Levels of schizophrenia
Stages of schizophrenia: Symptoms, causes, and treatments
Schizophrenia has three distinct phases, which share some overlapping symptoms. The three stages are prodromal, active, and residual. Diagnosing the stages of schizophrenia is important for an individual to receive the proper treatment to manage their condition.
Schizophrenia is a chronic mental illness that affects an estimated 24 million people worldwide.
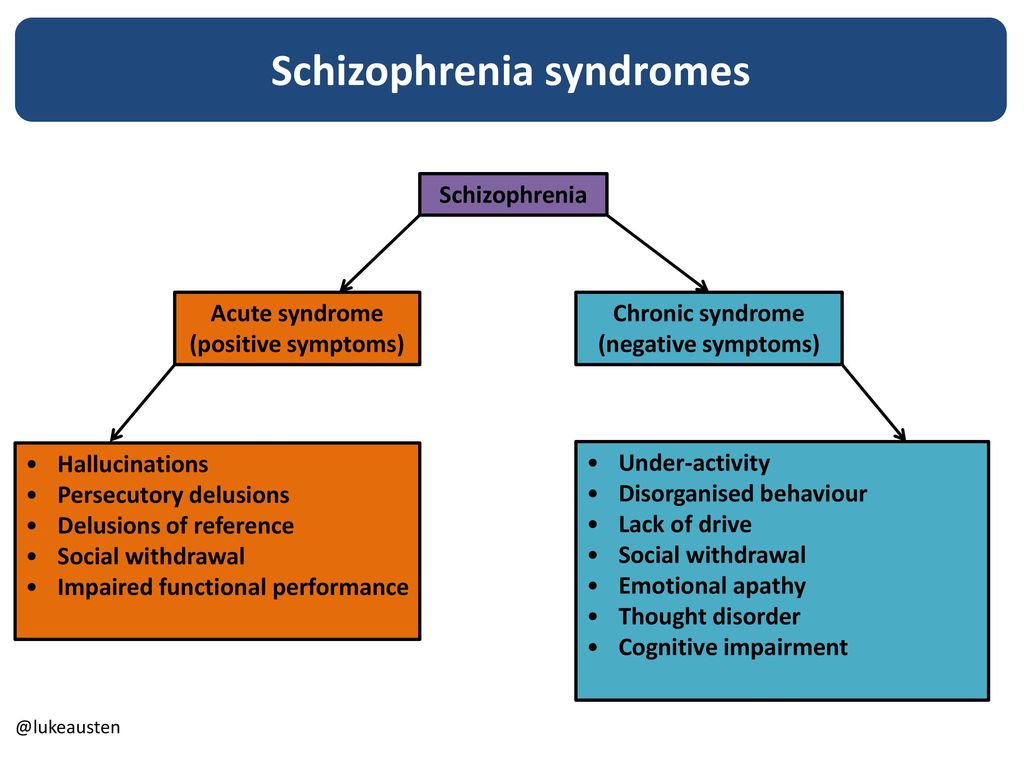
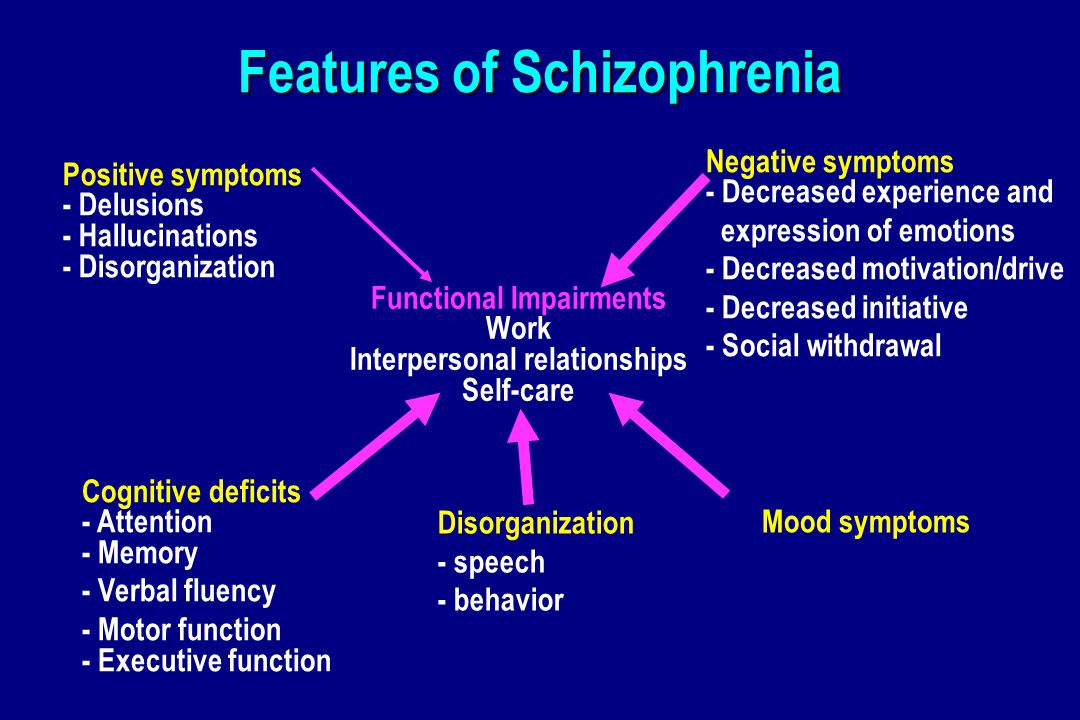
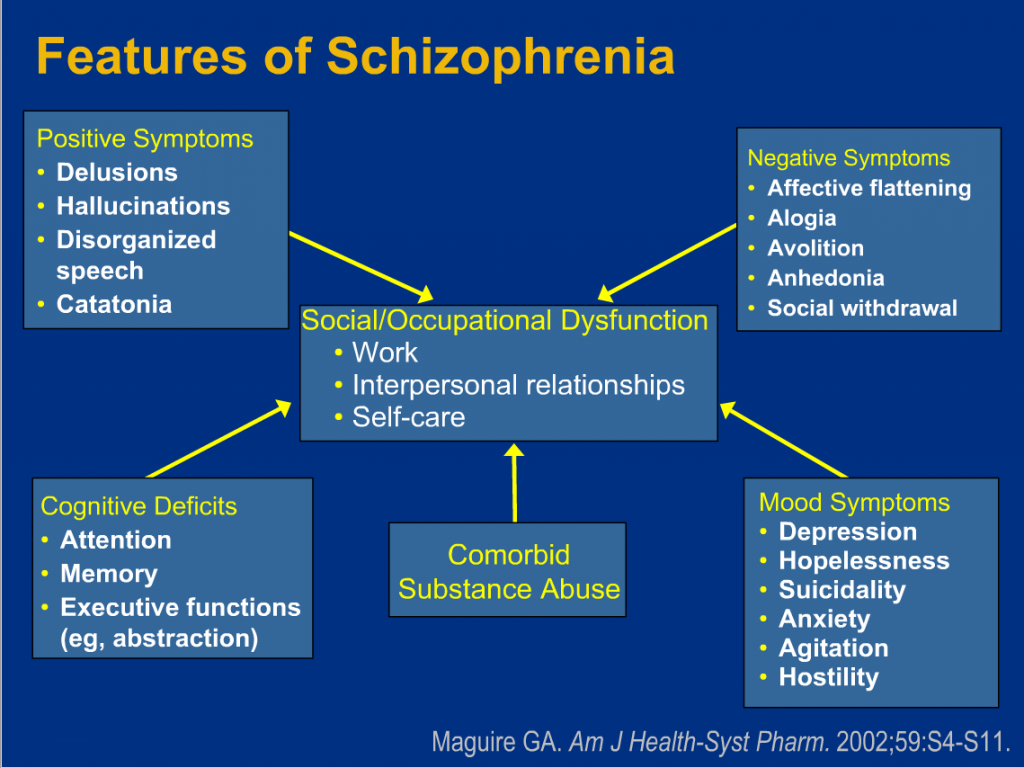
This illness affects the way a person thinks, feels, and behaves. People with schizophrenia may experience:
- delusions
- hallucinations
- depression
- memory problems
- disorganized thoughts and speech
People can manage their symptoms with the help of a care team that coordinates and delivers effective treatments. However, without treatment, symptoms of schizophrenia can severely impact a person’s ability to engage in work or school, live independently, and maintain healthy interpersonal relationships.
