Mild eating disorder symptoms
Types, Causes, Treatment, and Recovery
Although the term “eating” is in the name, eating disorders are about more than food. They’re complex mental health conditions that often require the intervention of medical and psychological experts to alter their course.
These disorders are described in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) (1).
In the United States alone, an estimated 28 million Americans have or have had an eating disorder at some point in their life (2).
This article describes six of the most common types of eating disorders and their symptoms.
Eating disorders are a range of psychological conditions that cause unhealthy eating habits to develop. They might start with an obsession with food, body weight, or body shape (3).
In severe cases, eating disorders can cause serious health consequences and may even result in death if left untreated. In fact, eating disorders are among the deadliest mental illnesses, second to opioid overdose (4).
People with eating disorders can have a variety of symptoms. Common symptoms include severe restriction of food, food binges, and purging behaviors like vomiting or overexercising.
Although eating disorders can affect people of any gender at any life stage, they’re increasingly common in men and gender nonconforming people. These populations often seek treatment at lower rates or may not report their eating disorder symptoms at all (5, 6).
Different types of eating disorders have different symptoms, but each condition involves an extreme focus on issues related to food and eating, and some involve an extreme focus on weight.
This preoccupation with food and weight may make it hard to focus on other aspects of life (3).
Mental and behavioral signs may include (7):
- dramatic weight loss
- concern about eating in public
- preoccupation with weight, food, calories, fat grams, or dieting
- complaints of constipation, cold intolerance, abdominal pain, lethargy, or excess energy
- excuses to avoid mealtime
- intense fear of weight gain or being “fat”
- dressing in layers to hide weight loss or stay warm
- severely limiting and restricting the amount and types of food consumed
- refusing to eat certain foods
- denying feeling hungry
- expressing a need to “burn off” calories
- repeatedly weighing oneself
- patterns of binge eating and purging
- developing rituals around food
- excessively exercising
- cooking meals for others without eating
- missing menstrual periods (in people who would typically menstruate)
Physical signs may include (7):
- stomach cramps and other gastrointestinal symptoms
- difficulty concentrating
- atypical lab test results (anemia, low thyroid levels, low hormone levels, low potassium, low blood cell counts, slow heart rate)
- dizziness
- fainting
- feeling cold all the time
- sleep irregularities
- menstrual irregularities
- calluses across the tops of the finger joints (a sign of inducing vomiting)
- dry skin
- dry, thin nails
- thinning hair
- muscle weakness
- poor wound healing
- poor immune system function
Experts believe that a variety of factors may contribute to eating disorders.
One of these is genetics. People who have a sibling or parent with an eating disorder seem to be at an increased risk of developing one (3).
Personality traits are another factor. In particular, neuroticism, perfectionism, and impulsivity are three personality traits often linked to a higher risk of developing an eating disorder, according to a 2015 research review (8).
Other potential causes include perceived pressures to be thin, cultural preferences for thinness, and exposure to media promoting these ideals (8).
More recently, experts have proposed that differences in brain structure and biology may also play a role in the development of eating disorders. In particular, levels of the brain messaging chemicals serotonin and dopamine may be factors (9).
However, more studies are needed before strong conclusions can be made.
Eating disorders are a group of related conditions involving extreme food and weight issues, but each disorder has unique symptoms and diagnosis criteria.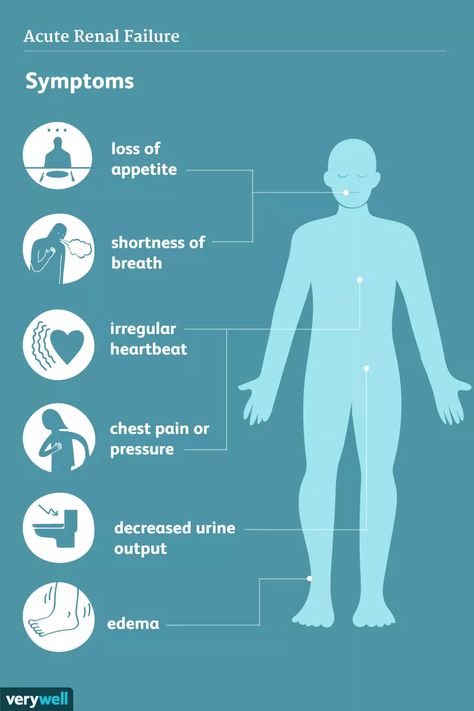 Here are six of the most common eating disorders and their symptoms.
Here are six of the most common eating disorders and their symptoms.
Anorexia nervosa is likely the most well-known eating disorder.
It generally develops during adolescence or young adulthood and tends to affect more women than men (10).
People with anorexia generally view themselves as overweight, even if they’re dangerously underweight. They tend to constantly monitor their weight, avoid eating certain types of foods, and severely restrict their calorie intake.
Common symptoms of anorexia nervosa include (1):
- very restricted eating patterns
- intense fear of gaining weight or persistent behaviors to avoid gaining weight, despite being underweight
- a relentless pursuit of thinness and unwillingness to maintain a healthy weight
- a heavy influence of body weight or perceived body shape on self-esteem
- a distorted body image, including denial of being seriously underweight
However, it’s important to note that weight should not be the major focus of diagnosing someone with anorexia.
Using body mass index as a factor in diagnosis is outdated because people who are categorized as “normal” or “overweight” can have the same risks.
In atypical anorexia, for example, a person may meet the criteria for anorexia but not be underweight despite significant weight loss (7).
