Can grief cause psychosis
Can Grief and Loss Lead to Mental Illness
Experiencing the loss of a loved one can be traumatic and truly heartbreaking. The mourning process can be confusing and you may feel that your life will never be the same.
Eventually most people are able to accept the loss and start living a normal life again. The journey to this point of acceptance is different for everyone and some people may take longer to get there than others. Along the way, most people will begin to feel the effects of grief on mental health, but some people will experience symptoms that are much more severe than others.
Grief is different for everyone, but most people would agree that dealing with loss can take a toll on your mental health. Feelings of sadness, anger, loneliness, and hopeless are all common emotions that people experience during the grieving process. These emotions can vary in severity, but for some people, they may be overwhelming.
Grief is typically an emotional rollercoaster, but sometimes this chronic grief can develop into a mental health disorder.
Some common symptoms of chronic grief include:
- Prolonged sadness on a daily basis
- Extreme focus on the loss
- Neglecting daily responsibilities because of depression
- No motivation to interact with people or attend social events
- Detachment from your friends and family
- Difficulty accepting the loss after ample time has passed
- Intense emotions such as anger and pain towards the loss
In some cases, grief may even lead to a state of depression. A longitudinal study found that 1 month after people were widowed, 40% of these people meet criteria for a major depression episode, but most researchers argue that this amount of time is not long enough to diagnose depression. Thankfully, this depression caused by grief decreased over time, and after one year, only 15% of this population met the criteria for major depression. 1
1
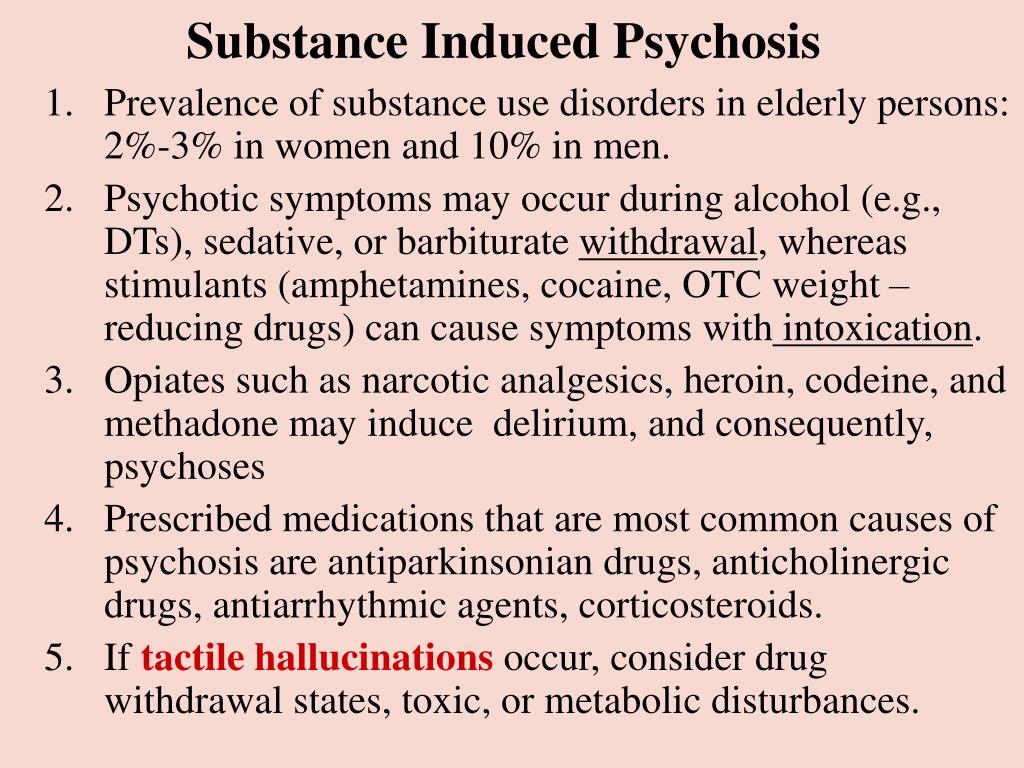
Depression isn’t the only connection between grief and mental illness. In rare cases, grief can cause psychosis or the development of psychotic symptoms. Research on the connection between bereavement and mental health disorders involving psychosis suggest that grief triggers the onset of these symptoms because of any underlying disorder, but research still needs to be done for a clearer answer.1
The mental effects of grief can negatively impact a person’s actions and behaviors as well. When people are struggling and neglect to get mental health or depression treatment, they may engage in dangerous or more risky behavior than normal. For some people, this may mean self-harm or suicidal actions. For other people, this may mean regularly turning to substances like drugs or illicit drugs to help them cope with their grief. Over time, this behavior can become habitual and an addiction may occur. At this point, these people should look for a dual diagnosis treatment center to address both problems as the same time.
While grief will impact your mental health in some way, typically, as time passes, an individual will be able to accept the loss and move on with their life. Someone who is dealing with chronic grief will experience increased pain over time and may develop a mental illness.
