Best natural supplements for depression and anxiety
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers. The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.
2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
- Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
- The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.
 4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH) - Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.
 7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month.
 The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people). - Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medications for Substance Use Disorders
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 03/22/2023
Evidence-Based Resources About Opioid Overdose
SAMHSA’s Evidence-Based Practice Resource Center (EBPRC) contains a wide variety of downloadable resources available from SAMHSA and other federal partners about opioid overdose and other substance use and mental health topics to help communities, clinicians, policy-makers and others with the information and tools to incorporate evidence-based practices into their communities or clinical settings.
Fact Sheet:
Using Naloxone to Reverse Opioid Overdose in the Workplace: Information for Employers and Workers | CDC (PDF | 785 KB) - This fact sheet helps employers understand the risk of opioid overdose and provides guidance about establishing a workplace naloxone program.
Tips for Teens: The Truth About Opioids | SAMHSA - This fact sheet for teens provides facts about opioids. It describes short- and long-term effects and lists signs of opioid use. The fact sheet helps to dispel common myths about opioids. Access sources cited in this fact sheet.
Toolkits:
Medication-Assisted Treatment (MAT) for Opioid Use Disorder in Jails and Prisons: A Planning and Implementation Toolkit | National Council of Behavioral Health - Developed by the National Council of Behavioral Health, this guide provides correctional administrators and healthcare providers tools for implementing MAT in correctional settings.
Opioid Overdose Prevention Toolkit | SAMHSA -This toolkit offers strategies to health care providers, communities, and local governments for developing practices and policies to help prevent opioid-related overdoses and deaths. Access reports for community members, prescribers, patients and families, and those recovering from opioid overdose.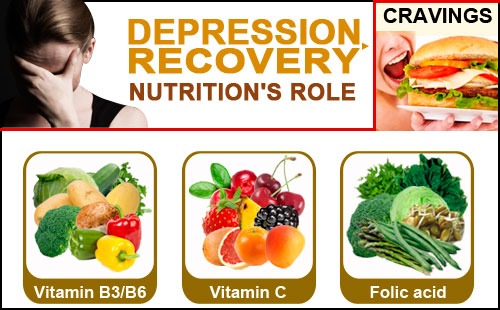
Evidence Reviews/Guidebooks:
Evidence-Based Strategies for Preventing Opioid Overdose: What’s Working in the United States | CDC (PDF | 11.5 MB) - This CDC document reviews evidence-based strategies to reduce overdose. It explains why these strategies work, the research behind them, and examples of organizations that have put these strategies into practice.
Use of Medication-Assisted Treatment in Emergency Departments | SAMHSA - This guide examines emerging and best practices for initiating medication-assisted treatment (MAT) in emergency departments.
Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings | SAMHSA -This guide focuses on using medication-assisted treatment for opioid use disorder in jails and prisons and during the reentry process when justice-involved persons return to the community.
Telehealth for the Treatment of Serious Mental Illness and Substance Use Disorders | SAMHSA - This guide reviews ways that telehealth modalities can be used to provide treatment for serious mental illness and substance use disorders including opioid overdose among adults.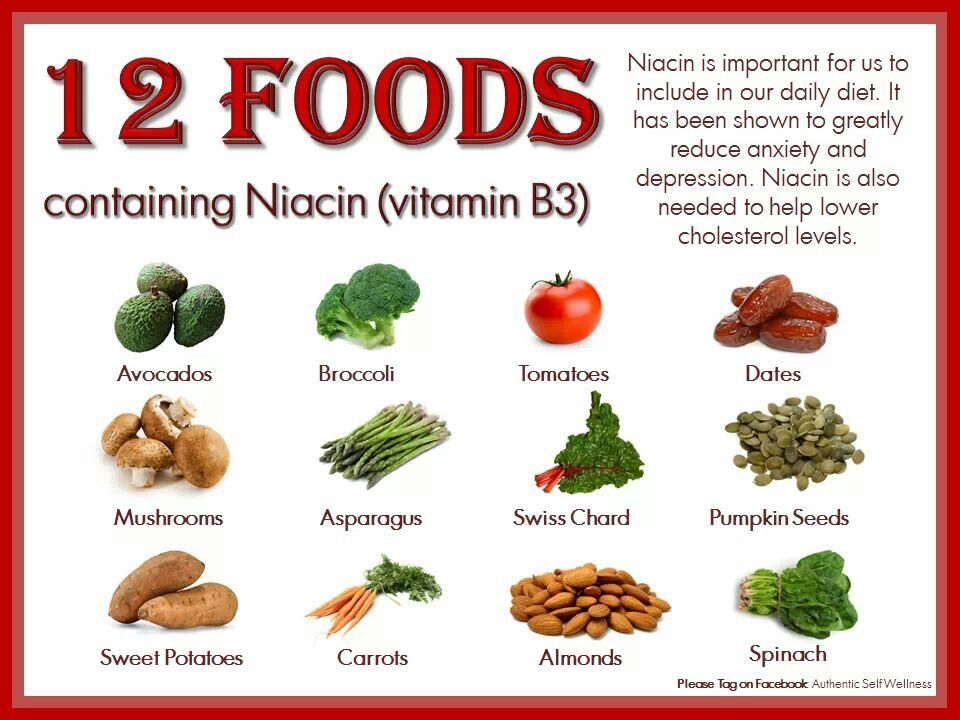
Treatment Improvement Protocols/Manuals:
TIP 63: Medications for Opioid Use Disorder | SAMHSA - This Treatment Improvement Protocol (TIP) reviews the use of the three Food and Drug Administration (FDA)-approved medications used to treat OUD—methadone, naltrexone, and buprenorphine.
