Dysthymia depression treatment
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery.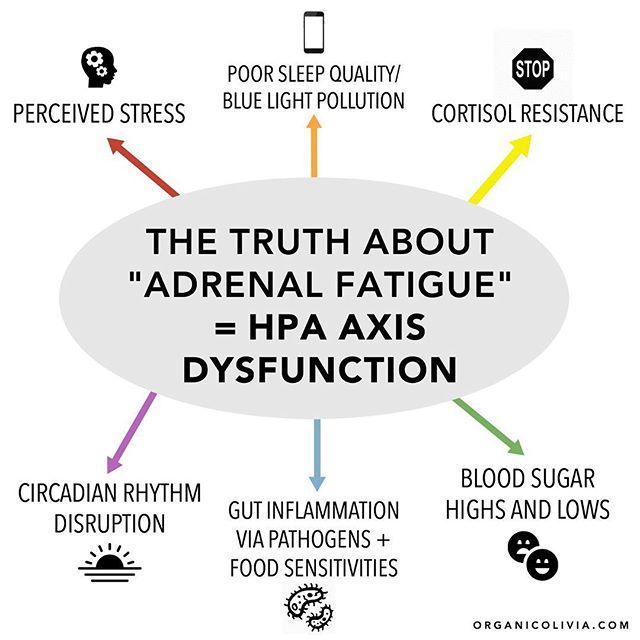 Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers.
 The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH) - Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
- The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.
 4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH) - Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.
 7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month.
 The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people). - Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 01/05/2023
Symptoms of dysthymia, treatment of dysthymia at the Allianz Central Medical Health Center
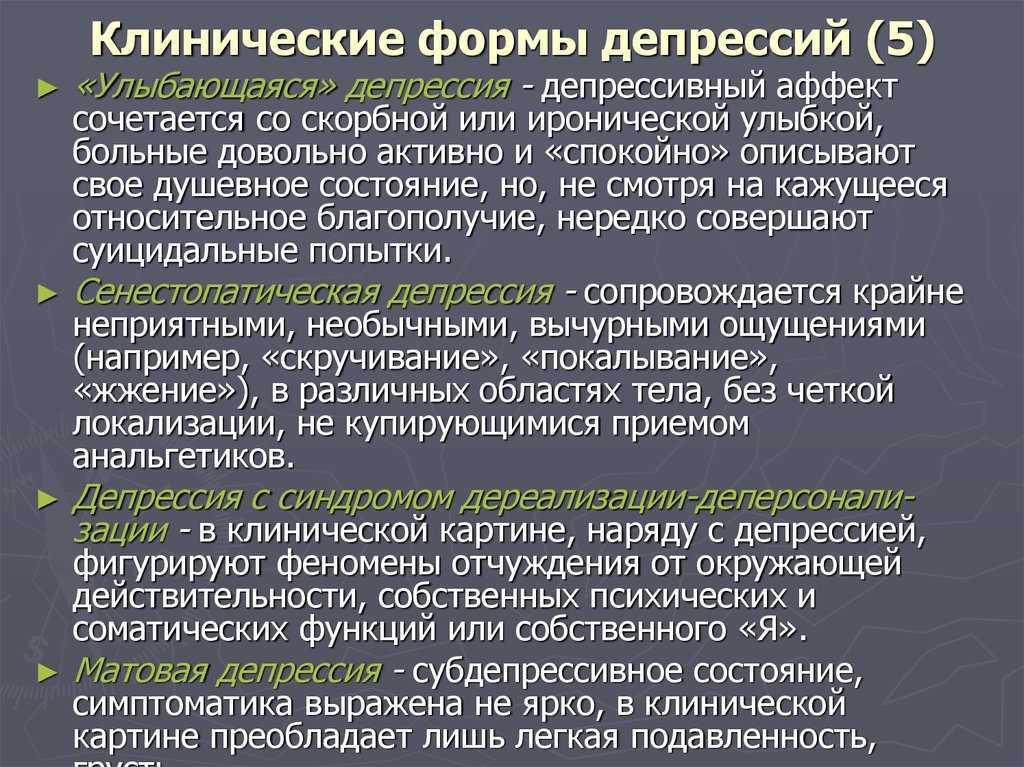
