What are ptsd nightmares like
What Can Cause PTSD Nightmares and How Can it Be Treated?
When someone experiences nightmares from PTSD, they can seem very real to them. They might feel like they are back in a situation that is not safe, the traumatic experience that caused the disruption in the first place.
Symptoms can keep them awake or unable to fall asleep for long periods of time. Sleep is essential to healing the body, keeping it healthy, and feeling secure. Find out why nightmares occur with PTSD and how to offer support for someone who is struggling.
Challenges with SleepThe brain and body are wired for sleep at certain hours of the day. When it is dark, people feel tired and ready for rest.
When it is light, people typically feel ready to do things like work, go out with friends, socialize, and take part in activities. Shift workers often struggle with staying up during the nighttime hours and sleeping when it is light outside.
A full night of sleep with PTSD can be challenging and taxing on the body. Nightmares are part of the symptoms of PTSD, which impact overall sleep quality.
With a night’s rest, sleep includes REM and non-REM sleep, alternating cycles throughout the night. Disruptions due to PTSD can cause feelings of hopelessness and despair as a person desperately wants to sleep but cannot.
When they do sleep, they are disturbed by dreams that put them back in a situation where they feel in harm’s way.
Impact on PTSDNightmares are a feature of PTSD. Even general nightmares can feel life-threatening, but with PTSD, they are actually tied to an existing trauma that happened in the near or far past.
Replaying traumatic events over and over can cause a struggle for someone to cope. A nightmare usually involves replaying the traumatic event, feeling like they are right back there again.
For veterans, this might mean re-witnessing horrific events or even deaths of people they witnessed while on combat missions. Physical abuse, violence, and other things can be triggering the nightmares and inability to sleep.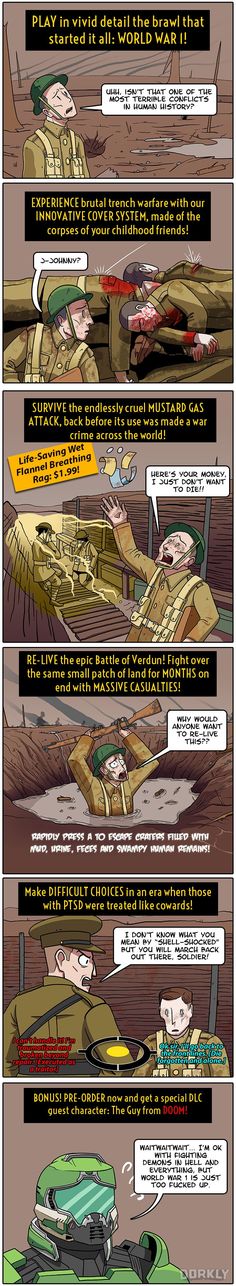
When someone fears going to sleep and is not wanting to go to bed, that can be traumatic. Sleep avoidance in combination with affected sleep cycles causes people to feel less connected to family, their work, and social life. They risk suicidal thoughts and are three times more likely to suffer PTSD-related risk factors such as addiction.
Treatment OptionsDual diagnosis, or experiencing PTSD symptoms with substance use, are not uncommon. It is one way people use to numb the feelings of pain and stress, including flashbacks and nightmares.
Appropriate treatment varies but every person should be evaluated thoroughly to see how they are coping with the nightmares and subsequent issues related to PTSD. This might include looking at relationships, work, and family life to see where they suffer the impact.
Cognitive Behavioral Therapy (CBT)CBT is used to identify and adjust thoughts, emotions, and behaviors they struggle with. These can include sleep therapies, self-exposure therapy, desensitization, and lucid dreaming therapy.
These can include sleep therapies, self-exposure therapy, desensitization, and lucid dreaming therapy.
CBT is a time to sit down with a therapist and work out what has gone on to see if there are identified triggers that may be helpful to work on. The techniques can be used in combination or alone, though future research is needed to determine the best practices related to trauma.
MedicationMedication for PTSD nightmares has had controlled trials and limited studies. One of the drugs looks to reduce the central nervous system’s sympathetic output.
This can help with people who have PTSD because their CNS output is relatively high. With controlled studies and the effects on sleep, this helps them to reduce nightmares.
Other proposed nightmare medications can be prescribed but must be closely monitored, especially with people who experience substance abuse or misuse of opioid and painkiller medications. They may be more sensitive to addictive medication and need to be mindful of what they use.
People who struggle with symptoms of PTSD often feel they are not safe or have moments of uncertainty over safety. Practicing good sleep hygiene involves adequate time for sleep.
Keeping electronic devices use to a minimum and away from the bedroom an hour before bed is most ideal. Sleeping when the body is tired is essential.
Whenever that is, let the body rest. Drop other activities for the time being that are non-essential and get rest.
Get help for substance use disorders and seek support for stress that may kick up negative feelings. Try some exercise to release stress and don’t worry about getting up and going to do things that don’t feel comfortable right now.
Helping a Loved One Through PTSDLoved ones who struggle with symptoms of PTSD can have trouble letting go. Research done on nightmares directly related to PTSD show that support is critical for them but it can be difficult to know how to help.
Seeking individual therapy for them is crucial. Veterans and first responders can use therapies to help align their thoughts and feelings in a different way so they view the world more openly rather than closing off and isolating themselves when they are struggling.
Alcohol and substance use disorders require dual diagnosis treatment when occurring with symptoms of PTSD. It helps to have someone come alongside and help deal with the symptoms.
Recovery groups and community support systems are also important so people know they are not alone in dealing with the reality of addiction and mental health issues.
Forge is a place to come and recover your life from addiction. We help you reimagine what is possible and create the life you’ve been dreaming of.
Call us today: 1-888-224-7312
How Post-Traumatic Stress Disorder Affects Sleep
PTSD related nightmares can persist for years, even after the disorder is controlled. Learn about the impact of PTSD nightmares and what treatments are available.
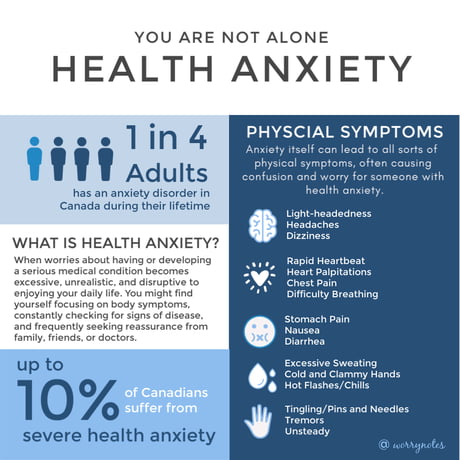
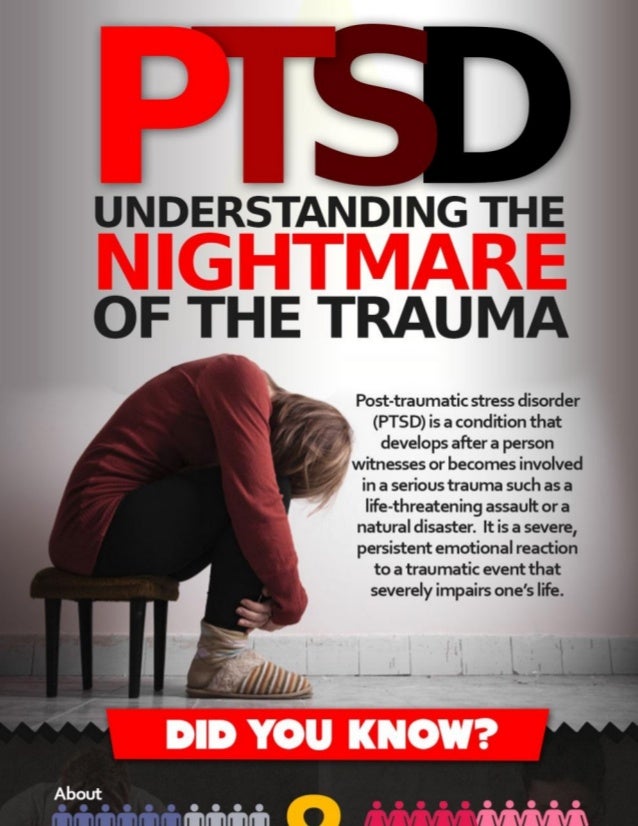
Nightmares can happen to anyone. While disturbing, most individuals can fall back to sleep. It is quite a different story for those who suffer from post-traumatic stress disorder (PTSD). Not only do these individuals live with distressing symptoms during their waking hours, but up to 72% also experience persistent nightmares. PTSD related nightmares can cause insomnia and further worsen other PTSD symptoms.