Grief is a natural part of the healing process, but when someone develops a mental illness because of it, this may happen for several reasons including:
- Underlying mental health disorder that is exacerbated by grief
- Genetic predisposition to mental illness
- Problems coping with grief in a healthy manner
- Substance abuse
- Brain changes that make it harder for some people to let go2
Everyone deals with grief and loss in their own way. Allowing yourself to take the time to grieve is important and accepting the loss of your loved one can come at different stages for different people.
Allowing yourself to take the time to grieve is important and accepting the loss of your loved one can come at different stages for different people.
Although it can be difficult to admit, if you are struggling to move past your grief, you should get professional help. Likewise, if you feel that your loved one has had an exceptionally difficult time grieving a loss, you should encourage them to go to a mental health facility for treatment.
At Banyan Mental Health in Boca, we help people regain control of their lives. For more information on how we may be able to help you or a loved one, call 888-280-4763.
Sources:
- Psychiatric Times - Bereavement-Related Depression
- Scientific American - Shades of Grief: When Does Mourning Become a Mental Illness?
Are Grief Hallucinations Common?
What grief does to your body isn’t yet fully understood. It may include hallucinations in some cases.![]() But they may have a purpose.
But they may have a purpose.
Everyone experiences and expresses grief differently. There’s certainly no right or wrong way to mourn a loss. In some cases, this may include seeing or feeling the presence of a departed loved one.
Although rare, bereavement hallucinations are possible when someone’s in a heightened state of emotional pain.
What are hallucinations?
Hallucinations are perceptions that are unique to you and that others can’t perceive at the same time. For example, seeing, hearing, smelling, touching, or tasting something without a stimulus.
A grief hallucination may involve seeing, feeling, or hearing someone you’ve recently lost.
Yes, you can experience hallucinations of a loved one during your grieving time.
You may hear their voice or feel their touch, for example, or you may see their presence in places you go.
Dr. Joseph Shrand, a psychiatrist in Dedham, Massachusetts, explains that hallucinations come in two general categories:
- enjoyable “egosyntonic”
- not enjoyable “egodystonic”
These terms come from psychoanalysis. Egosyntonic refers to experiences that are consistent with your idea of self and your needs, likes, or goals.
Egosyntonic refers to experiences that are consistent with your idea of self and your needs, likes, or goals.
Egodystonic refers to experiences that feel intrusive, offensive, hurtful, contradictory, or that you feel go against your sense of self.
Visions of a lost loved one tend to be egosyntonic hallucinations. They’re typically comforting and may make you feel like they’re still around, explains Shrand.
How common are grief hallucinations?
Since the early 1970s, research has indicated that bereavement hallucinations are commonplace.
Some of the most recent data, from 2015, indicates that as many as 60% of people who’ve lost their spouses report at least one grieving hallucinatory experience.
Research is inconclusive about what exactly causes someone to experience hallucinations of a loved one who has passed away.
Grief affects the body in many ways. Facing a loss may affect your mental and emotional health differently, although in most cases, the pain tends to decrease with time.
According to research on the neuroscience behind grief and loss, grieving can be a form of emotional learning. The brain may process the emotions related to grieving as a learning experience that helps reduce separation distress.
In other words, creating opportunities to feel like a part of your loved one is still with you might help you deal with intense emotional pain. Grief hallucinations may be the result of your brain trying to cope.
The same research suggests that prolonged grief disorder could be related to the brain having difficulty processing the loss.
Prolonged grief disorder, once known as complicated grief, is a condition listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5). You may be experiencing this long lasting grief if your pain doesn’t ease with time, escalates, or makes daily functioning a challenge.
There is no compelling evidence that grief causes psychosis. However, 2014 research suggests that the unexpected death of a loved one may lead to experiencing mental health conditions like post-traumatic stress disorder (PTSD) and major depressive disorder.
In some cases, these conditions can appear with symptoms of psychosis, including hallucinations.
Psychosis is a mental state that occurs when your brain isn’t able to distinguish between what’s real in your environment and what isn’t.
It’s possible some people may experience hallucinations when facing the loss of a loved one, explains Barbara Rubel, a board certified expert in traumatic stress from Kendall Park, New Jersey. But, most people don’t experience an episode of psychosis when grieving, she adds.
While they might sometimes fit the hallucination diagnostic criteria, grief hallucinations may not necessarily be a lapse in reality.
Research suggests sensory experiences during mourning, particularly sensing the presence of a lost loved one, might come from a subconscious effort to maintain a connection to that person.
In a 2009 review on grief and bereavement, experts noted hallucinations during acute grief provided study participants with a sense of connection to the loved one, as did keeping mementos like clothing, pictures, or favorite possessions.
Depression vs. grief
Symptoms of depression can accompany grief, so how can you tell what’s clinical depression and what’s bereavement?
Uncomplicated grief — and the intense emotions it may cause you — will tend to get better in time.
