Preventing bipolar disorder
Preventing Symptoms of Bipolar Disorder Depression & Mania
Written by WebMD Editorial Contributors
In this Article
- What are bipolar disorder symptoms?
- What are symptoms of bipolar depression?
- What are symptoms of bipolar mania?
- How is bipolar disorder treated?
- Can behavioral counseling help those with bipolar disorder?
- Can bipolar disorder be cured?
Bipolar disorder, sometimes called manic depression, is a mental health disorder that is distinguished by dramatic changes in a person's mood and energy, from the elated highs of mania to the lows of depression. Bipolar disorder affects all ages, genders, and ethnicities, and usually has its onset in late adolescence or young adulthood. We know that genetics can play a role in a person's vulnerability to bipolar disorder, as researchers have traced the incidence of bipolar disorder among generations of families.
While bipolar disorder cannot be prevented, it's important to be aware of early warning signs of an impending episode of bipolar depression or bipolar mania. Early recognition of bipolar warning signs and seeing your doctor regularly can allow you to monitor your mood and medications and keep illness from escalating.
In fact, although treating bipolar disorder moods is critical, there is a convincing case supported by scientific studies that the prevention of further mood episodes should be the greatest goal.
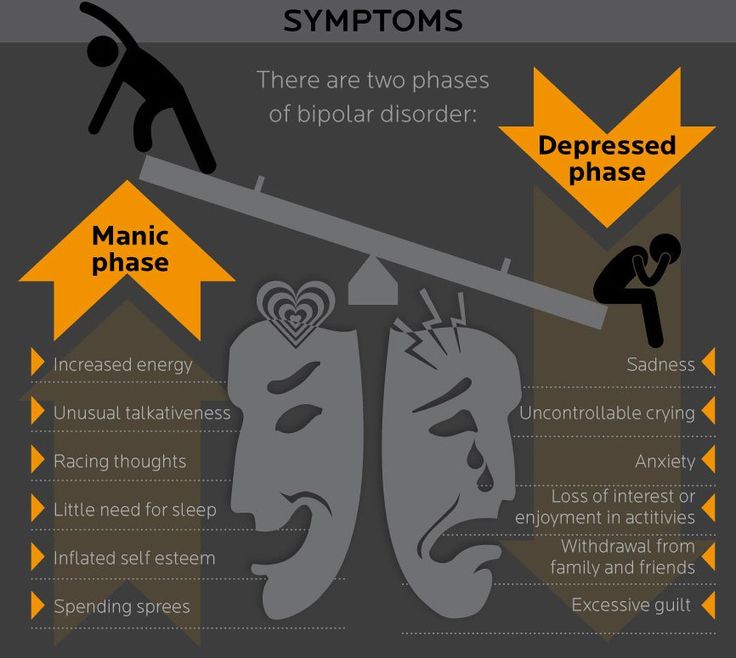
What are bipolar disorder symptoms?
Symptoms of bipolar disorder can fall between two extreme mood states:
- Bipolar depression, which includes feelings of being sad, hopeless, helpless, and worthless
- Bipolar mania, which includes feelings of elation and exuberance coupled with increased energy and activity and little need for sleep
In addition, people with bipolar disorder can have manic episodes that occur simultaneously with depressive symptoms, or vice versa. When a manic or depressive episode simultaneously includes symptoms of the opposite pole, that episode is said to have "mixed features. "
"
What are symptoms of bipolar depression?
Symptoms of the depressive phase of bipolar disorder may consist of the following:
- Depressed mood and low self-esteem
- Excessive crying spells
- Low energy levels and an apathetic view of life
- Sadness, loneliness, helplessness, feelings of guilt
- Slow speech, fatigue, and poor coordination and concentration
- Insomnia or oversleeping
- Thoughts of suicide or dying
- Changes in appetite (overeating/not eating)
- Unexplainable body aches and pains
- Lack of interest or pleasure in usual activities
What are symptoms of bipolar mania?
- Euphoria or irritability
- Excessive talking; racing thoughts
- Inflated self-esteem
- Grandiose thoughts
- Unusual energy; less need for sleep
- Impulsiveness, a reckless pursuit of gratification -- shopping sprees, impetuous travel, more and sometimes promiscuous sex, high-risk business investments, fast driving
- Hallucinations and or delusions (psychotic features such as these may be involved in about one out of every two of cases of bipolar mania)
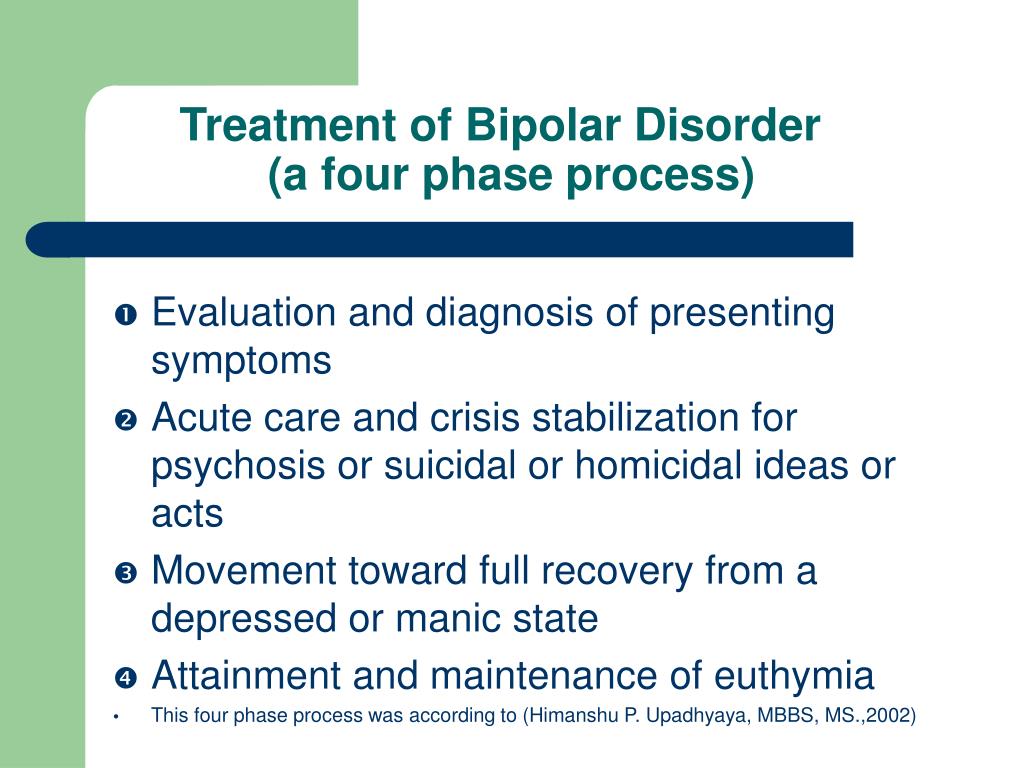
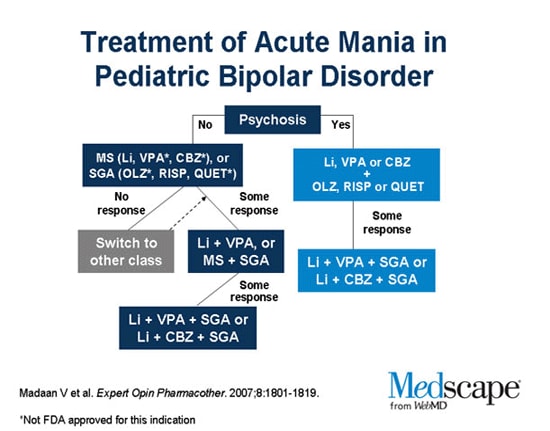
How is bipolar disorder treated?
Bipolar disorder is treated with medications to stabilize mood.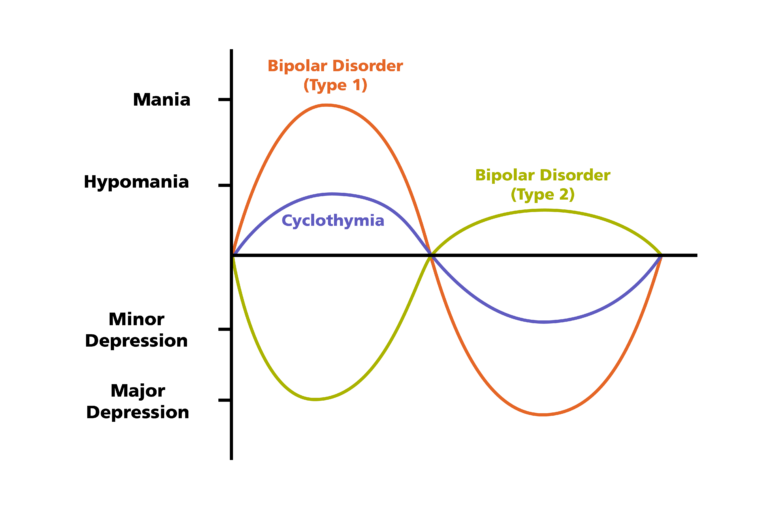 If the mood stabilizers do not fully manage the symptoms, other medications may be added to help calm the mania or ease the depression.
If the mood stabilizers do not fully manage the symptoms, other medications may be added to help calm the mania or ease the depression.
Along with mood stabilizers, psychotherapy is recommended to help the person develop appropriate and workable coping strategies to deal with everyday stressors and to increase medication compliance.
Can behavioral counseling help those with bipolar disorder?
Different types of talk therapy options are available to help those with bipolar disorder prevent or cope with a mood episode:
- Individual counseling: This is a one-on-one session with a professional therapist with experience in bipolar disorders in which the patient's problem areas are addressed. The session may include help accepting the diagnosis, education about bipolar moods, ways to identify warning signs, and intervention strategies to manage stress.
- Family counseling: Bipolar disorder extends beyond the patient and can affect the entire family.
 Families are frequently involved in outpatient therapy as they receive education about bipolar disorder and work with the therapist and patient to learn how to recognize early warnings of an impending manic or depressive episode.
Families are frequently involved in outpatient therapy as they receive education about bipolar disorder and work with the therapist and patient to learn how to recognize early warnings of an impending manic or depressive episode. - Group counseling: Group sessions allow for the sharing of feelings and the development of effective coping strategies. The give-and-take at group sessions can be the most productive way to change the way you think about bipolar disorder and improve coping skills as you face life's challenges.
Can bipolar disorder be cured?
There is no cure for bipolar disorder, but through behavior therapy and the right combination of mood stabilizers and other bipolar medicines, most people with bipolar disorder can live normal, productive lives and control the illness. That said, bipolar disorder is a lifelong mental illness that has a great risk of recurrent episodes. Taking prescribed medications and keeping doctor appointments are crucial to self-managing bipolar disorder and preventing serious episodes.
In addition, there are support groups available for patients and their family members to help them talk openly and learn how to support someone with bipolar disorder. One good organization is the National Association on Mental Illness(NAMI). Ongoing encouragement and support are needed after a person starts treatment. In fact, there are findings showing that the availability of social support systems increases the chances of employment in patients with bipolar disorder compared with those patients without support.
Bipolar Disorder Guide
- Overview
- Symptoms & Types
- Treatment & Prevention
- Living & Support
Bipolar disorder - Symptoms and causes
Overview
Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression).
When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When your mood shifts to mania or hypomania (less extreme than mania), you may feel euphoric, full of energy or unusually irritable. These mood swings can affect sleep, energy, activity, judgment, behavior and the ability to think clearly.
Episodes of mood swings may occur rarely or multiple times a year. While most people will experience some emotional symptoms between episodes, some may not experience any.
Although bipolar disorder is a lifelong condition, you can manage your mood swings and other symptoms by following a treatment plan. In most cases, bipolar disorder is treated with medications and psychological counseling (psychotherapy).