Advisory: Opioid Therapy in Patients With Chronic Noncancer Pain Who Are in Recovery From Substance Use Disorders | SAMHSA - This advisory addresses screening and assessment tools, nonpharmacologic and nonopioid treatment for chronic pain, and the role of opioid therapy in people with chronic noncancer pain and SUDs.
Overdose Prevention & Naloxone Manual | HRC - This Harm Reduction Coalition (HRC) manual outlines the process of developing an Overdose Prevention and Education Program that may involve a take-home naloxone component.
Websites:
SAMHSA
- Medication-Assisted Treatment (MAT)
- MAT Medications, Counseling, and Related Conditions
- Opioid Overdose
- Know the Risks of Using Drugs
Other federal websites
- HHS.
 gov/opioids
gov/opioids - Opioids | NIDA
- Drug Overdose | CDC
- Rx Awareness | CDC
Visit the EBPRC for additional information, including Treatment Improvement Protocols, toolkits, resource guides, clinical practice guidelines, and other science-based resources.
Do you experience symptoms of depression more often? Here are five natural approaches to fighting depression
The information in this blog has not been verified by your country's public health authority and is not intended as a diagnosis, treatment, or medical advice. More
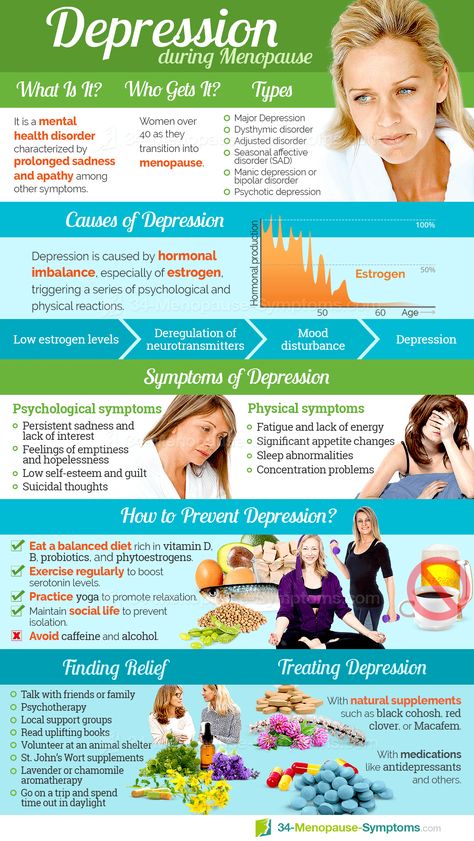
Depression is a mood disorder characterized by long periods of feelings of sadness, loneliness and apathy. Every tenth person in the world experiences symptoms of depression or depressed mood.
Depressive symptoms
Depression has many symptoms, including:
- loss of interest in usual activities;
- sadness;
- changes in appetite;
- feeling of guilt;
- complaints that daily activities take a lot of energy;
- anxiety;
- anxiety;
- trouble going to bed;
- sleep too long;
- irritability;
- outbursts of anger;
- difficulty concentrating or making decisions;
- unexplained (nonphysical) pain.

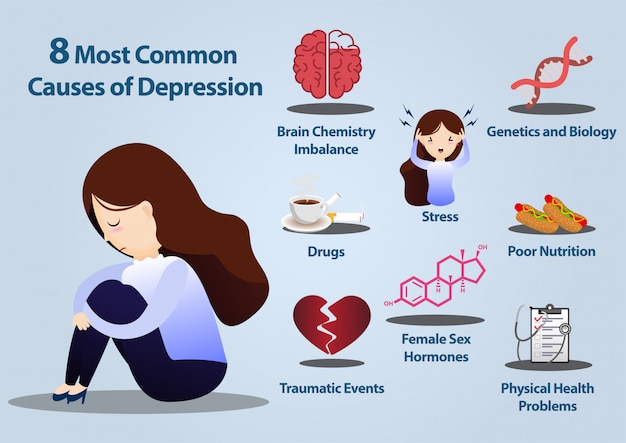
Causes of depression
Many factors can lead to depression. Sometimes symptoms of depression develop due to physical changes in the brain. For example, after a stroke, with prolonged use of alcohol, or after an injury.
Depression can also occur due to hormonal changes - with an increase or decrease in the level of thyroid hormones, sex hormones, glucocorticoids (for example, the stress hormone cortisol) or insulin / glucagon (hormones that control the conversion of sugar into energy).
Life changes can also cause depression. For example, its symptoms often develop after the loss of a loved one, the breakup of a relationship, financial problems, trauma. If your close relative suffers from episodes of depression, you may also have a genetic predisposition to a depressed mood.
Another reason is a chemical imbalance in the body. Brain function is regulated by a careful balance of chemicals known as neurotransmitters. They transmit signals to the brain and the body as a whole.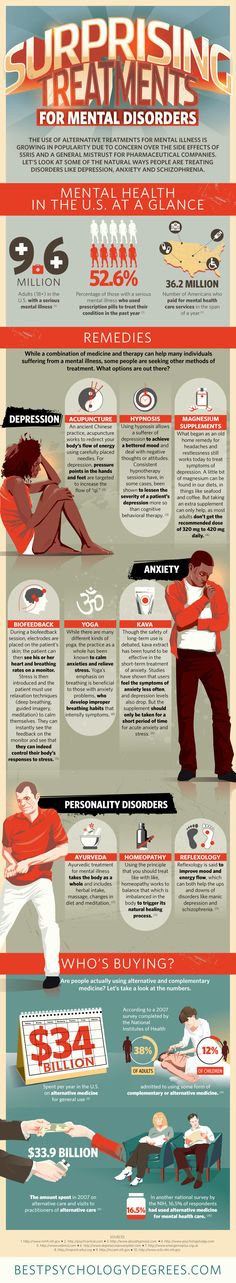 When the levels of neurotransmitters change, depression may develop.
