Lyme disease psychosomatic
The Unfortunate Connection Between Lyme Disease and Mental Illness
Medically reviewed by Scientific Advisory Board — By Christine Hammond, MS, LMHC on July 25, 2019
Carol has been a patient of mine for over five years. We have walked through some of the most difficult times in her life as she dealt with her failing marriage and then divorce, a move, significant career changes, undiagnosed medical issues, and co-parenting teenagers.
Yet during our discussions, there was an undercurrent of, I dont feel right. Her feelings were understandable given her life circumstances. But when life settled down, her complaints of pain, stress, fogginess, anxiety, and depression intensified. One medical doctor after the other ran tests with no conclusive diagnosis so she was labeled psychosomatic.
But that didnt make sense given that fact that she was consistent in therapy, did what was asked, and had significant improvements in several areas of her life. Something else seemed to be wrong. Finally, she found a doctor who tested her for Lyme disease, and she was properly diagnosed.
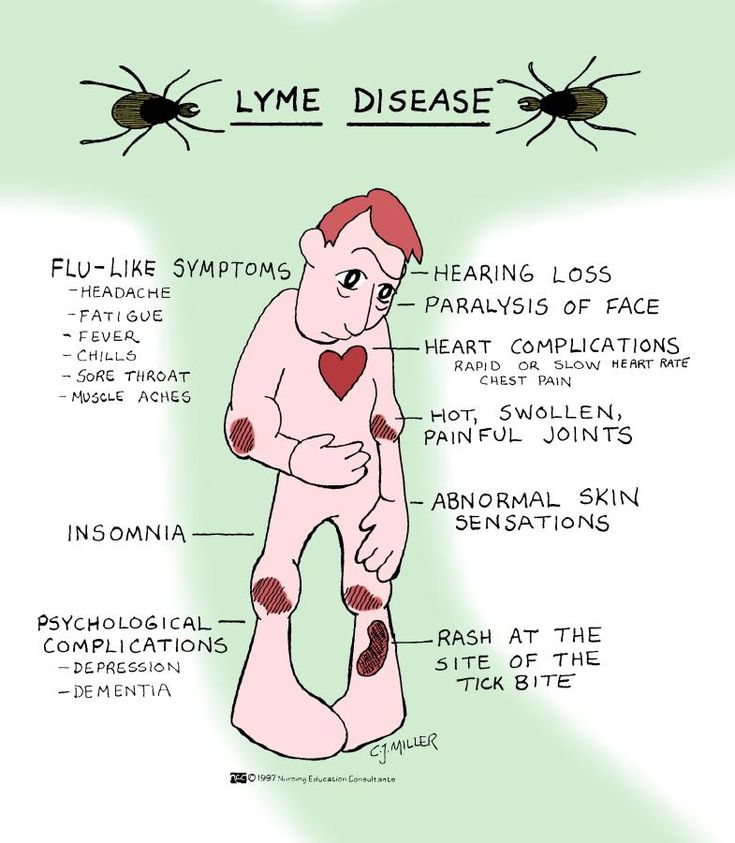
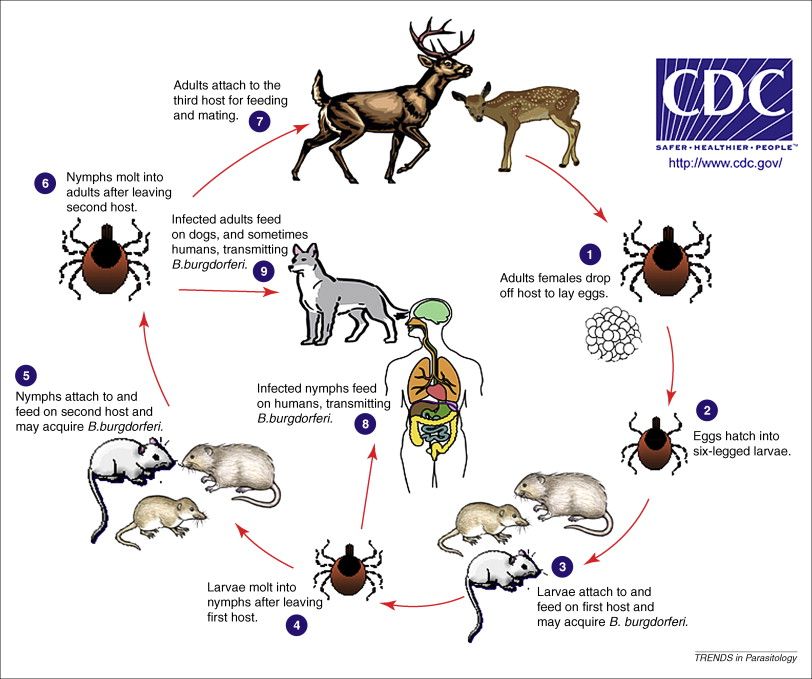
What is Lyme Disease? Lyme disease is aninfectious diseasecaused by abacteriaand spread byticks resulting in a suppression of the immune system. It can develop into a chronic multisystemic illness affecting the nervous system causing neurologic and psychiatric symptoms. These symptoms can mimic paranoia, dementia, schizophrenia, bipolar, panic attacks, depression, eating disorders, and obsessive-compulsive behaviors.
This explained everything. It was as if all the random pieces of a puzzle were put together for Carol. The problem is that the diagnosis doesnt solve the problem, it only identifies it. Counselors and therapists need to differentiate between atypical psychiatric disorders and those associated with having Lyme disease in order to properly treat their clients. Here are some other misconceptions about Lyme disease and mental illness.
- Often called psychosomatic.