Bipolar disorder care at Mayo Clinic
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
There are several types of bipolar and related disorders. They may include mania or hypomania and depression. Symptoms can cause unpredictable changes in mood and behavior, resulting in significant distress and difficulty in life.
They may include mania or hypomania and depression. Symptoms can cause unpredictable changes in mood and behavior, resulting in significant distress and difficulty in life.
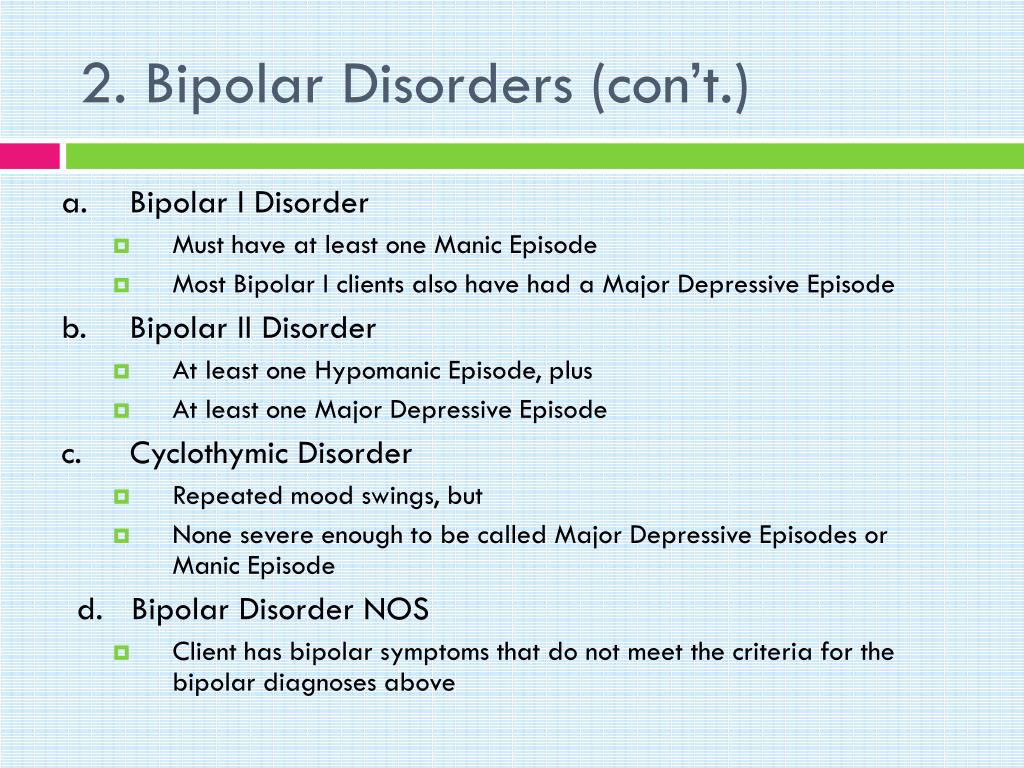
- Bipolar I disorder. You've had at least one manic episode that may be preceded or followed by hypomanic or major depressive episodes. In some cases, mania may trigger a break from reality (psychosis).
- Bipolar II disorder. You've had at least one major depressive episode and at least one hypomanic episode, but you've never had a manic episode.
- Cyclothymic disorder. You've had at least two years — or one year in children and teenagers — of many periods of hypomania symptoms and periods of depressive symptoms (though less severe than major depression).
- Other types. These include, for example, bipolar and related disorders induced by certain drugs or alcohol or due to a medical condition, such as Cushing's disease, multiple sclerosis or stroke.
Bipolar II disorder is not a milder form of bipolar I disorder, but a separate diagnosis. While the manic episodes of bipolar I disorder can be severe and dangerous, individuals with bipolar II disorder can be depressed for longer periods, which can cause significant impairment.
Although bipolar disorder can occur at any age, typically it's diagnosed in the teenage years or early 20s. Symptoms can vary from person to person, and symptoms may vary over time.
Mania and hypomania
Mania and hypomania are two distinct types of episodes, but they have the same symptoms. Mania is more severe than hypomania and causes more noticeable problems at work, school and social activities, as well as relationship difficulties. Mania may also trigger a break from reality (psychosis) and require hospitalization.
Both a manic and a hypomanic episode include three or more of these symptoms:
- Abnormally upbeat, jumpy or wired
- Increased activity, energy or agitation
- Exaggerated sense of well-being and self-confidence (euphoria)
- Decreased need for sleep
- Unusual talkativeness
- Racing thoughts
- Distractibility
- Poor decision-making — for example, going on buying sprees, taking sexual risks or making foolish investments
Major depressive episode
A major depressive episode includes symptoms that are severe enough to cause noticeable difficulty in day-to-day activities, such as work, school, social activities or relationships. An episode includes five or more of these symptoms:
An episode includes five or more of these symptoms:
- Depressed mood, such as feeling sad, empty, hopeless or tearful (in children and teens, depressed mood can appear as irritability)
- Marked loss of interest or feeling no pleasure in all — or almost all — activities
- Significant weight loss when not dieting, weight gain, or decrease or increase in appetite (in children, failure to gain weight as expected can be a sign of depression)
- Either insomnia or sleeping too much
- Either restlessness or slowed behavior
- Fatigue or loss of energy
- Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking about, planning or attempting suicide
Other features of bipolar disorder
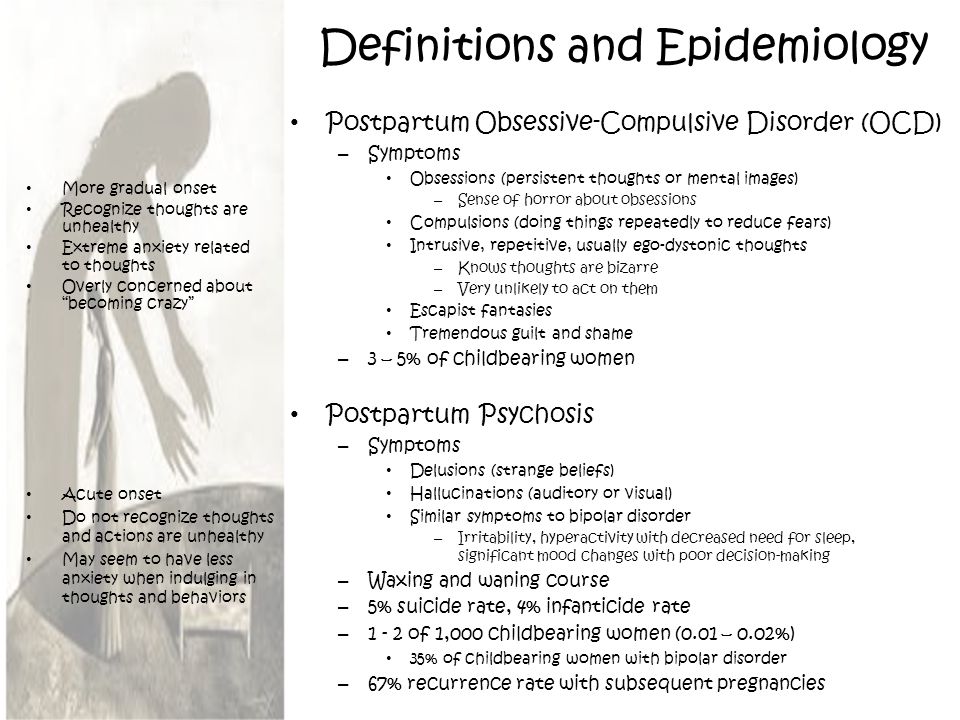
Signs and symptoms of bipolar I and bipolar II disorders may include other features, such as anxious distress, melancholy, psychosis or others.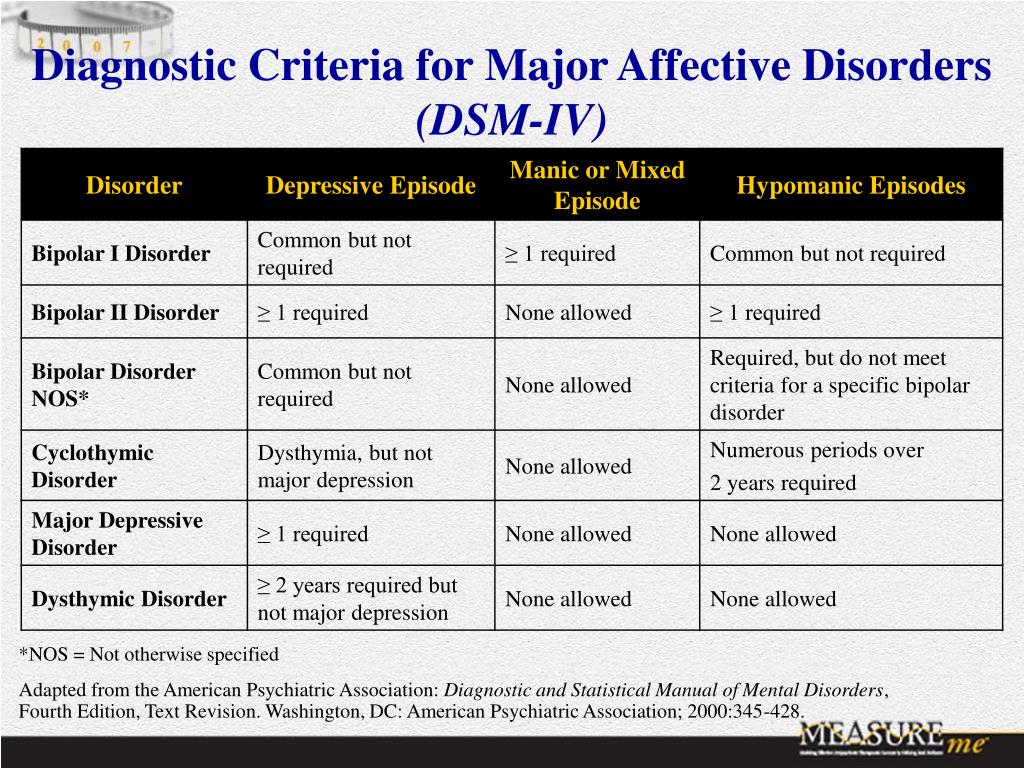 The timing of symptoms may include diagnostic labels such as mixed or rapid cycling. In addition, bipolar symptoms may occur during pregnancy or change with the seasons.
The timing of symptoms may include diagnostic labels such as mixed or rapid cycling. In addition, bipolar symptoms may occur during pregnancy or change with the seasons.
Symptoms in children and teens
Symptoms of bipolar disorder can be difficult to identify in children and teens. It's often hard to tell whether these are normal ups and downs, the results of stress or trauma, or signs of a mental health problem other than bipolar disorder.
Children and teens may have distinct major depressive or manic or hypomanic episodes, but the pattern can vary from that of adults with bipolar disorder. And moods can rapidly shift during episodes. Some children may have periods without mood symptoms between episodes.
The most prominent signs of bipolar disorder in children and teenagers may include severe mood swings that are different from their usual mood swings.
When to see a doctor
Despite the mood extremes, people with bipolar disorder often don't recognize how much their emotional instability disrupts their lives and the lives of their loved ones and don't get the treatment they need.
And if you're like some people with bipolar disorder, you may enjoy the feelings of euphoria and cycles of being more productive. However, this euphoria is always followed by an emotional crash that can leave you depressed, worn out — and perhaps in financial, legal or relationship trouble.
If you have any symptoms of depression or mania, see your doctor or mental health professional. Bipolar disorder doesn't get better on its own. Getting treatment from a mental health professional with experience in bipolar disorder can help you get your symptoms under control.