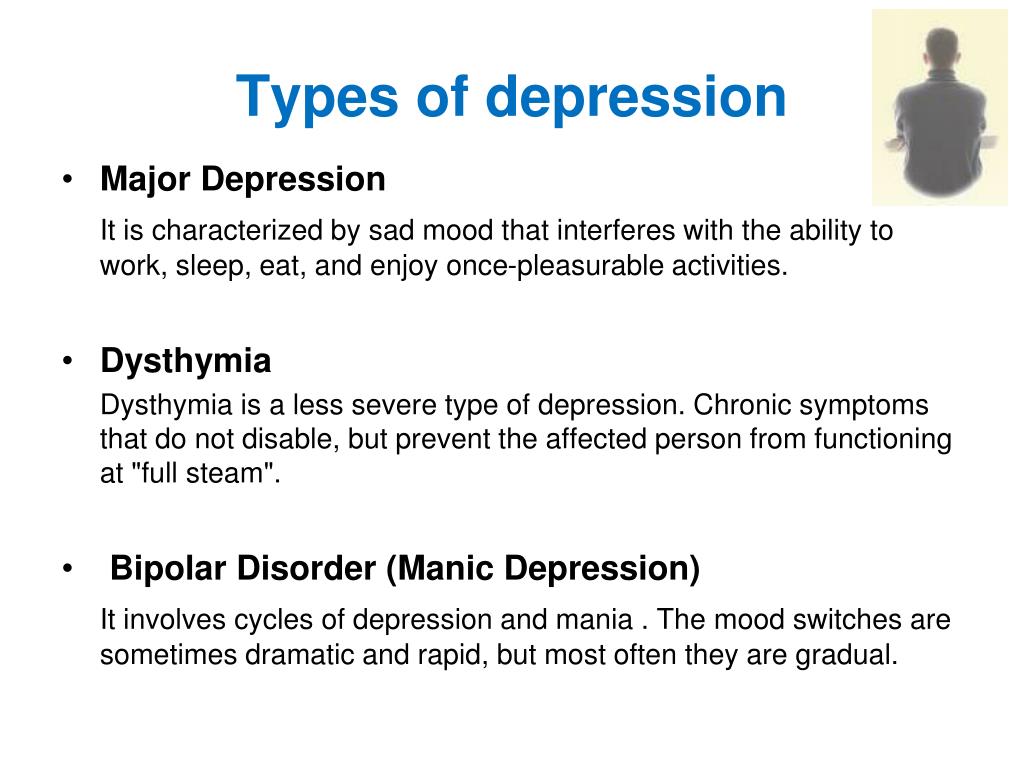
Dysthymia is a long-term mild depression that, in terms of the severity of symptoms, does not reach the classic depression, but in terms of duration it exceeds it. At various times, this condition was called neurotic depression, endoreactive dysthymia, chronic depressive disorder. One thing remains constant, dysthymia is a disorder that can and should be treated.
Despite the "lightness" - low severity of manifestations, dysthymia significantly affects the life and performance of a person.
Therefore, it must be treated by a psychotherapist.
Signs and symptoms of dysthymia
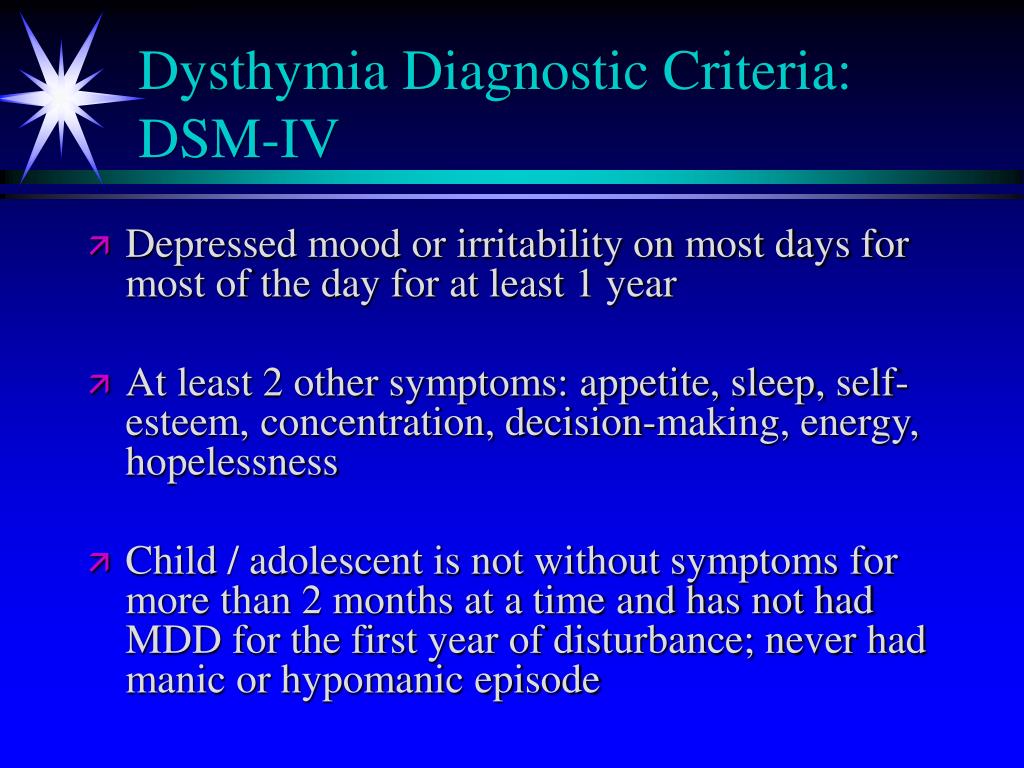
The diagnostic criteria for the disorder are difficult to recognize in practice, even for a specialist.