When the levels of neurotransmitters change, depression may develop.
Natural Treatments for Depression
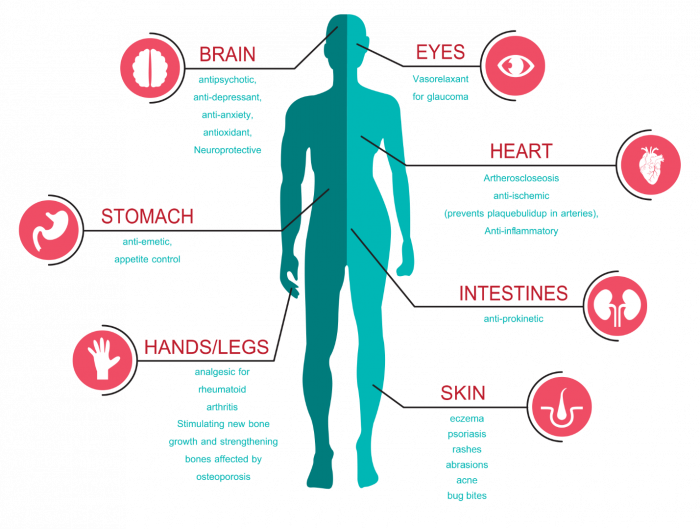
Scientists have studied many herbs, supplements and vitamins for their benefits in depression.
1. St. John's wort and management of depression
Hypericum perforatum (St. John's wort or St. John's wort) is a shrubby plant with yellow flowers. It grows wild throughout Europe, parts of Asia and Africa, and the western United States of America. St. John's wort has been used medicinally for centuries. It can help with a variety of health issues, including symptoms of depression.
The chemical composition of St. John's wort is well known and modern research supports the traditional uses of this plant. This medicinal herb has antidepressant, antiviral and antibacterial properties.
They are due to chemical compounds such as hypericin and flavonoid components. The antidepressant properties of St. John's wort may be primarily based on the hyperforin it contains.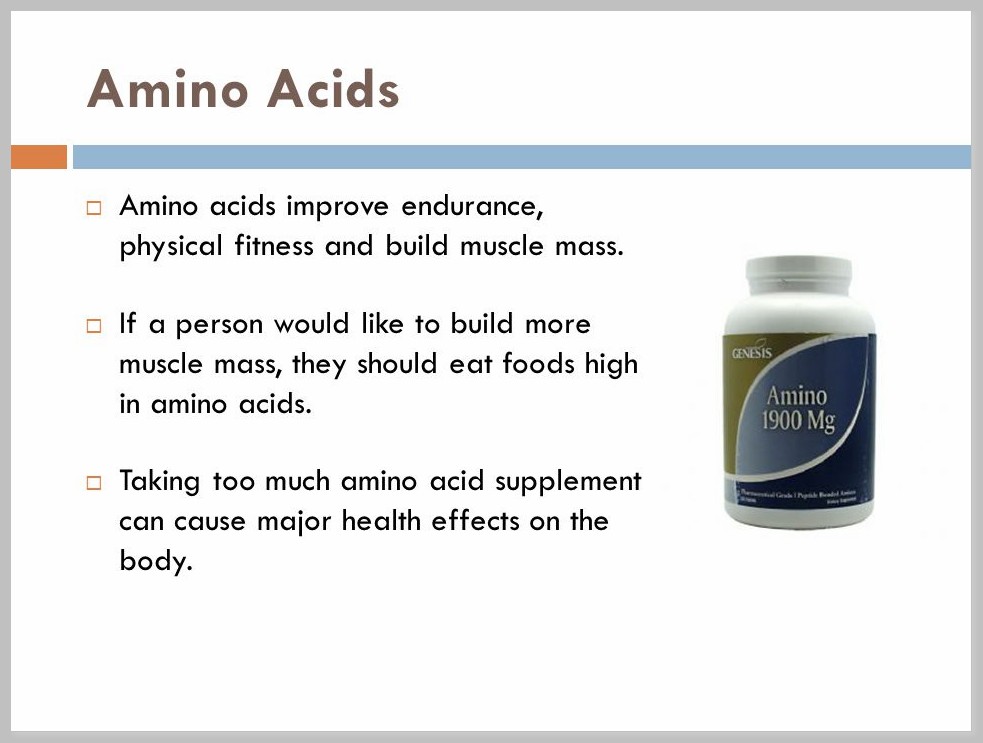 This substance can inhibit the uptake of neurotransmitters such as 5-hydroxytryptamine, dopamine, norepinephrine, GABA. Hyperforin maintains a chemical balance in the brain, eliminating one of the causes of depressive symptoms.
This substance can inhibit the uptake of neurotransmitters such as 5-hydroxytryptamine, dopamine, norepinephrine, GABA. Hyperforin maintains a chemical balance in the brain, eliminating one of the causes of depressive symptoms.
St. John's wort flowers are used in the manufacture of supplements and are sold in the form of teas, tablets and capsules.
2. S-Adenosyl-L-Methionine and Chemistry Balance
S-Adenosyl-L-Methionine (S-Adenosyl Methionine, SAM-e) is a compound naturally produced by the body and involved in many of its most important functions. In the brain, SAM-e promotes the synthesis of the neurotransmitters serotonin, melatonin, and dopamine. Serotonin is an important neurotransmitter that regulates mood, happiness, and anxiety.