This article discusses the stages of schizophrenia, their causes, symptoms, diagnosis, treatment options, and where to seek emergency care.
This is the first stage of schizophrenia. It occurs before noticeable psychotic symptoms appear. During this stage, a person undergoes behavioral and cognitive changes that can, in time, progress to psychosis.
The early stage of schizophrenia usually involves non-specific symptoms that also occur in other mental illnesses, such as depression.
Symptoms of prodromal schizophrenia include:
- social isolation
- lack of motivation
- anxiety
- irritability
- difficulty concentrating
- changes to one’s normal routine
- sleep problems
- neglecting personal hygiene
- erratic behavior
- mild or poorly formed hallucinations
According to the authors of one 2018 review, up to 73% of people with schizophrenia experience the prodromal stage before they develop the characteristic symptoms of schizophrenia.
Identifying individuals in the prodromal stage remains challenging.
In this stage, people with schizophrenia exhibit characteristic symptoms of psychosis, including hallucinations, delusions, and paranoia.
Active schizophrenia, or active psychosis, involves obvious symptoms such as:
- hallucinations, including seeing, hearing, smelling, or feeling things that others do not
- delusions, which are false notions or ideas that a person believes even when presented with evidence to the contrary
- confused and disorganized thoughts
- disordered or jumbled speech
- excessive or useless movement
- wandering
- mumbling
- laughing to oneself
- apathy or numbing of emotions
The Diagnostic and Statistical Manual, Fifth Edition (DSM-5) no longer recognizes this stage for diagnosing purposes. However, it is still useful for describing the symptoms of schizophrenia.
In residual schizophrenia, a person experiences fewer or less severe symptoms than those seen in the active stage.
Typically, people in this stage do not experience positive symptoms, such as hallucinations or delusions.
The residual stage is similar to the prodromal stage.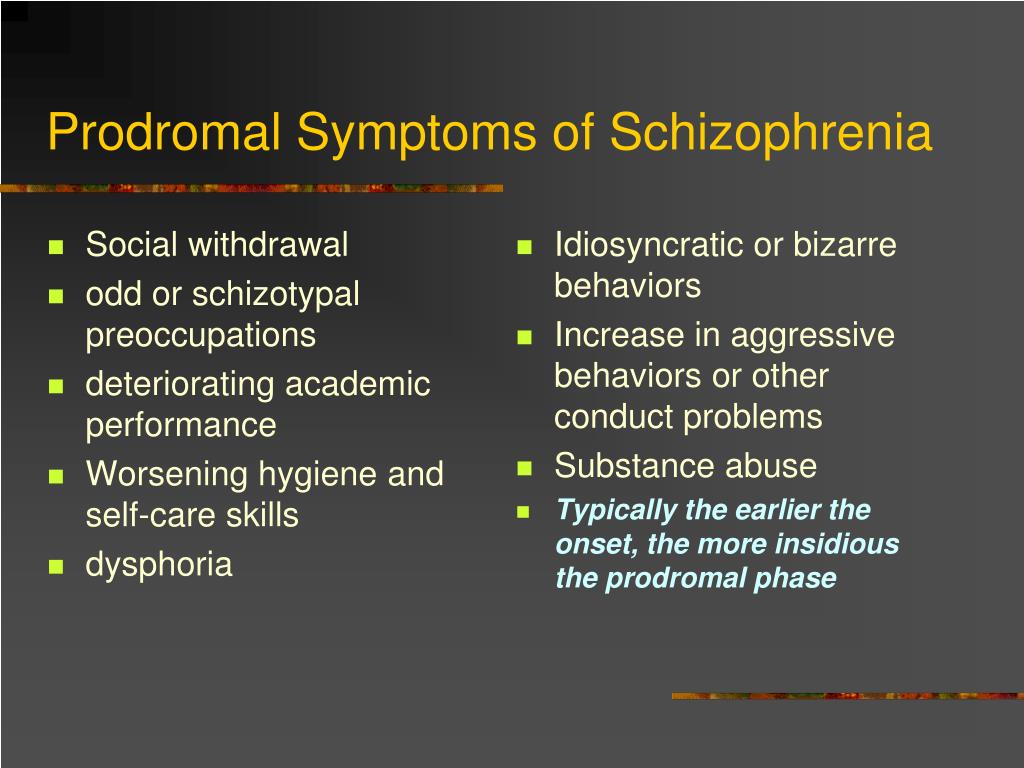 People may experience negative symptoms, such as a lack of motivation, low energy, or depressed mood.
People may experience negative symptoms, such as a lack of motivation, low energy, or depressed mood.
Symptoms of residual schizophrenia include:
- social withdrawal
- difficulty concentrating
- difficulty planning and participating in activities
- reduced or absent facial expressions
- flat, monotone voice
- general disinterest
Schizophrenia is a multidimensional condition that arises from a number of variables. Research has shed light on the possible causes of schizophrenia. However, the reasons why people move through the phases of schizophrenia remain unclear.