Clinical depression, however, is a mental health condition that lasts longer than 2 weeks and lasts even in the absence of grief. It may also intensify with time if no formal treatment is sought.
People living with prolonged grief disorder are more likely to experience grief hallucinations, according to the DSM-5.
But it’s also possible that anyone grieving a recent and unexpected loss can experience them as well.
A 2009 literature review noted that these sensory experiences could be common immediately after the loss of a loved one.
“Anyone bereaved can experience a hallucination,” says Rubel. “However, there are many influences that impact grief, such as sudden death, traumatic death, suicide, a love/hate relationship, a young child, for example. ”
”
The exact nature of bereavement sensory experiences is unclear.
By definition, seeing a loved one who has passed, hearing their voice, or feeling their touch are experiences that can be defined clinically as hallucinations.
What’s less clear is many people’s feeling of a loved one’s presence. Unlike traditional hallucinations, the perception that your loved one is near or in the same space as you isn’t clearly linked to one of your five senses.
It cannot be defined as a delusion either, another symptom of psychosis that refers to a firm belief that defies evidence.
Similarly, reminders of a loved one aren’t necessarily hallucinations. Smelling their essence when you’re in a store, for example, isn’t necessarily a hallucination.
The stimulus might be there — for example, a similar odor. You could associate the similarity to something familiar that makes you feel close to your lost loved one.
If you’re experiencing vivid, disruptive, or disorienting sensory changes, a health professional can help you explore potential causes.
A mental health specialist can also help you work through the grieving process, especially if you feel you’re having a hard time coping with the emotional pain.
If bereavement hallucinations aren’t impairing or persistent, Shrand suggests allowing them to take a natural course.
“I would not try to convince the person they were hallucinating and deprive them of that comfort,” he says. “Some spouses talk to their departed loved ones for decades. Some parents know their child is contacting them even if they can’t see them. Rather than experience overwhelming loss, they find a way to keep that loved one close.”
Sensing a loved one who has passed, hearing their voice, or catching a glimpse of them can be sensory experiences known as bereavement or grief hallucinations.
Many people find these moments comforting. In fact, grief hallucinations are considered by some experts as a common feature of the bereavement process.
Some forms of grief, like prolonged grief disorder, may present with other mental health symptoms and may require professional attention.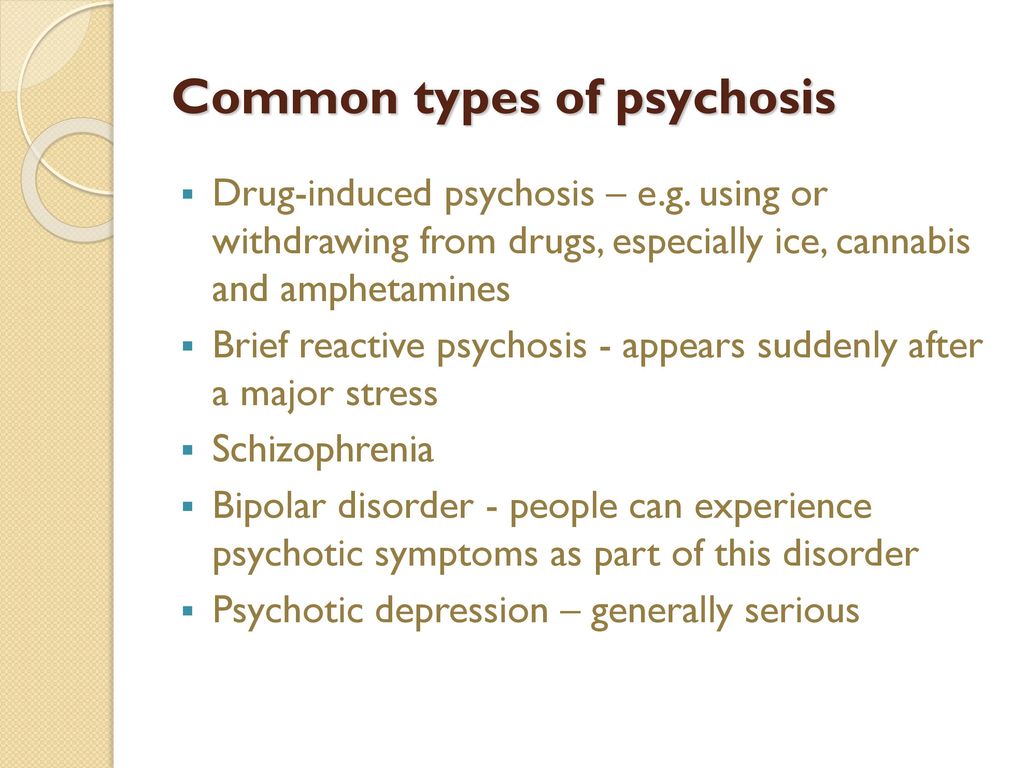
Experiencing a grief hallucination doesn’t mean you’ve developed psychosis or another mental health condition. Sometimes, bereavement hallucinations may be your way of coping with a loved one’s loss.
