The doubting disease
OCD: The Doubting Disease - SocialWorker.com
×
Expand
Photo credit: BigStockPhoto/anabaraulia
Obsessive Compulsive Disorder
by Brittany Stahnke, DSW, LCSW, LMFT
The second week of October is OCD Awareness Week. It is the time of year when sufferers reflect on all they’ve been through, all they’ve lost. It is the time when they think about how many more are out there, suffering in silence, unknowing to the true nature of their pain. We, as clinicians, can change this by first knowing how to identify the disorder when we see it in a client.
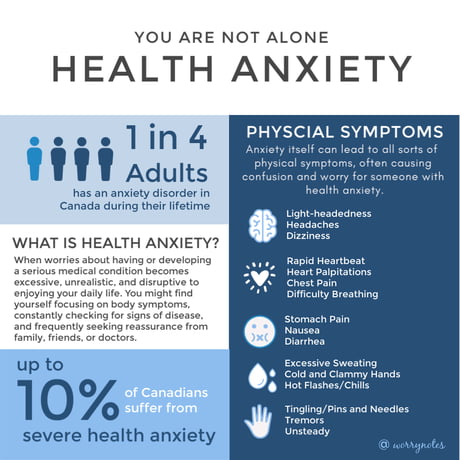
Obsessive-compulsive disorder (OCD) affects two to three percent of the population and has been considered one of the most disabling disabilities in our world as a result of the loss of income and quality of life (Ocduk.org, 2020). Because of existing ignorance about its presentation and treatment, OCD sufferers usually go undiagnosed for 10 or more years.
OCD is one of the most misdiagnosed and misunderstood disorders. One study that assessed clinicians’ abilities to correctly identify the presentation of obsessive-compulsive disorder found that 39% of clinicians, and as high as 44% depending on the specific OCD presentation, misdiagnosed cases of OCD (Glazier et al., 2013).
Although some professionals will under-diagnose with anxiety or depression, causing lack of proper treatment and likely a progression of symptoms, others will over-diagnose, possibly causing a quicker and uglier progression of those symptoms. In such cases, practitioners have been known to misdiagnose those with OCD with psychotic disorders. In one case study, a man misdiagnosed with the lifelong, severe, psychotic schizoaffective disorder was medicated with anti-psychotics, which led to a worsening of as well as new obsessive-compulsive symptoms (Leung & Palmer, 2016). In another case, a 13-year-old boy was believed to be psychotic, rather than having OCD, because he acted on his sexual obsessions (Rohanachandra & Vipulanandan, 2019). When prescribed anti-psychotics, his symptoms became worse. After being properly diagnosed and medicated for OCD, the patient improved, and compulsions disappeared. Months later, the patient remained healthy.
When prescribed anti-psychotics, his symptoms became worse. After being properly diagnosed and medicated for OCD, the patient improved, and compulsions disappeared. Months later, the patient remained healthy.
Psychotic disorders feature hallucinations and delusions as their hallmark symptoms. Unlike those with psychotic disorders, OCD patients’ hallmark symptoms are obsessions and compulsions. While those with severe OCD can feature psychotic features, these are caused by the obsessions rather than being stand-alone and primary symptoms.
The diagnosis of obsessive-compulsive disorder (American Psychiatric Association, 2022) requires the presence of:
- Obsessions (recurrent and persistent thoughts, urges, or impulses that are experienced, at some time during the disturbance, as intrusive and unwanted, and that in most individuals cause marked anxiety or distress) that an individual attempts to ignore or suppress; and/or
- Compulsions (repetitive behaviors - e.
 g., hand washing, ordering, checking, or mental acts such as praying, counting, repeating words silently) that the individual feels driven to perform in response to an obsession or according to rules that must be applied rigidly.
g., hand washing, ordering, checking, or mental acts such as praying, counting, repeating words silently) that the individual feels driven to perform in response to an obsession or according to rules that must be applied rigidly.
The obsessions and compulsions are time-consuming and take at least one hour per day, significantly impairing the functioning day-to-day life of the sufferer. Despite the DSM-V-TR listing OCD as requiring either obsessions or compulsions, OCD experts now know that OCD always has both. The compulsions of some individuals are simply invisible and are given the false misnomer of “Pure O OCD,” as they reside inside their minds.
Intrusive thought OCD or “Pure O” is the most severe form of the disorder, both before and after treatment (McCarty et al., 2017). It is also the most misdiagnosed (Glazier et al., 2013). While most people with taboo intrusive thoughts do not act on those thoughts, some individuals who have no insight into the thoughts can believe those thoughts have meaning and respond to them as commands in order to rid themselves of the thoughts.
Common compulsions to try to rid of such intrusive thoughts include counting, praying, talking back to thoughts, or “checking” if they are having a sexual urge. These unwanted thoughts can be violent or sexual, causing severe anxiety that the sufferer will act on the thought.
Clinicians can mistake these individuals as violent, pedophilic, or a number of other damaging labels. Thus, the difference between someone with OCD and someone who is violent or sexual is important. The person with OCD is repulsed by the thoughts, and there is no real desire to act on them. Instead, there is fear that they will.
When Doubting Is Disorder
People with OCD cannot tolerate doubt. A thought just like any other thought comes into our head. The thought is distasteful, negative, unpleasant. It may be a thought of putting a cat in a microwave. It may be a thought of touching a child’s genitals. Or having sex with a person of the sex that is not the true desire of that person. Or cheating. Shouting out inside of church.
Or cheating. Shouting out inside of church.
We all have these thoughts. All of us. In fact, a large study of 777 university students across 13 countries demonstrated this finding (Radomsky et al., 2014). But the differences between those who have OCD and those who do not is not the thought content. It is the reaction. OCD is very much a thought disorder—over time, these thoughts “stick” in a way that they do not in other brains, and we emotionally respond to these stuck thoughts. But more than a thought disorder, it is an emotional one.
People with OCD begin to over-analyze and over-consider the thought that comes. What does it mean? Does this mean I am a pedophile? Or I am going to harm my child? Or my cat? Can I trust myself to not shout profanities in inappropriate situations? Am I gay/straight? Is this the right relationship? Did I leave the oven on? Am I possessed? Did I get HIV from that handshake?
Obsessive-compulsive disorder is one of the few mental health diagnoses that has been found to be associated with brain abnormalities. There is difficulty in those with OCD recognizing “errors” in thinking and moving on from those errors without acting on them. In essence, the brain’s thoughts easily stick.
There is difficulty in those with OCD recognizing “errors” in thinking and moving on from those errors without acting on them. In essence, the brain’s thoughts easily stick.
PET scans of OCD brains reveal a brain that does not rest. Activity levels in certain parts of the brain, including the limbic system—the emotional center of the brain—are much higher than in comparison subjects. Further, fMRI scans show the same activity differences. On the other hand, in certain areas of the frontal cortex, responsible for our highest cognitive functioning, brains of people with OCD show less activity (Dieter et al., 1997).