When to get emergency help
Suicidal thoughts and behavior are common among people with bipolar disorder. If you have thoughts of hurting yourself, call 911 or your local emergency number immediately, go to an emergency room, or confide in a trusted relative or friend. Or contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline, available 24 hours a day, seven days a week. Or use the Lifeline Chat. Services are free and confidential.
Or use the Lifeline Chat. Services are free and confidential.
If you have a loved one who is in danger of suicide or has made a suicide attempt, make sure someone stays with that person. Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information.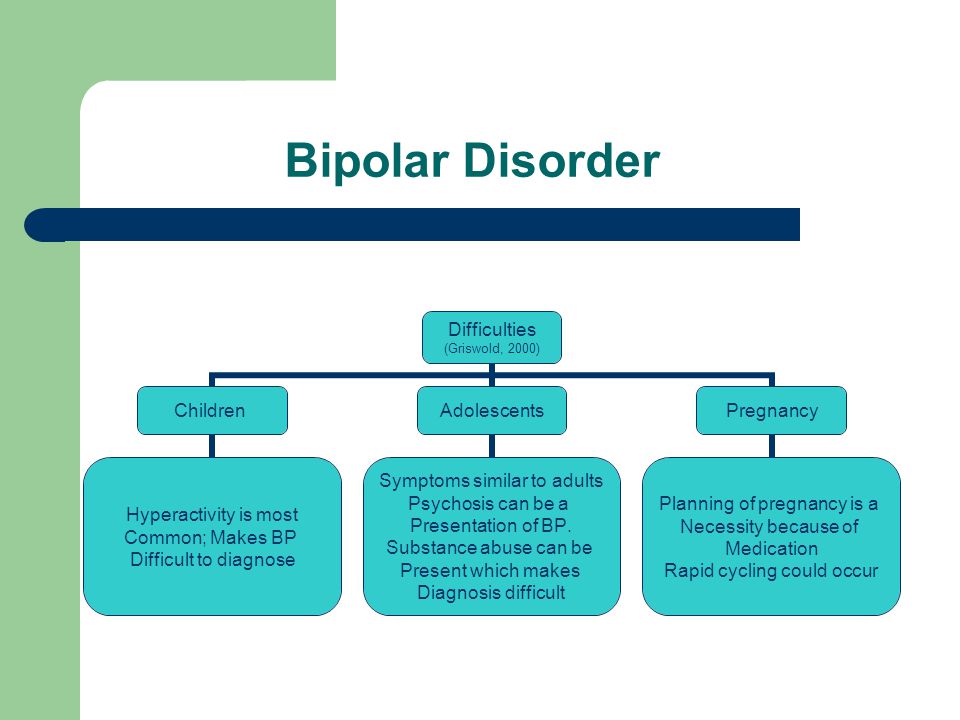 If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
The exact cause of bipolar disorder is unknown, but several factors may be involved, such as:
- Biological differences. People with bipolar disorder appear to have physical changes in their brains. The significance of these changes is still uncertain but may eventually help pinpoint causes.
- Genetics. Bipolar disorder is more common in people who have a first-degree relative, such as a sibling or parent, with the condition.
 Researchers are trying to find genes that may be involved in causing bipolar disorder.
Researchers are trying to find genes that may be involved in causing bipolar disorder.
Risk factors
Factors that may increase the risk of developing bipolar disorder or act as a trigger for the first episode include:
- Having a first-degree relative, such as a parent or sibling, with bipolar disorder
- Periods of high stress, such as the death of a loved one or other traumatic event
- Drug or alcohol abuse
Complications
Left untreated, bipolar disorder can result in serious problems that affect every area of your life, such as:
- Problems related to drug and alcohol use
- Suicide or suicide attempts
- Legal or financial problems
- Damaged relationships
- Poor work or school performance
Co-occurring conditions
If you have bipolar disorder, you may also have another health condition that needs to be treated along with bipolar disorder. Some conditions can worsen bipolar disorder symptoms or make treatment less successful.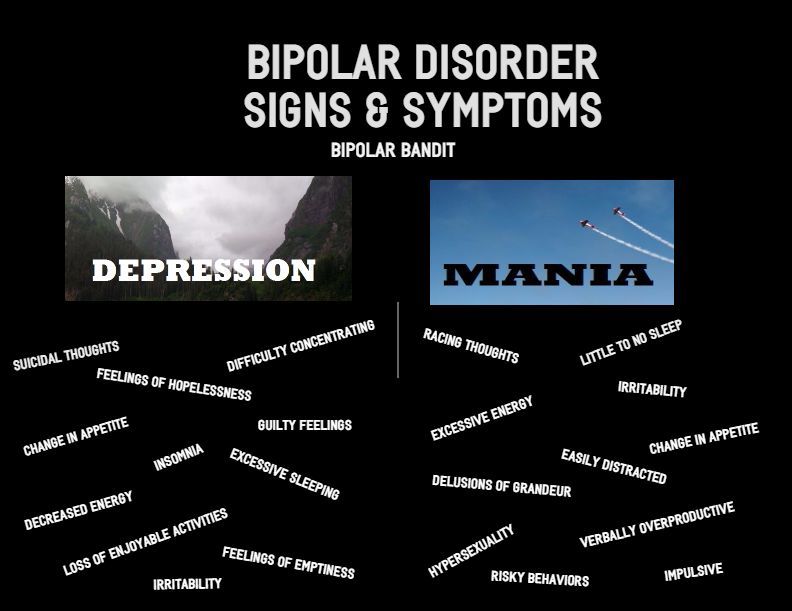 Examples include:
Examples include:
- Anxiety disorders
- Eating disorders
- Attention-deficit/hyperactivity disorder (ADHD)
- Alcohol or drug problems
- Physical health problems, such as heart disease, thyroid problems, headaches or obesity
More Information
- Bipolar disorder care at Mayo Clinic
- Bipolar disorder and alcoholism: Are they related?
Prevention
There's no sure way to prevent bipolar disorder. However, getting treatment at the earliest sign of a mental health disorder can help prevent bipolar disorder or other mental health conditions from worsening.
If you've been diagnosed with bipolar disorder, some strategies can help prevent minor symptoms from becoming full-blown episodes of mania or depression:
- Pay attention to warning signs. Addressing symptoms early on can prevent episodes from getting worse. You may have identified a pattern to your bipolar episodes and what triggers them.
 Call your doctor if you feel you're falling into an episode of depression or mania. Involve family members or friends in watching for warning signs.
Call your doctor if you feel you're falling into an episode of depression or mania. Involve family members or friends in watching for warning signs. - Avoid drugs and alcohol. Using alcohol or recreational drugs can worsen your symptoms and make them more likely to come back.
- Take your medications exactly as directed. You may be tempted to stop treatment — but don't. Stopping your medication or reducing your dose on your own may cause withdrawal effects or your symptoms may worsen or return.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
All About Bipolar Affective Disorder
What is Bipolar Affective Disorder?
Bipolar affective personality disorder, or manic-depressive psychosis, is a complex, mental illness characterized by constant mood swings. This is not an ordinary mood change that happens to every person, but a systematic psycho-emotional drop with a short-term normal state. It is the episodes from depression to an extremely agitated state that are called affective. In Russia, 1% of the population is affected by this disease. As a rule, it is observed among young women aged 20 to 30 years. However, men are also prone to bipolar disorder, and they begin it earlier than women. And if in women it begins with a depressive phase, then in men it starts with a manic phase. The appearance of symptoms of bipolar disorder in women is often associated with hormonal disorders and the characteristics of the menstrual cycle.
It is the episodes from depression to an extremely agitated state that are called affective. In Russia, 1% of the population is affected by this disease. As a rule, it is observed among young women aged 20 to 30 years. However, men are also prone to bipolar disorder, and they begin it earlier than women. And if in women it begins with a depressive phase, then in men it starts with a manic phase. The appearance of symptoms of bipolar disorder in women is often associated with hormonal disorders and the characteristics of the menstrual cycle.
Bipolar affective disorder can destroy personal relationships, impair the quality of work, reduce academic performance, and in some cases even lead to suicide. Therefore, it is so important to diagnose it in time and prescribe appropriate treatment.
Causes of bipolar affective disorder
To date, doctors cannot answer the question about the exact causes of this disease. It is known for certain that it can be genetically transmitted, but sometimes it is in "sleep mode" until it is triggered by some stressful event.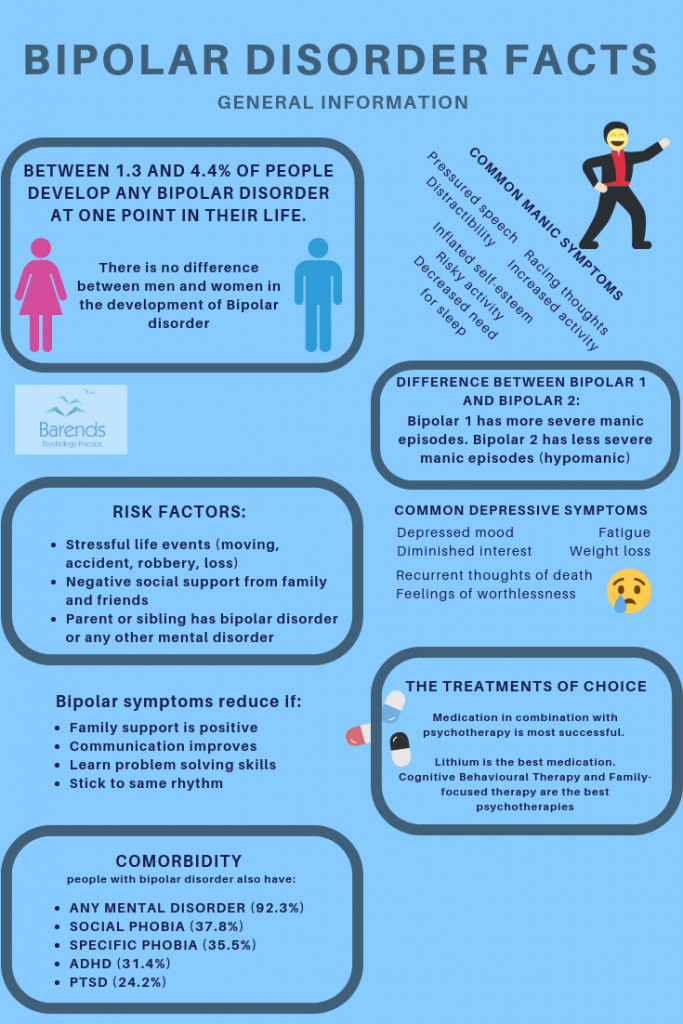 Also, pushing factors for the development of BAD can be:
Also, pushing factors for the development of BAD can be:
- chronic fatigue;
- overwork;
- emotional burnout;
- dissatisfaction with personal life;
- death of a loved one;
- financial problems;
- dissatisfaction with life;
- sensitivity and susceptibility to things;
- melancholic character;
- head injury;
- use of drugs and alcohol.
