Insomnia and ocd
How I Stopped Intrusive Thoughts At Night
Today’s story is written by Joe Antonellis, a student-athlete at Pomona College in California. Joe has the kind of enthusiasm about writing that makes you want to sit down and write too, and brings all this passion to his work writing about mental health and personal journeys.
Alone time is the worst. When you are alone, with nobody else there to pull you back into reality, OCD can kick your brain to the curb and grab control of your mind in an instant. Being alone with your obsessions somehow makes them more real, resistant, and powerful, enabling them to ambush you with ease.
When are these anxiety attacks most likely to occur? Right when your mind is meant to be at its quietest and most tranquil: sleep time. Even if you’re with a partner at this time, you’re forced to avoid interacting with them, as it would be rude to risk waking them up. This makes the time right before bed one of the most frightening times for people with OCD, invoking a deep and interesting relationship between the two very opposite factors.
I remember I would always dread going to sleep when I was suffering with OCD in my younger years. I would avoid bedtime, partaking in various other activities to put off the eventual loneliness of sleeping. I was terrified of being alone with my brain, as I didn’t have the confidence to deal with my OCD on my own when no other activity preoccupied me. Some nights it never struck, and I was able to sleep peacefully, but other nights, obsessions lingered until the I heard the birds singing at dawn. This led to a lack of sleep, of course, resulting in a very unhealthy lifestyle, which contributed negatively to my mental health in addition to my struggles with OCD. It’s not like I was distracting myself with beneficial activities either. Most of the time, the late nights were filled with binge eating, mindless TV shows, and violent video games.
In other cases, my bed would be the getaway place I would try to escape to when an obsession came on. Although torturous at times, it could also serve as a safe haven where I knew none of “my ideas” would come to fruition. It was the perfect excuse when I was younger. Whenever an activity or event came up that I knew would trigger my OCD, I could always say I wanted to take a nap or pretend I was sick to try and get out of it. This was just another defense mechanism to avoid the mental barriers instead of busting through them, and “sleeping,” although difficult due to the imminent loneliness associated with it, allowed an easy escape from my fears. As I said above, OCD is not only a mental condition, but an idea that creates fear in the brain, making those afflicted try to avoid confrontation with it at all costs. Sleep and OCD have a significant duality in the effects of the two on each other, which must be explored further.
It was the perfect excuse when I was younger. Whenever an activity or event came up that I knew would trigger my OCD, I could always say I wanted to take a nap or pretend I was sick to try and get out of it. This was just another defense mechanism to avoid the mental barriers instead of busting through them, and “sleeping,” although difficult due to the imminent loneliness associated with it, allowed an easy escape from my fears. As I said above, OCD is not only a mental condition, but an idea that creates fear in the brain, making those afflicted try to avoid confrontation with it at all costs. Sleep and OCD have a significant duality in the effects of the two on each other, which must be explored further.
Imagine you were forced to drink a full cup of coffee before going to bed every night. You would sit there in bed and stare at the ceiling, with distracting thoughts whirling in your mind for hours. You would never get a good night’s sleep this way, and would never feel rested the next day. Now, I’m sure many of you have experienced this feeling after accidentally having caffeine before bed, or when trying to work or study late into the night– but imagine feeling this way every night. This is what it is like for those suffering with OCD. Research has shown that those with OCD have higher than normal rates of insomnia, and even other sleep issues like delayed sleep phase disorder. These issues are shown to be caused by obsessive thoughts, which keep victims up all night, trapped in their thoughts.
Now, I’m sure many of you have experienced this feeling after accidentally having caffeine before bed, or when trying to work or study late into the night– but imagine feeling this way every night. This is what it is like for those suffering with OCD. Research has shown that those with OCD have higher than normal rates of insomnia, and even other sleep issues like delayed sleep phase disorder. These issues are shown to be caused by obsessive thoughts, which keep victims up all night, trapped in their thoughts.
As mentioned before, bedtime is the loneliest part of the day, but also one of the most important times of the day. Sleeping efficiently has many different contributing factors, one of the most important being your “sleep environment.” It takes time every night to get into the ideal sleeping position and get your surroundings all set. This includes factors like outside noise, lighting, bedding, and temperature. If you have OCD, though, one compulsion can disrupt all of this, resetting the sleeping process and delaying your much-needed time in dreamworld. For example, I would often run out of bed to check if the downstairs lights were off, and this alone would set my sleeping process back 20 minutes– assuming I only checked one time. Compulsive behaviors and the obsessive mental processes mentioned above make the ultimate combination standing in the way of a good night’s sleep, but other complexities muddle this process even more.
For example, I would often run out of bed to check if the downstairs lights were off, and this alone would set my sleeping process back 20 minutes– assuming I only checked one time. Compulsive behaviors and the obsessive mental processes mentioned above make the ultimate combination standing in the way of a good night’s sleep, but other complexities muddle this process even more.
Let’s assume that your OCD is taking away an hour’s worth of sleep from your night, at minimum. Whether it’s a constant stream of obsessive thoughts or compulsions, you never get to bed by the time you wanted to. This lack of sleep is not only affecting the sharpness of your brain and the fatigue of your body the next day, though. It’s probably increasing the severity of your OCD as well. Studies have shown that a lack of sleep can cause an increase in the commonality and duration of obsessions the next day. Thus, the relationship between sleep and OCD is not only causal, but by nature circular. First, OCD causes you to lose sleep, then this lack of sleep causes your OCD symptoms to arise more frequently. If you suffer with this OCD-related insomnia, this seemingly exponential relationship can seem very daunting and undefeatable, much like a runaway train, impossible to stop. The first issue is viewing the problem as the entire thousand-ton train. You must stop the train one gear at a time, picking off one little piece any chance you get, in order to stop it. The cycle can be stopped, and the first real step is to truly believe in your mind that it can be, recognizing that it will not be easy but can be done.
