Methods of brain imaging
Brain Imaging Techniques: Types and Uses
Many brain imaging techniques are used today, each one visualizing your brain in a unique way.
If your doctor has recently ordered a brain imaging scan, you might wonder what your upcoming session will be like or what types of brain imaging techniques might be used.
Experts have gradually improved techniques throughout the years to map out different parts of the brain and various brain functions.
There’s a lot that your doctor can learn from brain imaging, and the information that these scans provide can be helpful in forming a diagnosis and building a treatment plan.
While it may seem stressful to go in for brain imaging, you can take comfort in knowing that this is a safe and painless procedure.
The year 1924 marked the first human electroencephalography (EEG), recorded by German psychiatrist Hans Berger. This early EEG was able to detect electrical waves in the brain that would rise and fall as different brain cells communicated with each other.
Since then, neuroimaging techniques have gotten increasingly more sophisticated, and are an important tool for neurology and mental health specialists.
Commonly used brain imaging techniques are:
- functional magnetic resonance imaging (fMRI)
- computerized tomography (CT)
- positron emission tomography (PET)
- electroencephalography (EEG) and magnetoencephalography (MEG)
- functional near-infrared spectroscopy (fNIRS)
One of the benefits of brain imaging is how easily it can be performed. It doesn’t require invasive steps and often simply involves laying down and being still while the scan takes place around you.
These modern brain imaging techniques enable doctors to map out the regions and functions of your brain in a non-invasive way.
Brain imaging has many roles in health care and makes the jobs of diagnosticians easier. Some uses of brain imaging techniques include:
- identifying the effects of a stroke
- locating cysts and tumors
- finding swelling and bleeding
Doctors use a particular type of imaging method based on what they need to see in your brain. For example, if you are experiencing symptoms of multiple sclerosis (MS), your doctor can order an MRI scan to detect or rule out MS lesions. On the other hand, if you want to check for broken bones, they are more visible on a CT scan.
For example, if you are experiencing symptoms of multiple sclerosis (MS), your doctor can order an MRI scan to detect or rule out MS lesions. On the other hand, if you want to check for broken bones, they are more visible on a CT scan.
Brain imaging can also connect certain mental health issues to biological causes as well. According to a 2020 study, people with high levels of anxiety also displayed differences in brain connectivity when compared to people without anxiety. In addition, brain imaging can detect conditions such as early-stage psychosis.
fMRI
Functional magnetic resonance imaging (fMRI) can detect changes in blood flow and oxygen levels that result from your brain’s activity. It uses the magnetic field of the scanner to affect the magnetic nuclei of hydrogen atoms, so they can be measured and converted into images.
MRIs display anatomic structure and fMRIs measure metabolic function.
fMRIs have many uses, such as:
- assessing brain activity
- finding brain abnormalities
- creating pre-surgical brain maps
CT
A computerized tomography (CT) scan is a series of X-ray images converted into cross-sectional images of your brain. These X-rays are combined to form cross-sectional slices or even a 3-D model of your brain. The results of a CT scan can also provide more detail than a standard X-ray.
These X-rays are combined to form cross-sectional slices or even a 3-D model of your brain. The results of a CT scan can also provide more detail than a standard X-ray.
CT scans can:
- find certain types of brain injuries
- identify cancer
- locate brain swelling or bleeding
- reveal structural brain changes from schizophrenia
PET
A positron emission tomography (PET) scan uses a radioactive tracer that attaches to the glucose in your bloodstream. Since your brain uses glucose as its primary fuel source, the tracer accumulates in areas of higher brain activity.
A PET scan is able to see these tracers and observe how they move and accumulate in your brain. This allows doctors to see trouble spots where glucose isn’t moving correctly.
PET scans can evaluate:
- seizures
- Alzheimer’s
- tumors
EEG
An electroencephalography (EEG) test measures your brain waves. Before the scan, clinicians will attach small electrodes to your scalp that are attached to wires. These electrodes detect electrical activity in your brain and send it to a computer where it creates a graph-like image. Each type of frequency appears on its own line and gives your doctor information about your brain activity.
These electrodes detect electrical activity in your brain and send it to a computer where it creates a graph-like image. Each type of frequency appears on its own line and gives your doctor information about your brain activity.
EEG can detect issues such as:
- anxiety
- head injuries
- epilepsy
- sleep disruption
MEG
Magnetoencephalography (MEG) measures the magnetic field from neuron electrical activity. This type of scan can locate and identify malfunctioning neurons in your brain. Doctors use MEG to evaluate both spontaneous brain activity, as well as neuronal responses triggered by stimuli.