Disease pathogenesis
The pathogenesis of bipolar affective disorder, that is, the onset and development of the disease, is currently not fully understood. At 95%, we can only say that it is transmitted genetically and is associated with neurochemistry. According to studies, in 80% of cases the nature of the disease is associated with the environment of the patient and only 20% is transmitted genetically. The causes of manic phases are increased tone of the central nervous system, as well as hyperfunction of the thyroid gland and pituitary gland.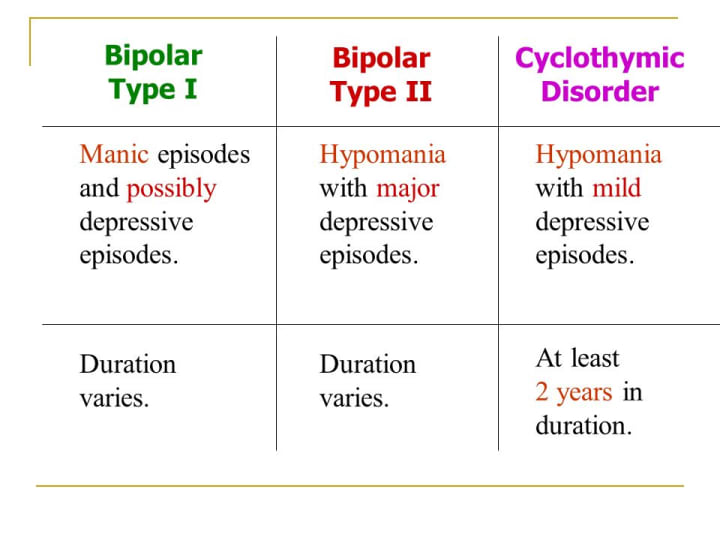
Symptoms or how the disease manifests itself
As a rule, signs of bipolar affective disorder are observed in patients in the autumn-winter and winter-spring periods. And the point is not only in climatic features, but also in weakened immunity at the indicated times of the year.
BAD is divided into 2 phases: depressive and manic, and can manifest itself equally in both phases. The frequency of the phases and their change is very individual for each individual patient and lasts from 2 weeks to 2 years. However, even the duration of the disease cannot lead to any mental defects, such as schizophrenia, on the contrary, rather, patients with schizophrenia develop a “bipolar disorder”.
Bipolar affective disorder is characterized precisely by the sequence of the above phases. A patient with mania can be recognized by the following features:
- increased hyperactivity;
- excitability for more than a week;
- fast speech;
- great flow of speech and confusion of thought;
- rapid change in mood;
- increased self-esteem.

The latter entails performing overwhelming tasks that patients cannot afford. Also, the patient is accompanied by irritability, mild euphoria, excessive frankness in conversations and behavior. A person sleeps little, and 2 hours of sleep is enough for him to feel good. In rare cases, the phase is accompanied by delusions of grandeur or persecution, sound and / or auditory hallucinations. At the same time, the symptoms of the depressive phase are slightly different. This:
- laziness and apathy;
- depressed mood;
- constant desire to sleep;
- physical ailment;
- anxiety;
- heaviness in legs and head;
- unwillingness to do something.
At the slightest detection of symptoms and signs of bipolar affective disorder in a patient, an early diagnosis and surgical treatment of the disease is required. This applies to any course of the disease, even if the depressed mood or the sudden change of mood in a person lasts only a few days.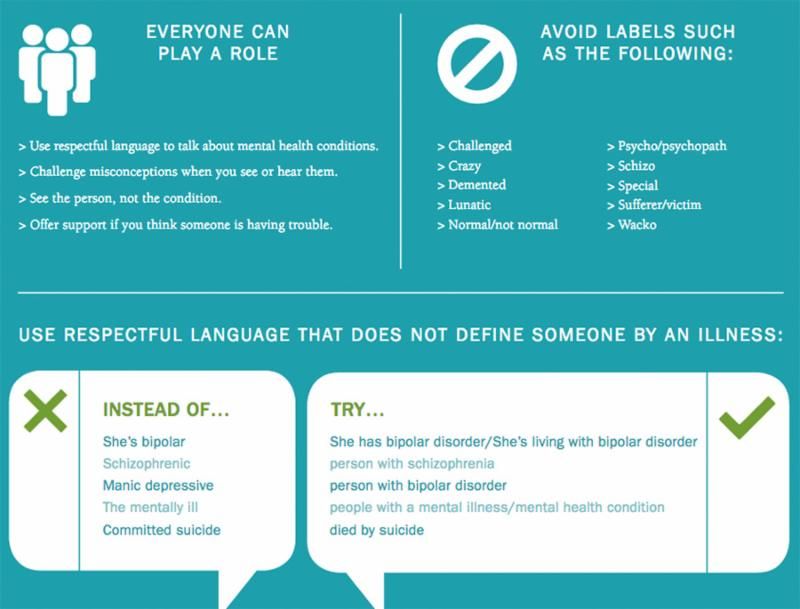 Any timely help will be salvation and help for the patient and will help to survive the course of the disease more easily. Painful perception of criticism, shallow depression, anxiety, unreasonable anxiety - all this, too, should alert and serve as an impetus for taking decisive action. As mentioned above, both men and women are prone to bipolar disorder, although they are more common in the latter. This is due not only to menstrual irregularities and hormonal disorders, but also to a severe course during childbirth, the so-called postpartum depression. As a rule, women are more susceptible to the unipolar course of bipolar disorder, when the course of the disease is accompanied by only one of the phases: manic or depressive. The latter is usually more common.
Any timely help will be salvation and help for the patient and will help to survive the course of the disease more easily. Painful perception of criticism, shallow depression, anxiety, unreasonable anxiety - all this, too, should alert and serve as an impetus for taking decisive action. As mentioned above, both men and women are prone to bipolar disorder, although they are more common in the latter. This is due not only to menstrual irregularities and hormonal disorders, but also to a severe course during childbirth, the so-called postpartum depression. As a rule, women are more susceptible to the unipolar course of bipolar disorder, when the course of the disease is accompanied by only one of the phases: manic or depressive. The latter is usually more common.
Bipolar affective disorder symptoms in women are accompanied by rapid cycles and mixed episodes. The prerequisites for them are eating disorders, alcohol or drug addiction, abuse of antidepressants. In addition, women are more prone to migraines, thyroid disorders, diabetes and obesity.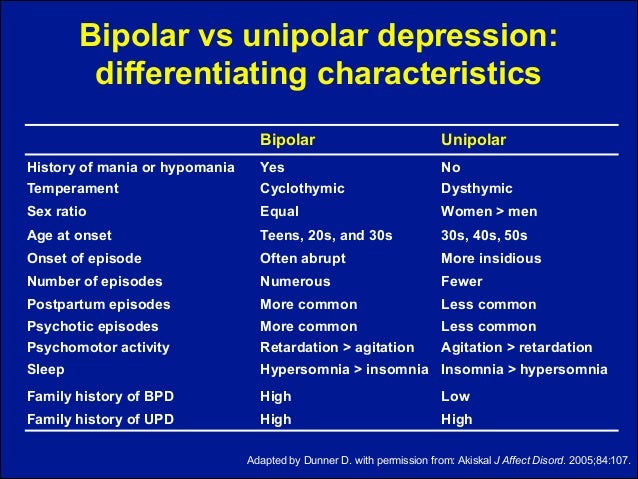 It is these external stimuli that become the prerequisites for the development of BAD. Childbirth also becomes one of the factors in the development of the depressive phase, if a woman has already been diagnosed with this disease before them. In this case, the risks of developing the disease increase several times. Women are also more likely to have suicidal thoughts.
It is these external stimuli that become the prerequisites for the development of BAD. Childbirth also becomes one of the factors in the development of the depressive phase, if a woman has already been diagnosed with this disease before them. In this case, the risks of developing the disease increase several times. Women are also more likely to have suicidal thoughts.
But in men, the symptoms of bipolar affective disorder largely depend on external factors, and the course of the disease is a little milder. The periods between phases are long and get worse over time. With inadequate and untimely treatment, the disease progresses and it becomes more difficult to get rid of it. Mostly in men, a mixed type of disorder is observed, which is accompanied by a short-term remission. In men, more often than women, the ability to do something is lost, concentration of attention decreases, and insomnia appears. And if in women one phase of BAD can last longer than another, then in men the duration is almost the same.
In addition to external factors that influence the development of bipolar disorder in men, such as unsettled life, problems in personal life and at work, financial difficulties, a common cause of the development of the disease is long-term alcohol consumption.
Classification of affective disorder
This disease is classified into different types and phases. So, according to the international classification of diseases (ICD-11), types of bipolar affective disorder are divided into 1 and 2. The classic course, as mentioned earlier, is manic and depressive, and one phase can either last a long time or change abruptly to another. Another phase is due to a sharp transition - from manic to depressive without any interruptions. Frequent, long phases with rapid cyclicity - 4 or more phases significantly affect the patient's condition, his quality of life and are a poor prognosis for the course of the disease.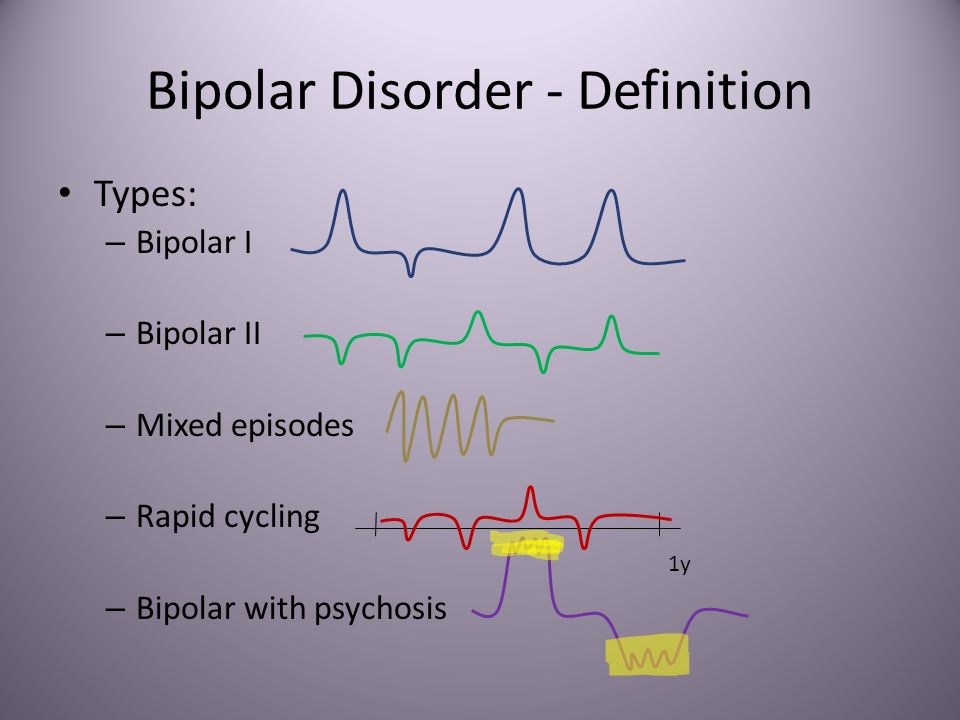
Bipolar affective disorder type 1 is accompanied by an aggravation of mania and pronounced depression, which leads to a violation of normal functioning. As a result - frequent hits in hospitals or police stations. Patients have a pronounced apathy, a complaint about themselves, the inability to do any business. The patient, as a rule, begins to blame himself, to consider himself incapable of anything.
