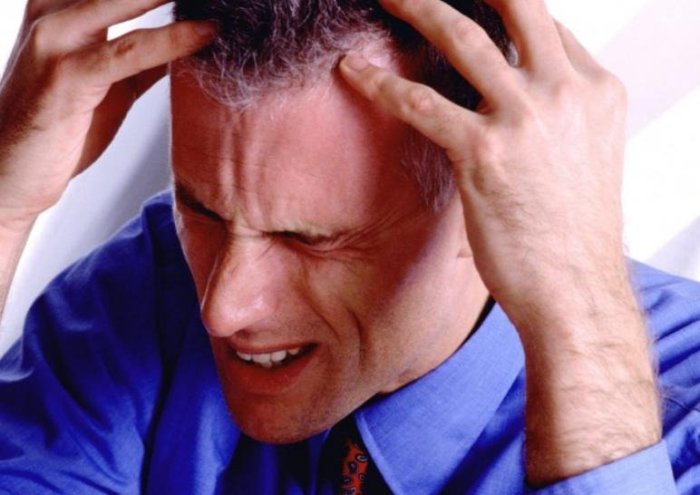
Migraine from crying
Causes, Other Symptoms, Treatment, and More
Why it happens
Crying is a natural response to a strong emotion — like watching a sad movie or going through a particularly painful breakup.
Sometimes the emotions you feel when you cry can be so intense that they lead to physical symptoms, like a headache.
How crying might cause headaches isn’t clear, but intense emotions, like stress and anxiety, seem to trigger processes in the brain that pave the way for headache pain.
Non-emotional or positive tears don’t seem to have the same effect. Researchers have found that crying while you cut onions or when you’re happy doesn’t provoke headaches. Only tears tied to negative emotions have this effect.
Read on to learn more about how these headaches present and what you can do to find relief.
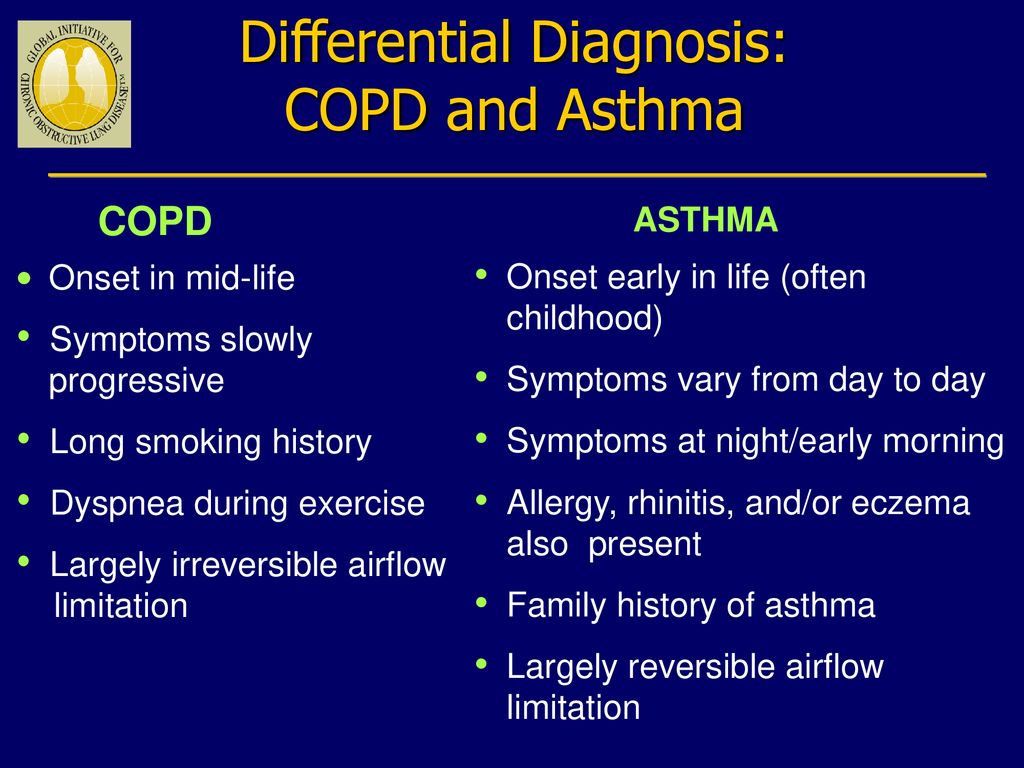
Migraine and tension headaches are two of the most common headache types:
- Migraines cause severe, pounding pain — often just on one side of your head.