Knowing why and how PTSD and nightmares occur can help broaden the understanding of this condition, as well as pave the way for effective treatment for those who suffer from PTSD nightmares.
Related Topic: How Post-Traumatic Stress Can Lead to PTSD (Video)
How PTSD Affects Sleep
Sleep is essential to healthy human functioning and without it, the brain cannot function or complete necessary tasks. However, obtaining a full night of sleep with PTSD can be a challenge for many. Researchers are not sure what the exact relationship is between nightmares and PTSD, but they both appear to be related to altered activity in the same region of the brain. In comparison to those without PTSD, the overall sleep quality of individuals with PTSD and nightmares is lower, with noted decreases in sleep time and increased nighttime awakenings.
In comparison to those without PTSD, the overall sleep quality of individuals with PTSD and nightmares is lower, with noted decreases in sleep time and increased nighttime awakenings.
A typical full night of sleep consists of both rapid eye movement (REM) and non-REM sleep. In one night, people cycle several times through these stages, with increasingly longer and deeper REM periods of sleep toward the early morning hours. PTSD sleep issues and nightmares can occur during any of these sleep stages but tend to more frequently occur during the latter part of the night. Frequent disruptions due to PTSD can cause sleep deprivation and feelings of helplessness in those it affects.
While PTSD and sleep disorders are two distinct conditions, one cannot be treated without addressing the other when they occur together. The effects of PTSD alone are enough to significantly impact an individual’s quality of life, but sleep deprivation due to nightmares can introduce additional health risks such as obesity, heart disease, diabetes and shortened life expectancy.
The Impact of Nightmares on PTSD
Nightmares are considered a central feature of PTSD. While a generic nightmare may feel extreme and life-threatening, it is usually unrelated to actual events. PTSD nightmares, however, are usually directly related to a previously experienced, traumatic event. For veterans, an example of a PTSD nightmare usually involves the replaying of traumatic events they witnessed or took part in. Similar to civilians who suffer from PTSD, their nightmares could be a replay of the traumatic event, such as physical abuse or violence.
One sleep therapist described what PTSD nightmares are like based on the experience of their clients. They involved a replay of traumatic and vivid images, such as being knocked over by blown up body parts of a close friend, seeing the face of a person they killed in battle, or seeing the same image over and over again, such as what occurred with many people who witnessed the terrorist attacks of 9/11.
The trauma of reliving these nightmares causes many to dread or fear sleep. The avoidance of sleep in combination with an already inefficient sleep cycle causes many to become irritable and affects family, professional and social life. In one study, the risk of becoming suicidal or having suicidal thoughts was three times more likely in PTSD sufferers. With the addition of nightmares, individuals can be made to feel defeated and hopeless, contributing to the risk for suicidal ideation.
The avoidance of sleep in combination with an already inefficient sleep cycle causes many to become irritable and affects family, professional and social life. In one study, the risk of becoming suicidal or having suicidal thoughts was three times more likely in PTSD sufferers. With the addition of nightmares, individuals can be made to feel defeated and hopeless, contributing to the risk for suicidal ideation.
In contrast to waking hours, where triggers can be clearly seen and often avoided by those with PTSD, nightmares occur irrespective of triggers and can persist even decades after the trauma originally occurred. Researchers have also noted that once nightmares are present, they can increase the rate at which PTSD progresses.
Treating Sleep Disorders in People with PTSD
The most appropriate treatment for PTSD nightmares varies from person to person and is determined by the individual and the provider’s assessment of the severity of the nightmares, and access to treatment options.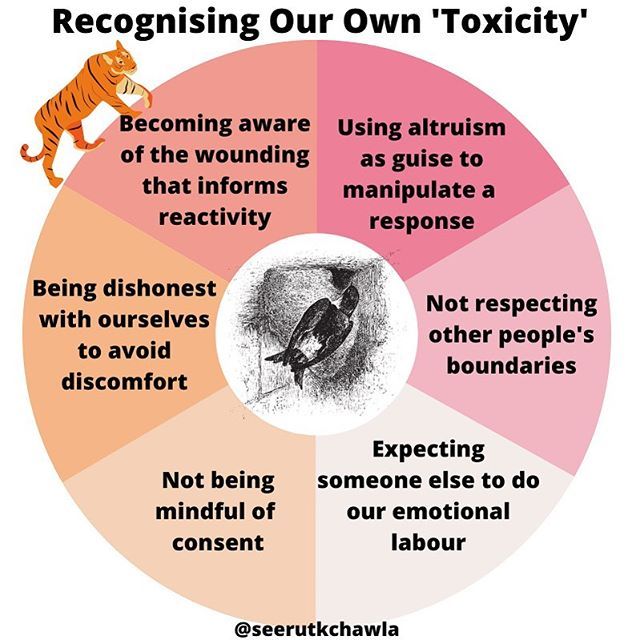 After a thorough assessment of the individual’s life experiences and symptoms, a treatment plan can be initiated to help them overcome PTSD nightmares. There are currently many types of treatment available to help people cope with PTSD, including image rehearsal therapy, cognitive behavioral therapy, EMDR therapy and medication.
After a thorough assessment of the individual’s life experiences and symptoms, a treatment plan can be initiated to help them overcome PTSD nightmares. There are currently many types of treatment available to help people cope with PTSD, including image rehearsal therapy, cognitive behavioral therapy, EMDR therapy and medication.
Image Rehearsal Therapy
Image rehearsal therapy is a preferred treatment for post-traumatic nightmares. The recurring nightmare is rehearsed during the day and altered into a new scene with a different ending. The newly modified script is to be rehearsed on a daily basis with the goal of removing the fear factor within the nightmares and replacing it with something more positive. This form of therapy typically lasts for 12 weeks and can be done in an individual or group format. In one study, 60% experienced a reduction in nightmares and PTSD symptoms.
Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) is often used to identify and adjust distorted thoughts and emotions and the behaviors they lead to. There are now specific techniques of CBT for nightmares related to PTSD.
There are now specific techniques of CBT for nightmares related to PTSD.
These include:
- Image rehearsal therapy
- Lucid dreaming therapy
- Sleep dynamic therapy
- Self-exposure therapy
- Systematic desensitization
These CBT techniques can be used in combination or alone, though future research is needed to determine the best practice for nightmares related to trauma.
EMDR Therapy
Eye movement desensitization and reprocessing (EMDR) therapy is an intervention that incorporates several different therapies and techniques into one. The idea behind EMDR is that nightmares, or the remembrance of a disturbing event, have not been completely processed in the brain but are retained in a dysfunctional form. Through EMDR a person is made to recall distressing images while performing a type of bilateral sensory input such as side to side eye movement or hand tapping. By doing these in tandem, the working memory becomes overloaded and emotional arousal and imagery decreases.
Noted physiologic and emotional changes seen during this type of therapy include synchronized respirations and a lowered heart rate, indicative of relaxation. EMDR for PTSD has shown positive and promising results, with one study demonstrating a reduction in the severity of nightmares in comparison to other interventions.
Medication
Medication for PTSD nightmares has been studied, though the small number of controlled trials limit what guidelines are in place. One such medication that has been studied and is recommended for PTSD is prazosin. Initially introduced as an antihypertensive medication, prazosin reduces the central nervous system’s (CNS) sympathetic output. This is significant for those with PTSD who typically experience elevated CNS activity. There have been many controlled studies thus far with prazosin, and the effects have included an increase in total sleep time and increased REM sleep time. In all the studies, prazosin had moderate to strong benefits on the participants, with a significant reduction in PTSD nightmares.