And if BAD type 1 is characterized by a phase change, then bipolar affective disorder type 2 is due to the presence of only a depressive episode without mania. The course of the disease is similar to unipolar depression, however, these are two completely different diseases. If in patients in the first case, with prolonged use of antidepressants, everything returns to normal, then in patients with BAD type 2, they are not only contraindicated, sometimes, but can also cause hypomania, which has an extremely negative effect on the course of the disease. The phases last longer, replace each other faster, a mixed state occurs, which a person can hardly endure.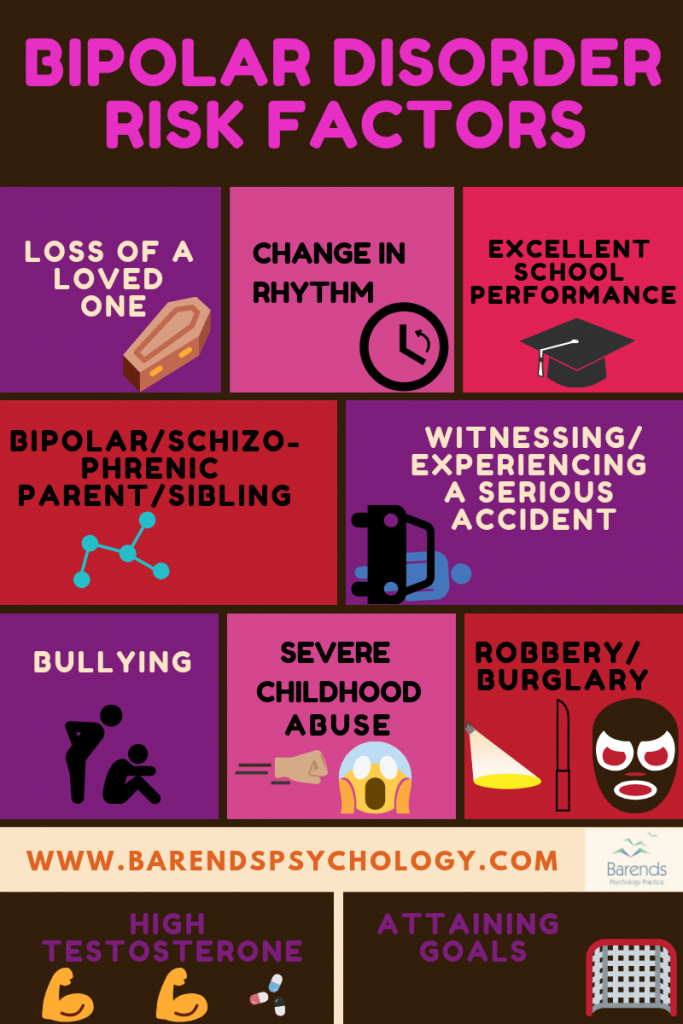
By phases, bipolar disorder is divided into the following types: manic, depressive, and also, a mixed episode of bipolar affective disorder is distinguished. The latter can be manifested by sudden outbursts of fun in a state of melancholic mood.
Other indicators are:
As a rule, the symptoms of this episode last about 1 week or quickly change. Sometimes a patient with a disorder is accompanied by insomnia, suicidal thoughts, lack of appetite. Pronounced symptoms are the reason for the patient's social and professional maladaptation and a significant deterioration in the quality of life.
If we talk about the depressive phase of bipolar affective disorder, then it is caused by several factors and is accompanied by the following symptoms:
- Endogenous depression (permanent depressed mood) accompanied by vitality - feeling alive, able to move, energetic.

- In the stage of the depressive triad, when a person does not feel like a full-fledged member of society and melancholy is fully manifested, slowness in speech and movement is observed.
- Pronounced change of mood. From the morning bad mood with a feeling of melancholy and anxiety, nothing remains by the evening.
- Disorder of appetite. Not a single meal seems tasty to the patient, he begins to lose weight, and in women there may be a violation of the monthly cycle up to complete disappearance.
- May present with psychomotor retardation.
- Constant feeling of melancholy.
- Complete decrease in sexual desire and loss of maternal instinct.
- Periodic occurrence of suicidal thoughts.
- Occasionally, some patients experience tachycardia, constipation and mydriasis - dilated pupils.
- Rarely, delusions, hallucinations may occur.
It is important to understand that patients are at high risk of suicide during this phase. According to statistics, this phenomenon occurs in 40% of cases. Therefore, it is so important to diagnose it in time for subsequent timely treatment.
According to statistics, this phenomenon occurs in 40% of cases. Therefore, it is so important to diagnose it in time for subsequent timely treatment.
The manic phase of bipolar affective disorder varies in severity from elevated mood to severe mania. In the first state there is no self-criticism, a person is adaptive to the environment. This phase is characterized by the following symptoms:
- Manic triad: increased mood, accelerated thinking, movements.
- Activity, energy, burst of energy. The patient takes on many things, but does not complete any one.
- Lack of concentration.
This phase has 5 stages:
- Hypomanic, which is characterized by increased mood and cheerfulness. Patients experience an increase in appetite and sleep duration.
- Expressive, which is accompanied by constant jokes and chatter against the background of short-term outbursts of anger.
- A violent state in which a prolonged excited state is accompanied by disorder and incoherent speech.
- Motor calmness.
- Reactive with the return of all symptoms of mania to normal. Sometimes in this scenario, patients may experience amnesia and some episodes of mania are simply forgotten.
If the main symptom of the manic phase of bipolar affective disorder is increased excitability, then in the depressive phase, on the contrary, the mood is constantly sluggish. Patients with a manic stage of development cannot soberly assess their behavior or completely deny it. In parallel with euphoria, irritability and anxiety develop. A person is uncomfortable in this state.
It is possible to make a diagnosis with a prolonged course of the disease - more than 1 week with the preservation of the phase at the main time of the day. Along with irritability, 4 additional symptoms will certainly appear. Symptoms can shift in different directions, turn from hypomania - a mild state, high activity and high spirits, into a manic psychosis. Patients with psychosis are visibly active, behaving erratically, sometimes screaming, sometimes singing.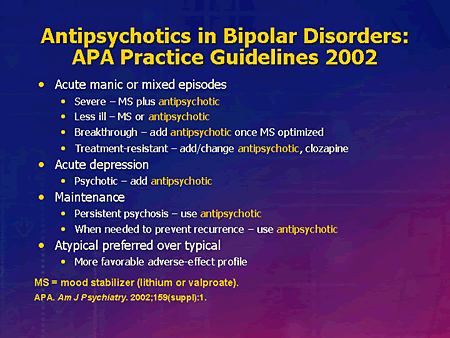 Excitation reaches its climax, the state is not stable, irritability increases, sometimes delusions or hallucinations develop. Manic psychosis is often confused with schizophrenia.
Excitation reaches its climax, the state is not stable, irritability increases, sometimes delusions or hallucinations develop. Manic psychosis is often confused with schizophrenia.
Mixed bipolar affective disorder is a mixture of two phases that literally drives the patient crazy. On the one hand, he has a pronounced stream of brilliant thoughts, on the other, suicidal thoughts and feelings of guilt. This is a very dangerous phase, which is a prerequisite for suicide. The feeling of anxiety grows even more than in the other two phases, especially if it is caused by alcohol.
A patient with bipolar disorder cannot perceive criticism and does not adequately assess his condition. Any episodes can cause rash actions, unreasonable risks that pose a threat to both him and other people.
No matter what type a person has and no matter how the course of bipolar affective disorder passes, timely diagnostics will help stop the course of the disease and prevent future complications. It is important to understand that a person's life is divided into several bands with the development of this disease: months of impenetrable darkness and the same amount of time of euphoria. The person himself does not understand that he needs help, and he does not consider himself sick.
It is important to understand that a person's life is divided into several bands with the development of this disease: months of impenetrable darkness and the same amount of time of euphoria. The person himself does not understand that he needs help, and he does not consider himself sick.
If a person develops bipolar disorder against the background of other concomitant mental illnesses, such as:
- obsessive state;
- alcohol or drug addiction;
- eating disorders;
- Attention deficit coupled with hyperactivity;
- social phobia;
- panic attacks and other diseases, the course of the disease can worsen significantly.
Complications of bipolar affective disorder
Complications of bipolar affective disorder are characterized by the development of non-medical diseases, namely asocial adaptation. Thought processes also change, mental ability and attention decrease, memory deteriorates. In some patients, the worldview changes completely.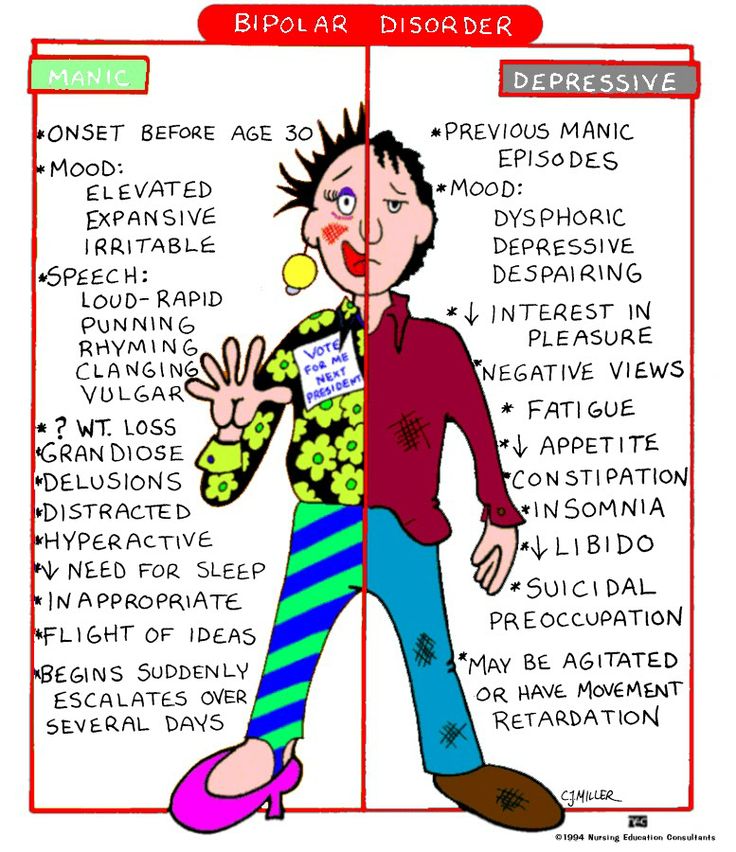 According to the conducted research, it was revealed that the creative potential directly depends on the course of BAD. People could not make contact with others. This applies, by the way, to both adults and children.
According to the conducted research, it was revealed that the creative potential directly depends on the course of BAD. People could not make contact with others. This applies, by the way, to both adults and children.
Patients with a depressive phase and suicidal thoughts are prone to it, which can also serve as a sad outcome for a person. A constant change of mood, a complete change in thoughts and consciousness, the inability to lead a full life, live in a family and raise children, the inability to adequately assess one's condition and others - these and many other possible consequences of bipolar affective disorder that need to be nipped in the bud and prevent the disease from developing .
When to see a doctor?
You need to consult a doctor already if one or two of the above symptoms occur, regardless of the phase, for 1 or more weeks.
When you understand that a person close to you is constantly in a depressed state and immediately becomes cheerful, when a person gets bored with life, his hands drop, or he is energetic, excited, grabs at everything, but does not complete everything to the end, then it is worth sounding the alarm. Only a doctor will be able to diagnose whether it is a disorder, what degree it has, and how the course develops.
Diagnostics
Diagnosis of bipolar affective disorder is based, first of all, on a survey of the patient himself. After all, he does not admit to the presence of hypomania or mania until he is asked. Questions about suicide, plans for the future, can be good helpers in identifying the disease. The second key point is the delivery of hormones to check the functions of the thyroid gland. Among other things, it is necessary to obtain an anamnesis for the use of drugs and alcohol by collecting urine and blood.
It is important to periodically evaluate people with schizophrenia for manic symptoms, however, unlike people who have bipolar disorder, they cannot return to normal between phases. Panic attacks, phobias, obsessive-compulsive disorders can make the diagnosis much more difficult.
Panic attacks, phobias, obsessive-compulsive disorders can make the diagnosis much more difficult.
Treatment
Treatment of bipolar affective disorder is possible both with the help of therapy and medication.
Treatment consists of several stages:
- Relief and control of symptoms.
- Long-term treatment until remission is achieved.
- Treatment maintenance and prevention. Trying to keep remission.
The choice of medicines is a little complicated by their possible side effects, moreover, no medicine can be called universal. It is important to apply the drugs previously prescribed to the patient, which gave a positive result. If the treatment will take place for the first time, then the appointment of drugs depends on the history of the disease and symptoms. Treatment of severe forms may be accompanied by the appointment of specific antidepressants, the effectiveness of which, however, has not been proven.