MEG allows doctors to assess areas such as:
- epilepsy sources
- motor areas
- sensory areas
- language and vision
NIRS
Near-infrared spectroscopy (NIRS) monitors your brain’s oxygen saturation. It uses infrared light to detect variations in hemoglobin oxygen levels in your blood. Since oxygen is critical for your brain to function properly, NIRS can assist doctors in any clinical setting where brain oxygen levels may fluctuate.
NIRS is used to monitor:
- brain oxygen levels during cardiac surgery
- brain function and oxygenation levels in preterm infants in a neonatal intensive care unit (NICU) setting
Brain imaging methods offer medical professionals a view of your brain to see if it’s structurally and functionally typical. There are several different brain scan types that map out different parts of your brain, but your specialist will know which one to use for the issue they’re investigating.
Brain imaging techniques do more than simply find medical issues, though. They can also identify brain differences associated with certain mental health conditions, such as schizophrenia, early-stage psychosis, and anxiety disorders.
If your doctor is sending you in for brain imaging, remember that this is a non-invasive procedure that will help your doctor have a clearer understanding of how your brain is functioning. After they receive the results, they can create the best and most accurate treatment plan specific to your needs.
Brain Imaging: What Are the Different Types?
Brain Scans
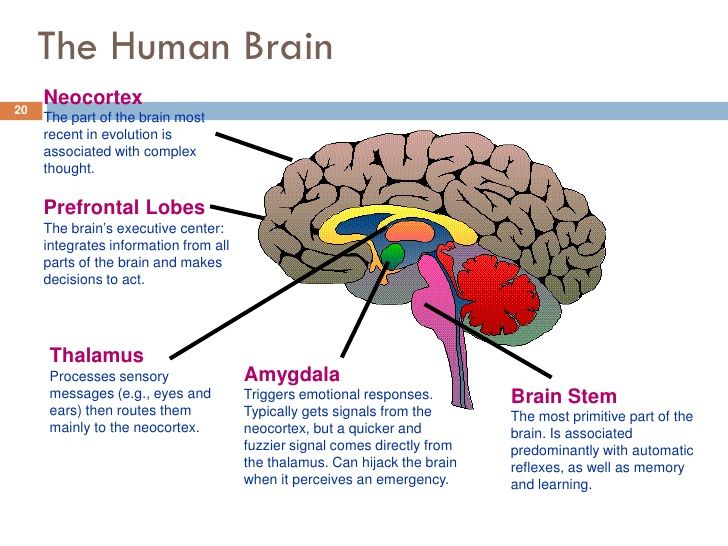
Neuroimaging—or brain scanning—includes the use of various techniques to either directly or indirectly image the structure, function, or pharmacology of the brain. Brain imaging methods allow neuroscientists to see inside the living brain. These methods help neuroscientists understand the relationships between specific areas of the brain and what function they serve.
Neuroimaging falls into two broad categories:
- structural imaging – deals with the structure of the brain and the diagnosis of large-scale intracranial disease—such as a tumor—as well as injury.
- functional imaging – measures an aspect of brain function, often with a view to understanding the relationship between activity in certain brain areas and specific mental functions. It is primarily used as a research tool in cognitive neuroscience and neuropsychology.
The main types of neuroimaging include:
- Computed Tomography Scan (CT)
- Magnetic Resonance Imaging (MRI)
- Functional Magnetic Resonance Imaging (fMRI)
- T1-Weighted MRI
- T2-Weighted MRI
- Diffusion-Weighted MRI (DWI)
- Fluid -Attenuated Inversion Recovery MRI (FLAIR)
- Gradient Record MRI (GRE)
- Positron Emission Tomography Scan (PET)
- Diffusion Tensor Imaging (DTI)
There is also an emerging technology called Transcranial Magnetic Stimulation (TMS), which is not a type of neuroimaging but is related.
Take a look at these slides and descriptions below to get a better understanding of the use of neuroimaging in the brain.
Computed Tomography Scan (CT)
Computed Tomography Scan (CT) scans use a series of X-ray beams passed through the head. The images are then developed on sensitive film. This method creates cross-sectional images of the brain and shows the structure of the brain, but not its function. It is the test of choice to evaluate for the four types of intracranial hemorrhage—subdural, epidural, intracerebral, or subarachnoid, which specifically means bleeding or swelling of the brain during the first 24 to 48 hours after injury. It is also used to detect a skull fracture.
Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging (MRI) scans use echo waves to discriminate among grey matter, white matter, and cerebrospinal fluid. These cans can show if there’s a fracture or bleeding. An MRI may be helpful if a person’s symptoms continue for 48 hours or more after the injury, or if symptoms get worse.
“For diagnostic purposes, and even for characterization of the extent of injury, we predominantly rely upon magnetic resonance imaging. This is our standard imaging modality. With an MRI, our standard measures are good at characterizing whether there's been blood, whether there's been a contusion or a bruise to the brain, or whether there is significant damage to axons that actually result in lesions that we characterize in the brain. It's also, of course, very good at tumor, at stroke, at ischemic damage.” — Deborah Little, PhD, professor, Department of Psychiatry and Behavioral Sciences, director of research for the Trauma and Resilience Center, McGovern Medical School, University of Texas
Functional MRI (fMRI)
Functional magnetic resonance imaging (fMRI) scans are a series of MRIs measuring brain function via a computer’s combination of multiple images taken less than a second apart. For this imaging test, doctors ask patients to do something while in the MRI machine like opening and closing their right hand for 30 seconds and then opening and closing their left hand for 30 seconds.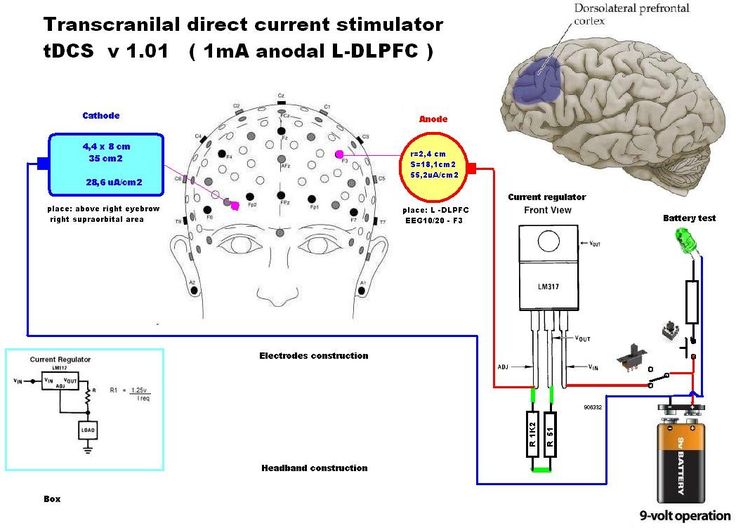 Then, the doctors model the change in signal associated with an increase in blood related to that task. So, areas involved in opening the right hand will show increased signal. This allows images to be created that reveal how the brain does tasks. This is potentially useful in brain injury when the brain structures all appear normal but the brain is functioning in a different way. It is important to know that fMRI is not approved for clinical use for diagnosis of TBI.
Then, the doctors model the change in signal associated with an increase in blood related to that task. So, areas involved in opening the right hand will show increased signal. This allows images to be created that reveal how the brain does tasks. This is potentially useful in brain injury when the brain structures all appear normal but the brain is functioning in a different way. It is important to know that fMRI is not approved for clinical use for diagnosis of TBI.
T1-Weighted MRI
The T1-Weighted MRI is the standard imaging test and part of every general MRI exam. It provides doctors with a very clear view of brain anatomy and structure. It can also show damage in brain injury but generally only when the damage is very significant.
T2-Weighted MRI
The T2-Weighted MRI is also a standard part of every MRI exam. But unlike T1-weighted imaging, the T2 allows visualization of severe diffuse axonal injury such as what is expected following severe TBI. T2-weighted scans are used to measure white matter and cerebrospinal fluid in the brain, as this type of scan is more suited to measure fluid rather than soft tissues.
Diffusion Weighted MRI (DWI)
Diffusion Weighted MRI (DWI) shows alterations in tissue integrity— the ability of body tissues to regenerate and/or repair to maintain normal physiological processes. In ischemic injury—such as many types of stroke or when blood is not able to get to all parts of the brain—there is a chemical reaction in the cells. As the cells die because of lack of blood flow (with oxygen), there is an increase in sodium and this changes (increases) the amount of water in the tissue. DWI is very sensitive to this change. In fact, using DWI, doctors can identify a stroke or ischemic injury within seconds of occurrence.
Fluid-Attenuated Inversion Recovery (FLAIR) MRI
Fluid-Attenuated Inversion Recovery (FLAIR) MRI is also sensitive to water content in brain tissue. This is very useful in patients who have reductions in brain tissue following an injury. Most commonly, however, FLAIR is used to visualize alterations in tissue in diseases such as multiple sclerosis.