S-adenosylmethionine is found in every living cell of the body and is formed from the essential amino acid methionine and adenosine triphosphate. It performs many important functions, one of which is methylation - it is due to this reaction that the synthesis of neurotransmitters is controlled.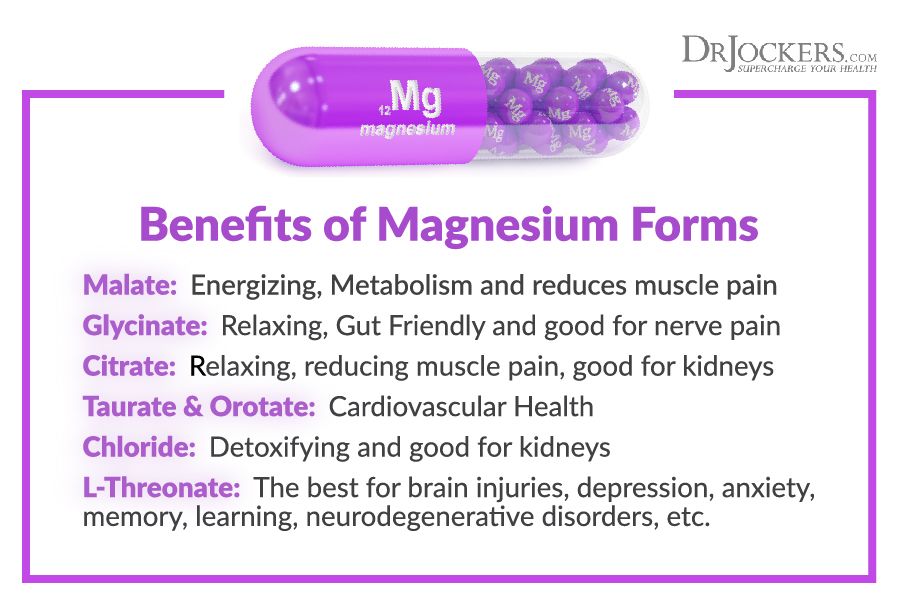
Methylation is a chemical process in which a group of one carbon molecule and three hydrogen molecules is added to another chemical group. S-adenosylmethionine acts as a donor of this methyl group. Roughly speaking, S-adenosylmethionine donates a piece of itself (a methyl group) to another compound. After the methyl group is detached, it attaches to another chemical compound and thereby either creates a new neurotransmitter or deactivates an existing one. The methylation reactions taking place with the participation of S-adenosylmethionine are necessary for the synthesis and deactivation of neurotransmitters (norepinephrine, adrenaline, dopamine, serotonin and histamine).
In other words, S-adenosylmethionine can maintain chemical balance in the brain.
3. 5-hydroxytryptophan and brain serotonin levels
5-hydroxytryptophan (5-HTP) is a compound synthesized by the body from the amino acid tryptophan. Tryptophan is found naturally in some foods, such as turkey, chicken, milk, seaweed, sunflower seeds, turnips, kale, potatoes, and pumpkin. The body extracts this amino acid from food and converts it into 5-hydroxytryptophan.
The body extracts this amino acid from food and converts it into 5-hydroxytryptophan.
5-HTP is a precursor of the essential amino acid L-tryptophan, which plays a major role in the synthesis of serotonin. The enzyme tryptophan hydroxylase converts L-tryptophan to 5-hydroxytryptophan. Tryptophan hydroxylase activity can be suppressed by a variety of factors, including stress, impaired sugar metabolism, vitamin B6 or magnesium deficiency.
In the presence of any of these factors, it is more difficult for the body to produce serotonin. A decrease in serotonin levels leads to an imbalance of brain chemicals and can lead to depression.
5-hydroxytryptophan can help increase the level of serotonin in the brain and thus maintain the correct chemical balance. This substance is sold in the form of supplements made from the seeds of the African plant Griffonia simplicifolia.
4. Omega-3 fatty acids and energy
Omega-3 fatty acids are polyunsaturated fats. This means that they have more than one double chemical bond.
This means that they have more than one double chemical bond.
Many people's diets are deficient in these acids. The industrial farming of domesticated animals (including fish) has led to changes in the diet of animals, resulting in products containing less omega-3 fatty acids than before.
Omega-3 fatty acids are known to be important for a healthy metabolism (the conversion of food into energy). In addition to omega-3s, there are other types of fatty acids, such as omega-6s. Ideally, the ratio of omega-6 to omega-3 fatty acids should be 4:1. The average diet, which includes many processed foods, is high in omega-6s, resulting in a ratio of 10:1 or even 50:1. This can affect the chemical balance and normal brain function.
Omega-3 fatty acid supplements may be made from plant or animal products. Fish-derived omega-3 fatty acids are eicosapentaenoic (EPA) and docosahexaenoic (DHA) acids. Alpha-linolenic acid (ALA) is obtained from plant sources. The omega-3 fatty acids EPA and DHA are most commonly recommended for depression.
5. Vitamin D and Depression Symptoms
Vitamin D can have many benefits for the body, including bone, immune, and cardiovascular support. The body produces vitamin D when the skin is exposed to ultraviolet radiation. Many people are deficient in vitamin D as we spend more time indoors with advances in technology and more computer-related work.
Vitamin D can be obtained from food. For example, it is found in dairy products, sardines and eggs. Vitamin D supplements can easily make up for your deficiency. There is a correlation between low vitamin D levels and symptoms of depression.
An imbalance of depression-related chemicals in the brain can occur when calcium ions (charged particles) are elevated in brain neurons. Large amounts of calcium ions can inhibit the release of certain neurotransmitters. It is believed that vitamin D can reduce the amount of calcium ions and thus help restore the balance of neurotransmitter levels.
Depression is a very common occurrence in the modern world. Luckily, we have healthy and natural ways to deal with it.
Luckily, we have healthy and natural ways to deal with it.
Sources:
- McCarter, T. Depression Overview. Am Health Drug Benefits. 2008 Apr; 1(3): 44-51.