They’re often accompanied by symptoms like nausea, vomiting, and extreme sensitivity to light and sound.
- Tension headaches cause an aching pain and pressure that can feel like a band tightening around your head. Your neck and shoulders might also ache.
In one 2003 study, researchers found that anxiety-provoking and stressful situations were the biggest triggers for migraine and tension headaches. They saw crying as a likely and common but less well-known trigger worthy of further study and discussion.
What you can do
Medication can help prevent tension and migraine headaches as well as relieve symptoms once they start.
You may be able to stop a headache in its tracks with:
- Over-the-counter (OTC) pain relievers, such as aspirin, ibuprofen (Advil), and acetaminophen (Tylenol), may be enough to relieve mild headache pain. If your symptoms are more moderate, look for a pain reliever that combines acetaminophen or aspirin with caffeine for maximum effect.
- Triptans change blood flow in the brain to bring down inflammation. They can help with severe migraine pain. Sumatriptan (Imitrex) is available OTC. Frovatriptan (Frova), rizatriptan (Maxalt), and other triptans are available by prescription only.
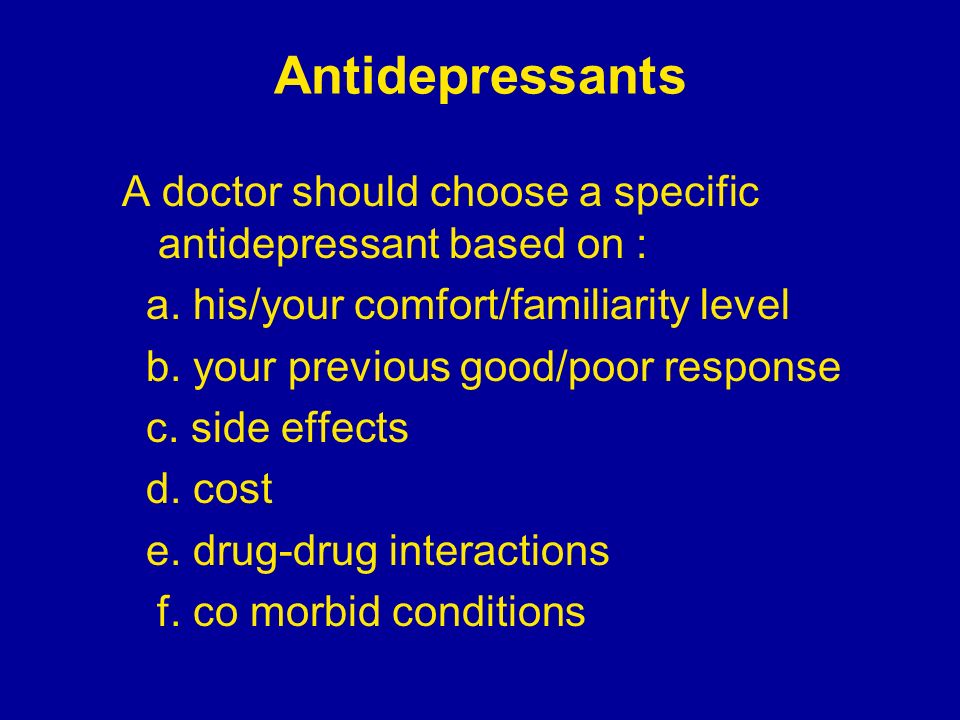
If you get regular migraine or tension headaches, your doctor might prescribe one of these drugs to help prevent them:
- Cardiovascular drugs treat high blood pressure and coronary artery disease, but they also prevent migraine headaches. This includes beta-blockers like metoprolol (Lopressor) and calcium channel blockers like verapamil (Calan).