Other proposed PTSD nightmare medications include:
- Clonidine
- Trazodone
- Risperidone
- Topiramate
- Cortisol
- Gabapentin
- Sertraline
- Paroxetine
Related Topics:
Is there a cure for PTSD
Coping Skills for PTS and PTSD (Video)
Preventing PTSD Nightmares
While PTSD nightmares can occur regularly and persistently, there are some simple steps people can incorporate to help prevent PTSD nightmares.
These include:
- Creating a comfortable and safe sleeping space: Practicing good sleep hygiene involves setting adequate time for sleep and avoiding electronic devices or blue light that can add to insomnia.
- Sleeping when needed and avoiding forcing sleep: Taking naps during the day is okay. It’s also okay to get up at night when sleep is not coming easily. Engaging in a quiet activity until becoming sleepy is much better than forcing oneself to sleep and adding more stress to an already stressful situation.

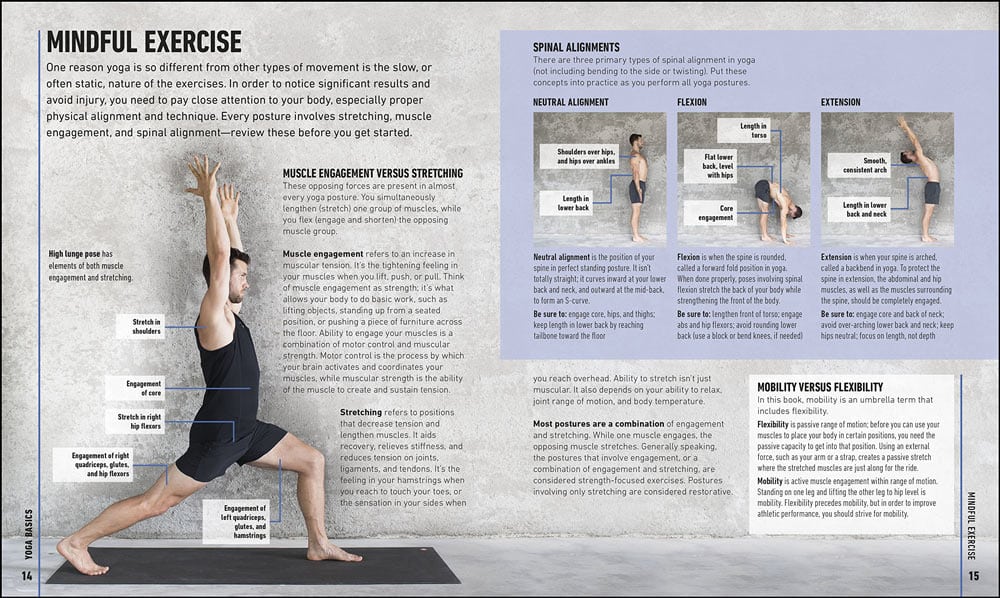
- Avoiding alcohol and drugs: Turning to alcohol or drugs to forget the pain associated with trauma can only add to the problem. When faced with the stress of those negative feelings, try a form of exercise to release stress, such as walking, running or yoga.
If you want to help someone with PTSD nightmares, offering support in practical ways can be of the most benefit. Being available to listen or act as a companion for some activity can be of great encouragement to a person with PTSD.
Summing Up: PTSD Nightmares
PTSD nightmares can be scary, but they don’t have to be a regular, nightly feature. With many forms of therapy available, it is possible to welcome sleep instead of avoiding it. Much of the research done on nightmares is directly related to PTSD and the results show much promise.
Current therapies and medications to keep in mind when considering treatment for PTSD include:
- Prazosin: A medication that decreases CNS output
- Image Rehearsal Therapy: A form of therapy that rewrites the original story of trauma to include a positive ending
- EMDR Therapy: A form of therapy that helps to lessen arousal associated with traumatic memories
If you or someone you know struggles with PTSD nightmares and uses alcohol or other substances to cope, know you are not alone. Contact The Recovery Village today to speak to a representative and discuss a treatment plan appropriate for you.
Contact The Recovery Village today to speak to a representative and discuss a treatment plan appropriate for you.
Editor – Megan Hull
Megan Hull is a content specialist who edits, writes and ideates content to help people find recovery. Read more
Medically Reviewed By – Dr. Karen Vieira, PhD
Dr. Karen Vieira has a PhD in Biomedical Sciences from the University of Florida College of Medicine Department of Biochemistry and Molecular Biology. Read more
El-Solh, Ali A. “Management of nightmares in patients wit[…]current perspectives.” Nature and Science of Sleep, November 26, 2018. Accessed June 28, 2019.
NHS. “Why lack of sleep is bad for your health.” Last reviewed May 30, 2018. Accessed June 28, 2019.
Aurora, R. Nisha; et al. “Best Practice Guide for the Treatment of[…] Disorder in Adults.” Journal of Clinical Sleep Medicine, August 15, 2010. Accessed June 29, 2019.
Medical Disclaimer
The Recovery Village aims to improve the quality of life for people struggling with substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes.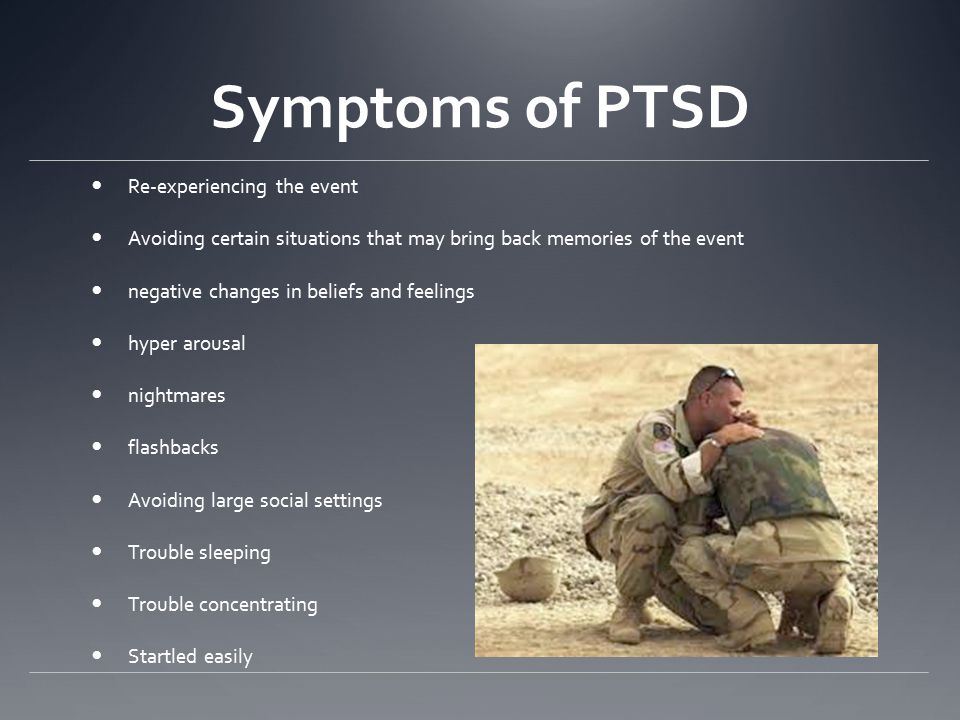 We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.
We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.
PTSD
") end if %>
Variant of Acrobat Samana Gaze | Acrobat Reader Samana Download
PTSD is a normal response
for severe traumatic events.
This booklet deals with signs,
symptoms and treatments for PTSD.
New York State
Department of Mental Health
Have you experienced a terrible and dangerous event? Note please, those cases in which you recognize yourself.
- Sometimes, out of the blue, everything that happened to me is happening again. I never know when to expect it again.

- I have nightmares and memories of the terrible incident which I have experienced.
- I avoid places that remind me of that incident.
