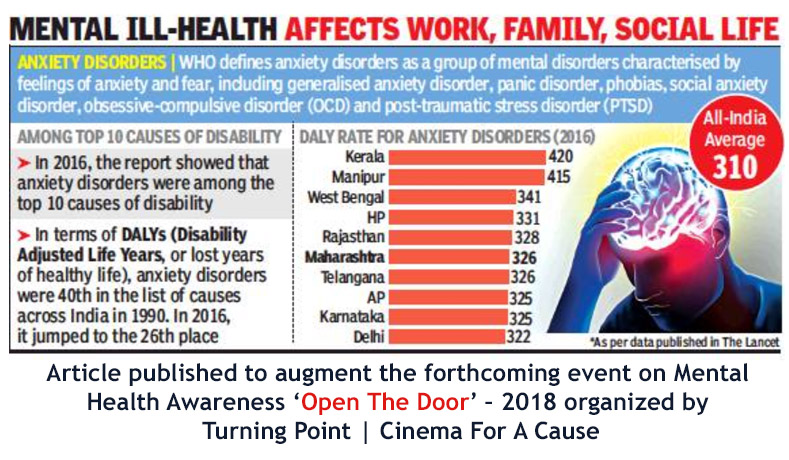
Mental health disorders definition
Schizophrenia
Schizophrenia- All topics »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Resources »
- Fact sheets
- Facts in pictures
- Multimedia
- Publications
- Questions & answers
- Tools and toolkits
- Popular »
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Monkeypox
- All countries »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Regions »
- Africa
- Americas
- South-East Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- WHO in countries »
- Statistics
- Cooperation strategies
- Ukraine emergency
- All news »
- News releases
- Statements
- Campaigns
- Commentaries
- Events
- Feature stories
- Speeches
- Spotlights
- Newsletters
- Photo library
- Media distribution list
- Headlines »
- Focus on »
- Afghanistan crisis
- COVID-19 pandemic
- Northern Ethiopia crisis
- Syria crisis
- Ukraine emergency
- Monkeypox outbreak
- Greater Horn of Africa crisis
- Latest »
- Disease Outbreak News
- Travel advice
- Situation reports
- Weekly Epidemiological Record
- WHO in emergencies »
- Surveillance
- Research
- Funding
- Partners
- Operations
- Independent Oversight and Advisory Committee
- Data at WHO »
- Global Health Estimates
- Health SDGs
- Mortality Database
- Data collections
- Dashboards »
- COVID-19 Dashboard
- Triple Billion Dashboard
- Health Inequality Monitor
- Highlights »
- Global Health Observatory
- SCORE
- Insights and visualizations
- Data collection tools
- Reports »
- World Health Statistics 2022
- COVID excess deaths
- DDI IN FOCUS: 2022
- About WHO »
- People
- Teams
- Structure
- Partnerships and collaboration
- Collaborating centres
- Networks, committees and advisory groups
- Transformation
- Our Work »
- General Programme of Work
- WHO Academy
- Activities
- Initiatives
- Funding »
- Investment case
- WHO Foundation
- Accountability »
- Audit
- Budget
- Financial statements
- Programme Budget Portal
- Results Report
- Governance »
- World Health Assembly
- Executive Board
- Election of Director-General
- Governing Bodies website
- Home/
- Newsroom/
- Fact sheets/
- Detail/
- Schizophrenia
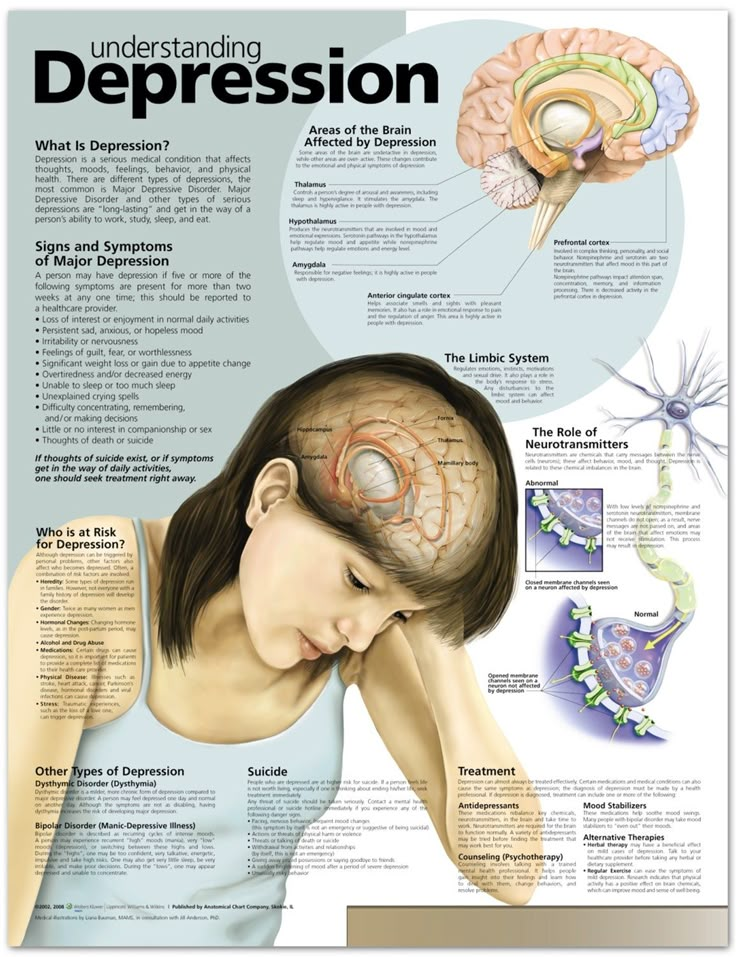
Key facts
- Schizophrenia causes psychosis and is associated with considerable disability and may affect all areas of life including personal, family, social, educational, and occupational functioning.
- Stigma, discrimination, and violation of human rights of people with schizophrenia are common.
- More than two out of three people with psychosis in the world do not receive specialist mental health care.
- A range of effective care options for people with schizophrenia exist and at least one in three people with schizophrenia will be able to fully recover.