- Antidepressants prevent both migraines and tension headaches. This includes tricyclics like amitriptyline and selective serotonin-norepinephrine reuptake inhibitors (SNRIs) like venlafaxine (Effexor).
- Anti-seizure drugs, such as topiramate (Topamax), can reduce the number of migraine headaches you get.
 These drugs might prevent tension headaches, too.
These drugs might prevent tension headaches, too.
Your emotions and your sinuses are more closely linked than you might think. More than 20 percent of the people with chronic sinus problems report feeling depressed. This may be because both conditions stem from inflammation.
Inflamed sinuses may also contribute to depression by interfering with sleep and reducing quality of life.
Crying bouts are common in people who are depressed. Crying can worsen sinus symptoms like congestion and a runny nose. Pressure and congestion in your sinuses can contribute to headache pain.
Other symptoms of a sinus problem include:
- stuffed nose
- pain around your cheeks, eyes, forehead, nose, jaw, and teeth
- thick discharge from your nose
- dripping in the back of your throat (postnasal drip)
- cough
- sore throat
What you can do
OTC and prescription-strength nasal corticosteroids can bring down inflammation in the sinus passages.
Popular options include:
- beclomethasone (Beconase AQ)
- budesonide (Rhinocort)
- fluticasone (Flonase)
- mometasone (Nasonex)
Corticosteroids are also available in oral and injected forms.
If you have severe sinus symptoms that don’t improve with medicine, your doctor might recommend surgery to open up your sinus passages.
Both your body and brain need the right balance of fluids and electrolytes to work properly. If you don’t drink enough fluids, or you lose them too quickly, you can become dehydrated.
When your brain loses too much fluid, it shrinks. This reduction in brain volume can cause headache pain. Dehydration might also trigger or prolong migraine headache attacks.
People who’ve experienced a dehydration headache say the pain feels like an ache. It may get worse when you move your head, walk, or bend down.
Other signs of dehydration include:
- dry mouth
- extreme thirst
- less frequent urination
- dark urine
- confusion
- dizziness
- fatigue
Crying is very unlikely to dehydrate you, unless you haven’t been drinking enough fluid. Dehydration is usually the result of:
Dehydration is usually the result of:
- excess sweating
- increased urination
- diarrhea or vomiting
- fever
What you can do
Oftentimes, the pain will go away after you have a glass or two of water or an electrolyte drink, like Gatorade.
You can also take an OTC pain reliever, like aspirin, ibuprofen (Advil), or acetaminophen (Tylenol).
You shouldn’t take pain relievers or other drugs that contain caffeine. They can increase fluid loss.
You should seek immediate medical attention if you have a headache and experience:
- trouble seeing or talking
- confusion
- vomiting
- fever of 102°F (about 39°C) or higher
- numbness or weakness on one side of your body
It may also be a good idea to see your doctor if your headache symptoms don’t improve within a day or two. Your doctor can confirm the underlying cause and recommend more targeted treatment.
You should also talk to your doctor if you cry often or you regularly feel down. This could be the result of an underlying condition like depression.
This could be the result of an underlying condition like depression.
Other signs of depression include:
- feeling hopeless, guilty, or worthless
- losing interest in things you once loved
- having very little energy
- feeling extremely tired
- being irritable
- having trouble concentrating or remembering
- sleeping too much or too little
- gaining or losing weight
- thinking about dying
Antidepressant drugs and therapy can help relieve your depression — and with it, your crying bouts.
Headache after crying: Why does it happen?
Crying is a natural response to many emotions, including sadness, grief, stress, and even happiness. Some people experience a headache after crying.
The body produces tears when the limbic system, which is responsible for emotional arousal, sends a signal to the lacrimal glands. These glands, located just above each eyelid, produce tears.
When a person cries, they may also experience a runny nose and tension in the muscles around their face and head.
This article discusses the types of headaches that people might experience after crying and how to treat or prevent them.
To discover more evidence-based information and resources for headache and migraine, visit our dedicated hub.
Scientists do not know the exact link between crying and headaches.