Dysthymia, the symptoms of which are similar to those of recurrent depression, can begin as early as adolescence. Compared to a recurrent disorder, its manifestations are less pronounced and stretched over time - for two years or more. If the maturation of the personality occurs under the distorting influence of dysthymia, then such a person, having matured, perceives the signs of the disorder as part of his "melancholy nature". And only a professional can separate the constitutional and personal characteristics of a person from the symptoms of the disease.
Below are the main signs that must be present for at least two years in a row (at adolescence - 1 year). There may be episodes of improvement lasting no more than a few weeks.
- decreased ability to concentrate;
- negative assessment of the future, present, and past.
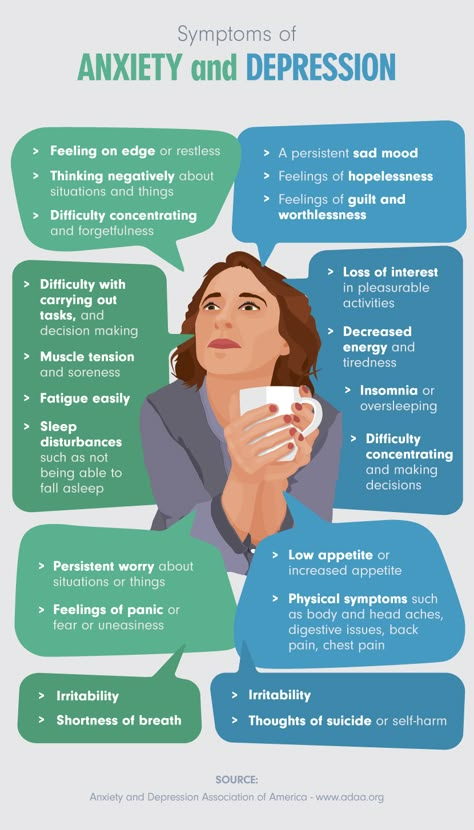 Alternatively, the past can, on the contrary, be idealized, and then the state acquires the features of a nostalgic depression;
Alternatively, the past can, on the contrary, be idealized, and then the state acquires the features of a nostalgic depression; - feeling of uselessness, hopelessness;
- decreased or, rarely, increased appetite;
- insomnia, daytime sleepiness;
- decline in vitality;
- reduced self-confidence, self-esteem;
- decreased libido;
- lack of pleasure from what used to bring joy.
The longer a person is sick, the worse his quality of life becomes - other diseases join (addiction to psychoactive substances, panic attacks, social phobia), the transition of the disease to bipolar affective disorder is also possible.
Important
If the disorder is not treated, against the background of the above described signs of dysthymia, severe depressive episodes occur - the so-called double depressions.
Dysthymia diagnostics
The diagnosis is made by a psychotherapist after a clinical and anamnestic examination. It includes an assessment of symptoms, the order in which they appear, and their connection with events in a person's life - stress, overload, trauma, infectious or other diseases.
It includes an assessment of symptoms, the order in which they appear, and their connection with events in a person's life - stress, overload, trauma, infectious or other diseases.
To confirm the diagnosis, a clinical psychologist performs a pathopsychological study. It gives a conclusion about the characteristics of the patient's personality and reveals deviations in cognitive processes (thinking, memory, attention).
For differential diagnosis, instrumental and laboratory studies are carried out:
- EEG - with organic damage to the nervous system;
- Neurophysiological test system and Neurotest with endogenous diseases (schizophrenia, schizotypal disorder).