If you’re finding it hard to cope with your loss, it may be a good idea to reach out to a support group or mental health professional.
Study: Climbing mountains causes mental changes
Mysterious voices, strange visions and the feeling of the presence of someone else are faithful companions of climbers ascending to great heights. Scientists have found that these hallucinations are not associated with physiological changes in the body and are obviously caused by the psyche.
Climbers climbing to a height of more than 7000 m often encounter various hallucinations. Both visual and auditory hallucinations are common - climbers notice movement where there is none, hear music or voices. And more often this is faced by those who climb the mountain alone.
Thus, the Austrian climber Hermann Buhl, who was the first to conquer the 8126-meter-high Nanga Parbat peak in the northwestern Himalayas - the ninth largest peak in the world, nicknamed the "killer mountain" because 31 climbers died while climbing it, - on the way back suddenly discovered that he had a company, although he climbed to the top alone: “At the Silbersattel, I saw two points. And he almost screamed with joy: someone is going up.
And he almost screamed with joy: someone is going up.
I heard voices, someone called "Herman!", but then I realized that these were stones on the peak of Chongra, towering behind. The disappointment was bitter. Depressed, I set off again. Such realizations happened frequently. Then I heard voices, distinctly heard my name - hallucinations.
Another type of hallucination is so common that it has a separate name - the third person factor. With it, climbers get the feeling that there is someone else on the mountain besides them.
This type of hallucination is not unique to rock climbers - for example, polar explorer Sir Ernest Shackleton wrote about a similar experience during an expedition to Antarctica in 1914. The report featured a fourth person who accompanied the three members of the expedition.
"It often seemed to me that there were four of us instead of three," wrote Shackleton.
American pilot Charles Lindbergh cited similar evidence. During his famous transatlantic flight, he felt as if he was not alone in the cockpit: “The fuselage behind me was filled with ghostly creatures - vague silhouettes, transparent, moving, weightlessly traveling with me in the plane,” he wrote. Their appearance did not surprise me. There was no suddenness in it ... Without turning my head, I saw them as clearly as in the usual field of view.
Their appearance did not surprise me. There was no suddenness in it ... Without turning my head, I saw them as clearly as in the usual field of view.
In The Third Man Factor, writer John Geiger lists conditions associated with perceived presence:
monotony, darkness, barren landscape, isolation, cold, injury, dehydration, hunger, fatigue, and fear.
For a long time, the "third factor" was associated with altitude sickness, which occurs due to oxygen starvation. Its symptoms include dizziness, nausea, insomnia, bleeding in the eyes and, in severe cases, swelling of the brain and lungs. A variation of altitude sickness is mountain sickness, in the occurrence of which physical overwork, dehydration, hypothermia, sudden changes in temperature, and severe weather conditions also play a role. But still oxygen starvation remains the main pathological factor.
Experts from the Eurac Research Center in Italy and the Leopold and Franz University of Innsbruck in Austria believe that hallucinations are not the result of oxygen starvation and occur independently of it. The researchers presented their findings in an article in the journal Psychological Medicine .
The researchers presented their findings in an article in the journal Psychological Medicine .
They reviewed 83 episodes of hallucinations in climbers and examined the accompanying symptoms.
“In our study, we found that there is a group of symptoms that are purely psychotic,” says Hermann Brugger, one of the authors of the work. -
That is, although they occur at high altitude, they cannot be attributed to organic factors such as cerebral edema, fluid loss, or infection.”
However, scientists cannot name the cause of hallucinations with certainty. They suggest that the appearance of the apparent "third" may be due to loneliness or being in a small group or difficult climbing conditions. It is known that when returning to a safe altitude, the hallucinations disappear and have no long-term effects.
"This discovery allows for a more thorough study of transient psychoses in healthy people, which may provide clues to understanding the nature of mental illnesses such as schizophrenia," said study co-author Katharina Hüfner.
Also, the results of the study will allow climbers to better prepare for the ascent and make a plan of action in case they have to deal with high-altitude psychosis.
In addition, researchers can try to reproduce the results in the lab using low pressure, low oxygen chambers.
Next year, the team, in collaboration with specialists from Nepal, is going to more accurately estimate the incidence of psychosis, as well as clarify the factors of its occurrence and potential risks.
Help for a loved one with a mental disorder
Basic concepts
There is a lot of talk these days about the rise in the number of mental disorders in society, but many people have very vague ideas about this very vague concept. Despite the fact that now psychiatrists are doing everything possible to inform the population as best as possible about stress, depression, anxiety, neuroses, more severe mental disorders, there is very little literature written by experts for the average layman, and on the Internet there is an abundance of information written either difficult language, or simply illiterate. All this ultimately leads to the fact that such information is not only contrary to reality, but also harmful.
All this ultimately leads to the fact that such information is not only contrary to reality, but also harmful.