Often when a person is crying, they may be experiencing pain or strong emotions, which put the body under stress. The body releases hormones, such as cortisol, when experiencing stress, which can cause a range of physical and emotional reactions in the body.
Crying also engages several facial muscles, which may cause tension around the face, head, and neck.
These emotional and physical processes may be responsible for triggering several different types of headaches after crying.
One type of headache that a person may experience after crying is a tension headache.
When a person cries, several muscles in their face tense up. They may also feel tension in their jaw, down their neck, and at the back of their head. If a person is crying over a prolonged period, the continuous contractions of these muscles may result in a tension headache.
If a person is crying over a prolonged period, the continuous contractions of these muscles may result in a tension headache.
Tension headaches are the most common primary headache, a headache that is not the result of another condition.
Symptoms of a tension headache may include:
- pain on both sides of the head, neck, or face
- a pain that feels like a tight vice or band around the head
- tender feeling in the affected area which may worsen with touch
When a person cries, their tears drain into small holes in the corners of the eyelids, known as puncta. If a person produces a lot of tears, this drainage system becomes overwhelmed, and tears overflow down their cheeks. Some of these tears can also drain into their nasal passage.
Within the nasal passage are small, hollow spaces, known as the sinuses, that run along the cheekbones and forehead. When tears drain into the sinuses, they mix with mucus and can cause a runny nose. This buildup of mucus and tears can cause pressure in the sinuses, which may lead to a headache.
A person experiencing a sinus headache may feel pain and pressure across their forehead, cheeks, or around their eyes. These areas may also be tender and painful to touch. The pain and pressure of a sinus headache may worsen with sudden movements or when a person leans forward.
However, it is important to note that sinus headaches are not common and people experience them as a result of sinusitis. Furthermore, there is an overlap between the symptoms of sinus headaches and a migraine, so it may be difficult for a person to know which one they are experiencing.
If a person is crying due to feeling overwhelmed and stressed, this may trigger a migraine attack.
Stress is a common trigger for migraines. Researchers found that 80% of people who experience migraines reported stress as one of their common triggers and 57.7% reported fatigue as another.
There are also some common links between the processes involved with crying and those that trigger a migraine attack.
Research has found that crying may activate the autonomic nervous system. Additionally, research shows that migraine attacks may occur due to dysregulation of the sympathetic nervous system, which is part of the autonomic nervous system, indicating a possible connection between the two.
Migraine attacks are a common type of headache, with around 15% of Americans experiencing them. Migraines may involve a throbbing or pounding pain across the head and face. This pain can be moderate to severe and tends to worsen with activity.
It is common for this pain to be on one side but it can occur anywhere across the face, head, and neck. Some people may mistake a migraine for a sinus headache, as the pain can also occur across the nose and behind the eyes and a runny nose may accompany it.
Along with pounding head pain, other symptoms of a migraine may include:
- nausea
- vomiting
- sensitivity to light, sound, or smells
There are several ways a person may reduce the discomfort of a headache after crying. A person may consider speaking with a doctor about headache treatments because different types of headaches may respond better to different treatments. People should speak with a doctor before taking any medications to manage their headaches.
A person may consider speaking with a doctor about headache treatments because different types of headaches may respond better to different treatments. People should speak with a doctor before taking any medications to manage their headaches.
A person may wish to try some of the following techniques:
- gently massaging the head and neck muscles to reduce tension
- placing a warm or cool pack on the affected area to help relieve pressure and lessen muscle tension
- taking over-the-counter pain medications, such as aspirin, acetaminophen, or ibuprofen
- taking triptans, a prescription medication that aims to treat migraines
- resting in a cool, dark, quiet room
In addition to the above treatments, if a person experiencing a crying-induced headache suspects it may be a sinus headache, they may wish to try the following:
- using a nasal irrigation device to help decongest the sinuses to relieve sinus pressure — the Food and Drug Administration (FDA) has a guide on how to safely use one
- leaning over a warm bowl of water and inhaling the vapor
- staying hydrated
Headaches are a common occurrence and can often cause mild discomfort. However, if a person is experiencing frequent headaches that impact their quality of life, they may wish to discuss potential causes and treatments with a doctor.