Obsessive-compulsive symptoms are also often present. For instance, many people with anorexia are preoccupied with constant thoughts about food, and some may obsessively collect recipes or hoard food.
They may also have difficulty eating in public and exhibit a strong desire to control their environment, limiting their ability to be spontaneous (3).
Anorexia is officially categorized into two subtypes — the restricting type and the binge eating and purging type (1).
Individuals with the restricting type lose weight solely through dieting, fasting, or excessive exercise.
Individuals with the binge eating and purging type may binge on large amounts of food or eat very little. In both cases, after they eat, they purge using activities such as vomiting, taking laxatives or diuretics, or exercising excessively.
In both cases, after they eat, they purge using activities such as vomiting, taking laxatives or diuretics, or exercising excessively.
Anorexia can be very damaging to the body. Over time, individuals living with it may experience thinning of their bones, infertility, and brittle hair and nails.
In severe cases, anorexia can result in heart, brain, or multi-organ failure and death.
Bulimia nervosa is another well-known eating disorder.
Like anorexia, bulimia tends to develop during adolescence and early adulthood and appears to be less common among men than women (10).
People with bulimia frequently eat unusually large amounts of food in a specific period of time.
Each binge eating episode usually continues until the person becomes painfully full. During a binge, the person usually feels that they cannot stop eating or control how much they are eating.
Binges can happen with any type of food but most commonly occur with foods the individual would usually avoid.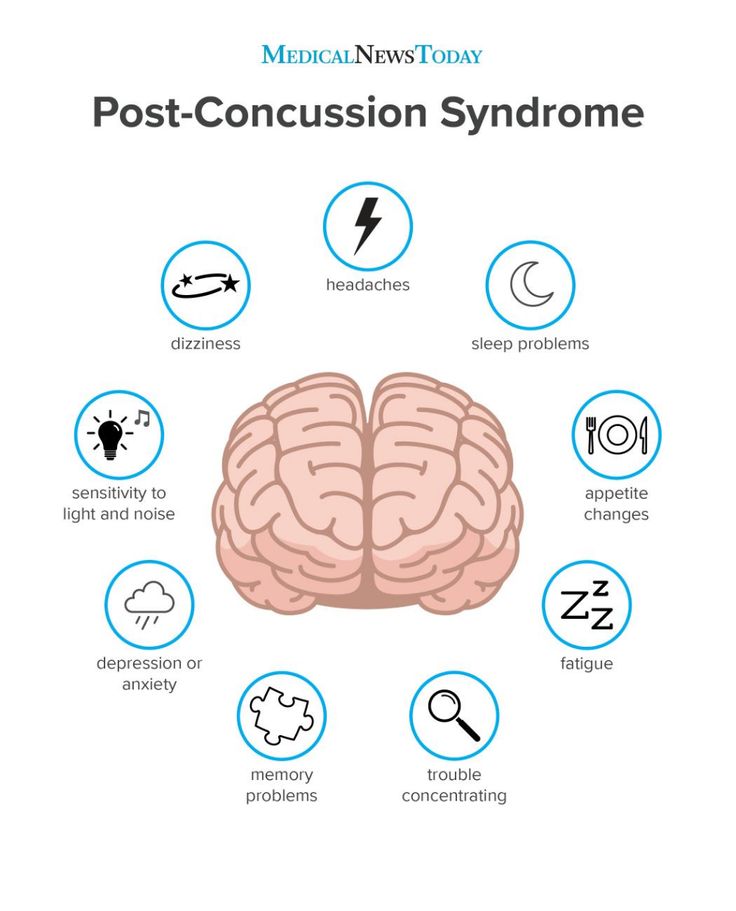
Individuals with bulimia then attempt to purge to compensate for the calories consumed and to relieve gut discomfort.
Common purging behaviors include forced vomiting, fasting, laxatives, diuretics, enemas, and excessive exercise.
Symptoms may appear very similar to those of the binge eating or purging subtypes of anorexia nervosa. However, individuals with bulimia usually maintain a relatively typical weight rather than losing a large amount of weight.
Common symptoms of bulimia nervosa include (1):
- recurrent episodes of binge eating with a feeling of lack of control
- recurrent episodes of inappropriate purging behaviors to prevent weight gain
- self-esteem overly influenced by body shape and weight
- a fear of gaining weight, despite having a typical weight
Side effects of bulimia may include an inflamed and sore throat, swollen salivary glands, worn tooth enamel, tooth decay, acid reflux, irritation of the gut, severe dehydration, and hormonal disturbances (11).
In severe cases, bulimia can also create an imbalance in levels of electrolytes, such as sodium, potassium, and calcium. This can cause a stroke or heart attack.
Binge eating disorder is the most prevalent form of eating disorder and one of the most common chronic illnesses among adolescents (12).
It typically begins during adolescence and early adulthood, although it can develop later on.
Individuals with this disorder have symptoms similar to those of bulimia or the binge eating subtype of anorexia.
For instance, they typically eat unusually large amounts of food in relatively short periods of time and feel a lack of control during binges.
People with binge eating disorder do not restrict calories or use purging behaviors, such as vomiting or excessive exercise, to compensate for their binges (12).