Similarly, in a study with 1,700 participants in Amsterdam, major differences in the structure of OCD brains were found (Boedhoe et al., 2018). In particular, they noted that the parietal lobe—a part of the brain thought to be involved in attention, planning, and response inhibition—was thinner in people with the disorder. These brain functions are often impaired in people with OCD, and such abnormalities might contribute to patients’ uncontrolled repetitive behaviors.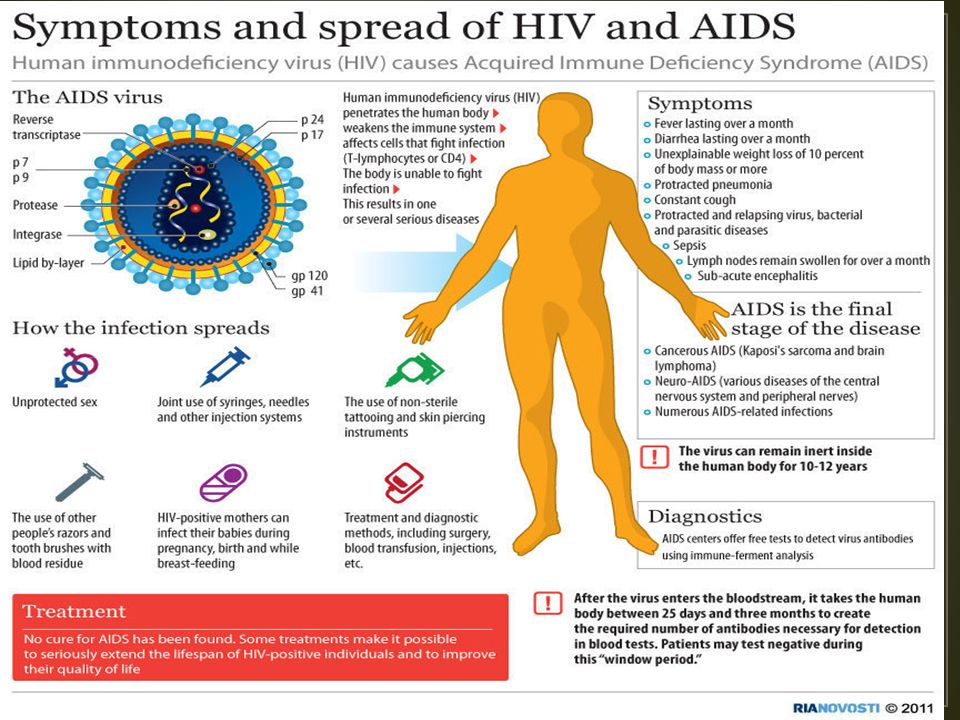
Accurate diagnosis is crucial. Without educating ourselves to the OCD mind, we leave our clients vulnerable to those minds. Minds that will always be present, in every bad or good thing that happens to them. Minds that are looking for vulnerabilities, flaws, opportunities to doubt, and traumas to feed them.
To Do
When people think of OCD, or joke that they are “so OCD,” they mean one of a few things. They are clean; they are picky; they want things a certain way. They are essentially perfectionistic.
This is not OCD. Most of us with OCD are not super clean or super hygienic. OCD is not cleanliness. OCD is not arranging things, and it is certainly not perfectionism. Although some people with OCD have obsessions about cleanliness, health, and symmetry that would present with associated compulsions, this is only one presentation.
OCD is not a disorder that anyone who knows its true nature would joke about. It is a disorder in which the obsessions of the mind take over to a degree that controls your thoughts, emotions, behaviors, and eventually, your life.
It is a disorder in which the obsessions of the mind take over to a degree that controls your thoughts, emotions, behaviors, and eventually, your life.
Obsessive-compulsive disorder, like many other mental illnesses, takes lives, breaks families, and erases identities. For anyone who suffers a serious mental illness, it is isolating. But the most isolating factor is the misunderstanding from society, family, and friends, and even clinicians whose job it is to understand.
These misperceptions and misdiagnoses can be minimized through an effort toward knowledge and away from stereotype—through education and ethical care. We cannot ever be confident enough to risk the health of a client. When someone isn’t improving, refer. When we do not know or only claim to know, refer. When we cannot truly understand the nature of an illness, refer. But otherwise, learn.
References
American Psychiatric Association. (2022). Obsessive-compulsive and related disorders. Diagnostic and statistical manual of mental disorders, 5-TR ed.
Diagnostic and statistical manual of mental disorders, 5-TR ed.
Boedhoe, P. S. W., Schmaal, L., Abe, Y., Alonso, P., Ameis, S. H., Anticevic, A., Arnold, P.D., Batistuzzo, M. C., Benedetti, F., Beucke, J. C., Bollettini, I., Bose, A., Brem, S., Calvo, A., Calvo, R., Cheng, Y., Cho, K. I. K., Ciullo, V., Dallaspezia, S., …Kathmann, N. (2018). Cortical abnormalities associated with pediatric and adult obsessive-compulsive disorder: Findings from the ENIGMA obsessive-compulsive disorder working group. American Journal of Psychiatry, 175(5), 453-462. https://doi.org/10.1176/appi.ajp.2017.17050485
Dieter, E., Speck, O., König, A., Berger, M., Hennig, J., & Hohagen, F. (1997). 1H-magnetic resonance spectroscopy in obsessive-compulsive disorder: Evidence for neuronal loss in the cingulate gyrus and the right striatum. Psychiatry Research: Neuroimaging, 74(3), 173-176. https://doi.org/10.1016/S0925-4927(97)00016-4
Glazier, K., Calixte, R. M., & Rothschild, R.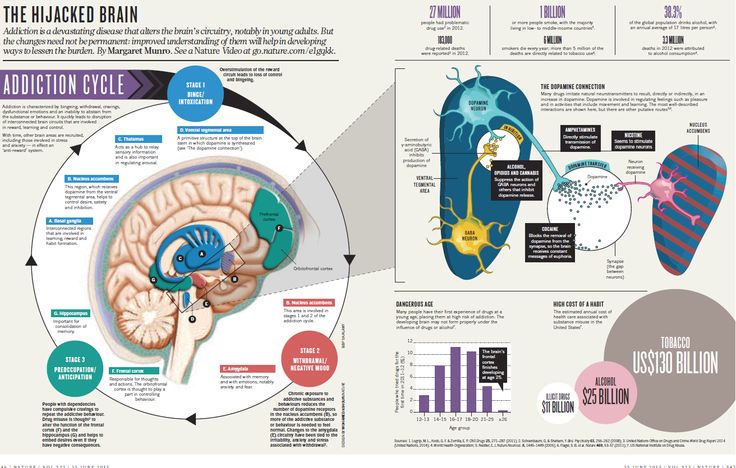 (2013). High rates of OCD symptom misidentification by mental health professionals. Annals of Clinical Psychiatry, 25(3), 201–209.
(2013). High rates of OCD symptom misidentification by mental health professionals. Annals of Clinical Psychiatry, 25(3), 201–209.
Leung, J. G., & Palmer, B. A. (2016). Psychosis or obsessions? Clozapine associated with worsening obsessive-compulsive symptoms. Case Reports Psychiatry, 1–5. https://doi.org/10.1155/2016/2180748.