First, OCD causes you to lose sleep, then this lack of sleep causes your OCD symptoms to arise more frequently. If you suffer with this OCD-related insomnia, this seemingly exponential relationship can seem very daunting and undefeatable, much like a runaway train, impossible to stop. The first issue is viewing the problem as the entire thousand-ton train. You must stop the train one gear at a time, picking off one little piece any chance you get, in order to stop it. The cycle can be stopped, and the first real step is to truly believe in your mind that it can be, recognizing that it will not be easy but can be done.
When it comes to OCD and sleep, it is best to start off by gaining a few small victories. First, I would like to address the in-bed compulsions that could cause you to wreck your sleeping environment and set back your sleep cycle. Let’s say you feel a strong urge to check something in your house. Getting up and checking it is self-defeating, so the main goal is to not perform the compulsion. If you have strategies that work during the daytime (like counting backwards from 200 by multiples of seven, or observing 10 things in your immediate environment) then you can try those at night too.
Getting up and checking it is self-defeating, so the main goal is to not perform the compulsion. If you have strategies that work during the daytime (like counting backwards from 200 by multiples of seven, or observing 10 things in your immediate environment) then you can try those at night too.
If you don’t have any strategies yet, or they’re not working, distraction is your next best bet. Try something that won’t keep you awake, like journaling, reading, or listening to quiet music. As long as it won’t ultimately be harmful to your health, anything you can come up with will be better than giving in to your compulsions. Try new things, especially if they’re things you’re actually interested in. And don’t be discouraged if things don’t work out too well at first: the goal is improvement, not perfection.
Although reassurance-seeking is not an ideal strategy, and can be another compulsion in itself, in extreme cases the need for sleep might outweigh your OCD treatment goals in the immediate short term. Let’s say you have a final exam tomorrow, and you just can’t get yourself to sleep. Maybe, for one night only, it might make sense to put yourself at ease. For example, if you always have to double-check that the lights are off in the house, a strategy to allow yourself to relax could be taking a picture of the dark room, to reassure yourself on your own without any outside help. Again, reassurance is not a great strategy because it tends to strengthen the obsessive-compulsive circles in the long run. It always feels good to get reassurance in the immediate, but for your long-term recovery it’s important to work on strategies to for diffusion or distraction, not reassurance. But we won’t pretend like there are never nights when it’s better to sacrifice this treatment objective and get some sleep.
Let’s say you have a final exam tomorrow, and you just can’t get yourself to sleep. Maybe, for one night only, it might make sense to put yourself at ease. For example, if you always have to double-check that the lights are off in the house, a strategy to allow yourself to relax could be taking a picture of the dark room, to reassure yourself on your own without any outside help. Again, reassurance is not a great strategy because it tends to strengthen the obsessive-compulsive circles in the long run. It always feels good to get reassurance in the immediate, but for your long-term recovery it’s important to work on strategies to for diffusion or distraction, not reassurance. But we won’t pretend like there are never nights when it’s better to sacrifice this treatment objective and get some sleep.
Although these are steps to help you prevent compulsive behaviors, it is harder to deal with the obsessive thoughts that plague your brain for hours when you’re alone in bed. Meditation practice often helps me in these situations, combined with a form of self-questioning. If you ever find yourself obsessing all night, it is best to start taking deep, slow breaths, trying to focus all your attention on the rising and falling of your chest. This will allow for at least an attempt to clear your mind of the obsession for a moment. Next, after calming down your stream of thought, try to question the validity of the obsession. Why am I thinking this? Why is this important? Do I have to think this? Note that if one of your compulsions is to try to figure out the answer to these questions, this particular strategy probably won’t help you. Otherwise, these questions might help put your obsession in perspective, and perhaps this combination will help you drift off to sleep faster than you previously would have.
If you ever find yourself obsessing all night, it is best to start taking deep, slow breaths, trying to focus all your attention on the rising and falling of your chest. This will allow for at least an attempt to clear your mind of the obsession for a moment. Next, after calming down your stream of thought, try to question the validity of the obsession. Why am I thinking this? Why is this important? Do I have to think this? Note that if one of your compulsions is to try to figure out the answer to these questions, this particular strategy probably won’t help you. Otherwise, these questions might help put your obsession in perspective, and perhaps this combination will help you drift off to sleep faster than you previously would have.
