Mental illnesses and their definitions
Mental Health Screening: MedlinePlus Medical Test
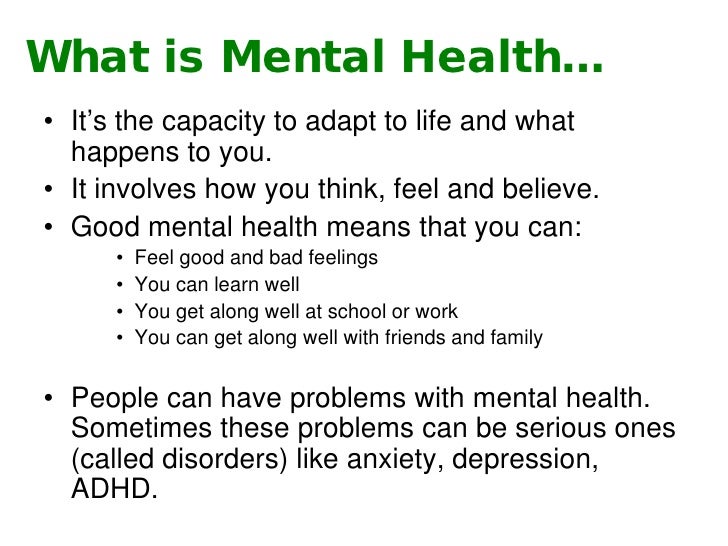
What is a mental health screening?
A mental health screening is a standard set of questions that a person answers to help a health care provider check for signs of a mental disorder. The questions help the provider learn about a person's mood, thinking, behavior, and memory.
A mental health screening is a way to catch mental health conditions early. If the screening shows signs of a disorder, more testing is usually needed to diagnose a specific mental disorder. Mental disorders are also called mental illnesses, and a mental health screening may be called a "mental illness test" or a "psychology test."
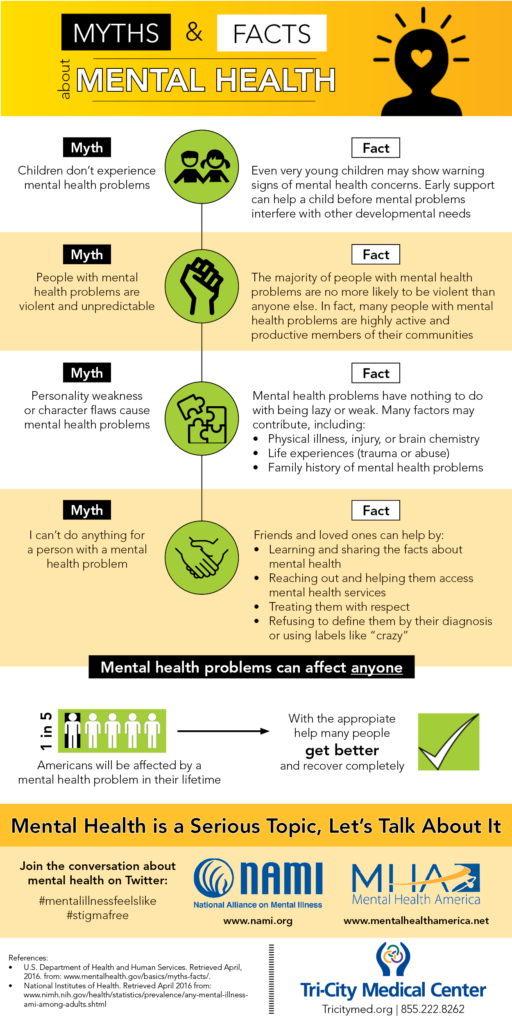
More than half of all Americans will have a mental disorder at some point in their lives. Their symptoms may range from mild to severe. Common mental disorders include:
- Mood disorders, which include depression, bipolar disorder, seasonal affective disorder (SAD), and self-harm.
- Anxiety disorders, which include panic disorder, phobias, and obsessive-compulsive disorder (OCD).
Anxiety is a common disorder in children.
- Eating disorders, which include anorexia and bulimia.
- Attention deficit hyperactivity disorder (ADHD). ADHD is one of the most common mental health disorders in children. It can also continue into adulthood.
- Post-traumatic stress disorder (PTSD).
- Personality disorders.
- Substance use disorders, which include alcohol use disorder and drug use and addiction.
- Psychotic disorders, which include schizophrenia.
These and other mental disorders affect people of all ages, including children. So, there are special mental health screening tests designed for children, teenagers, and older adults. Some screening tests look for general signs of the most common mental disorders. Other screening tests look for signs related to specific types of disorders.
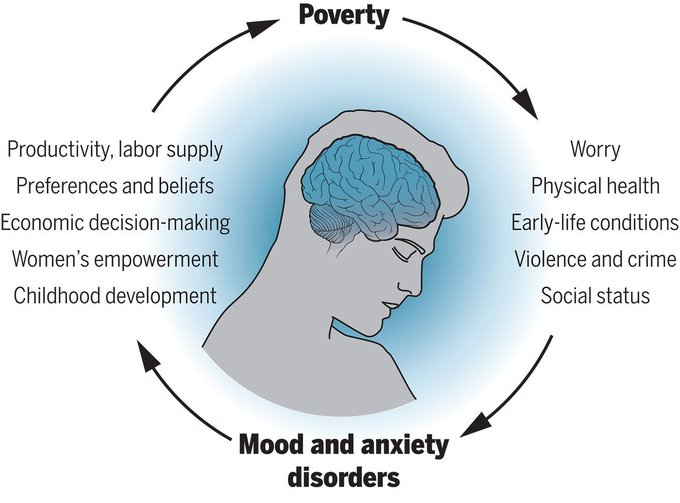
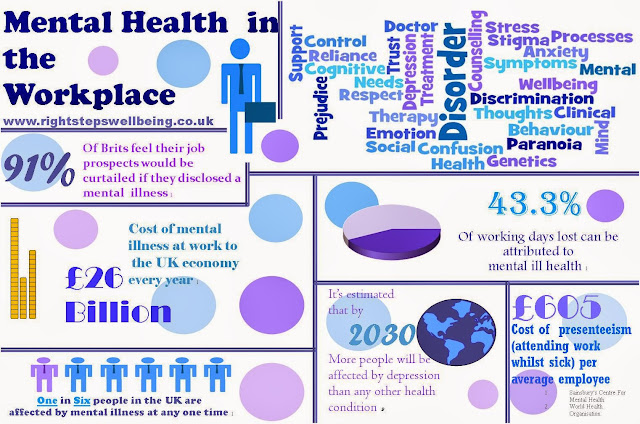
Mental health screening can be an important part of your total health at every stage of life. Mental health symptoms can be a sign of certain physical conditions. And certain mental disorders can increase the risk of developing physical health problems. With proper mental health screening, diagnosis, and treatment, people with mental health disorders can get better and many recover completely.
