Vitamin d deficiency anxiety
Does Vitamin D Boost Mental Health?
Written by WebMD Editorial Contributors
Medically Reviewed by Dan Brennan, MD on March 30, 2021
In this Article
- Impact of Vitamin D Deficiency on Mental Health
- Symptoms of Vitamin D Deficiency
- Vitamin D and Depression
- Treating Vitamin D Deficiency
Vitamin D deficiency leads to both medical and psychosocial problems. It has re-emerged as an epidemic that mainly affects the minority populations.
Impact of Vitamin D Deficiency on Mental Health
The body needs Vitamin D at the proper level for it to function as it should.
How Vitamin D Works In The Body
Your muscles, heart, brain, and immune system have vitamin D receptors. The body transports the vitamin to the kidneys and liver, where it converts into an active hormone. In this form, it assists the body in absorbing calcium.
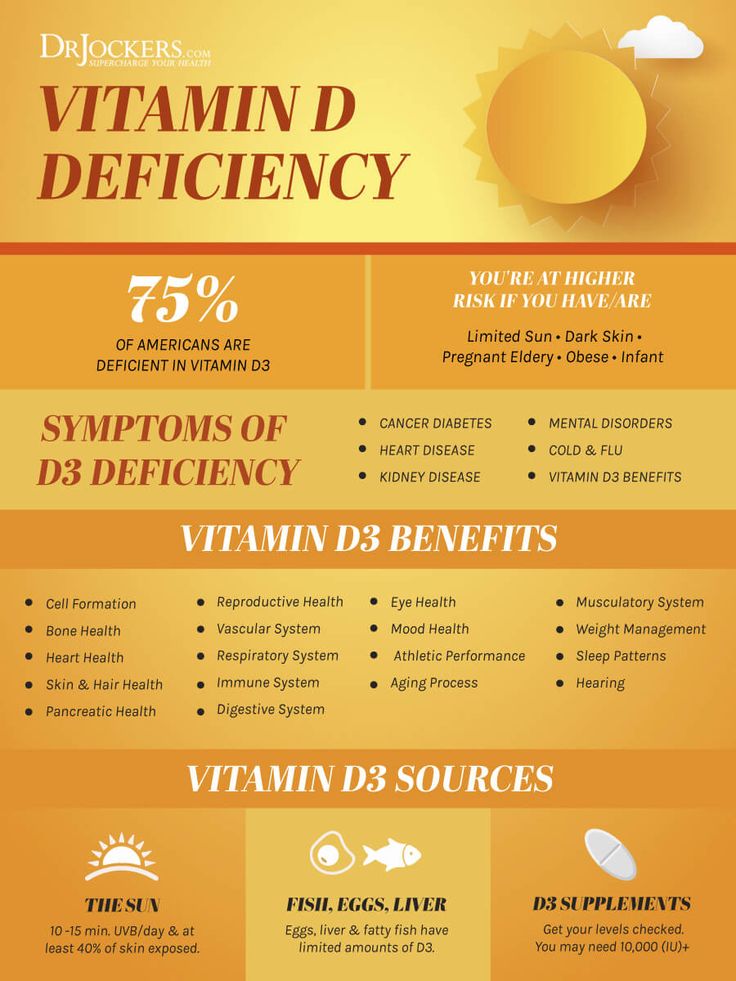
Your body acquires vitamin D through sun exposure. Certain foods and supplements can also be sources of vitamin D. Dark-skinned people have a high level of melanin.
It’s the component that determines coloring in the human and animal world. This pigmentation prevents the skin from absorbing vitamin D correctly.
How Vitamin D Deficiency Leads to Mental Health Effects
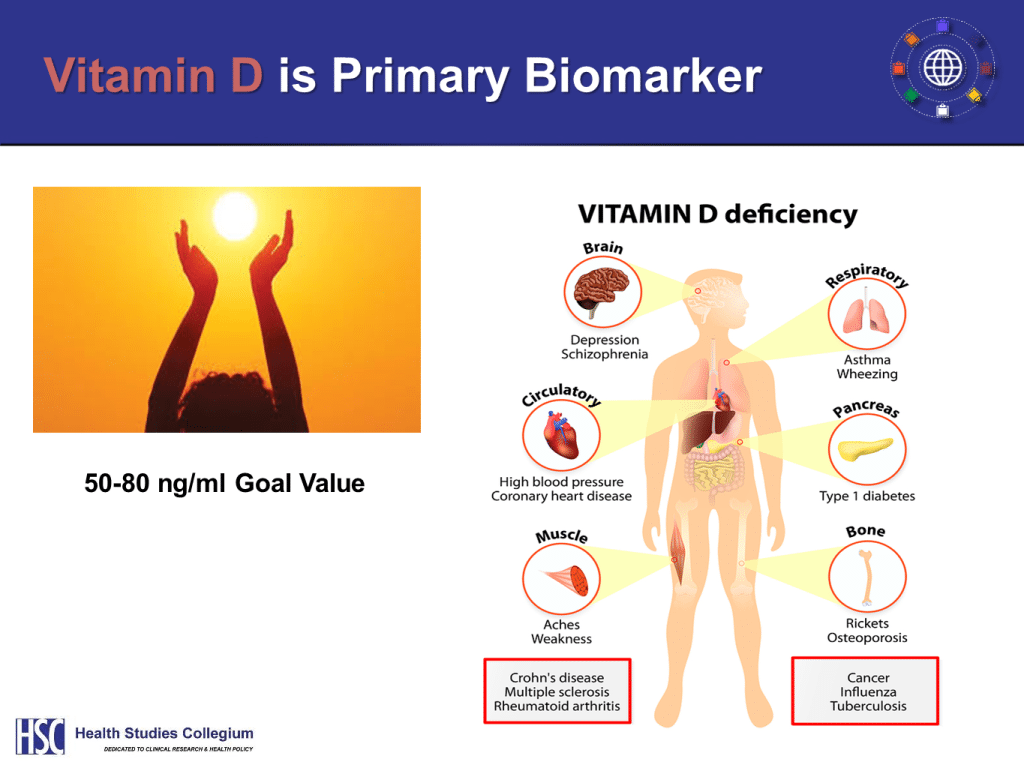
Low levels of the vitamin may contribute to schizophrenia in adults, depression, and seasonal affective disorder. Other health problems that can arise from the deficiency include:
- Low bone density
- Bone softening
- Heart disease
- Rickets in children
- Cancer
Those At Risk of Vitamin D Deficiency
A large portion of the population is at risk of vitamin D deficiency. People who live far from the equator, and those with conditions like liver disease, renal disease, and celiac, are at a higher risk. The elderly and people with darker skin also fall in this category.
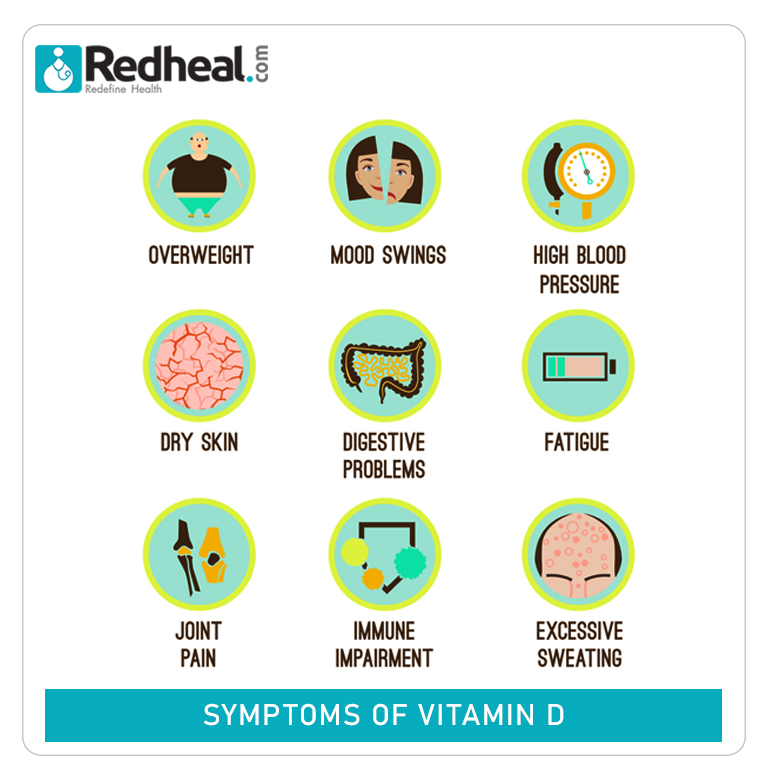
Symptoms of Vitamin D Deficiency
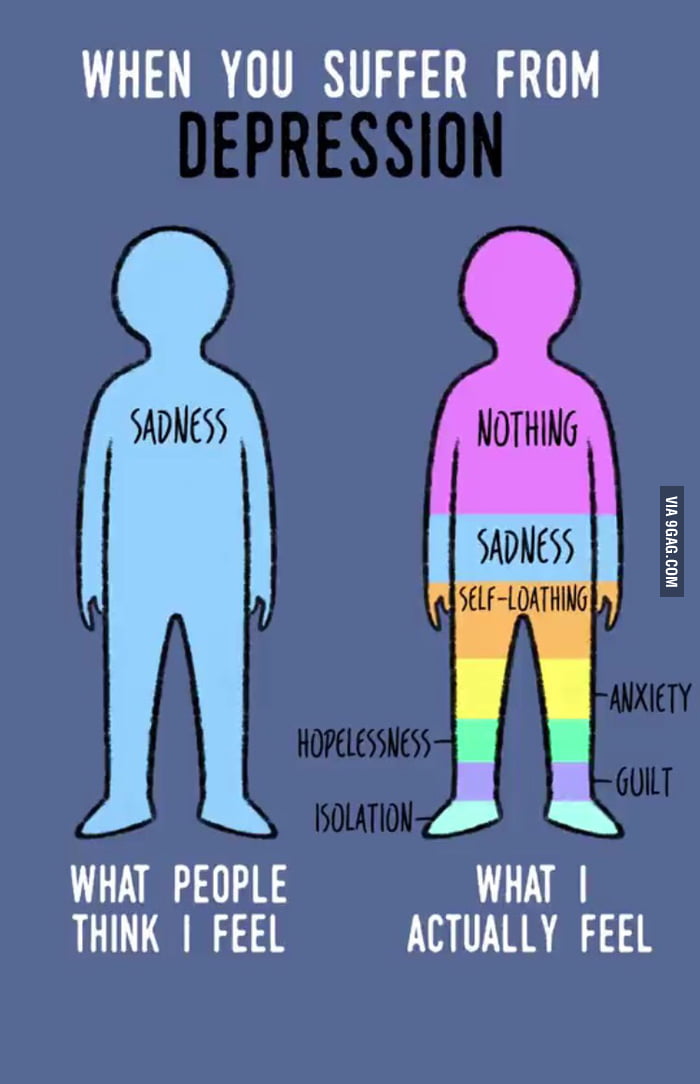
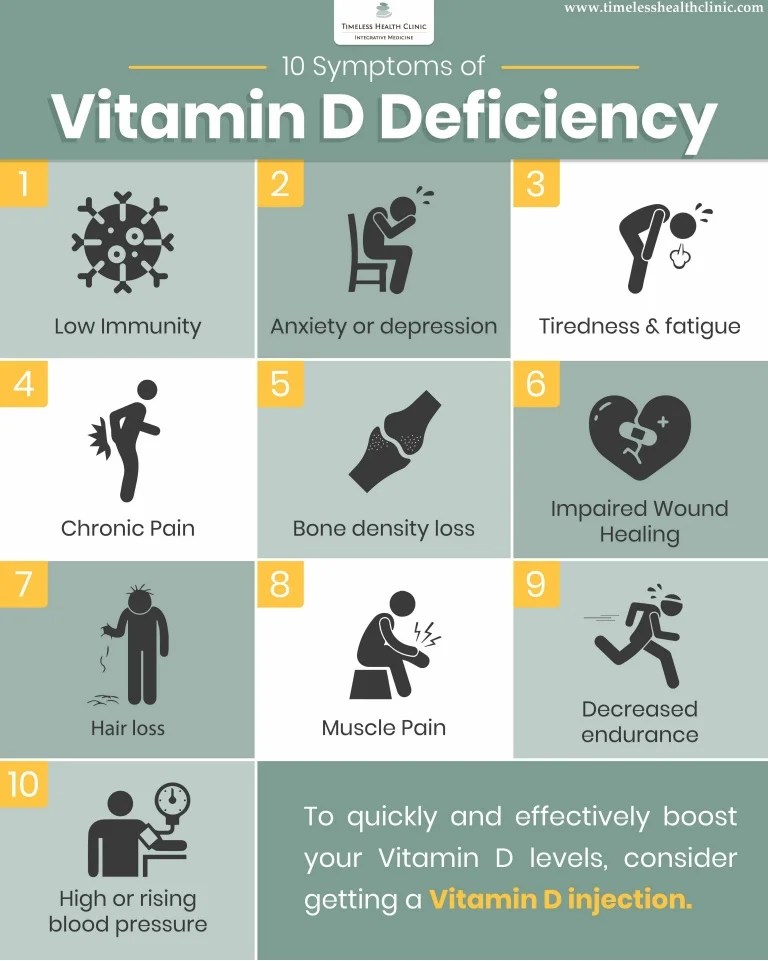
Vitamin D deficiency presents similar symptoms to those of depression:
- Mood changes accompanied by overwhelming feelings of hopelessness, sadness, and hopelessness
- Fatigue
- Forgetfulness
- Loss of interest in activities that previously sparked excitement
- Suicidal thoughts
- Anxiety
- Loss of appetite
- Excessive weight loss or gain
- Trouble sleeping
If you experience any of these symptoms similar to depression, have your vitamin D levels checked. Your doctor will do a test to determine the level of the vitamin in your blood.
