (R).
- Baikal skullcap
- Magnolia
- etc.
Another method that has been used for OCD is deep brain stimulation (DBS). The procedure includes drilling holes in your skull and inserting rods into your brain that change the function of various nuclei. It has been shown to suppress the HPA axis and increase thyroid hormone levels, which correlates with improvement in symptoms (R).
It has been shown to suppress the HPA axis and increase thyroid hormone levels, which correlates with improvement in symptoms (R).
This is what 0.01% of people with OCD would do, but it's interesting to note that DBS lowered cortisol levels and increased thyroid levels. Thus, thyroid function is also likely to be suboptimal in people with OCD.
This study showed that in patients with OCD, the TSH response to TRH is blunted, meaning they are more likely to have insufficient T4 and T3 with elevated prolactin (TRH increases prolactin) (R).
Melatonin
In patients with obsessive-compulsive disorder, 24-hour melatonin secretion was reduced compared to healthy controls, while its circadian rhythm was preserved (R).
Agomelatine, a melatonin receptor agonist and also a 5-HT2C serotonin receptor antagonist, is useful in obsessive-compulsive disorder (R, R).
Serotonin
Serotonin appears to be involved/disturbed in almost all psychiatric disorders.
Serotonin is created by tryptophan hydroxylase 2 (TPh3) in the brain from the amino acid tryptophan. Serotonin binds to its receptors, 5-HT1 to 5-HT7. (R , R ).
By activating serotonin receptors, 5-HT1A, 1B and 1D have anti-OCD effects, reducing production of serotonin (R, R). Ketamine, a 5-HT1B agonist, has rapid anti-obsessive-compulsive disorder properties in animal models at low doses (R).
mCPP, a potent serotonergic drug, when given to untreated OCD patients increases their anxiety, depression, and dysphoria, and worsens their OCD symptoms (R).
Clomipramine, the gold standard treatment for obsessive-compulsive disorder, inhibits serotonin and norepinephrine reuptake but is a potent α1-adrenergic receptor, histamine h2 receptor, serotonin 5-HT2A, 5-HT2C, 5-HT3, 5-HT6 and 5-HT7 receptors, dopamine D1, D2 and D3 receptors and muscarinic acetylcholine receptors (M1 - M5).
It is clear that the "beneficial" serotonergic drugs work not only by increasing serotonin levels, as shown above, since gold standard serotonergic drugs block most serotonin receptors.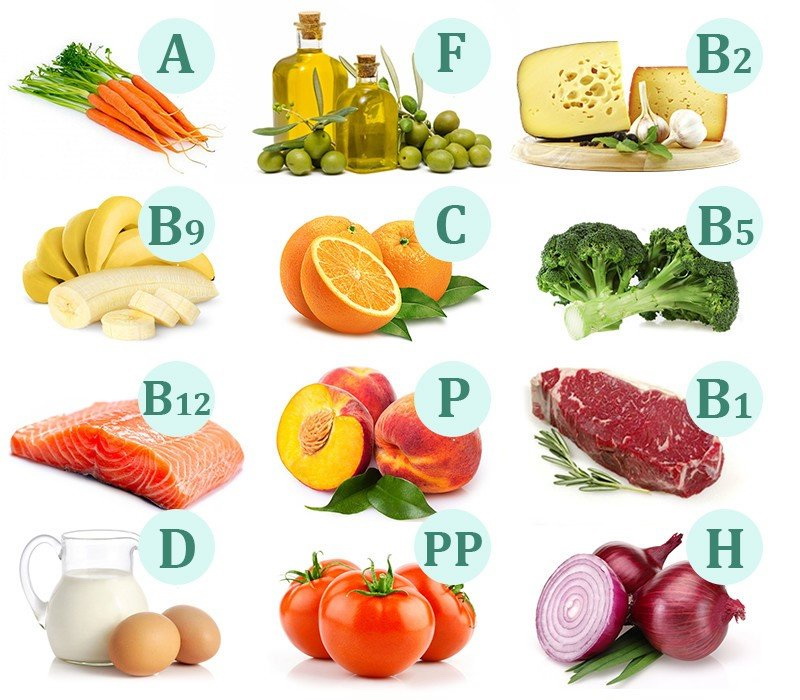
On the other hand, metergoline, which is an antiserotonergic agent, does not improve OCD symptoms because it is a 5-HT1B/D antagonist, meaning that it may increase serotonin levels in certain areas of the brain and may worsen mood in some people .