Mental health symptoms can be a sign of certain physical conditions. And certain mental disorders can increase the risk of developing physical health problems. With proper mental health screening, diagnosis, and treatment, people with mental health disorders can get better and many recover completely.
Other names: mental health assessment, mental illness test, psychological evaluation, psychology test, psychiatric evaluation
What is it used for?
A mental health screening is usually used as the first step to find out if a person has signs of a mental disorder. It may be part of a routine checkup. A screening test is used to see whether a person:
- Has a risk for developing a mental disorder
- Needs more testing to diagnose or rule out a mental health disorder
- Needs mental health care right away, before diagnostic testing can be finished
Mental health screening may also be used to see if treatment for a mental disorder is working.
A primary care provider may use mental health screening to help decide if a person needs to see a mental health provider for testing and/or treatment. A mental health provider is a health care professional who specializes in diagnosing and treating mental health problems. A mental health provider may use the results of a screening test to choose which other tests are needed to diagnose or rule out a specific mental disorder.
Why do I need a mental health screening?
You or your child may need a mental health screening if you have symptoms of a mental disorder. Different disorders have specific symptoms.
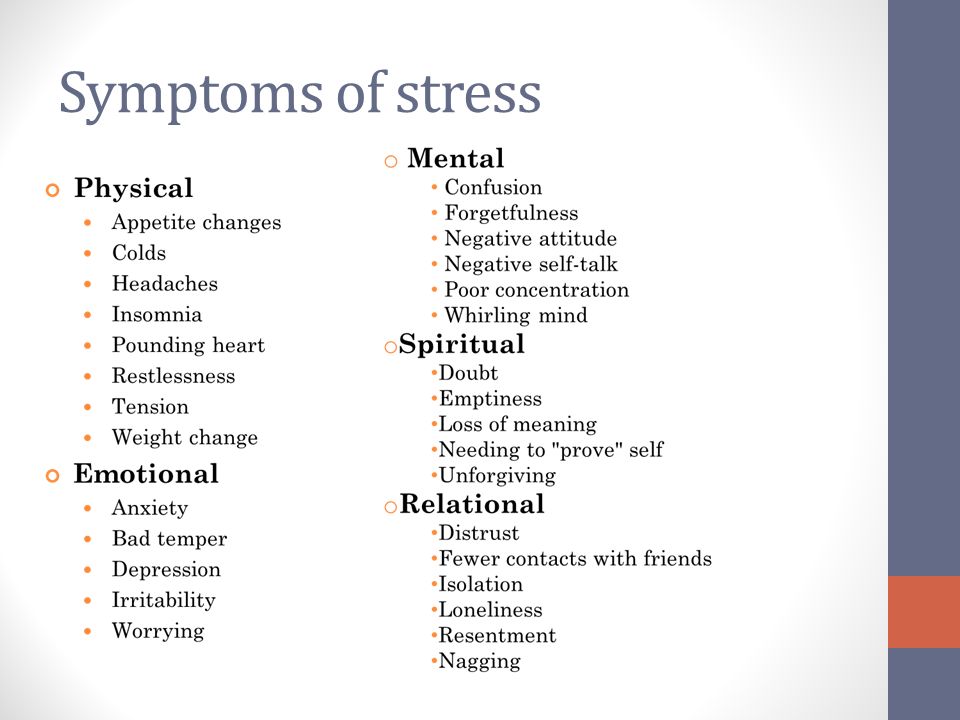
General symptoms of mental disorders may include:
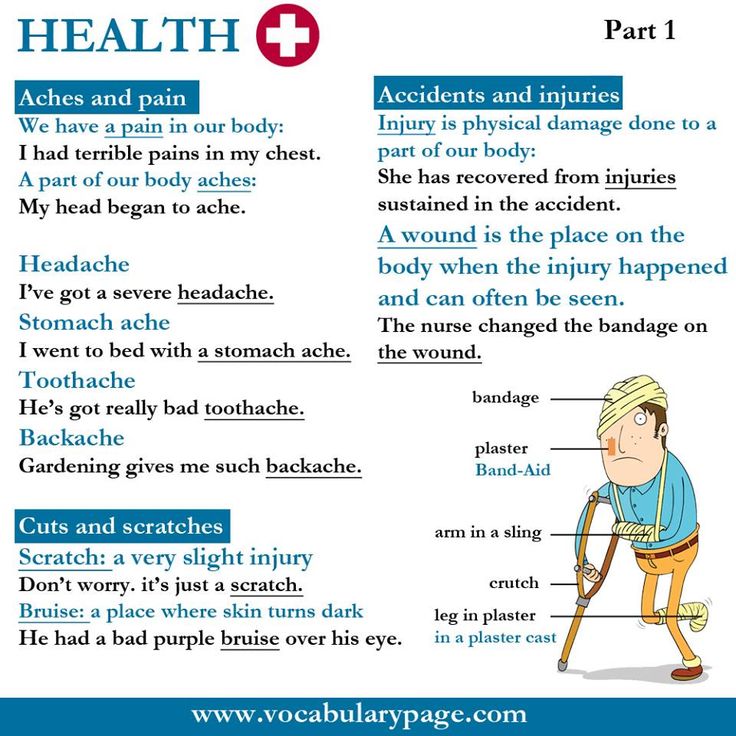
- Eating or sleeping too much or too little
- Pulling away from people and usual activities
- Fatigue and lack of energy
- Feeling helpless, hopeless, or numb like nothing matters
- Smoking, drinking, or using drugs more than usual
- Feeling unusually confused, forgetful, nervous, angry, worried, or scared
- Severe mood swings that cause problems in relationships
- Thoughts and memories that you can't get out of your head
- Hearing voices or believing things that aren't true
- Thinking about death, suicide or harming yourself or others
Signs of mental disorders in children may also include:
- Frequent tantrums and other behavior problems
- Frequent stomachaches or headaches without a known medical cause
- Difficulty in school
- Repeating actions or constantly checking things out of fear that something bad will happen
- Talking a lot about fears, worries, death, or suicide
If you or someone you know needs immediate help for a mental health disorder:
- Call 911 or go to your local emergency room
- Contact a crisis hotline.