Among the drugs for the treatment of bipolar affective disorder, mood stabilizers and antipsychotics of the 2nd generation are distinguished. They can be used both separately and in combination with each other. For a more effective recovery, the patient needs to independently work to improve his condition. Hospitalization is possible, but only in a manic episode with type 1 bipolar disorder. At the same time, treatment can be both voluntary and compulsory. Staying in the clinic during this period is a long stage, as full outpatient treatment is carried out.
They can be used both separately and in combination with each other. For a more effective recovery, the patient needs to independently work to improve his condition. Hospitalization is possible, but only in a manic episode with type 1 bipolar disorder. At the same time, treatment can be both voluntary and compulsory. Staying in the clinic during this period is a long stage, as full outpatient treatment is carried out.
In addition to drug treatment, therapy for bipolar affective disorder is used. This can be phototherapy during the bipolar season of any type. However, this method is concomitant. The main treatment is medication and symptomatic relief.
It is also important to correctly predict the further course of the disease, because the quality of treatment depends on this. Among all types of phases and periods, a fast-cyclic disorder can be predicted the worst, since it is often diagnosed incorrectly, which entails subsequent incorrect treatment.
+7 (495) 121-48-31
Prevention or advice in case of illness
There are no clinical guidelines for bipolar affective disorder as such.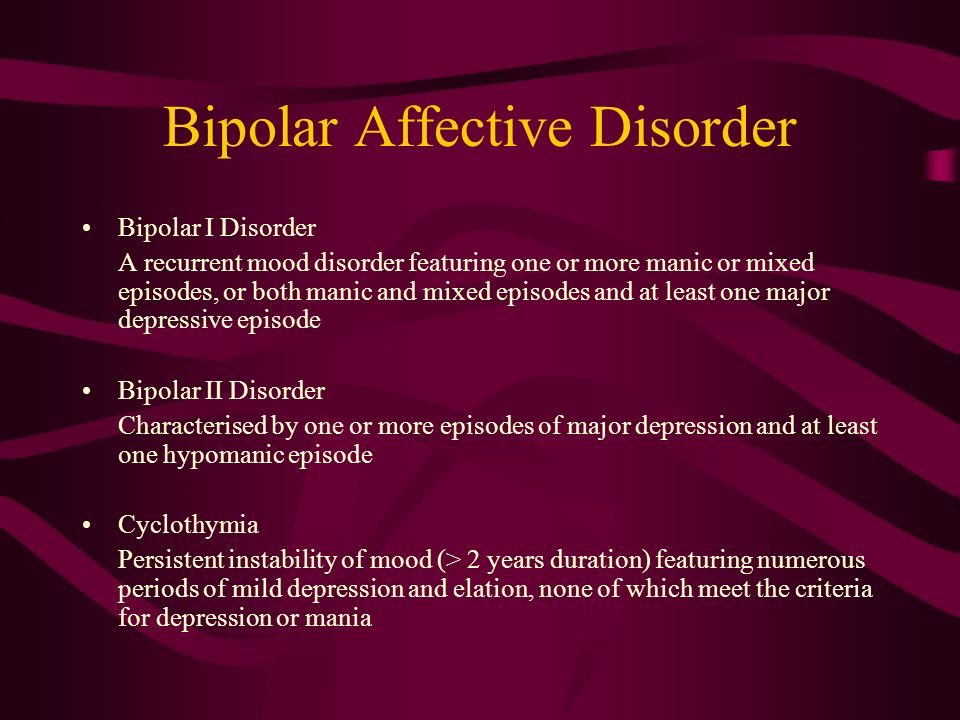 It is important not only to maintain therapy, but also to exclude factors that can cause the development of the disease and eliminate all negative factors:
It is important not only to maintain therapy, but also to exclude factors that can cause the development of the disease and eliminate all negative factors:
- exclude alcohol and any psychotropic substances;
- observe sleep and food intake;
- lead a healthy lifestyle;
- actively communicate with colleagues and friends;
- try not to be alone;
- find any hobbies outside of work.
These simple rules will help, if not cured, then delay the approach of the disease for a long time and make it easier to endure its course. If you notice any of the above symptoms in yourself or your loved ones, be sure to consult a doctor. The specialists of our clinic will help to make a timely diagnosis, highlight the phase of bipolar disorder and prescribe the right treatment that will give a positive result. Be healthy!
References:
- Zhmurov V.A. Mental disorders
- Tyuvina N. A., Stolyarova A.
 E., Smirnova V. N. Bipolar affective disorder: gender characteristics of the course and therapy
E., Smirnova V. N. Bipolar affective disorder: gender characteristics of the course and therapy - Tiganov A.S., Snezhnevsky A.V., Orlovskaya D.D., Manual of Psychiatry
- Tiganov A.S. Manual of Psychiatry - M. Medicine
- Bukhanovsky A.O., Kutyavin Yu.A., Litvak M.E. General psychopathology
- A.V. Snezhnevsky - Clinical Psychiatry
- Gert Sauer Siberian Lectures on Analytical Psychology
Bipolar affective disorder (BAD) - causes, symptoms, treatment
Bipolar affective disorder (BAD) is a severe mental illness characterized by mood and energy swings with recurring episodes of depression followed by episodes of mania or hypomania. BD is highly heritable. Early onset, chronic course and lack of optimal treatment make it one of the most disabling diseases. The lifetime prevalence of bipolar disorder across the spectrum is estimated at 2–4% of the general population and is the sixth leading cause of disability worldwide.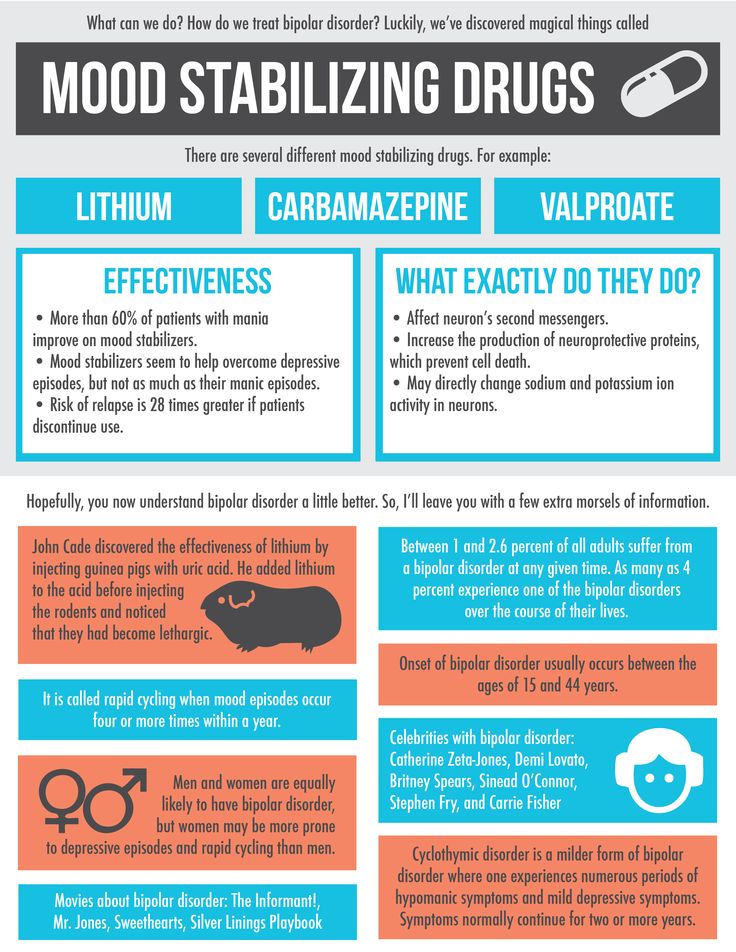
The average age at onset of bipolar affective disorder varies. According to epidemiological studies, the peak period is 20 years. It is also reported that approximately 20% of all patients show some signs of the disease in adolescence, about 50% by 30 years and 99% by 60 years.
Overall, the data indicate that bipolar disorder is more common in women, but the disease is also widespread among men. Currently, no relationship has been found between incidence and belonging to any social class. By comparison, there is a clear downward social drift among schizophrenic patients.
BAR types
The current diagnostic classification describes two main subtypes: bipolar I disorder and bipolar II disorder, which are distinguished by the absence of full-blown manic episodes in type II bipolar disorder. Type I bipolar disorder can be diagnosed on the basis of a single manic episode, but depressive episodes occur in most cases. Type II bipolar disorder is diagnosed if at least one hypomanic and one depressive episode has occurred. Hypomanic episodes are, by definition, clinically less severe than manic episodes, potentially of shorter duration, not markedly impaired in social or occupational functioning, and do not require hospitalization; the appearance of any psychotic symptoms qualifies the episode as manic.
Hypomanic episodes are, by definition, clinically less severe than manic episodes, potentially of shorter duration, not markedly impaired in social or occupational functioning, and do not require hospitalization; the appearance of any psychotic symptoms qualifies the episode as manic.
Causes of BAD
The mechanisms of the development of the disease are complex, multifaceted and not fully established. Among them, there are genetic predisposition, disturbances in the metabolism of neurotransmitters at the level of the brain, endocrine causes, environmental factors, and others.
Psychiatric genetic research has led to the understanding that bipolar affective disorder and its associated diagnoses undoubtedly have a genetic basis, however, they are not caused by a single abnormal gene, but rather have a highly polygenic structure that is not specific to a particular diagnosis. Large pedigree studies show that BAD accumulates in families. The relative risk for immediate family members of patients with bipolar affective disorder is ~7–10%. It is also known that bipolar I disorder tends to aggregate more in families than bipolar type Ⅱ disorder. BAD runs in families with related diagnoses such as major depressive disorder and schizophrenia. At the same time, schizophrenia is more often associated with BAD type Ⅰ compared to BAD type Ⅱ, and major depressive disorder is clearly not combined with a specific BAD subtype.
It is also known that bipolar I disorder tends to aggregate more in families than bipolar type Ⅱ disorder. BAD runs in families with related diagnoses such as major depressive disorder and schizophrenia. At the same time, schizophrenia is more often associated with BAD type Ⅰ compared to BAD type Ⅱ, and major depressive disorder is clearly not combined with a specific BAD subtype.
In the 1960s, the instrumental possibilities for conducting experiments with brain samples expanded. It became realistic to evaluate their response to the introduction of certain drugs. The results of such experiments, combined with clinical observations, have generated many hypotheses about a single neurotransmitter responsible for the development of a particular mental illness. The catecholamine theory of the occurrence of bipolar affective disorder is popular. Its central principle is that the two clinical poles of bipolar disorder - mania and depression - arise as a result of functional changes in the activity of catecholamines, while low activity causes a depressive state, and high activity causes a manic state.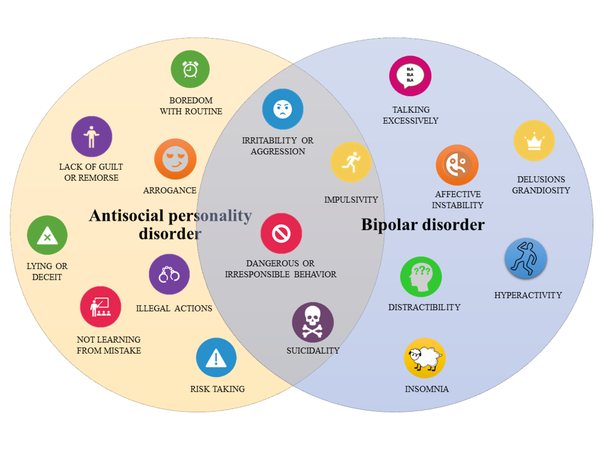 There is currently strong evidence that the clinical symptoms of BAD can be mimicked and alleviated by pharmacological modulation of the catecholamine system, but there is no direct evidence that the catecholamine system is involved in the pathogenesis of BAD. The same conclusion has been drawn from contemporary evaluations of other influential hypotheses, such as the dopamine hypothesis of schizophrenia.