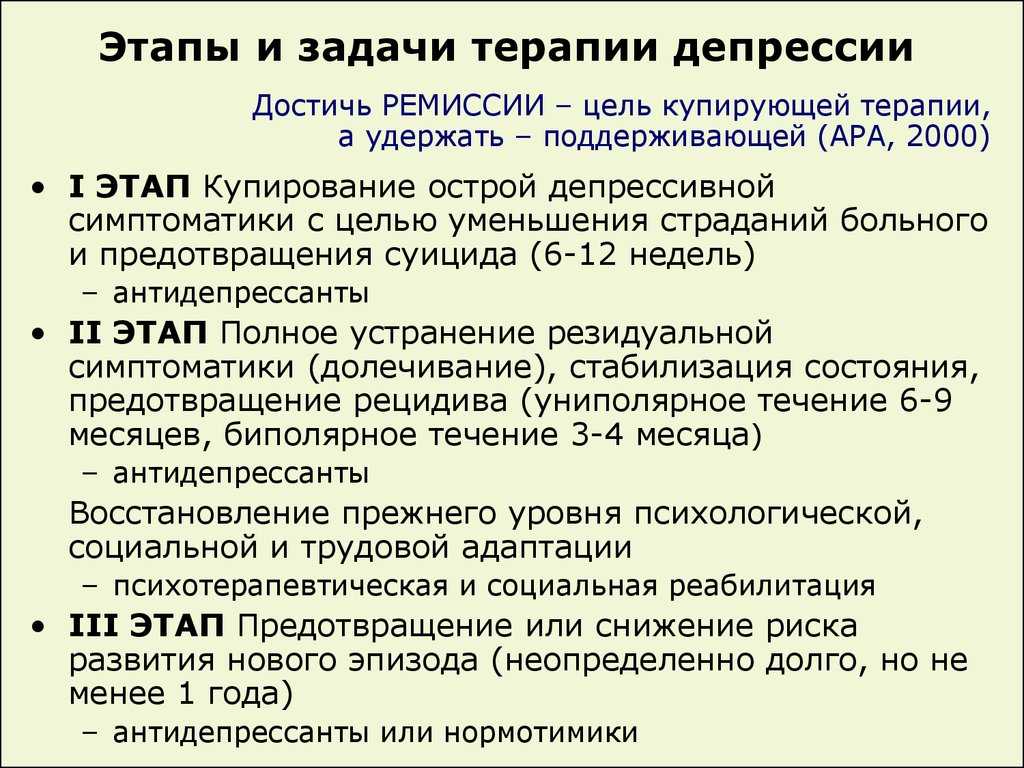
Dysthymia - treatment
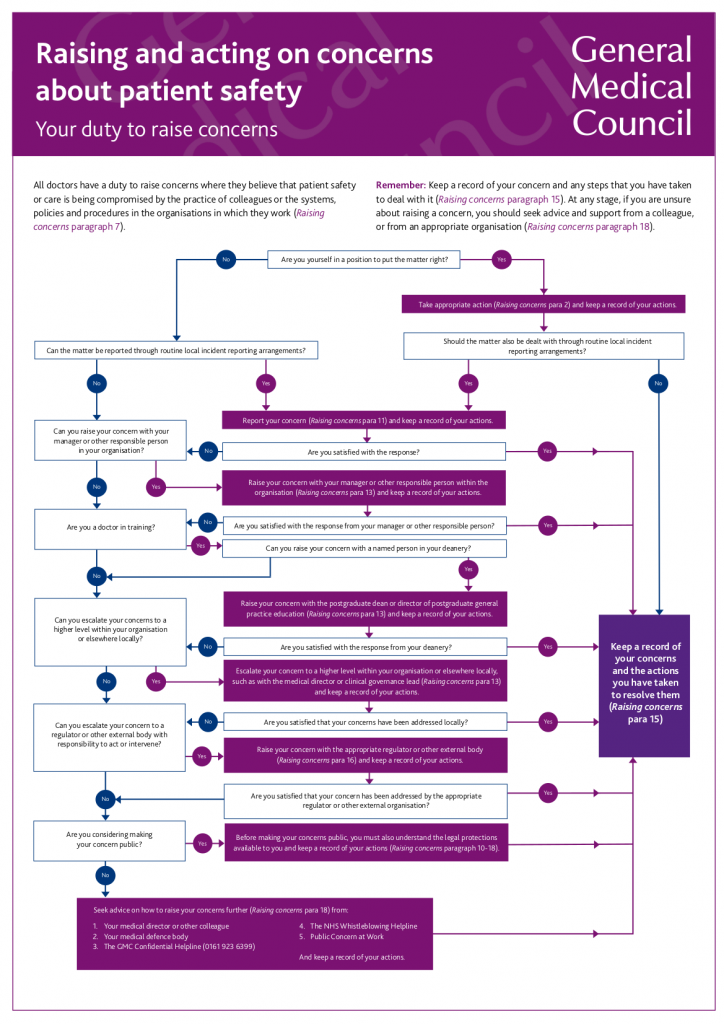
After confirming the diagnosis of "dysthymia", treatment is prescribed individually and includes three main areas:
- Psychotherapy.