 In the United States, you can reach the National Suicide and Crisis Lifeline at any time:
In the United States, you can reach the National Suicide and Crisis Lifeline at any time: - Call or text 988
- Chat online with Lifeline Chat
- TTY users: Use your preferred relay service or dial 711 then 988
- Veterans can contact the Veterans Crisis Line:
- Call 988 then press 1
- Text 838255
- Chat online
- Call your mental health provider or other provider
- Reach out to a loved one or close friend
What happens during a mental health screening?
If you are having a mental health screening, you'll answer a set of questions about your symptoms. The questions will be about your feelings, mood, sleep, appetite, and other parts of your life. A provider may ask you the questions or you may fill out a questionnaire and discuss your answers afterwards. It's important that your answers are honest and complete.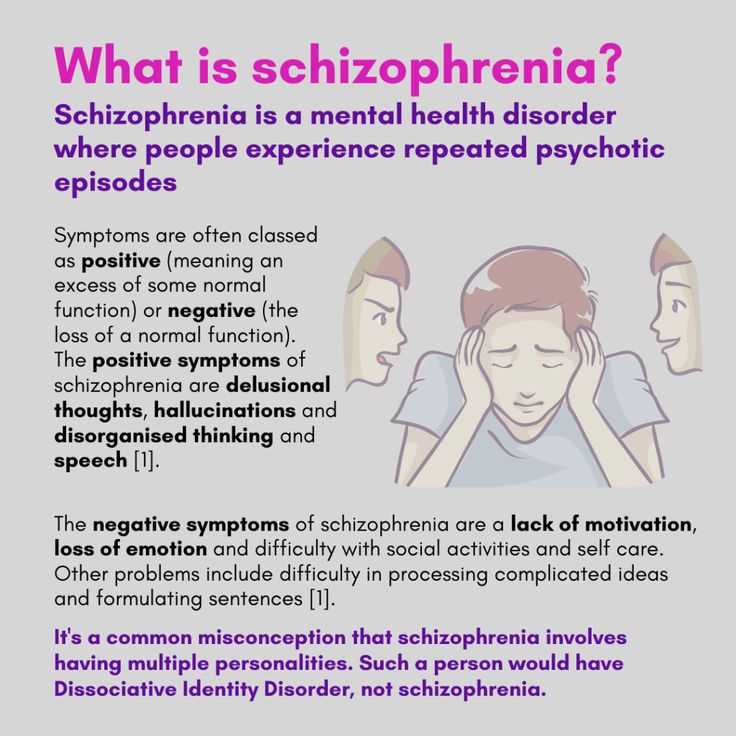
If your primary care provider is doing the screening, you may also have a physical exam and blood tests. There are no medical tests that can diagnose mental health disorders. But certain blood tests can show if a physical condition, such as thyroid disease or an electrolyte imbalance, is causing mental health symptoms.
During a blood test, a health care professional will take a blood sample from a vein in your arm, using a small needle. After the needle is inserted, a small amount of blood will be collected into a test tube or vial. You may feel a little sting when the needle goes in or out. This usually takes less than five minutes.
If your provider thinks your symptoms could be caused by physical problems with your brain or nerves, you may have a neurological exam or imaging tests of your brain.
If your child is having a mental health screening, the test will be geared to your child's age and abilities. You may be asked to fill out a questionnaire about your child's behavior.
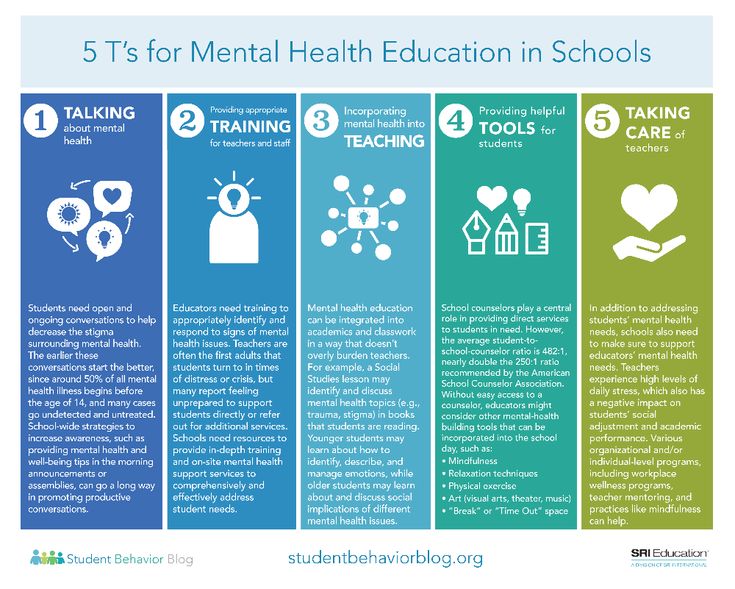
The screening may be done by your child's primary care provider or a mental health provider who works with children and teenagers. Your child's provider may also order medical tests to look for physical causes of mental disorders. Some schools provide mental health screening services.
Will I need to do anything to prepare for a mental health screening?