Gradient Record MRI (GRE)
Gradient Record MRI (GRE) shows blood or hemorrhaging in the brain tissue. This is very important in acute brain injury. CT scans are also very useful in this stage but sometimes miss very small bleeds—or so called microbleeds—in the brain. Other types of MRI cannot easily detect these types of injury, so GRE is particularly useful to physicians who suspect these injuries may be present in a patient.
Positron Emission Topography (PET)
Positron Emission Tomography Scan (PET) measures brain metabolism. Different applications of PET allow one to "see" pathology associated with Alzheimer's disease, for instance, that cannot be visualized any other way. Used in a different way, PET also allows doctors to see how different areas of the brain use oxygen or glucose—both very important in understanding not just what the damage might look like but also how the brain provides energy to itself. In brain injury research, PET scans are used to identify how metabolic processes may be changed after a brain injury. For instance, the brain may absorb less glucose (sugar) after a brain injury, which may affect how an individual processes information. PET has recently been used in tandem with MRI to identify (with a high degree of spatial accuracy) specific brain regions that may be experiencing metabolic changes after injury.
For instance, the brain may absorb less glucose (sugar) after a brain injury, which may affect how an individual processes information. PET has recently been used in tandem with MRI to identify (with a high degree of spatial accuracy) specific brain regions that may be experiencing metabolic changes after injury.
“PET scans look at metabolism in the brain. We inject the radiotracer glucose, and the glucose is utilized in the brain, and areas of the brain that use more glucose light up stronger, and areas that use less glucose do not light up as strong. So, we can see areas of the brain that are potentially damaged and not utilizing glucose as much as they should be.” — Gerard Riedy, MD, PhD, neuroradiologist, National Intrepid Center of Excellence (NICoE), Walter Redd National Military Medical Center Bethesda
Diffusion Tensor Imaging (DTI)
Diffusion Tensor Imaging (DTI) shows white matter tracts in brain tissue. These tracts allow different parts of the brain to talk to each other. Think of the brain as if it were a computer. With DTI, doctors can see and measure the "cables" connecting parts of the brain. DTI can provide information about damage to parts of the nervous system as well as about connections among brain regions.
Think of the brain as if it were a computer. With DTI, doctors can see and measure the "cables" connecting parts of the brain. DTI can provide information about damage to parts of the nervous system as well as about connections among brain regions.
Transcranial Magnetic Stimulation (TMS)
Although not an neuroimaging technique, per se, TMS is an FDA-cleared noninvasive treatment that uses gentle magnetic pulses to activate areas of the brain involved in mental health and addiction conditions. The treatment is well-tolerated, has no systemic side effects.
“Though still in the research stages, TMS may be a useful non-invasive brain stimulation tool to study the effects of targeted TMS treatment on individuals with chronic symptoms after brain injury.” — Cooper Hodges, PhD, Polytrauma Research fellow at the DC VA hospital
Posted on BrainLine April 22, 2011. Reviewed October 25, 2021.
NEUROIMAGING METHODS IN THE DIAGNOSTICS OF PATHOLOGICAL CHANGES IN THE BRAIN IN CHILDREN | Maratskaya
1. Barashnev, Yu.I. Perinatal neurology / Yu.I. Barashnev. - 2nd ed. - M. : Triada-X, 2005. - 672 p.
Barashnev, Yu.I. Perinatal neurology / Yu.I. Barashnev. - 2nd ed. - M. : Triada-X, 2005. - 672 p.
2. Smirnova, T.A. Neurosonography in the diagnosis of cerebral lesions in children with congenital viral infection / T.A. Smirnova, M.G. Khrameshina // Sonoace Int. - 2002. - No. 10. – P. 52–56.
3. Features of morbidity and physical development of young children with perinatal CNS lesions depending on the level of neuropsychic development / O.M. Filkina [et al.] // Palliative. medicine and rehabilitation. - 2010. - No. 3. – p. 19-22.
4. Veltishchev, Yu.E. The health status of children and the overall strategy for disease prevention: a lecture for physicians: adj. to the journal "Russian Bulletin of Perinatology and Pediatrics" / Yu.E. Veltishchev. - M., 1994. - 67 p.
5. Shabalov, N.P. Neonatology: in 2 volumes / N.P. Shabalov. - 4th ed., Rev. and additional - M. : MEDpress-inform, 2006. - T. 1. - 608 p.