For depression diagnosis, you may have to complete a self-assessment test. A blood test can't diagnose depression but may test other conditions that cause depressive symptoms.
Vitamin D and Depression
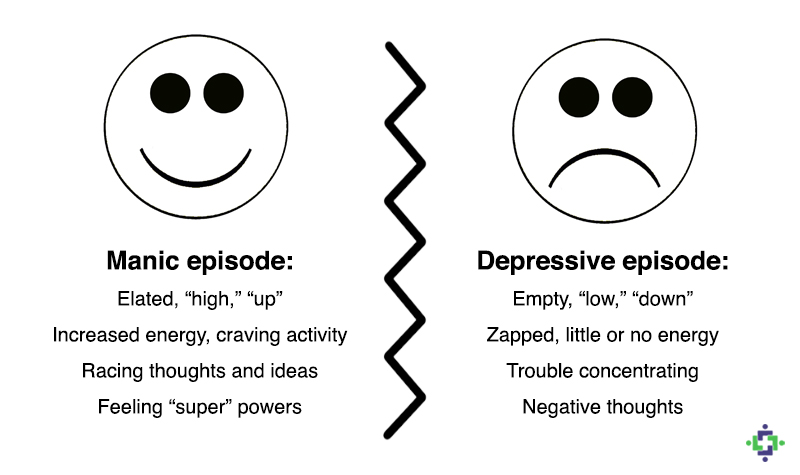
Depression is a medical condition that changes the thoughts, feelings, or behaviors of an individual.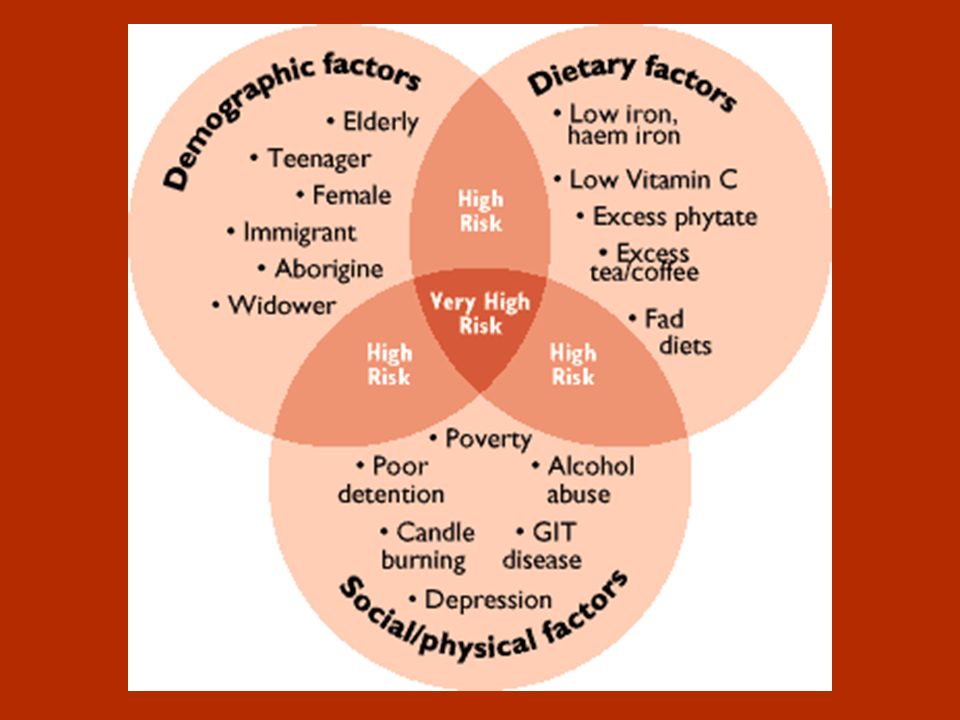 Symptoms include:
Symptoms include:
- Loss of interest in activities the individual previously liked
- Isolation and withdrawal
- Lack of concentration and focus
- Difficulty sleeping or eating
- Suicidal tendencies or ideations
What Research Shows
Studies on vitamin D supplementation and depression show a relationship between the two.
The only limitation of the studies is that they don’t prove that vitamin D deficiency causes depression. People with depression may have lower vitamin D levels, but the deficiency did not cause the illness.
How Vitamin D Deficiency is Linked to Depression
If the cause of depression was a lack of the vitamin, then supplementation would help reduce the signs and symptoms. An increase in the levels of the vitamin would also prevent depression from occurring, but this is not the case.
There is another possible explanation of the correlation between vitamin D deficiency and depression. Many groups at a high risk of depression are also likely to have vitamin D deficiency.
Many groups at a high risk of depression are also likely to have vitamin D deficiency.
Adolescents, people with obesity, the elderly, and those with chronic illnesses are the most prone to having vitamin D deficiency. They are also at a higher risk of depression.
Possible Causes for This Correlation
As noted above, some symptoms of clinical depression include withdrawal and social isolation. Since these individuals spend less time outside, they lack the much-needed exposure to process enough vitamin D.
Severe cases of depression make it hard for the person to get out of bed or take part in outdoor activities. Social isolation only makes the symptoms worse. This is why healthcare providers encourage people with depression to spend more time with others.
Additionally, people dealing with depression have a hard time taking care of themselves properly. They may not eat properly and may not get vitamin D supplements for themselves. Depression alters their behavior and thought processes, making them engage in behaviors that worsen vitamin D deficiency.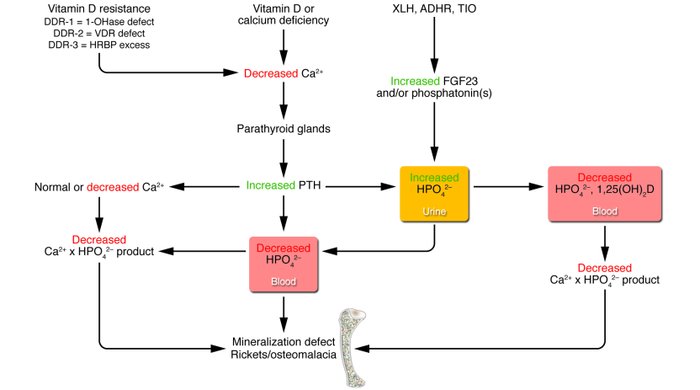
Treating Vitamin D Deficiency
The best way to treat vitamin D deficiency is to:
- Increase your exposure to the sun
- Increase your intake of food fortified with vitamin D
- Take supplements
Your doctor may also give you antidepressants to treat depression. You can take them separately or with dietary supplements. Join a support group, exercise regularly and practice proper sleeping habits.
Preventing Vitamin D Deficiency
Vitamin D is as vital for mental health as it's essential for physical health. There is sufficient research to show that not having enough of the vitamin can lead to depression-like symptoms. People with depression have higher chances of having vitamin D deficiency. Prevent this from happening by adding food rich in Vitamin D to your diet and getting adequate sun exposure.
Is Vitamin D Important in Anxiety or Depression? What Is the Truth?
Introduction
Depression and anxiety are mood disorders that affect individuals’ daily lives and health status with their social and economic dimensions, which are frequently observed.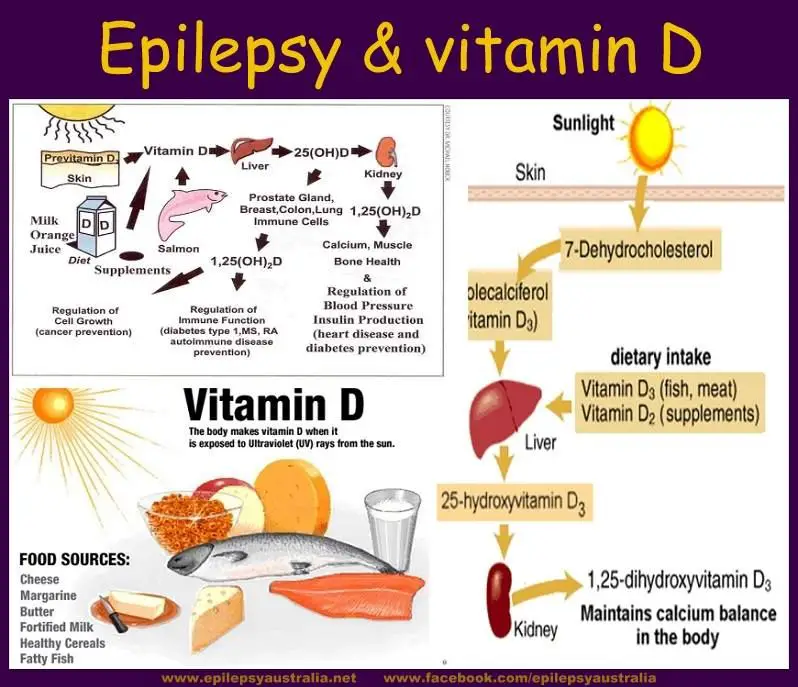 Identifying the factors that cause these mood disorders is a cornerstone to prevent or delay their occurrence. It is important to provide disease management for individuals diagnosed with mood disorders.