McCarty, R. J., Guzick, A. G., Swan, L. K., & McNamara, J. P. H. (2017). Stigma and recognition of different types of symptoms in OCD. Journal of Obsessive-Compulsive and Related Disorders, 12, 64-70. https://doi.org/10.1016/j.jocrd.2016.12.006
Ocduk.org. (2020). World Health Organisation and OCD. https://www.ocduk.org/ocd/world-health-organisation/
Radomsky, A. S., Alcolado, G. M., Abramowitz, J. S., Alonso, P., Belloch, A., Bouvard, M., Clark, D. A., Coles, M. E., Doron, G., Fernández-Álvarez, H., Garcia-Soriano, G., Ghisi, M., Gomez, B., Inozu, M., Moulding, R., Shams, G., Sica, C., Simos, G., & Wong, W.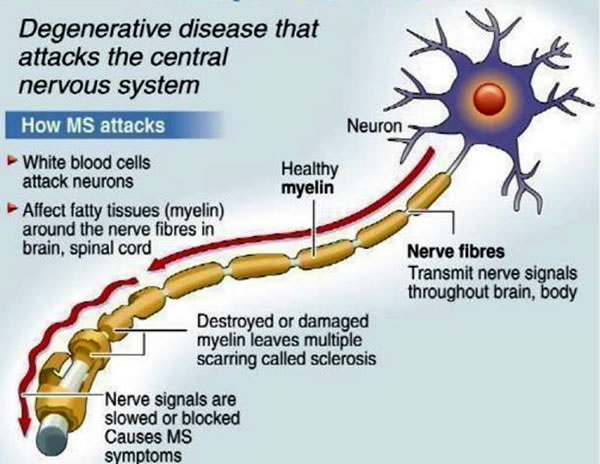 (2014). Part 1—You can run but you can’t hide: Intrusive thoughts on six continents. Journal of Obsessive-Compulsive and Related Disorders, 3(3), 269-279. https://doi.org/10.1016/j.jocrd.2013.09.002
(2014). Part 1—You can run but you can’t hide: Intrusive thoughts on six continents. Journal of Obsessive-Compulsive and Related Disorders, 3(3), 269-279. https://doi.org/10.1016/j.jocrd.2013.09.002
Rohanachandra, Y. M., Vipulanandan, S. (2019). A case of an unusual presentation of obsessive-compulsive disorder in an adolescent. Asian Journal of Psychiatry, 43, 34–36. https://doi.org/10.1016/j.ajp.2019.05.008
Brittany Stahnke, DSW, LCSW, LMFT, is an assistant professor at Newman University, where she teaches and conducts research on mental health, marriage, and suicide. She holds doctorate and master’s degrees in social work. Dr. Stahnke is the author of The Doubting Disease.
Why it Happens and What to Do
OCD — also known as the “doubting disorder” — can make you question things that you were sure of just 5 minutes ago.
Obsessive-compulsive disorder (OCD) is a mental health condition where you experience obsessive often uncontrollable anxious thoughts with frequent compulsions in response to those thoughts.
If you have OCD, you may find yourself fixated on a single thing, like making sure the dishes are clean. Even after confirming the dishes have been washed, you might start to doubt your memory of having checked the dishes or doubt that you washed them properly. You might go back out and rewash the dishes — just to be sure.
“OCD is also known as the ‘doubting disorder,’” says Dr. Holly Schiff, a licensed clinical psychologist based in Connecticut.
“One of the driving forces of compulsions in OCD is chronic doubt. Your brain tricks you into thinking that something has been overlooked, and this fear drives the individual into repeating the action again,” Schiff explains. “Doubt is a hallmark of the disorder, and it overrides any sense of logic or intelligence an individual might have.”
At the core of OCD is doubt of your own memory. Trying to remember if something happened or if you did something correctly can quickly become an obsession. This level of obsession can interfere with your life and quickly consume your focus.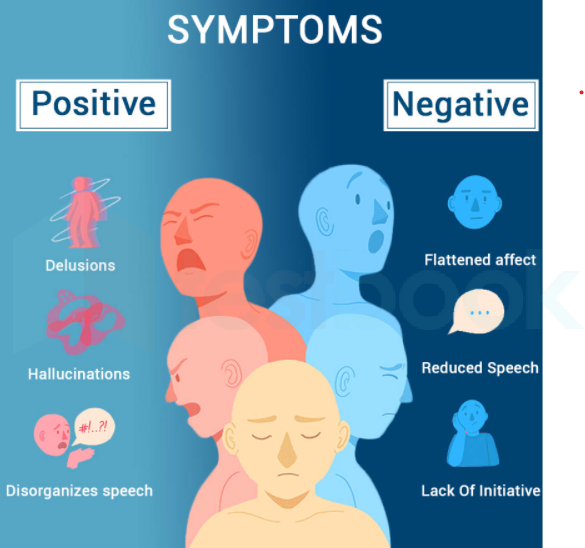
“Memory is a tricky thing,” explains Dr. Amy Marschall, a licensed psychologist.
“With OCD, the person has more doubt and uncertainty about their memory than is typical or helpful, and they have a fear of what will happen if they are misremembering,” she says.
This leads to the compulsive element of OCD, where you feel compelled to verify and double-check something as a way to relieve stress and anxiety temporarily.
The doubt that comes with OCD can really start to influence your home and work lives over time, too.
For example, if you’re trying to get a work task done but are obsessively thinking about your safety and doubting if you locked the front door, you might stop working while you think through all the possible negative consequences of leaving the door unlocked.
You might lose more work time as you act on the compulsion, leave your computer, and check on the door.
If you think you may be experiencing symptoms of OCD, you may benefit from talking with a mental health professional who specializes in OCD and other related disorders. They can help set up an effective treatment plan.
They can help set up an effective treatment plan.
Talk with a therapist
After talking with a mental health professional about your experiences, they can provide a professional diagnosis and set up treatment options for you.
“OCD can be diagnosed by a mental health professional through a thorough diagnostic interview where you answer questions about your history and symptoms,” explains Marschall.
It is also important to talk with a professional because OCD symptoms can be shared with other disorders, meaning that while your symptoms may present as OCD, they may be stemming from a different or comorbid disorder.
“OCD can be present if someone also has another disorder, such as anxiety or depression, and it can be present in individuals with neurodevelopmental differences such as ADHD and autism,” says Marschall.
Therapy options
There are several ways that a therapist can help you manage your OCD symptoms. One of the most commonly used methods of OCD therapy is cognitive behavior therapy (CBT). This therapy aims to address and help you rethink negative behaviors so that they have less control of your life.
This therapy aims to address and help you rethink negative behaviors so that they have less control of your life.
One of the most successful methods of CBT is exposure and response prevention (ERP). A 2019 review concluded that ERP is one of the most effective treatment options for OCD.
“[With ERP], you create a stimulus that triggers the desire to engage in the compulsive behavior but prevents the client from doing the compulsion,” explains Marschall. “This reduces the stress and anxiety by showing the brain that the compulsion is not needed.”
While CBT can’t fully cure OCD, it can make the symptoms of OCD more manageable.
“People with OCD can also benefit from traditional talk therapy from orientations other than cognitive behavioral therapy,” says Marschall. “There are medication options for OCD as well.”
Support groups
Therapy costs can often be out of reach for some people, which means you may need to consider lower-cost alternatives. One of the best alternatives to therapy, when you are on a tight budget, is to attend a support group.
While it isn’t a substitute for one-on-one therapy, you can find a lot of comfort in hearing other people’s stories and sharing your own.
In addition, the more you can connect with people also dealing with OCD, the less likely you will feel alone in facing its challenges.
The International OCD Foundation provides a list of support groups that you can filter to find meetings closest to you. Also, there are options to attend meetings online.
According to the National Institute of Mental Health, the causes of OCD are unknown, but common risk factors are genetics, brain structure, brain function, and the presence of childhood trauma.
In other words, the factors that put you at risk for OCD are all things outside your control today.
OCD is a very real disorder and can’t be easily “fixed” by talking yourself out of it or deciding to stop doubting yourself.
It is important to remember that OCD is a complex mental health disorder and shouldn’t be ignored if it begins to take hours away from your day. Know that you don’t have to struggle with OCD alone, and there is help available if you choose it.
Know that you don’t have to struggle with OCD alone, and there is help available if you choose it.