- Medical support.
- Treatment of associated diseases.
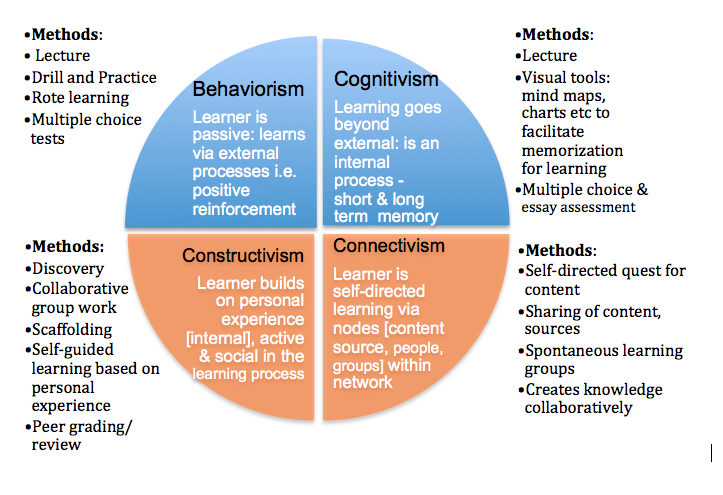
Psychotherapy. From the point of view of evidence-based medicine, the direction of choice is cognitive-behavioral therapy, however, depending on the specific situation, personal characteristics, as well as the preferences of the client, rational, family, group psychotherapy, biofeedback therapy or psychoanalytic therapy are used.
From the point of view of evidence-based medicine, the direction of choice is cognitive-behavioral therapy, however, depending on the specific situation, personal characteristics, as well as the preferences of the client, rational, family, group psychotherapy, biofeedback therapy or psychoanalytic therapy are used.
Some researchers attribute dysthymia to personality disorders (congenital character traits). This confirms that the main method of treatment is psychotherapy, that is, the joint work of the patient and the doctor on attitudes, attitudes towards life, the ability to deal with symptoms and achieve goals.
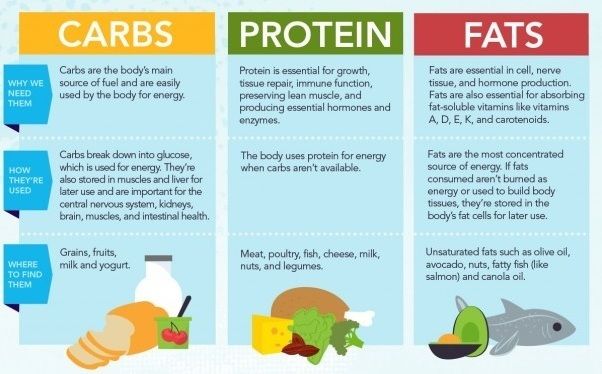
Drug therapy is aimed at neutralizing the symptoms of dysthymia and maintaining the mood and emotional-volitional sphere of the individual within the normal range. Medical way out of the state of chronic depression allows the development of psychotherapeutic intervention.