Common symptoms of binge eating disorder include (11):
- eating large amounts of food rapidly, in secret, and until uncomfortably full, despite not feeling hungry
- feeling a lack of control during episodes of binge eating
- feelings of distress, such as shame, disgust, or guilt, when thinking about the binge eating behavior
- no use of purging behaviors, such as calorie restriction, vomiting, excessive exercise, or laxative or diuretic use, to compensate for the binge eating
People with binge eating disorder often consume an excessive amount of food and may not make nutritious food choices.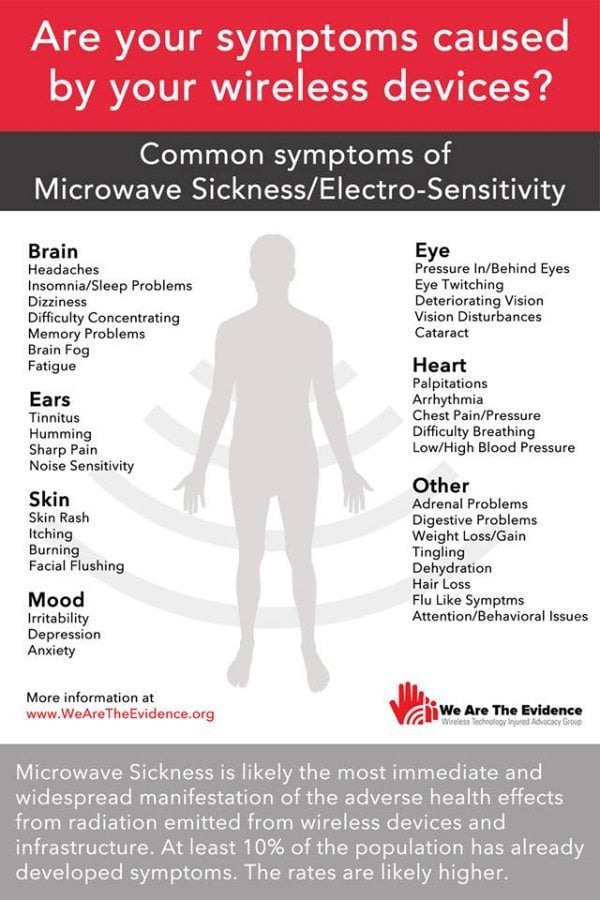 This may increase their risk of medical complications such as heart disease, stroke, and type 2 diabetes (13).
This may increase their risk of medical complications such as heart disease, stroke, and type 2 diabetes (13).
Pica is an eating disorder that involves eating things that are not considered food and that do not provide nutritional value (14).
Individuals with pica crave non-food substances such as ice, dirt, soil, chalk, soap, paper, hair, cloth, wool, pebbles, laundry detergent, or cornstarch (11).
Pica can occur in adults, children, and adolescents.
It is most frequently seen in individuals with conditions that affect daily functioning, including intellectual disabilities, developmental conditions such as autism spectrum disorder, and mental health conditions such as schizophrenia (14).
Individuals with pica may be at an increased risk of poisoning, infections, gut injuries, and nutritional deficiencies. Depending on the substances ingested, pica may be fatal.
However, for the condition to be considered pica, the eating of non-food substances must not be a typical part of someone’s culture or religion.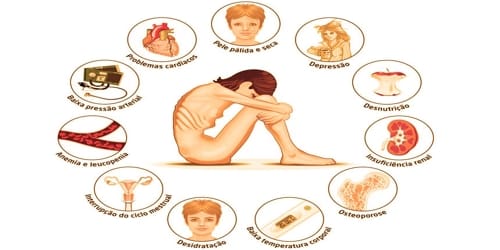 In addition, it must not be considered a socially acceptable practice by a person’s peers.
In addition, it must not be considered a socially acceptable practice by a person’s peers.
Rumination disorder is another newly recognized eating disorder.
It describes a condition in which a person regurgitates food they have previously chewed and swallowed, re-chews it, and then either re-swallows it or spits it out (15).
This rumination typically occurs within the first 30 minutes after a meal (16).
This disorder can develop during infancy, childhood, or adulthood. In infants, it tends to develop between 3 and 12 months of age and often disappears on its own. Children and adults with the condition usually require therapy to resolve it.
If not resolved in infants, rumination disorder can result in weight loss and severe malnutrition that can be fatal.
Adults with this disorder may restrict the amount of food they eat, especially in public. This may lead them to lose weight and become underweight (16).
Avoidant/restrictive food intake disorder (ARFID) is a new name for an old disorder.
The term has replaced the term “feeding disorder of infancy and early childhood,” a diagnosis previously reserved for children under age 7 (17).
Individuals with this disorder experience disturbed eating due to either a lack of interest in eating or a distaste for certain smells, tastes, colors, textures, or temperatures.
Common symptoms of ARFID include (11):
- avoidance or restriction of food intake that prevents the person from eating enough calories or nutrients
- eating habits that interfere with typical social functions, such as eating with others
- weight loss or poor development for age and height
- nutrient deficiencies or dependence on supplements or tube feeding
It’s important to note that ARFID goes beyond common behaviors such as picky eating in toddlers or lower food intake in older adults.
Moreover, it does not include the avoidance or restriction of foods due to lack of availability or religious or cultural practices.
In addition to the six eating disorders above, other less known or less common eating disorders also exist.
These include (18):
- Purging disorder. Individuals with purging disorder often use purging behaviors, such as vomiting, laxatives, diuretics, or excessive exercising, to control their weight or shape. However, they do not binge.
- Night eating syndrome. Individuals with this syndrome frequently eat excessively at night, often after awakening from sleep.
- Other specified feeding or eating disorder (OSFED). While it is not found in the DSM-5, this category includes any other conditions that have symptoms similar to those of an eating disorder but don’t fit any of the disorders above.