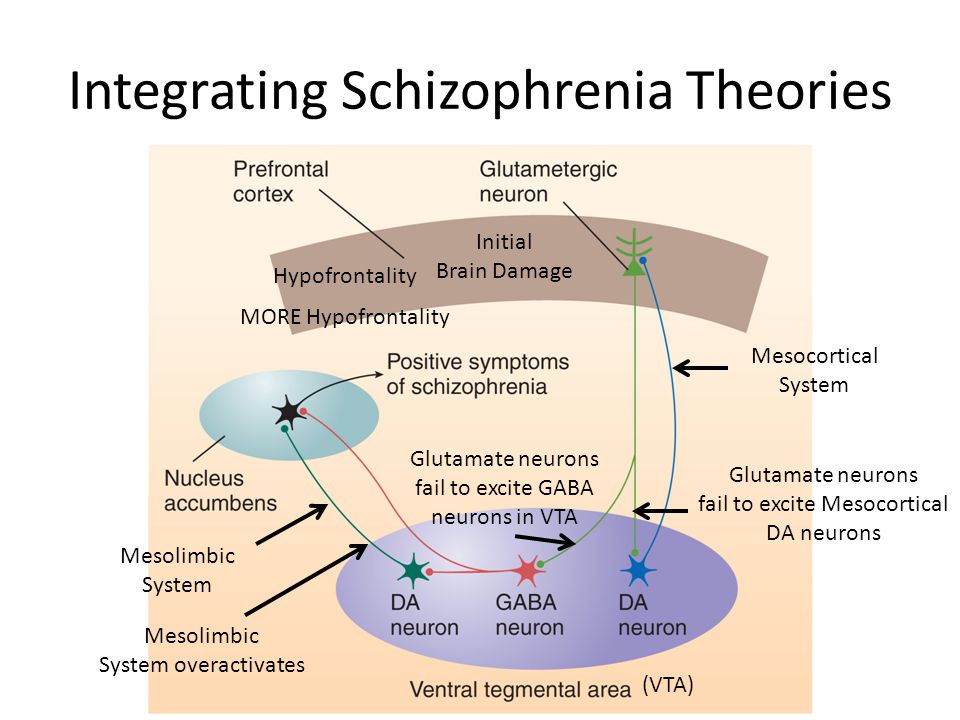
A combination of environmental, genetic, and physiological factors may alter the brain’s structure and chemistry. These changes lead to schizophrenia.
Experts associate the following factors with schizophrenia:
- Genetics: According to the National Alliance on Mental Illness (NAMI), people with a family history of schizophrenia are six times more likely to develop the condition.
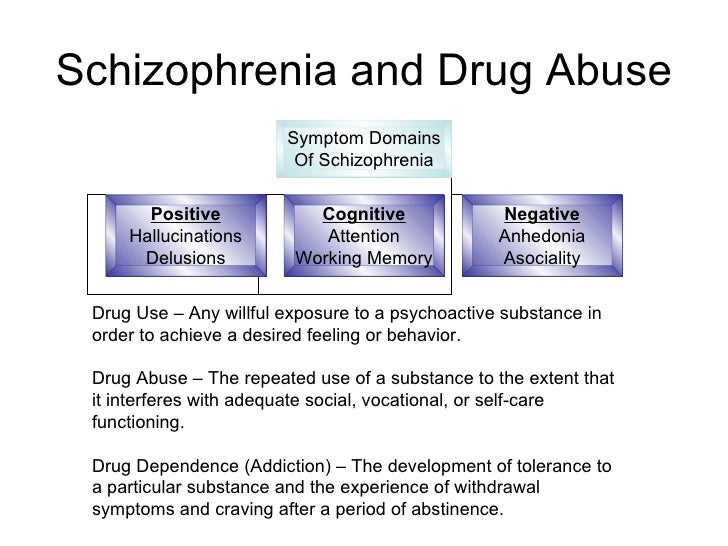
- Environment: A person’s environment can impact their risk for schizophrenia and other mental illnesses. The National Institute of Mental Health (NIMH) state that exposure to viruses, stress, and poverty may play a role in the development of schizophrenia. Lifestyle choices, trauma, and substance abuse may also have an impact.
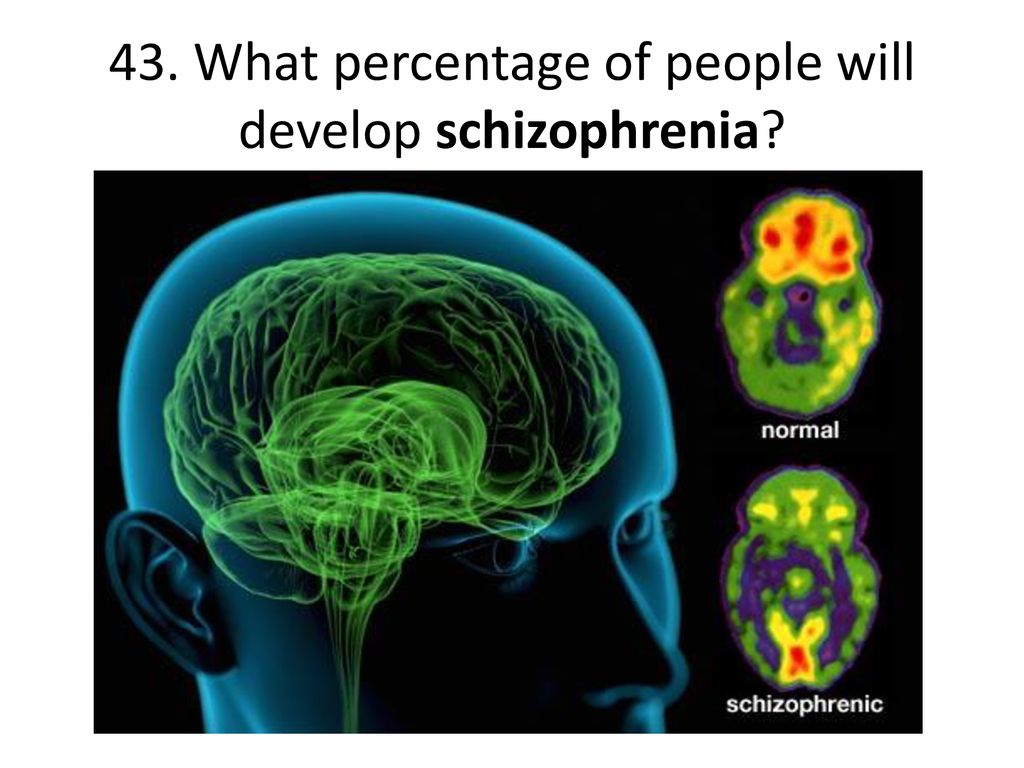
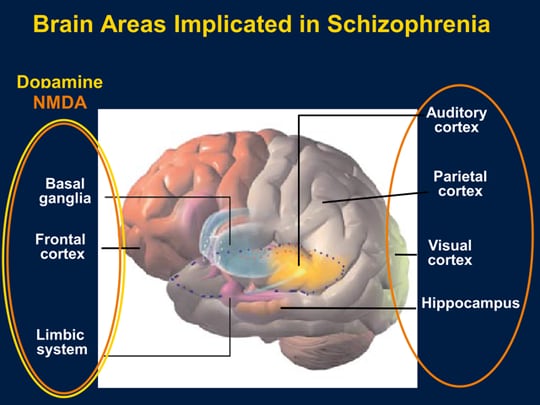
- Brain structure: Changes in brain structure and function can result in abnormal interactions between the brain’s neurotransmitters, such as dopamine. These changes may contribute to psychotic episodes and the progression of schizophrenia.