Effective, specialized OCD therapy is here
Learn more
Sleep is the quiet force that allows us to keep living. All humans need it, but much like everything else in the world, everyone’s ability to attain it varies.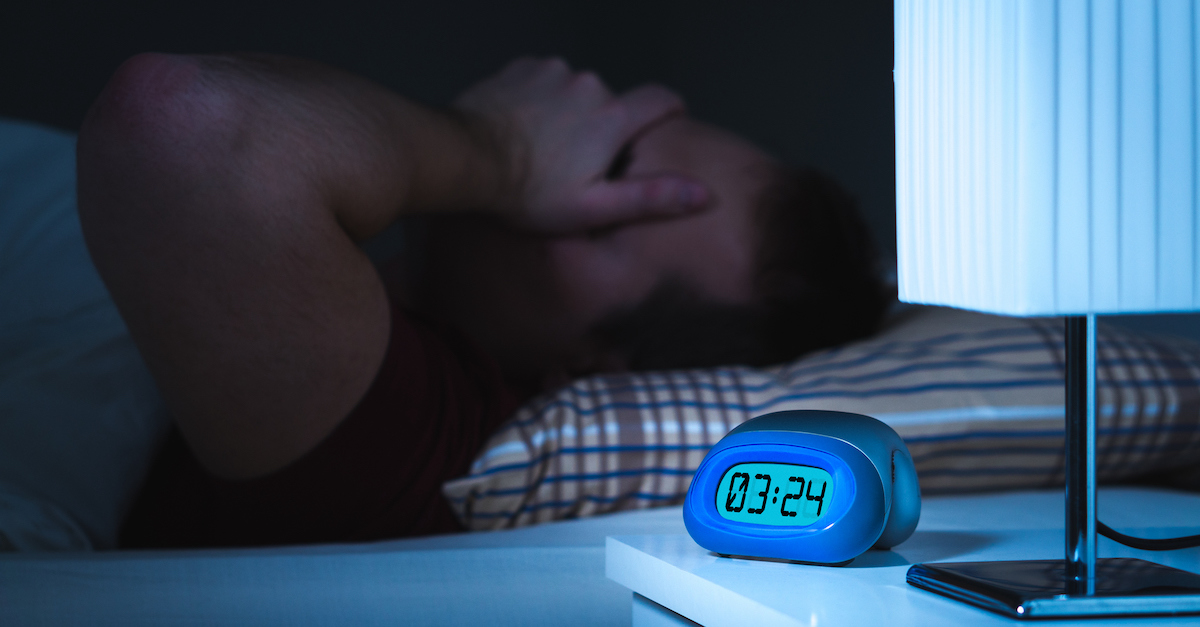 I would like to conclude with Walt Whitman’s famous poem In Midnight’s Sleep, a recount of the horrors he saw in the Civil War, and how they constantly reappeared in his dreams and disrupted him in the middle of the night. I want you all to visualize OCD as a war going on in the mind. Just like in the poem below, there is hope of ending the war, but this hope is not there without the existence of hard-fought battles. This hope is not there without the recognition of beauty in the struggle. And finally, this hope is not there without dreams. I encourage you to keep fighting these battles everyday, no matter how small. Be resilient in your efforts, and be strong, because no matter what you think, it is inside each and every one of you.
I would like to conclude with Walt Whitman’s famous poem In Midnight’s Sleep, a recount of the horrors he saw in the Civil War, and how they constantly reappeared in his dreams and disrupted him in the middle of the night. I want you all to visualize OCD as a war going on in the mind. Just like in the poem below, there is hope of ending the war, but this hope is not there without the existence of hard-fought battles. This hope is not there without the recognition of beauty in the struggle. And finally, this hope is not there without dreams. I encourage you to keep fighting these battles everyday, no matter how small. Be resilient in your efforts, and be strong, because no matter what you think, it is inside each and every one of you.
If you need treatment for OCD, ERP is the most effective form, especially when the therapist conducting the treatment has experience with OCD and training in ERP. At NOCD, all therapists specialize in OCD and receive ERP-specific training. If you are ready to seek treatment, you can schedule a free call with the NOCD clinical team to learn more about how a licensed therapist can help you.
We’re interested in sharing more stories like this one. To talk with us about submitting your story to the NOCD blog, please email [email protected]
And if you’re interested in learning more about the NOCD app, a platform for treating your OCD and finding a community of other people dealing with anxiety disorders, click here.
If you or someone you know is struggling with OCD, you can schedule a free call today with the NOCD clinical team to learn more about how a licensed therapist can help. At NOCD, all therapists specialize in OCD and receive ERP-specific training. ERP is most effective when the therapist conducting the treatment has experience with OCD and training in ERP.
Sleep and OCD: How to Win The Battle for Better Sleep
Most people experience sleepless nights every once in a while. However, research has shown that those with obsessive-compulsive disorder (OCD) have higher-than-normal rates of insomnia. These issues are shown to be caused by obsessive thoughts, which can keep people up all night, trapped in their thoughts. It’s a miserable cycle, and it can be hard to know where to start to improve your restless nights.
These issues are shown to be caused by obsessive thoughts, which can keep people up all night, trapped in their thoughts. It’s a miserable cycle, and it can be hard to know where to start to improve your restless nights.
There isn’t a one-size-fits-all approach to rectifying sleep issues when it comes to OCD, and people should speak with their doctors or OCD therapists to find the best solutions when applicable. However, if you’re looking for ways to improve your sleep quality, here are a few of our best tips for those with OCD.
Practice good sleep hygiene
One of the first steps in getting a better night’s sleep while navigating OCD is practicing good sleep hygiene. We don’t mean brushing your teeth or washing your face — though these are important rituals too.
Sleep hygiene refers to the patterns you build around your sleep habits. For example, it’s important to try to go to bed and wake up at around the same times on a regular basis. You can do this using an alarm, or you can use a daylight lamp, which may be a gentler way to signal the body that it’s time to sleep or wake.
Create a headspace for sleep
Make sure that you have a designated area just for sleeping. It sounds obvious — of course our beds are meant for sleeping! But many of us, those with OCD and those without, often find ourselves perusing Instagram or Facebook before bed, checking notifications or doing some late-night online shopping to distract ourselves. For someone with OCD, these behaviors can also trigger obsessive thoughts or cycles.
It may be a nice momentary distraction, but unfortunately, these activities signal your brain to be more alert than it needs to be. This means it can take even longer for you to fall asleep after you’re done scrolling. Make sure you’re limiting your screen time before bed to help send the right signals to your brain, and try to keep your sleep space dedicated just for sleep.
During the day, it can also be tempting to work from bed, but that can often lead to you being tired during work (because your brain is used to sleeping in that environment) or doing the opposite — keeping you up at night because you’re trying to rest in your “work” environment.
Don’t give in to sleep-stealing compulsions
Try not to give in to compulsions during your designated sleep time, because it can become self-defeating. For example, if you feel the urge to get up and do something in your house, resist the urge to do so.
Effective, specialized OCD therapy is here
Learn more
Try meditation and mindfulness
Meditation has been shown to have a number of benefits for everyone, especially people dealing with OCD, anxiety and depression. One study examined the use of mindfulness and meditation versus the use of distraction in 30 patients with OCD. Those who used mindfulness skills felt less compelled to give in to their compulsions to neutralize them, and those who used only distraction strategies saw no change.