Identifying the factors that cause these mood disorders is a cornerstone to prevent or delay their occurrence. It is important to provide disease management for individuals diagnosed with mood disorders.
It has been determined that oxidative stress and inflammation are involved in the pathophysiology of these mood disorders along with many diseases [1]. Thereupon, the relationship between antioxidant and immunomodulatory nutrients and these diseases was examined. In this review, it is aimed to explain the place of vitamin D in the pathophysiology of depression and anxiety, the effect of vitamin D supplementation, and its interactions with the drugs used.
Vitamin D
Vitamin D is a fat-soluble vitamin that has been reported to have efficacy in many tissues, as well as its effects on calcium-phosphate homeostasis and bone health. Approximately one-fifth of vitamin D is provided by dietary intake, and the remaining 80% is synthesized from 7-dehydrocholesterol in the skin by ultraviolet rays [2]. Then, calcidiol, which is the serum form of the vitamin, is hydroxylated in the liver with the enzyme 25-hydroxylase (CYP2R1), and calcidiol is re-hydroxylated in the kidney and brain with the enzyme 1-α-hydroxylase (CYP27B1) and turns into 1,25 (OH)2 cholecalciferol, also called calcitriol, which is the active form of the vitamin [3]. Vitamin D synthesis and active form formation stages are presented in Fig. 1. This active form binds to vitamin D receptors located on cell membranes of many tissues to mediate gene transcription and non-genomic reactions [2].
Then, calcidiol, which is the serum form of the vitamin, is hydroxylated in the liver with the enzyme 25-hydroxylase (CYP2R1), and calcidiol is re-hydroxylated in the kidney and brain with the enzyme 1-α-hydroxylase (CYP27B1) and turns into 1,25 (OH)2 cholecalciferol, also called calcitriol, which is the active form of the vitamin [3]. Vitamin D synthesis and active form formation stages are presented in Fig. 1. This active form binds to vitamin D receptors located on cell membranes of many tissues to mediate gene transcription and non-genomic reactions [2].
Vitamin D synthesis and active form formation stages
Full size image
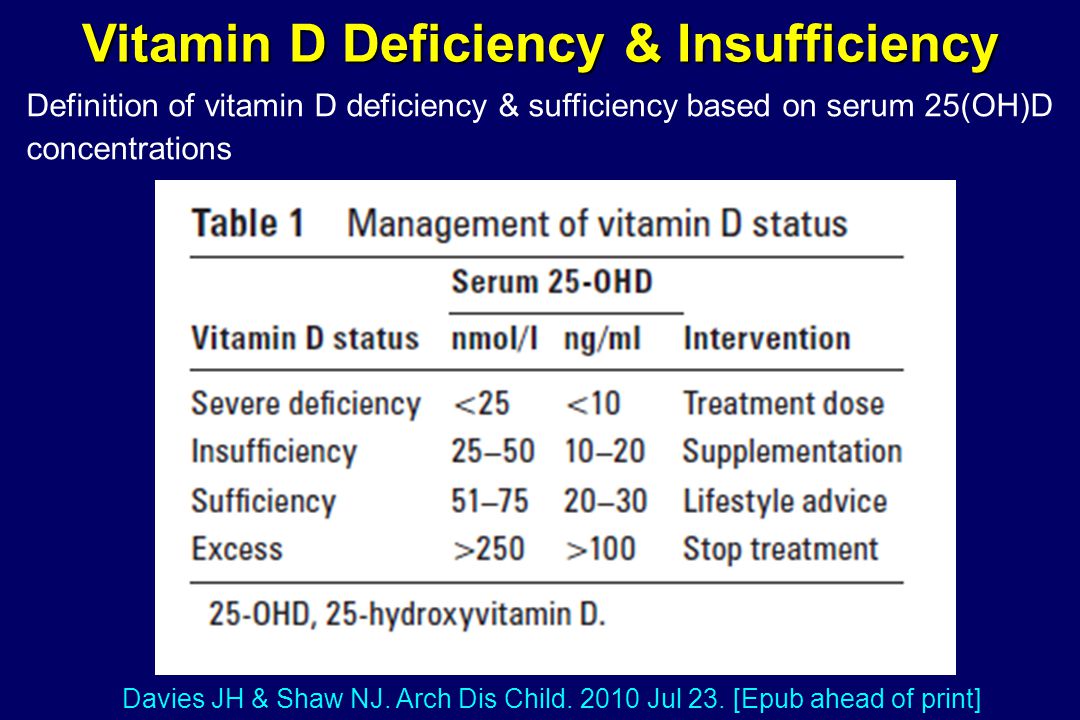
Serum 25(OH) cholecalciferol (calcidiol) level is taken into account to evaluate the sufficiency status for vitamin D. However, there is no international consensus on the cut-off points of this parameter for proficiency/inability. The cut-off points determined by different authorities vary. The data generated on this subject are presented in Table 1 [4, 5].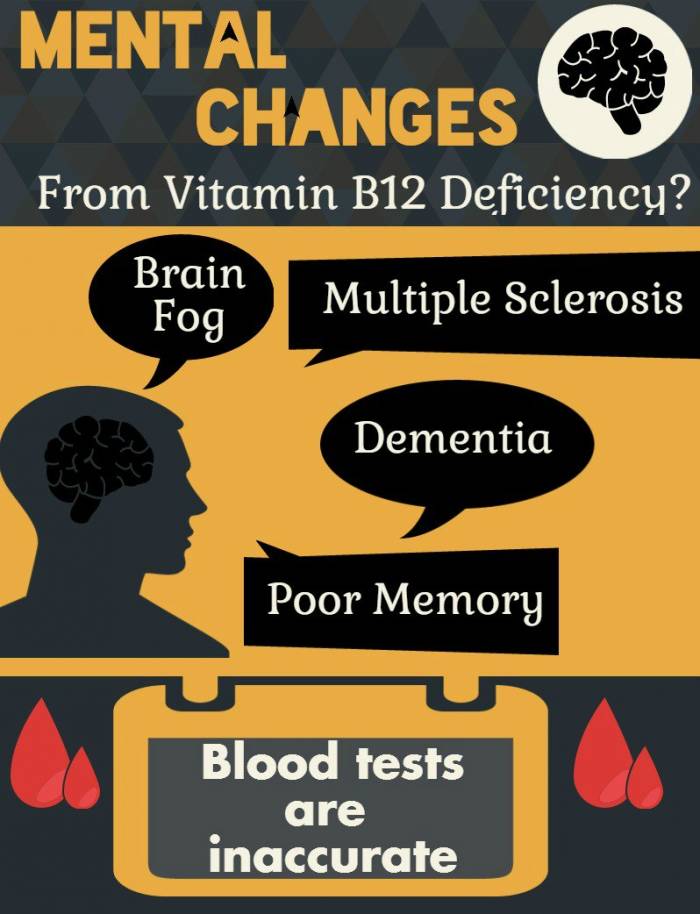
Full size table
When the causes of vitamin D deficiency are examined, it may be caused by decreased exposure to sunlight, decreased endogenous synthesis with the deterioration in liver-kidney functions, malabsorption (cystic fibrosis, short bowel syndrome, gastric bypass, chronic pancreatic insufficiency, etc.), the drugs used (phenobarbital, carbamazepine, dexamethasone, nifedipine, spironolactone, clotrimazole, and rifampin), increased catabolism, and genetic resistance to vitamin D [5].
Adequate intake of vitamin D is particularly dependent on sunlight. Synthesis occurs with short-term (15–20 min) direct exposure to sunlight. In longer exposure to sunlight, compounds called lumesterol and which do not show vitamin D activity are formed. However, vitamin D synthesis levels in exposure to sunlight are affected by various factors such as skin pigmentation, sunscreen use, latitude, season, and age, and dietary or supplemental intake does not directly contribute to 25(OH) cholecalciferol levels. It is emphasized that factors such as body mass index, body fat percentage, and calcium intake are also effective on serum vitamin D levels [6]. When the prevalence of vitamin D insufficiency is examined, it is reported that 40% of Europe has vitamin D insufficiency, and 13% of them have severe insufficiency [7].
It is emphasized that factors such as body mass index, body fat percentage, and calcium intake are also effective on serum vitamin D levels [6]. When the prevalence of vitamin D insufficiency is examined, it is reported that 40% of Europe has vitamin D insufficiency, and 13% of them have severe insufficiency [7].
Vitamin D receptors located in many tissues are also located in the brain specifically in the prefrontal cortex, hippocampus, cingulate gyrus, thalamus, hypothalamus, and substantia nigra. These regions are of extra importance for this research as they are defined in the pathophysiology of depression [8]. It has also been determined that the vitamin D activating enzyme 1-α-hydroxylase (CYP27B1) is widely distributed in many different cell types of many brain regions, especially in neurons in the amygdala and glial cells in the hypothalamus. This distribution strengthens the relationship between vitamin D and neuropsychiatric diseases. It is reported that the active form of vitamin D can cross the blood–brain barrier, which increases the possibility of vitamin D being directly or indirectly involved in brain and cognitive functions [9].
There are many studies in the literature reporting that vitamin D deficiency was associated with symptoms of depression and anxiety [10,11,12,13,14]. Although the cause and effect relationship of vitamin D and related diseases has not been clarified, it has been reported that vitamin D deficiency exacerbates the symptoms specific to these diseases [9]. Therefore, it is important to detect vitamin D deficiency and to plan appropriate treatments.