One disorder that may currently fall under OSFED is orthorexia. Although orthorexia is increasingly mentioned in the media and in scientific studies, the DSM does not yet recognize it as a separate eating disorder (19).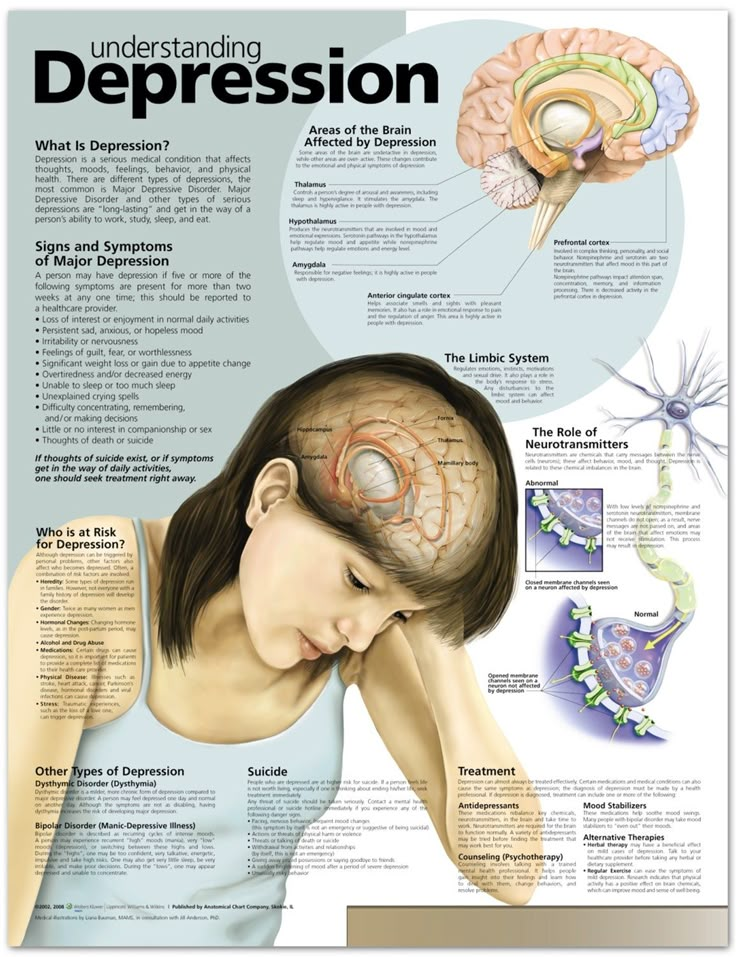
Individuals with orthorexia tend to have an obsessive focus on healthy eating to an extent that disrupts their daily lives. They may compulsively check ingredient lists and nutritional labels and obsessively follow “healthy lifestyle” accounts on social media.
Someone with this condition may eliminate entire food groups, fearing that they’re unhealthy. This can lead to malnutrition, severe weight loss, difficulty eating outside the home, and emotional distress.
Individuals with orthorexia are rarely focused on losing weight. Instead, their self-worth, identity, or satisfaction is dependent on how well they comply with their self-imposed diet rules (19).
If you have an eating disorder, identifying the condition and seeking treatment sooner will improve your chances of recovering. Being aware of the warning signs and symptoms can help you decide whether you need to seek help.
Not everyone will have every sign or symptom at once, but certain behaviors may signal a problem, such as (20):
- behaviors and attitudes that indicate that weight loss, dieting, and control over food are becoming primary concerns
- preoccupation with weight, food, calories, fats, grams, and dieting
- refusal to eat certain foods
- discomfort with eating around others
- food rituals (not allowing foods to touch, eating only particular food groups)
- skipping meals or eating only small portions
- frequent dieting or fad diets
- extreme concern with body size, shape, and appearance
- frequently checking in the mirror for perceived flaws in appearance
- extreme mood swings
If these symptoms resonate with you and you think you may have an eating disorder, it’s important to reach out to a medical professional for help.
Making the decision to start eating disorder recovery might feel scary or overwhelming, but seeking help from medical professionals, eating disorder recovery support groups, and your community can make recovery easier.
If you’re not sure where to start, you can contact the National Eating Disorders Association helpline for support, resources, and treatment options for yourself or someone you know.
To contact, call: (800) 931-2237
Monday–Thursday 11 a.m.–9 p.m. ET
Friday 11 a.m.–5 p.m. ET
Text: (800) 931-2237
Monday–Thursday 3 p.m.–6 p.m. ET
Friday 1 p.m.–5 p.m. ET
Eating disorder treatment plans are specifically tailored to each person and may include a combination of multiple therapies.
Treatment will usually involve talk therapy, as well as regular health checks with a physician (21).
It’s important to seek treatment early for eating disorders, as the risk of medical complications and suicide is high (11).