- Barnes, J., Anderson, L.A., and Phillipson, J.D., St. John's Wort (Hypericum perforatum): a review of its chemistry, pharmacology and clinical properties. J Pharm Pharmacol. 2001;53(5):583-600.
- Teodoro, B. S-Adenosyl-L-methionine (SAMe): from the bench to the bedside—molecular basis of a pleiotrophic molecule. Am Journal of Clinical Nutrition. 2002; 76(5): 1151S-1157S.
- Birdsall, T.C. 5-Hydroxytryptophan: A Clinically-Effective Serotonin Precursor. Altern Med Rev. 1998;3(4):271-80.
- Wani, L. Ahmad, S., Bhat, I et al. Omega-3 fatty acids and the treatment of depression: a review of scientific evidence. Integr Med Res. 2015; 4(3): 132-141.
- Berridge, M.J. Vitamin D and Depression: Cellular and Regulatory Mechanisms. Pharmacol Rev. 2017;69(2):80-92.
Non-prescription antidepressants for anxiety and depression, list of titles
BIOLOGICALLY ACTIVE SUPPLEMENT (BAA). Avitamin Evitamin Kvitamin Rvitamin Rvitamin, the Svitamin of the adult, is not an adult immunity-to-mamaglius memaglius-3 if the immunity-toacle, the author of Article
dietary dietary, fitness-stagnation, fitness-stagnation. Diploma of Medical Education: DVS 1724848
All authorsArticle content
- Seasonal depression or beriberi - how to tell the difference?
- Why are we sad in winter?
- Non-prescription antidepressants, drug names
- Which antidepressant is best for anxiety and depression
- What is the safest antidepressant
- Antidepressants and alcohol
- Ask an expert on the topic of the article
Outside the window is gray and empty. Summer colors faded, replaced by winter cold. Together with the withering of nature, the mood fades, and sadness rolls over every now and then. There is a close relationship between the onset of cold weather and depression of the psycho-emotional state.
Summer colors faded, replaced by winter cold. Together with the withering of nature, the mood fades, and sadness rolls over every now and then. There is a close relationship between the onset of cold weather and depression of the psycho-emotional state.
Manifestations of dissatisfaction with oneself and the world around can be mild, not always noticeable, but can literally “cover”, deprive one of the desire to do something. Then hopelessness is felt, tearfulness appears. If you have these symptoms, you need specialist help. But with a breakdown, irritability, general lethargy, you can cope on your own. There are effective remedies that will help cheer you up during the seasonal spleen. In this article, we will tell you how to return the former energy, get rid of the winter blues and see all the colors of life again.
Seasonal depression or beriberi - how to tell the difference?
Depression is experienced by 264 million people in the world - these are the WHO data. If depression drags on, becomes moderate or severe, it can lead to serious health problems.
If depression drags on, becomes moderate or severe, it can lead to serious health problems.
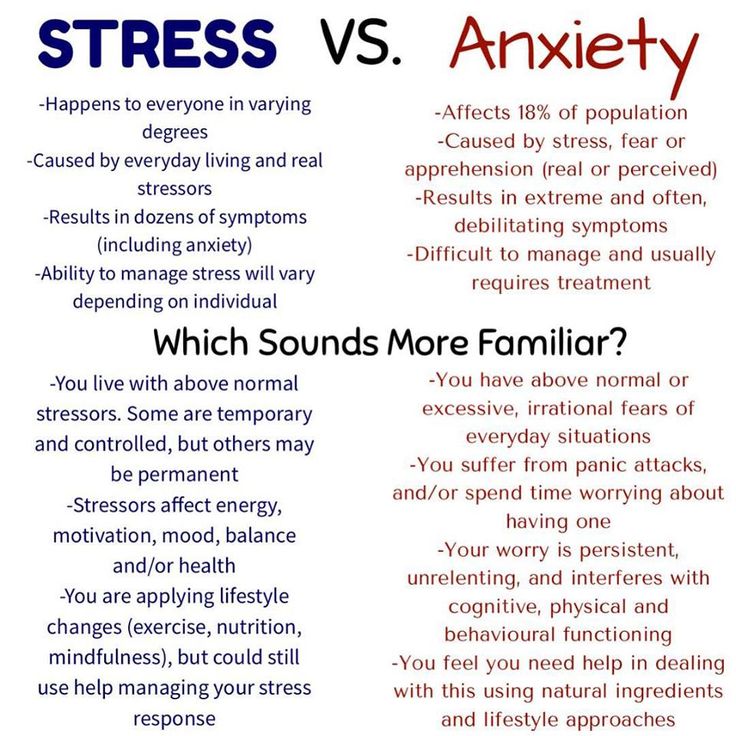
Seasonal depression, in contrast to a simple drop in mood due to stress or beriberi, has its own characteristics:
- Lasts longer than two weeks, there is a decrease in mood.
- Apathy occurs, there is a decrease in activity.
- Appetite disorder appears. A person gains weight up to 6-7 kg in 2-3 months, or, conversely, loses weight dramatically.
- Dramatically increases the duration of sleep.
Why are we sad in winter?
In the last two decades, the number of patients with seasonal depression has increased. According to doctors, from 4 to 10% of people suffer from such depressions. There are several reasons for winter melancholy. Let's talk about the main ones.
- Lack of sun. In summer, there is enough sunshine and you feel comfortable. With the onset of cold weather, the dose of the sun decreases, biochemical processes slow down.
 The body begins to "protest", there is fatigue in the muscles, nervousness. The fact that the sun is the “supplier” of vitamin D has been known to everyone since childhood. And it is the lack of this vitamin that provokes an unstable psycho-emotional state in people of different ages. For example, Italian scientists from the National Institute of Aging have found a relationship between vitamin D deficiency and the onset of depressive symptoms in patients aged 65 and older. The lower the level of the "sunshine" vitamin, the higher was the risk of developing a depressive mood. And researchers from the UK have identified such a relationship in adolescents and concluded that the relationship between the concentration of vitamin D and depression occurs in childhood.