Schizophrenia is characterised by significant impairments in the way reality is perceived and changes in behaviour related to:
- persistent delusions: the person has fixed beliefs that something is true, despite evidence to the contrary;
- persistent hallucinations: the person may hear, smell, see, touch, or feel things that are not there;
- experiences of influence, control or passivity: the experience that one’s feelings, impulses, actions, or thoughts are not generated by oneself, are being placed in one’s mind or withdrawn from one’s mind by others, or that one’s thoughts are being broadcast to others;
- disorganized thinking, which is often observed as jumbled or irrelevant speech;
- highly disorganised behaviour e.
 g. the person does things that appear bizarre or purposeless, or the person has unpredictable or inappropriate emotional responses that interfere with their ability to organise their behaviour;
g. the person does things that appear bizarre or purposeless, or the person has unpredictable or inappropriate emotional responses that interfere with their ability to organise their behaviour; - “negative symptoms” such as very limited speech, restricted experience and expression of emotions, inability to experience interest or pleasure, and social withdrawal; and/or
- extreme agitation or slowing of movements, maintenance of unusual postures.
People with schizophrenia often also experience persistent difficulties with their cognitive or thinking skills, such as memory, attention, and problem-solving.
At least one third of people with schizophrenia experiences complete remission of symptoms (1). Some people with schizophrenia experience worsening and remission of symptoms periodically throughout their lives, others a gradual worsening of symptoms over time.
Magnitude and impact
Schizophrenia affects approximately 24 million people or 1 in 300 people (0.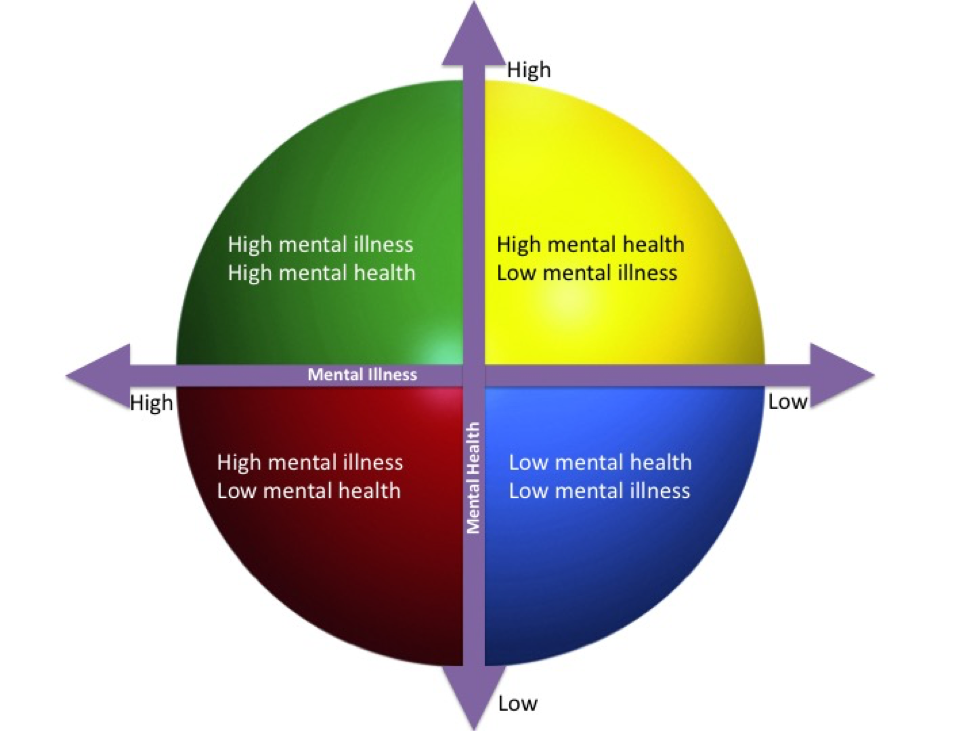 32%) worldwide. This rate is 1 in 222 people (0.45%) among adults (2). It is not as common as many other mental disorders. Onset is most often during late adolescence and the twenties, and onset tends to happen earlier among men than among women.
32%) worldwide. This rate is 1 in 222 people (0.45%) among adults (2). It is not as common as many other mental disorders. Onset is most often during late adolescence and the twenties, and onset tends to happen earlier among men than among women.
Schizophrenia is frequently associated with significant distress and impairment in personal, family, social, educational, occupational, and other important areas of life.
People with schizophrenia are 2 to 3 times more likely to die early than the general population (3). This is often due to physical illnesses, such as cardiovascular, metabolic, and infectious diseases.
People with schizophrenia often experience human rights violations both inside mental health institutions and in community settings. Stigma against people with this condition is intense and widespread, causing social exclusion, and impacting their relationships with others, including family and friends. This contributes to discrimination, which in turn can limit access to general health care, education, housing, and employment.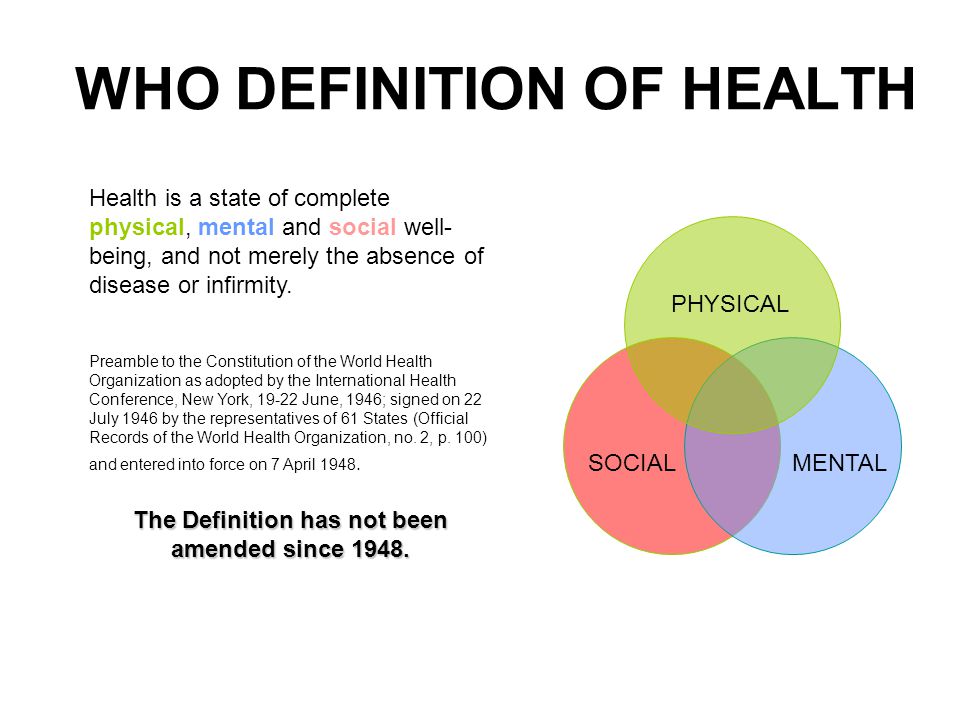
During humanitarian and public health emergencies, extreme stress and fear, breakdown of social supports, isolation and disruption of health-care services and supply of medication can occur. These changes can have an impact on the lives of people with schizophrenia, such as exacerbation of existing symptoms. During emergencies, people with schizophrenia are more vulnerable than others to various human rights violations, including neglect, abandonment, homelessness, abuse and exclusion.