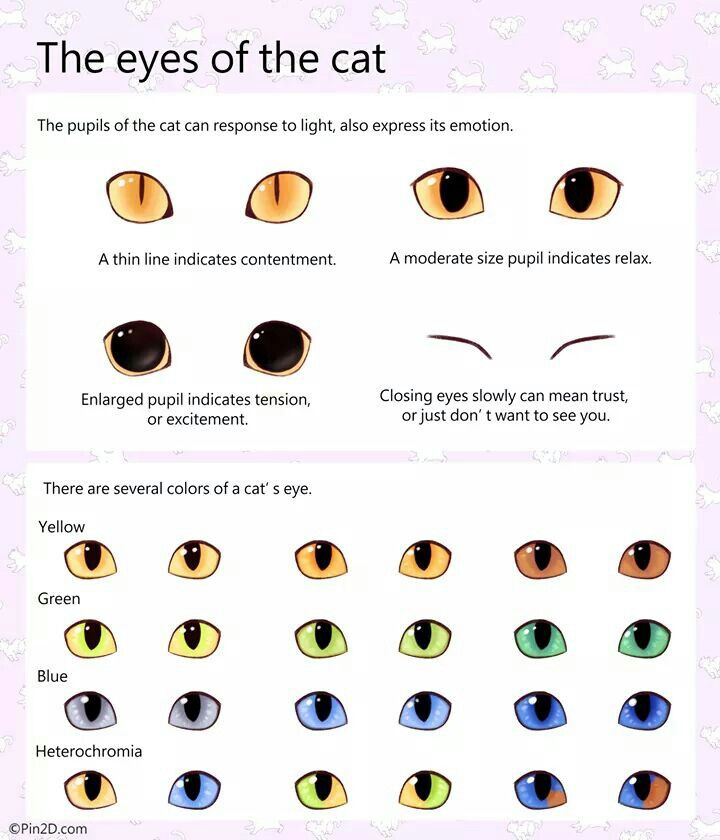
- I jump on the spot and feel uneasy at any sudden movement or surprise. I feel alert all the time.
- It's hard for me to trust someone and get close to someone.
- Sometimes I just feel emotionally drained and deaf.
- I get angry very easily.
- I am tormented by guilt that others died, but I survived.
- I sleep poorly and experience muscle tension.
PTSD is a very serious condition that needs to be treated.
Many people who have experienced terrible events suffer from this disease.
It is not your fault that you fell ill, and you should not suffer from it.
Read this booklet to find out how you can be helped.
You can get well and enjoy life again!
What is post-traumatic stress disorder (PTSD/PTSD)?
PTSD is a very serious condition.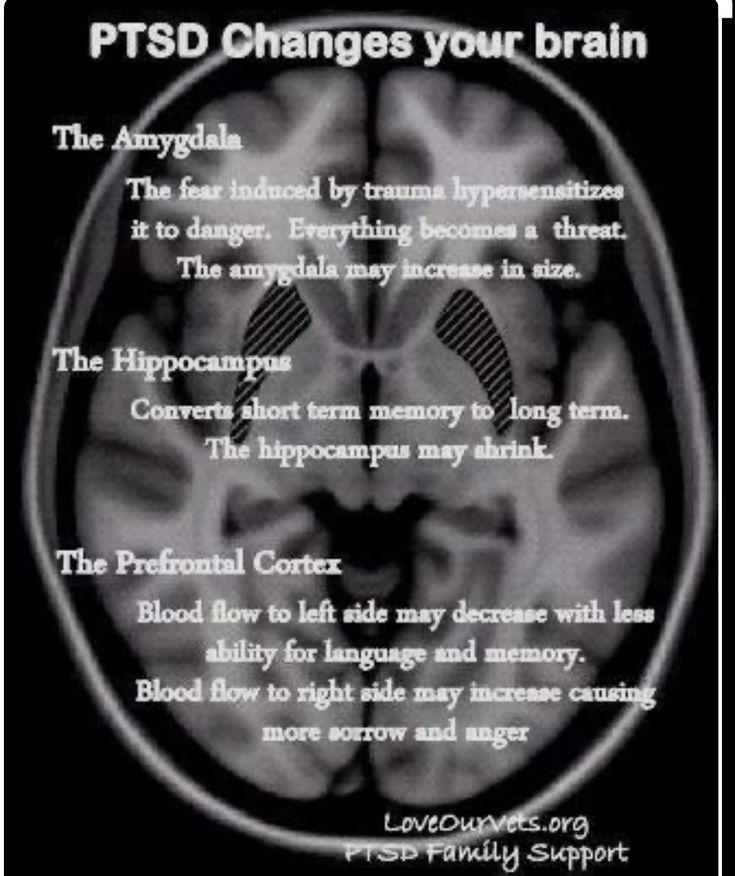 PTSD symptoms may occur in a person who has experienced a terrible traumatic event. This disease is susceptible medical and therapeutic treatment.
PTSD symptoms may occur in a person who has experienced a terrible traumatic event. This disease is susceptible medical and therapeutic treatment.
PTSD can occur after you:
- Have been a victim of sexual abuse
- Have been a victim of physical or emotional domestic violence
- Victim of a violent crime
- Been in a car accident or plane crash
- Survived a hurricane, tornado, or fire
- Were at war
- Survived a life-threatening event
- Witnessed any of the above events
If you have post-traumatic stress disorder, you often have nightmares or memories associated with the event. you try to hold on away from anything that might remind you of the experience.
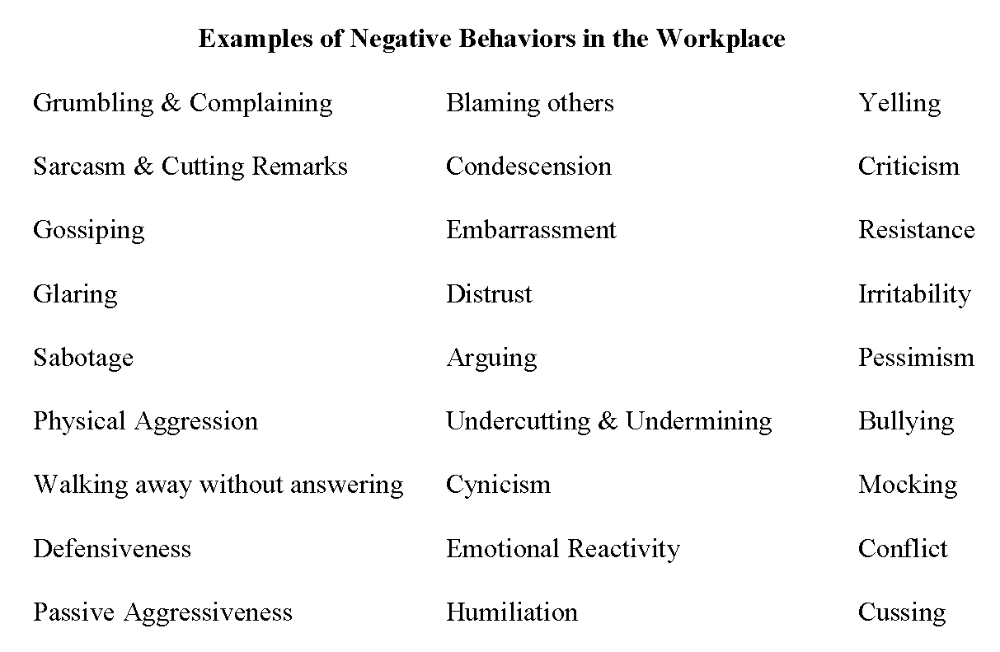
You are bitter and unable to trust or care for others. You are always on your guard and see a hidden threat in everything. You become not by itself, when something happens suddenly and without warning.
When does PTSD start and how long does it last?