Ischemic heart disease (CHD) - symptoms, diagnosis, treatment - Axis Medical Center (Zelenograd)
General information about coronary artery disease
Types and forms of IHD
Symptoms of coronary artery disease
IHD diagnostics
Causes of IBS
IHD treatment
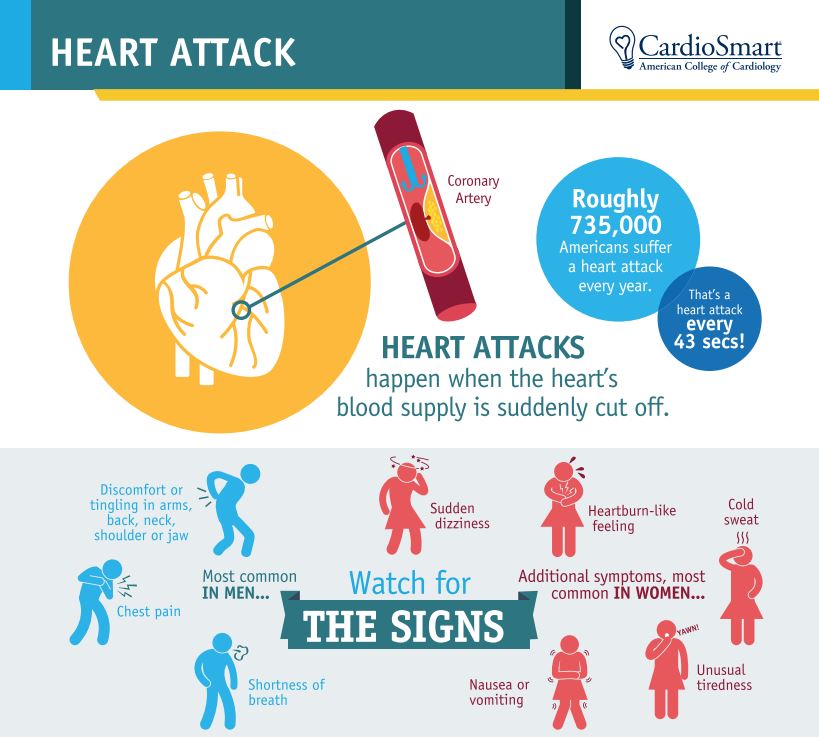
Ischemic heart disease is a worldwide problem. The disease is constantly getting younger, becoming more common. The relevance is that pathology can overtake everyone. It is one of the leading causes of death in developed countries. In Russia, more than 10 million people suffer from ischemia. In men, coronary artery disease occurs 4-5 times more often than in women. After 70 years, the indicators level off.
General
Coronary artery disease (CHD) is a disease in which the myocardium does not receive sufficient blood supply due to damage to the coronary arteries (vessels that feed the heart and deliver oxygenated blood to it). Figuratively speaking, the “motor” does not receive enough “fuel”, it lacks oxygen and nutrients.
Figuratively speaking, the “motor” does not receive enough “fuel”, it lacks oxygen and nutrients.
The heart muscle performs a colossal job throughout life, pumping blood throughout the body. Oxygen and nutrients are supplied with blood to organs and tissues. The heart itself needs it. Oxygen enters with blood through two coronary arteries. Deficiency immediately causes disturbances in the functioning of the heart, which means that the whole body suffers.
Types and forms of IHD
The ICD10 disease code is 120-125.
Clinical types of IHD:
- Sudden coronary death (primary cardiac arrest) - with successful resuscitation or death.
- Angina pectoris - there are angina pectoris, stable, unstable (vasospastic) and spontaneous.
- Painless (silent) form.
- Myocardial infarction: small or large focal (severe consequence of acute coronary syndrome).
- Postinfarction cardiosclerosis.

- Heart failure.
- Arrhythmic form - manifested by atrial fibrillation (atrial fibrillation). May be paroxysmal. The arrhythmic form itself refers to atypical angina pectoris.
According to the nature of the course of IHD, there can be two types:
- Acute - acute coronary syndrome - a sudden decrease in blood flow to the myocardium.
- Chronic - manifested by angina pectoris, chronic heart failure, arrhythmias.
IHD stages:
- Predisease — accumulation of risk factors and narrowing of the coronary artery less than 50%;
- Short-term ischemia - no more than 15-20 minutes;
- Dystrophic-necrotic - angina attacks last for 40 minutes;
- Sclerotic - foci of fibrosis.
IHD symptoms
“If you are experiencing similar symptoms, we advise you to make an appointment with a doctor. You can also sign up by phone: +7 (499) 214-00-00
You can also sign up by phone: +7 (499) 214-00-00
In the early stages, the disease does not particularly manifest itself. Occasionally there are attacks of shortness of breath, changes in the heartbeat, a feeling of fading in the heart. A person associates this with overwork, not paying attention. Moreover, after the rest everything goes away. Pathology can be detected during preventive examinations by a cardiologist and therapist.
The first signs of the development of ischemia of the heart include the following manifestations:
- dyspnea on exertion;
- rise or pressure surges;
- Pressing sensation behind the sternum.
After 35 years, coronary artery disease leads in men, but the prognosis in women is worse - they often die after the first heart attack or within a year after it. After 50 years, the incidence rate in men becomes 2 times higher, in people over 60 the rates level off.
As the disease progresses, angina or chest pain becomes the most common symptom. Other manifestations are also characteristic:
Other manifestations are also characteristic:
- feeling of pressure behind the breastbone;
- chest heaviness;
- burning and constriction in the region of the heart;
- pain;
- shortness of breath;
- heartbeat, which may be irregular, with missed beats;
- tachycardia;
- sweating;
- nausea;
- weakness and dizziness.
Angina pectoris can radiate to the left arm, lower jaw, epigastrium, under the scapula. Most often, angina attacks occur in the morning.
IHD diagnostics
Diagnosis begins with the collection of anamnesis and examination. Further, instrumental research methods are connected:
- ECG - at rest and under load. It can be removed for a day or more (Holter ECG monitoring). It will help to assess the contractility of the myocardium and the permeability of nerve signals.
 With an ECG, a chimes test (intravenously administered) can also be performed to detect coronary insufficiency, especially when an exercise test is not possible.
With an ECG, a chimes test (intravenously administered) can also be performed to detect coronary insufficiency, especially when an exercise test is not possible. - Stress Test or Bicycle Ergometry (BEM) - Cardiac function changes when using a stationary bike. So it is possible to reveal latent coronary insufficiency and exercise tolerance. Evaluation criteria: positive, negative (85%), doubtful.
- EchoCG - ultrasound of the heart, determines the size of the heart, the nature of blood flow, myocardial contractility, will reveal such complications of acute infarction as the formation of parietal blood clots in the heart cavities, the appearance of a heart aneurysm, ruptures of the interventricular septum or separation of the papillary muscles.
- Coronary angiography (CAG) is an invasive method, the most accurate and informative today. It is considered the "gold standard" for diagnosing coronary artery disease. A contrast agent is injected into the patient's blood and an x-ray is taken.
 It is CAG that makes it possible to resolve the issue of treatment tactics, including surgery.
It is CAG that makes it possible to resolve the issue of treatment tactics, including surgery. - Laboratory tests: blood tests.
- Differential diagnosis of angina pectoris is also needed to distinguish coronary artery disease from other pathologies of the heart (PE, pericarditis, etc.).
Causes of IHD
The main reason for impaired blood supply to the heart is the difficulty in the movement of blood flow through the coronary arteries due to their damage by atherosclerosis (in 95–97% of cases, IHD is associated with the formation of cholesterol plaques on the walls of blood vessels). At stage 3 atherosclerosis, blockage of the vessel can cause death.
Increased blood viscosity contributes to slowing down blood flow with a tendency to develop and form blood clots.