There are lots of ways to meditate and countless free resources you can use to help you get started with mindfulness techniques. As with anything, meditation can take some practice. You may benefit from starting with just a few minutes at a time and working your way up to longer sessions. Build this time into your nightly sleep hygiene routine!
You may benefit from starting with just a few minutes at a time and working your way up to longer sessions. Build this time into your nightly sleep hygiene routine!
Herbal remedies and supplements
As with any supplement or herbal remedy, it’s important to check with your doctor to ensure that it won’t interfere with any medications you’re taking or treatments you’re using. However, many people with OCD may find melatonin and valerian root beneficial for sleeplessness. You can find melatonin or valerian supplements at most pharmacies or health stores, and you can also drink various herbal teas to promote relaxation, including chamomile, valerian, lavender and more.
Take it one step at a time
As with any journey toward improved health, your path to a peaceful night’s sleep might take some trial and error. Be patient with yourself, consult with your physician or therapist, and take each win as a victory. OCD can make your nights unbearable, but you can claim your sleep back. All it takes is a little practice and finding the right techniques for you.
All it takes is a little practice and finding the right techniques for you.
Find a therapist who can help you manage your OCD
Find therapist
If you are suffering from OCD and you think you need help, please contact NOCD to schedule a free call today. ERP is most effective when the therapist conducting the treatment has experience with OCD and training in ERP. At NOCD, all therapists specialize in OCD and receive ERP-specific training. Let NOCD show you how ERP therapy has proven effective in 80% of patients.
The impact of obsessive-compulsive disorder (OCD) on sleep - Health
Video: Obsessive Compulsive Disorder (OCD) | About it | SecretsContents
- Symptoms and signs of obsessive-compulsive disorder
- How does OCD affect sleep and cause insomnia?
- Medicines used in the treatment of OCD
- Word from Verywell
How can obsessive-compulsive disorder (OCD) affect sleep? One anxiety disorder, obsessive-compulsive disorder, can significantly interfere with daily activities. Does it disrupt sleep, causing sleep problems and insomnia? What are the most common symptoms of mental illness? Can obsessive-compulsive disorder interfere with your ability to sleep at night? Learn the facts, symptoms and effective treatments for the problem.
Does it disrupt sleep, causing sleep problems and insomnia? What are the most common symptoms of mental illness? Can obsessive-compulsive disorder interfere with your ability to sleep at night? Learn the facts, symptoms and effective treatments for the problem.
Symptoms and signs of obsessive-compulsive disorder
Obsessive-compulsive disorder is one of the anxiety disorders that can develop at an early age. It can affect children, more often boys, who also have a diagnosis of attention deficit hyperactivity disorder (ADHD). It is also diagnosed in adolescence and early adulthood. Among adults, it affects men and women equally. It occurs in 0.5–1% of people in a given year. OCD is characterized by two characteristics: obsessions and compulsions.
Obsessions are persistent thoughts, images or impulses that seem intrusive or inappropriate. These ideas are associated with anxiety or stress. One common obsession has to do with cleanliness and the belief that items are contaminated with germs. Some people with OCD may worry that the task was not done or not done properly. For example, you may be worried about turning off the stove or locking the door, even though they were actually secure. These obsessions are often ignored or suppressed by other thoughts or actions, which is called compulsion.
Some people with OCD may worry that the task was not done or not done properly. For example, you may be worried about turning off the stove or locking the door, even though they were actually secure. These obsessions are often ignored or suppressed by other thoughts or actions, which is called compulsion.
Compulsions are defined as repetitive and deliberate actions that occur in response to a specific obsession. By performing these compulsive actions, you can temporarily suppress intrusive thoughts. Compulsions are performed in a very predictable and ritualized manner. Many have compulsions of a superstitious nature. To reduce anxiety about fear of germs, a cleansing can be done. To make sure the door is really locked, it can be checked three times. Common compulsions include:
- Washing hands
- Order
- Count
- Pray
- Repetition of words
- Pressure
These compulsions can provide temporary relief, but soon the alarm begins to increase again, and the intrusive effect must be repeated. When these activities take up more than 1 hour a day and interfere with a normal lifestyle, OCD is diagnosed.
When these activities take up more than 1 hour a day and interfere with a normal lifestyle, OCD is diagnosed.
How does OCD affect sleep and cause insomnia?
You may conclude that OCD-related thoughts and behaviors can interfere with sleep. If you're trying to sleep at night but keep thinking about what you need to check, you may experience insomnia. In fact, behavior testing can be devastating if it involves getting out of the dream environment to calm yourself down.
Surprisingly, there is little evidence that this condition leads to abnormalities that can be detected by a sleep study called a polysomnogram. Some studies suggest that there may be less total sleep or more sleep disturbances, but this has not been consistently demonstrated. This may be due not only to OCD, but also to the depression that often coexists with it.
More research is needed on the possible link between OCD and sleep disorders.
Medications used to treat OCD
There are many treatment options for people with OCD, which can be especially important if the condition is affecting daily life.
Drugs commonly used include tricyclic antidepressants (including clomipramine) and selective serotonin receptor inhibitors (SSRIs). Some of the most commonly used SSRIs:
- Fluoxetine
- Fluvoxamine
- Paroxetine
- Sertraline
In addition to medication, it may be helpful to work with a psychologist who is trained in desensitization and cognitive behavioral therapy. In very rare cases, deep brain stimulator implantation surgery may be used to relieve symptoms.
Word from Verywell
If you think you may be suffering from OCD, you can start by talking to your primary care physician, who can suggest a referral to a psychiatrist to help you feel better. When sleep is disturbed, mood, thinking, and function can quickly be disrupted. By correcting this condition, you can finally get the rest you need to improve your health and well-being.
Sleep disorders in anxiety and anxiety-depressive disorders | Kovrov G.
 V., Lebedev M.A., Palatov S.Yu., Merkulova T.B., Posokhov S.I.