Causes of schizophreniaResearch has not identified one single cause of schizophrenia. It is thought that an interaction between genes and a range of environmental factors may cause schizophrenia. Psychosocial factors may also affect the onset and course of schizophrenia. Heavy use of cannabis is associated with an elevated risk of the disorder.
ServicesCurrently, the vast majority of people with schizophrenia around the world are not receiving mental health care.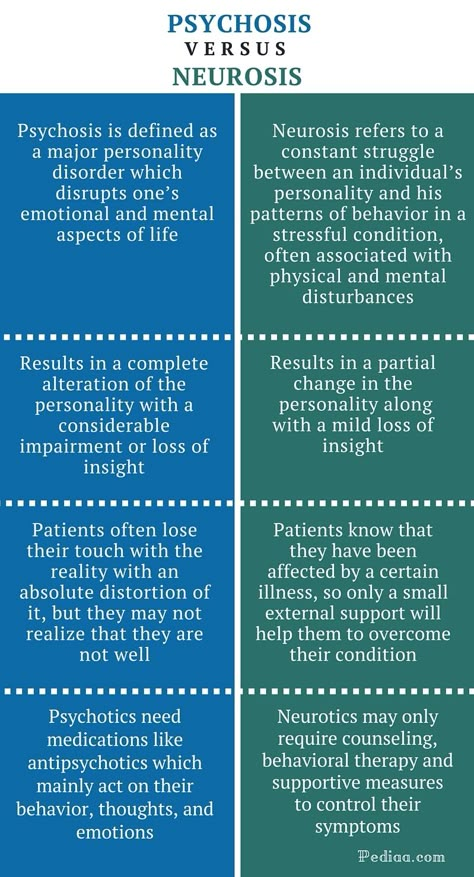 Approximately 50% of people in mental hospitals have a schizophrenia diagnosis (4). Only 31.3% of people with psychosis receive specialist mental health care (5). Most resources for mental health services are inefficiently spent on care within mental hospitals.
Approximately 50% of people in mental hospitals have a schizophrenia diagnosis (4). Only 31.3% of people with psychosis receive specialist mental health care (5). Most resources for mental health services are inefficiently spent on care within mental hospitals.
There is clear evidence that mental hospitals are not effective in providing the care that people with mental health conditions need and, regularly, violate the basic human rights of persons with schizophrenia. Efforts to transfer care from mental health institutions to the community need to be expanded and accelerated. Such efforts start with the development of a range of quality community-based mental health services. Options for community-based mental health care include integration in primary health and general hospital care, community mental health centres, day centres, supported housing, and outreach services for home-based support. The engagement of the person with schizophrenia, family members and the wider community in providing support is important.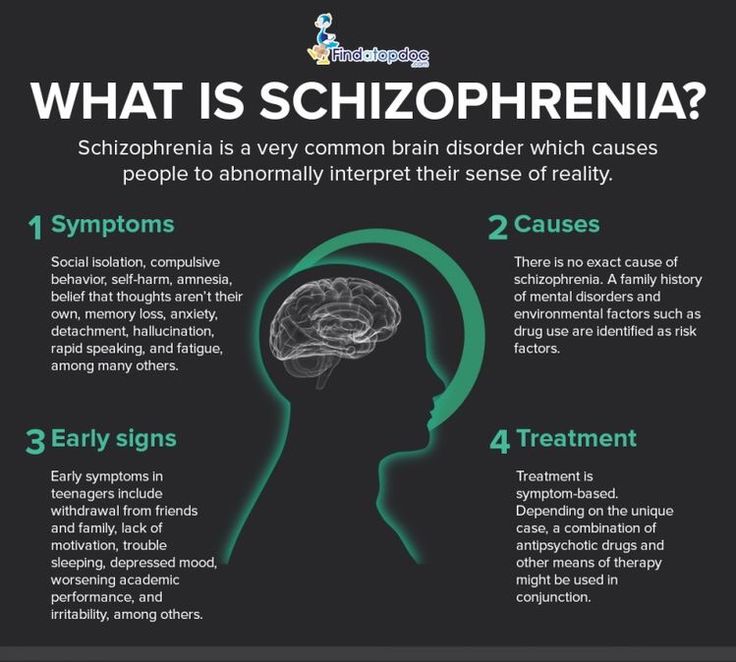
A range of effective care options for people with schizophrenia exist, and these include medication, psychoeducation, family interventions, cognitive-behavioural therapy and psychosocial rehabilitation (e.g., life skills training). Facilitated assisted living, supported housing and supported employment are essential care options that should be available for people with schizophrenia. A recovery-oriented approach – giving people agency in treatment decisions – is essential for people with schizophrenia and for their families and/or caregivers as well.
WHO responseWHO’s Comprehensive Mental Health Action Plan 2013-2030 highlights the steps required to provide appropriate services for people with mental disorders including schizophrenia. A key recommendation of the Action Plan is to shift services from institutions to the community. The WHO Special Initiative for Mental Health aims to further progress towards objectives of the Comprehensive Mental Health Action Plan 2013-2030 by ensuring 100 million more people have access to quality and affordable care for mental health conditions.
WHO's Mental Health Gap Action Programme (mhGAP) uses evidence-based technical guidance, tools and training packages to expand service in countries, especially in resource-poor settings. It focuses on a prioritized set of conditions, including psychosis, directing capacity building towards non-specialized health-care providers in an integrated approach that promotes mental health at all levels of care. Currently mhGAP is being implemented in more than 100 WHO Member States.