Treatment options include:
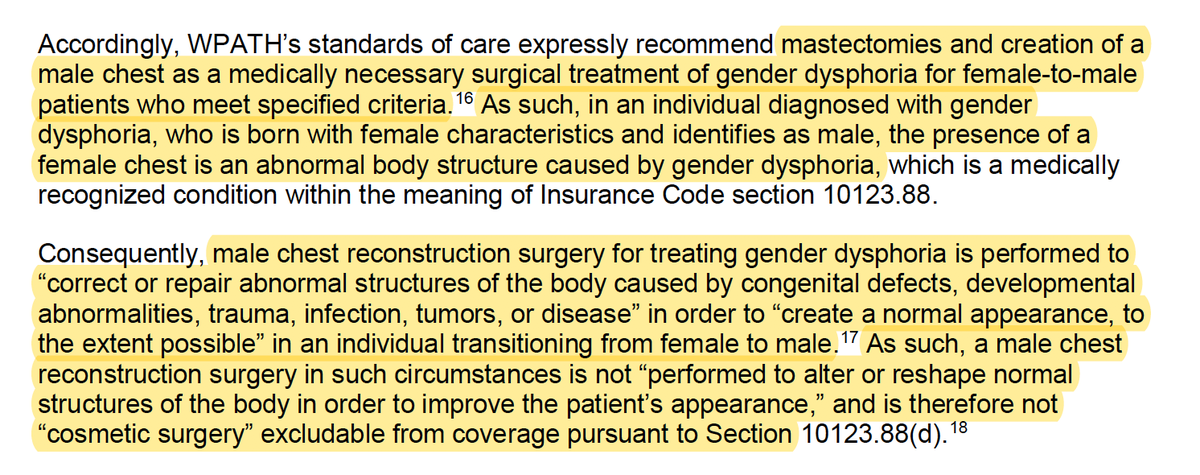
- Individual, group, or family psychotherapy. A type of psychotherapy called cognitive behavioral therapy (CBT) may be recommended to help reduce or eliminate disordered behavior such as binge eating, purging, and restricting. CBT involves learning how to recognize and change distorted or unhelpful thought patterns (11).
- Medications. A doctor may recommend treatment with medications such as antidepressants, antipsychotics, or mood stabilizers to help treat an eating disorder or other conditions that may occur at the same time, such as depression or anxiety (11).
- Nutritional counseling. This involves working with a dietitian to learn proper nutrition and eating habits and may also involve restoring or managing a person’s weight if they have experienced significant weight changes. Studies suggest that combining nutritional therapy with cognitive therapy may significantly improve treatment outcomes (22).

If you think someone in your life has an eating disorder, your best bet is to support and encourage them to seek help from a healthcare professional.
This can be extremely difficult for someone living with an eating disorder, but supporting them in other ways will help them feel cared for and encouraged in their recovery.
Recovering from an eating disorder can take a long time, and this person may have periods of relapsing into old behaviors, especially during times of stress. If you’re close to this person, it’s important to be there for them, and be patient, throughout their recovery (21).
Ways to support someone with an eating disorder include (21):
- Listening to them. Taking time to listen to their thoughts can help them feel heard, respected, and supported. Even if you don’t agree with what they say, it’s important that they know you’re there for them and that they have someone to confide in.
- Including them in activities.
 You can reach out and invite them to activities and social events or ask if they want to hang out one-on-one. Even if they do not want to be social, it’s important to check in and invite them to help them feel valued and less alone.
You can reach out and invite them to activities and social events or ask if they want to hang out one-on-one. Even if they do not want to be social, it’s important to check in and invite them to help them feel valued and less alone. - Trying to build their self-esteem. Make sure they know that they are valued and appreciated, especially for nonphysical reasons. Remind them why you are their friend and why they are valued.
The categories above are meant to provide a better understanding of the most common eating disorders and dispel myths about them.
Eating disorders are mental health conditions that usually require treatment. They can also be damaging to the body if left untreated.
If you have an eating disorder or know someone who might have one, you can seek help from a healthcare professional who specializes in eating disorders.
You can book an appointment with an eating disorder specialist in your area using our Healthline FindCare tool.
Read this article in Spanish.
Signs and Symptoms | Eating Disorder Foundation.org
Below is a list of common signs and symptoms that may be present if a person is struggling with an eating disorder. This is not a diagnostic tool; the presence or absence of any signs or symptoms does not necessarily mean someone does or does not have an eating disorder. Because each eating disorder presents itself differently, the signs and symptoms are broken down by diagnosis.
Anorexia Nervosa
- Low body weight – may have dramatic weight loss
- Feels as though he or she is overweight, even when that is clearly not the case
- Denial of hunger
- Preoccupation with body weight and shape (frequent weighing and comments regarding weight and shape)
- Obsession with food and its nutrients (calories, fat, carbohydrates, etc.)
- Food rituals (cutting into very small pieces, excessive chewing, etc.)
- Excessive exercise and dieting
- Anxiety regarding weight, meal time, and social activities or gatherings
- Frequent fatigue and overall weakness
- Dry, thinning, or loss of hair
- Dry skin and brittle nails
- Frequently cold, wearing multiple layers to hide body or to stay warm
- Downy hair covering body, called lanugo
- Amenorrhea (loss of menstruation in women)
Bulimia Nervosa
- Frequent fluctuations in body weight
- Frequent episodes of bingeing (consuming large amounts of food) followed by purging (compensatory behaviors including self-induced vomiting, misuse of diuretics, laxatives, or enemas)
- Hiding food to eat in private
- Feeling of loss of control during binge episodes
- Feelings of shame and guilt when eating
- Preoccupied with body weight and shape
- Preoccupied with exercise and dieting
- Signs of purging include frequent trips to bathroom (especially after meals), swollen cheeks, cuts or scabs on knuckles and back of hands, discolored teeth and tooth decay
- Withdrawal from social activities and gatherings
Binge Eating Disorder
- Frequent episodes of bingeing (consuming large amounts of food)
- Feeling of loss of control during binge episodes
- Hiding food to eat in private
- Feelings of shame and guilt when eating
- Eating when not physically hungry
- Eating past the point of discomfort
- Eating alone
Diabulimia
- May have extreme weight loss
- Disordered eating behaviors including restriction or bingeing
- Secrecy around insulin administration
- Frequent episodes of hypoglycemia
- Nausea and vomiting
- Increase of thirst and urnination
- Diabetic ketoacidosis, DKA
- Yeast infection, bladder infection
- Liver disease
If you think you or someone you know is struggling with an eating disorder, express your concern and seek professional help immediately.