Depression
The global burden of the disease is generally assessed by the World Health Organization (WHO) based on disability-adjusted life years (DALY). From this point of view, mood disorders are reported to be at the top of the global disease burden [15]. Depression, one of the mood disorders, results from the complex interaction of social, psychological, and biological factors and is a common disease globally. According to 2019 data, it is reported that 5.0% of adults, 5.7% of individuals over the age of 60, and 3.8% of the global population suffer from depression [16, 17].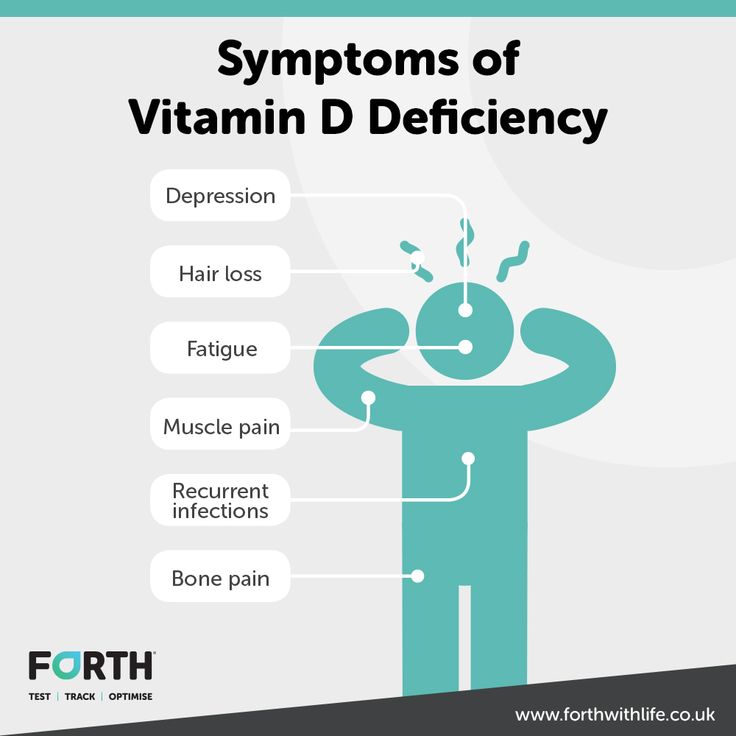 Although depression is different from the usual mood swings and short-term emotional reactions to the difficulties in daily life, it can deeply affect the lives of individuals, especially with the accompanying major depression [16].
Although depression is different from the usual mood swings and short-term emotional reactions to the difficulties in daily life, it can deeply affect the lives of individuals, especially with the accompanying major depression [16].
The presence of five or more symptoms over a 2-week period is essential for the diagnosis of a major depressive episode according to DSM-5 criteria. At least one of the symptoms must be depressed mood or anhedonia, and secondarily, it may include appetite or bodyweight changes, sleep difficulties, psychomotor agitation, fatigue, decreased cognitive abilities, feelings of worthlessness, and extreme guilt. These symptoms are rated as always (1) or never (0) [18]. DSM-V assumes that depression can be accepted as one-dimensional and suggests that major depression can be determined by the sum of these degrees of change. However, it has been reported that depression may have different dimensions. It is stated that grouping the changes determined by DSM-V and mentioned above as somatic (insomnia, changes in appetite or body weight, decreased cognitive abilities, fatigue, and psychomotor agitation) and non-somatic (depressed mood, anhedonia, feelings of worthlessness, and suicidal thoughts) changes is the best representative. No correlation has been identified between the number of changes and the severity of depression. Scales are used for the severity of depression, and it has been reported that the most frequently used one is the Hamilton Depression Scale (HDS) [19].
No correlation has been identified between the number of changes and the severity of depression. Scales are used for the severity of depression, and it has been reported that the most frequently used one is the Hamilton Depression Scale (HDS) [19].
Depression can lead to cardiovascular events and stroke due to these changes that affect daily life and lifestyle changes, and as a result, it can increase mortality and morbidity [20]. In addition, depression can extend to suicide, and it has been reported that the fourth cause of death for individuals aged 15–29 is suicide [16, 19]. When all these are evaluated together, the prevention, diagnosis, and treatment of depression are important. The WHO highlights the steps needed to provide appropriate interventions for many mental disorders, including depression, in the Mental Health Action Plan 2013–2030 [21].
The underlying biological mechanisms for depression have not been fully elucidated. However, some possible pathways are indicated.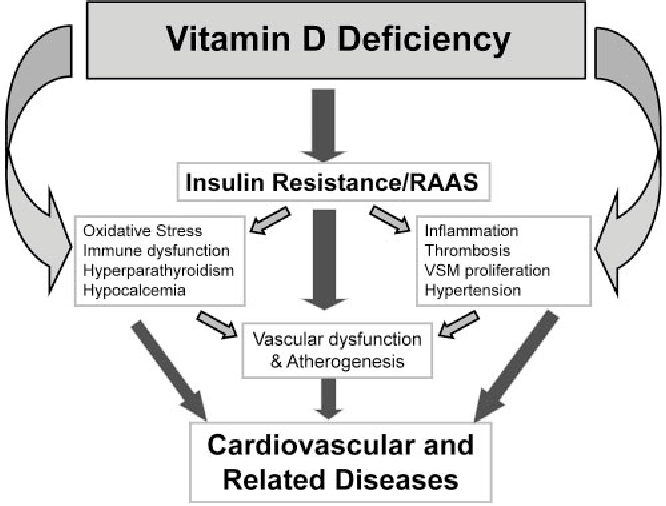 It mainly focuses on 3 hypotheses, including the effects of vitamin D on neurotrophy, monoamine neurotransmission, and immunomodulation [9, 20, 22].
It mainly focuses on 3 hypotheses, including the effects of vitamin D on neurotrophy, monoamine neurotransmission, and immunomodulation [9, 20, 22].
It has been stated that the determination of the role of inflammation in the pathophysiology of depression may provide hope for anti-inflammatory agents for this mood disorder. Changes involving oxidative stress and neuroinflammation may cause activation of peripheral macrophages and central microglia, dysfunction of the hypothalamus–pituitary–adrenal (HPA) axis, and hypercortisolemia. As a result of all these, dendritic growth, synaptic plasticity, and deterioration in synaptic communication can be seen. It has been stated that the effect of vitamin D on the pathophysiology of depression may also be due to its immunomodulatory properties [6]. It is reported that with this feature, it can show a neuroprotective effect by preventing the abnormal function of the immune system [20, 22]. However, it was emphasized that these results were not at the level of evidence that could be used in clinical guidelines [6].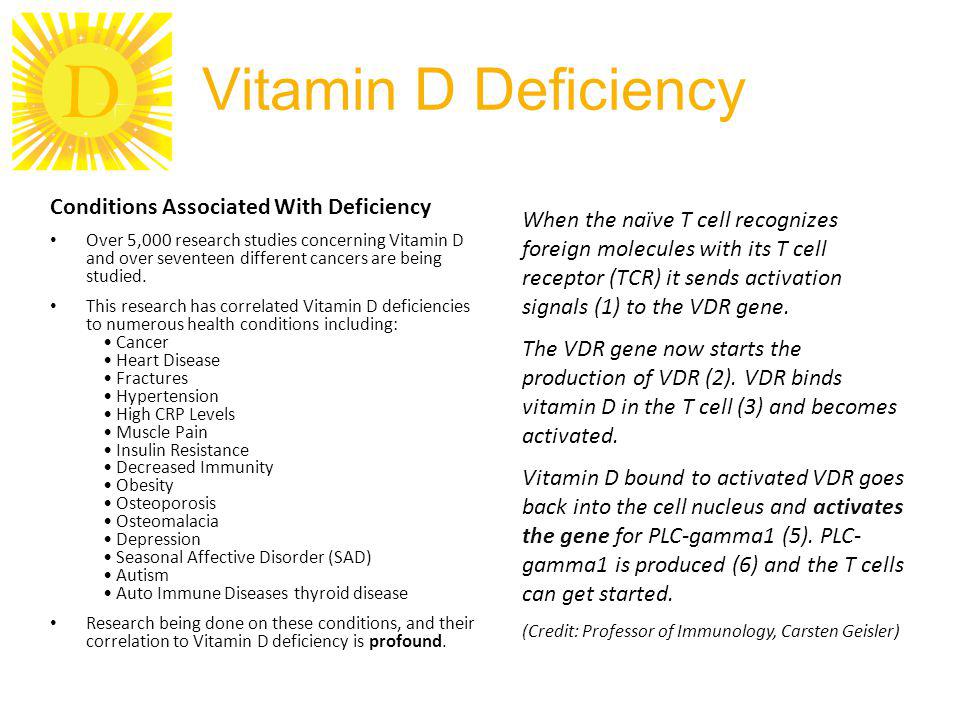
It is thought that increased expression of region-specific vitamin D receptors (VDR) in brain regions known to play an important role in mood regulation (such as prefrontal and cingulate cortices) may be effective on the progression of depression [20, 22]. Because the hippocampal structure can control memory, emotional functions in other brain regions, and limbic structure atrophy, it has been determined that individuals with disorders in this hippocampal structure suffer from chronic depression. After detecting the presence of VDR in the hippocampus, the activity of vitamin D in this structure was examined, and it was revealed that vitamin D is a potent modulator of the expression of neurotrophic agents such as nerve growth factor (NGF), brain-derived neurotrophic factor (BDNF), and neurotrophin (NT)-3. Neurotrophic factors are necessary for the viability, growth, and migration of neurons that display their biological functions by combining with cognate tropomyosin-related kinase (Trk) receptors, and vitamin D can increase the expression of these neurotrophic factors.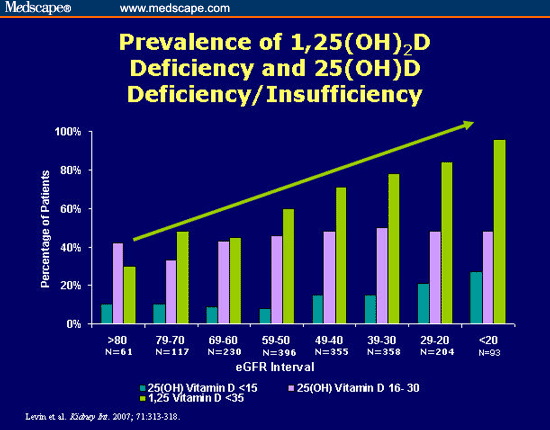 It is emphasized that neurons that secrete neurotransmitters, and therefore neurogenesis, are important in depression and that vitamin D has an important role in maintaining the vitality of neurons [9].
It is emphasized that neurons that secrete neurotransmitters, and therefore neurogenesis, are important in depression and that vitamin D has an important role in maintaining the vitality of neurons [9].
Calcitriol, also called neurosteroid hormone due to its immunomodulatory and neurotrophic roles, is effective in the synthesis of neurotransmitters (serotonin, dopamine, noradrenaline, adrenaline) that play a role in the pathophysiology of mood disorders by activating the gene expression of the tyrosine hydroxylase enzyme, reported as the rate-limiting step in catecholamine synthesis [14, 23]. Vitamin D both protects serotonergic neuron health with its neurotrophic effect and supports serotonin synthesis by providing gene expression of enzymes that are active in synthesis. Alteration of serotonin synthesis in case of vitamin D deficiency is also evident [22]. In addition to the synthesis, it is also stated that vitamin D takes part in the metabolism of these neurotransmitters and prevents their depletion [14, 20]. Vitamin D is also thought to be a factor in the onset of depression with its potential roles in correcting this calcium and glutamate-γ-aminobutyric acid (GABA) imbalance by regulating intracellular calcium stores and cellular signals [22]. Considering all this, it is reported that vitamin D provides modulation of the HPA axis [20]. It is emphasized that vitamin D is neuroprotective for neurons that secrete neurotransmitters (especially dopamine), but it may show neurotoxic effects when plasma levels exceed the threshold value [23].