6. Neuroimaging of brain organogenesis disorders / А. К. Akhmetbaeva [et al.] // Science and health care. - 2012. - No. 5. – P. 73–76. nine0003
К. Akhmetbaeva [et al.] // Science and health care. - 2012. - No. 5. – P. 73–76. nine0003
7. Belov, S.A. Magnetic resonance imaging of the brain of children aged from the neonatal period to 15 years / S.A. Belov, V.I. Shumsky, T.A. Akhadov // Almanac clinical. medicine. - 1999. - No. 2. - S. 271-280.
8. Zhukova, L.I. Echographic picture of inflammatory diseases of the brain and their consequences in infants / L.I. Zhukova, O.S. Zueva, T.M. Ryabov // Protection of motherhood and childhood. - 2013. - No. 1 (21). – P. 59–63.
9. Dvoryakovsky, I.V. Ultrasonic anatomy of a healthy child / I.V. Dvoryakovsky. - M. : Firma STROM, 2009. – 384 p.
10. Radiation diagnostics in pediatrics / National project "Health"; editor: A.Yu. Vasiliev, S.K. Ternovoy. - M. : GEOTAR-Media, 2010. - 368 p. – (National Guidelines for Radiation Diagnostics and Therapy).
11. Mikhailov, M.K. The role and place of radiation diagnostics in modern conditions / M.K. Mikhailov // Prakt. medicine. - 2010. - No. 2. – P. 15–19.
medicine. - 2010. - No. 2. – P. 15–19.
12. Ternovoy, S.K. Modern computed tomography in clinical medicine / S.K. Ternova, I.Yu. Nasnikova, S.P. Morozov // Kremlin. medicine. Wedge. vestn. - 2008. - No. 2. – p. 9-13.
13. Neonatal MRI to predict neurodevelopmental outcomes in preterm infants / L.J. Woodward [et al.] // The New England J. of Med. - 2006. - Vol. 355. – P. 685–694.
14. Kleshchenko, E.I. The use of diffusion-weighted magnetic resonance imaging to detect hypoxic-ischemic brain lesions in newborns / E.I. Kleshchenko, E.V. Shimchenko, K.F. Goloseev // Pediatrician. pharmacology. - 2014. - T. 11, No. 1. – P. 69–73.
15. Vatolin, K.V. Ultrasound diagnosis of brain diseases. Children's ultrasound diagnostics / K.V. Vatolin; under total ed. M.I. Pykova, K.V. Vatolin. - M. : Vidar, 2001. - 680 p. nine0003
16. Peculiarities of application of methods of radiation diagnostics in pediatric practice / G.E. Trufanov [et al.] // Vestn. modern wedge. medicine. - 2013. - V. 6, no. 6. – P. 48–54.
- 2013. - V. 6, no. 6. – P. 48–54.
17. Zubareva, E.A. Neurosonography in children of early age / E.A. Zubareva, E.A. Ulezko. - Minsk: Paradox, 2004. - 192 p.
18. Ulezko, E.A. Neonatal encephalopathy and birth traumatic brain injury: clinical and neurophysiological studies, differential diagnosis, pathomorphology, treatment / E.A. Ulezko, G.G. Shanko, M.K. Nedzved. – Minsk : Harvest, 2009. – 320 s.
19. Greenhalch, T. Fundamentals of evidence-based medicine: per. from English. / T. Greenhalch. - M. : GEOTAR-MED, 2004. - 240 p.
20. Lyutaya, E.D. Radiation diagnostics in the mirror of evidence-based medicine / E.D. Fierce // Vestn. Volgograd. state honey. university - 2006. - No. 4. – P. 20–26.
21. Bokonbaeva, S.J. Neurosonography of premature newborns with low birth weight / S.J. Bokonbaeva, N.V. Vychigzhanina // Vestn. Kyrgyz.-ros. Slavs. university - 2011. - T. 11, No. 3. – pp. 87–91.
22. Finger, A.B. Hypoxic-ischemic encephalopathy of newborns / A.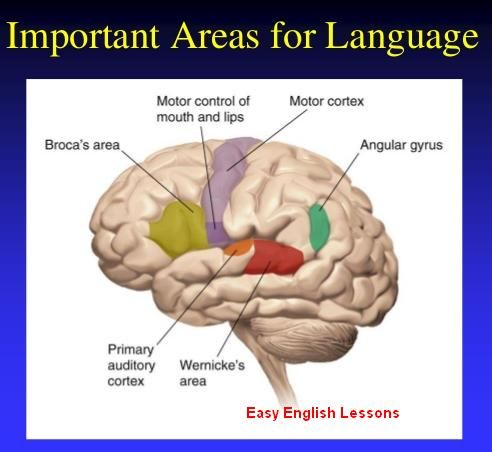 B. Finger, N.P. Shabalov. - St. Petersburg. : Peter, 2000. - 224 p.