Treatment of associated diseases - secondary diseases that have developed against the background of dysthymia: addiction to psychoactive substances, panic attacks and generalized anxiety disorder, social phobia.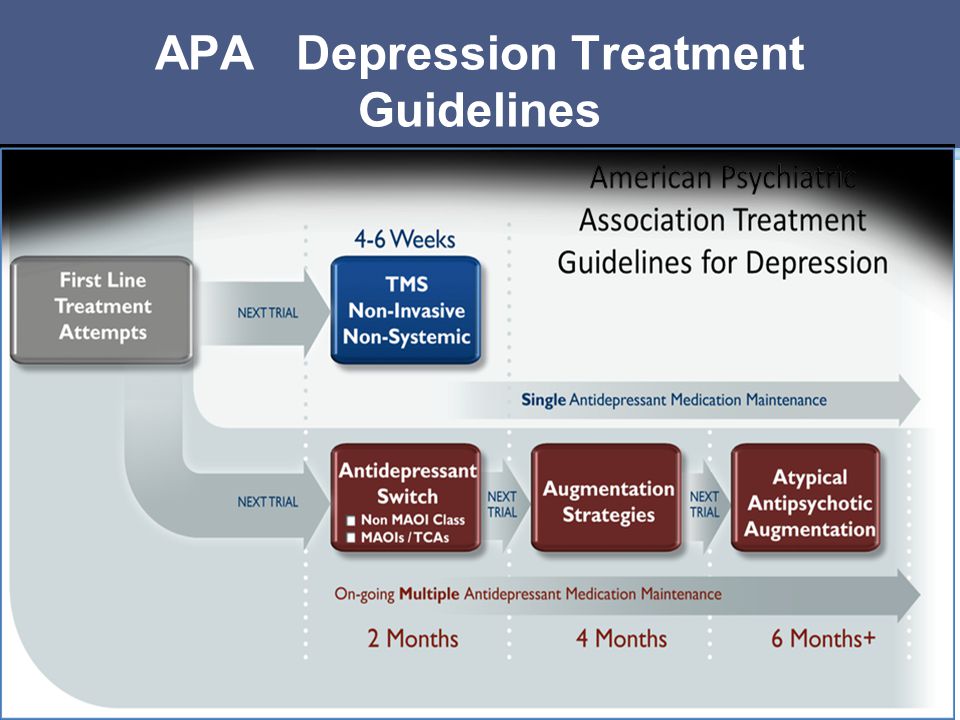 This group also includes general medical diseases, the course of which can renew dysthymia in a predisposed person. To exclude these diseases and ensure the adequacy of treatment, a full-fledged diagnosis by a psychotherapist is required.
This group also includes general medical diseases, the course of which can renew dysthymia in a predisposed person. To exclude these diseases and ensure the adequacy of treatment, a full-fledged diagnosis by a psychotherapist is required.
What is dysthymia and how does it differ from depression
Sometimes depression seems to become part of the personality - this is the danger of dysthymia. Recognizing it is more difficult than depression. Read more about how to do this in the RBC Trends review
What is dysthymia
The term dysthymia comes from the Greek roots "dys" - "disease" and "thymia" - "mind" or "emotions".
Dysthymia is a prolonged (chronic) but milder form of depression. With dysthymia, a person loses interest in normal daily activities and lives with a sense of hopelessness. In a patient with chronic depression, self-esteem decreases, productivity decreases, and a sense of the adequacy of what is happening is lost. This condition can last for years and significantly affect relationships, work, school, and any other daily activity.
One of the main problems of dysthymia is that often sufferers of it, like those around them, accept the disease as part of their personality. A person suffering from chronic depression may be described as a "gloomy person" who constantly complains and is unable to have fun.
Dysthymia Prevalence
According to the National Institute of Mental Health, approximately 1.5% of American adults have dysthymia. In Russia, according to reports from the Ministry of Emergency Situations, dysthymic disorders are more common - up to 4.5-5% of citizens suffer from them. At the same time, in various emergency situations, such as a pandemic, for example, the number of people suffering from chronic forms of depression increases to 31.4% of the country's population.
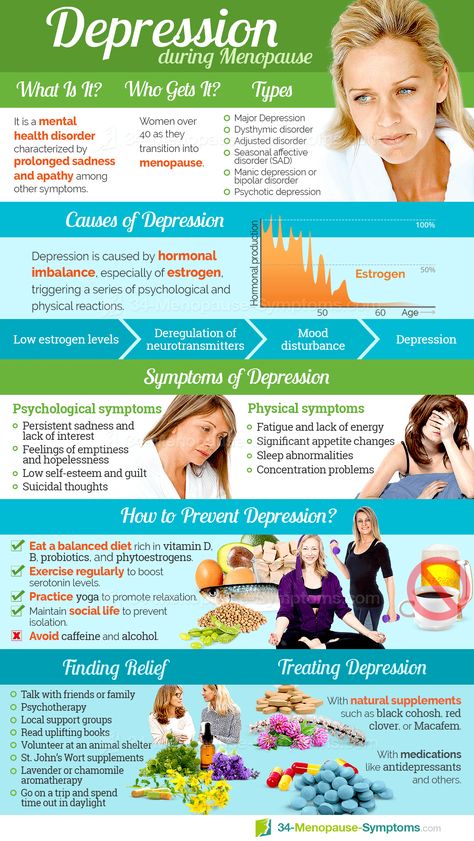
Women are more likely than men to suffer from dysthymia. The disease can begin both in adolescence and in adulthood, but in Russia, most cases occur in people from 18 to 45 years old.