The body begins to "protest", there is fatigue in the muscles, nervousness. The fact that the sun is the “supplier” of vitamin D has been known to everyone since childhood. And it is the lack of this vitamin that provokes an unstable psycho-emotional state in people of different ages. For example, Italian scientists from the National Institute of Aging have found a relationship between vitamin D deficiency and the onset of depressive symptoms in patients aged 65 and older. The lower the level of the "sunshine" vitamin, the higher was the risk of developing a depressive mood. And researchers from the UK have identified such a relationship in adolescents and concluded that the relationship between the concentration of vitamin D and depression occurs in childhood. - Psychological factors. The autumn-winter period is a kind of completion of the annual cycle. People begin to analyze their time, sum up. And plans not always conceived at the beginning of the year are implemented by the end of the year.
 Therefore, there is a feeling of dissatisfaction. By the end of the year, physical and moral strength is also running out, and the lack of rest, experienced emotional upheavals cause a feeling of melancholy. Sudden mood swings are possible.
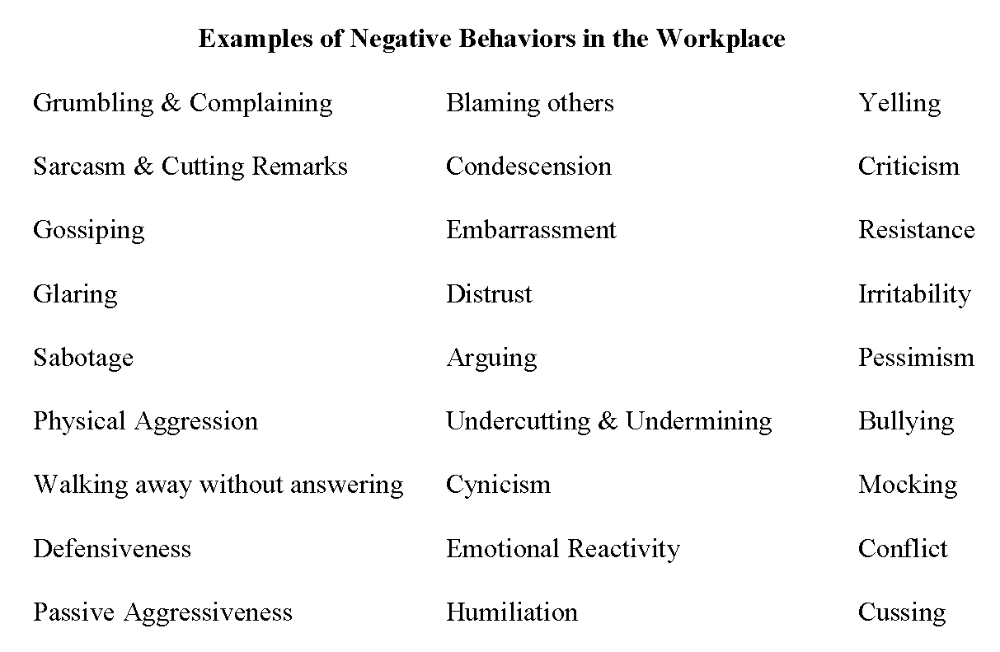
Therefore, there is a feeling of dissatisfaction. By the end of the year, physical and moral strength is also running out, and the lack of rest, experienced emotional upheavals cause a feeling of melancholy. Sudden mood swings are possible. - Stress. An emergency at work, conflicts in the family lead to the fact that a person begins to negatively perceive everything that happens. According to statistics, the peak of nervous tension and fatigue occurs precisely at the end of autumn - the beginning of winter.
- Reduced immunity. According to experts, this feature of autumn depression is associated with a decrease in the quality of the immune system. The lack of vitamins and nutrients, as well as the exacerbation of chronic diseases against the background of a decrease in immunity, negatively affects the state of the human psyche.
Over-the-counter antidepressants, drug names
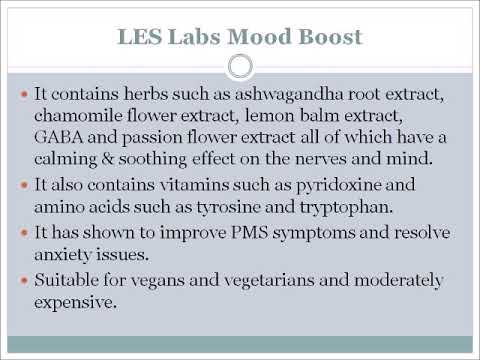
Naturally formulated supplements can help with seasonal disorders and mild depression.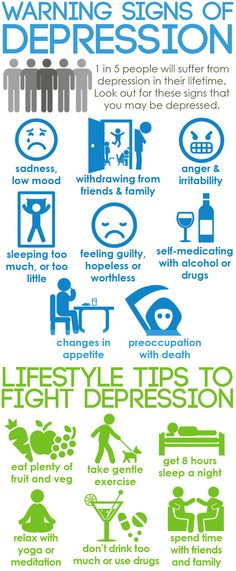 We have collected the top 5 most popular according to the retail audit of the pharmaceutical market in Russia. Let's talk about the pros and cons of each dietary supplement.
We have collected the top 5 most popular according to the retail audit of the pharmaceutical market in Russia. Let's talk about the pros and cons of each dietary supplement.