However, if a person is experiencing frequent headaches that impact their quality of life, they may wish to discuss potential causes and treatments with a doctor.
If a person experiences a headache with the following symptoms, it could be a sign of a more serious condition that requires medical attention:
- severe pain that is worse than any headache they have previously experienced
- a severe headache with a sudden onset
- a high fever
- repeated vomiting
- problems with their speech, vision, or balance
If a person frequently feels overwhelmed and is crying far more often than usual, this may be a sign that they are experiencing a mental health condition. A doctor can help a person understand their symptoms and find the right support and treatment for them.
To help support your mental well-being and that of your loved ones, visit our dedicated mental health hub for more research-backed information and resources.
If a person is experiencing any of the headaches discussed above frequently, the best prevention is to follow a treatment plan provided by a doctor.
A doctor may prescribe medications for persistent migraine and tension headaches that aim to prevent reoccurring headaches, such as beta-blockers.
If a person is experiencing frequent sinus pain, a doctor may prescribe steroid nasal sprays or antihistamines.
Other ways a person may prevent crying-induced headaches include:
- stress management
- practicing good posture to reduce tension in the neck and shoulders
- maintaining a regular sleep and exercise routine
Some people experience headaches after crying. Although scientists are not exactly sure why this occurs, facial muscle tension, sinus issues, and stress may play a role.
A person can try different techniques for preventing and treating headaches that occur after crying. However, if the headaches are frequent and impact their daily life, they may wish to see a doctor.
A doctor can discuss a person’s situation with them to help them decide the best course of treatment.
Headache in children (cephalgia in children)
Why does the child have a headache?
Headache (cephalgia) is any discomfort that occurs in the area from the eyebrows to the back of the head. This is one of the few sufferings familiar to almost anyone. At the appointment with a neurologist, every fifth patient complains of a headache.
It has long been believed that cephalalgia in children, especially young children, is rare. Actually it is not. It's just that kids can't describe how they feel when they have a headache, and older children don't like to complain about it and even hide this fact from their parents.
The most common causes of cephalalgia in children are mental, physical and emotional stress, vegetative-vascular dystonia, migraine, head injuries, inflammatory diseases in the head and neck. It is worth paying attention to how much time the child spends near the computer or TV. Prolonged stress on the organs of vision and hearing can provoke a headache.
Often cephalalgia occurs in a child who spends a long time in a stuffy room or eats irregularly. By the way, children who do not attend kindergarten are more likely to experience pain. This is due to the fact that parents do not always adhere to the daily routine for the child in a family environment, while in kindergarten there is timely meals and daytime sleep.
Sometimes a severe and especially sudden headache can signal problems in the brain or central nervous system. Also, cephalgia may indicate emotional or psychological problems, or a viral disease: tonsillitis, colds, flu.
Parents should remember that headache complaints are subjective and difficult to verify. There are "phenomena of pain" that make it possible to judge the presence and nature of the pain syndrome. It is necessary to analyze how a child with complaints of cephalalgia behaves. With complaints that deserve attention, the mood background is reduced, interest in the environment is weakening, the child seeks to lie down. There is a serious facial expression, sometimes shifted eyebrows, wrinkles over the bridge of the nose. Sometimes there is crying or moaning. The pallor or redness of the face, dark circles under the eyes, cold fingers are striking.
There is a serious facial expression, sometimes shifted eyebrows, wrinkles over the bridge of the nose. Sometimes there is crying or moaning. The pallor or redness of the face, dark circles under the eyes, cold fingers are striking.
Headache in infants is manifested by general anxiety, sleep disturbance, refusal to eat, regurgitation "fountain", fever. In severe cases, there is a monotonous "brain" cry. At 1-2 years old, instead of complaining of a headache, children talk about fatigue, they want to lie down. They may redden the whites of their eyes, yawning appears. Children from 3 to 7 years old can already distinguish and describe cephalalgia.
Nowadays, schoolchildren constantly experience stress and overwork. Among all types of cephalalgia in adolescents, in 80% of cases and more often there is a headache of muscle tension. Children complain of a feeling of "tightness" around the head, tension and soreness of the scalp muscles are felt, discomfort occurs when combing the hair.