Vitamin D is also thought to be a factor in the onset of depression with its potential roles in correcting this calcium and glutamate-γ-aminobutyric acid (GABA) imbalance by regulating intracellular calcium stores and cellular signals [22]. Considering all this, it is reported that vitamin D provides modulation of the HPA axis [20]. It is emphasized that vitamin D is neuroprotective for neurons that secrete neurotransmitters (especially dopamine), but it may show neurotoxic effects when plasma levels exceed the threshold value [23].
The results of preclinical studies examining the relationship between vitamin D and depression were found to be inconsistent. It was determined that high-dose vitamin D administration (5 mg/kg/day) for 14 days in ovariectomized rats (n = 96) showed antidepressant-like behavior in depression caused by ovariectomy [24]. Low levels of vitamin D have also been observed in the offspring (n = 15) of mothers exposed to low levels of vitamin D from pre-pregnancy to the end of the lactation period.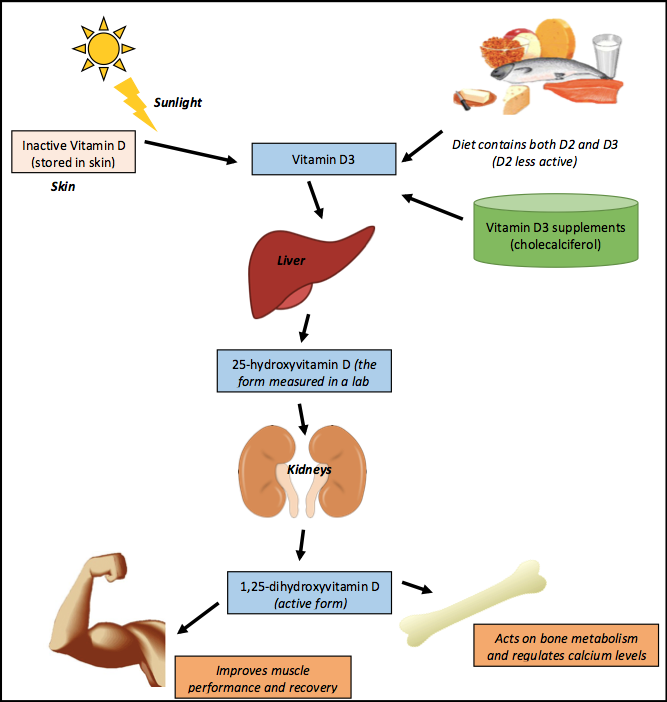 In addition, low vitamin D levels were found to cause anhedonia, an important marker of depression in offspring [25]. It has been reported that the administration of vitamin D3 for 7 days effectively prevents depressive-like behavior caused by corticosteroid exposure and brain oxidative stress markers, and this antidepressant effect may also be due to oxidative stress modulation [26]. Another study showed that intraperitoneal treatment with 1,25(OH)2 vitamin D3 (5, 10 µg/kg, twice a week) for 5 weeks effectively ameliorated anhedonia with chronic mild stress [27]. However, there is also a study in the literature reporting that vitamin D deficiency does not affect the proliferation or survival of neurons in rats [28].
In addition, low vitamin D levels were found to cause anhedonia, an important marker of depression in offspring [25]. It has been reported that the administration of vitamin D3 for 7 days effectively prevents depressive-like behavior caused by corticosteroid exposure and brain oxidative stress markers, and this antidepressant effect may also be due to oxidative stress modulation [26]. Another study showed that intraperitoneal treatment with 1,25(OH)2 vitamin D3 (5, 10 µg/kg, twice a week) for 5 weeks effectively ameliorated anhedonia with chronic mild stress [27]. However, there is also a study in the literature reporting that vitamin D deficiency does not affect the proliferation or survival of neurons in rats [28].
When the epidemiological and clinical studies were examined, cross-sectional and cohort studies were encountered that revealed an inverse relationship between plasma 25(OH)D3 and depression symptoms and major depressive disorder [29,30,31,32,33]. In these studies, the cut-off points considered for vitamin D adequacy, insufficiency, and deficiency, the group in which the study was conducted and the scale used to determine depressive symptoms, show heterogeneity. However, it is emphasized in all studies that individuals with high vitamin D levels are less likely to develop depressive symptoms/depression. In a 4-year follow-up cohort study, which was planned especially in a large sample and aimed to reveal the causality between vitamin D and depression, it was determined that individuals with vitamin D deficiency were 75% more likely to develop depression when compared to individuals with adequate levels [29].
In these studies, the cut-off points considered for vitamin D adequacy, insufficiency, and deficiency, the group in which the study was conducted and the scale used to determine depressive symptoms, show heterogeneity. However, it is emphasized in all studies that individuals with high vitamin D levels are less likely to develop depressive symptoms/depression. In a 4-year follow-up cohort study, which was planned especially in a large sample and aimed to reveal the causality between vitamin D and depression, it was determined that individuals with vitamin D deficiency were 75% more likely to develop depression when compared to individuals with adequate levels [29].
There are also studies evaluating the polymorphism, reporting that the relationship between plasma vitamin D levels and depression is not significant [34, 35]. Although these studies were planned as case control, vitamin D classification was not made, and interpretations were made on the averages of plasma 25 (OH) vitamin D levels.![]()
In addition to these studies, there are also studies in which vitamin D therapy has been used as a therapeutic agent alone or as an adjuvant to classical pharmacotherapy in major depressive disorder [14, 36,37,38,39,40,41,42]. In a cell culture study examining the effect of vitamin D on serotonin reuptake transporters (SERT), which is the target of serotonin reuptake inhibitors (SSRI) used in the treatment of depression, and monoamine oxidase (MAO), which catalyzes the destruction of serotonin, it was determined that 10 nmol vitamin D application could suppress the expression of SERT and MAO (59%, 51%, respectively). However, it was also emphasized that there was no statistically significant difference for other doses (1 nmol/100 nmol) [14]. Epidemiological studies in which vitamin D supplementation was carried out were conducted on the effect of depressive symptoms observed due to the presence of chronic diseases such as diabetes, ulcerative colitis, and Chron’s rather than individuals with a diagnosis of depression.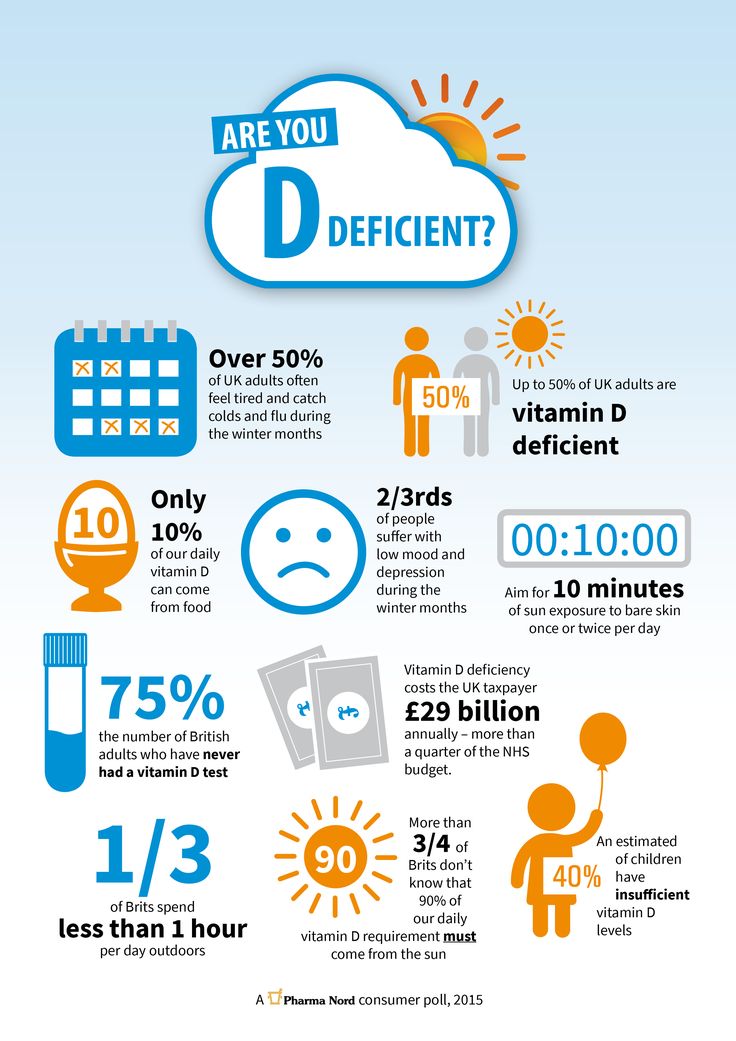 Therefore, it was thought that the positive outcomes of vitamin D supplementation obtained from studies on depressive symptoms may be related to its effect on metabolic and inflammatory markers as an immunomodulator. In a placebo-controlled double-blind randomized clinical study evaluating the effect of vitamin D supplementation (50,000 IU for 2 weeks) on plasma 25 (OH) vitamin D levels and some neurotransmitters in individuals (n = 56) with mild and moderate depression, it was reported that serum 25 (OH) vitamin D levels increased significantly in the intervention group, and the severity of depression decreased. In the same study, it was reported that no significant change was observed in platelet serotonin levels [13]. In the meta-analysis of 25 studies (n = 7534) evaluating the effectiveness of vitamin D supplementation on depression, it was reported that vitamin D was effective in individuals with major depressive disorder and plasma 25(OH)D levels ≤ 50 nmol/L and this effect was achieved with supplements less than 4000 IU for ≥ 8 weeks [11].