B. Finger, N.P. Shabalov. - St. Petersburg. : Peter, 2000. - 224 p.
23. Rennie, J.M. Neonatal cerebral ultrasound / J.M. Rennie. - UK : Cambridge University Press, 2000. - 245 p.
24. Ultrasonography in neuropediatrics. New opportunities and perspectives: ultrasonography. atlas / A.S. Job [and others]. - St. Petersburg. : Petrovsky and K°, 1997. - 160 p.
25. Krivtsova, L.A. Neuroimaging methods in predicting outcomes of cerebral ischemia in children of the first year of life / L.A. Krivtsova, V.V. Belsky // Vestn. new honey. technologies. - 2013. - T. 20, No. 2. - S. 423-427. nine0003
26. Radchenko, E.V. Influence of intrauterine hypoxia and intrauterine infections on the results of neurosonography and electroencephalography in children / E.V. Radchenko // Intern. magazine experimental education. - 2015. - No. 5. – P. 39–40.
27. Clinical guide to ultrasound diagnostics / ed. B.V. Mitkova, M.V. Medvedev. - M. : Vidar, 1997. - T. 3. - 320 p.
28. Neuroradiology of childhood / A.N. Konovalov [i dr.]. - M. : ANTIDOR, 2001. - 436 p.
Neuroradiology of childhood / A.N. Konovalov [i dr.]. - M. : ANTIDOR, 2001. - 436 p.
29. White matter injury in the premature infant: a comparison between serial cranial sonographic and MR findings at term / T.E. Inder [et al.] // Am. J. Neuroradiol. - 2003. - Vol. 24, No. 5. - P. 805–809.
30. Comparison of findings on cranial ultrasound and magnetic resonance imaging in preterm infants / E.F. Maalouf [et al.] // Pediatrics. - 2001. - Vol. 107, No. 4. - P. 719–727.
31. Ternovoy, S.K. The development of computed tomography and the progress of radiation diagnostics / S.K. Ternovoy, V.E. Sinitsyn // Therapist. archive. - 2006. - No. 1. – P. 10–13. nine0003
32. Khoruzhik, S.A. Quality indicators of computed tomographic images / S.A. Khoruzhik, I.G. Tarutin, A.N. Mikhailov // Topical issues of radiation imaging : Sat. scientific works dedicated to 70th anniversary of acad. National acad. Sciences of Belarus A.N. Mikhailov and the 55th anniversary of the department.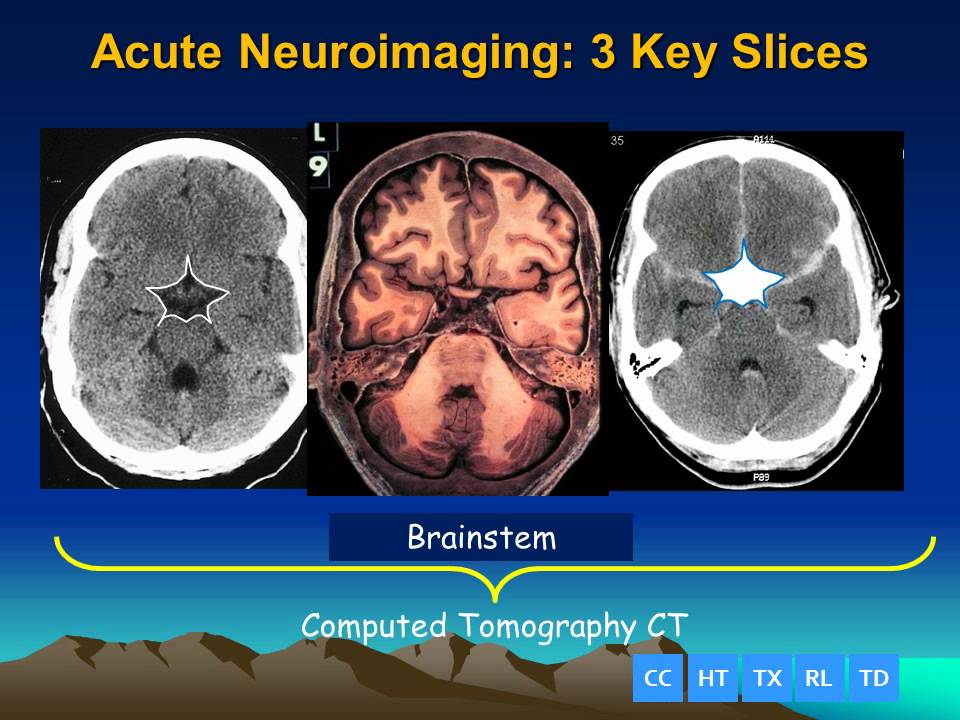 radiology Belarus. honey. acad. last plom. education. - Minsk: BelMAPO, 2006. - S. 28–33.
radiology Belarus. honey. acad. last plom. education. - Minsk: BelMAPO, 2006. - S. 28–33.