V., Lebedev M.A., Palatov S.Yu., Merkulova T.B., Posokhov S.I. In clinical practice, sleep disorders are usually combined with anxiety and depression. Existing studies show a close relationship between sleep disorders and anxiety and depressive disorders [1, 2]. A clear dependence of the severity of the course of both groups of diseases on concomitant sleep disorders was shown [1]. In general somatic practice, the prevalence of insomnia reaches 73% [3], in borderline psychiatry, clinically defined insomnia occurs in 65%, and changes in nocturnal sleep according to polysomnography are noted in 100% of cases [4].
Combination of sleep disorders and anxiety disorders
It is known that the relationship between sleep disorders and anxiety disorders is noted, on the one hand, when sleep disorders can provoke the development of anxiety disorders [5], and on the other hand, when the onset of an anxiety disorder precedes the onset of sleep disorders. Complaints about problems associated with sleep are typical for patients with all diseases included in the group of anxiety disorders. In the case of major generalized disorder and post-traumatic stress disorder (PTSD), sleep disturbances are one of the criteria required for a diagnosis. There are objective reasons for the development of sleep disorders within anxiety disorders, namely: anxiety is manifested by increased cortical activation, which entails the difficulty of falling asleep and maintaining sleep.
In the case of major generalized disorder and post-traumatic stress disorder (PTSD), sleep disturbances are one of the criteria required for a diagnosis. There are objective reasons for the development of sleep disorders within anxiety disorders, namely: anxiety is manifested by increased cortical activation, which entails the difficulty of falling asleep and maintaining sleep.
In the clinic, anxiety is manifested by anxiety, irritability, motor excitation, decreased concentration of attention, increased fatigue [6].
The most striking manifestation of anxiety disorders is generalized anxiety disorder (GAD), which is diagnosed on the basis of the presence of at least 3 of the following symptoms: restlessness, fatigue, difficulty concentrating, irritability, muscle tension, sleep disturbances. The duration of the disease should be at least 6 months, the symptoms should cause psychosomatic discomfort and / or social disadaptation.
Sleep disorders in this situation are one of the 6 diagnostic criteria for GAD. The main symptom of GAD, excessive, persistent anxiety, is a major predisposing factor in the development of insomnia. Insomnia and GAD are closely related, usually comorbid disorders. The difference between insomnia in anxiety disorder and primary insomnia, not associated with other diseases, is the nature of the experiences in the process of falling asleep. In the case of GAD, the patient is concerned about current problems [7] (work, study, relationships), which hinders the process of falling asleep. In the case of primary insomnia, the anxiety itself is caused by the disease itself.
The main symptom of GAD, excessive, persistent anxiety, is a major predisposing factor in the development of insomnia. Insomnia and GAD are closely related, usually comorbid disorders. The difference between insomnia in anxiety disorder and primary insomnia, not associated with other diseases, is the nature of the experiences in the process of falling asleep. In the case of GAD, the patient is concerned about current problems [7] (work, study, relationships), which hinders the process of falling asleep. In the case of primary insomnia, the anxiety itself is caused by the disease itself.
A polysomnographic study can reveal changes characteristic of insomnia: increased time to fall asleep, frequent awakenings, reduced sleep efficiency, and a decrease in its total duration.
Another striking example of anxiety disorders is panic disorder, which is manifested by recurrent states of severe anxiety (panic). Attacks are accompanied by phenomena of depersonalization and derealization, as well as severe autonomic disorders. In the behavior of the patient, avoidance of situations in which the attack occurred for the first time is noted. There may be a fear of loneliness, a repetition of the attack. A panic attack occurs spontaneously, outside of formal situations of danger or threat.
In the behavior of the patient, avoidance of situations in which the attack occurred for the first time is noted. There may be a fear of loneliness, a repetition of the attack. A panic attack occurs spontaneously, outside of formal situations of danger or threat.
Panic disorder is more common in women and typically begins around the age of 20. A hallmark of panic disorder are spontaneous episodes of panic attacks, characterized by bouts of fear, anxiety, and other autonomic manifestations. About 2/3 of patients with this disorder experience some form of sleep disturbance. Patients complain of difficulty falling asleep, non-restorative sleep, and characteristic nocturnal panic attacks. It should be noted that the presence of certain problems associated with sleep can lead to aggravation of anxiety disorders, including panic disorder.
Polysomnographic examination can detect frequent awakenings, reduced sleep efficiency and a reduction in its total duration [8]. It is not uncommon to see depression coexisting with anxiety disorders, and it is possible that the presence of other changes in sleep patterns in patients with panic disorder is associated with comorbid depression, and therefore the diagnosis of depression should be ruled out in patients with similar sleep disorders.
The sleep paralysis characteristic of narcolepsy can also occur with panic disorder. It is a movement paralysis that occurs during falling asleep or waking up, during which patients experience fear, a feeling of pressure in the chest, and other somatic manifestations of anxiety. This symptom also occurs in patients with post-traumatic stress disorder.
Nighttime panic attacks are a common occurrence in this disease [9]. They are manifested by a sudden awakening and all the symptoms characteristic of panic attacks. Awakening occurs during the phase of non-REM sleep, which most likely excludes their connection with dreams. It was also found that nocturnal attacks are an indicator of a more severe course of the disease. It must be remembered that patients, fearing the recurrence of such episodes, deprive themselves of sleep, which leads to more serious disorders and, in general, reduces the quality of life of these patients.
PTSD is a disease from the group of anxiety disorders, in which sleep disturbances are a diagnostic criterion. Sleep disorders in this disease include 2 main symptoms: nightmares and insomnia. Other phenomena inherent in PTSD and associated with sleep are: somnambulism, sleep-talking, hypnagogic and hypnopompic hallucinations. The changes detected by polysomnography are not specific and in some cases may be absent. Possible changes include: an increase in the representation of the 1st stage of sleep, a decrease in the representation of the 4th stage of sleep. Also, with PTSD, breathing disorders during sleep are often found.