 When a patient is improperly diagnosed or not diagnosed at all, some physicians deem their condition to be psychosomatic. This is a mischaracterization of psychosomatic disorders. Lyme pain is real, not imagined. Often, patients lose their health, livelihoods, relationship, home, and dignity in the process of getting diagnosed. This is not due to an improper coping mechanism or a cognitive manifestation of emotional stress. Never tell a Lyme patient that what they feel is not real.
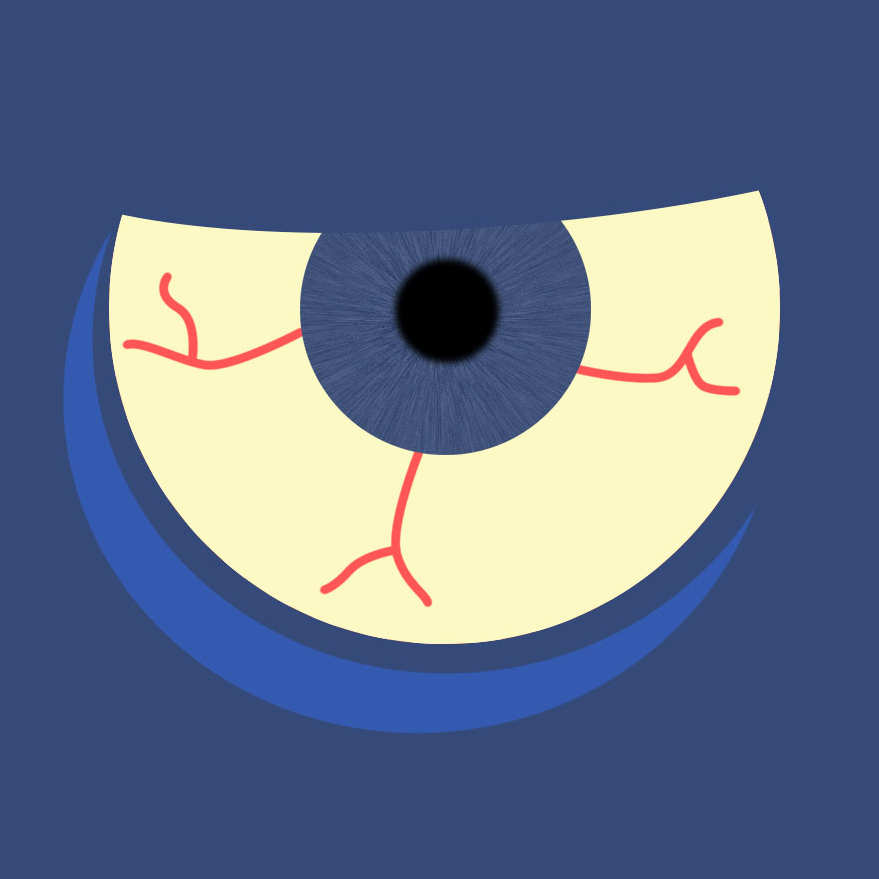
When a patient is improperly diagnosed or not diagnosed at all, some physicians deem their condition to be psychosomatic. This is a mischaracterization of psychosomatic disorders. Lyme pain is real, not imagined. Often, patients lose their health, livelihoods, relationship, home, and dignity in the process of getting diagnosed. This is not due to an improper coping mechanism or a cognitive manifestation of emotional stress. Never tell a Lyme patient that what they feel is not real. - Neuropsychiatric symptoms are prominent. Lyme patients tend to have trouble with mood regulation, cognition, energy, sensory processing, and/or sleep. This can manifest into paranoia, hallucinations, mania, and/or obsessive-compulsive behaviors. Memory loss and concentration issues mirror other psychological disorders. This might make a patient look like they are in the early stages of dementia, have attention-deficit, or a traumatic brain injury. Sensory processing issues such as sensitivity to lights and sounds are also typical.
 This results in avoiding daylight, staying at home, avoiding crowned areas such as stores, parks, or restaurants.
This results in avoiding daylight, staying at home, avoiding crowned areas such as stores, parks, or restaurants. - Often misdiagnosed. Lyme disease looks like other neurological conditions and sometimes is misdiagnosed as chronic fatigue or fibromyalgia. Patients experience extreme fatigue despite sleeping for 10-12 hours a night and/or napping. When they push through one day, they may need 2-3 days of taking it easy to fully recover. The misdiagnosis is frustrating for the patients because it slows down proper treatment.
- Lyme can resemble Alzheimers. Unfortunately, Lyme disease looks like the early phases of Alzheimers with rage, short-term memory loss, personality changes, a slower speed of thinking, difficulty remembering words or names, and impaired fine motor control such as buttoning a shirt. This misdiagnosis has devastating consequences as often Alzheimers patients are placed in assisted living or locked nursing homes.
- Anxiety and panic attacks are side effects.
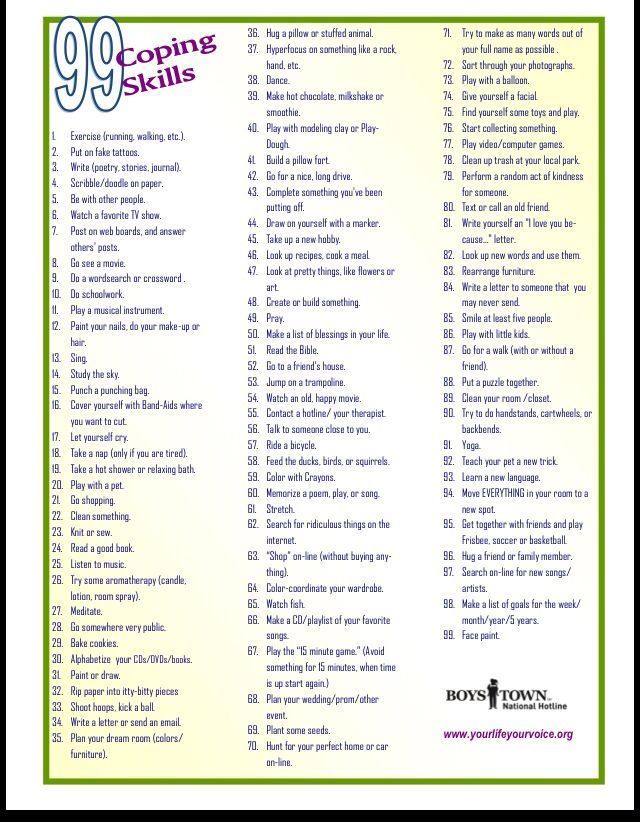
 Having been told by doctors that what they are feeling is a figment of their imagination, Lyme patients naturally develop anxious thoughts. In addition, some of the medical treatments for Lyme can have a side effect of increased anxiety. Left unchecked, this manifests into panic attacks. Further left alone, turns into paranoid thoughts, actions, and phobias. Many become fearful of the attacks and therefore isolate from social gatherings.