At the age of 12-13, hormonal changes begin in the child's body, affecting the functioning of his vessels and his psycho-emotional state, which can provoke the development of vascular headaches. There is a strong dependence on changes in weather conditions.
Migraine may be a possible cause of recurrent headaches. The probability of a migraine in a child is higher, the more his adult relatives are susceptible to it. An attack can provoke hunger, some foods, such as cheese, chocolate. Headache is accompanied by nausea, in severe cases - vomiting, "spots" appear before the eyes, photophobia.
To clarify the nature of cephalalgia in many children, it becomes necessary to conduct laboratory and instrumental studies, which makes it possible to exclude volumetric formations of the brain, the presence of concomitant diseases.
Treatment
Currently, in addition to drug therapy, a wide range of therapeutic methods and interventions are used to treat cephalalgia. The amount of drug assistance is determined by the doctor in each case.
The amount of drug assistance is determined by the doctor in each case.
Treatment of episodic headaches in children should begin with the correction of diet and diet, creating comfortable conditions for sleep. Daily walks in the fresh air are essential. Of the sports disciplines, preference is given to swimming, wushu, karate, and yoga. For children who are emotionally labile, impressionable, relaxation sessions with a psychotherapist, training in auto-training are recommended.
Physical therapy can be an alternative to drug therapy.
Children's clinics "ProMedicina" successfully use the methods of transcranial micropolarization (for cephalgia after head injuries) and interstitial electrical stimulation on the Gerasimov apparatus (for migraine, vascular headache) to treat headaches. Children with vegetative-vascular dystonia are shown acupuncture, massage, therapeutic baths.
In most cases, a child's headache is benign, but we must not forget that in some cases the headache becomes a manifestation of a serious illness. That is why it is important not to disregard even the rare complaints of the child. Parental anxiety is often understandable and justified.
That is why it is important not to disregard even the rare complaints of the child. Parental anxiety is often understandable and justified.
Author of the article: neurologist of the highest category Tukhfaeva Svetlana Gennadievna
Cluster headaches - treatment, symptoms, causes, diagnosis
Cluster headaches are characterized by pain that occurs on one side of the head. This headache is often described as pain that is localized around, behind or above the eye and along the temporal region, in cyclic patterns or clusters.
The pain in this type of headache is intense; many patients describe the pain as "boring". To be classified as a true cluster headache, there are specific autonomic manifestations such as lacrimation, redness of the conjunctiva, rhinorrhea or nasal congestion, droopy eyelids, sweating on one side of the face, or changes in pupil size (compared to the healthy side, the pupil on the affected side becomes narrower) . Headache lasts from 15 minutes to a maximum of 3 hours; however, the headache may recur up to eight times a day. Cluster headaches were originally described in the 17th century, but it was not until the mid-20th century that they were given this name.
Cluster headaches were originally described in the 17th century, but it was not until the mid-20th century that they were given this name.
Men are two to four times more likely to develop cluster headaches than women. However, the overall incidence is quite low, with a prevalence rate of about 1 in 1000. Due to the rarity of these types of headache, information on this type of headache is limited.
Although the vast majority of patients are adults, cluster headache occasionally occurs in children as young as 6 years of age.
Symptoms
Cluster headaches are always unilateral. However, some patients may experience some sensation on the opposite side of the affected part. Most patients describe pain around or behind the eye; the pain is also described as extending into the forehead, into the jaw, or along the line of the gums and teeth, or down the cheek on the affected side. Sometimes, the pain may radiate to the ear, neck, or shoulder. Although tearing is a characteristic feature of cluster headaches, some patients may only have conjunctival redness. Eyelid drooping or swelling and a runny nose are also often associated with cluster headache. The symptoms are often migraine-like, including sensitivity to light, sounds, or smells. However, unlike migraines, movement does not make cluster headaches worse. Also, many patients (more than 90%) describe feelings of anxiety during a cluster headache attack.