Sleep disorders in this disease include 2 main symptoms: nightmares and insomnia. Other phenomena inherent in PTSD and associated with sleep are: somnambulism, sleep-talking, hypnagogic and hypnopompic hallucinations. The changes detected by polysomnography are not specific and in some cases may be absent. Possible changes include: an increase in the representation of the 1st stage of sleep, a decrease in the representation of the 4th stage of sleep. Also, with PTSD, breathing disorders during sleep are often found.
Agoraphobia can also be a manifestation of anxiety disorders, which is defined as anxiety that occurs in response to situations, the way out of which, according to the patient, is difficult. In the clinical picture, as a rule, there is a persistent fear of the patient to be in a crowded place, public places (shops, open squares and streets, theaters, cinemas, concert halls, workplaces), fear of independent long trips (by various modes of transport). The situational component of the agoraphobia syndrome is expressed in the confinement of phobic experiences to certain situations and in the fear of getting into situations in which, according to patients, a repetition of painful sensations is likely. Often, agoraphobic symptoms cover many fears of various situations, forming panagoraphobia - the fear of leaving the house with the development of deep social maladaptation. There are attempts by the patient to overcome their own experiences, in adverse cases, there is a restriction of social activity.
Often, agoraphobic symptoms cover many fears of various situations, forming panagoraphobia - the fear of leaving the house with the development of deep social maladaptation. There are attempts by the patient to overcome their own experiences, in adverse cases, there is a restriction of social activity.
Specific phobias are characterized by an association of anxiety with certain situations (air travel, contact with animals, the sight of blood, etc.), also accompanied by an avoidance reaction. Patients are critical of their experiences, however, phobias have a significant impact on various areas of activity of patients. There are the following forms: cardiophobia, cancerophobia, claustrophobia, etc. Sleep disturbances in these patients are non-specific, and from the point of view of the patient, they are a minor manifestation of the disease.
In general, the most common manifestations of sleep disturbances in anxiety states are presomnic disorders. The initial phase of sleep consists of 2 components: drowsiness, a kind of craving for sleep, and actually falling asleep. Often, patients have no desire to sleep, no desire to sleep, muscle relaxation does not occur, they have to perform various actions aimed at falling asleep. In other cases, there is an inclination to sleep, but its intensity is reduced, drowsiness becomes intermittent, undulating. Drowsiness occurs, the muscles relax, the perception of the environment decreases, the patient takes a comfortable position for falling asleep, and a slight drowsiness appears, but soon it is interrupted, disturbing thoughts and ideas arise in the mind. In the future, the state of wakefulness is again replaced by mild drowsiness and superficial drowsiness. Such changes in states can be repeated several times, leading to emotional discomfort that prevents the onset of sleep.
Often, patients have no desire to sleep, no desire to sleep, muscle relaxation does not occur, they have to perform various actions aimed at falling asleep. In other cases, there is an inclination to sleep, but its intensity is reduced, drowsiness becomes intermittent, undulating. Drowsiness occurs, the muscles relax, the perception of the environment decreases, the patient takes a comfortable position for falling asleep, and a slight drowsiness appears, but soon it is interrupted, disturbing thoughts and ideas arise in the mind. In the future, the state of wakefulness is again replaced by mild drowsiness and superficial drowsiness. Such changes in states can be repeated several times, leading to emotional discomfort that prevents the onset of sleep.
In a number of patients, experiences about disturbed sleep can acquire an overvalued hypochondriacal coloration and come to the fore according to the mechanisms of actualization, often there is an obsessive fear of insomnia - agripnophobia. It is usually combined with an anxious and painful expectation of sleep, certain requirements for others and the creation of the above-mentioned special conditions for sleep.
It is usually combined with an anxious and painful expectation of sleep, certain requirements for others and the creation of the above-mentioned special conditions for sleep.
Anxiety depression is characterized by the patient's constant experience of anxiety, a sense of impending danger and insecurity. Anxious experiences change: anxiety about their loved ones, fears about their condition, their actions. The structure of anxious depression, as a rule, includes anxiety, feelings of guilt, motor restlessness, fussiness, fluctuations in affect with worsening in the evening, and somatovegetative symptoms. Anxious and melancholy affects often occur simultaneously, in many cases it is impossible to determine which of them is leading in the patient. Anxiety depression is most often found in people of involutionary age and proceeds according to the type of protracted phases. In addition, it is actually the leading type of neurotic depression [10].
The patient exhibits a variety of symptoms of anxiety and depression. Initially, one or more physical symptoms (eg, fatigue, pain, sleep disturbances) may be present. Further questioning allows us to state a depressive mood and/or anxiety.
Initially, one or more physical symptoms (eg, fatigue, pain, sleep disturbances) may be present. Further questioning allows us to state a depressive mood and/or anxiety.
Signs of anxiety depression:
- depressed mood;
- loss of interest;
- severe anxiety.
The following symptoms are also often seen:
- sleep disorders;
- physical weakness and loss of energy;
- fatigue or reduced activity;
- difficulty concentrating, fidgeting;
- impaired concentration;
- excitation or retardation of movements or speech;
- appetite disorders;
- dry mouth;
- tension and anxiety;
- irritability;
- tremor;
- heartbeat;
- dizziness;
- suicidal thoughts.
Often with anxiety depression, variants of presomnic disorders are observed, in which the desire to sleep is pronounced, drowsiness increases rapidly, and the patient falls asleep relatively easily, but wakes up suddenly after 5-10 minutes, drowsiness completely disappears, and then within 1-2 hours he does not can fall asleep. This period without sleep is characterized by unpleasant ideas, thoughts, fears, reflecting to a greater or lesser extent the experienced conflict situation and the reaction to the inability to sleep. There is also hyperesthesia to sensory stimuli. Those suffering from this form of sleep disorder react extremely painfully to the slightest sensory stimuli, up to flashes of affect.