- Substance use: Recent research suggests that substance use, especially during adolescence, can increase the risk of developing schizophrenia later in life. The authors of the NIMH article suggest that the genetic factors associated with schizophrenia may also contribute to the brain changes involved in addiction.
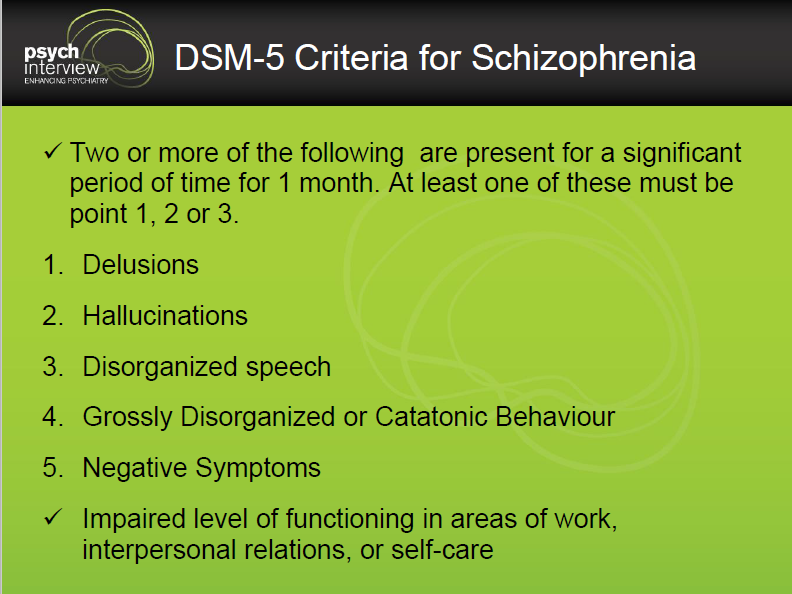
Doctors and mental health practitioners often diagnose schizophrenia during the active stage, when symptoms are most prominent.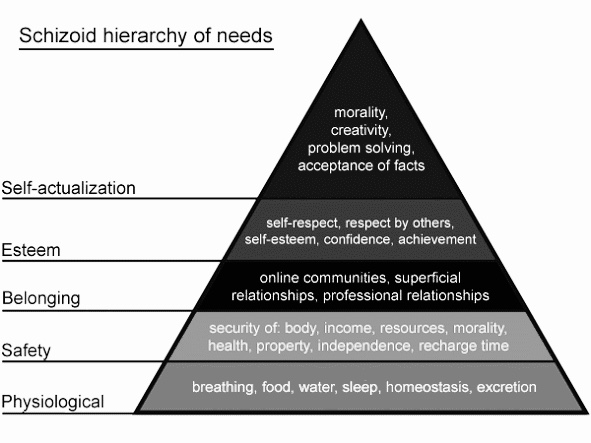
A doctor must follow the criteria outlined in the DSM-5 to diagnose schizophrenia.
According to the DSM-5, a schizophrenia diagnosis consists of the following elements:
- A person exhibits at least two of the following symptoms for a 1-month period:
- delusions
- hallucinations
- disorganized speech
- disorganized or catatonic behavior
- negative symptoms, such as reduced emotional expression or apathy
- The symptoms reduce a person’s ability to function, affecting their professional or academic performance, interpersonal relations, or self-care.
- Reduced functioning lasts for at least 6 months. During this 6-month period, a person exhibits symptoms for at least 1 month.
- The active phase symptoms occur independently of major depressive or manic episodes.
- Symptoms did not result from another medical condition, substance abuse, or medication.
While a person can develop schizophrenia at any age, the average age of onset varies slightly between men and women.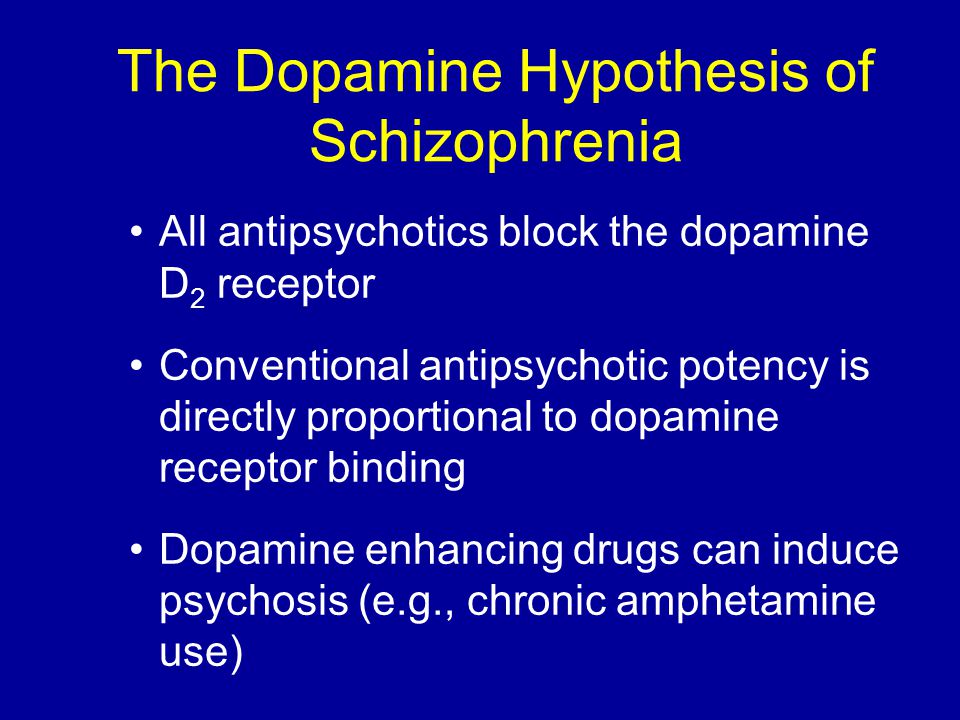
According to NAMI, the initial symptoms of schizophrenia usually appear between the late teens to early 20s for men and the late 20s to early 30s for women.
The authors of one 2018 case report state that schizophrenia can occur in children less than 13 years old, though this appears to be rare.
Although schizophrenia is a lifelong condition, it is treatable. Receiving timely and effective treatment can help manage symptoms and prevent relapses.