There is currently strong evidence that the clinical symptoms of BAD can be mimicked and alleviated by pharmacological modulation of the catecholamine system, but there is no direct evidence that the catecholamine system is involved in the pathogenesis of BAD. The same conclusion has been drawn from contemporary evaluations of other influential hypotheses, such as the dopamine hypothesis of schizophrenia.
The influence of environmental factors is not studied as widely as the influence of genes. However, some reviews show the role of childhood adversity in the development of bipolar disorder, as well as the role of perinatal complications, maternal influenza infection during pregnancy, exposure to maternal smoking in utero, older paternal age at conception, and others.
Although stressful life events in and of themselves are not considered a cause of bipolar disorder, they can be a trigger for relapse.
Clinical picture
Bipolar affective disorder refers to mood disorders.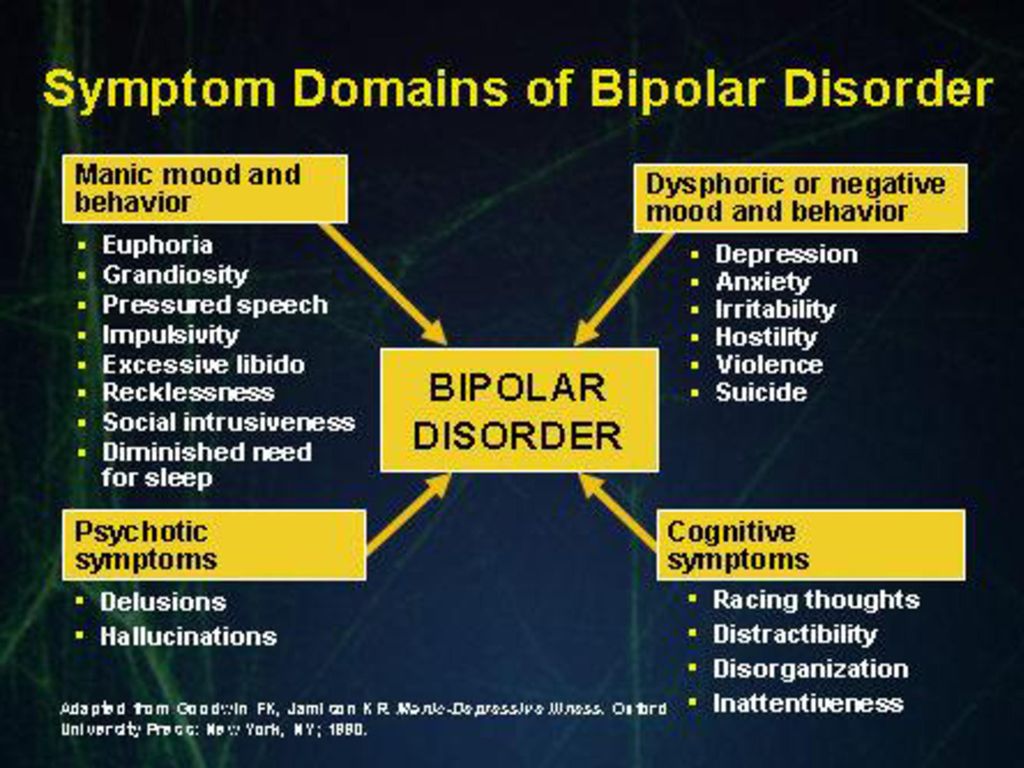 It manifests itself in different types of episodes - manic, depressive, mixed, which can be expressed in mild, moderate and severe degrees.
It manifests itself in different types of episodes - manic, depressive, mixed, which can be expressed in mild, moderate and severe degrees.
In the case of a depressive syndrome, this can range from subclinical depression to a severe condition that patients perceive as the worst thing that happened in their life. The addition of psychotic symptoms to a severe depressive episode is also likely. These may be delusional ideas of sinfulness, imminent poverty and other misfortunes, for which, according to the patient, he himself is responsible. Auditory hallucinations insult and humiliate, accuse a person, and olfactory hallucinations are most often represented by the smell of sewage. The patient perceives his life as a series of tragic mistakes. Psychomotor retardation can develop up to stupor. Severe depression at least deprives a person of the opportunity to work and maintain social relationships, and in the worst case can lead to suicide.
Patients with a mild or even moderate depressive episode certainly experience a reluctance to engage in daily activities, but they usually do not stop functioning fully.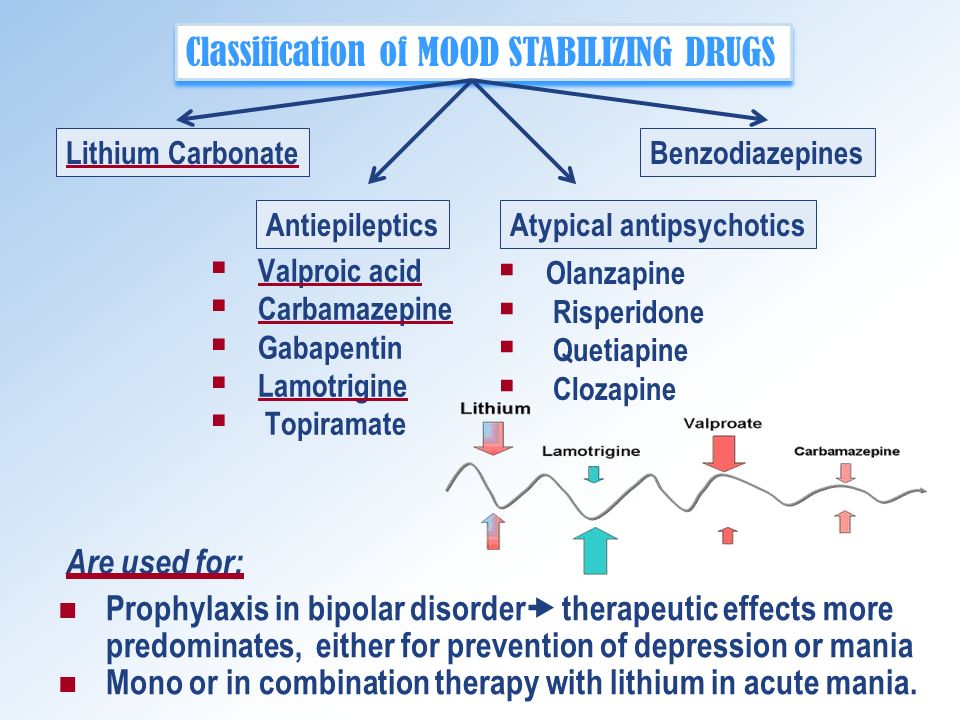 They have a significant decrease in mood, loss of interest in the surrounding reality, anhedonia - an inability to enjoy, they feel weak, fatigued. Other symptoms include a decrease in the ability to concentrate, low self-esteem, ideas of one's own insignificance, gloomy ideas about the future, sleep disturbances, and a decrease in appetite.
They have a significant decrease in mood, loss of interest in the surrounding reality, anhedonia - an inability to enjoy, they feel weak, fatigued. Other symptoms include a decrease in the ability to concentrate, low self-esteem, ideas of one's own insignificance, gloomy ideas about the future, sleep disturbances, and a decrease in appetite.
For a definite diagnosis of depression in bipolar affective disorder, the duration of an episode must be at least two weeks.
Manic syndrome can also be expressed in varying degrees: from hypomania to severe mania with psychotic symptoms.
During the period of hypomania, patients are more socially adapted than in mania. However, in both cases, an important detail is missing - criticism of one's own condition, awareness of oneself as sick.
The manic stage of bipolar disorder is subjectively more pleasant than the depressive stage. Classical mania, the so-called "jolly mania", is characterized by a typical triad of symptoms: increased mood, ideational-psychic excitement, desire for activity.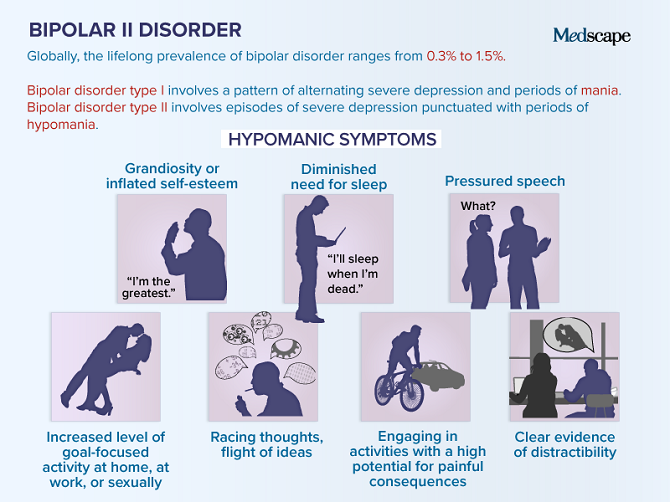 Patients are in a great mood, they love the whole world, they love themselves. They do not have the slightest doubt in their own abilities, in their own genius, and in addition they have a large supply of energy: many sacrifice sleep for the sake of activity, sleep an hour a day, while not feeling overwhelmed. A person in mania has a false sense of being productive, but new ideas come to him so quickly that old ones remain unfulfilled.
Patients are in a great mood, they love the whole world, they love themselves. They do not have the slightest doubt in their own abilities, in their own genius, and in addition they have a large supply of energy: many sacrifice sleep for the sake of activity, sleep an hour a day, while not feeling overwhelmed. A person in mania has a false sense of being productive, but new ideas come to him so quickly that old ones remain unfulfilled.
The danger lies in the many rash actions performed by a person on the rise. To give away property, to collect loans, to have questionable sexual contacts, leaving the family and children - a patient with bipolar affective disorder is capable of all this, and he will later have to regret all this.
In addition to classical mania, angry, dysphoric mania also takes place in the structure of the disease. The patient becomes irritable and aggressive beyond measure, especially towards those who do not support his ideas.
The mixed episode combines seemingly incompatible manifestations: melancholy with significant motor arousal, excellent mood simultaneously with stupor, many ideas in parallel with suicidal thoughts.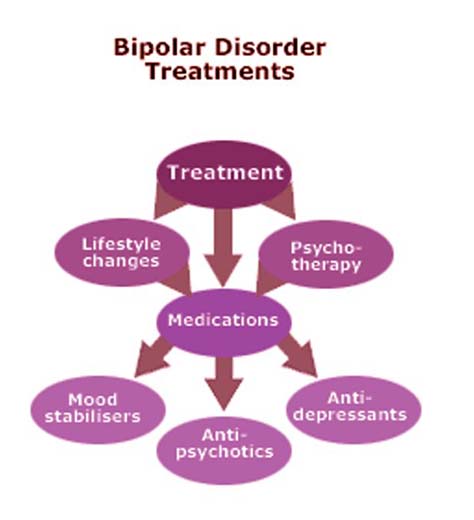 A person is extremely emotionally unstable, which may be a harbinger of an unfavorable outcome of the course of BAD.
A person is extremely emotionally unstable, which may be a harbinger of an unfavorable outcome of the course of BAD.
The German psychiatrist Emil Kraepelin noted as early as the 19th century that states of manic arousal can vary greatly in duration from weeks to months, and that more severe forms of mania with marked arousal and psychotic features tend to have relatively long episodes. He also believed that melancholic (depressive) states are usually longer than manic episodes, can sometimes persist for years, and tend to become more pronounced than mania at older ages. Modern research confirms these ancient ideas.