33. Pediatric CT: strategies to lower radiation dose / C. Zacharias [et al.] // Am. J. Roentgenol. - 2013. - Vol. 200, N 5. - P. 950–956.
34. Shestova, E.P. The value of routine MRI studies of the brain in motor disorders in young children (lack of evidence is not proof of absence) / E.P. Shestova, S.K. Evtushenko, E.A. Savchenko // Intern. nevrol. magazine - 2014. - No. 3 (65). – P. 176– 177.
35. Anikin, A.V. Modern possibilities of magnetic resonance imaging in pediatrics / A.V. Anikin, M.Z. Karkashadze, G.V. Kuznetsova // Vopr. diagnostics in pediatrics. – 2009. - No. 2. – P. 50–54.
36. Possibilities of assessing the motor and sensory pathways of the brain using diffusion-tensor tractography in children with cerebral palsy / A.M. Mamedyarov [et al.] // Vestn. Ros. acad. honey. Sciences. - 2014. - No. 9–10. – P. 70–76.
37. Shekhtman, A.G. Application of the method of magnetic resonance imaging in the clinical assessment of brain structures in normal conditions and in tumor pathology / A.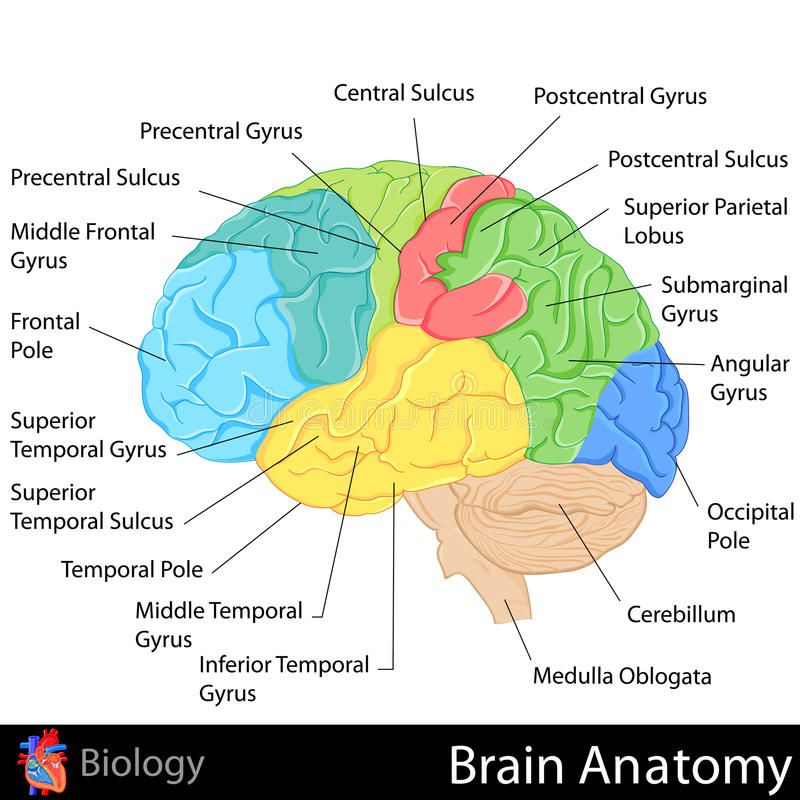 G. Shekhtman, O.Ya. Malygina // Med. almanac. - 2014. - No. 5 (35). - S. 174-178. nine0003
G. Shekhtman, O.Ya. Malygina // Med. almanac. - 2014. - No. 5 (35). - S. 174-178. nine0003
38. Rinkk, P.A. Magnetic resonance in medicine. The main textbook of the European Forum on Magnetic Resonance / P.A. Rinkk; per. from English. V.E. Sinitsyna, D.V. Ustyuzhanin; ed. V.E. Sinitsyn. - M. : GEOTAR-MED, 2003. - 256 p. Newborn brain imaging0090
S. Todd Sorokan, Ann L. Jefferies, Stephen P. Miller
Canadian Pediatric Society, Committee on Fetuses and Newborns, Ottawa, Ontario
. Although ultrasonography (ultrasound) and computed tomography (CT) may provide some information, magnetic resonance imaging (MRI) is currently the main method of brain imaging because MRI is the most sensitive technology for detecting and quantifying brain abnormalities, which does not expose children to radiation. The following describes the principle, role, and limitations of these three imaging modalities and provides recommendations for their use in neonatal examinations.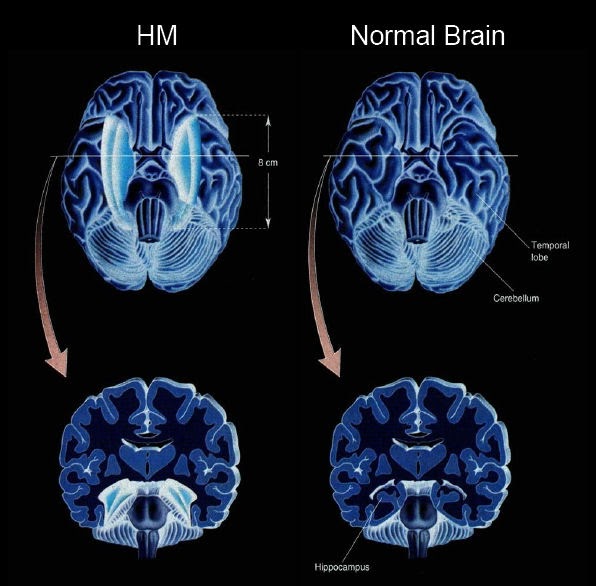 ..
..
Brain imaging is an important step in the diagnosis and treatment of sick newborns and especially for children with neonatal encephalopathy (NE), seizures, unexplained sleep apnea, infections, metabolic disorders, birth trauma, suspected structural abnormalities of the brain. The information obtained from the images can help establish the underlying diagnosis, determine treatment and predict the development of the nervous system...
DIAGNOSIS METHODS
Ultrasound (US)
Ultrasound uses high-frequency sound waves emitted by a transducer to bounce off body structures. Returning sound waves (echoes) create an image based on the frequency and strength of the signal, and the time it takes for the transducer to return.