It is impossible to “sort things out” in one article and give clear instructions on the relationship between the patient and his relatives, but it is possible to bring to a holistic picture the idea of this complex group of diseases (the terms “disease” and “disorder” from a medical point of view are largely close, but not identical*). Therefore, my task is to acquaint the reader with this complex problem, primarily related to relationships and assistance to those suffering from severe mental illnesses.
* It is desirable to know the most basic terms, then it will be easier for the doctor to help both the patient himself and his relatives. In addition, you should not use terms that are not well known to you, it is better to describe the situation or condition as you understand it.
So, mental (or mental, because psyche - translated from Greek means soul ) disorders - are painful conditions of a person with psychopathological (i.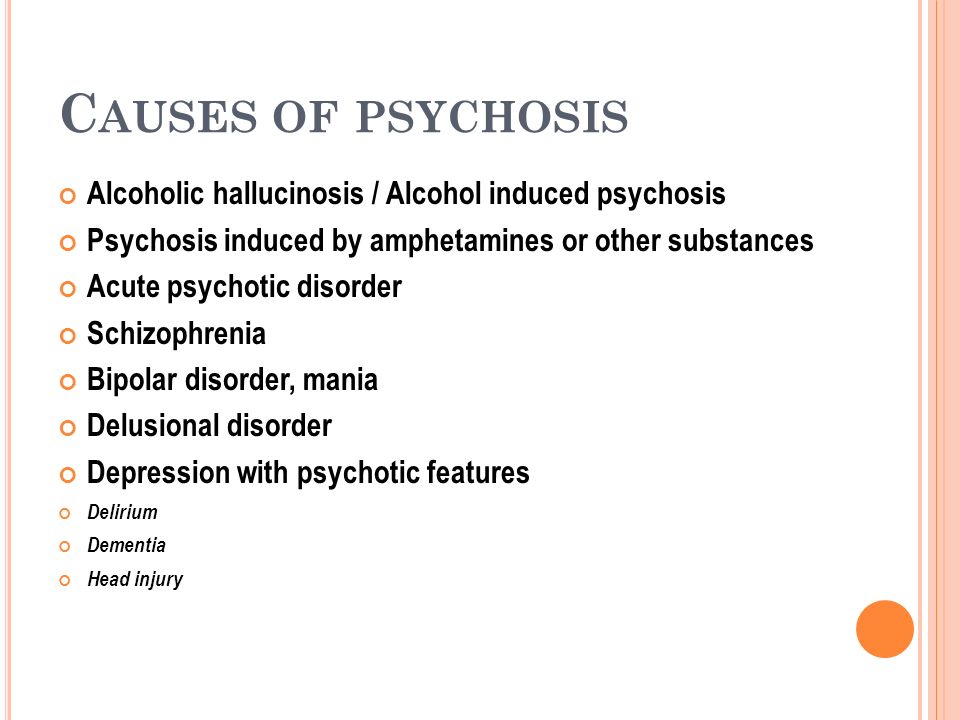 e., with mental disorders) and behavioral (i.e., they do not always appear, for example, in case of neuroses, when a person by an effort of will keeps himself within the limits of a cultural society up to a certain point) manifestations due to the influence of biological, psychological, social and other factors.
e., with mental disorders) and behavioral (i.e., they do not always appear, for example, in case of neuroses, when a person by an effort of will keeps himself within the limits of a cultural society up to a certain point) manifestations due to the influence of biological, psychological, social and other factors.
Let's not confuse with psychosis (or psychotic) disorders, which are characterized by gross and contradictory environmental disorders of thinking, perception and behavior (delusions, in a medical, not philistine view; hallucinations; psychomotor agitation; suicidal behavior, etc.).
It is important to note that the problem of mental disorders is interdisciplinary and even interdepartmental, social. Rehabilitation is needed, not just treatment.
As for the diagnosis. Diagnosis - definition and recognition, an indication of the disease. In medicine, and especially in psychiatry, diagnosis does not always mean treatment in strict accordance with the diagnosis. Diagnosis is often a statistical category needed to understand, roughly speaking, how the condition of one patient is similar to another.
Diagnosis is often a statistical category needed to understand, roughly speaking, how the condition of one patient is similar to another.
I am sometimes puzzled by the desire of a person to look at the records of a doctor. After all, a special interpretation, justification of the diagnosis, terminology can not only frighten and offend an unprepared person, but cause unreasonable distrust of a specialist and, even worse, aggravate disturbed mental balance, upset not only the patient, but also relatives.
It is much more important to trust each other (the doctor, the patient, his relatives), to ask questions of interest. It is on trust that the desired result is achieved - a cure or a stable remission, if the disorder is chronic.
I will not decipher concepts and terms much in this article. Let's talk about the topic corresponding to the title. We will talk about such diseases as schizophrenia, dementia, severe depression, drug addiction (alcoholism, drug addiction), etc. I will try to give basic, a kind of "universal" recommendations.
I will try to give basic, a kind of "universal" recommendations.