In most cases, post-traumatic stress manifests itself approximately three months after the traumatic event.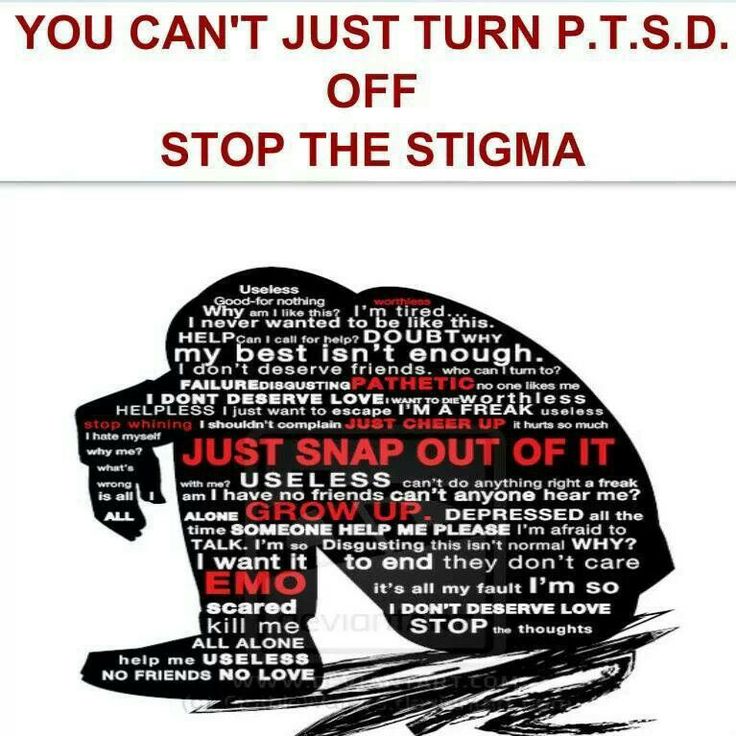 In some cases, signs Post-traumatic stress symptoms only show up years later. Post-traumatic Stress affects people of all ages. Even children are not immune from it.
In some cases, signs Post-traumatic stress symptoms only show up years later. Post-traumatic Stress affects people of all ages. Even children are not immune from it.
Some get better after six months, others may suffer from it illness for much longer.
Am I the only one with this disease?
No, you are not alone. Every year, 5.2 million Americans suffer from PTSD.
Women suffer from this disease two and a half times more often than men. The most common traumatic events that cause PTSD in men are: rape, participation in hostilities, abandonment and abuse in childhood. The most traumatic events in women are rape, sexual molestation, physical assault, threat weapons and childhood abuse.
What other conditions can accompany PTSD?
Common depression, alcoholism and drug addiction, or other anxiety disorders. The likelihood of successful treatment increases if these comorbidities to identify and treat in time.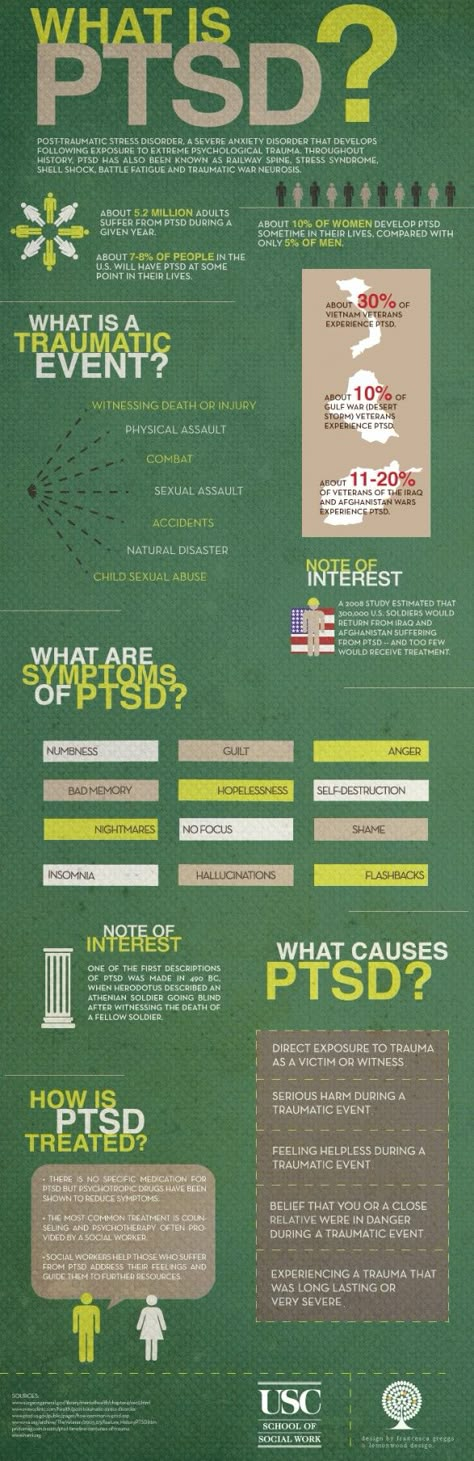
Frequent headaches, gastroenterological problems, problems with the immune system, dizziness, chest pain or discomfort in other parts of the body. It often happens that a doctor treats physical symptoms, unaware that their cause lies in PTSD.
The National Institute of Mental Health (NIMH) recommends therapists to learn from patients about experiences of violence, recent losses and traumatic events, especially when symptoms persist are returning. After diagnosing PTSD, it is recommended to refer patient to a mental health specialist who has experience in the treatment of patients with PTSD.
What should I do to help myself in this situation?
Talk to your doctor and tell him about your experience, and how you feel. If you are visited by terrible memories, overcomes depression and sadness if you have trouble sleeping and constantly embittered - you should tell your doctor about all this. Tell him Are any of these conditions preventing you from doing your daily activities? lead a normal life. You may want to show this booklet to your doctor. This may help explain to him how you feel. Ask your doctor examine you to make sure there are no physical illnesses.
You may want to show this booklet to your doctor. This may help explain to him how you feel. Ask your doctor examine you to make sure there are no physical illnesses.
Ask your doctor if he has had patients with post-traumatic stress. If your doctor does not have a special preparation, ask him for directions to doctor with relevant experience.
How can a doctor or psychotherapist help me?
Your doctor may prescribe medicine to help reduce your fear or tension. However, it should be borne in mind that usually several weeks before the medicine starts to work.
Many PTSD sufferers benefit from talking with a professional or other people who have experienced traumatic events. This is called "therapy". Therapy will help you get over your nightmare.
One man's story:
"After I was attacked, I He constantly felt fear and depression, became irritable. I couldn't sleep well and lost my appetite. Even when I tried not think about what happened, I was still tormented nightmares and terrible memories.
Even when I tried not think about what happened, I was still tormented nightmares and terrible memories.
“I was completely at a loss and didn't know what to do. one buddy advised to see a doctor. My doctor helped me find a specialist in post-traumatic stress."
“I needed a lot of strength, but after medication and a course of therapy, I gradually come to my senses. It’s good that I called my doctor then.”
PTSD and the military
If you are in the military, you have probably been in combat. You, probably got into terrible and life-threatening situations. They shot at you you have seen your friend shot, you have seen death. experienced you events can cause PTSD.
Experts say that PTSD occurs:
- Nearly 30% of Vietnam War veterans
- Nearly 10% of Gulf War veterans (Operation Desert Storm)
- Almost 25% of veterans of the war in Afghanistan (operations "Introducing freedom") and veterans of the war in Iraq (operations "Iraqi Freedom")
Other factors of the military situation can serve as an additional stress to and so stressful situation and can contribute to the development of PTSD and other mental problems. Among these factors are the following: your military specialty, the political aspects of the war, where the battle takes place and who your enemy is.
Among these factors are the following: your military specialty, the political aspects of the war, where the battle takes place and who your enemy is.
Another reason that contributes to PTSD in military personnel can be Military Sexual Assault (MST) – any form of sexual harassment or sexual abuse while serving in the military. MST can happen with men and women, and can occur in peacetime, during war training or during the war.
Veterans Affairs (VA) health care approximately:
- 23 out of 100 women (23%) report sexual violence during military service
- 55 out of 100 women (55%) and 38 out of 100 men (38%) were exposed to sexual harassment while serving in the army
Although the trauma of sexual assault is more common in the military among women, more than half of veterans who have experienced sexual trauma violence in the army - it's men.