This period without sleep is characterized by unpleasant ideas, thoughts, fears, reflecting to a greater or lesser extent the experienced conflict situation and the reaction to the inability to sleep. There is also hyperesthesia to sensory stimuli. Those suffering from this form of sleep disorder react extremely painfully to the slightest sensory stimuli, up to flashes of affect.
For disturbed falling asleep, lengthening of the drowsy period is characteristic. This drowsy state is often accompanied by motor, sensory and visceral automatisms, sharp shudders, vivid perceptions of sounds and visual images, palpitations, sensations of muscle spasms. Often these phenomena, awakening the patient, cause various painful ideas and fears, sometimes acquiring an obsessive character.
Sleep disorders and their polysomnographic manifestations among mental illnesses are the most studied for depressive disorder. Among the sleep disorders in depressive disorder, insomnia is the most common. The severity and duration of insomnia are manifestations of a more severe depressive disorder, and the appearance of insomnia during remission indicates the imminent occurrence of a recurrent depressive episode [1]. In addition, sleep disorders in this disease are the most persistent symptom. The close relationship of this disorder with sleep disorders is explained by the biochemical processes characteristic of depression. In particular, in depressive disorder, there is a decrease in the level of serotonin, which plays a role in the initiation of REM sleep and the organization of delta sleep [11]. Depressive disorder is characterized by the following manifestations of sleep disturbances: difficulty falling asleep [10], non-restorative sleep, as a rule, reduced total sleep time. The most specific symptoms for depression are frequent nocturnal awakenings and early terminal awakenings. Complaints about difficulty falling asleep are more often observed in young patients, and frequent awakenings are more characteristic of the elderly [12].
The severity and duration of insomnia are manifestations of a more severe depressive disorder, and the appearance of insomnia during remission indicates the imminent occurrence of a recurrent depressive episode [1]. In addition, sleep disorders in this disease are the most persistent symptom. The close relationship of this disorder with sleep disorders is explained by the biochemical processes characteristic of depression. In particular, in depressive disorder, there is a decrease in the level of serotonin, which plays a role in the initiation of REM sleep and the organization of delta sleep [11]. Depressive disorder is characterized by the following manifestations of sleep disturbances: difficulty falling asleep [10], non-restorative sleep, as a rule, reduced total sleep time. The most specific symptoms for depression are frequent nocturnal awakenings and early terminal awakenings. Complaints about difficulty falling asleep are more often observed in young patients, and frequent awakenings are more characteristic of the elderly [12].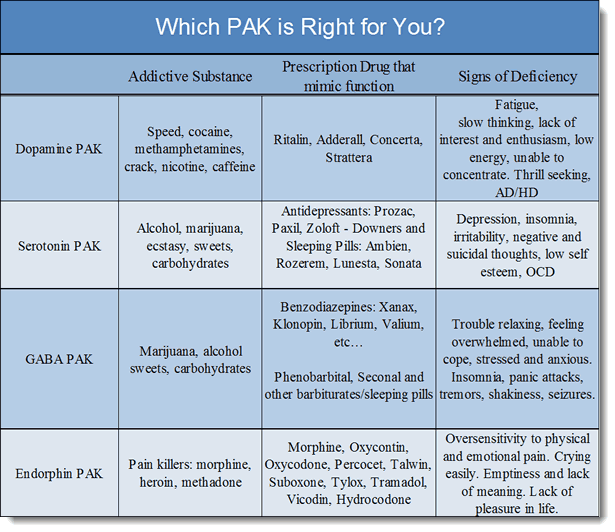
With masked depression, complaints of sleep disturbances may be the only manifestation of the disease. In depression, in contrast to primary insomnia, there are complaints of sleep disturbances typical of this disease: frequent awakenings, early morning awakening, etc. [12].
In polysomnographic study, the following changes are observed: an increase in the time to fall asleep, a decrease in sleep efficiency. The most common and depressive disorder-specific symptoms are shortened REM sleep latency and reduced delta sleep. It has been found that patients with a higher proportion of delta sleep stay in remission longer than those with a decrease in the proportion of delta sleep [13].
Attempts have been made to explore the possibility of using depression-specific sleep disturbances as markers of depressive disorder. Due to the heterogeneity of the manifestations of sleep disorders, this issue remains not fully resolved.
The features of sleep disorders in various types of depression were also highlighted. For patients with a predominance of the anxious component, difficulty falling asleep and early awakenings are more characteristic. With this type of depression, dream plots are associated with persecution, threats, etc. In addition, in these patients, in general, there was a high level of wakefulness before falling asleep. For depressions with the leading affect of melancholy, early morning awakenings and dreams of static types of gloomy content are most characteristic. Depression with the affect of apathy is characterized by early awakenings and rare, unsaturated dreams. Also typical of depression with apathetic affect is the loss of a sense of boundaries between sleep and wakefulness. Patients with bipolar disorder have a similar polysomnographic pattern [14].
For patients with a predominance of the anxious component, difficulty falling asleep and early awakenings are more characteristic. With this type of depression, dream plots are associated with persecution, threats, etc. In addition, in these patients, in general, there was a high level of wakefulness before falling asleep. For depressions with the leading affect of melancholy, early morning awakenings and dreams of static types of gloomy content are most characteristic. Depression with the affect of apathy is characterized by early awakenings and rare, unsaturated dreams. Also typical of depression with apathetic affect is the loss of a sense of boundaries between sleep and wakefulness. Patients with bipolar disorder have a similar polysomnographic pattern [14].
Features of sleep disturbance in bipolar disorder are a significant decrease in the duration of sleep during a manic episode and a greater tendency of patients to hypersomnia during depressive episodes compared with the unipolar course of the disorder. Complaints of sleep disturbances during manic episodes are usually absent.
Complaints of sleep disturbances during manic episodes are usually absent.