Eating Disorders Treatment - Sheba Medical Center
Eating Disorders Treatment
Eating disorders treatment is carried out in a specialized eating disorders treatment unit, which is part of the psychiatric department of the Sheba Medical Center Rehabilitation Hospital. Our center of excellence is the only one of its kind in Israel. Experienced teams of psychiatrists, psychologists, social workers, nutritionists, psychotherapists, nurses and physical education instructors work here. We provide comprehensive medical advice, laboratory testing, state-of-the-art imaging, intensive care and comprehensive follow-up care for a range of eating disorders.
Integrative care is provided in four areas: full hospitalization, one-day hospitalization, outpatient care and information resource center. The patient can start treatment for an eating disorder in one of these units and move to another if necessary. Even after moving to another unit, the patient will continue to be served by the same medical staff, providing continuous and personalized treatment.
Why is it important to treat eating disorders?
Eating disorders are complex mental disorders characterized by abnormal eating habits that impair a person's physical, psychological and social status. If such disorders are pronounced and last a long time, then they can be life-threatening. Since an eating disorder can harm any system in the body, it is imperative to see a specialist as soon as possible.
Different types of eating disorders affect health in different ways, but they all increase the risk of death and significantly reduce the quality of life.
What types of eating disorders are treated at Sheba?
Eating Disorders Physicians treat the following diseases:
Anorexia Nervosa
Anorexia is characterized by extreme low weight, a morbid fear of obesity, and a distorted perception of body weight. Anorexics will do anything to keep from gaining weight, even if it ruins their lives. This disease is most common among adolescents and occurs more often in girls than in boys.
This disease is most common among adolescents and occurs more often in girls than in boys.
As a rule, the main symptom of the disease is severe restriction of the amount of calories consumed. This can be done with enemas, vomiting after meals, laxatives or diuretics. Some patients resort to excessive physical activity. However, regardless of the degree of exhaustion, a person will continue to be afraid of gaining weight.
Other physical manifestations and symptoms of anorexia include extreme thinness, fatigue, insomnia, dizziness, fainting, abnormal blood counts, bluish discoloration of the skin of the fingers, hair loss, cessation of menstruation, dry skin, arrhythmias, low blood pressure, dehydration, and limb edema.
Emotional and behavioral signs - refusal to eat or regular skipping meals, preoccupation with the process of cooking (without eating it), following strict rules when eating, eating only alone, constantly looking for imaginary physical defects in the mirror, wearing bulky clothes to hide your body, irritability and isolation.
Anorexia nervosa has a higher risk of death than any other psychiatric disorder. In addition, this disease increases the risk of developing heart, kidney and liver failure, osteoporosis, anemia, hypoglycemia, gastrointestinal diseases, amenorrhea (absence of menstruation in women), infertility, low testosterone levels (in men), electrolyte imbalance and suicide.
Anorexia is not inherently related to food. It is a life-threatening way of coping with emotional disturbances that equates thinness with perfection.
Bulimia Nervosa
Bulimia is a potentially life-threatening eating disorder characterized by recurrent bouts of binge eating followed by stomach emptying to get rid of excess calories. Bulimia is associated with low self-esteem, it can develop in people obsessed with proper weight.
As a rule, patients with bulimia cannot control themselves when eating. To avoid gaining weight, they use various methods such as enemas, inducing vomiting, taking laxatives or diuretics, and weight loss products.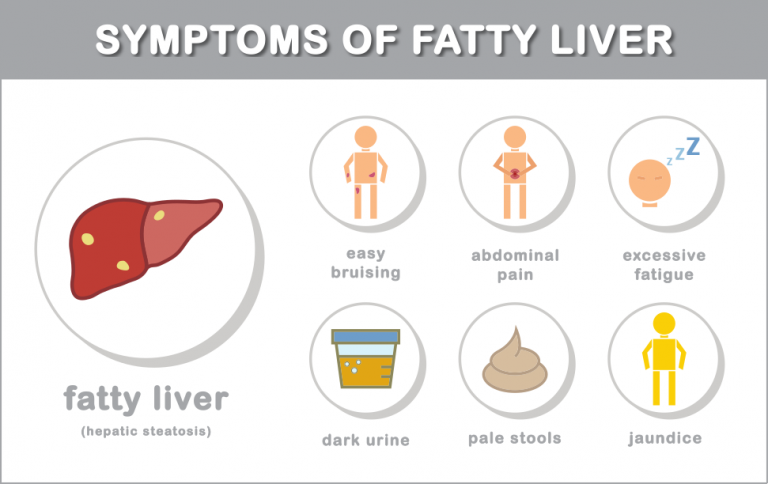
Signs of bulimia include persistent concern about one's own weight, having a distorted or negative body image, not eating in public places, going to the bathroom immediately after eating (or staying there for a long period of time), sores or calluses on the skin of the hands or joints, swelling of the hands and feet, as well as inflammation in the face due to enlarged glands.