Recommendations
1 situation: a relative (both a 16-year-old child and an old grandfather, a researcher in the past or present) became “somehow not like that”, began to withdraw, get annoyed for no apparent reason, although “he had never been aggressive before ', to talk, to talk to oneself.
Usually, such behavior is first perceived as a joke, then surprise, then a discussion with a sick person begins, which can lead to serious conflicts and distrust. If you suspect that a person close to you has a mental disorder (we do not take emergency situations, for example, in case of severe aggression, the police and medical workers are already intervening here), you cannot argue.
It is also desirable not to support the painful delusions of a person, to try to be patient and caring, to persuade a loved one to seek medical help. Unfortunately, in our society, when it comes to psychiatry, in most cases it causes a smile, fear, surprise, but not sympathy and a desire to help a sick person, especially if it refers to a relative. Only later, when a sick person can feel and even understand that the help of a psychiatrist is for his benefit, will he himself reach out to her.
Only later, when a sick person can feel and even understand that the help of a psychiatrist is for his benefit, will he himself reach out to her.
At the initial stage, it is worth trying to persuade a person to calm down, assess his degree of adequacy (if he used to trust you, but now he doesn’t groundlessly, whether he understands you or is completely in his experiences, etc.), to understand whether there are threats to him and surrounding.
It is impossible to forcibly help a person (involuntary hospitalization in a psychiatric hospital is carried out only by a court decision), but everything possible must be done: to involve relatives who will correctly understand and support people who are authoritative for the patient, consult a doctor.
Situation 2: patients were brought to a psychiatrist. There can be 2 ways here. The doctor will help to understand the situation, make a diagnosis, prescribe treatment, give recommendations. Everything here is very individual. But it may also be that the doctor gives a recommendation, but not only the patient (due to inadequacy), but also a relative does not want to follow it.
But it may also be that the doctor gives a recommendation, but not only the patient (due to inadequacy), but also a relative does not want to follow it.
I can give an example. A mother brings her 20-year-old daughter to a psychotherapist. The daughter has painful sensations in her body: the bones, according to her, “go back and forth, fall through and hurt.” All specialists were examined, all studies were carried out, including MRI, no diseases were found, the symptoms do not correspond to the alleged physical pathology.
A mental illness was diagnosed, drugs were prescribed, and after a couple of months there was a significant improvement. The patient stops taking the medicine, after a while she comes to the doctor with her mother, complains about the deterioration, assures that the medicines do not help, refuses help, runs out of the office, rushes about, says that she does not want to live. Hospitalization is proposed, since adequate dosages of drugs can only be prescribed in a hospital, in response - a categorical refusal.