The WHO QualityRights Project involves improving the quality of care and human rights conditions in mental health and social care facilities and to empower organizations to advocate for the health of people with mental health conditions and psychosocial disabilities.
The WHO guidance on community mental health services and person-centred and rights-based approaches provides information and support to all stakeholders who wish to develop or transform their mental health system and services to align with international human rights standards including the UN Convention on the Rights of Persons with Disabilities.
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J. Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
(2) Institute of health Metrics and Evaluation (IHME). Global Health Data Exchange (GHDx). http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/27a7644e8ad28e739382d31e77589dd7 (Accessed 25 September 2021)
(3) Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annual Review of Clinical Psychology, 2014;10, 425-438.
(4) WHO. Mental health systems in selected low- and middle-income countries: a WHO-AIMS cross-national analysis. WHO: Geneva, 2009
(5) Jaeschke K et al. Global estimates of service coverage for severe mental disorders: findings from the WHO Mental Health Atlas 2017 Glob Ment Health 2021;8:e27.
WHO’s Comprehensive Mental Health Action Plan 2013-2030
WHO Special Initiative for Mental Health
WHO's Mental Health Gap Action Programme (mhGAP)
WHO QualityRights Project
WHO guidance on community mental health services and person-centred and rights-based approaches
More on mental health
Autism
It is estimated that worldwide about one in 100 children has autism(1). This estimate represents an average figure, and reported prevalence varies substantially across studies. Some well-controlled studies have, however, reported figures that are substantially\r\n higher. The prevalence of autism in many low- and middle-income countries is unknown.
This estimate represents an average figure, and reported prevalence varies substantially across studies. Some well-controlled studies have, however, reported figures that are substantially\r\n higher. The prevalence of autism in many low- and middle-income countries is unknown.
Causes
Available scientific evidence suggests that there are probably many factors that make a child more likely to have autism, including environmental and genetic factors.
Available epidemiological data conclude that there is no evidence of a causal association between measles, mumps and rubella vaccine, and autism. Previous studies suggesting a causal link were found to be filled with methodological flaws(2)(3).
There is also no evidence to suggest that any other childhood vaccine may increase the risk of autism. Evidence reviews of the potential association between the preservative thiomersal and aluminium adjuvants contained in inactivated vaccines and the\r\n risk of autism strongly concluded that vaccines do not increase the risk of autism.
Assessment and care
A broad range of interventions, from early childhood and across the life span, can optimize the development, health, well-being and quality of life of autistic people. Timely access to early evidence-based psychosocial interventions can improve the ability\r\n of autistic children to communicate effectively and interact socially. The monitoring of child development as part of routine maternal and child health care is recommended.
It is important that, once autism has been diagnosed, children, adolescents and adults with autism and their carers are offered relevant information, services, referrals, and practical support, in accordance with their individual and evolving needs and\r\n preferences.
The health-care needs of people with autism are complex and require a range of integrated services, that include health promotion, care and rehabilitation. Collaboration between the health sector and other sectors, particularly education, employment and\r\n social care, is important.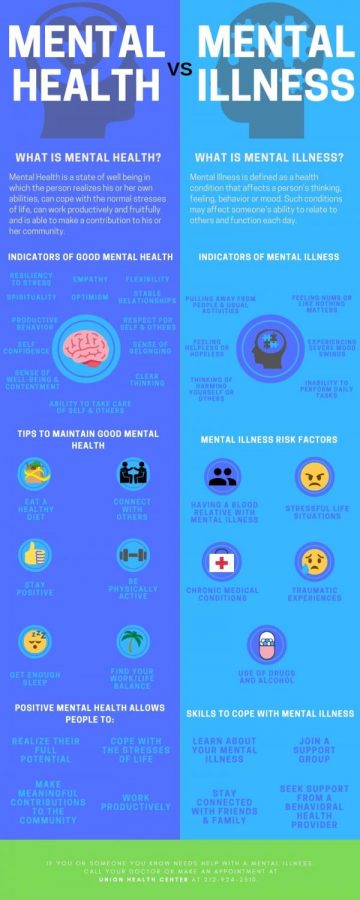
Interventions for people with autism and other developmental disabilities need to be designed and delivered with the participation of people living with these conditions. Care needs to be accompanied by actions at community and societal levels for greater accessibility, inclusivity and support.
Human rights
All people, including people with autism, have the right to the enjoyment of the highest attainable standard of physical and mental health.
And yet, autistic people are often subject to stigma and discrimination, including unjust deprivation of health care, education and opportunities to engage and participate in their communities.
People with autism have the same health problems as the general population. However, they may, in addition, have specific health-care needs related to autism or other co-occurring conditions. They may be more vulnerable to developing chronic noncommunicable\r\n conditions because of behavioural risk factors such as physical inactivity and poor dietary preferences, and are at greater risk of violence, injury and abuse.
People with autism require accessible health services for general health-care needs like the rest of the population, including promotive and preventive services and treatment of acute and chronic illness. Nevertheless, autistic people have higher rates\r\n of unmet health-care needs compared with the general population. They are also more vulnerable during humanitarian emergencies. A common barrier is created by health-care providers’ inadequate knowledge and understanding of autism.
WHO resolution on autism spectrum disorders
In May 2014, the Sixty-seventh World Health Assembly adopted a resolution entitled Comprehensive and coordinated efforts for the management of autism spectrum disorders,\r\n which was supported by more than 60 countries.
The resolution urges WHO to collaborate with Member States and partner agencies to strengthen national capacities to address ASD and other developmental disabilities.