Bulimia increases the risk of dehydration and electrolyte imbalance, heart and kidney failure, digestive problems, peptic ulcers (stomach and small intestine), pancreatitis, dental caries, inflammation and rupture of the esophagus, acid reflux, arrhythmia, and ruptured blood vessels eye.
Psychogenic and compulsive overeating
Psychogenic and compulsive overeating consists in eating extremely large portions of food, accompanied by a feeling of inability to stop. Unlike ordinary overeating, these disorders are regular excessive meals, in the absence of any control. Unlike anorexia and bulimia, people with these disorders do not seek to get rid of excess calories through vomiting or exercise.
Unlike anorexia and bulimia, people with these disorders do not seek to get rid of excess calories through vomiting or exercise.
Most patients with these disorders are overweight or obese. As a rule, they consume a large amount of food in a short period of time, often in secret from others, without experiencing hunger. With psychogenic or compulsive overeating, a person is ashamed of himself, he may be disgusted by this habit and try to stop. However, the desire to satiate is very strong and almost impossible to overcome without proper treatment.
These eating disorders are associated with a high risk of gastric rupture, obesity, obstructive sleep apnea, hypertension, type 2 diabetes, cardiovascular disease, depression, nervousness, and other mood disorders.
Morbid obesity
This disease has become one of the most common eating disorders in children and adults. As a rule, its cause is a combination of several factors and a number of environmental, hormonal, metabolic, genetic, physiological, psychological and behavioral components. There is growing evidence that morbid obesity is not related to a problem of self-control or lack of willpower, but is a complex disorder related to energy metabolism and appetite regulation.
There is growing evidence that morbid obesity is not related to a problem of self-control or lack of willpower, but is a complex disorder related to energy metabolism and appetite regulation.
Read about the treatment of obesity in Israel
This disease has become one of the most common eating disorders in children and adults. It is typically caused by a combination of several factors and a range of environmental, hormonal, metabolic, genetic, physiological, psychological and behavioral components. There is growing evidence that morbid obesity is not related to a problem of self-control or lack of willpower, but is a complex disorder related to energy metabolism and appetite regulation.
Diagnosis is usually made by determining the body mass index (BMI), which is calculated as the ratio of weight and height. If a person has a BMI over 40 and is 50 kg overweight, or a BMI over 35 and suffers from a disease caused by obesity (such as type 2 diabetes or hypertension), then a diagnosis of morbid obesity is made.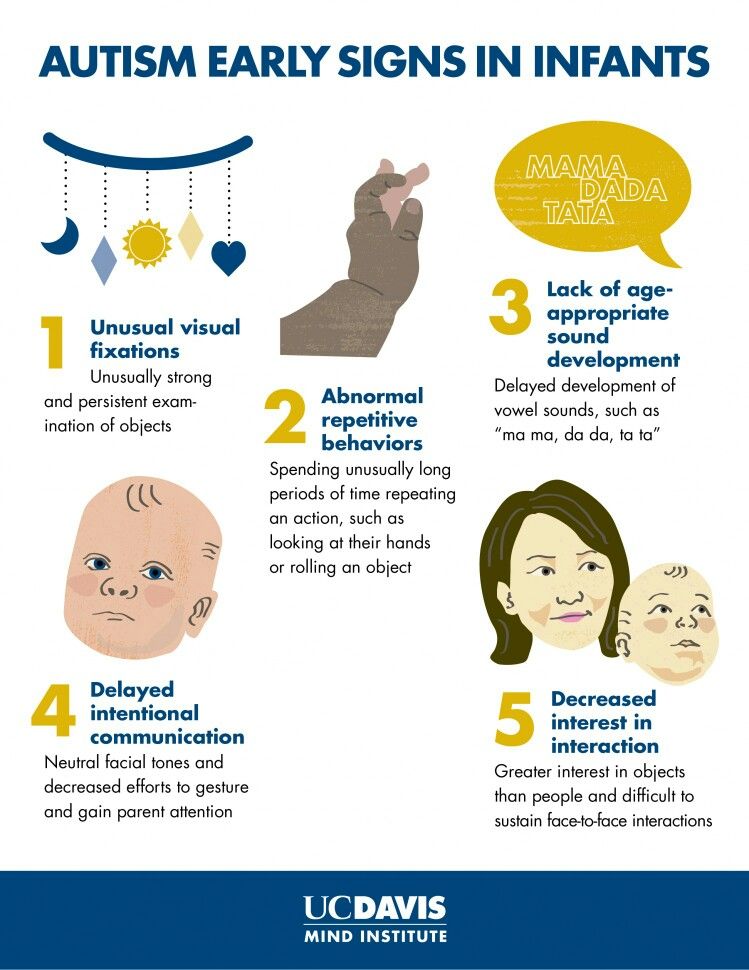
Morbid obesity impairs basic bodily functions such as walking and breathing, and increases the risk of developing hypertension, hypercholesterolemia, type 2 diabetes, cardiovascular disease, stroke, gallbladder disease, body aches, obstructive sleep apnea syndrome , some types of cancer, clinical depression and other mental disorders.
What types of treatment for eating disorders do we offer?
Total hospitalization
If the patient is in a critical or rapidly deteriorating condition, he needs intensive treatment in a hospital setting. The main goal of inpatient treatment is to stabilize and strengthen the patient's physical and mental health for a quick return to daily life.