With difficulty he manages to calm down, persuade him to give an injection, agrees to resume taking medications. The doctor suggests that the mother call a psychiatric team to resolve the issue of hospitalization, in connection with the suicidal risk, to which he receives the answer: “Well, she will kill herself, then this is her fate, I will not put her in a psychiatric hospital.” On receipt released home. The mother calls the next day, the daughter gets a little better, then disappears for six months. Another call to the doctor's personal phone: the daughter lies in bed, does not want to get up, complains about "movements in the body of some creatures" that cause severe pain.
Recommendations were given, the patient was finally hospitalized in a psychiatric hospital with schizophrenia. She was discharged with improvement, criticism of her condition appeared, adequate therapy was selected.
Bottom line: fortunately, this story ended happily, but the patient suffered for several months, while the mother believed in the need for hospitalization; I had to prescribe heavier drugs, the treatment was delayed.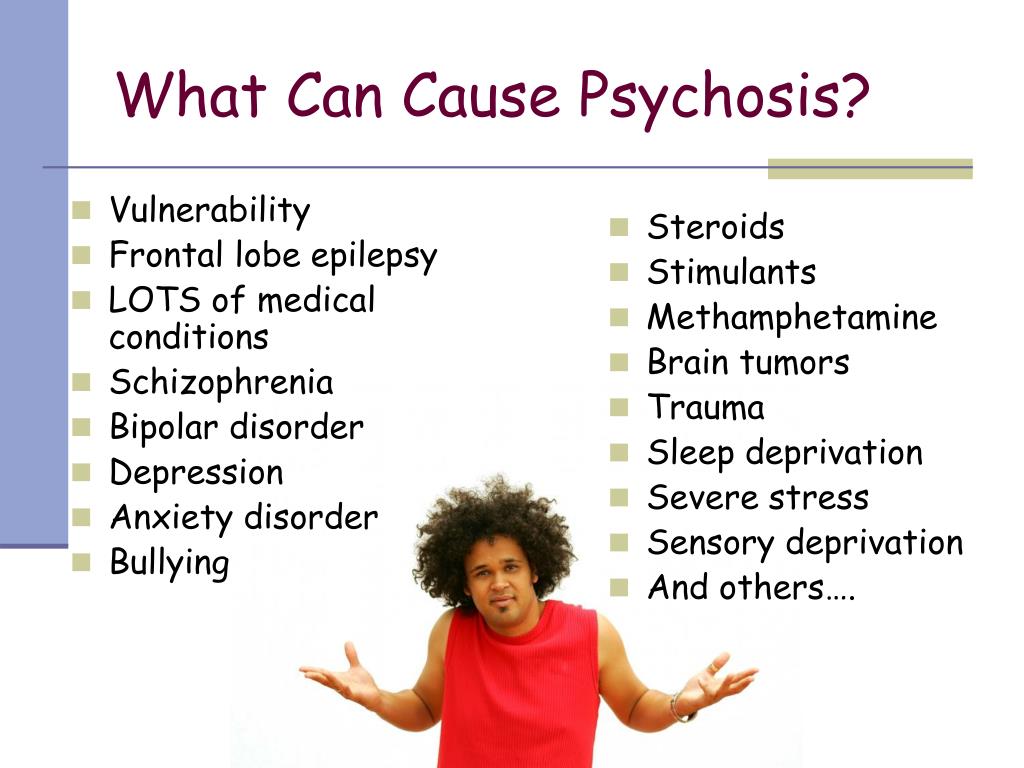
There is nothing wrong if the patient refuses this doctor (for example, the patient has included the doctor in his delusional system) or the doctor himself understands that he will not be able to provide adequate assistance. Then it is necessary to attract colleagues, send them to a hospital, together with relatives, think over options for assistance and choose the best one. It happens that the patient returns after treatment, apologizes for his behavior, because he did not understand the pain and inadequacy at that time.
You should not change specialists (sometimes people come to me with dozens of recommendations from different doctors of the same specialty, which is puzzling). Well, 2-3 opinions is understandable, but more than 10!? The most common reason is that medications do not immediately help, side effects.
Some patients soon stop taking their medications, and many diseases are chronic and require many months or even years of maintenance therapy.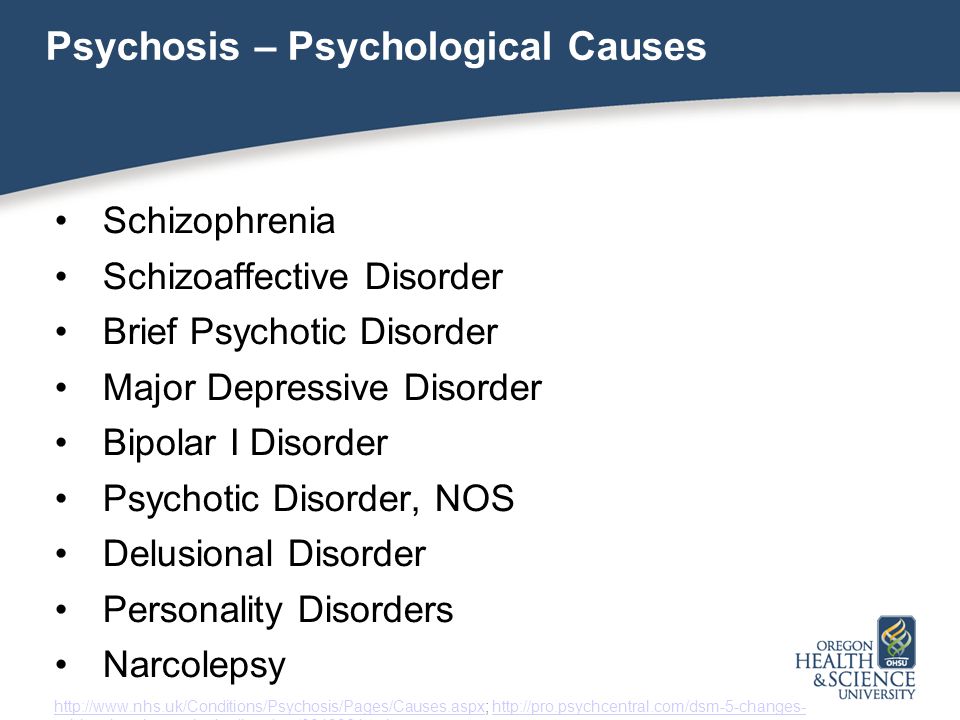 A natural deterioration sets in, the new doctor does not yet know the specifics of the course of the disorder in this patient, experiments with treatment begin, a new selection of medicines begins, resistance to treatment is formed, and previously effective drugs cease to work.
A natural deterioration sets in, the new doctor does not yet know the specifics of the course of the disorder in this patient, experiments with treatment begin, a new selection of medicines begins, resistance to treatment is formed, and previously effective drugs cease to work.
And one more thing: it is desirable, at the initial visit to the doctor, to bring, if not all, then the main examinations, extracts, and tests. A psychiatrist is a doctor like everyone else, and the more information about the patient, the easier it is to understand the diagnosis. For example, if a person has a pathology of the thyroid gland, it is advisable to bring the last tests for hormones, since when the hormonal background changes, the state of mind also changes (irritability, sleep disturbances, mood swings, etc.).