Treatment options include:
- Antipsychotic drugs: These medications are available as daily oral doses or monthly injections. People who take antipsychotics as prescribed may experience less intense and less frequent psychotic symptoms. While effective, antipsychotic drugs can have adverse effects, such as weight gain and drowsiness.
- Psychotherapy, such as:
- Cognitive behavioral therapy: This form of treatment can help people develop useful coping skills and strategies for working through disruptive thoughts.
- Psychodynamic therapy: Also known as psychoanalytic therapy, psychodynamic therapy involves conversations between a psychologist and their patient. These conversations attempt to uncover emotional experiences and unconscious processes that contribute to a person’s current mental state.
- Acceptance and commitment therapy (ACT): ACT is a type of behavioral therapy that encourages people to accept, rather than challenge, their deep feelings. ACT also focuses on commitments to personal goals and values and improving one’s overall quality of life. Finally, ACT teaches mindfulness skills that can help keep a person focused on the present moment instead of being consumed by negative thoughts or experiences. Combining these three conditions, a person can change their behaviors by first changing their attitude towards themself.
- Family therapy: This form of psychotherapy involves families and significant others of people with schizophrenia and other mental health conditions.
 It focuses on education, stress reduction, and emotional processing. It helps family members better communicate and resolve conflicts with one another.
It focuses on education, stress reduction, and emotional processing. It helps family members better communicate and resolve conflicts with one another.
- Cognitive behavioral therapy: This form of treatment can help people develop useful coping skills and strategies for working through disruptive thoughts.
- Coordinated specialty care (CSC): CSC involves a team of health professionals that manage medication, deliver psychotherapy, and provide education and employment support.
If you or a loved one is experiencing suicidal thoughts or exhibiting dangerous or risky behaviors, please seek emergency care:
- Dial 911 or visit the nearest emergency department
- Call the NAMI HelpLine at 1-800-950-NAMI (6264)
- Call the SAMHSA’s National Helpline at 1-800-622-HELP (4357)
- Find a local extended observation unit (EOU) or crisis stabilization unit (CSU)
Suicide prevention
If you know someone at immediate risk of self-harm, suicide, or hurting another person:
- Ask the tough question: “Are you considering suicide?”
- Listen to the person without judgment.
- Call 911 or the local emergency number, or text TALK to 741741 to communicate with a trained crisis counselor.
- Stay with the person until professional help arrives.
- Try to remove any weapons, medications, or other potentially harmful objects.
If you or someone you know is having thoughts of suicide, a prevention hotline can help. The 988 Suicide and Crisis Lifeline is available 24 hours a day at 988. During a crisis, people who are hard of hearing can use their preferred relay service or dial 711 then 988.
Click here for more links and local resources.
Schizophrenia is a complex, long-term condition that can significantly impact a person’s ability to function and maintain healthy relationships.
Effective treatments are available that can help a person manage their symptoms and prevent relapses.
People with schizophrenia also benefit from the support of their family and friends and access to community services.
Schizophrenia consists of three stages — prodromal, active, and residual.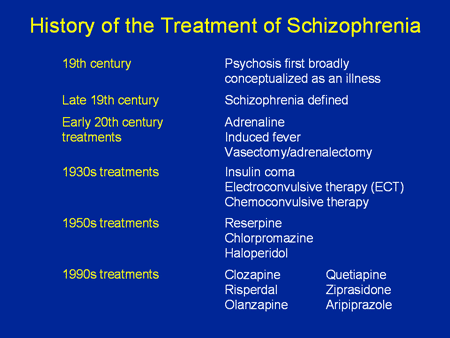
The prodromal stage consists of non-specific symptoms, such as lack of motivation, social isolation, and difficulty concentrating.
Prodromal symptoms are not always obvious. As a result, diagnosing schizophrenia in this stage can be extremely difficult.
Active schizophrenia involves noticeable psychotic symptoms, such as hallucinations and delusions. People require immediate medical attention at this stage.
Timely diagnosis and prompt treatment can help reduce the severity and frequency of psychotic episodes.
The residual stage is no longer acknowledged as a diagnostic criterion, but it helps explain the progression of schizophrenia.
In the residual stage, hallucinations, delusions, and disorganized thinking are mild or completely absent. A person may continue experiencing symptoms from the prodromal stage.
Types of Schizophrenia and the Schizophrenia Spectrum
Written by Terri D'Arrigo
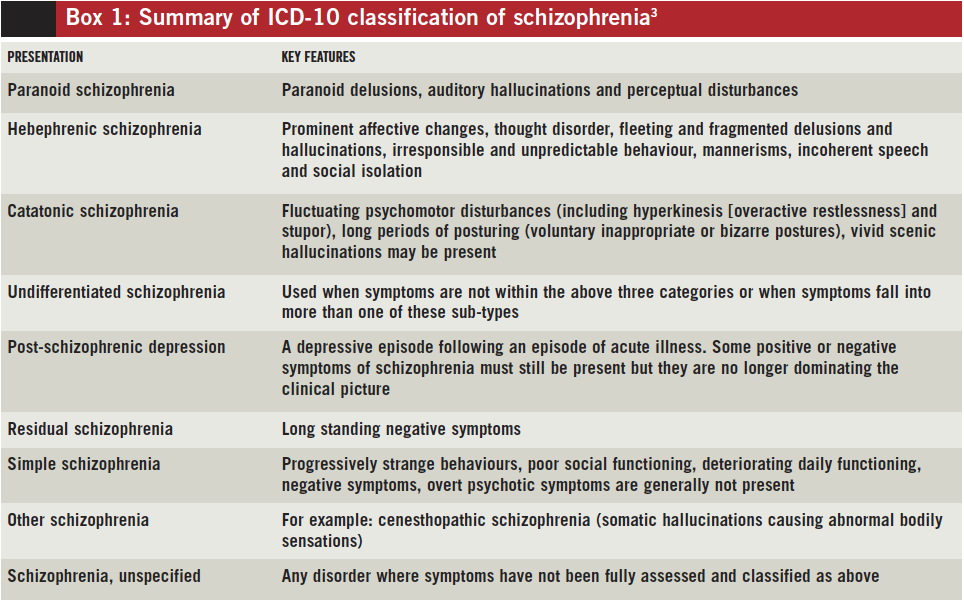
Doctors who specialize in mental health used to divide schizophrenia into different subtypes:
- Catatonic
- Disorganized
- Paranoid
- Residual
- Undifferentiated.

But that system didn’t work well. Now, experts talk about schizophrenia as a spectrum disorder that includes all the previous subtypes. It's a group of related mental disorders that share some symptoms. They're like variations on a theme in music. They affect your sense of what's real. They change how you think, feel, and act.
It's a psychosis, which means that what seems real to you isn't. You could have:
- Hallucinations: Seeing or hearing things that aren't there.
- Delusions: Mistaken but firmly held beliefs that are easy to prove wrong, like thinking you have superpowers, are a famous person, or people are out to get you.