Having been told by doctors that what they are feeling is a figment of their imagination, Lyme patients naturally develop anxious thoughts. In addition, some of the medical treatments for Lyme can have a side effect of increased anxiety. Left unchecked, this manifests into panic attacks. Further left alone, turns into paranoid thoughts, actions, and phobias. Many become fearful of the attacks and therefore isolate from social gatherings. - Brain fog looks like abuse fog. Because Lyme disease can affect the brain, patients often look like they are not thinking clearly. This mimics abuse fog which occurs when a person is being abused. Thoughts tend to be hopeless, distorted, and disorganized. Patients are unable to concentrate, to comprehend during reading, have memory issues, and poor mental clarity. Everyday tasks can become more difficult including participating in therapy.
- Depression is common. All chronic illnesses potentially cause major depression due to the recurrent nature of the disease.
 Depression can range from moderate to severe levels and occurs in approximately 60% of patients. Feelings of being moody and irritable are common. Inflammation, pain, interpersonal stressors, economic loss, and a sense of doom contribute to the severity of the depression. Typical depression remedies do not work on Lyme patients. Therapy is very helpful as are support groups with other Lyme patients.
Depression can range from moderate to severe levels and occurs in approximately 60% of patients. Feelings of being moody and irritable are common. Inflammation, pain, interpersonal stressors, economic loss, and a sense of doom contribute to the severity of the depression. Typical depression remedies do not work on Lyme patients. Therapy is very helpful as are support groups with other Lyme patients. - Psychological ramifications are untreated. Most therapists are not aware of the damaging effects of a long-term chronic illness like Lyme disease and as a result, fail to properly diagnose. As a result, some Lyme patients are unnecessarily hospitalized in mental facilities. This further increases the existing social isolation done by friends, family, and community which contribute to feelings of loss.
- Increase in suicidal and suicide. Living with Lyme disease is hard and debilitating. Friends and family rarely comprehend the magnitude of the disease resulting in a feeling of isolation.
 Discouragement, fear, helplessness, frustration, loss, grief, and loneliness are a result. As the disease progresses and mobility or cognitive functioning decreases, suicidal ideation increases. Some, seeing no way out, do unfortunately take their own lives.
Discouragement, fear, helplessness, frustration, loss, grief, and loneliness are a result. As the disease progresses and mobility or cognitive functioning decreases, suicidal ideation increases. Some, seeing no way out, do unfortunately take their own lives.
Lyme patients often feel abandoned by the medical community, friends, and family members. It is imperative that therapists be sensitive to this and not contribute these feelings whether by accident in misdiagnosis of other mental illnesses or more intentional by not being empathetic to a person suffering from a chronic illness.
If you or someone you know is struggling, please reach out for assistance. The national suicide prevention lifeline is 800-273-8255 or www.suicidepreventionlifeline.org.
Lyme disease: a neuropsychiatric illness
Save citation to file
Format: Summary (text)PubMedPMIDAbstract (text)CSV
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Add to My Bibliography
- My Bibliography
Unable to load your delegates due to an error
Please try again
Your saved search
Name of saved search:
Search terms:
Test search terms
Email: (change)
Which day? The first SundayThe first MondayThe first TuesdayThe first WednesdayThe first ThursdayThe first FridayThe first SaturdayThe first dayThe first weekday
Which day? SundayMondayTuesdayWednesdayThursdayFridaySaturday
Report format: SummarySummary (text)AbstractAbstract (text)PubMed
Send at most: 1 item5 items10 items20 items50 items100 items200 items
Send even when there aren't any new results
Optional text in email:
Create a file for external citation management software
Full text links
Atypon
Full text links
Review
. 1994 Nov;151(11):1571-83.
1994 Nov;151(11):1571-83.
doi: 10.1176/ajp.151.11.1571.
B A Fallon 1 , J A Nields
Affiliations
Affiliation
- 1 Department of Psychiatry, College of Physicians and Surgeons, Columbia University, New York.
- PMID: 7943444
- DOI: 10.1176/ajp.151.11.1571
Review
B A Fallon et al. Am J Psychiatry. 1994 Nov.
. 1994 Nov;151(11):1571-83.
doi: 10. 1176/ajp.151.11.1571.
1176/ajp.151.11.1571.
Authors
B A Fallon 1 , J A Nields
Affiliation
- 1 Department of Psychiatry, College of Physicians and Surgeons, Columbia University, New York.
- PMID: 7943444
- DOI: 10.1176/ajp.151.11.1571
Abstract
Objective: Lyme disease is a multisystemic illness that can affect the central nervous system (CNS), causing neurologic and psychiatric symptoms. The goal of this article is to familiarize psychiatrists with this spirochetal illness.
Method: Relevant books, articles, and abstracts from academic conferences were perused, and additional articles were located through computerized searches and reference sections from published articles.