Remember, you can get the help you need right now:
Tell your doctor about your experience and how you feel. If your doctor does not have special training in the treatment of PTSD, ask him for a referral to a doctor who has relevant experience.
If your doctor does not have special training in the treatment of PTSD, ask him for a referral to a doctor who has relevant experience.
PTSD research
To help those suffering from PTSD, the National Institute of Conservation Mental Health (NIMH) supports research into the study of PTSD, as well as other thematically related to PTSD research on problems anxiety and fear. The challenge for research is to find new ways to help people cope with trauma, as well as find new treatment options and, The main thing is to prevent disease.
Research on possible risk factors for PTSD
Today, the attention of many scientists is focused on genes that play a role in having terrible memories. Understanding the mechanism of "creation" of scary memories can help improve or find new ways to alleviate symptoms of PTSD. For example, PTSD researchers have identified genes that are responsible for:
Statmin is a protein involved in the formation of terrible memories. During one experiment, mice were placed in environment designed to instill fear in them. In this situation mice lacking the statmin gene, in contrast to normal mice were less likely to "freeze" - i.e. exercise natural defensive response to danger. Also in the environment designed to evoke innate fear in them, they demonstrated it to a lesser extent than normal mice, more willingly mastering the open "dangerous" space. 1
During one experiment, mice were placed in environment designed to instill fear in them. In this situation mice lacking the statmin gene, in contrast to normal mice were less likely to "freeze" - i.e. exercise natural defensive response to danger. Also in the environment designed to evoke innate fear in them, they demonstrated it to a lesser extent than normal mice, more willingly mastering the open "dangerous" space. 1
GRP (gastrin-releasing peptide/GRP) - signal substance brain released during emotional events. At in mice, GWP helps control the fear response, and lack of GWP can lead to a longer memory of fear. 2
Scientists have also discovered a variant of the 5-HTTLPR gene that controls serotonin (a brain substance associated with mood), which, as it turns out, feeds the fear response. 3 It seems that, like in the case of other mental disorders, in the development of PTSD different genes are involved, each of which contributes to the formation of the disease.
Understanding the causes of PTSD can also be helped by studying different areas brain responsible for fear and stress. One of these areas is cerebellar amygdala, responsible for emotions, learning and memory. It turned out that she plays an active role in the emergence of fear (or other words, "teaches" to be afraid of something, for example, to touch a hot stove), as well as in the early phases of fear repayment (or in other words, "teaches" Do not be scared). 4
The retention of faded memories and the weakening of the initial fear reaction are associated with the prefrontal cortex (PFC / PFC) of the brain, 4 responsible for decision making, problem solving and situation assessment. Each zone PFC has its own role. For example, when the PFC believes that a stressor is amenable to control, the medial prefrontal zone of the PFC suppresses the anxiety center deeply in the brainstem and controls the response to stress.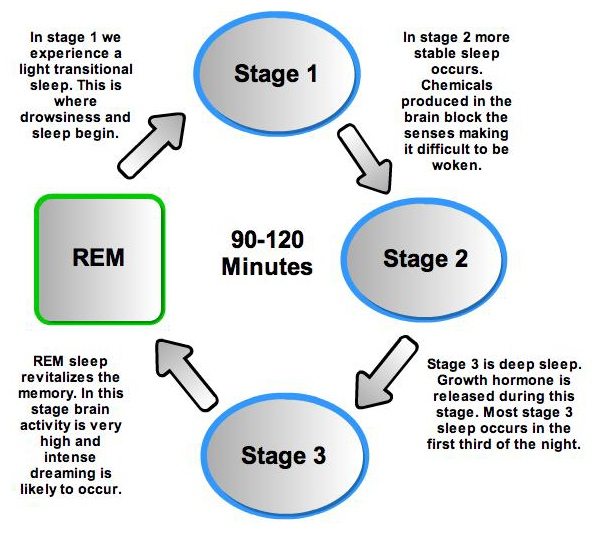 5 Ventromedial PFC helps maintain long-term fading of fearful memories, and her ability to perform this feature can be affected by its size. 6
5 Ventromedial PFC helps maintain long-term fading of fearful memories, and her ability to perform this feature can be affected by its size. 6
Individual differences in genes or characteristics of regions of the brain brain can only set the stage for PTSD, but by themselves do not cause no symptoms. environmental factors such as childhood trauma, head trauma or mental illness in family, favor the development of the disease and increase the risk of disease, affecting the brain in the early stages of its growth. 7 Except In addition, how people adapt to trauma is likely to be influenced by and characteristics of character and behavior, such as optimism and a tendency to consider problems in a positive or negative way, as well as social factors such as availability and use of social support. 8 Further research may show what combination of these factors or what other factors will allow ever predict who has a traumatic event cause PTSD, and who doesn't.
PTSD research
Currently, psychotherapy is used in the treatment of PTSD ("talk" therapy), drugs or drug-therapeutic combination.
Psychotherapy
Cognitive behavioral therapy (CBT) helps you learn differently think and react to frightening events that are the impetus for development PTSD, and can help bring the symptoms of the disease under control. There are several types cognitive behavioral therapy, including:
"Push" method - uses mental images, notes or visiting a place experienced trauma to help those affected face the overwhelming their fear and take control of it.
Behavior restructuring (cognitive restructuring) - encourages survivors of a traumatic event express depressing (often erroneous) thoughts about experienced trauma, challenge these thoughts and replace them with more balanced and appropriate.
Implementation in a stressful situation - teaches ways to reduce anxiety and the ability to cope with it, helping to reduce the symptoms of PTSD, and helps to correct the erroneous train of thought associated with the trauma experienced.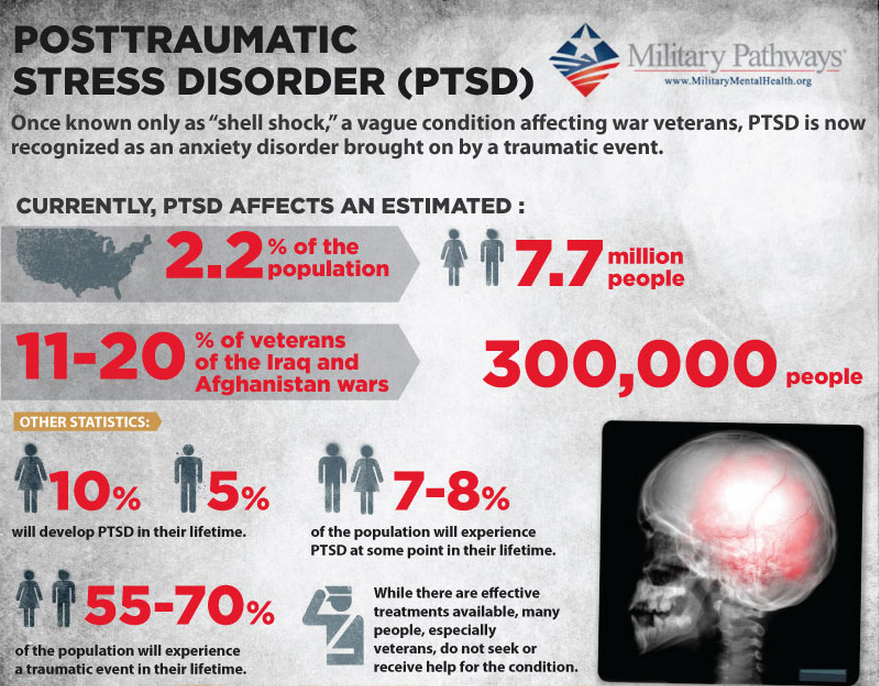 NIMH is currently conducting research to study the reaction brain response to cognitive behavioral therapy versus response sertraline (Zoloft) - one of two drugs recommended and approved US Food and Drug Administration funds (FDA) for the treatment of post-traumatic stress. This research may help find out why some people respond better to medications, and others for psychotherapy
NIMH is currently conducting research to study the reaction brain response to cognitive behavioral therapy versus response sertraline (Zoloft) - one of two drugs recommended and approved US Food and Drug Administration funds (FDA) for the treatment of post-traumatic stress. This research may help find out why some people respond better to medications, and others for psychotherapy
Drugs
Recently, in a small study, NIMH scientists found that if patients who are already taking a dose of prazosin (Minipress) at bedtime, add a daily dose, then this weakens the general symptoms of PTSD and stress reaction to reminders of the trauma experienced. 9
Another drug of interest is D-cycloserine (Seromycin), which increases the activity of a brain substance called N-methyl-D-aspartate, needed to pay off fear. During the study, which was attended by 28 people suffering from a fear of heights, scientists found that patients who received "push" therapy before a session D-cycloserine, showed lower levels of fear during the session compared to those who did not receive the drug. 10 Currently scientists study the effectiveness of the combined use of D-cycloserine and therapy for the treatment of post-traumatic stress.