In some cases, antidepressants are not only not needed, but can be harmful, it may be worth limiting yourself to the appointments of an endocrinologist and psychotherapy.![]() Elderly people with diabetes can confuse events and even behave inappropriately with an increase in blood glucose, here prescribed antipsychotics are also not always necessary.
Elderly people with diabetes can confuse events and even behave inappropriately with an increase in blood glucose, here prescribed antipsychotics are also not always necessary.
3 situation: the patient has been examined for a long time, the diagnosis is known, but the disease is progressing. Relatives begin to "look for a miracle": consult the patient with leading specialists, go to the main scientific centers, someone is looking for help abroad.
I have had a number of cases where patients have returned from the US, Europe, Israel, etc. with complaints that the prescription of drugs selected in Russia was refused, or that the treatment was simply ineffective, worsened. Here I would advise you to find a specialist you trust and coordinate your actions with him. Only together can we help sick people provide adequate assistance and, if not cured, then improve the quality of life as much as possible.
4 situation: terminally ill in the final stage. There is an opinion, or rather another myth, that one does not die from mental illness, however, mental illness is the same as somatic (i.e. body diseases), only the brain is sick, regardless there is a visible focus there (for example, as a result of a craniocerebral injury to the damaged part of the brain) or not. For example, severe progressive dementia, the final stage of alcoholism with multiple organ disorders, the terminal stage in malignant forms of schizophrenia, and others. Here it is necessary to decide individually, depending on the specific case.
There is an opinion, or rather another myth, that one does not die from mental illness, however, mental illness is the same as somatic (i.e. body diseases), only the brain is sick, regardless there is a visible focus there (for example, as a result of a craniocerebral injury to the damaged part of the brain) or not. For example, severe progressive dementia, the final stage of alcoholism with multiple organ disorders, the terminal stage in malignant forms of schizophrenia, and others. Here it is necessary to decide individually, depending on the specific case.
“If a person cannot be cured, this does not mean that he cannot be helped.”
If you are destined to die, it is easier to do this among loving relatives on your bed, even if a person does not understand anything and does not recognize anyone. But he FEELS the attitude towards him. How a small child feels the caress of his mother, smiles or cries when his mother is gone. You will say - there is no comparison, children are our future, and here is a dying person who does not understand anything.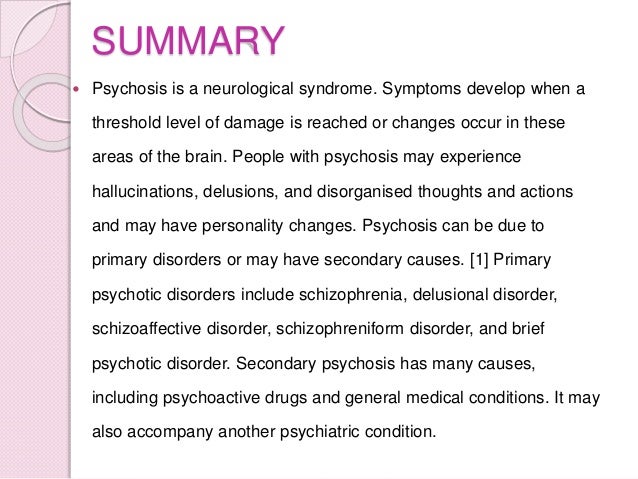 Yes, this is true, but we must understand that any of us can, God forbid, be in the place of this person ...
Yes, this is true, but we must understand that any of us can, God forbid, be in the place of this person ...
Nursing staff
Well, a few words about help for those who care for the sick. It is difficult to give specific recommendations here, only one thing is clear: you cannot take the position of either a rescuer or a victim, you just need to fulfill your human duty to the best of your ability and ability. Don't forget yourself.
Any person who lives with a sick person, and even more so caring for him, experiences enormous personal and emotional stress. Therefore, you should think about how you will cope with the disease in the future. By understanding your own emotions properly, you will be able to deal more effectively with both the patient's problems and your own problems. You may have to experience emotions such as grief, shame, anger, embarrassment, loneliness and others.
For some people who care for the sick, the family is the best helper, for others it brings only grief. It is important not to reject the help of other family members if they have enough time, and not to try to bear the sometimes difficult burden of caring for the sick alone.
It is important not to reject the help of other family members if they have enough time, and not to try to bear the sometimes difficult burden of caring for the sick alone.
If family members upset you with their unwillingness to help, or criticize your work because of the lack of information about this disorder, you can form a family council to discuss care problems. In particular, make a decision to involve an employee, at least for the period of time necessary for your rest and recuperation, and, if necessary, treatment.
And the last. Don't keep problems to yourself. Feeling that your emotions are a natural reaction in your position, it will be easier for you to cope with your problems. Don't reject the help and support of others, even if you feel like you're making it difficult. Even psychotherapists themselves (seemingly knowing how to minimize stress as much as possible) often have their own psychotherapist, and it is bad for the doctor who neglects the help of his colleagues.