Risk factors can be divided into: controlled (modifiable), that is, removable, and uncontrolled (non-modifiable), which cannot be influenced, but it is important to take into account in the treatment and prevention.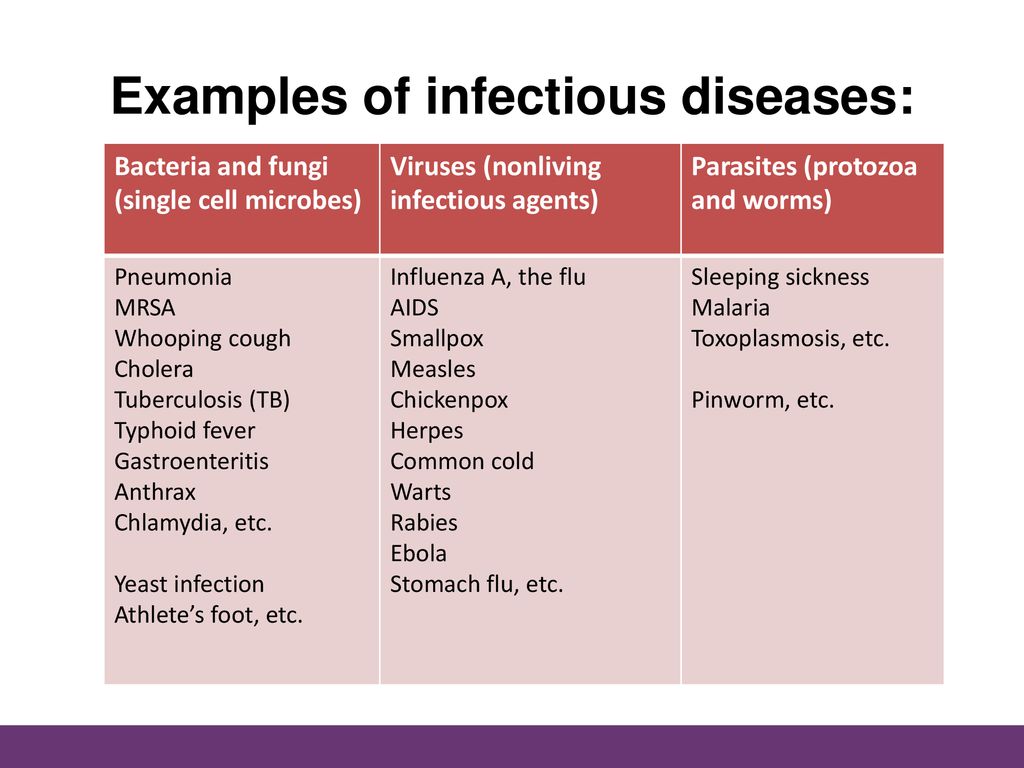
Controlled factors:
- bad habits - smoking and alcohol abuse;
- hypodynamia - a sedentary lifestyle;
- malnutrition with a predominance of animal fats and refined products;
- stresses;
- arterial hypertension;
- obesity;
- diabetes mellitus;
- hyperlipidemia.
Uncontrollable factors:
- age — after 50-60 years the risk of coronary artery disease increases markedly;
- gender - men are more susceptible to disease;
- genetics - detection of coronary artery disease in close relatives, while there is a predisposition to coronary disease itself, disorders of cholesterol metabolism, increased thrombosis.
Uncontrollable factors are the main causes.
IHD treatment
The principles of IHD therapy are the elimination of risk factors and an integrated approach. The elderly require hospital treatment. In most cases, a complete cure is impossible - vascular changes are irreversible, only an improvement in the condition. Treatment regimens are selected by the doctor. In the early stages, treatment is conservative, that is, medication.
The elderly require hospital treatment. In most cases, a complete cure is impossible - vascular changes are irreversible, only an improvement in the condition. Treatment regimens are selected by the doctor. In the early stages, treatment is conservative, that is, medication.
Protocols of treatment standards provide for the appointment of the following drugs:
- Anticoagulants and antiaggregants - drugs prevent the formation of blood clots, thin the blood, it becomes easier for the heart to pump it.
- Beta-blockers - block beta receptors, reducing blood pressure and slowing down the pulse. The purpose of these funds is to reduce myocardial oxygen demand due to slower pumping of blood.
- Statins - to reduce "bad" cholesterol in the blood.
Non-drug recommendations include exercise therapy (during the rehabilitation period).
When CAD is diagnosed, treatment may include modern antiarrhythmic drugs and diuretics.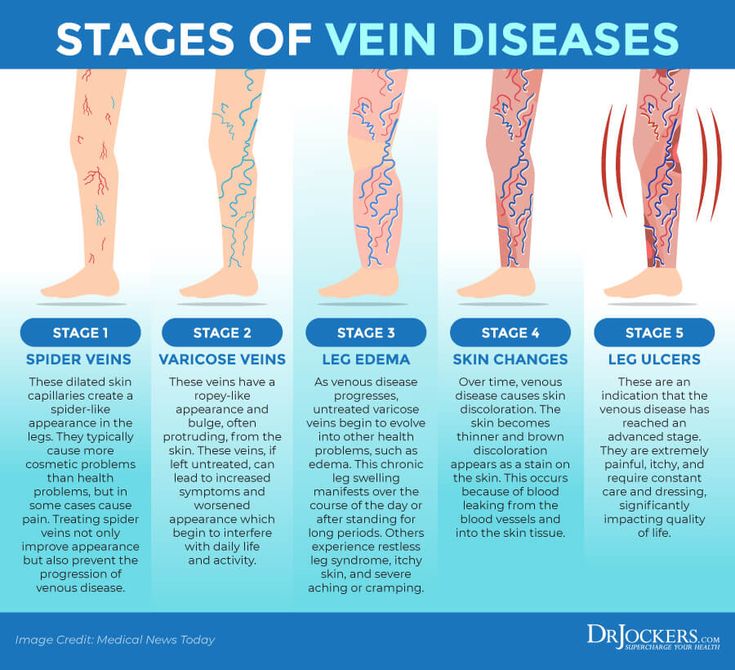
With the ineffectiveness of drug treatment and damage to the coronary vessels, surgical intervention is indicated. It consists in angioplasty of the vessel with its subsequent stenting.
Prevention of coronary artery disease - maintaining a healthy lifestyle, controlling cholesterol and pressure.
Benefits of contacting Axis Medical Center
The Axis Medical Center in Zelenograd employs experienced and highly qualified specialists. Among them are doctors of the highest category, candidates and doctors of sciences.
The center offers treatment for such a formidable disease as coronary artery disease, according to modern medical protocols. Patients receive the help of qualified cardiologists with great experience, who diagnose the pathology in the shortest possible time and select an individual treatment. You can contact the clinic at any time convenient for you. The center has the latest generation equipment for high-quality and safe diagnostics.
a selection of dubious diagnoses worth consulting with another doctor
Daniil Davydov
medical journalist
Author profile
You can get a non-existent diagnosis and inadequate treatment not only in our country, but also abroad. It is difficult to calculate how often this happens, and there are many reasons why such diagnoses appear.
Adepts of alternative medicine invent some non-existent diseases in order to sell their services — sometimes such diagnoses are also called commercial ones. Other "diagnoses" are actually a variant of the norm, and still others are a kind of "garbage dump" for symptoms that doctors do not have time to deal with.
In this article, we have collected 9 dubious diagnoses and tried to explain what is wrong with them.
What is Alternative Medicine - NHS England
The Dangers of Alternative Medicine - American Cancer Society
If you or someone close to you has been diagnosed with one of our lists, it makes sense to get a second opinion from another doctor. This will help you understand what problems the symptoms are actually associated with and get the most effective treatment.
This will help you understand what problems the symptoms are actually associated with and get the most effective treatment.
Hypoadrenia, or adrenal fatigue
What is it. Commercial diagnosis from the field of alternative medicine. According to chiropractor James Wilson, who invented the disease in 1998, hypoadrenia is caused by physical and psychological stress that supposedly disrupts the adrenal glands. As a result, they stop creating hormones necessary for a normal response to stress, and a person’s health deteriorates and well-being is disturbed.
What is Adrenal Fatigue - American Endocrinological Society
In order to get the adrenal glands working again, patients are advised to adopt a healthy lifestyle and prescribe dietary supplements with bovine and porcine adrenal extract. For example, dietary supplement "Suprenamin", which is supposed to be taken 2-3 times a day for 10-14 days. Moreover, the course will have to be repeated every 3-6 months. One pack of this supplement costs $870.