Results: Up to 40% of patients with Lyme disease develop neurologic involvement of either the peripheral or central nervous system. Dissemination to the CNS can occur within the first few weeks after skin infection. Like syphilis, Lyme disease may have a latency period of months to years before symptoms of late infection emerge. Early signs include meningitis, encephalitis, cranial neuritis, and radiculoneuropathies. Later, encephalomyelitis and encephalopathy may occur. A broad range of psychiatric reactions have been associated with Lyme disease including paranoia, dementia, schizophrenia, bipolar disorder, panic attacks, major depression, anorexia nervosa, and obsessive-compulsive disorder.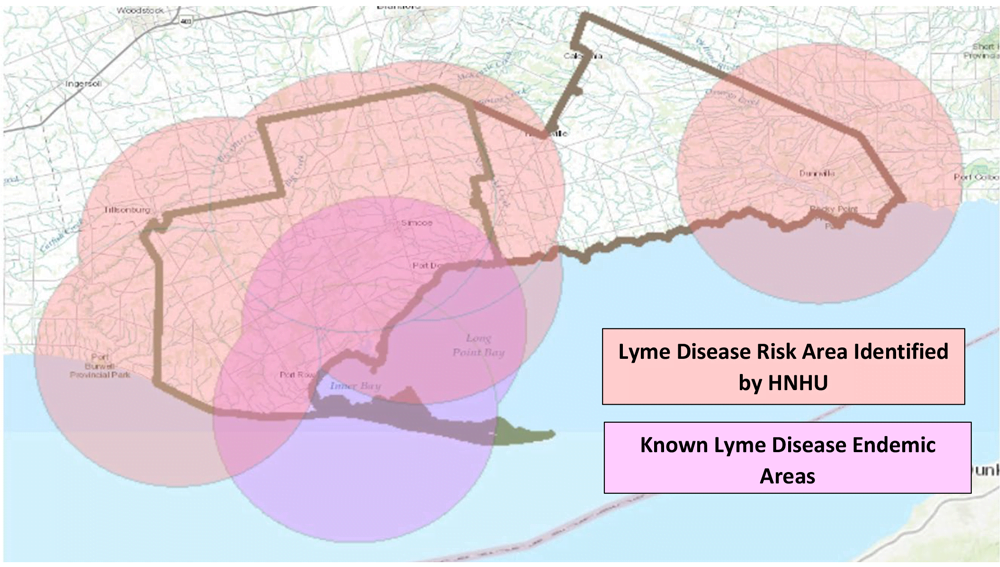 Depressive states among patients with late Lyme disease are fairly common, ranging across studies from 26% to 66%. The microbiology of Borrelia burgdorferi sheds light on why Lyme disease can be relapsing and remitting and why it can be refractory to normal immune surveillance and standard antibiotic regimens.
Depressive states among patients with late Lyme disease are fairly common, ranging across studies from 26% to 66%. The microbiology of Borrelia burgdorferi sheds light on why Lyme disease can be relapsing and remitting and why it can be refractory to normal immune surveillance and standard antibiotic regimens.
Conclusions: Psychiatrists who work in endemic areas need to include Lyme disease in the differential diagnosis of any atypical psychiatric disorder. Further research is needed to identify better laboratory tests and to determine the appropriate manner (intravenous or oral) and length (weeks or months) of treatment among patients with neuropsychiatric involvement.
Similar articles
-
[Signs and significance of a tick-bite: psychiatric disorders associated with Lyme disease].
Sno HN.
 Sno HN. Tijdschr Psychiatr. 2012;54(3):235-43. Tijdschr Psychiatr. 2012. PMID: 22422416 Review. Dutch.
Sno HN. Tijdschr Psychiatr. 2012;54(3):235-43. Tijdschr Psychiatr. 2012. PMID: 22422416 Review. Dutch. -
Nervous system Lyme disease.
Halperin JJ. Halperin JJ. Vector Borne Zoonotic Dis. 2002 Winter;2(4):241-7. doi: 10.1089/153036602321653824. Vector Borne Zoonotic Dis. 2002. PMID: 12804165 Review.
-
Psychiatric manifestations of Lyme borreliosis.
Fallon BA, Nields JA, Parsons B, Liebowitz MR, Klein DF. Fallon BA, et al. J Clin Psychiatry. 1993 Jul;54(7):263-8. J Clin Psychiatry. 1993. PMID: 8335653
-
Borrelia burgdorferi in the nervous system: the new "great imitator".
Pachner AR. Pachner AR. Ann N Y Acad Sci. 1988;539:56-64. doi: 10.1111/j.1749-6632.1988.tb31838.x. Ann N Y Acad Sci. 1988. PMID: 3190104
-
Neuro-ophthalmic manifestations of Lyme disease.
Balcer LJ, Winterkorn JM, Galetta SL. Balcer LJ, et al. J Neuroophthalmol. 1997 Jun;17(2):108-21. J Neuroophthalmol. 1997. PMID: 9176782 Review.
See all similar articles
Cited by
-
Neurological Pain, Psychological Symptoms, and Diagnostic Struggles among Patients with Tick-Borne Diseases.
Maxwell SP, Brooks C, McNeely CL, Thomas KC. Maxwell SP, et al. Healthcare (Basel). 2022 Jun 23;10(7):1178. doi: 10.3390/healthcare10071178. Healthcare (Basel).
 2022. PMID: 35885705 Free PMC article.
2022. PMID: 35885705 Free PMC article. -
Lyme Neuroborreliosis Presenting as Multiple Cranial Neuropathies.
Sriram A, Lessen S, Hsu K, Zhang C. Sriram A, et al. Neuroophthalmology. 2021 Jul 23;46(2):131-135. doi: 10.1080/01658107.2021.1951769. eCollection 2022. Neuroophthalmology. 2021. PMID: 35273419 Free PMC article.