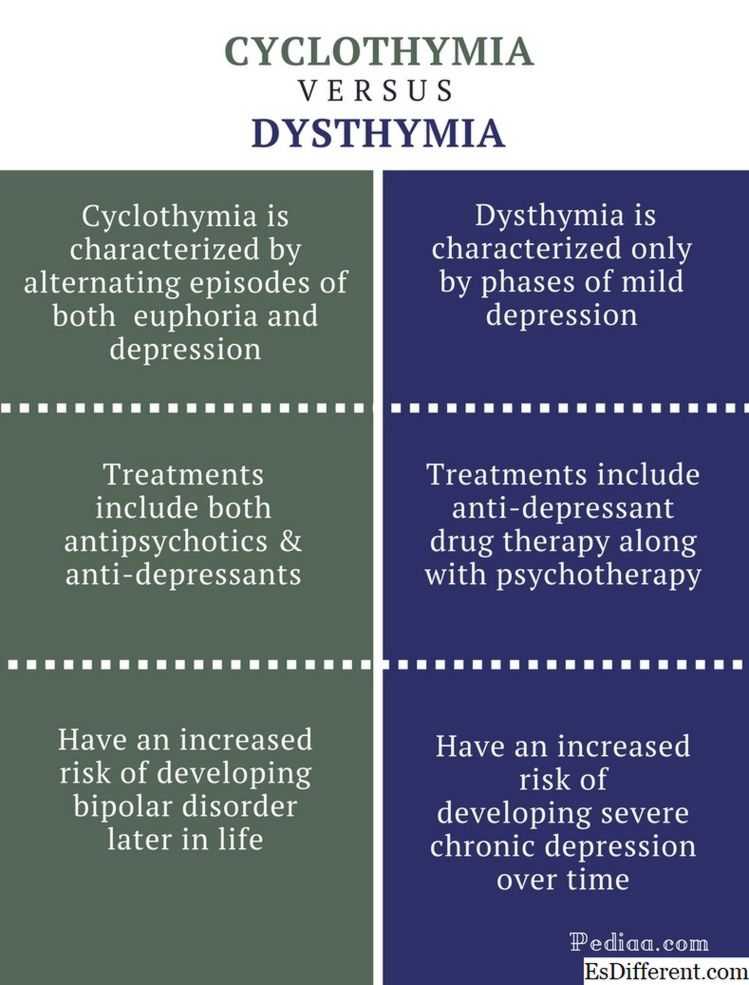
How dysthymia differs from depression
Roughly speaking, dysthymia is depression, but it has become chronic. With dysthymia, depressive symptoms do not disappear for two or more years, while they are regular. People with depression may have days or periods when they feel normal. Dysthymia is always bad, and it is usually accompanied by eating disorders. Bouts of double depression can also occur - when deeper depressive episodes are periodically added to moderate dysthymia. Double depression occurs in 75% of people with dysthymia.
With dysthymia, depressive symptoms do not disappear for two or more years, while they are regular. People with depression may have days or periods when they feel normal. Dysthymia is always bad, and it is usually accompanied by eating disorders. Bouts of double depression can also occur - when deeper depressive episodes are periodically added to moderate dysthymia. Double depression occurs in 75% of people with dysthymia.
Dysthymia is a serious disorder. Because its symptoms may be less pronounced than those of severe clinical depression, it can be tempting to think of it as some kind of intermediate state between the norm and the disease. In fact, dysthymia is even more like a disability than classic depression, and the risks of suicidal behavior are more pronounced with it.
Symptoms of dysthymia
Signs of dysthymia are very similar to symptoms of clinical depression. The main difference lies in the length of time - at least two years for adults and a year for children and adolescents.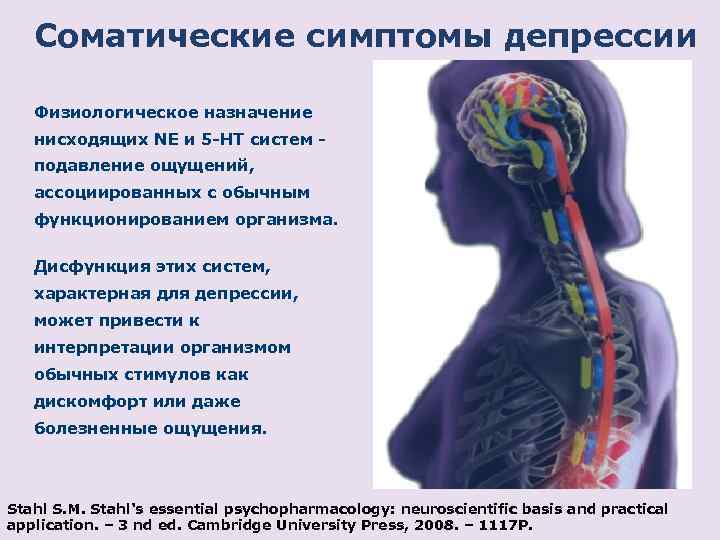
How to recognize dysthymia:
- decreased performance;
- feeling of guilt;
- feeling of helplessness;
- sadness;
- hopelessness;
- overeating or malnutrition;
- irritability;
- fatigue and lack of energy;
- loss of interest and pleasure in daily activities;
- bad mood;
- low self-esteem;
- sleep problems;
- Difficulty making decisions and concentrating.