You usually don't need any special preparations for a mental health screening. If your child is having a screening, you may be asked to keep notes on your child's behavior for a few days before the test.
Are there any risks to screening?
There is no risk to having a physical exam or taking a questionnaire.
There is very little risk to having a blood test. You may have slight pain or bruising at the spot where the needle was put in, but most symptoms go away quickly.
What do the results mean?
Usually, the provider who did the screening will explain the results. If the results show signs of a mental health disorder, the next steps depend on the type of disorder and how serious it may be.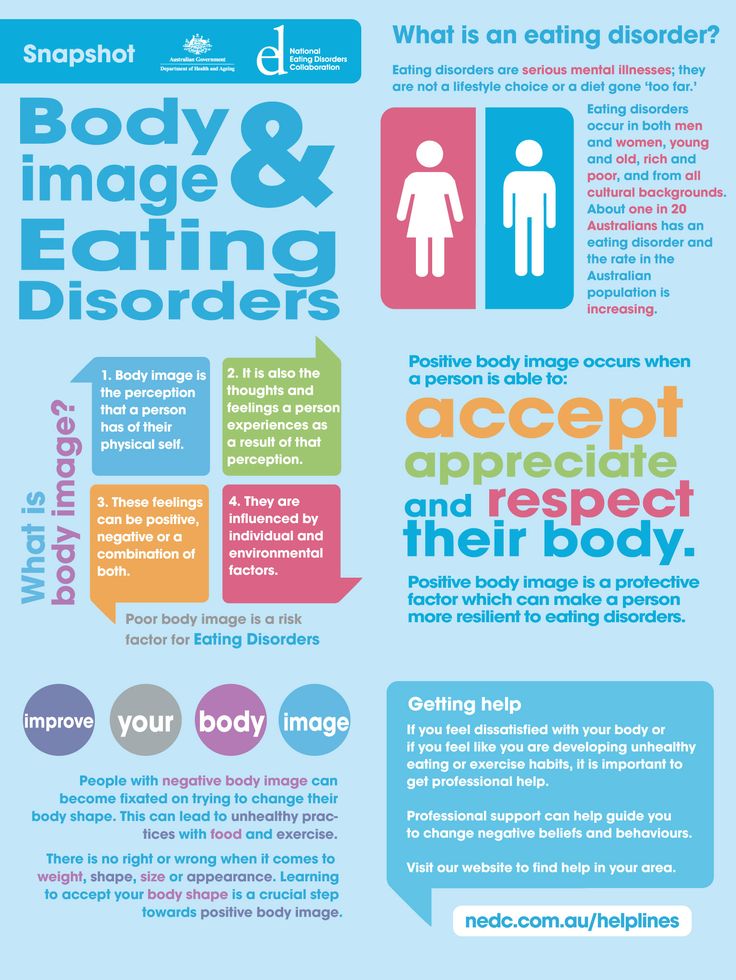 If a primary care provider did the screening, the provider may:
If a primary care provider did the screening, the provider may:
- Talk with you about treatments
- Order tests to check for other health problems that may be causing symptoms
- Refer you or your child to a mental health provider
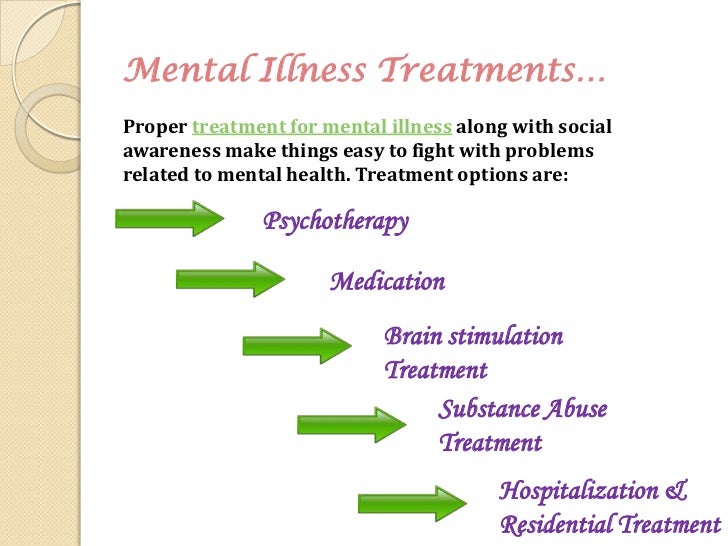
A mental health provider may do more tests to confirm a diagnosis and help develop a treatment plan. Starting treatment as soon as possible may improve the chance of recovery.
Learn more about laboratory tests, reference ranges, and understanding results.
Is there anything else I need to know about a mental health screening?
There are many types of mental health providers who treat mental disorders. Your or your child's primary health care provider or school can help you find the right support.
These are some of the providers who have training to treat mental health disorders:
- Psychiatrists are medical doctors who specialize in mental health. Psychiatrists can prescribe medicine.
- Psychologists generally have doctoral degrees, but they do not have medical degrees. They can't prescribe medicine unless they have a special license. Some psychologists work with providers who can prescribe medicine. Psychologists may use one-on-one counseling and/or group therapy sessions.
- Psychiatric-mental health nurses are nurses with special training in mental health problems. Nurses who may have a master's or doctoral degree in psychiatric-mental health nursing include, advanced practice registered nurses (APRNs), certified nurse practitioners (CNPs), and clinical nurse specialists (CNSs). In some states, certain nurses can prescribe medicines.
- Licensed clinical social workers have at least a master's degree in social work with special training in mental health. They can't prescribe medicine, but may work with providers who can prescribe medicine. Providers who are licensed clinical social workers usually have LCSW or LICSW after their names.

- Licensed professional counselors (LPC) may also be called clinicians or therapists. States have different names of these licenses, such as LMFT (licensed marriage and family therapist). These professionals usually have a master's degree in a field related to mental health. They can't prescribe medicine but may work with providers who can prescribe.