Antagonism of 5-HT2A and 5-HT2C receptors has an anti-OCD effect since both of these receptors are highly sensitive in OCD (R). Fluoxetine, another serotonergic drug, may be useful in obsessive-compulsive disorder by desensitizing 5-HT2C (R).
Agomelatine inhibits/increases the release of norepinephrine and dopamine, especially in the frontal cortex, by inhibiting the 5-HT2C receptor, making it very useful in OCD (R, R).
Desensitization of serotonin receptors and decreased prolactin levels (associated with less 5-HT2C activation) are associated with improved symptoms (R). This alteration in response to endogenous serotonin may mediate the anti-obsessional effects of clomipramine (R).
Moreover, ondansetron's 5-HT3 antagonism may be useful in obsessive-compulsive disorder (R).
Vitamins and minerals
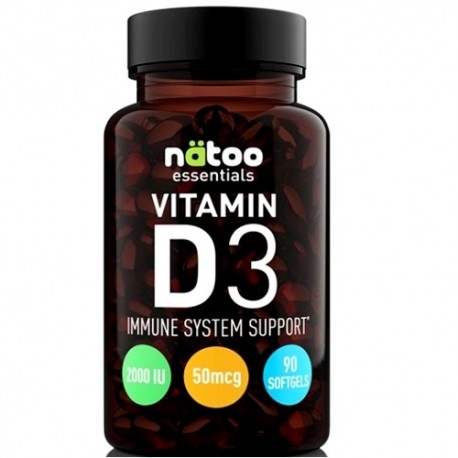
Vitamin D
Vitamin D levels are negatively correlated with symptom severity in patients with OCD (R).
People with OCD tend to have low vitamin D levels and are more likely to develop ADHD (R).
Vitamin D reduces hair pulling in OCD (trichotillomania) (R).
Vitamin D:
- Increases tyrosine and tryptophan hydroxylase, which can lead to increased levels of dopamine and serotonin.
- Has an antioxidant effect and inhibits inducible nitric oxide synthase, which has neuroprotective properties similar to agmatine.
Zinc, selenium, iron and magnesium
Some people with OCD have been found to have low levels of zinc, selenium, iron and magnesium. In a randomized, placebo-controlled clinical trial, one group received fluoxetine plus zinc and the other group received fluoxetine plus placebo for 8 weeks. This study showed that the zinc group had greater improvement compared to the placebo group (R).
Magnesium and OCD:
The introduction of magnesium reduces anxiety, panic and phobias, improves the state of attention deficit and sleep disorders. We believe that magnesium acts mainly by:
a) reducing the presynaptic release of glutamate;
b) decreased activity of the NMDA receptor due to competition with calcium in calcium channels associated with the NMDA receptor;
c) positive allosteric modulatory action at the level of some metabotropic presynaptic glutamate receptors, reducing presynaptic release of glutamate and stimulating release of GABA;
d) decrease in the release of catecholamines due to the direct presynaptic effect under the influence of some factors, including calcium.
Link
Folic acid and B12
According to this study, patients with OCD tend to be more likely to have low folic acid and B12 levels with elevated homocysteine, which correlates significantly with symptom severity (R).
Nitric Oxide
Nitric Oxide modulates neurotransmitters involved in OCD, and OCD patients have higher plasma nitrate levels, and OCD medications reduce nitric oxide (R) levels. Agmatine is effective in improving compulsive behavior in mice, which appears to be related to brain nitric oxide (R).
> Find out more here about nitric oxide and how to lower it (coming soon)
Healthy Supplements
- Amantadine (100mg) (R).
- Memantine (5-20mg) (R).
- NAC (500mg-2g per day) (R).
- Caffeine (300 mg) (R)
- pro-opioids (which may help reduce anxiety) (R) such as tianeptine (R), selank (R), agmatine (makes other opioids more effective), gluten , dairy products, etc.
- Saffron . "Our results indicate that saffron (30 mg) is as effective as fluvoxamine in treating patients with mild to moderate obsessive-compulsive disorder" (R).