Therefore, it was thought that the positive outcomes of vitamin D supplementation obtained from studies on depressive symptoms may be related to its effect on metabolic and inflammatory markers as an immunomodulator. In a placebo-controlled double-blind randomized clinical study evaluating the effect of vitamin D supplementation (50,000 IU for 2 weeks) on plasma 25 (OH) vitamin D levels and some neurotransmitters in individuals (n = 56) with mild and moderate depression, it was reported that serum 25 (OH) vitamin D levels increased significantly in the intervention group, and the severity of depression decreased. In the same study, it was reported that no significant change was observed in platelet serotonin levels [13]. In the meta-analysis of 25 studies (n = 7534) evaluating the effectiveness of vitamin D supplementation on depression, it was reported that vitamin D was effective in individuals with major depressive disorder and plasma 25(OH)D levels ≤ 50 nmol/L and this effect was achieved with supplements less than 4000 IU for ≥ 8 weeks [11].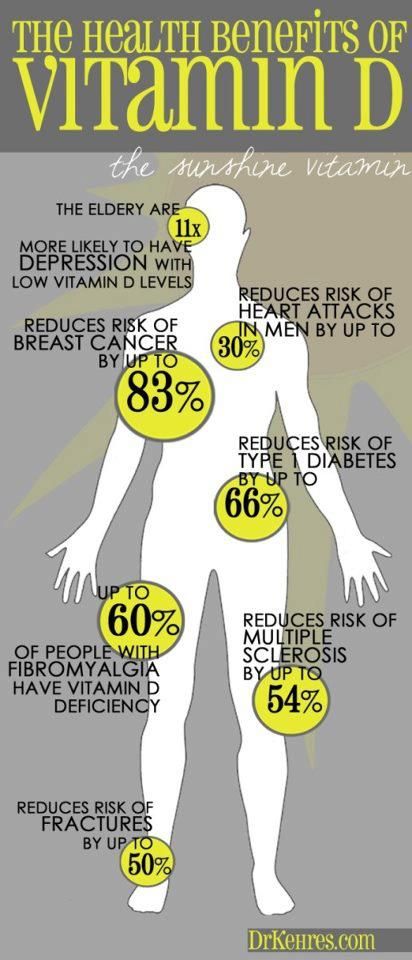 However, there is also a study in the literature that vitamin D supplementation does not affect depressive symptoms [43].
However, there is also a study in the literature that vitamin D supplementation does not affect depressive symptoms [43].
Anxiety
Anxiety disorders (generalized anxiety disorder, phobia, panic disorder, and others) are defined as a negative, uncertain, and unpleasant emotional state resulting from the anticipation of a potential danger with multifactorial causes. It represents a group of common mental health disorders that negatively affect daily life and well-being. Anxiety disorders involve excessive and persistent fear, worry, and/or avoidance of perceived threats in the external (e.g., social situations) or internal (e.g., bodily sensations) environment, often accompanied by panic attacks [44]. Anxiety and depression or other mental health disorders can also be observed together [6, 45]. Although the developmental ages of the subtypes of anxiety disorders vary, it is reported that they are mostly onset in childhood and adolescence. It has been reported that DSM-V and ICD-10 criteria are used in the classification of anxiety disorders, and these two classifications are similar [44].
In the meta-analysis study on the global prevalence of anxiety, it was reported that the prevalence of anxiety in Asia was 32.9% (13 studies), while the prevalence of anxiety in Europe was 23.8% (3 studies) [46]. However, this current study is given depending on the COVID-19 process. Anxiety, like depression, is among the mental disorders that affect the quality of life and therefore daily life and health costs [44, 47]. It has been determined that anxiety is in the second place in terms of DALY burden. Although anxiety, which is attributed to the 4.2% burden in DALY, is observed to be low, this burden increases with comorbidity depression [44]. Therefore, the prevention and treatment of anxiety disorders are important.
Some hypotheses have been defined in anxiety disorders. In the hypothesis defined for the neural circuit, it is reported that fear and anxiety are regulated by a mixture of bidirectional connections in the amygdala, ventromedial prefrontal hypothalamus, and anterior cingulate cortex with the functional effect of the hippocampus. It is emphasized that the discord between these centers plays a role in anxiety disorders (hyperactivation in the amygdala, decreased activation in the ventromedial prefrontal hypothalamus) [44]. It has been reported that amygdala hyperactivation, especially in response to a threat, is associated with the risk of developing anxiety in later years [48]. Another hypothesis is a defect in the HPA axis, which is also involved in the pathophysiology of depression [44]. Vitamin D activity should be considered due to the increased expression of the vitamin D receptor in these regions and the presence of the 1-α-hydroxylase enzyme. It has been reported that there are irregularities in the HPA axis in vitamin D deficiency [13]. This information supports the relationship between vitamin D and anxiety. It is stated that the deficiency of substrates such as dopamine, serotonin, and norepinephrine is also involved in the pathophysiology, but it is generally associated with reduced inhibitory signalling by GABA or hyperexcitability caused by increased excitatory glutaminergic neurotransmission.
It is emphasized that the discord between these centers plays a role in anxiety disorders (hyperactivation in the amygdala, decreased activation in the ventromedial prefrontal hypothalamus) [44]. It has been reported that amygdala hyperactivation, especially in response to a threat, is associated with the risk of developing anxiety in later years [48]. Another hypothesis is a defect in the HPA axis, which is also involved in the pathophysiology of depression [44]. Vitamin D activity should be considered due to the increased expression of the vitamin D receptor in these regions and the presence of the 1-α-hydroxylase enzyme. It has been reported that there are irregularities in the HPA axis in vitamin D deficiency [13]. This information supports the relationship between vitamin D and anxiety. It is stated that the deficiency of substrates such as dopamine, serotonin, and norepinephrine is also involved in the pathophysiology, but it is generally associated with reduced inhibitory signalling by GABA or hyperexcitability caused by increased excitatory glutaminergic neurotransmission. In addition, it is thought that vitamin D may also be a factor in anxiety due to oxidative stress and inflammation in the pathophysiology [6].
In addition, it is thought that vitamin D may also be a factor in anxiety due to oxidative stress and inflammation in the pathophysiology [6].
In a study on ovariectomized rats (n = 96), in which anxiety was evaluated as well as depression, it was found that low-dose vitamin D administration (1 mg/kg/day) for 14 days had an anti-anxiolytic effect, in contrast to depression [24].
The results of epidemiological studies conducted to determine the relationship between anxiety and vitamin D show a negative correlation similar to depression [10, 12]. In a study evaluating the relationship between vitamin D levels and anxiety in individuals with rheumatoid arthritis (n = 161), it was concluded that there was an inverse relationship between vitamin D levels and the presence of anxiety [30]. In the systematic review of fourteen studies published by Fallah et al., it was determined that 10 studies reported a direct relationship between vitamin D levels and anxiety, and one study reported an indirect relationship [49].
In a randomized controlled clinical study evaluating the efficacy of vitamin D supplementation on anxiety, it was reported that the administration of 1600 mg of vitamin D for 6 months improved anxiety symptoms [43]. In the study in which different vitamin D supplements applied to individuals (n = 34) in the remission stage of Crohn’s disease were examined, it was reported that only high-dose (10,000 IU) vitamin D supplementation significantly increased serum vitamin D levels, but both doses improved the symptoms of depression and anxiety [40].
Conclusion and Recommendations
In conclusion, vitamin D has immunomodulatory, neuroprotective, and neurotrophic properties and may affect the brain tissues involved in the pathophysiology of depression and anxiety. The results of studies in the literature on the relationship of vitamin D levels with supplementation, depression, and anxiety are inconsistent. It is thought that the reason for the inconsistency in studies examining vitamin D levels may be due to the use of different cut-off points regarding vitamin D adequacy, the differences in the groups in which the studies were conducted, and the differences in the tools used to determine depression and anxiety.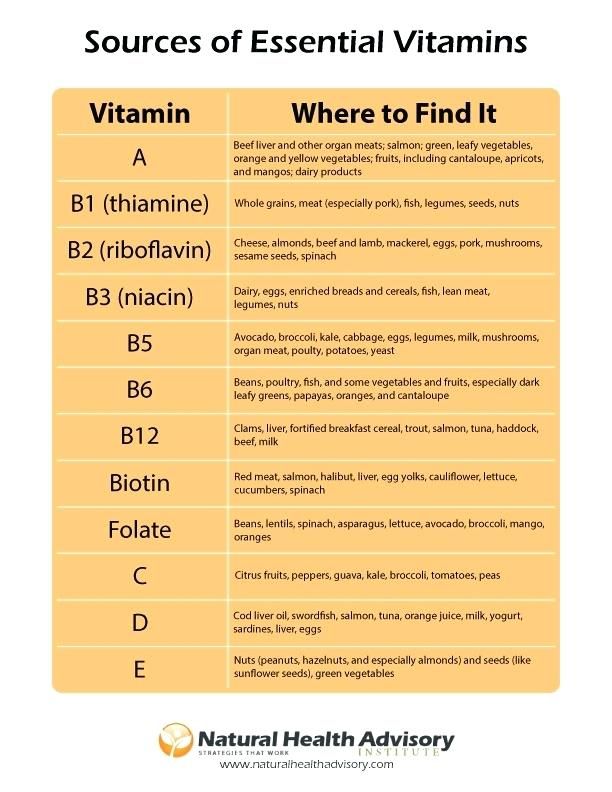 It is thought that many factors may have contributed to the inconsistency in the studies in which vitamin D supplementation was evaluated, including the difference between the groups applied, the severity of depressive symptoms, the presence of comorbidities, initial 25(OH)D3 level, vitamin D supplement dose, supplement form, and duration. In addition, studies in the literature include not only individuals with symptoms of major depression or anxiety but also individuals with chronic inflammatory diseases such as ulcerative colitis, Crohn’s, and diabetes. Therefore, positive outcomes in individuals with these diseases can be associated with the effect of vitamin D as an immunomodulator on metabolic and inflammatory markers. Although the cause and effect relationship of vitamin D with depression and anxiety has not been clarified in the literature, it is emphasized that low vitamin D levels cause an increase in the symptoms of these diseases. It is important to screen for vitamin D deficiencies regarding mood disorders, to plan appropriate treatments, and to determine the optimal dose.
It is thought that many factors may have contributed to the inconsistency in the studies in which vitamin D supplementation was evaluated, including the difference between the groups applied, the severity of depressive symptoms, the presence of comorbidities, initial 25(OH)D3 level, vitamin D supplement dose, supplement form, and duration. In addition, studies in the literature include not only individuals with symptoms of major depression or anxiety but also individuals with chronic inflammatory diseases such as ulcerative colitis, Crohn’s, and diabetes. Therefore, positive outcomes in individuals with these diseases can be associated with the effect of vitamin D as an immunomodulator on metabolic and inflammatory markers. Although the cause and effect relationship of vitamin D with depression and anxiety has not been clarified in the literature, it is emphasized that low vitamin D levels cause an increase in the symptoms of these diseases. It is important to screen for vitamin D deficiencies regarding mood disorders, to plan appropriate treatments, and to determine the optimal dose. Because although there are studies in the literature reporting that the level of side effects and toxicity of vitamin D is low, it is also reported that the course of vitamin D levels above the threshold value is neurotoxic. Therefore, the necessity of monitoring vitamin D levels in planned vitamin D supplements is also clear. Besides, vitamin D is not included in the guidelines in the literature on mood disorders. For this disease group, cohort studies are needed to determine the effectiveness of vitamin D levels, supplement dose, and form.
Because although there are studies in the literature reporting that the level of side effects and toxicity of vitamin D is low, it is also reported that the course of vitamin D levels above the threshold value is neurotoxic. Therefore, the necessity of monitoring vitamin D levels in planned vitamin D supplements is also clear. Besides, vitamin D is not included in the guidelines in the literature on mood disorders. For this disease group, cohort studies are needed to determine the effectiveness of vitamin D levels, supplement dose, and form.