References
- American Academy of Pediatrics [Internet]. Elk Grove Village (IL): American Academy of Pediatrics; c2022. Patient Care: Screening Tools: Pediatric Mental Health Minute Series; [cited 2022 Oct 18]; [about 6 screens]. Available from: https://www.aap.org/en/patient-care/mental-health-minute/screening-tools/
- American Psychiatric Nurses Association [Internet]. Falls Church (VA): American Psychiatric Nurses Association; Psychiatric Mental Health Nurses; [cited 2022 Oct 12]; [about 1 screen]. Available from: https://www.apna.org/about-psychiatric-nursing/?pageid=3292
- American Psychological Association [Internet].
 Washington D.C.: American Psychological Services Inc.; c2022. Distinguishing Between Screening and Assessment for Mental and Behavioral Health Problems; [2014 Dec; cited 2022 Oct 18]; [about 3 screens]. Available from: https://www.apaservices.org/practice/reimbursement/billing/assessment-screening?_ga=2.102075329.1186226343.1666222147-627372789.1666222147
Washington D.C.: American Psychological Services Inc.; c2022. Distinguishing Between Screening and Assessment for Mental and Behavioral Health Problems; [2014 Dec; cited 2022 Oct 18]; [about 3 screens]. Available from: https://www.apaservices.org/practice/reimbursement/billing/assessment-screening?_ga=2.102075329.1186226343.1666222147-627372789.1666222147 - Centers for Disease Control and Prevention [Internet]. Atlanta: U.S. Department of Health and Human Services: Children's Mental Health [updated 2022 Jun 3; cited 2022 Oct 12]; [about 3 screens]. Available from: https://www.cdc.gov/childrensmentalhealth/index.html
- Centers for Disease Control and Prevention [Internet]. Atlanta: U.S. Department of Health and Human Services; Learn About Mental Health [updated 2021 Jun 28; cited 2022 Oct 12]; [about 2 screens]. Available from: https://www.cdc.gov/mentalhealth/learn
- Giardino A. Pediatric Depression Workup. [Update 2017 Nov 15; cited 2022 Oct 18]. In Medscape eMedicine:Drugs & Disease [Internet].
 Atlanta (GA): WebMD LLC; c. 1994-2022. Available from: https://emedicine.medscape.com/article/914192-workup
Atlanta (GA): WebMD LLC; c. 1994-2022. Available from: https://emedicine.medscape.com/article/914192-workup - Healthfinder.gov. [Internet]. Washington D.C.: Office of Disease Prevention and Health Promotion; U.S. Department of Health and Human Services; Get Your Teen Screened for Depression; [updated 2022 Jul 15; cited 2022 Oct 18]; [about 5 screens]. Available from: https://health.gov/myhealthfinder/healthy-living/mental-health-and-relationships/get-your-teen-screened-depression#the-basics-tab
- Johns Hopkins Medicine [Internet]. The Johns Hopkins University, The Johns Hopkins Hospital, and Johns Hopkins Health System; c2022. Health: Blood Test; [cited 2022 Oct 18]; [about 3 screens]. Available from: https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/blood-test
- Mayo Clinic [Internet]. Mayo Foundation for Medical Education and Research; c1998–2022. Mental health providers: Tips on finding one; [cited 2022 Oct 12]; [about 5 screens]. Available from: https://www.
 mayoclinic.org/diseases-conditions/mental-illness/in-depth/mental-health-providers/art-20045530
mayoclinic.org/diseases-conditions/mental-illness/in-depth/mental-health-providers/art-20045530 - Mayo Clinic [Internet]. Mayo Foundation for Medical Education and Research; c1998–2022. Mental illness: Diagnosis and treatment; [cited 2022 Oct 12]; [about 11 screens]. Available from: https://www.mayoclinic.org/diseases-conditions/mental-illness/diagnosis-treatment/drc-20374974
- Mayo Clinic [Internet]. Mayo Foundation for Medical Education and Research; c1998–2022. Mental illness in Children: Know the Signs; [cited 2022 Oct 18]; [about 7 screens]. Available from: https://www.mayoclinic.org/healthy-lifestyle/childrens-health/in-depth/mental-illness-in-children/art-20046577
- Mayo Clinic [Internet]. Mayo Foundation for Medical Education and Research; c1998–2022. Mental illness: Symptoms and causes; [cited 2022 Oct 12]; [about 7 screens]. Available from: https://www.mayoclinic.org/diseases-conditions/mental-illness/symptoms-causes/syc-20374968
- Michigan Medicine: University of Michigan [Internet].
 Ann Arbor (MI): Regents of the University of Michigan; c1995–2022. Mental Health Assessment; [updated 2022 Feb 9; cited 2022 Oct 12]; [about 6 screens]. Available from: https://www.uofmhealth.org/health-library/aa79756#tp16777
Ann Arbor (MI): Regents of the University of Michigan; c1995–2022. Mental Health Assessment; [updated 2022 Feb 9; cited 2022 Oct 12]; [about 6 screens]. Available from: https://www.uofmhealth.org/health-library/aa79756#tp16777 - MentalHealth.gov [Internet]. Washington (DC): U.S. Department of Health and Human Services; What to Look For; [updated 2022, Mar 10; cited 2022 Oct 10]; [about 2 screens]. Available from: https://www.mentalhealth.gov/what-to-look-for
- National Alliance on Mental Illness [Internet]. Arlington (VA): NAMI; c2022. Warning Signs and Symptoms; [cited 2022 Oct 12]; [about 2 screens]. Available from: https://www.nami.org/About-Mental-Illness/Warning-Signs-and-Symptoms
- National Alliance on Mental Illness [Internet]. Arlington (VA): NAMI; c2022. Types of Mental Health Professionals; [cited 2022 Oct 12]; [about 3 screens]. Available from: https://www.nami.org/About-Mental-Illness/Treatments/Types-of-Mental-Health-Professionals
- National Institute of Mental Health [Internet].