One pack of this supplement costs $870.
Which doctor makes the diagnosis. Professionals who position themselves as experts in alternative medicine. These are not only chiropractors - some endocrinologists, immunologists and therapists can make such a diagnosis.
/list/endocrinologia/
10 important questions for endocrinologist Yuri Poteshkin
Who is being diagnosed. People who complain of fatigue, trouble sleeping, low mood, need for stimulants such as large amounts of coffee, and a very strong desire to eat sugary foods or fast food.
What is wrong with the diagnosis. All real diseases have two components:
Nursing Diagnostic Manual - An online textbook for nurses
- Root cause - that is, an infection or other factor that damages a specific internal organ or disrupts the interaction of several organs.
- Signs of disorders that result from these injuries.
Even if the disease proceeds without symptoms, that is, without health problems that the patient himself can notice - such as atherosclerosis in the early stages, a real disease should still have signs that can be detected with the help of tests and examinations.
So, dopplerography, that is, an ultrasound examination of blood vessels, and a set of biochemical analyzes called a lipid profile help to detect atherosclerosis.
/biochemical-analysis/
What does a biochemical blood test show?
But adrenal fatigue does not meet any of the criteria for real illness.
First, there is no conclusive evidence that chronic stress is the root cause of adrenal dysfunction. Many modern people suffer from it, but most of them do not show any signs of adrenal dysfunction.
However, a disease in which the adrenal glands secrete too little cortisol does exist and is called "adrenal insufficiency." But stress does not lead to this disease at all.
Primary adrenal insufficiency develops due to damage to the adrenal cortex, such as an autoimmune disease or hemorrhage, while secondary insufficiency develops due to a malfunction of the pituitary gland, a small gland in the brain that controls the adrenal glands.
Primary Adrenal Insufficiency - Medical Handbook MSD
Secondary Adrenal Insufficiency - MSD
Second, signs of adrenal fatigue cannot be detected by tests and examinations. This diagnosis is made simply on the basis of a questionnaire that the doctor gives to the patient. The person must answer whether he has right now or had in the past, for example, constant stress in his personal life or at work, and whether it was difficult for him to get up in the morning.
James Wilson's Adrenal InventoryPDF, 24KB
Adrenal Fatigue Doesn't Exist: A Systematic Review - Endocrine Disorders
Controversial Theories in Allergology and Immunology - Proceedings of Allergy and Asthma Journal
After all, every person has faced similar problems at least once in their life. If you fill out this questionnaire honestly, then "adrenal fatigue" can be diagnosed in anyone.
If you fill out this questionnaire honestly, then "adrenal fatigue" can be diagnosed in anyone.
All this makes us suspect that the diagnosis was invented solely in order to sell bioadditives, the safety and effectiveness of which no one has tested.
What to do next. Hypoadrenia can also be "diagnosed" in a completely healthy person who is just tired. Therefore, it makes sense to rest and wait two weeks. If everything goes away on its own, you don't need to do anything.
But if weakness, sleep problems and bad mood persist for more than two weeks, a psychotherapist or clinical psychologist should be consulted - similar symptoms occur, for example, with depression.
Community 11/23/21
What is depression?
And if these symptoms are accompanied by problems with appetite, headaches, muscle pain and other unpleasant sensations in the body, it makes sense to start with a visit to a therapist. The doctor will help you figure out what the problem is - after all, such symptoms can indicate a variety of problems: from overtraining to, for example, post-covid syndrome.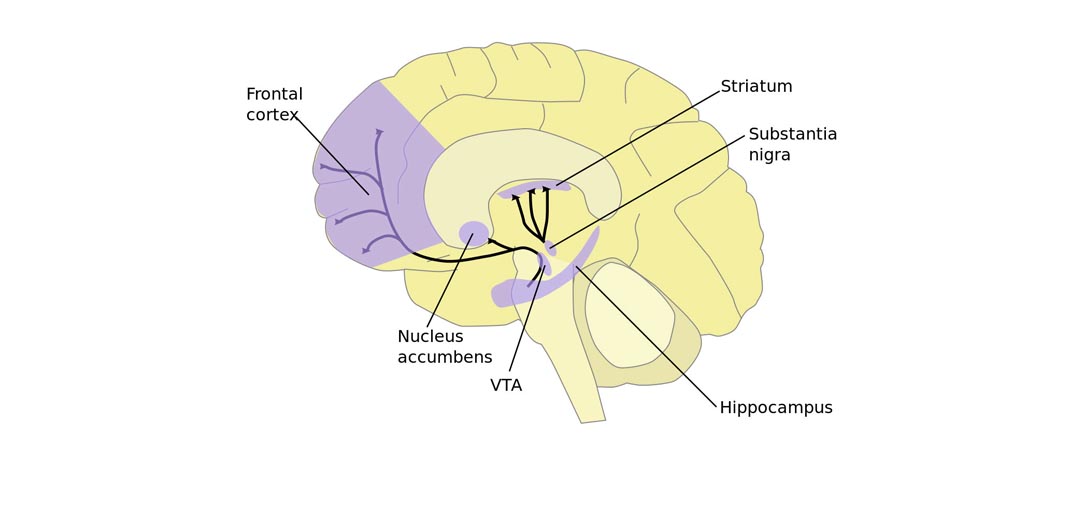
What is rehabilitation after coronavirus disease and who needs it
Dyscirculatory encephalopathy
What is it. This is not a diagnosis, but a term from Soviet medicine that combines any problems associated with impaired blood circulation in the brain. There can be many reasons for impaired blood supply to the brain: from hypertension and stroke to damage to the brain vessels during radiation therapy.
60 years of the concept of dyscirculatory encephalopathy - is it possible to pour new wine into old wineskins? - Journal of Neurology and Psychiatry
What is Encephalopathy - RxList Pharmaceutical Directory
In the International Classification of Diseases 10 and 11 revisions of the diagnosis "dyscirculatory encephalopathy" are not available. But in different groups of diseases in ICD-11 there is another, even more general term - encephalopathy. This term is used when they want to describe any disease, damage or disturbance in the brain associated with any cause - from head injuries to liver disease.
Which doctor makes the diagnosis. Russian neurologists.
Who is being diagnosed. Since the term "dyscirculatory encephalopathy" covers a very large number of pathologies, a variety of people fall under the criteria: from patients with moderate cognitive impairment - when a person complains of problems with memory and that recently it has become, for example, more difficult for him to count in mind, to people with dementia, walking disorders and pseudobulbar syndrome - when, due to problems with the nerves of the muscles of the pharynx, a person cannot swallow and speak normally.
What is wrong with the diagnosis. The criteria for this term are too broad. If a neurologist uses it as a diagnosis, then this says little about what is really happening with a person. Because of this, it is also impossible to choose the right treatment - after all, it is obvious that a forgetful, but otherwise healthy person needs to be treated differently than a person who cannot swallow.
What is the problem with dyscirculatory encephalopathy - a reference book by neurologist Nikita Zhukov Encyclopatia
In addition, people who receive such a diagnosis are often prescribed drugs that do not have convincing evidence of effectiveness - antioxidants, neuroprotectors or nootropics.
Nootropics: do they really improve brain function
What to do next. Get a second opinion from another neurologist who can clarify the diagnosis and prescribe the right treatment.
Mental retardation
What is it. Psychological and pedagogical concept, which was invented by employees of the Soviet Research Institute of Defectology in the 60s of the last century.
Mental retardation: issues of differentiation and diagnosis — journal "Psychology and Pedagogical Practice"
Theoretical and applied model of psychological assistance to children with mental retardation — the journal "Higher Education in Russia"
coping with the curriculum. They proposed to call these first-graders children with mental retardation, or mental retardation, and developed a correctional program for them, which helped them catch up with their peers in studies.