WHO response
WHO and partners recognize the need to strengthen countries' abilities to promote the optimal health and well-being of all people with autism.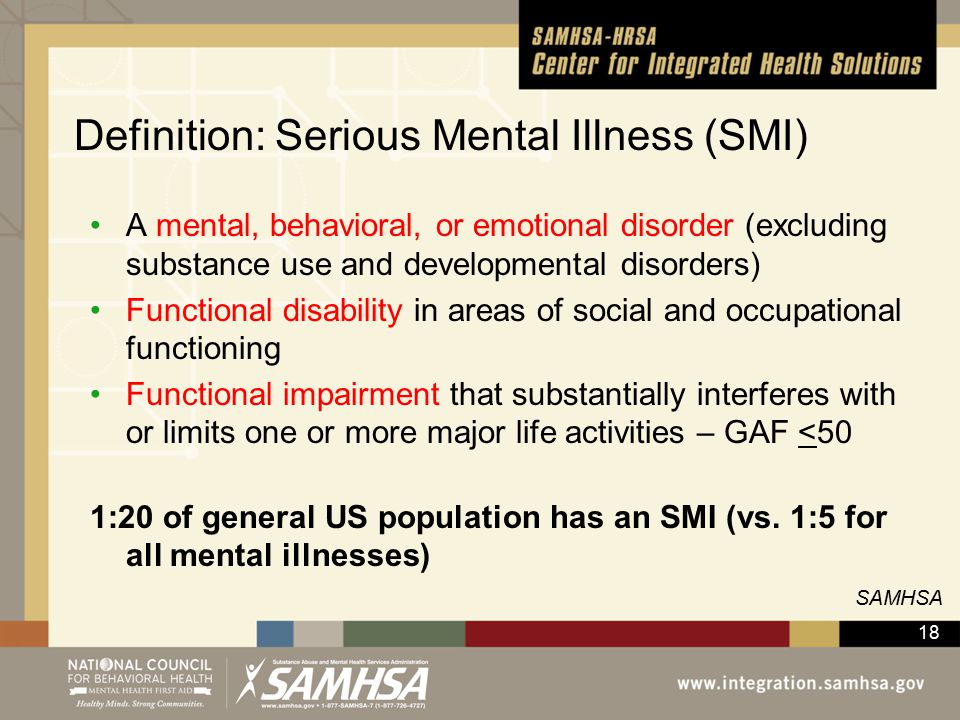
WHO's efforts focus on:
- increasing the commitment of governments to taking action to improve the quality of life of people with autism;
- providing guidance on policies and action plans that address autism within the broader framework of health, mental and brain health and disabilities;
- contributing to strengthening the ability of the health workforce to provide appropriate and effective care and promote optimal standards of health and well-being for people with autism; and
- promoting inclusive and enabling environments for people with autism and other developmental disabilities and providing support to their caregivers.
WHO Comprehensive mental health action plan 2013–2030 and World Health Assembly Resolution WHA73.10 for “global actions on epilepsy and other neurological disorders” calls on countries to address the current significant\r\n gaps in early detection, care, treatment and rehabilitation for mental and neurodevelopmental conditions, which include autism.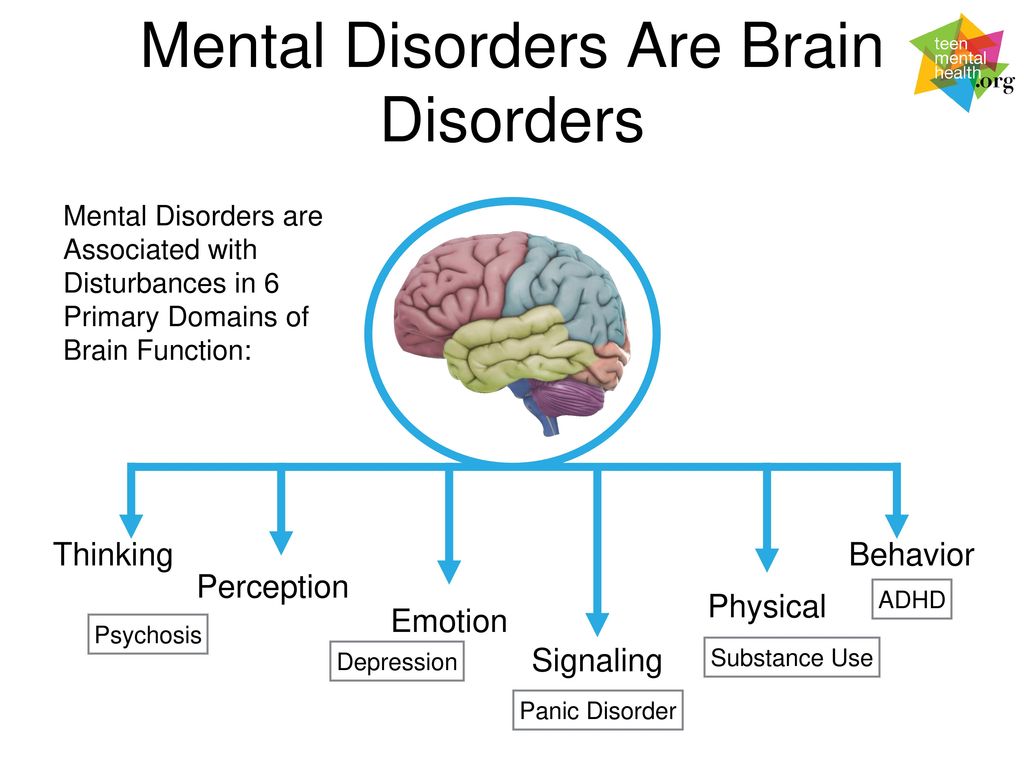 It also calls for counties to address the social, economic, educational and inclusion needs of people living with mental\r\n and neurological disorders, and their families, and to improve surveillance and relevant research.
It also calls for counties to address the social, economic, educational and inclusion needs of people living with mental\r\n and neurological disorders, and their families, and to improve surveillance and relevant research.
References
(1) Global prevalence of autism: A systematic review update. Zeidan J et al. Autism Research 2022 March.