Diagnostics
Bipolar disorder of both types (BAD type Ⅰ and BAD type Ⅱ) is difficult to accurately diagnose in clinical practice, especially in the early stages. Only 20% of patients with bipolar disorder who have had a depressive episode are diagnosed within the first year after seeking treatment, and the average delay between onset and diagnosis is 5–10 years. The main reason for the difficulty in diagnosis is to differentiate bipolar type I or II disorder from unipolar depression, a disease characterized by recurrent depressive episodes, especially in patients who present directly during a depressive episode and in those who do not have a clear history. mania or hypomania. Unipolar depression has been reported to be a common misdiagnosis in patients with bipolar disorder, especially in bipolar II disorder, since patients with this disorder, by definition, never experience major manic episodes.
The main reason for the difficulty in diagnosis is to differentiate bipolar type I or II disorder from unipolar depression, a disease characterized by recurrent depressive episodes, especially in patients who present directly during a depressive episode and in those who do not have a clear history. mania or hypomania. Unipolar depression has been reported to be a common misdiagnosis in patients with bipolar disorder, especially in bipolar II disorder, since patients with this disorder, by definition, never experience major manic episodes.
In recent years, the diagnostic criteria for bipolar disorder have been revised to address this problem to include both mood changes and activity or energy changes. New rating scales for self-administration and clinical use have been developed to help improve the early detection of clinical signs suggestive of a diagnosis of bipolar disorder in people with a history of depressive episodes.
As with most mental illnesses, physicians are forced to focus only on a carefully collected history and observation of the clinical picture, due to the lack of laboratory or instrumental studies that could help establish the diagnosis of bipolar disorder.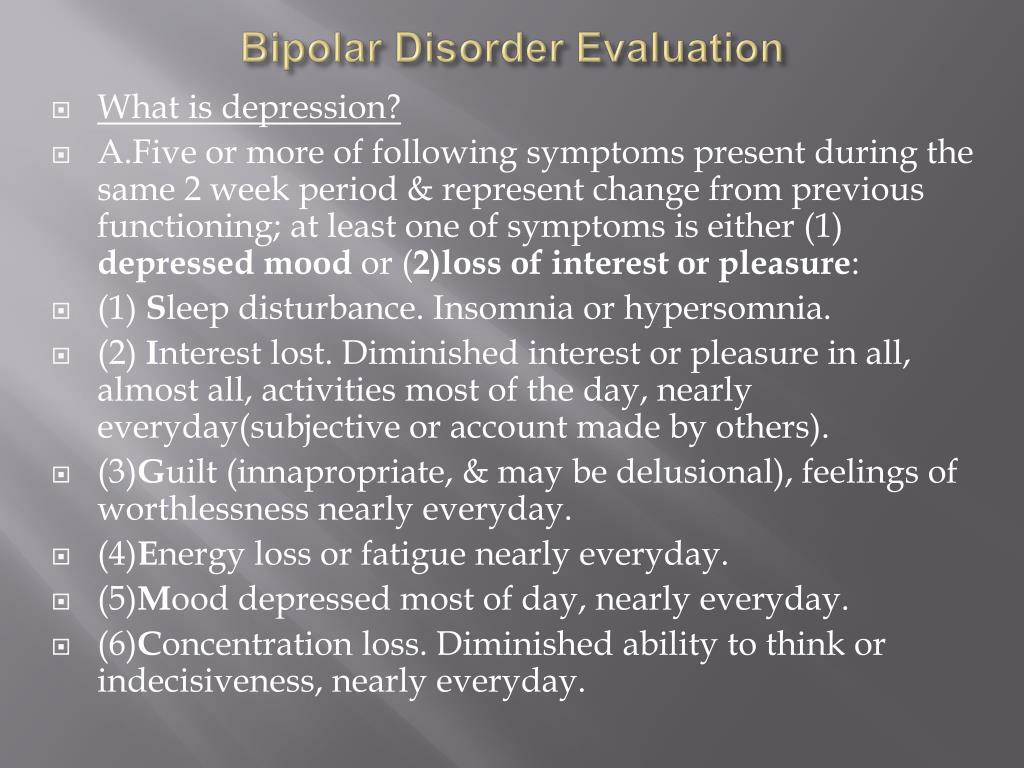 It requires an analysis of subjective - collected from the words of the patient, as well as objective - collected from the words of the immediate environment, anamnestic data, isolating information about affective episodes, the nature, duration and severity of their course.
It requires an analysis of subjective - collected from the words of the patient, as well as objective - collected from the words of the immediate environment, anamnestic data, isolating information about affective episodes, the nature, duration and severity of their course.
Features of the course of BAD in women
There is not much difference between the sexes in lifetime prevalence of bipolar affective disorder. However, there are several clinical characteristics that distinguish men and women with bipolar disorder.
Women have a later age of onset than men. They are more likely to debut during the fifth decade. Women with bipolar disorder are more likely to experience an episode of depression followed by mania, while men with bipolar disorder are either as likely or more likely to experience episodes of mania followed by depression.
A bimodal peak in psychiatric hospitalizations in spring and autumn is observed in women with bipolar disorder compared to a unimodal peak in men in the spring.
Some studies have shown gender differences in the long-term outcome of bipolar disorder. Women face significantly greater disruption to social/recreational and family life. This, apparently, is due to their irritability, increased self-confidence, talkativeness, windiness and excessive financial extravagance, since such behavior on the part of a woman is more condemned in society than on the part of a man.
Women are hospitalized much more often than men because they feel worse and tend to seek medical attention more often.
Complications
The most formidable complication of the disease, of course, is the possible suicide of the patient. The determination of suicidal risk is carried out at the very first diagnostic stage of the survey. It includes clarification of anamnestic data related to previous suicide attempts (if any), as well as an assessment of risk factors. There are special questionnaires that can help with this, for example, the Columbia Suicidal Intention Severity Scale.
Loss of connection with reality during the period of mania, in turn, can also lead to a person causing harm of varying degrees of severity to both himself and others.
BAD treatment
Medical therapy
Due to advances in research on pharmacological and psychosocial treatments for bipolar disorder, recommendations for the treatment of the disorder are frequently revised.
According to recent data, there are several types of treatment for acute mania: mood stabilizers (such as lithium and valproic acid) are widely used in combination with atypical antipsychotics (quetiapine, olanzapine, aripiprazole, risperidone, asenapine, paliperidone, and cariprazine). Typical neuroleptics are also effective in mania, although there is a risk of it switching to depression.
On the other hand, treatment options for acute bipolar depression are relatively limited. There is evidence supporting the efficacy of quetiapine and olanzapine, as well as the combination of olanzapine and fluoxetine, an antidepressant from the group of selective serotonin reuptake inhibitors.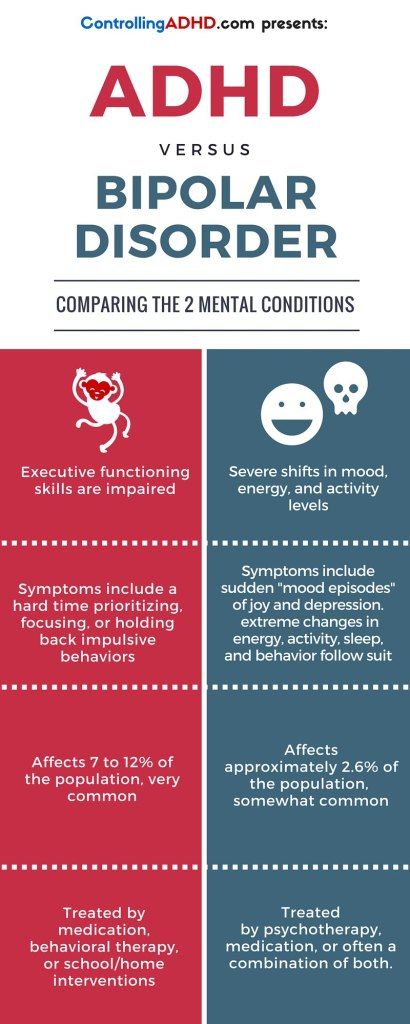 In the depressive phase, it is also possible to prescribe lithium.
In the depressive phase, it is also possible to prescribe lithium.
Widely available and common tricyclic antidepressants can cause rapid episode cycling and manic reversal, so they should not be used in bipolar disorder, even when combined with mood stabilizers.
Ketamine, which has a rapid antidepressant effect on treatment-resistant depression, can also be used to treat bipolar depression.
Neuromodulation
Electroconvulsive therapy finds its use in therapeutically resistant depression in bipolar disorder.
Transcranial magnetic stimulation is effective in unipolar depression and mania, but its effectiveness in bipolar depression has not yet been proven.
Other drugs and supplements
Some research suggests a possible beneficial effect of N-acetylcysteine, an antioxidant, on bipolar depression and ramelteon, a melatonin agonist, on mood stability. A meta-analysis found that omega-3 fatty acids are effective for bipolar depression but not for mania.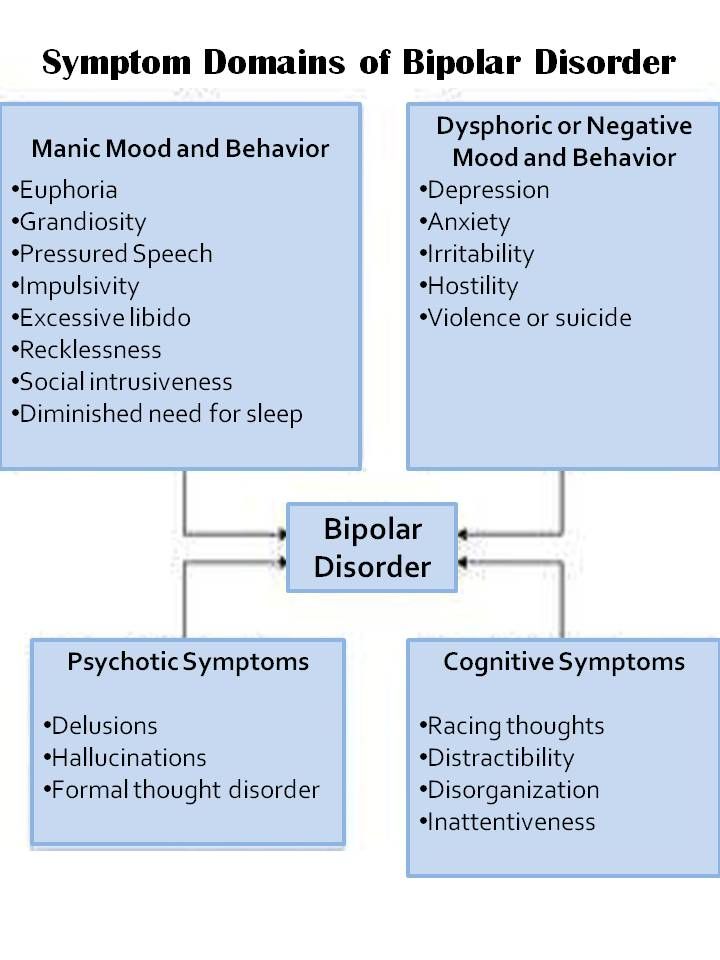 Clinical trials of nutritional supplements that improve mitochondrial function are currently ongoing.
Clinical trials of nutritional supplements that improve mitochondrial function are currently ongoing.
Psychosocial treatments
In the treatment of bipolar disorder, pharmacological and psychosocial approaches must work closely together.
With regard to psychosocial treatment, psychoeducation is paramount and should be carried out for all patients, as this significantly reduces the number of relapses.
Various types of psychotherapy are used in the treatment of bipolar disorder: interpersonal and social rhythm therapy (IPSRT) - a modified version of interpersonal therapy specifically designed for the treatment of bipolar disorder, family therapy, cognitive behavioral therapy (CBT).
Prognosis and prevention
Primary prevention of mental illness, the causes of which are not fully understood, is a difficult task. It seems rational to periodically screen the risk group - children of parents with an established diagnosis of bipolar disorder, the attentive attitude of doctors to the presence of an anxiety disorder in them, to subclinical symptoms of mood changes.