Eyelid drooping or swelling and a runny nose are also often associated with cluster headache. The symptoms are often migraine-like, including sensitivity to light, sounds, or smells. However, unlike migraines, movement does not make cluster headaches worse. Also, many patients (more than 90%) describe feelings of anxiety during a cluster headache attack.
Cluster headaches occur in groups of attacks. While the duration of a headache is short (15 minutes on average), headaches can recur up to eight times in a 24 hour period. Headaches can sometimes last up to 3 hours. Cyclic group attacks can last for only one day or last for many weeks.
Cause of cluster headaches
The specific cause and morphological nature of cluster headaches is not known. MRI data suggest that the ophthalmic artery dilates during a cluster headache attack, while PET scans show activity in the cavernous sinus. At the same time, many patients with other types of headache also showed abnormalities in similar regions, so the results of PET and MRI are not conclusive. There is some evidence that the hypothalamus may be involved in headache cycling. Activation of the trigeminal ganglion can induce many of the autonomic changes associated with cluster headache, but there is as yet no evidence that this triggers the activation of a pain attack.
There is some evidence that the hypothalamus may be involved in headache cycling. Activation of the trigeminal ganglion can induce many of the autonomic changes associated with cluster headache, but there is as yet no evidence that this triggers the activation of a pain attack.
Triggers
Many patients report having headaches while they sleep. In addition, alcohol can cause headaches in patients who have already begun pain cycles. Histamines and nitroglycerin can also cause headaches in patients. There was also some seasonal variability, but this was not observed in all patients. In some patients, cluster headache attacks were due to changes in the environment, the level of stress, or the level of physical activity. Hormonal factors or menstruation do not appear to cause cluster headaches. Other risk factors include: smoking and hereditary determinism.
Diagnosis
Diagnosis of headache is usually based on history, clinical findings and physical examination. Cluster headaches are symptomatic and often only the history and symptoms are sufficient. While no imaging modality can confirm the diagnosis of cluster headache, an MRI or CT scan of the brain may be needed to rule out other possible conditions that may mimic cluster headache symptoms. In some cases, an eye examination is needed to rule out problems within the eye itself that may be causing the symptoms.
Cluster headaches are symptomatic and often only the history and symptoms are sufficient. While no imaging modality can confirm the diagnosis of cluster headache, an MRI or CT scan of the brain may be needed to rule out other possible conditions that may mimic cluster headache symptoms. In some cases, an eye examination is needed to rule out problems within the eye itself that may be causing the symptoms.
Treatment
Treatment of cluster headache can be divided into two categories - relief of acute headache and prevention of future headache attacks. Inhalation of oxygen through a mask effectively helps 70% of patients and relieves an attack in a short time. However, this method of relief is cumbersome and most patients are unable or unwilling to carry an oxygen tank with them, especially if they plan to travel. Injectable sumatriptan is also effective in 75% of patients with cluster headache. But the injectable use of sumatriptan is contraindicated in patients with heart disease or hypertension. The nasal spray or tablets of this drug are less effective than the injections. IV dihydroergotamine can be very effective in relieving cluster headache, but it is not always possible to give it immediately after an attack and cannot be used if the patient has already received sumatriptan within the previous 24 hours. Nasal lidocaine can be a treatment option for a pain attack, but must be given in a specific order and is ineffective unless used incorrectly.
The nasal spray or tablets of this drug are less effective than the injections. IV dihydroergotamine can be very effective in relieving cluster headache, but it is not always possible to give it immediately after an attack and cannot be used if the patient has already received sumatriptan within the previous 24 hours. Nasal lidocaine can be a treatment option for a pain attack, but must be given in a specific order and is ineffective unless used incorrectly.
Steroids can be very effective in reducing the headache cycle; they can be used sporadically, as long-term use can lead to significant complications. Verapamil, lithium, valproic acid, topiramate, and melatonin may also be used to reduce the frequency and severity of cluster headache cycles. In severe cases of cluster headaches, surgical treatment may be indicated. Radiofrequency destruction of the trigeminal ganglion may reduce the frequency of headache clusters, but is associated with significant side effects and nerve damage; techniques such as Gamma Knife disruption and deep brain stimulation are currently in clinical trials.