 Bethesda (MD): U.S. Department of Health and Human Services; Child and Adolescent Mental Health; [reviewed 2021 May; cited 2022 Oct 18]; [about 5 screens]. Available from: https://www.nimh.nih.gov/health/topics/child-and-adolescent-mental-health
Bethesda (MD): U.S. Department of Health and Human Services; Child and Adolescent Mental Health; [reviewed 2021 May; cited 2022 Oct 18]; [about 5 screens]. Available from: https://www.nimh.nih.gov/health/topics/child-and-adolescent-mental-health - National Institute of Mental Health [Internet]. Bethesda (MD): U.S. Department of Health and Human Services; Chronic Illness and Mental Health: Recognizing and Treating Depression; [revised 2021; cited 2022 Oct 18]; [about 6 screens]. Available from: https://www.nimh.nih.gov/health/publications/chronic-illness-mental-health
- National Institute of Mental Health [Internet]. Bethesda (MD): U.S. Department of Health and Human Services; Eating Disorders; [updated 2021 Dec; cited 2022 Oct 12]; [about 3 screens]. Available from: https://www.nimh.nih.gov/health/topics/eating-disorders
- National Institute of Mental Health [Internet]. Bethesda (MD): U.S. Department of Health and Human Services; Mental Illness; [updated 2022 Jan; cited 2022 Oct 12]; [about 7 screens].
 Available from: https://www.nimh.nih.gov/health/statistics/mental-illness
Available from: https://www.nimh.nih.gov/health/statistics/mental-illness - Patti L, Gupta M. Change in Mental Status. [Updated 2022 Aug 8; cited 2022 Oct 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441973/
Personality Disorders: MedlinePlus
On this page
Basics
- Summary
- Start Here
- Treatments and Therapies
Learn More
- Specifics
See, Play and Learn
- No links available
Research
- Statistics and Research
- Clinical Trials
- Journal Articles
Resources
- Find an Expert
For You
- Patient Handouts
Personality disorders are a group of mental illnesses.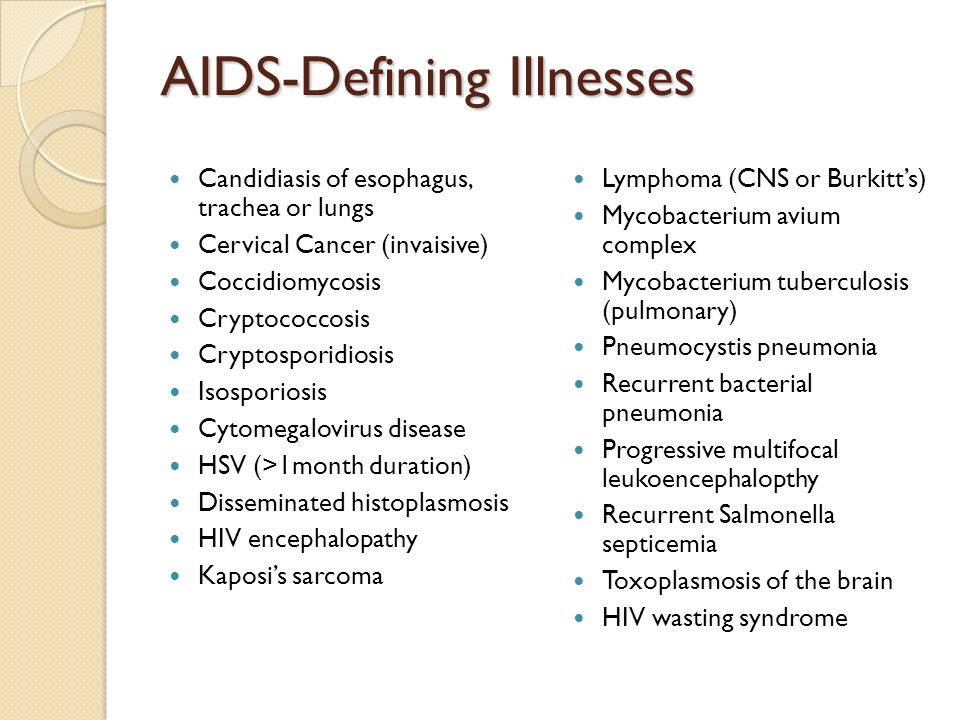 They involve long-term patterns of thoughts and behaviors that are unhealthy and inflexible. The behaviors cause serious problems with relationships and work. People with personality disorders have trouble dealing with everyday stresses and problems. They often have stormy relationships with other people.
They involve long-term patterns of thoughts and behaviors that are unhealthy and inflexible. The behaviors cause serious problems with relationships and work. People with personality disorders have trouble dealing with everyday stresses and problems. They often have stormy relationships with other people.
The cause of personality disorders is unknown. However, genes and childhood experiences may play a role.
The symptoms of each personality disorder are different. They can mild or severe. People with personality disorders may have trouble realizing that they have a problem. To them, their thoughts are normal, and they often blame others for their problems. They may try to get help because of their problems with relationships and work. Treatment usually includes talk therapy and sometimes medicine.
- Personality Disorders (Mental Health America)
- Borderline Personality Disorder: Psychotherapy (Borderline Personality Disorder Resource Center)
- Mental Health Medications (National Institute of Mental Health)
- Psychotherapies (National Institute of Mental Health)
- Borderline Personality Disorder (Mayo Foundation for Medical Education and Research)
- Borderline Personality Disorder (National Institute of Mental Health)
- Narcissistic Personality Disorder (Mayo Foundation for Medical Education and Research)
- Paranoia and Delusional Disorders (Mental Health America)
- Schizoid Personality Disorder (Mayo Foundation for Medical Education and Research)
- Schizotypal Personality Disorder (Mayo Foundation for Medical Education and Research)
- Personality Disorders (National Institute of Mental Health)
- ClinicalTrials.
 gov: Antisocial Personality Disorder (National Institutes of Health)
gov: Antisocial Personality Disorder (National Institutes of Health) - ClinicalTrials.gov: Borderline Personality Disorder (National Institutes of Health)
- ClinicalTrials.
 gov: Personality Disorders (National Institutes of Health)
gov: Personality Disorders (National Institutes of Health)
- Article: Sexual Dream Experiencing and Personality Disorder Functioning Styles in Frequent Sexual.
 ..