- Disorganized speech: Using words and sentences that don't make sense to others.
- Strange behavior: Acting in an odd or repetitive way, like walking in circles or writing all the time, or sitting perfectly still and quiet for hours on end.
- Withdrawn and lifeless: Showing no feelings or motivation, or lacking interest in normal daily activities.
People with schizophrenia have at least two of these symptoms for at least 6 months. One of them must be hallucinations, delusions, or disorganized speech. A single voice that offers ongoing comments about your thoughts and actions, or voices that talk to each other, is enough.
There could have been times when you didn't have any symptoms, but the first one would have started at least 6 months ago. And you must have had them for at least a month continuously.
You may have different symptoms at different times, and they may get worse or better -- and it's still schizophrenia.
Doctors may categorize your schizophrenia according to your main symptom to make a diagnosis clearer. But rather than saying you have "paranoid schizophrenia," they would say you have "schizophrenia with paranoia,” for example. Learn more about the symptoms of schizophrenia.
What makes schizophrenia different from some similar disorders in the spectrum is how long you've had symptoms and whether you also have signs of a mood disorder.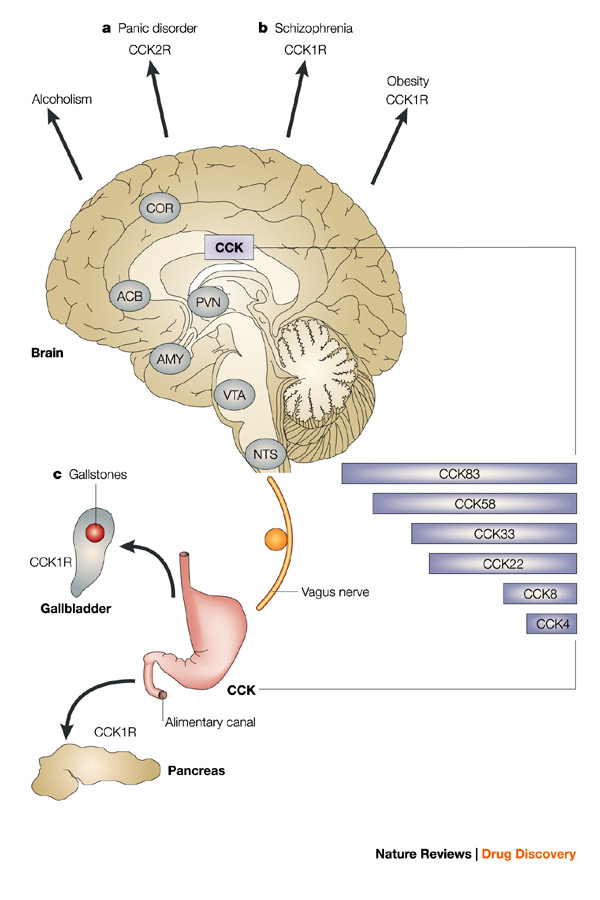
- Schizophreniform: You've had psychotic symptoms for at least a month but less than 6 months. Many people with this disorder go on to have schizophrenia. In other words, schizophreniform is often early schizophrenia. But for about one-third of people, the symptoms just go away.
- Schizoaffective disorder: You’ll have a combination of psychotic symptoms along with depression (major depressive disorder) or bipolar disorder. You could feel very down, or swing between super high-energy or highly irritable and very low, too. Psychotic symptoms have to sometimes happen even when your mood is OK for you to have schizoaffective disorder. This is a rare, serious, lifelong illness.
Read more about the types of psychotic disorders and their symptoms.
© 2020 WebMD, LLC. All rights reserved. View privacy policy and trust infoSchizophrenia
Schizophrenia- Healthcare issues »
- A
- B
- B
- G
- D
- E
- and
- 9000 About
- P
- P
- With
- T
- in
- F
- x
- 9 h
- K.
- S
- B
- E
- S
- I
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find country »
- A
- B
- C
- g
- D
- E
- and
- th
- K
- L
- 9000 N
- 9000
- in
- Ф
- x
- C hours
- Sh
- Sh.
- K
- E 9000 WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Schizophrenia
Key Facts
- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.
- Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life.
- People with schizophrenia are often subject to stigma, discrimination and human rights violations.
- Worldwide, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective care options for patients with schizophrenia that can lead to a complete recovery of at least one in three patients.
Symptoms
Schizophrenia is characterized by significant disturbances in perception of reality and behavioral changes such as:
- persistent delusions: the patient has a persistent belief in the truth of certain things, despite evidence to the contrary;
- persistent hallucinations: the patient hears, sees, touches non-existent things and smells non-existent smells;
- feeling of external influence, control or passivity: the presence in the patient of the feeling that his feelings, impulses, actions or thoughts are dictated from outside, put in or disappear from consciousness at the will of others, or that his thoughts are broadcast to others;
- disorganized thinking, often expressed in incoherent or pointless speech;
- Significant disorganization of behavior, which is manifested, for example, by the patient performing actions that may seem strange or meaningless, or in an unpredictable or inappropriate emotional reaction that does not give the patient the opportunity to organization of their behavior;
- "negative symptoms" such as extreme poverty of speech, smoothness of emotional reactions, inability to feel interest or pleasure, social autism; and/or
- Extreme agitation or, on the contrary, slowness of movements, freezing in unusual postures.
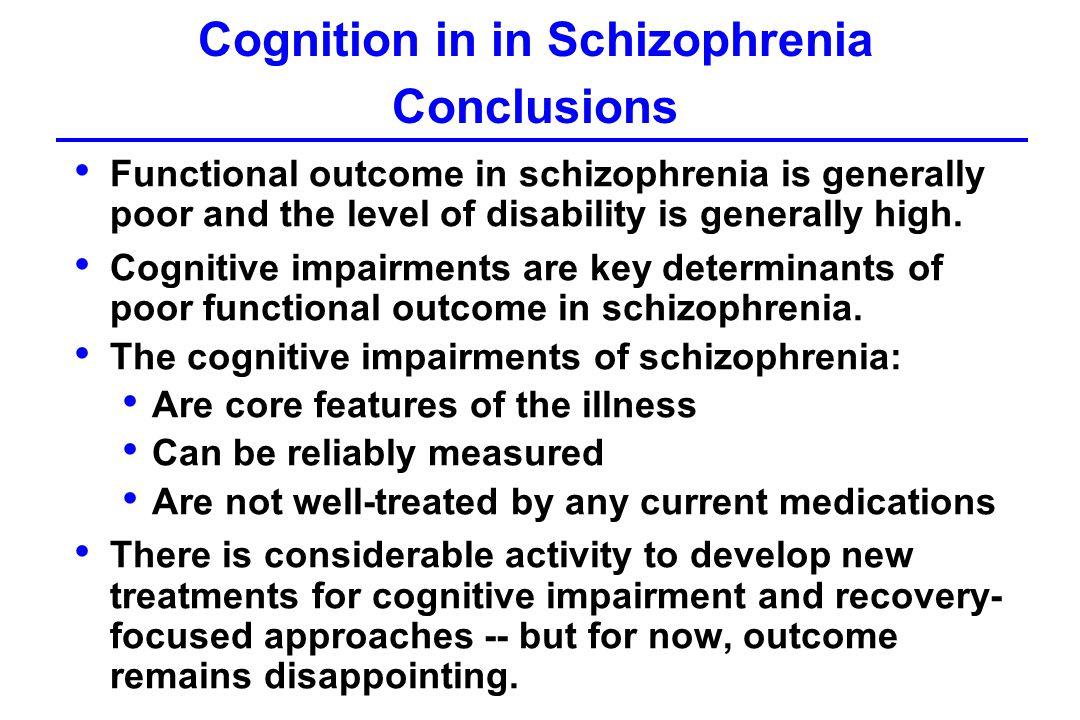
People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms.