-
Borrelia burgdorferi Co-Localizing with Amyloid Markers in Alzheimer's Disease Brain Tissues.
Senejani AG, Maghsoudlou J, El-Zohiry D, Gaur G, Wawrzeniak K, Caravaglia C, Khatri VA, MacDonald A, Sapi E. Senejani AG, et al. J Alzheimers Dis. 2022;85(2):889-903. doi: 10.3233/JAD-215398. J Alzheimers Dis. 2022. PMID: 34897095 Free PMC article.
-
Anorexia Nervosa Caused by Polymicrobial Tick-Borne Infections: A Case Study.
Kinderlehrer DA. Kinderlehrer DA. Int Med Case Rep J. 2021 May 10;14:279-287. doi: 10.2147/IMCRJ.S311516. eCollection 2021. Int Med Case Rep J. 2021. PMID: 34007219 Free PMC article.
-
Symptom heterogeneity and patient subgroup classification among US patients with post-treatment Lyme disease: an observational study.
Rebman AW, Yang T, Aucott JN. Rebman AW, et al. BMJ Open. 2021 Jan 13;11(1):e040399. doi: 10.1136/bmjopen-2020-040399. BMJ Open. 2021. PMID: 33441353 Free PMC article.
See all "Cited by" articles
Publication types
MeSH terms
Full text links
Atypon
Cite
Format: AMA APA MLA NLM
Send To
''Lyme disease or it seems'': the fear of ticks continues among the population | Diseases and treatment
Acarophobia and "borreliophobia" among the population does not subside, so I decided to write this post.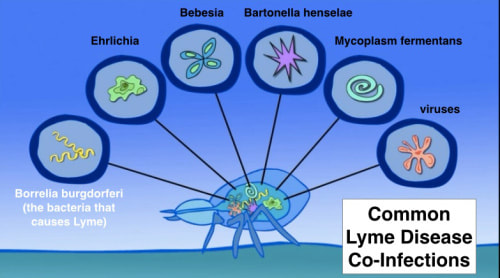 I have been planning for a long time, but now I was inspired to this action by the comment of one patient, which I quote below in full.
I have been planning for a long time, but now I was inspired to this action by the comment of one patient, which I quote below in full.
Indeed, friends, our world is becoming more and more virtual, access to any kind of information is simply fantastic, sometimes it seems - well, I listened to professional information, read it, and already know everything about this or that problem. Forgetting that we know a lot, but we don’t know even more, and I always adhere to the iron rule in medicine - do no harm. Because there are more and more opportunities for us, doctors, to harm our patients every year. In my various lectures, I pay a lot of attention to such issues and try to explain what I mean by saying that the human body is an excellent self-regulating system and our main task in the treatment of infectious patients is not to interfere with the patient to get sick properly. Or get well. You also need to heal properly.
Video of the day
But back to ticks and Lyme borreliosis.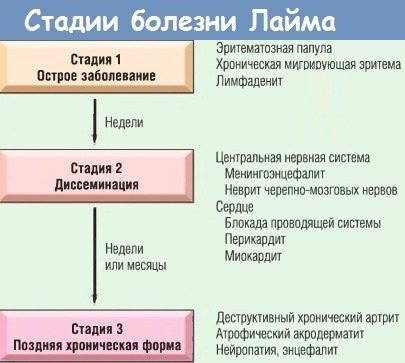 Of course, in my long medical practice there were different cases. Here is one patient before the New Year fell at home, going down the stairs from the second floor, lost consciousness, on MRI - foci, through a whole investigation, they found an appeal to a dermatologist six months before this episode about a red spot on her leg, Lyme was confirmed, cured, everything went away without a trace, it was ten years ago, the case was published. And recently, an elderly man with not very specific symptoms was also diagnosed with Lyme, and was also diagnosed with infectious-toxic myocarditis, which he had no idea about. A young girl who lost consciousness on the street due to A-V blockade of the 3rd degree and was hospitalized in cardiology, also after an appropriate diagnosis, underwent a long course of therapy with complete remission, which has been lasting for three years, we also published this case. Etc.
Of course, in my long medical practice there were different cases. Here is one patient before the New Year fell at home, going down the stairs from the second floor, lost consciousness, on MRI - foci, through a whole investigation, they found an appeal to a dermatologist six months before this episode about a red spot on her leg, Lyme was confirmed, cured, everything went away without a trace, it was ten years ago, the case was published. And recently, an elderly man with not very specific symptoms was also diagnosed with Lyme, and was also diagnosed with infectious-toxic myocarditis, which he had no idea about. A young girl who lost consciousness on the street due to A-V blockade of the 3rd degree and was hospitalized in cardiology, also after an appropriate diagnosis, underwent a long course of therapy with complete remission, which has been lasting for three years, we also published this case. Etc.
But, dear colleagues and patients, we must remember that the modern complex world with its flow of information (sometimes completely superfluous for a particular patient, remember the rule - the main thing is not to google your illness), instability that makes one doubt tomorrow, lack of sleep and various stresses (acute, chronic) - this is all that can cause a PSYCHOSOMATIC state - a special reaction of the body, expressed in the appearance of absolutely real symptoms in the mind of the patient. And in the problem of Lyme borreliosis and pseudo Lyme borreliosis, the presence of psychosomatics is very obvious. In addition, it must be admitted that today there is no generally accepted consensus on the management of such patients, especially chronic forms, the approaches of different associations and organizations are very different both in terms of diagnosis and treatment, the problem of co-infections in Lyme has not been solved, and, finally, no clear criteria for cure. All this invariably gives rise to rumors, abuses, gives reason to refer to particular cases, opinions that can in no way be an absolute statement on this issue. All this only exacerbates the panic among patients and potential patients who are trying to figure out the most difficult problem of this spirochetosis on their own. And once again, this does not at all underestimate the very problem of borreliosis, in no way simplifies or belittles it.