- Minocycline . Minocycline is a fat-soluble antibiotic that can cross the blood-brain barrier. In the brain, it has neuroprotective and neurogenic properties in amyotrophic lateral sclerosis and Parkinson's disease. Minocycline reduces levels of pro-inflammatory agents, including nitric oxide, tumor necrosis factor-α, and interleukin-1β, and reduces glutamate-induced neurotoxicity. Minocycline has a therapeutic effect on neurodegenerative diseases and this can be achieved by blocking glutamate-mediated excitotoxicity (R).
It can be useful not only because it reduces inflammation, but also because it is an antibiotic. Early onset of sudden obsessive-compulsive disorder preceded by streptococcus. The infection was known as PANDAS (Childhood Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections) (R). - Myo-inositol . 18 g/day appears to be helpful in obsessive compulsive disorder (R).
- Glycine (60g, but this dose caused a high dropout rate due to nausea and vomiting (R)).
- Milk Thistle . Results from a single randomized controlled trial (n=35) of milk thistle for the treatment of obsessive-compulsive disorder showed no significant difference in treatment effects between milk thistle (600 mg/day) and fluoxetine . Milk thistle has been shown to have similar effects to fluoxetine in OCD symptoms, and its positive effect begins in the fifth week without serious side effects " (P).
- Valerian extract at 765 mg/day is useful in obsessive-compulsive disorder by activating the GABA (R) system.
- Ashwagandha 120 mg/day (crude extract) (R).
- Curcumin . “ After oral curcumin for 35 days, compulsive checking and ritualistic behaviors were significantly reduced, and quinpyrol-induced aggravations were reversed. These effects of curcumin were comparable to paroxetine " (R).
- Borage extract (500 mg) (R).
- Vitamin B1 . It helps against the anxious part of OCD. Doses of 250 mg/day (thiamine hydrochloride) (R) are commonly used. You can always try sulbutiamine, benfotiamine, or allithiamin, which can be more effective than regular thiamine.
- Psilocybin * (R).
- Uridine . There is no scientific reference to this drug, but there is a lot of anecdotal evidence that it helps with obsessive-compulsive disorder. This is most likely due to the fact that it increases dopamine and increases the number of dopamine receptors, which are reduced in obsessive-compulsive disorder (R, R).
- Kundalini Yoga (R). Not a supplement, but it can be dosed as a supplement if you feel comfortable thinking that way. And this applies not only to kundalini yoga, but also to other styles of yoga or meditation, because it is about calming the mind, deep breathing and reducing overall stress.
Continued discussion of this material on the English-language forum: here
* Psilocycin is on the list of prohibited substances in the Russian Federation.
Categories
Recent records
clinical picture and treatment methods
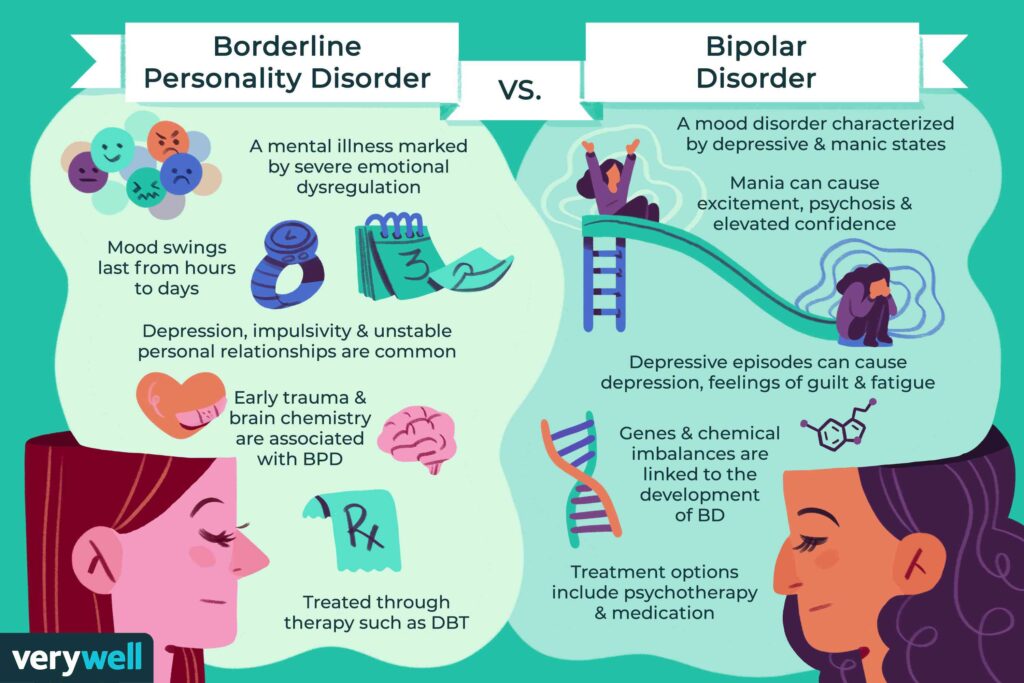
Until recently, obsessive-compulsive disorder (OCD) was considered one of the varieties of anxiety disorders that are combined into a single etymological group based on a common symptom for them - a high level of anxiety in the patient. However, although OCD is often accompanied by anxiety, it cannot be said to be a factor in the development of the disease. Therefore, the latest version of the DSM-V Diagnostic Guidelines for Mental Illness classifies OCD as a special condition that is not included in the group of anxiety disorders. This means that the anxiety that accompanies OCD in some cases is not the core of the disease, although it remains one of its characteristic symptoms.