.. - Article: Development and validation of an instrument to measure personality in adolescence:...
- Article: Personality descriptions influence perceived cuteness of children and nurturing motivation toward.
 ..
.. - Personality Disorders -- see more articles
- APA District Branch / State Association Directory (American Psychiatric Association)
- FindTreatment.
 gov (Substance Abuse and Mental Health Services Administration)
gov (Substance Abuse and Mental Health Services Administration) - Help for Mental Illnesses (National Institute of Mental Health) Also in Spanish
- NAMI
- National Institute of Mental Health Also in Spanish
Mental illness - Adamant Medical Clinic
Adamant
medical clinic
St.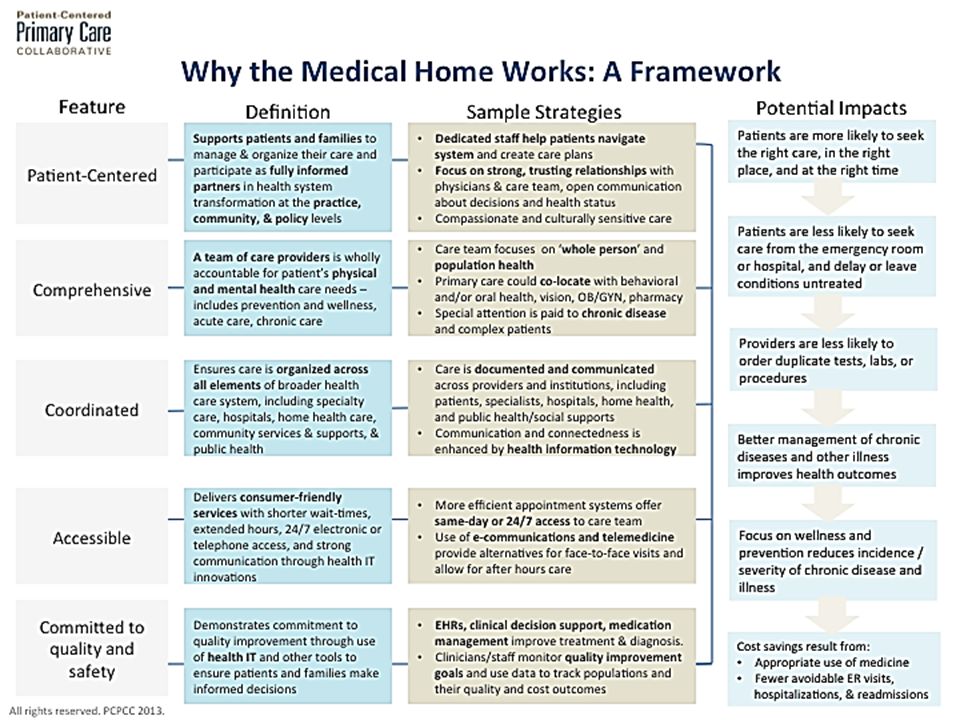 Petersburg, embankment of the river Moika, 78.
Petersburg, embankment of the river Moika, 78.
+7 (812) 740-20-90
Content:
Mental illness - in a broad sense, this is a state of the human psyche that is different from normal.
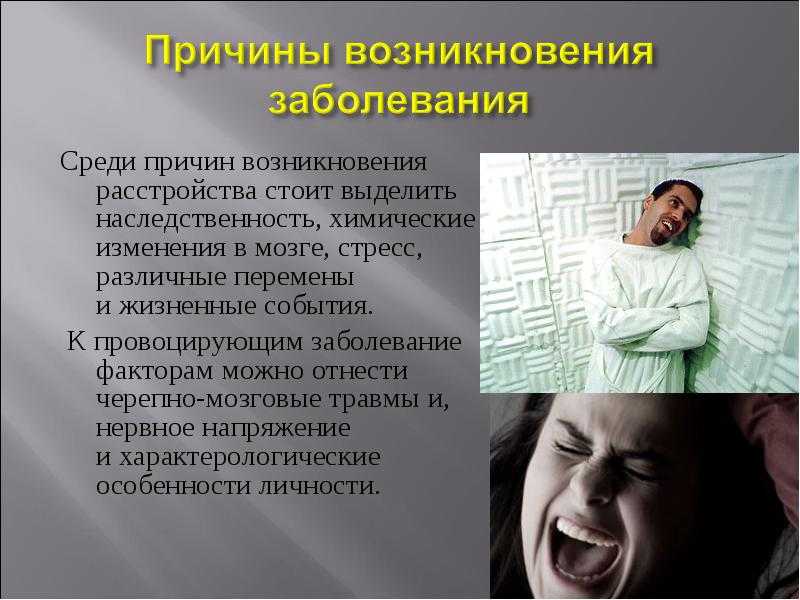
Any disturbance of the mental state is associated with changes in the structure or functions of the brain. They are exogenous, when a person is influenced by external factors - such as various toxic substances, injuries, viruses, etc. Separately, endogenous factors are distinguished - these are hereditary and gene diseases, chromosome disorders, etc.
Mental illness can significantly harm the patient and those around him. That is why they require immediate medical attention. The main difficulty here is to identify the presence of a mental disorder.
List of mental illnesses
Below is a list and description of mental illnesses.
- Conditions caused by diseases of the brain - the patient has impaired cognitive functions (learning, thinking, memory), and may also show hallucinations, delusions and mood swings.
- Schizophrenia - abrupt changes in the nature of the patient, a change in the sphere of interests and the emergence of unusual hobbies, decreased performance. In the extreme form, the patient has absolutely no sanity and awareness of the events that are happening around.
- Neuroses, phobias - a group of psychological diseases of a person that cause panic attacks, paranoia, chronic stress and somatic deviations in a patient when faced with certain objects, situations and phenomena.
- Conditions that are caused by violations of physiology - the patient is unable to eat (overeating, anorexia, etc.), sleep (hypersomnia, insomnia, etc.) and all kinds of sexual deviations (increased libido, frigidity, etc.).
- Affective disorders - a description of a group of mental illnesses includes baseless cardinal mood swings, all kinds of mania, depressive states of various etiologies and course.