Over time, mental retardation penetrated into child psychology and turned into a psychological diagnosis, which began to be made, including preschoolers - that is, children aged 5-6 years. Nowhere, except for the countries of the former USSR, this diagnosis is used, it is not in ICD-10 and ICD-11.
Instead, ICD-11 has a separate group of conditions called Developmental Learning Disorder. And within this group there are many smaller and specialized subgroups: there are learning disorders associated with impaired reading, writing, and mathematical abilities. With the help of such a division, it is easier to figure out what problem the child is facing and help him.
Which doctor makes the diagnosis. Child psychologist or psychiatrist.
Who is being diagnosed. There are no clear criteria for ZPR. As a rule, the diagnosis is made according to the parents. For example, if they complain that the child began to walk, talk or draw later than their peers - or seems too forgetful, absent-minded or impulsive.
/list/charlatan-doctors/
How to tell a doctor from a charlatan on Instagram without wasting your money
This means that both completely healthy children with whom they simply do not have enough training, and children with speech and language developmental disorders, autism, ADHD and other features of the development of the nervous system can fall into the group of mental retardation.
What is wrong with the diagnosis. ZPR, in principle, cannot be considered a medical diagnosis. According to the definition, this is a developmental anomaly, which is most often detected at the initial stages of education and manifests itself in the difficulties of assimilating knowledge, skills and abilities, adapting to educational requirements.
However, in fact, different children face different problems during learning, so it is wrong to combine them into one group. The condition of each child must be dealt with separately and a suitable program of adaptation and study should be selected for him.
/list/pediatr-deti/
11 important questions to pediatrician Sergei Butriy
What to do next. Get a second opinion from another child psychologist or psychiatrist. Without this, it will not be possible to figure out what is really happening with the child and how to help him.
Non-existent gynecological STIs
What is it. Diagnoses that are made as real - based on bacterial culture or PCR analysis of biomaterial from the vagina or cervix.
If the following bacteria are found in the biomaterial:
- Mycoplasma hominis — mycoplasmosis is diagnosed;
- Ureaplasma urealyticum or Ureaplasma parvum - diagnose ureaplasmosis;
- Gardnerella vaginalis - diagnose gardnerellosis.
/pcr-test/
How much does a PCR test cost?
Patients with these diagnoses are usually prescribed antibiotics. If after a course of antibiotics these bacteria reappear in the tests, antibiotics are prescribed again.
Which doctor makes the diagnosis. Most often a gynecologist, sometimes a urologist.
Who is being diagnosed. Women who submitted a biomaterial for analysis in the direction of a gynecologist. They may not have any unpleasant symptoms at all, or they complain of itching or burning in the vagina, pain during sex, note the appearance of whitish-gray vaginal discharge with an unpleasant odor.
What is wrong with the diagnosis. There are no diagnoses of "gardnerellosis" and "ureaplasmosis" in either international or Russian clinical guidelines. They also do not have a diagnosis of mycoplasmosis. However, in practice, this is sometimes called an STI, which is caused by another type of mycoplasma - Mycoplasma genitalium.
Urogenital diseases caused by Mycoplasma genitalium — Russian clinical guidelines
Overview of the composition of the vaginal microbiota — Journal of Nutrients
Antibiotics destroy the intestinal microflora - "Advanced research in cellular and infectious microbiology"
In contrast to the pathogens of STIs, which in principle should not be in healthy people, gardnerella, both types of ureaplasmas and Mycoplasma hominis can occur in the vagina in completely healthy women . Most gynecologists and microbiologists consider these bacteria to be components of the normal microflora of the vagina.
The International Society for the Fight against STIs does not recommend testing for these bacteria and getting rid of them with antibiotics, as this will not bring health benefits. But it can cause real harm, because antibiotics have side effects. For example, they destroy the beneficial intestinal microflora, and this causes diarrhea. And some drugs can provoke allergies.
What to do next. Consult another gynecologist.
/guide/antibiotics/
Antibiotics: what are the differences and how to take them
Normally, there should be neither unpleasant sensations in the vagina nor thick discharge with an unpleasant odor. But it will not work to figure out what the problem really is, since there are quite a lot of diseases and conditions with similar symptoms.
For example, a thick, foul-smelling vaginal discharge can occur with bacterial vaginosis, a condition in which the healthy balance of bacteria in the vaginal mucosa is disturbed. Normally, lactobacilli live there, which keep all other bacteria under control.
What is bacterial vaginosis - an international reference book for doctors UpToDate
selection. To restore a healthy ratio of bacteria in the vagina, you need a doctor to prescribe the right treatment.
Sand in kidneys
What is it. The "folk" name for small kidney stones, the size of which does not exceed 3-5 mm in diameter.
Which kidney stones are considered small - Cleveland Clinic
Which doctor diagnoses. Ultrasound doctor or radiologist.
When the diagnosis is made. Based on the results of an ultrasound, x-ray or CT examination of the pelvic organs.
What is wrong with the diagnosis. Stones form in the kidneys and leave them through the ureter. When the stone comes out, the person experiences excruciating pain - renal colic. And if it gets stuck, urine will stop coming out of the kidney, and as a result, a person may develop severe inflammation - pyelonephritis.
How I had a stone removed from my kidney according to OMS
Stones form in the kidney, but leave them through the ureter The diameter of the ureter is 6-8 mm. As a rule, stones up to 5 mm in diameter leave the kidneys completely painlessly, so that a person often does not even know about it. If a person does not have unpleasant symptoms, he does not need treatment. But so that the sand does not turn into stones, it is recommended to follow the drinking regime and revise the diet: reduce the amount of sweet, meat and salt.
What to do next. As a rule, an ultrasound diagnostician does not write "sand in the kidneys" in the conclusion, but reports it in words. In this situation, it makes sense to clarify the size of the stones. If the diameter is less than 3 mm, there is no cause for serious concern - to avoid the growth of stones, it is enough to limit yourself to changes in diet. And if the size of the stones approaches 5 mm, it makes sense to consult a nephrologist. He will tell you if you need to change the diet, or if there is no threat, so you can continue to live a normal life.
Subluxation of the cervical vertebrae
What is it. From the point of view of classical medicine, subluxation of the cervical vertebra is a situation when, due to a neck injury, which happened, for example, as a result of a car accident, the ligaments in the back of the neck are partially torn. At the same time, the upper cervical vertebra, which they held, is displaced relative to the cervical vertebra, which lies below it.
The meaning of the term "anterior subluxation of the cervical vertebra" in traumatology - Medscape 9 medical reference book0003
Meaning of the term "subluxation" in chiropractic and osteopathic publications - Journal of Human Chiropractic
It is very painful, and the victim needs a long rehabilitation. And in some cases, to prevent further displacement of the vertebrae, a complex surgical operation is needed.
The red arrow shows the true subluxation of the vertebrae, and the red line shows the degree of displacement relative to the anatomically accurate position. Source: researchgate.net In alternative medicine, subluxation is a slight displacement of a cervical vertebra. A person can be born with it, or it occurs during life due to the gradual wear of the intervertebral discs. If the displacement of the cervical vertebrae does not exceed 50% and does not interfere with turning the head, it is not necessary to correct it.
However, advocates of alternative approaches believe that harmless misalignment of the cervical vertebrae causes a variety of health problems, from headaches to infertility. As a treatment measure, they offer procedures during which a vertebra that has moved out needs to be “put in place”.
/spondylolisthesis/
Is it true that the displacement of the cervical vertebrae is very dangerous?