What then is OCD, and how has the approach to treating the disease changed?
Types of obsessive-compulsive disorder and differences in their clinical presentation
It should be noted that OCD is initially a heterogeneous disease: the obsessions that make up its clinical picture can manifest themselves both in the thoughts and in the actions of the patient. In one case, doubts attacking the patient's consciousness force him to perform repetitive actions (for example, constantly double-checking whether the door is locked, whether electrical appliances are turned off, etc.), which are of a ritual nature and are called " compulsions ". In the other, the patient is haunted by various obsessive memories, visual images and representations, which are involuntary fantasies, fears about the unfavorable development of certain events. These representations are by no means hallucinations, but have a strong effect on the daily life of the OCD sufferer, taking up the lion's share of his attention, mental activity, and resulting vitality. Burdened with obsessive thoughts, a person is not able to concentrate on daily activities, freely surrender to his hobbies or communicate with friends.
In one case, doubts attacking the patient's consciousness force him to perform repetitive actions (for example, constantly double-checking whether the door is locked, whether electrical appliances are turned off, etc.), which are of a ritual nature and are called " compulsions ". In the other, the patient is haunted by various obsessive memories, visual images and representations, which are involuntary fantasies, fears about the unfavorable development of certain events. These representations are by no means hallucinations, but have a strong effect on the daily life of the OCD sufferer, taking up the lion's share of his attention, mental activity, and resulting vitality. Burdened with obsessive thoughts, a person is not able to concentrate on daily activities, freely surrender to his hobbies or communicate with friends.
Modern psychiatric science is trying in many ways to explain the phenomenon of the development of OCD.
Ultimately, his personal and professional life suffers, the person seeks self-isolation, which brings only temporary and insignificant relief, without freeing the OCD patient from obsessions.
This development inevitably contributes to the emergence of anxiety and depressive conditions that complicate the clinical picture of OCD.
Practice shows that, despite the long course of the disease (the vast majority of OCD sufferers seek professional help only a few years after the first episodes), there are proven treatment methods that in most cases allow patients to return to a full life, or at least teach to resist the paralyzing effect of obsessions.
Causes of OCD
Modern psychiatric science is trying in many ways to explain the phenomenon of the development of OCD. How is the mechanism of obsessions formed, what is it based on: neurological or psychological premises? And how do logical and emotional relationships intertwine in this or that case? Some of these questions are still the subject of debate. And the development and course of OCD is trying to explain several theoretical models at once, starting with the theory of information integration, which separates the concepts of actual and emotional memory and explains which parts of the brain are involved in the processing of information entering it, and ending with neuroanatomical hypotheses.
The most effective way to treat the type of obsessional neurosis in which compulsive actions dominate is the method of exposure.
However, none of these theoretical models has been supported by applied research data. Therefore, to insist on any of the theories of the development of OCD, alas, is not possible. And because it is ineffective to treat a suspected but unidentified cause, OCD therapy focuses primarily on the symptoms of the disease. After all, they complicate the daily life of the patient.