- Mental retardation is a congenital mental disorder, which is characterized by a decrease in intellectual functions.
- Personality disorders in adulthood - a disorder of sexual preferences (pedophilia, fetishism, etc.), a violation of self-identification by gender (transvestism, transsexualism, etc.), a violation of habits and inclinations (pyromania, gambling, etc.)
This list of mental illnesses is general and describes the most common symptoms to which patients are susceptible. If they are found, seek medical attention immediately. Remember that in the absence of treatment for mental illness, a sick person is dangerous for himself and his loved ones!
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- W
- B
- S
- B
- E
- S
- I
- WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Events
- Photo reports
- Questions and answers
- Latest information
- Emergencies "
- News "
- Disease Outbreak News
- WHO Data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Schizophrenia
Key Facts- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.
- Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life.
- People with schizophrenia are often subject to stigma, discrimination and human rights violations.
- Worldwide, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective options for helping patients with schizophrenia, which can lead to a complete recovery of at least one in three patients.
Symptoms
Schizophrenia is characterized by significant disturbances in the perception of reality and behavioral changes, such as:
- News bulletin
- persistent hallucinations: the patient hears, sees, touches non-existent things and smells non-existent smells;
- feeling of external influence, control or passivity: the presence in the patient of the feeling that his feelings, impulses, actions or thoughts are dictated from outside, put in or disappear from consciousness by someone else's will, or that his thoughts are broadcast to others;
- disorganized thinking, often expressed in incoherent or pointless speech;
- Significant disorganization of behavior, which manifests itself, for example, in the performance by the patient of actions that may seem strange or meaningless, or in an unpredictable or inappropriate emotional reaction that does not give the patient the opportunity to organization of their behavior;
- "negative symptoms" such as extreme poverty of speech, smoothness of emotional reactions, inability to feel interest or pleasure, social autism; and/or
- Extreme agitation or, on the contrary, slowness of movements, freezing in unusual postures.
People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of people with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms.
Magnitude of the problem and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease.
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.
People with schizophrenia are 2-3 times more likely to die early than the population average (2). It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment.
Humanitarian emergencies and health crises can cause severe stress and fear, disrupt social support mechanisms, lead to isolation and disruption of health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease. People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion.
People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion.
Causes of schizophrenia
Science has not established any one cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.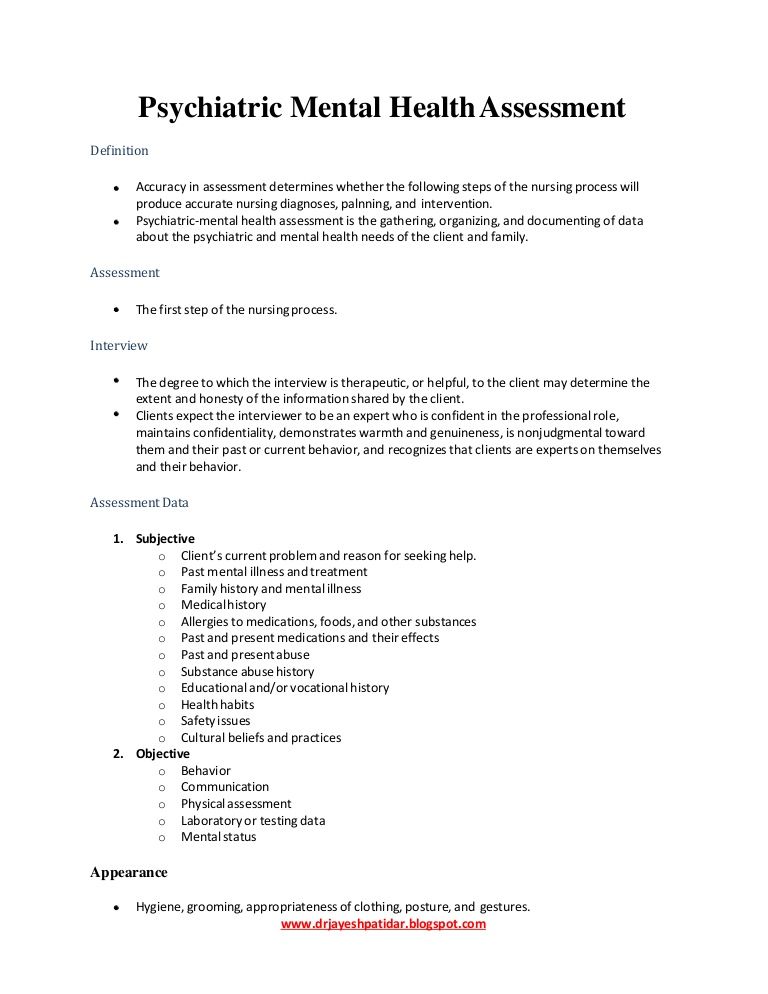
The available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective treatment for mental disorders and is regularly associated with violations of the fundamental rights of patients with schizophrenia. Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is essential the patient with schizophrenia, his family members and members of local communities.
Schizophrenia management and care
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg, life skills education).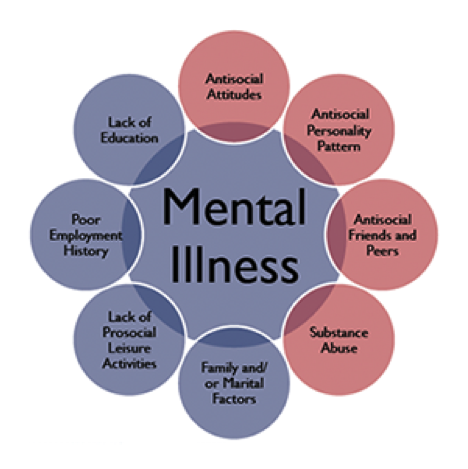 The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
WHO action
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care.
The WHO Mental Health Gap Action Program (mhGAP) is developing evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings. The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services. health in accordance with international human rights standards, including the UN Convention on the Rights of Persons with Disabilities.
Bibliography
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J.