Computed tomography (CT)
CT combines a series of x-ray images using a computer to create a transverse image. Although computed tomography of the head has been used to detect hemorrhage, brain injury, and edema secondary to hypoxic-ischemic injury, sinus venous thrombosis, masses, and structural abnormalities, MR imaging has replaced CT as the imaging modality of choice in most of these indications. nine0003
nine0003
Magnetic Resonance Imaging (MRI)
MRI creates images using the body's natural magnetic properties. The magnetic field of the scanner forms the axes of the protons of the hydrogen atoms, which evenly line up. Energy impulses from radio waves knock these axes out of order, followed by reconstruction and relaxation when these energy impulses cease...
RECOMMENDATIONS
there are signs of encephalopathy, or a suspected brain injury, or some kind of anomaly. nine0003
2. Ultrasound (ultrasound) may be useful as a first imaging modality in the presence of experienced radiologists. Although ultrasonography may help detect bleeding, severe structural abnormalities, or calcification, it is not recommended as the sole examination of newborns who have evidence of moderate or severe encephalopathy, seizures, or other neurological symptoms suggestive of congenital metabolic problems, traumatic brain injury, or malformations of the brain, because the extent of the lesion is underestimated compared to the level of accuracy that an MRI examination provides. nine0003
nine0003
3. Computed tomography (CT) may be useful for initial evaluation in emergency situations when MRI is not available, when the child is too unstable to undergo MRI, or when trauma or skull fracture is suspected.
4. For children with hypoxic-ischemic encephalopathy, MRI should be performed on the 3-5th day of life or after undergoing a course of therapeutic hypothermia, as soon as the child has warmed up. Timely MR imaging is critical in determining an accurate diagnosis, in advising parents about the prognosis and possible consequences, and in prescribing an appropriate course of treatment. A follow-up MRI examination should be performed between the ages of 10 and 14 days if the images and clinical signs do not match, or when the diagnosis is not fully established. nine0003
5. When CT is used to evaluate children with hypoxic-ischemic encephalopathy, it should be performed within 72 hours of suspected stroke, ideally within 72 ± 12 hours. Follow-up MRI is also recommended.
 detection of intracranial hemorrhage in infants with a history of acute encephalopathy, significant birth trauma, and evidence of low hematocrit or coagulopathy
detection of intracranial hemorrhage in infants with a history of acute encephalopathy, significant birth trauma, and evidence of low hematocrit or coagulopathy