And in the problem of Lyme borreliosis and pseudo Lyme borreliosis, the presence of psychosomatics is very obvious. In addition, it must be admitted that today there is no generally accepted consensus on the management of such patients, especially chronic forms, the approaches of different associations and organizations are very different both in terms of diagnosis and treatment, the problem of co-infections in Lyme has not been solved, and, finally, no clear criteria for cure. All this invariably gives rise to rumors, abuses, gives reason to refer to particular cases, opinions that can in no way be an absolute statement on this issue. All this only exacerbates the panic among patients and potential patients who are trying to figure out the most difficult problem of this spirochetosis on their own. And once again, this does not at all underestimate the very problem of borreliosis, in no way simplifies or belittles it.
At the present time I am trying to systematize all the currently available knowledge on this issue of various specialists, schools, incl.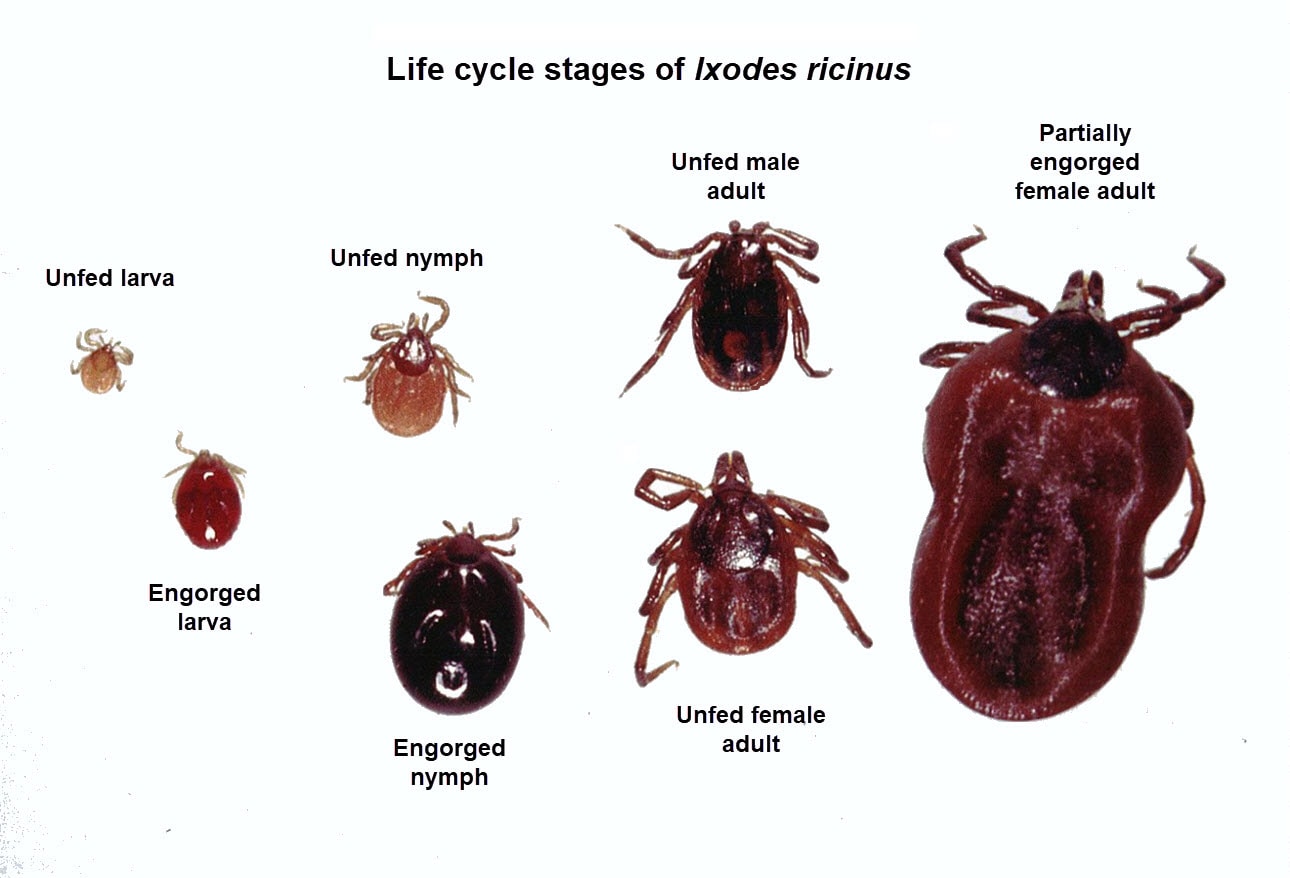 and ours, and I will try to present all this in the form of an appropriate lecture and publications.
and ours, and I will try to present all this in the form of an appropriate lecture and publications.
And this message of mine is aimed at, firstly, focusing on this problem, showing that it exists, and if your doctor considers it necessary in ANY CASE to undergo appropriate treatment or talk to a psychologist, it is better to follow his recommendations. No need to be offended, offended, doubt and resist. No need to take endless tons of tests, most of which are uninformative, fantastic, and sometimes just ridiculous. Of course, if you trust the doctor. But it shouldn't be otherwise. There are always three participants in the battle with the disease (the disease, the patient and the doctor), and we, dear patients, are always on your side.
Text from the forum:
"Reading this forum 3 years after my Lime.
My opinion will not be popular on this forum, but I really want to convey it to the author of the topic and many other "seekers" of infection and so on.
3 years ago I was bitten by a tick in the Moscow region. I didn’t particularly betray this value, I just threw it out and that’s it.
I didn’t particularly betray this value, I just threw it out and that’s it.