10 Currently scientists study the effectiveness of the combined use of D-cycloserine and therapy for the treatment of post-traumatic stress.
Propranolol (Inderal), a beta-blocker drug, also under study whether it can be used to reduce post-traumatic stress and break the chain of scary memories. First experiments gave consoling results: it was possible to successfully weaken and, it seems, prevent PTSD in a small number of victims of traumatic events. 11
For example, in one preliminary study, scientists created a website self-help, based on the use of a psychotherapeutic method implementation in a stressful situation. First, patients with PTSD meet in person with doctor. After this meeting, participants can go to the site to find more information about PTSD and how to deal with the problem; their doctors may also visit the site to give advice or briefing. In general, scientists believe that therapy in this form - promising treatment for a large number of people suffering from PTSD. 12
12
Scientists are also working to improve methods for testing early treatment and monitoring of survivors of massive trauma, on developing ways to teach them self-assessment skills and introspection and referral mechanism to psychiatrists (if necessary).
Prospects for PTSD research
In the last decade, rapid progress in the study of mental and biological PTSD has led scientists to conclude that there is a need to focus on prevention, as the most realistic and important goal.
For example, in order to find ways to prevent PTSD, with funding NIMH conducts research to develop new and orphan drugs, aimed at combating the underlying causes of the disease. During another research scientists are looking for ways to enhance behavioral, personality and social protective factors and minimizing risk factors for prevent the development of PTSD after trauma. Another study is studying the question of what factors influence the difference in response to one or another method of treatment, which will help in the development of more individual, effective and productive methods of treatment.
Where can I find more information?
MedlinePlus - resource from the American National Library of Medicine (U.S. National Library of Medicine and the National Institutes of Health) - offers the latest information on many health issues. Information about You can find PTSD at: www.nlm.nih.gov/medlineplus/posttraumaticstressdisorder.html.
National Institute of Mental Health
Office of Science Policy, Planning, and Communications
[National Institute of Mental Health
Science Policy Division research, planning and communications]
6001 Executive Boulevard
Room 8184, MSC 9663
Bethesda, MD 20892-9663
Phone: 301-443-4513; Fax: 301-443-4279
fax answering system Free answering machine: 1-866-615-NIMH (6464)
Text phone: 1-866-415-8051 toll-free
Email: [email protected]
National Center for Post-traumatic Stress Disorder
[National PTSD Center]
VA Medical Center (116D)
215 North Main Street
White River Junction, VT 05009
802-296-6300
www. ncptsd.va.gov
ncptsd.va.gov
NOTES
- Shumyatsky GP, Malleret G, Shin RM, et al. Stathmin, a Gene Enriched in the Amygdala, Controls Both Learned and Innate Fear. cell. Nov 18 2005;123(4):697-709.
- Shumyatsky GP, Tsvetkov E, Malleret G, et al. Identification of a signal network in lateral nucleus of amygdala important for inhibiting memory specifically related to learned fear. cell. Dec 13 2002;111(6):905-918.
- Hariri AR, Mattay VS, Tessitore A, et al. Serotonin transporter genetic variation and the response of the human amygdala.Science. Jul 192002;297(5580):400-403.
- Milad MR, Quirk GJ. Neurons in medial prefrontal cortex signal memory for fear extinction. Nature. Nov 7 2002;420(6911):70-74.
- 5 Amat J, Baratta MV, Paul E, Bland ST, Watkins LR, Maier SF. Medial prefrontal cortex determines how stressor controllability affects behavior and dorsal raphe nucleus.
 Nat Neurosci. Mar 2005;8(3):365-371.
Nat Neurosci. Mar 2005;8(3):365-371. - Milad MR, Quinn BT, Pitman RK, Orr SP, Fischl B, Rauch SL. Thickness of ventromedial prefrontal cortex in humans is correlated with extinction memory. Proc Natl Acad Sci USA. Jul 26 2005;102(30):10706-10711.
- Gurvits TV, Gilbertson MW, Lasko NB, et al. Neurological soft signs in chronic posttraumatic stress disorder.Arch Gen Psychiatry. Feb 2000;57(2):181-186.
- Brewin CR. Risk factor effect sizes in PTSD: what this means for intervention. J Trauma Dissociation. 2005;6(2):123-130.
- Taylor FB, Lowe K, Thompson C, et al. Daytime Prazosin Reduces Psychological Distress toTrauma Specific Cues in Civilian Trauma Posttraumatic stress disorder. Biol Psychiatry. Feb 3 2006.
- Ressler KJ, Rothbaum BO, Tannenbaum L, et al. Cognitive enhancers as adjuncts to psychotherapy: use of D-cycloserine in phobic individuals to facilitate extinction of fear.
 Arch Gen Psychiatry. Nov 2004;61(11):1136-1144.
Arch Gen Psychiatry. Nov 2004;61(11):1136-1144. - Pitman RK, Sanders KM, Zusman RM, et al. Pilot study of secondary prevention of posttraumatic stress disorder with propranolol.Biol Psychiatry. Jan 15 2002;51(2):189-192.
- Litz BTWL, Wang J, Bryant R, Engel CC.A therapist-assisted Internet self-help program for traumatic stress. Prof Psychol Res Pr. December 2004;35(6):628-634.
New York State Department of Mental Health expresses thanks to the National Institute of Mental Health for the information, used in this booklet.
Published by the State Department of Mental Health New York, June 2008.
New York State
Andrew M. Cuomo Governor
Mental Health
Head of Department Michael F. Hogan, PhD
For more information about this edition contact:
New York State Office of Mental Health
Community Outreach and Public Education Office
[New York State Division of Mental Health
Public Relations and Community Education Department]
44 Holland Avenue
Albany, NY 12229
866-270-9857 (toll free)
www. omh.ny.gov
omh.ny.gov
For questions and complaints about mental health services Health in New York contact:
New York State Office of Mental Health
Customer Relations
[New York State Division of Mental Health
Customer Service ]
44 Holland Avenue
Albany, NY 12229
800-597-8481 (toll-free)
For information about mental health services in your neighborhood, contact
nearest New York State Department of Mental Health (NYSOMH) regional office:
Western New York Field Office
[Western New York Regional Office]
737 Delaware Avenue, Suite 200
Buffalo, NY 14209
(716) 885-4219
Central New York Field Office
[Central New York Regional Office]
545 Cedar Street, 2nd Floor
Syracuse, NY 13210-2319
(315) 426-3930
Hudson River Field Office
[Hudson River Regional Office]
4 Jefferson Plaza, 3rd Floor
Poughkeepsie, NY 12601
(845) 454-8229
Long Island Field Office
[Long Island Regional Office]
998 Crooked Hill Road, Building #45-3
West Brentwood, NY 11717-1087
(631) 761-2508
New York City Field Office
[NYC Regional Office]
330 Fifth Avenue, 9th Floor
New York, NY 10001-3101
(212) 330-1671
Are the "Afghan syndrome" waiting for all eyewitnesses?
- Claudia Hammond
- BBC Future
Sign up for our 'Context' newsletter to help you understand what's going on.
Image copyright Getty
It is said that psychological trauma, such as that experienced by eyewitnesses to the Parisian satirical magazine Charlie Hebdo, can provoke a stress disorder in anyone. Correspondent BBC Future decided to find out - is not another medical myth in front of us?