The duration of hospitalization varies depending on the needs of the patient. The average term is 2-3 months. Treatment is carried out according to a strict schedule, which includes the mandatory attendance of group meetings and individual sessions of psychotherapy. The diet is specially developed by a nutritionist for each patient, and meals are taken under strict supervision in the common dining room. The physical activity program includes daily evening walks. After the condition improves, the patient is allowed to rest at home. In addition, there is the possibility of holding family meetings.
The diet is specially developed by a nutritionist for each patient, and meals are taken under strict supervision in the common dining room. The physical activity program includes daily evening walks. After the condition improves, the patient is allowed to rest at home. In addition, there is the possibility of holding family meetings.
Depending on the progress, the doctors may recommend a transfer to a day hospital with follow-up at the place of residence. This gradual, step-by-step approach allows each patient to cope with the disease at their own pace. As part of post-discharge follow-up, we hold regular appointments at the outpatient clinic.
When undergoing treatment for an eating disorder, the path to complete recovery can be long and interspersed with relapses of the disease. In such cases, repeated hospitalization is sometimes recommended.
Outpatient care
Outpatient clinic services:
- Evaluation of the patient's condition to select the most appropriate treatment program.

- Comprehensive monitoring of patients after discharge and during outpatient treatment.
- Re-evaluate if relapsed or as needed.
As part of our outpatient treatment, we provide individual and group psychotherapy sessions, as well as behavioral, cognitive and psychodynamic therapies. An integral part of any outpatient program are consultations with a nutritionist. In addition, we strive to ensure that every patient can attend a support group after discharge.
Meet our Head of Department
Dr. Eitan Gur
Head of Eating Disorders Therapy
Dr. Gur graduated from the Hadassah School of Medicine at the Hebrew University of Jerusalem. He specialized in the treatment of eating disorders at the Hadassah Medical Center. Dr. Gur runs the only medical facility in Israel that provides full inpatient care to patients over the age of 18 with eating disorders.
REQUEST A CONSULTATION
Sheba Clinic provides state-of-the-art personalized medical services to patients from all over the world. Sheba is the largest hospital in the region, which provides comprehensive medical care and an individual approach to each patient.
Sheba is the largest hospital in the region, which provides comprehensive medical care and an individual approach to each patient.
Request a consultation and Sheba International Patients will contact you shortly:
New patients Current and returning patients Refer a patient
Eating disorders | Tervisliku toitumise informatsioon
Eating disorders are psychiatric illnesses that damage a person's physical and mental health and overall quality of life - relationships, work and personal development suffer.
Eating disorders disrupt the connection with one's own body, resulting in highly problematic eating behavior. Weight and body shape are overemphasized, underweight is idealized, and various methods are used to lose weight or prevent weight gain.
Approximately 8% of women and 2% of men will develop an eating disorder during their lifetime. Eating disorders occur in any population, regardless of gender, age, ethnicity, or socioeconomic status. However, they are most common in girls and young women.
However, they are most common in girls and young women.
Eating disorders are a group of diseases that are distributed differently in different classifications. The most common eating disorders are anorexia ( anorexia nervosa ), bulimia ( bulimia nervosa ) and compulsive overeating ( binge-eating disorder ).
The term "eating disorder" is often erroneously used as a synonym for selective eating disorder, as both are associated with eating disorders. However, the reasons for them are different: an eating disorder is caused by a desire to control weight, while in a selective eating disorder, eating certain foods causes anxiety or fear.
Other eating disorders
Anorexia, bulimia and binge eating disorders are the three most common and well-known eating disorders. However, often not all of the symptoms of a person with an eating disorder correspond to one specific disorder. In such cases, these disorders are referred to as "atypical" or "other eating disorders". A common myth is that in such cases the course of the disease is milder and treatment is treated more lightly. However, this is erroneous, since the name of the disease indicates only its diagnostic criteria, and not the severity or course.
A common myth is that in such cases the course of the disease is milder and treatment is treated more lightly. However, this is erroneous, since the name of the disease indicates only its diagnostic criteria, and not the severity or course.
All eating disorders, no matter how they are called or classified, are dangerous conditions that impair quality of life and require treatment.
Causes of Eating Disorders
There is never one single cause of an eating disorder. These are complex diseases, in the development of which a combination of many factors plays an important role. Genetic, biological and environmental factors always play a role. Modern social representations, including the culture of diets and the cult of slimness, contribute to the development of psychological vulnerability, which can become a fertile environment for the formation of eating disorders. Probably for the same reasons, a higher incidence of eating disorders is observed in sports in which weight is of great importance, and among representatives of professions focused on appearance. However, it should be emphasized that browsing social networks or playing a certain sport does not contribute to the development of the disease. There are many factors involved in the development of the disease that are usually beyond the control of the individual. However, it is often more practical and even more important to identify the factors that support the disease, since changing them is associated with better treatment outcomes.
However, it should be emphasized that browsing social networks or playing a certain sport does not contribute to the development of the disease. There are many factors involved in the development of the disease that are usually beyond the control of the individual. However, it is often more practical and even more important to identify the factors that support the disease, since changing them is associated with better treatment outcomes.
Treatment Options for Eating Disorders
Eating disorders can be life-threatening illnesses with a long and chronic course; they have one of the highest mortality rates of any psychiatric illness. Treating eating disorders is often a lengthy and complex process. However, early intervention is paramount to achieve a good treatment outcome.
Diagnosis and treatment of an eating disorder usually begins with a family doctor. Family sisters can provide advice on healthy eating. Psychiatrists are specialists in the diagnosis and treatment of eating disorders as a psychiatric illness.