To suspect dysthymia, only two symptoms persist for a long time. However, even if all the symptoms coincided, it is impossible to diagnose yourself (and even more so to self-medicate) - this is just an excuse to consult a specialist.
Causes of dysthymia
Primary or "pure" dysthymia is distinguished - it begins at an early age (before 21 years) and by itself, without connection with any other mental disorders. Secondary dysthymia begins against the background of an already existing mental or somatic disease.
The exact cause of dysthymia, like depression, is usually impossible to determine, but there are some factors that can have a negative effect:
- The balance of brain neurotransmitters. Traumatic brain injuries, stress and anxiety can change the ratio of chemicals in the brain - they affect the mood and behavior of a person. Antidepressants affect the balance of neurotransmitters.
- Environmental factors. Loss of a job, social isolation, the experience of the death of a loved one, or major political catastrophes can cause mental trauma, leading to depression or dysthymia.
- Genetics . The tendency to mental disorders may be congenital. If one of the relatives had depression, then the risk of its development increases for all blood members of the family.
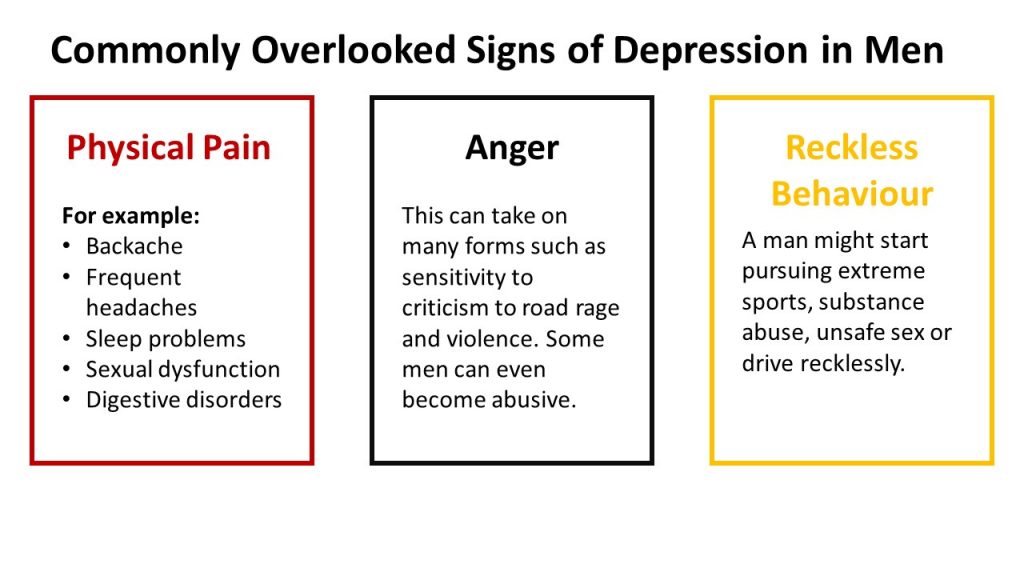
Factors can overlap - this also increases the risk of dysthymia. Dysthymia usually develops as a result of chronic stress or as a reaction to a physical disability. In men, a decrease in testosterone can also be the cause of prolonged depression.
In men, a decrease in testosterone can also be the cause of prolonged depression.
One of the main dangers is that neuropsychiatric diseases can be accompanied or caused by malfunctions of the thyroid gland. Therefore, antidepressants alone or talking therapy may not help, and when contacting a psychotherapist, you can ask about the need for an analysis of TSH. Also, dysthymia often occurs with heart disease, oncology, or against the background of substance abuse.
Achievement causes dysthymia
There are studies linking an increased risk of dysthymia and anxiety disorders in people with high levels of perfectionism. In this case, chronic depression occurs against the background of a protracted motivational conflict. Perfectionists strive for the impossible - they want to succeed, while doing everything to avoid risks and failures.
Marriage as a risk factor
The risk of developing chronic depression is higher for women than for men. Negative influences include traumatic experiences of physical or sexual abuse, interpersonal problems, or unstable family relationships.