Any terrible event - be it a car accident or a natural disaster - can have a significant lasting impact on the human condition. It is generally accepted that post-traumatic stress disorder (PTSD, a severe mental condition, which is often also called "Vietnam syndrome", "Afghan syndrome", "Chechen syndrome" - depending on the war in which those suffering from this disorder participated) can develop in everyone. Therefore, at 1990s Attempts have been made to introduce a mandatory one-time visit to a psychotherapist or participation in a crisis interview for people who have experienced an extreme situation.
(Similar articles from the "Journal" section)
However, the effectiveness of this approach has not been confirmed. Based on the results of a comprehensive analysis of such practices, it was concluded that the mandatory visit to a psychotherapist after receiving a psychological trauma should be abolished, and some experts even state that the "industry of emergencies" advocated such therapy without objective grounds. According to the available information, the claim that PTSD develops in most people is not correct. Moreover, there are other misconceptions in this area.
Based on the results of a comprehensive analysis of such practices, it was concluded that the mandatory visit to a psychotherapist after receiving a psychological trauma should be abolished, and some experts even state that the "industry of emergencies" advocated such therapy without objective grounds. According to the available information, the claim that PTSD develops in most people is not correct. Moreover, there are other misconceptions in this area.
Immediately after a severe event, its eyewitnesses, for quite understandable reasons, go into a state of shock, experience anxiety and fear. What happened takes an important place in their minds, and for several days or weeks they may be tormented by memories, nightmares and a constant sense of danger. Of course, there is little pleasant, but all these feelings are a normal reaction to a situation in which a threat to life arises or a person becomes a witness to the injury or death of other people.
image copyrightGetty
Image caption, The symptoms of PTSD are very real and very scary, but why they don't happen to everyone is still a mystery.
Memories can become so intrusive that they begin to interfere with normal mental activity. Feeling guilty, a person returns to the experience again and again, for example, asking himself the question of what else could have been done to save others. He does his best to avoid any places or actions that remind him of what happened, or even stops responding to the world around him, just to not feel anything. He is constantly on the alert and is frightened even by random passers-by: it is enough to walk past him along the street - and now he is fettered by horror, and his heart is ready to jump out of his chest.
Amazing resilience
Yes, the symptoms of PTSD are very real and very scary. For those who have them, it is important to provide the necessary assistance. But for a diagnosis of PTSD, these symptoms must persist for at least one month after the event and have a negative impact on the victim's work or personal life, or prevent him from doing what he loves.
It should be noted that for most people, these symptoms gradually resolve, so PTSD is actually not as common as one might expect. Even such extreme situations as war do not have a significant impact on most people. For example, only 4% of British servicemen who returned from Iraq developed PTSD (among those who took part in the hostilities in Iraqi territory, this figure was 6.9%). Among the military reserve, symptoms of PTSD appeared on average in 6% of people. According to the researchers, this may be due to the fact that, having returned to their former life "in civilian life", the former military are forced to cope with their problems alone, while active military personnel are among their colleagues who know firsthand what war is.
Image copyright, Getty
Image caption,Not everyone has symptoms of PTSD, even survivors of a terrible tragedy
Attacks on civilians also do not cause PTSD in most people. A study of more than 10,000 people, including police and construction workers who assisted victims of the September 11, 2001 attacks, found that 75% of eyewitnesses had no lasting impact from the events.
True, sometimes the symptoms may appear later. Approximately 8.5% of study participants developed problems after a significant time. There are even cases when servicemen who took part in the Second World War returned home in a seemingly normal condition, worked all their lives as if nothing had happened, and in retirement they suddenly began to be overcome by difficult memories and nightmares again.
Experience from Norway
I went to Norway and met survivors of the tragedy that happened on the Norwegian island of Utøya in 2011. On that terrible day, a terrorist shot 69 youth camp participants; many witnessed the killings. Some managed to hide in the toilets - they sat there for three hours, knowing that the killer was wandering around and looking for new victims.
Immediately after this event, Atle Dyuregrove, director of the Center for Crisis Psychology in Bergen, Norway, stated that he estimated that 30-50% of eyewitnesses would develop serious psychological problems, including PTSD.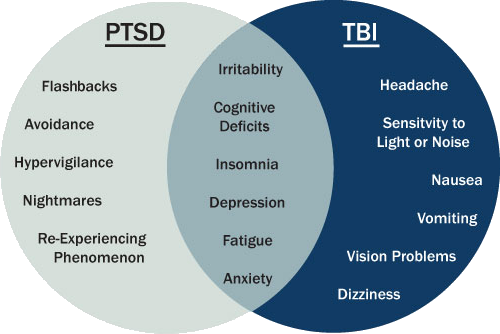 And although in the end the maximum value of the range he named turned out to be correct, all the same, half of the participants in the tragedy, who saw the death of their friends and fled to save their lives, were able to somehow recover from the shock.
And although in the end the maximum value of the range he named turned out to be correct, all the same, half of the participants in the tragedy, who saw the death of their friends and fled to save their lives, were able to somehow recover from the shock.
Image copyright, Getty
Image caption,About half of the survivors of the 2011 Utøya youth shootings experienced long-term psychological problems, including PTSD
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it is important and what will happen next.
episodes
The End of the Story Podcast
The tragedy happened during the summer holidays, and most of the children had to transfer to new schools in the fall, which complicated the situation. But the country has already developed a plan of action in such circumstances caused by a natural disaster or a crime, and support was provided to eyewitnesses of the events. The staff of each school where victims of psychological trauma studied were instructed on the procedure, and strict attendance requirements were relaxed for the children. They were also offered the opportunity to choose when and how to tell their new classmates what had happened.
But the country has already developed a plan of action in such circumstances caused by a natural disaster or a crime, and support was provided to eyewitnesses of the events. The staff of each school where victims of psychological trauma studied were instructed on the procedure, and strict attendance requirements were relaxed for the children. They were also offered the opportunity to choose when and how to tell their new classmates what had happened.
Some teenagers, wanting to avoid questions, decided to speak to the whole class and share their experiences. Relatives of the dead and the children who survived were given the opportunity to visit the island again at another time, because it was known from the experience of past emergencies that later people begin to perceive the situation a little differently.
This assistance proved to be effective, and now other countries are adopting Norway's experience.
No one is insured?
Another myth about PTSD suggests that only the weak develop symptoms of the disorder. In fact, the reason why, even after the most terrible events, PTSD does not manifest itself in everyone, is still a mystery.
In fact, the reason why, even after the most terrible events, PTSD does not manifest itself in everyone, is still a mystery.
Until recently, the Handbook of American Psychiatrists, The Diagnostic and Statistical Manual of Mental Disorders, outlined people's reactions to the event itself. Strong fear, helplessness, or dread were thought to be precursors to PTSD, but these signs had to be omitted from the latest edition because it was found that they did not tell who would develop the condition and who would not.
Of course, the reaction of the psyche also depends on the nature of the event itself. Thus, in the US armed forces, the prevalence of PTSD is almost three times higher than in the UK - partly due to the fact that there are more reserve soldiers, but also because the duration of service is a year, not half a year, as in the UK. According to numerous studies conducted after the September 11, 2001 attacks among those who worked in the Twin Towers, people who were most likely to develop PTSD were observed in people who were injured, were on the top floors, saw others fall or jump off buildings, as well as those whose employers died as a result of the tragedy.
But the same goes for women, young people, low-paid workers and those who have faced other crises in previous years. Thus, the development of PTSD is determined by a number of different factors.
Image copyright, Getty
Image caption,Police and military are the most obvious victims of PTSD, but they are also the most prepared for stressful situations. They also get PTSD. Dozens of studies conducted among displaced children were analyzed to identify factors contributing to the condition. Naturally, violence was one of the factors, but guessing who is at risk for developing PTSD is still not easy, and even the amount of psychological trauma inflicted on a child is not an indicator.
In addition to risk factors, there are those that contribute to the resilience of victims and protect them from the development of PTSD. Family and colleagues can help a lot.
But these signs do not allow you to accurately determine who is at risk.