- Detrimax from Unipharm. The composition of "Detrimax" includes vitamin D3 (cholecalciferol). This vital fat-soluble vitamin is needed for the activity of almost all organs and systems of the body, including the nervous one. Regulates the psycho-emotional sphere, improves memory, performance, mood, increases the overall tone of the body. "Detrimax" has no contraindications during pregnancy, but it should be taken with caution. Clinical studies conducted by medical scientists of the St. Petersburg North-Western State Medical University named after I.I. Mechnikov, confirmed the effectiveness of the drug. Patients improved cognitive function, decreased levels of anxiety and depression.
- "Neurouridin" from "Unipharm". Replenishes the deficiency of biologically active substances. Strengthens the nervous system, improves the general condition of the body, memory, attention.
 Reduces stress reactions. As part of the drug: uridine monophosphate, choline, vitamins B6, B1 and B12. Uridine Monophosphate is important for the rapid recovery of damaged nerves. B vitamins ensure the normal functioning of the nervous system. Folic Acid is important for the brain and maintaining mental and emotional health. Choline improves the transmission of neuromuscular signals, increases the speed of transmission of impulses along nerve fibers. The disadvantages of the drug include the fact that it can not be used during pregnancy and lactation.
Reduces stress reactions. As part of the drug: uridine monophosphate, choline, vitamins B6, B1 and B12. Uridine Monophosphate is important for the rapid recovery of damaged nerves. B vitamins ensure the normal functioning of the nervous system. Folic Acid is important for the brain and maintaining mental and emotional health. Choline improves the transmission of neuromuscular signals, increases the speed of transmission of impulses along nerve fibers. The disadvantages of the drug include the fact that it can not be used during pregnancy and lactation. - Stressovit from Unipharm. Has a sedative effect. Helps reduce psycho-emotional stress, relieve stress, improves overall well-being, increases efficiency. The main component of the drug is magnesium . Magnesium has been proven to be the fourth most abundant mineral in the body. Magnesium deficiency leads to increased irritability, fatigue, sleep disturbance. A sufficient amount of magnesium in the body increases resistance to stress, reduces the excitation of the nervous system, and normalizes sleep.
 The composition of "Stressovita" also includes motherwort, hops and linden flowers. Motherwort relieves manifestations of psycho-emotional overstrain. It has a calming, anti-stress and relaxing effect. Hops - soothes and reduces stress. A similar effect in linden flowers. It is not recommended to use "Stressovit" with individual intolerance to its components, as well as pregnant and lactating mothers.
The composition of "Stressovita" also includes motherwort, hops and linden flowers. Motherwort relieves manifestations of psycho-emotional overstrain. It has a calming, anti-stress and relaxing effect. Hops - soothes and reduces stress. A similar effect in linden flowers. It is not recommended to use "Stressovit" with individual intolerance to its components, as well as pregnant and lactating mothers. - "Kinetop" from "Artlife". Improves mood, increases efficiency, relieves stress, anxiety, eliminates irritability. An important component of Kinetop is 5-hydroxy-L-tryptophan (5-HTP), an amino acid that serves as an intermediate for the conversion of tryptophan into serotonin. It is often referred to as the "happiness hormone". Serotonin improves mood. Lack of hormone leads to depression, insomnia. There is an unhealthy craving for sweets. Kinetop contains the optimal dosage of 5-HTP, as well as magnesium, zinc, vitamins B5 and B6. Another plus of Kinetop is that it does not cause addiction and withdrawal syndrome.
 At the same time, the drug should not be used during pregnancy, lactation, and up to 18 years.
At the same time, the drug should not be used during pregnancy, lactation, and up to 18 years. - Calm formula from Evalar. Dietary supplement based on motherwort . The composition of the drug also includes magnesium and vitamin B6. It has a sedative, anti-anxiety effect. Helps to resist stress, better endure psycho-emotional stress. "Calm formula" is used for increased nervous excitability, irritability, anxiety, insomnia. The drug can not be used for peptic ulcer of the stomach and duodenum in the acute phase, children under 18 years of age, severe renal failure. Not recommended for pregnant and lactating women. Dietary supplement may cause allergic reactions, abdominal pain, nausea, heartburn, flatulence, diarrhea, constipation.
All products DetrimaxImportant! Non-prescription herbal antidepressants are not a panacea. It is an accompanying and restorative element. He will not be able to cure a severe disease.
20 reviews
Add color and positive to your life!
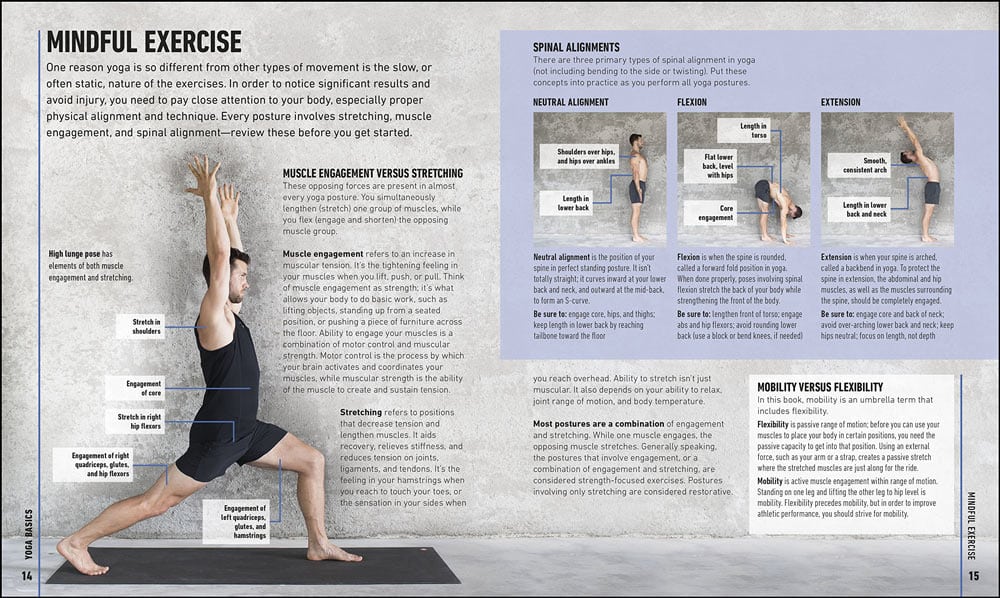
Many say that dietary supplements are a placebo. In most cases, we assign them to ourselves and think that they work. And so it happens, because the power of thought is already a medicine. Think positively and a good mood will not keep you waiting. Positive emotions in life will bring the purchase of various little things that will improve your mood. The colors of life will return the study of something new, self-development, communication with relatives and friends, playing sports. Physical activity has a positive effect on the psycho-emotional balance due to the stimulation of the nervous system. Pay attention to yoga. Scientifically proven fact: Indian hatha yoga helps to forget about depression. Scientists from the Smolensk State Medical Academy studied the effects of yoga therapy on people with various forms of depressive disorders and asthenia. Patients attended classes three times a week for a month and a half. After a yoga course, 12 out of 19patients noted a significant improvement in well-being, up to the complete disappearance of signs of fatigue, increased activity, working capacity, improved mood, significantly improved overall self-esteem.