(2) Wakefield's affair: 12 years of uncertainty whereas no link between autism and MMR vaccine has been proved. Maisonneuve H, Floret D. Presse Med. 2012 Sep; French (https://www.ncbi.nlm.nih.gov/pubmed/22748860).\r\n
(3) Lancet retracts Wakefield’s MMR paper. Dyer C. BMJ 2010;340:c696. 2 February 2010 (https://pubmed.ncbi.nlm.nih.gov/20124366/)\r\n
","datePublished":"2022-03-30T13:32:00.0000000+00:00","image":"https://cdn.who.int/media/images/default-source/health-topics/mental-health/autism.jpg?sfvrsn=d518329b_8","publisher":{"@type":"Organization","name":"World Health Organization: WHO","logo":{"@type":"ImageObject","url":"https://www.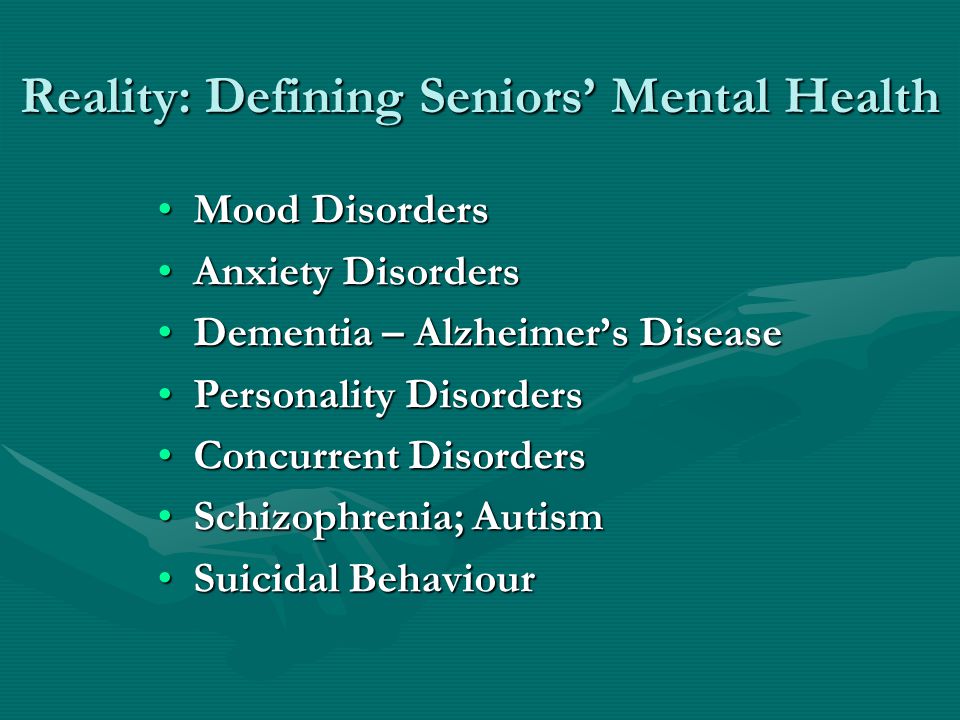 who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified":"2022-03-30T13:32:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/news-room/fact-sheets/detail/autism-spectrum-disorders","@context":"http://schema.org","@type":"Article"};
who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified":"2022-03-30T13:32:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/news-room/fact-sheets/detail/autism-spectrum-disorders","@context":"http://schema.org","@type":"Article"};
Personality disorder test
- Tests
- types
- articles
- news
- Members
- Search
This test is also available in these languages:
This 105-question Personality Disorder Test will tell you what your personality traits are. This test provides more dynamic and detailed information about your personal qualities than the Jung test or the Big Five test.
While taking this test, it is normal to feel that many of the aspects presented describe your personality.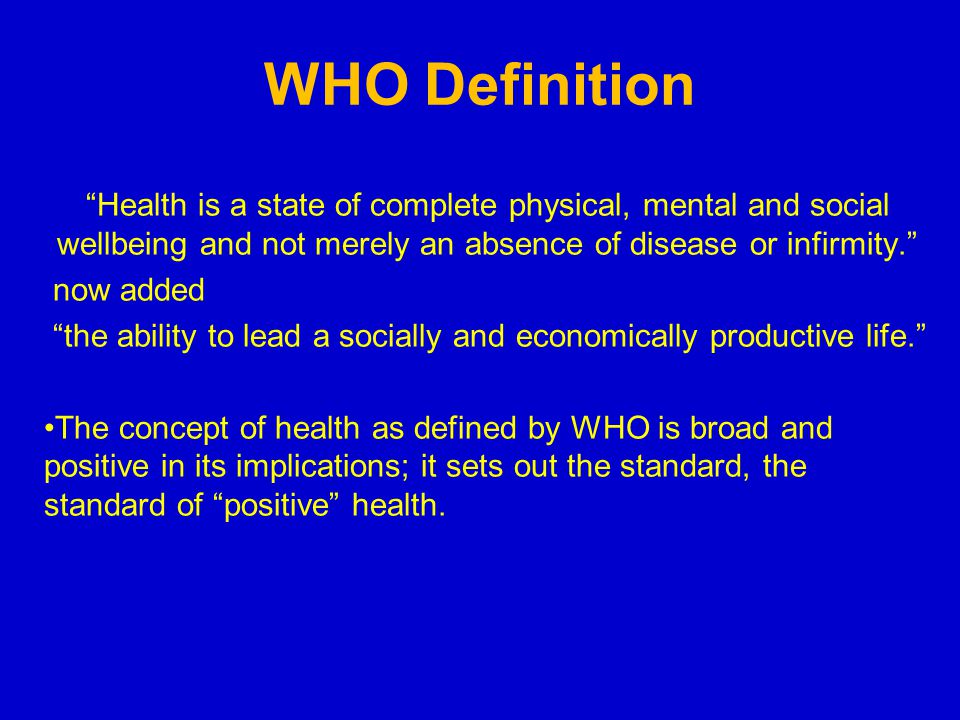 However, for best results, DO NOT click Agree if the statement only partially describes your behavior or character. If you are in doubt, please click "I disagree".
However, for best results, DO NOT click Agree if the statement only partially describes your behavior or character. If you are in doubt, please click "I disagree".
Question 1 of 105
I'm planning far more events and projects than I can physically handle - even though a moon base is a good idea!
I agree I disagree
PROCEED BACK
Advertisement
The Personality Disorder Test is the property of IDR Labs International, but pays homage to the work of Theodore Millon, Seth Grossman, Aaron T. Beck, Arthur Freeman, and Nancy McWilliams.
This test helps to identify a possible mental disorder in your personality, however, it is worth noting that the results of the test do not necessarily correspond to real clinical studies conducted by registered medical professionals with the personal presence of the respondent, numerous conversations with the respondent and the presence of his or her personal and family data , in particular.
Accordingly, please note that this test provides information about personality types for educational purposes only. The information is provided "as is" and should not be construed as the provision of professional services or warranties of any kind. The Company is under no obligation to provide legal, medical, financial or any other professional services. If you need qualified assistance, please contact the relevant institutions.