See also
Myths about diagnosing mental illness
Treatment options for obsessive-compulsive disorder
After all the uncertainties about the occurrence of obsessional neurosis, two approaches are clearly distinguished in its treatment, one of which is successfully used to eliminate compulsive actions, and the other to combat obsessive thoughts.
The most effective treatment for that type of obsessional neurosis in which compulsive acts dominate is exposure method . Its essence lies in the fact that the OCD patient consciously intensifies his obsessive reactions, bringing them almost to the point of absurdity. This gives him the opportunity to face the manifestation of irrational anxiety more closely and, thus, reduce its intensity. After that, it will be much easier for the psychotherapist to influence the original component of OCD, obsessive thoughts and urges.
However, the exposure method is less effective when it comes to the type of disease in which compulsions are practically not observed, and the leading role is played by obsessive ideas, images and fears. In this case, therapy focuses on the interaction of logical and emotional connections in the patient's life, teaches to trace and share them among themselves. This type of OCD is more difficult to treat. The task of therapy in this case will be to change the established way of thinking, the correlation between the logic of thinking and its emotional content.
The stress and depression that accompanies OCD makes it difficult for the patient to focus on dealing with the underlying thoughts and feelings.
As a rule, OCD patients are people with a high level of intelligence, and everything is in order with logic. The trap of the disease is that, relying on obvious logic, OCD patients ignore the emotional component of their disorder. Just as a person who is rapidly gaining weight does not notice changes in his own appearance from day to day, an OCD patient does not notice changes in the causal relationships that are formed at the level of his logical and emotional reactions. That is why his fears and doubts seem to him groundless, but he is not able to get rid of them by an effort of will.
Medication for OCD
Medications in the treatment of OCD are used solely to address psychological symptoms that interfere with cognitive behavioral therapy.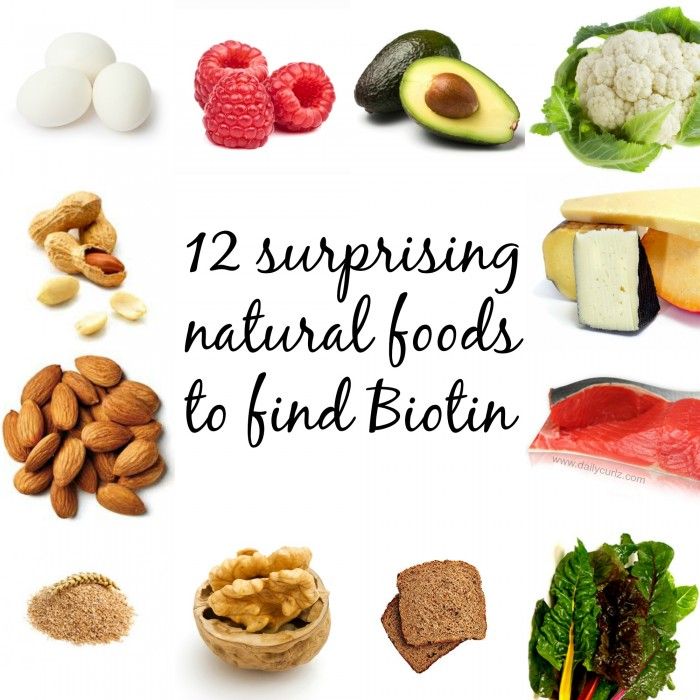 The stress and depression that accompanies OCD makes it difficult for the patient to focus on dealing with the underlying thoughts and feelings. Therefore, OCD patients are prescribed sedatives, antidepressants, and drugs known as serotonin reuptake inhibitors.
The stress and depression that accompanies OCD makes it difficult for the patient to focus on dealing with the underlying thoughts and feelings. Therefore, OCD patients are prescribed sedatives, antidepressants, and drugs known as serotonin reuptake inhibitors.
See also
First aid for anxiety attacks
Serotonin is one of the enzymes that is produced in the brain. It is the so-called neurotransmitter - a substance through which information is transmitted at the cellular level. Studies show that psychiatric and neurological disorders are often accompanied by sharp fluctuations in serotonin levels - and these fluctuations are especially pronounced in OCD.
By themselves, medications are a crude tool in the treatment of any mental disorder, but when used correctly, they provide the necessary support for psychotherapy.
Despite the optimistic treatment forecasts, obsessive-compulsive disorder is a dangerous disease that subjugates almost the entire life of the patient.