In most cases, we assign them to ourselves and think that they work. And so it happens, because the power of thought is already a medicine. Think positively and a good mood will not keep you waiting. Positive emotions in life will bring the purchase of various little things that will improve your mood. The colors of life will return the study of something new, self-development, communication with relatives and friends, playing sports. Physical activity has a positive effect on the psycho-emotional balance due to the stimulation of the nervous system. Pay attention to yoga. Scientifically proven fact: Indian hatha yoga helps to forget about depression. Scientists from the Smolensk State Medical Academy studied the effects of yoga therapy on people with various forms of depressive disorders and asthenia. Patients attended classes three times a week for a month and a half. After a yoga course, 12 out of 19patients noted a significant improvement in well-being, up to the complete disappearance of signs of fatigue, increased activity, working capacity, improved mood, significantly improved overall self-esteem.
Look around - the world is full of joy at any time of the year. The main thing is to notice it in time. If your depression is not clinical in nature, you can get rid of the disease yourself and look at life with different eyes.
Sources:
- PubMed: Serum 25-hydroxyvitamin D and depressive symptoms in older women and men. National Institute on Aging, Clinical Research Unit, USA.
- PubMed: "Association of serum 25-hydroxyvitamins D3 and D2 with depressive symptoms in childhood - a prospective cohort study." Center for Causal Analysis in Translational Epidemiology, School of Social and Community Medicine, University of Bristol, UK.
- Russian pharmaceutical market.
- Medical scientific and practical journal "Attending Doctor": "Evaluation of the effectiveness of the use of vitamin D3 (cholecalciferol) in the correction of cognitive disorders in patients with cerebrovascular disease." G. I. Shvartsman, E. M. Pervova, I. V. Chistova, E.
 A. Yurkina. FGBOU VO SZGMU them. I. I. Mechnikov of the Ministry of Health of Russia, St. Petersburg.
A. Yurkina. FGBOU VO SZGMU them. I. I. Mechnikov of the Ministry of Health of Russia, St. Petersburg. - Magnesium in Prevention and Therapy, Academy of Micronutrient Medicine, Germany.
- Sciencedirect.com: "Effect of magnesium supplementation on depressive status in depressed magnesium-deficient patients: a randomized, double-blind, placebo-controlled trial." Department of Nutrition, Faculty of Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
- Cyberleninka.ru: "Application of the Hatha Yoga system as a stage in the complex therapy of depressive disorders." Scientific article by K. A. Yakunin I. A. Zubova.
- World Health Organization.
- Register of medicines of Russia.
Which antidepressant is best for anxiety and depression
Do you want to understand drug analogues in order to skillfully select drugs for your budget? Our manual from expert pharmacists "Analogues of popular drugs" will help you with this! Getting a training manual is easy: subscribe to our social networks and write “analogues” in the messages.
Megapharmacy in social networks: VKontakte, Telegram, OK, Viber
Antidepressant drugs are prescribed strictly by a doctor, after consultation. Thus, it is not possible to say which antidepressant is better, as the doctor decides. For each individual case.
Let's talk about some prescribed antidepressants:
- Phenibut is a prescription drug. Helps reduce or disappear feelings of anxiety, tension, anxiety and fear, normalizes sleep, has some anticonvulsant effect.
- Phenazepam is a prescription drug. The effect is manifested in a decrease in emotional stress, weakening anxiety, fear, anxiety.
- Anafranil is a prescription drug. It has a strong antidepressant effect and common side effects. In addition to the antidepressant effect, it reduces obsession and anxiety.
22 reviews
All products Anafranil5 reviews
All products Phenazepam20 reviews
Which antidepressant is the safest
The safest antidepressant, like the best, has yet to be invented. Any drugs have side effects. We can talk about drugs that have less, compared to others, negative reactions to the patient.
Any drugs have side effects. We can talk about drugs that have less, compared to others, negative reactions to the patient.
These include antidepressants from the group of SSRIs - selective serotonin reuptake inhibitors. Their advantages:
- high efficiency
- short course of treatment
- simple dose adjustment
- good tolerance
Because of their properties, they are often prescribed:
- Zoloft
- Paxil
- Prozac
- Trittiko
- Fevarin
- Cipralex
- Cipramil
Antidepressants of a new class: Brintellix and Valdoxan also have minimal side effects.
Antidepressants and alcohol
Drinking alcohol for depression is common. What happens if antidepressants are added to this relaxation method? The group of antidepressants includes drugs with different mechanisms of action. The effect of co-administration of alcohol and antidepressants is not well understood.