Personality Disorder Test© is the property of IDR Labs International. To find out more, please see our Terms of Service.
Mental disorders: classification and definition of mental disorders, causes of occurrence
According to their classification, mental disorders can be divided into two groups: endogenous and exogenous. The first group includes diseases that have a genetic cause or metabolic disorders, the second group includes diseases provoked by environmental factors - drugs, alcohol, infections, conflicts with others, etc. In the process of diagnosis, it is important to establish what led to a mental disorder and work with the cause of the disease.
The first group includes diseases that have a genetic cause or metabolic disorders, the second group includes diseases provoked by environmental factors - drugs, alcohol, infections, conflicts with others, etc. In the process of diagnosis, it is important to establish what led to a mental disorder and work with the cause of the disease.
Submit an application for diagnosis and treatment
I confirm that I accept the terms of consent to the processing of personal data.
Mental illnesses are mental disorders ranging from minor ones, like a stress response, to severe ones, like schizophrenia or a personality disorder. Any mental disorders cause certain changes in the behavior and thinking of a person. For quite a long time, psychiatry was considered the most frightening branch of medicine, this was due to the fact that it used quite radical methods, such as lobotomy, shock therapy and insulin coma, as a result of which the patient could lose basic vital functions.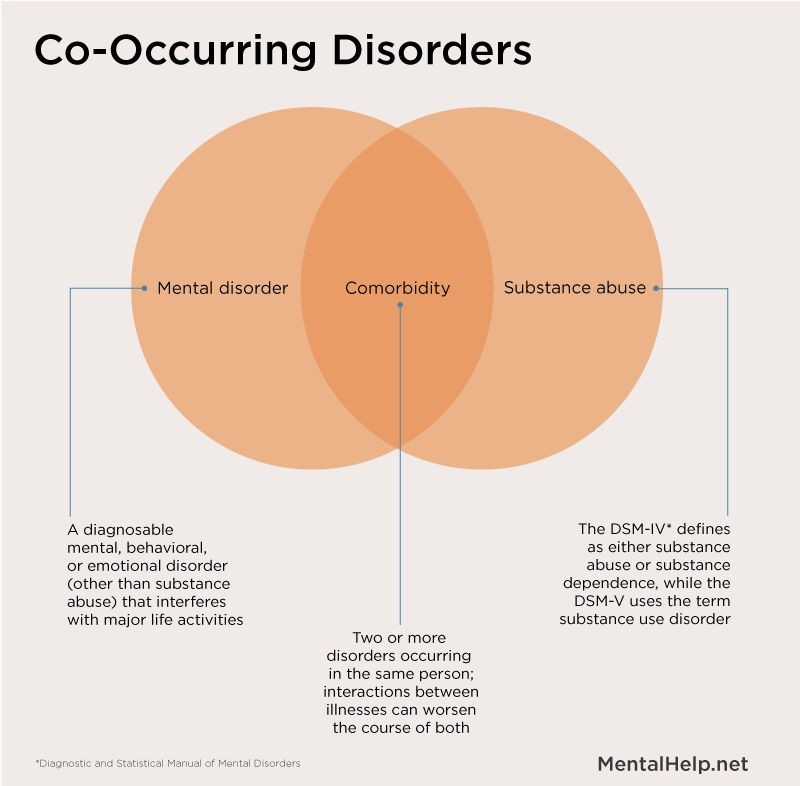 Many patients are still afraid to visit a psychiatrist, even if they themselves understand that there are mental problems. What types of mental disorders exist? How to recognize them?
Many patients are still afraid to visit a psychiatrist, even if they themselves understand that there are mental problems. What types of mental disorders exist? How to recognize them?
Causes of mental disorders
All types of mental disorders occur due to disturbances in the functions of the brain, in particular, in the emotional sphere, cognitive aspects. Specialists identify 2 groups of factors that can cause mental disorders:
- Endogenous factor. This includes genetic, hereditary diseases, various disorders in the chromosomes. However, the catalysts that trigger the disease process are still unknown to science;
- Exogenous factor. This should include narcotic, toxic substances, industrial poisons, alcoholic beverages, viruses, traumatic brain injuries, stress and other factors that affect a person's mental health.
According to statistics, about a quarter of all people are prone to pathological changes in behavior and to the occurrence of various types of mental disorders.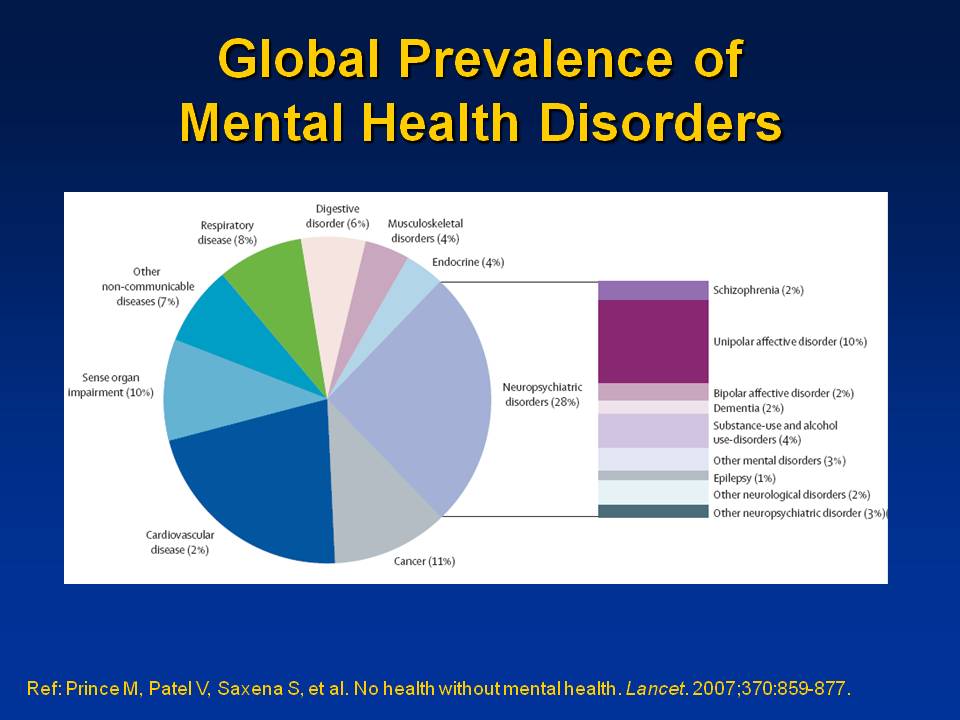 There are psychological and biological factors that contribute to the launch of mental illness. Psychological reasons include, in particular, improper upbringing, various mental traumas, stressful environment in which the patient has been for a long time. Biological factors include various diseases - diabetes mellitus, stroke, infectious lesions. Also, this should include the constant abuse of alcohol and psychoactive substances.