Treatment
For the treatment of anxiety and depressive disorders, drugs of various pharmacological groups are used: tranquilizers (mainly long-acting or short-acting benzodiazepine drugs), selective serotonin reuptake inhibitors, selective serotonin reuptake stimulants, tricyclic antidepressants. All these drugs, to one degree or another, affect a person’s sleep, making it easier to fall asleep, reducing the number and duration of nocturnal awakenings, thereby affecting the recovery processes that occur during a night’s sleep. When constructing tactics for the treatment of sleep disorders associated with anxiety and depressive manifestations, it is important to remember that insomnia itself can increase anxiety, worsen well-being, mood, as a rule, in the morning hours after poor sleep [15]. In this regard, the use of hypnotics in the treatment may be promising in the presence of a predominance of insomnia symptoms in the clinical picture in order to prevent exacerbation of anxiety and depressive disorders. In this regard, the most effective helpers can be sleeping pills that affect the GABAergic (GABA - γ-aminobutyric acid) system - histamine receptor blockers (Valocordin®-Doxylamine) and melatonin preparation. The most convenient to use in the treatment of insomnia is Valocordin®-Doxylamine, which is available in drops, which allows you to select an individual dose of the drug.
In this regard, the most effective helpers can be sleeping pills that affect the GABAergic (GABA - γ-aminobutyric acid) system - histamine receptor blockers (Valocordin®-Doxylamine) and melatonin preparation. The most convenient to use in the treatment of insomnia is Valocordin®-Doxylamine, which is available in drops, which allows you to select an individual dose of the drug.
Valocordin®-Doxylamine is a unique drug used as a hypnotic. Most known hypnotic drugs (benzodiazepines, cyclopyrrolones, imidazopyridines, etc.) act on the GABAergic complex, activating the activity of somnogenic systems, while histamine receptor blockers act on wakefulness systems, not sleep ones, reducing their activation. A fundamentally different mechanism of hypnotic action makes it possible to use Valocordin®-Doxylamine more widely: when changing one drug to another, reducing the dosages of "habitual hypnotics", and also, if necessary, canceling hypnotics.
A drug study conducted on healthy subjects showed that doxylamine succinate leads to a decrease in the duration of nocturnal awakenings and stage 1 sleep and an increase in stage 2 without a significant effect on the duration of stages 3 and 4 sleep and REM sleep. There was no significant subjective effect on the reports of healthy volunteers, however, compared with placebo, doxylamine increased the depth of sleep and improved its quality [16].
There was no significant subjective effect on the reports of healthy volunteers, however, compared with placebo, doxylamine increased the depth of sleep and improved its quality [16].
In Russia, one of the first studies was carried out under the supervision of A.M. Wayne [17]. It has been shown that under the influence of doxylamine such subjective characteristics of sleep as the duration of falling asleep, the duration and quality of sleep, the number of night awakenings and the quality of morning awakenings improve. An analysis of the objective characteristics of sleep showed that while taking doxylamine, there was a reduction in the time of wakefulness during sleep, a decrease in the duration of falling asleep, an increase in the duration of sleep, the time of the REM sleep phase, and the sleep quality index. It was also shown that doxylamine did not reduce the effectiveness of other drugs in patients, such as antihypertensive, vasoactive, etc. The results of a study of the effect of doxylamine on patients with insomnia indicate the effectiveness of this drug in these patients. Subjective feelings of a positive effect are confirmed by objective studies of the structure of sleep, which undergoes positive shifts, which affect such indicators as sleep duration, falling asleep duration, REM sleep phase. Of great importance is also the absence of any changes in the results of personal data regarding drowsiness and sleep apnea syndrome, which indicates the absence of an aftereffect of the drug in relation to the worsening of the course of obstructive sleep apnea syndrome. However, if obstructive sleep apnea is suspected, doxylamine should be used with caution.
Subjective feelings of a positive effect are confirmed by objective studies of the structure of sleep, which undergoes positive shifts, which affect such indicators as sleep duration, falling asleep duration, REM sleep phase. Of great importance is also the absence of any changes in the results of personal data regarding drowsiness and sleep apnea syndrome, which indicates the absence of an aftereffect of the drug in relation to the worsening of the course of obstructive sleep apnea syndrome. However, if obstructive sleep apnea is suspected, doxylamine should be used with caution.
Modern clinical studies do not reveal serious side effects in the treatment of therapeutic doses of the drug, but it is always necessary to remember the possible appearance of symptoms that arise due to the individual characteristics of the body, and contraindications (glaucoma; difficulty urinating due to benign prostatic hyperplasia; age up to 15 years; increased drug sensitivity).
Simultaneous administration of the drug Valocordin®-Doxylamine and sedative drugs that affect the central nervous system (CNS): neuroleptics, tranquilizers, antidepressants, hypnotics, analgesics, anesthetics, antiepileptic drugs, may enhance their effect. Procarbazines and antihistamines should be combined with caution to minimize CNS depression and possible drug potentiation. During treatment with Valocordin®-Doxylamine, alcohol should be avoided as it may unpredictably affect the effects of doxylamine succinate.
Procarbazines and antihistamines should be combined with caution to minimize CNS depression and possible drug potentiation. During treatment with Valocordin®-Doxylamine, alcohol should be avoided as it may unpredictably affect the effects of doxylamine succinate.
During the use of this drug, it is recommended to exclude driving a car and working with mechanisms, as well as other activities accompanied by an increased risk, at least at the first stage of treatment. The attending physician is advised to evaluate the individual reaction rate when choosing a dose. It is important to consider these features of the effect of the drug in the treatment of patients with insomnia in order to increase the effectiveness of Valocordin®-Doxylamine and exclude possible undesirable effects.
Conclusion
When diagnosing a disease, it is important to remember that, as a rule, problems falling asleep indicate the presence of severe anxiety, early awakenings are a manifestation of depression.