Then I don't know why, I got into the Internet and came across this forum...
Oh... if I had known in advance, I wouldn't have wasted a year of my life...
I read the information from this forum, my hair stood on end ... it turns out that I can get a terrible, "incurable" disease and suffer all my life ... And they don’t diagnose it in Russia, I have to go to Germany or Poland and be treated for all types of infection. ..
After reading all this, I decided to take my temperature, and miraculously, it turned out to be 37.3...
Exactly, this is it, I thought....
Then I learned that tests should be taken after 3 weeks, earlier they are not indicative ...
During these 3 weeks I have already re-read the entire forum and planned treatment abroad....
After 3 weeks I passed the tests: the result. ELISA-negative, immunochip positive for G (as many as 4 positions) and doubtful for M (1 position)
Then there was a panic, an appointment with the doctor, who was "alarmed" but said that according to such analyzes, she could not deliver Borreliosis and advised me to take an analysis in Germany.
Further tests in Germany: result. ELISA negative and their main analysis, I don't remember what it's called, with results of +2, +2 for borrelia.
Then there is 100% confidence in the disease... A letter to a Polish doctor with a description of the symptoms and test results, an absentee assumption of the Polish doctor about the presence of the disease and an offer to come to see him...
-
Now about my symptoms:
-
Temperature 37-37.2 every day.
-
Sweating, sometimes sweating.
-
Twitching all over the body, in different places, many times during the day.
-
Sleep disorders, insomnia.
-
"Fog in the head"
-
Self -gait, derealization
-
depressed moral condition, depression
-
a month after the bite, stains throughout the body
-
pain in the limbs
-
Facial numbness
-
Subjective visual impairment
How do you like this set of symptoms, coupled with positive tests? Borreliosis, right? Also, coupled with KO infections for sure . ..
..
My husband also got sick... having read about the sexual transmission of Lyme, I dragged him for tests... and, miraculously, my husband has a positive immunochip for G and a dubious one for M... Now my husband also has lime, for sure...
The condition was simply terrible... the doctor prescribed antibiotics "for prophylaxis", 21 days of antibiotics, the condition does not improve... I constantly sit on the forum and I feel worse. Relatives twist their fingers to their temples, doctors send them to a psychiatrist ... but I know, they say on the forum that our doctors are stupid, they don’t understand anything ... We have to wait for Poland .... Familiar, right? More pain in the joints... palpable...
My husband almost forcibly made an appointment with a psychiatrist... went... kind uncle, talked to me, prescribed antidepressants... diagnosed me with an endogenous anxiety-depressive disorder. His words sunk into my head that every second of his patients has the same symptoms . .. At that moment I thought that he could understand! ?? I’m normal, I haven’t gone crazy, I just have Lyme and CO infections...
.. At that moment I thought that he could understand! ?? I’m normal, I haven’t gone crazy, I just have Lyme and CO infections...
My husband made me take pills and, lo and behold... A week later, sleep returned, anxiety disappeared, but other symptoms remained... After 2- For 3 weeks the twitches, pains in the limbs, numbness were gone... there was derealization, unsteadiness... I stopped sitting on the forum and measuring my temperature. After 3 months, all the symptoms completely disappeared and I became my former self ... I drank pills for half a year ... I got off them a long time ago and live a normal life, as before ... "
Now imagine: all the symptoms point to Lyme, and even some tests are positive... 100% in Poland and Germany would start treatment... If I had not taken the pills, the symptoms would not have gone away, I would have been treated indefinitely, the family would only work to pay for the clinic... And the Polish and German doctors would receive money from me, make smart faces and continue to treat me. ..
..
find a normal psychotherapist and drink antidepressants... If you suddenly feel better, you may not have to look further for something that may not be there...
I think most of the participants will throw stones at me) But still... Think critically: almost all of my and your acquaintances were bitten by ticks at least 1-2 times in their lives... how many of them are sick? 3 years ago I was 100% sure that I was sick with Lyme, and everyone around is idiots and they don’t understand me) The result is that the tick bit, Lyme is gone, the neurosis is cured. The neurosis is caused by an abundance of information and destructive allegations about the worldwide "Lyme Conspiracy" about the uniqueness and incurability of the disease..."
Important: the opinion of the editors may differ from the author's. The editors of the site are not responsible for the content of blogs, but strive to publish different points of view. More detailed about the editorial policy of OBOZREVATEL PAN .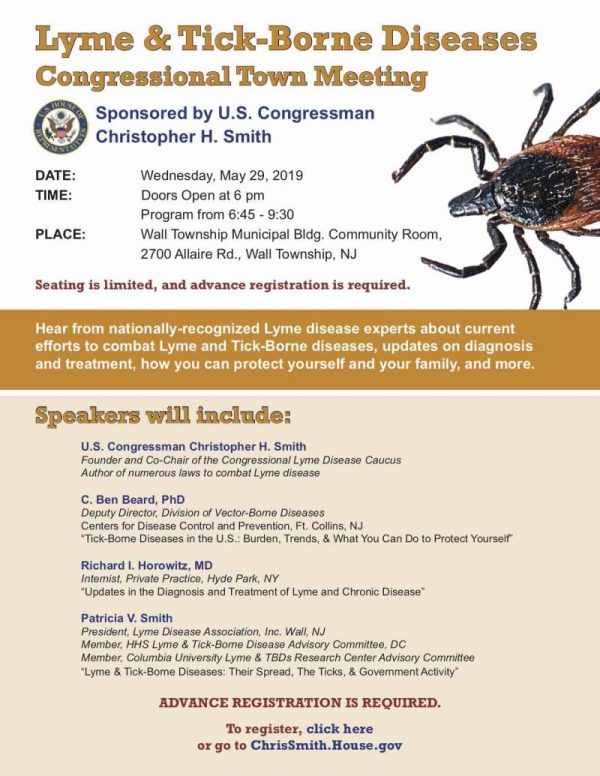 ..