Which doctor makes the diagnosis. Non-existent subluxation of the cervical vertebrae is a diagnosis made by chiropractors, osteopaths, sometimes chiropractors. Real subluxation of the cervical vertebrae is a diagnosis made by traumatologists, neurologists and radiologists.
When the diagnosis is made. If a person comes to an alternative doctor with complaints of headache, back or neck pain.
What is wrong with the diagnosis. In most cases, headache, pain in the neck and back do not develop at all due to displacement of the cervical vertebrae, but due to physical activity, sudden incorrect movements, uncomfortable posture, including in sleep, incorrect lifting of weights - and another 30% of all cases of headache are associated with migraine. It is useless to treat all this by “repositioning” the cervical vertebra.
Side effects of spinal manipulation: a systematic review - Journal of the Royal Society of Medicine
Moreover, the attempt to "reposition" the vertebrae itself can lead to serious injury. Cases are described when manipulations by chiropractors led to dissection of the vertebral artery - in some people this ended in a stroke.
What to do next. It is life-threatening to agree to the "reduction of the cervical vertebra". You should stay away from a doctor who offers such procedures.
/osteochondrosis/
How much does it cost to cure osteochondrosis
If the headache occurs no more than 1-2 times a month, it is enough to take a tablet of a non-steroidal anti-inflammatory drug, such as 400 mg of ibuprofen.
See a neurologist if:
- more than 3-5 times a month;
- unusually strong and painful;
- is accompanied by vision problems, weakness and numbness of the arms and legs.
Back and neck pain often goes away on its own within a week. Until then, you can take a non-steroidal anti-inflammatory drug tablet, such as 400 mg ibuprofen once a day.
If your neck hurts, you can put a warm compress on it, and if your back, a cold compress will do. With acute pain, it makes sense to lie down for a couple of days, but then you need to return to walking and other light activities like going to the store with a light bag. Physical activity will help you recover faster. But you should not forget about sports even after recovery. Regular exercise strengthens the muscles of the back and neck - and this reduces the likelihood that the neck will hurt in the future.
/list/nevrolog-vopros/
9 important questions for neurologist Pavel Brand
If back and neck pain does not go away in a week, consult a neurologist.
Leaky gut syndrome
What is it. Commercial diagnosis from the field of alternative medicine. According to the immunologist Alessio Fasano, who invented this disease in 2003, under the influence of gluten, sugar, dairy products, bacteria and their toxins, certain drugs, parasites and stress, the walls between intestinal cells are gradually destroyed, and intestinal contents enter the blood.
Debunking the Leaky Gut Syndrome Myth - Canadian Gastrointestinal Society
The immune system overreacts to an invasion, damaging healthy cells. According to Fasano, this causes irritable bowel syndrome, allergies, autoimmune diseases like rheumatoid arthritis, chronic fatigue, depression and many other diseases. All these conditions can be treated with dietary supplements that contain probiotics - supplements with beneficial intestinal bacteria from the Lactobacillus and Bifidobacterium groups.
Which doctor makes the diagnosis. Supporters of the concept can be doctors of any specialty, but more often they are gastroenterologists, nutritionists or therapists.
/gluten/
Who should be tested for gluten sensitivity?
When the diagnosis is made. The diagnosis is so universal that it fits almost any complaint. Most often, it is given to people who complain of fatigue, excess weight and skin problems.
What is wrong with the diagnosis. Diseases in which intestinal permeability is impaired do exist. These are, for example, autoimmune diseases like celiac disease and Crohn's disease. But a person without a genetic predisposition cannot get sick with them, no matter what he eats and no matter how he lives.
In what diseases can intestinal permeability be disturbed - Current Opinion in Gastroenterology
The second group of diseases in which intestinal permeability is impaired is intestinal infections. They are indeed caused by parasites, pathogenic viruses and bacteria and parasites.
At the same time, there is no convincing evidence that large molecules from the intestines that enter the bloodstream trigger an immune response that leads to any kind of disease.
In addition, Leaky Gut Syndrome has the same problem as another commercial diagnosis, adrenal fatigue. This diagnosis is also made on the basis of non-specific symptoms that can indicate a host of other diseases. All this suggests that leaky gut syndrome was also invented mainly in order to distribute probiotic supplements.
What to do next. Get a second opinion from another gastroenterologist, nutritionist, or physician.
Frequently ill child
What is it. The concept proposed by the Soviet pediatricians Valery Albitsky and Alexander Baranov in 1986. They considered those who catch colds as frequently ill children:
- under the age of one year - four or more times a year;
- in 1-3 years - six or more times a year;
- in 4-5 years - five or more times a year;
- over 5 years old - four or more times a year.
Once again about the problems of the concept of "frequently ill children" - the journal PediatricsPDF, 150 KB
According to Soviet pediatricians, the health of these children is more fragile than that of their peers, so it makes sense for parents to closely monitor their health and regularly take them to the clinic for examination.
Community 11/14/22
Why does a child often get sick in kindergarten and what to do about it?
Which doctor makes the diagnosis. Pediatrician.
When the diagnosis is made. As a rule, pediatricians classify children in the PIC group without any tests and examinations, simply from the words of the parents.
What is wrong with the diagnosis. It is normal for a child between six months and six years of age to have 6-8 colds per year. The child's immune system is still young and inexperienced. To learn how to defend against colds, the immune system needs to get acquainted with the most common cold viruses and learn from all the vaccinations that children are supposed to do.
As the immune system learns, the child gets sick less and less. Older schoolchildren and adults without chronic diseases, on average, catch a cold only 2-4 times a year.
/vaccination/
How to save on childhood vaccinations without saving on health
How to proceed. If frequent colds are the only problem, and the child is growing and developing normally, there is no point in continuing to examine him again.
Continue testing only if the child has two or more of the following:
- there are people in the child's family with confirmed primary immunodeficiency;
- the child is not gaining weight or cannot grow normally;
- within one year the child had four or more ear infections, or two or more nose infections, or two or more pneumonias, i.e. inflammation of the lungs;
- the child has persistent thrush in the mouth or a fungal infection on the skin;
- the child suffers from deep abscesses, that is, ulcers on the body, which return again and again;
- the child had two or more serious infections, including sepsis, i.e. blood poisoning;
- the child was treated with antibiotics for two months or longer, but this did not help;
- The child has to be given intravenous antibiotics to treat infections.
Electromagnetic hypersensitivity
What is it. A condition in which a person complains of health problems associated with exposure to electromagnetic fields - for example, from wires or household appliances.
Electromagnetic Hypersensitivity: A Critical Review of Explanatory Hypotheses - State of the Environment Journal
Which doctor makes the diagnosis. Such a diagnosis does not exist, patients "make" it themselves. But, having suspected electromagnetic hypersensitivity, people, as a rule, turn to therapists and dermatologists with these problems.
When the diagnosis is made. Symptoms are usually non-specific and variable. They can be associated with the skin - usually redness, tingling and burning, and with general well-being - this is fatigue, problems with concentration, dizziness, nausea, heart palpitations and digestive disorders.
What is wrong with the diagnosis. There is no evidence that electromagnetic radiation, which is generated during the operation of telephones, chargers, irons or any other household appliances, has any effect on people's health.
/magnetic-storm/
Is it true that magnetic storms affect human health?
Although very strong magnetic fields can cause a weak electric current in the human body, which could interfere with the normal functioning of muscles and nerve cells, household magnetic fields are too weak for this.
Even the most powerful magnetic fields that break mobile phones in electrolysis shops do not cause the slightest harm to people working there.
Community 10/12/21
Is it harmful to sleep next to a charging phone?
Of course, it can be assumed that the workers chose such work only because they do not care about electromagnetic fields. However, studies show that if people who complain of hypersensitivity are told that they are now being affected by a magnetic field, they develop symptoms - even if in fact there was not a single switched-on electrical appliance nearby.