References
Czarny P, et al. The interplay between inflammation, oxidative stress, DNA damage, DNA repair and mitochondrial dysfunction in depression. Prog Neuropsychopharmacol Biol Psychiatry. 2018;80:309–21.
Article CAS Google Scholar
Sassi F, Tamone C, D’Amelio P. Vitamin D: nutrient, hormone, and immunomodulator.
 Nutrients. 2018;10(11):1656.
Nutrients. 2018;10(11):1656.Chang S-W, Lee H-C. Vitamin D and health-the missing vitamin in humans. Pediatr Neonatol. 2019;60(3):237–44.
Article Google Scholar
Lips P, et al. Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: a position statement of the European Calcified Tissue Society. Eur J Endocrinol. 2019;180(4):P23–54.
Article CAS Google Scholar
Sizar O, et al. Vitamin D deficiency. StatPearls. 2020.
Casseb GA, Kaster MP, Rodrigues ALS. Potential role of vitamin D for the management of depression and anxiety. CNS Drugs. 2019;33(7): p. 619–637. It is an important review that summarizes the vitamin D roles in potential pathways.
Amrein K, et al. Vitamin D deficiency 2.
 0: an update on the current status worldwide. Eur J Clin Nutri. 2020;74(11): p. 1498–1513.
0: an update on the current status worldwide. Eur J Clin Nutri. 2020;74(11): p. 1498–1513.Parker GB, Brotchie H, Graham RK. Vitamin D and depression. J Affect Disord. 2017;208:56–61.
Article CAS Google Scholar
Geng C, et al. Vitamin D and depression: mechanisms, determination and application. Asia Pacific J Clin Nutr. 2019;28(4): p. 689–694. It is an important review for explaining the that brain regions with vitamin D receptor density are given and attention is drawn to its possible role in common with mood disorders such as depression.
Bičíková M, et al. Vitamin D in anxiety and affective disorders. Physiol Res. 2015;64(Suppl 2):S101–3.
Article Google Scholar
Cheng YC, Huang YC, Huang WL. The effect of vitamin D supplement on negative emotions: a systematic review and meta-analysis.
 Depress Anxiety. 2020;37(6):549–564.
Depress Anxiety. 2020;37(6):549–564.Karonova TL, et al. Anxiety/depressive disorders and vitamin D status. Zh Nevrol Psikhiatr Im S S Korsakova. 2015;115(10 Pt 2):55–8.
CAS Google Scholar
Kaviani M, et al. Effects of vitamin D supplementation on depression and some involved neurotransmitters. J Affect Disord. 2020;269:28–35.
Article CAS Google Scholar
Sabir MS, et al. Optimal vitamin D spurs serotonin: 1, 25-dihydroxyvitamin D represses serotonin reuptake transport (SERT) and degradation (MAO-A) gene expression in cultured rat serotonergic neuronal cell lines. Genes Nutr. 2018;13(1):1–11.
Article CAS Google Scholar
Ogasawara K, et al. Issues on the diagnosis and etiopathogenesis of mood disorders: reconsidering DSM-5.
 J Neural Transm. 2018;125(2):211–22.
J Neural Transm. 2018;125(2):211–22.Article Google Scholar
Depression. 2021; Available from: https://www.who.int/news-room/fact-sheets/detail/depression.
Institute of Health Metrics and Evaluation. Global Health Data Exchange (GHDx). [cited 2021 04.11]; Available from: http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/d780dffbe8a381b25e1416884959e88b
American Psychiatric Association D and AP Association, Diagnostic and statistical manual of mental disorders: DSM-5. 2013, Washington, DC: American psychiatric association.
Tolentino JC, Schmidt SL. DSM-5 criteria and depression severity: implications for clinical practice. Front Psych. 2018;9:450.
Article Google Scholar
Menon V, et al. Vitamin D and depression: a critical appraisal of the evidence and future directions Indian J Psychol Med 2020;42(1):11–21.
 It is the most important review that the role of vitamin D in mood disorders such as depression and anxiety is discussed by explaining other possible mechanisms besides the antioxidant mechanism presented with evidence.
It is the most important review that the role of vitamin D in mood disorders such as depression and anxiety is discussed by explaining other possible mechanisms besides the antioxidant mechanism presented with evidence.World Health Organization (WHO). Mental Health Gap Action Programme (mhGAP). [cited 2021 05.11.2021]; Available from: https://www.who.int/teams/mental-health-and-substance-use/treatment-care/mental-health-gap-action-programme.
Berridge MJ. Vitamin D and depression: cellular and regulatory mechanisms. Pharmacol Rev. 2017;69(2):80–92.
Article CAS Google Scholar
Eyles DW, Burne TH, McGrath JJ. Vitamin D, effects on brain development, adult brain function and the links between low levels of vitamin D and neuropsychiatric disease. Front Neuroendocrin. 2013;34(1):47–64.
Fedotova J, et al.
 Different effects of vitamin D hormone treatment on depression-like behavior in the adult ovariectomized female rats. Biomed Pharmacother. 2016;84:1865–72.
Different effects of vitamin D hormone treatment on depression-like behavior in the adult ovariectomized female rats. Biomed Pharmacother. 2016;84:1865–72.Article CAS Google Scholar
Fu L, et al. Vitamin D deficiency impairs neurobehavioral development in male mice. Physiol Behav. 2017;179:333–9.
Article CAS Google Scholar
Camargo A, et al. Cholecalciferol counteracts depressive-like behavior and oxidative stress induced by repeated corticosterone treatment in mice. Eur J Pharmacol. 2018;833:451–61.
Article CAS Google Scholar
Sedaghat K, et al. Mesolimbic dopamine system and its modulation by vitamin D in a chronic mild stress model of depression in the rat. Behav Brain Res. 2019;356:156–69.
Article CAS Google Scholar
Groves NJ, et al. Behavioural effects of adult vitamin D deficiency in BALB/c mice are not associated with proliferation or survival of neurons in the adult hippocampus. PLoS ONE. 2016;11(4): e0152328.
Article Google Scholar
Briggs R, et al. Vitamin D deficiency is associated with an increased likelihood of incident depression in community-dwelling older adults. J Am Med Dir Assoc. 2019;20(5):517–23.
Article Google Scholar
Pu D, et al. Prevalence of depression and anxiety in rheumatoid arthritis patients and their associations with serum vitamin D level. Clin Rheumatol. 2018;37(1):179–84.
Article Google Scholar
Sherchand O, et al. Association between vitamin D deficiency and depression in Nepalese population. Psychiatry Res. 2018;267:266–71.
Article CAS Google Scholar
Song BM, et al. Association between serum 25-hydroxyvitamin D concentrations and depressive symptoms in an older Korean population: a cross-sectional study. J Affect Disord. 2016;189:357–64.
Article CAS Google Scholar
Vidgren M, et al. Serum concentrations of 25-hydroxyvitamin D and depression in a general middle-aged to elderly population in Finland. J Nutr Health Aging. 2018;22(1):159–64.
Article CAS Google Scholar
Michaëlsson K, Melhus H, Larsson SC. Serum 25-hydroxyvitamin D concentrations and major depression: a Mendelian randomization study. Nutrients 2018;10(12):1987.
Şahin Can M, et al. Vitamin D levels and vitamin D receptor gene polymorphism in major depression.
 Psychiatr Danub. 2017;29(2):179–85.
Psychiatr Danub. 2017;29(2):179–85.Article Google Scholar
Alavi NM, et al. Effect of vitamin D supplementation on depression in elderly patients: a randomized clinical trial. Clin Nutr. 2019;38(5):2065–70.
Article CAS Google Scholar
Bahrami A, et al. High dose vitamin D supplementation is associated with a reduction in depression score among adolescent girls: a nine-week follow-up study. Journal of dietary supplements. 2018;15(2):173–82.
Article CAS Google Scholar
Ghaderi A, et al. Clinical trial of the effects of vitamin D supplementation on psychological symptoms and metabolic profiles in maintenance methadone treatment patients. Prog Neuropsychopharmacol Biol Psychiatry. 2017;79:84–9.
Article CAS Google Scholar
Libuda L, et al. Effect of vitamin D deficiency on depressive symptoms in child and adolescent psychiatric patients: results of a randomized controlled trial. Eur J Nutr. 2020;59(8):3415–24.
Article CAS Google Scholar
Narula N, et al. Impact of high-dose vitamin D3 supplementation in patients with Crohn’s disease in remission: a pilot randomized double-blind controlled study. Dig Dis Sci. 2017;62(2):448–55.
Article CAS Google Scholar
Penckofer S, et al. Vitamin D supplementation improves mood in women with type 2 diabetes. J Diab Res 2017.
Sharifi A, et al. Vitamin D decreases Beck Depression Inventory score in patients with mild to moderate ulcerative colitis: a double-blind randomized placebo-controlled trial. Journal of dietary supplements. 2019;16(5):541–9.
Article CAS Google Scholar
Zhu C, et al. Vitamin D supplementation improves anxiety but not depression symptoms in patients with vitamin D deficiency. Brain Behav. 2020;10(11): e01760.
Article Google Scholar
Craske MG, et al. Anxiety disorders Nat Rev Dis Primers. 2017;3:17024.
Article Google Scholar
Kandola A and B Stubbs. Exercise and anxiety. Physical Exercise for Human Health. 2020:345–352.
Salari N, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis Glob Health. 2020;16:(1)1–11. It is an important systematic review to describe vitamin D role in anxiety and depression.
Qiuping L, et al. The impact of depression and anxiety on quality of life in Chinese cancer patient-family caregiver dyads, a cross-sectional study.
 Health Qual Life Outcomes. 2018;16(1):1–15.
Health Qual Life Outcomes. 2018;16(1):1–15.Google Scholar
Swartz JR, et al. A neural biomarker of psychological vulnerability to future life stress. Neuron. 2015;85(3):505–11.
Article CAS Google Scholar
Fallah M, Askari G, Asemi Z. Is vitamin D status associated with depression, anxiety and sleep quality in pregnancy: a systematic review. Advanced Biomedical Research. 2020;9.
Download references
Vitamins to reduce stress and anxiety.
https://vitamina.ru/
Feeling a little uneasy?
How not to feel if the world has gone crazy. Lots of reasons to be a little nervous. Feeling irritated lately and looking for something to help you deal with your anxiety?
Here are a few simple anxiety vitamins that can help:
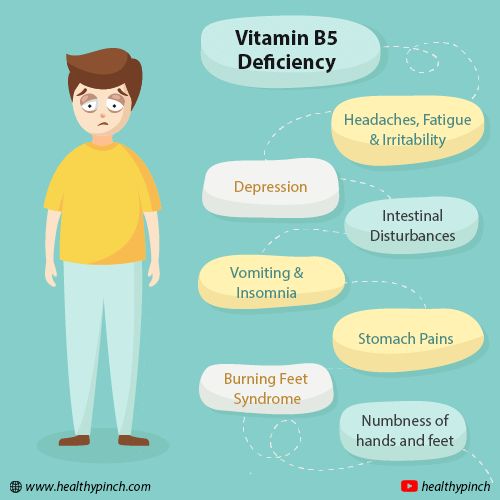
B vitamins are vitamins that play a key role in the natural treatment of anxiety. They are most important for the proper functioning of the nerves. nine0005
They are most important for the proper functioning of the nerves. nine0005
Magnesium also ranks high on the list of effective nutritional supplements. This important mineral plays many key roles in the body, mainly helping the nerves and muscles to function optimally.