..
do not rake up from the tick: what is the dangerous borreliosis and how to understand that
Komsomolskaya Pravda
Health and Health
Anna Kukartseva May
9000, May 1922 14:15as According to statistics, there are still few bitten by ticks, but nevertheless, Rospotrebnadzor experts warn that Lyme disease can be very dangerous if treatment is not started on time
The faster you notice and remove the tick, the higher the chance that dangerous pathogens will not have time to enter the body. Photo: Nikolai OBEREMCHENKO
June. But isolated cases were registered even in March. Basically, arthropods live in the areas closest to the capital - they traditionally attack the territories of the Moscow, Tver, Kaluga, Tula, Vladimir regions. But they are also found in Moscow parks.
WHAT IS LYME DISEASE DANGEROUS
There are almost no ticks carrying dangerous encephalitis in the Moscow region and nearby regions. But there are many ticks infected with borrelia - the causative agents of Lyme disease. About one in four ticks are infected with these bacteria. Yes, borreliosis is treated with antibiotics, yes - it is much easier than encephalitis, but this does not mean that it is a harmless disease.
But there are many ticks infected with borrelia - the causative agents of Lyme disease. About one in four ticks are infected with these bacteria. Yes, borreliosis is treated with antibiotics, yes - it is much easier than encephalitis, but this does not mean that it is a harmless disease.
Here are some important points that the leading expert of the CMD Center for Molecular Diagnostics of the Central Research Institute of Epidemiology of Rospotrebnadzor reminded Mikhail Lebedev:
1. An imperceptible beginning.
The main danger of borreliosis is that you will not realize that you are sick until the symptoms of an acute period appear (and it may not be) or already serious complications.
The bacterium enters the body through a tick and acts imperceptibly - there is rarely a temperature, sometimes aching muscles.
The only clear sign is a red swelling at the site of the tick bite, often with a white center. Doctors call this erythema annulare. In a few days, it can grow up to 5 cm.
In a few days, it can grow up to 5 cm.
2. May become chronic.
If antibiotic prophylaxis is not carried out in time (preferably in the first few days after the bite), then the disease can “hide” in the body and appear only after a few weeks or even months.
3. Diverse and difficult to diagnose.
Worst of all, the disease has many faces, often mistaken for neurological disorders, even mental (psychosomatic) relapses. Since the bacterium can affect the skin, the heart, and muscles, it is difficult for doctors to understand what is happening to a patient who is not helped by any treatment. And rarely does anyone realize that you need to take an analysis for the presence of antibodies to Borrelia. And the longer the treatment is delayed, the worse the person becomes.
Luckily, Lyme disease can be treated with antibiotics, and with the right therapy, you can almost completely cure a person. But in some cases it is already too late - the central nervous system can be affected and recovery will take a very long time.
Ticks are traditionally more common in Moscow, Tver, Kaluga, Tula, Vladimir regions. But Moscow parks also have them. Photo: Maria LENTS0003
According to Rospotrebnadzor in Moscow, twice as many areas of parks and forest parks have already been treated for ticks this year in the capital than last year. Nevertheless, ticks continue to live in Moscow parks. As of the end of May, a total of 37 ticks attacked people in the forest parks of Moscow. It's official. And how many people chose to remove the parasite from themselves and not carry it anywhere?
According to Rospotrebnadzor, more than 3,000 ticks have been tested in Moscow laboratories this year, about the same number as last year. At the same time, parasites infected with borreliosis at the moment were 2.6 times less.
But that doesn't mean that if you see a tick stuck on you, you don't have to worry. What if you were bitten by an infected person?
- Don't risk it, take it to the laboratory for analysis. Try to remove it carefully so as not to crush it, otherwise the laboratory will not be able to determine whether the tick has been infected. A live tick can be put in a jar, a dead one can be brought on a piece of ice, such studies are also being done in our laboratory, - says Mikhail Lebedev, an expert at the Center for Molecular Diagnostics of the Central Research Institute of Experimental Establishment.
Try to remove it carefully so as not to crush it, otherwise the laboratory will not be able to determine whether the tick has been infected. A live tick can be put in a jar, a dead one can be brought on a piece of ice, such studies are also being done in our laboratory, - says Mikhail Lebedev, an expert at the Center for Molecular Diagnostics of the Central Research Institute of Experimental Establishment.
And remember, the sooner prophylaxis is carried out, the more likely it is that serious complications will bypass you.
IMPORTANT!
Look for a tick where it is soft
Ticks in adults rarely rise above the neck, so look for them below - under the knees, in the groin, where they are warm and soft, and where the skin is thinner. The faster you notice and remove the tick, the higher the chance that dangerous pathogens will not have time to enter the body.
If not immediately available for examination, store in a cool place in a sealed bottle with a damp cloth.
Read also
Age category of the site 18+
EDITOR-IN-CHIEF - NOSOVA OLESIA VYACHESLAVOVNA.
I.O. chief editor of the site - Viktor Fedorovich Kansky
Messages and comments from site readers are posted without preliminary editing. The editors reserve the right to remove them from the site or edit them if the specified messages and comments are an abuse of freedom mass media or violation of other requirements of the law.
JSC "Publishing House "Komsomolskaya Pravda". TIN: 7714037217 PSRN: 1027739295781 127015, Moscow, Novodmitrovskaya d. 2B, Tel. +7 (495) 777-02-82.
Exclusive rights to materials posted on the website www.kp.ru, in accordance with the legislation of the Russian Federation for the Protection of the Results of Intellectual Activity belong to JSC Publishing House Komsomolskaya Pravda, and do not be used by others in any way form without the written permission of the copyright holder.