There are psychological and biological factors that contribute to the launch of mental illness. Psychological reasons include, in particular, improper upbringing, various mental traumas, stressful environment in which the patient has been for a long time. Biological factors include various diseases - diabetes mellitus, stroke, infectious lesions. Also, this should include the constant abuse of alcohol and psychoactive substances.
Classification of mental disorders
The World Health Organization has developed a table of classification and definitions of mental disorders:
| Schizotypal disorder and schizophrenia | previously a person's hobbies, in a decrease in interest in life and work. If all the symptoms described are mild, then we are talking about a schizotypal disorder. |
| Neuroses and phobias | These include panic attacks, neuroses.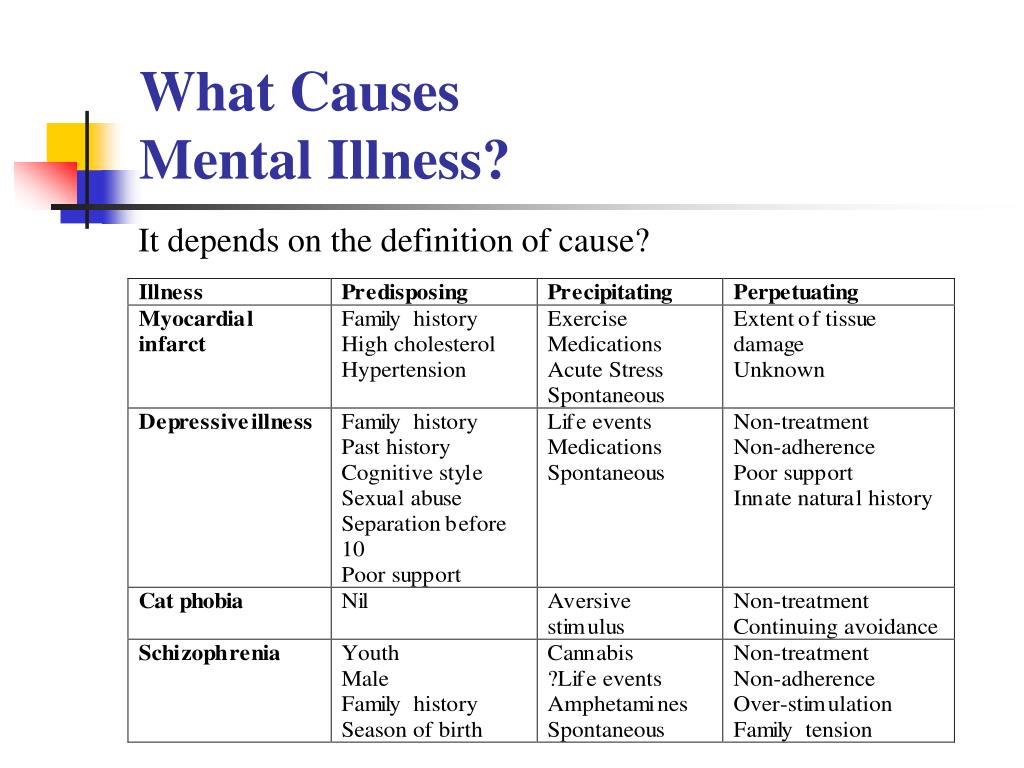 Also, such patients suffer from chronic stress and paranoia. Phobias can manifest themselves in relation to certain objects or situations. Also, such patients suffer from chronic stress and paranoia. Phobias can manifest themselves in relation to certain objects or situations. |
| Affective disorder | This group should include various depressive conditions, dysthymia and cyclothymia. In particular, the most prominent representative of this group is bipolar affective disorder. The main characteristic is frequent and abrupt mood swings, the presence of depression and mania. |
| Mental problems caused by substance or alcohol abuse | This group includes conditions caused by the abuse of drinks or drugs, sedatives, hallucinogenic drugs and others. |
| Mental health problems caused by organic brain lesions | This group includes post-stroke conditions, conditions after traumatic brain injury and systemic diseases. In particular, there are not only changes in thinking, memory and behavior, but there may be hallucinations, delirium, sudden changes in mood, and more. |
| Mental retardation | This disorder can only be congenital. Manifested in a decrease in the ability of the intellect. The patient cannot fully think, speak, think. Memory and adaptation in society also suffer. Retardation can be mild, moderate, moderate and severe. The most common causes are lack of attention to the child in infancy, hereditary factors, intrauterine growth retardation and trauma during childbirth. |
| Physiological causes of disorders | This group includes diseases such as bulimia, anorexia, overeating, as well as sleep problems - insomnia, somnambulism and hypersomnia. Also, this also includes problems of a sexual nature - premature ejaculation, frigidity and more. |
| Problems in psychological development | Disorders of this group begin in childhood and persist throughout life. It is expressed in problems with memory, speech, emotional and cognitive development. It does not have remissions or relapses, the condition persists permanently. |
| Personality disorder | Disorders of this group appear in adulthood. This group includes many conditions - in particular, those associated with sexual addictions (masochism or sadism, fetishism, voyeurism), gender identity. Also, kleptomania, sociopathy, self-harm should be attributed to the disorders of this group. |
| Attention-related disorders | This type of mental disorder mainly affects children with hyperactivity, which still often manifests itself in a tendency to aggression. |
We have listed the main definitions of mental disorders. If you or your loved one notice unusual emotions, behavioral patterns, illogical speech, neglect of appearance, sleep problems, excessively elevated or, on the contrary, depressed state, hallucinations, derealization, you should contact a specialist. Most likely, it is a mental disorder. Specialists of the private clinic "IsraClinic" are experienced professional doctors who know how to work with each patient individually.