Magnesium helps muscles relax. The usefulness of this supplement for stress and anxiety cannot be underestimated.
Vitamin D is by no means proven to be the right vitamin to take for stress or anxiety. However, we want to suggest that he can play a role. nine0005
Science has shown that vitamin D deficiency is associated with low levels of serotonin.
Low levels of this chemical in the brain are known to cause depression and anxiety.
Without that, taking a safe dose of vitamin D is a good idea.
Vitamin D is recommended for most of us for many reasons, including its important role in immunity.
Treating anxiety and stress is not just about vitamins.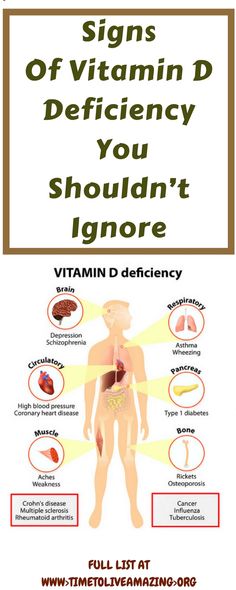 What else, you ask? nine0014
What else, you ask? nine0014
It turns out there are many simple things you can do besides taking vitamins.
The good old lifestyle advice is still very relevant. Physical exercise and healthy sleep.
In addition to these lifestyle basics, it is also worth paying attention to meditation. There are many videos on Youtube or applications on the phone.
And always remember, one important thing when choosing vitamins is to consult a doctor.
10/11/2020
You may also be interested
06 22 2022
Evening or bedtime rituals can be a great way to improve overall sleep. The purpose of these activities is to relax and de-stress your mind and body. They will help you calm down, sleep longer and better. Let's take a look at 6 things you can add to your evening ritual for better sleep.
Read more >
06 21 2022
Detox doesn't always have to be a quick juice cleanse or intense fasting.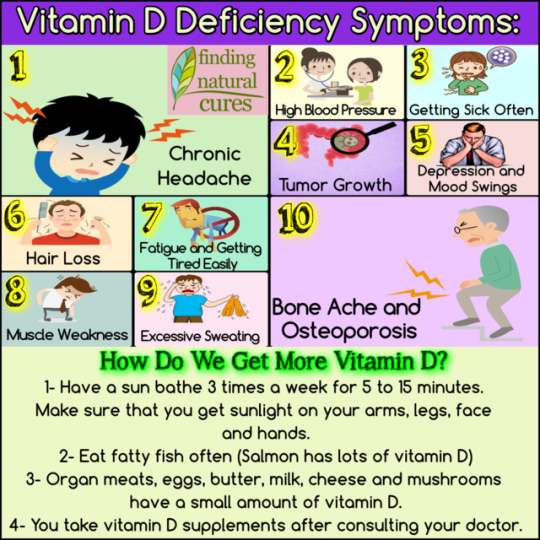 In fact, we must change our lifestyle every day in order to constantly cleanse the body of toxins. To prevent the buildup of toxins, here are 10 easy ways to detox daily.
In fact, we must change our lifestyle every day in order to constantly cleanse the body of toxins. To prevent the buildup of toxins, here are 10 easy ways to detox daily.
Read more >
06 sixteen 2022
Spirulina supplements have been one of the best-selling superfoods for years, as these natural algae are incredibly nutritious and can provide a host of health benefits. If you're still not convinced, here are 8 reasons to try spirulina. nine0005
Read more >
06 15 2022
When you eat fermented foods, you get probiotics, which are known to promote a healthier digestive system and also boost your immune system. What's more, some of these foods are easy to ferment at home. So here are 7 fermented foods that are easy to make at home.
Read more >
Share this article
The most scarce.
 Why is vitamin D deficiency dangerous? – 4fresh blog
Why is vitamin D deficiency dangerous? – 4fresh blog Building a healthy diet helps us avoid vitamin deficiencies. With the exception of just one, but a very important vitamin - vitamin D. In our strip, where there are more cloudy days per year than sunny days, vitamin D deficiency occurs in every first one. What to do with it?
Let's start with why its lack can end badly for us. Vitamin D is included in the list of 13 vital vitamins and is involved in various physiological processes: nine0005
- Regulates the absorption of calcium and phosphorus by the body. The spine, bones, teeth, joints lose strength if a deficiency develops in the body.
- Participates in the formation and maintenance of immunity. Did you get sick often? Consider getting tested for vitamin deficiencies.
- Supports eye and skin health along with vitamin A.
- It improves neuromuscular conduction, and this is the speed of our reactions and actions.
 Who is actively involved in sports here? You can't do without vitamin D! nine0089
Who is actively involved in sports here? You can't do without vitamin D! nine0089 - Suppresses inflammatory processes in the body.
Sufficient consumption is important for every person, regardless of gender and age. But there are several categories of people for whom a deficiency is especially dangerous: these are children under 13, pregnant and lactating mothers, and the elderly.
Vitamin D deficiency symptoms
You have probably heard stories about weakness, pale skin and brittle nails. But these are more inventions of bloggers than real symptoms of beriberi. nine0005
In the early stages of vitamin D deficiency development, there are:
- loss of appetite up to loss of interest in food,
- difficulty sleeping, insomnia,
- weight loss,
- nausea,
- burning in throat and mouth,
- blurred vision.
If the deficiency is not corrected in a timely manner, osteoporosis develops - bone fragility, and immunity is significantly reduced.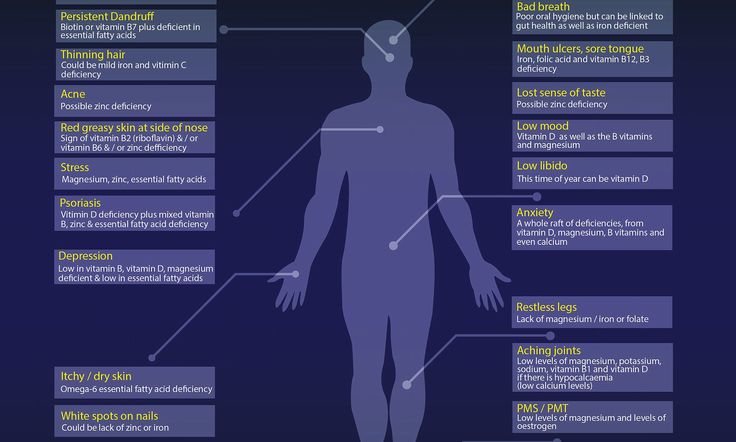 Children suffer from rickets, scoliosis and kyphosis, as well as growth retardation. nine0005
Children suffer from rickets, scoliosis and kyphosis, as well as growth retardation. nine0005
How to take vitamin D
To avoid vitamin D deficiency, it must be taken daily at a dosage of 600-1000 IU from October to May. Today, vitamin D can be found in capsules, tablets, drops, and even as a spray!
Natural vitamin D3 from lanolin LYL sunD3 in the form of a spray provides an instant supply of the substance into the bloodstream, bypassing the gastrointestinal tract. This is especially important for people who cannot take tablets or capsules due to allergies or gastrointestinal problems. nine0005
Vitamin D emulsion improves absorption by up to 95%. During clinical trials of the spray, serum vitamin D increased by 132% within a month - this is an excellent opportunity to compensate for the deficiency at the first symptoms.
One bottle of 25 mg will last for 4 months. You can take it with you on a trip, to work and use it in any circumstances.
Item 1 of 4
Should I get tested for vitamin D deficiency?
Worth it if you have symptoms of a lack of vitamin D or anxiety about it. To detect a deficiency, you need to pass only one analysis - 25 (OH) D. And it is best to contact an endocrinologist with the results and complaints to discuss the treatment regimen.
The norm of vitamin D according to blood tests is from 30 to 100 ng / ml, a content in the range of 10-30 ng / ml indicates a deficiency, and a level of less than 10 ng / ml indicates that you are deficient. nine0005
Do not self-medicate or exceed the dosage prescribed by your doctor. An overdose of vitamin D is more dangerous than its deficiency! The most innocuous symptoms in case of an overdose will be itching, unquenchable thirst, nervousness and vomiting, and the worst ones are kidney failure and the deposition of calcium salts in the tissues of the organs.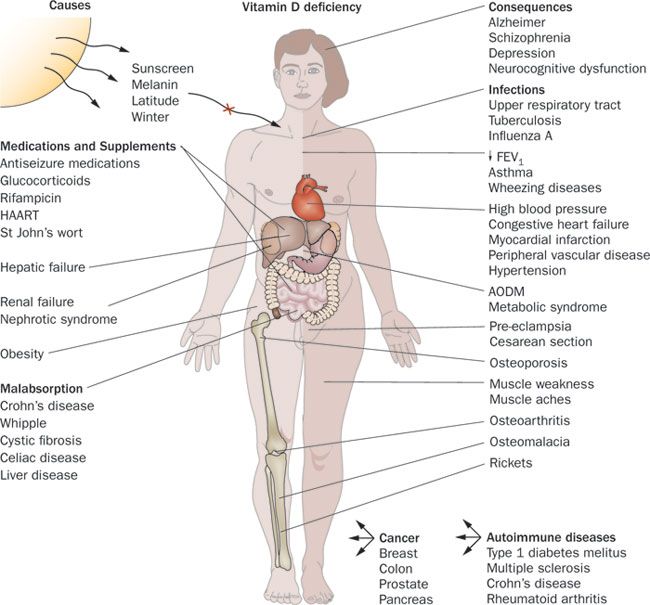
As you can see, it’s better not to joke with this vitamin!
Where is vitamin D found
When exposed to sunlight, our skin produces vitamin D in the right amount. To do this, it is enough to be in the open sun for only 20 minutes from 11 to 14 hours of the day, without hiding your hands and face. But in Russia, this recommendation of endocrinologists is relevant only from April to October. This means that for six cold dark months we must get vitamin D from other sources. nine0005
You can get it from food, but it is difficult. First of all, because the list of foods rich in this vitamin is small, and you need to eat them in large quantities in order to get the daily norm.
Here are the TOP 7 foods containing vitamin D:
- Wild salmon - 600-1000 IU per 100 g
- Som — 500 IU per 100 g
- Canned sardines - 500 IU per 100g nine0088 Herring - 300-1600 IU per 100 g
- Mushrooms (UV grown) - 400 IU per 100g
- Farm salmon, mackerel, tuna - 100-250 IU per 100g
- Milk fortified with vitamin D - 50 IU per 100 ml.