Scope and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease.
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.
Individuals with schizophrenia are 2-3 times more likely to die early than the population average (2).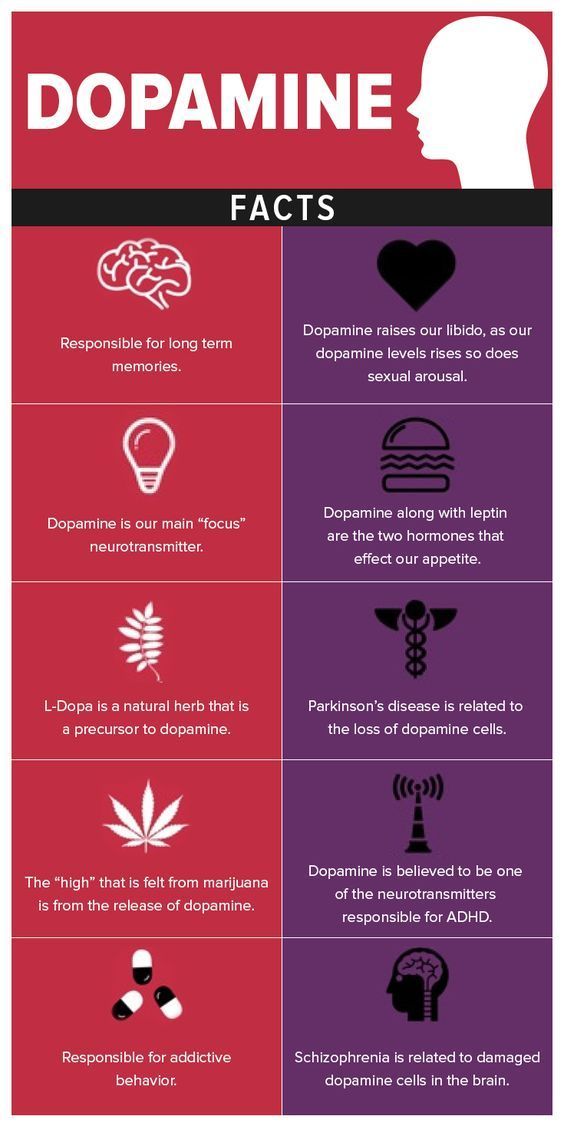 It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment.
Humanitarian emergencies and health crises can cause intense stress and fear, disrupt social support mechanisms, lead to isolation and disruption of health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease. People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion.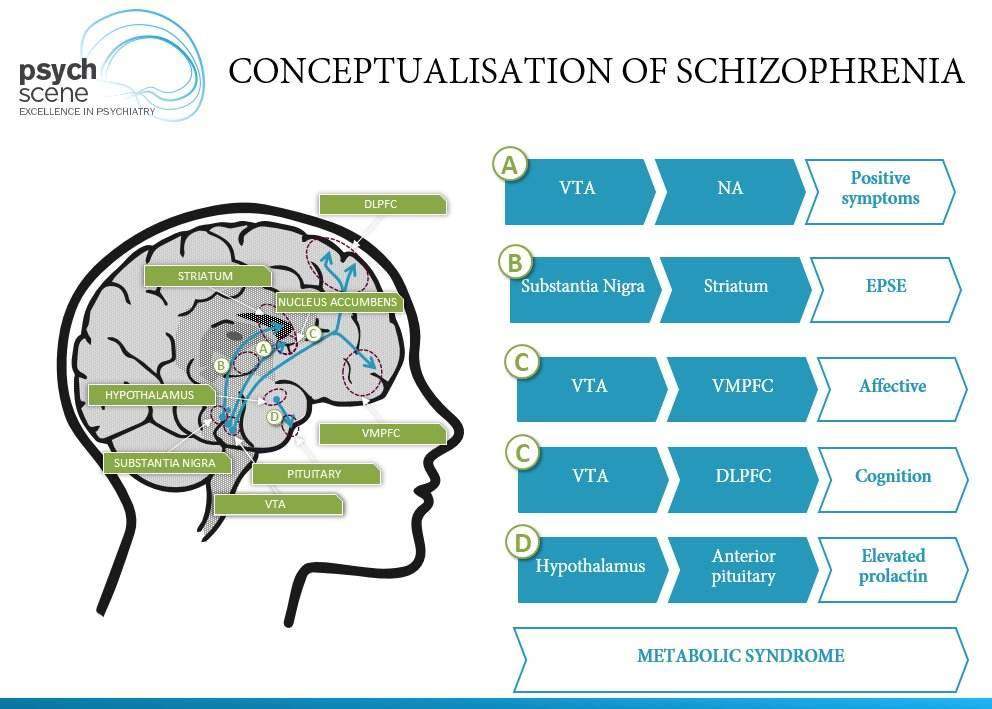
Causes of schizophrenia
Science has not established any one cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.
Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective treatment for mental disorders and is regularly associated with the violation of the basic rights of patients with schizophrenia.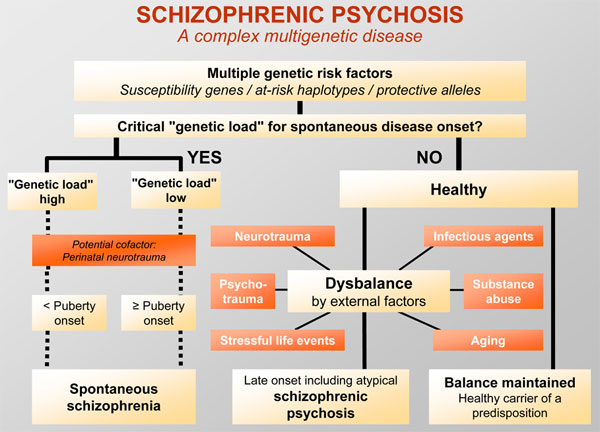 Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is important the patient with schizophrenia, his family members and members of local communities.
Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is important the patient with schizophrenia, his family members and members of local communities.
Schizophrenia management and care
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg, life skills education).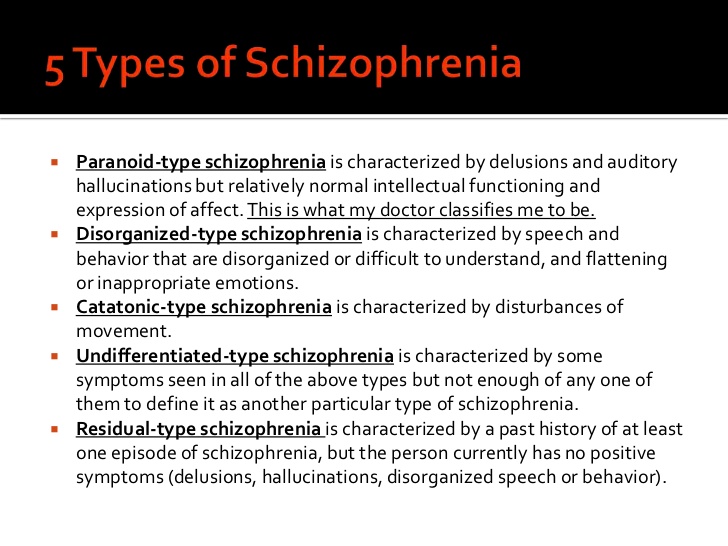 The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
WHO action
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care.
The WHO Mental Health Gap Action Program (mhGAP) is working to develop evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings.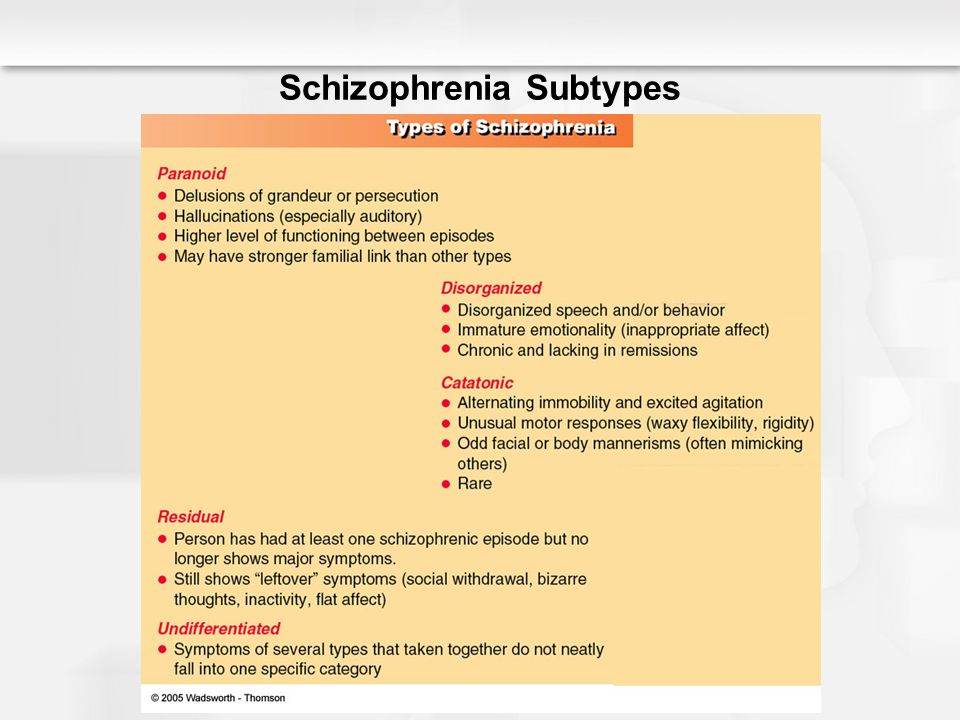 The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services. health in accordance with international human rights standards, including the UN Convention on the Rights of Persons with Disabilities.
Bibliography
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J.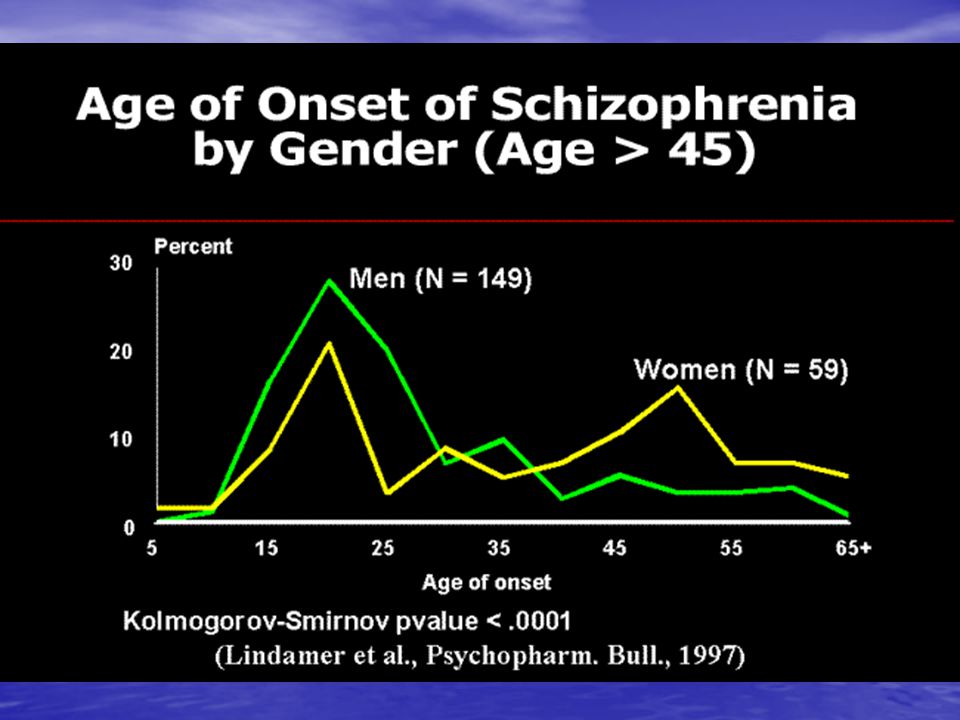 Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
(2) Institute of Health Metrics and Evaluation (IHME). Global Health Data Exchange (GHDx). http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/27a7644e8ad28e739382d31e77589dd7 (accessed 25 September 2021)
(3) LaursenTM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annual Review of Clinical Psychology , 2014;10, 425-438.
(4) WHO. Mental health systems in selected low- and middle-income countries: a WHO-AIMS cross-national analysis. WHO: Geneva, 2009
(5) Jaeschke K et al. Global estimates of service coverage for severe mental disorders: findings from the WHO Mental Health Atlas 2017 Glob Ment Health 2021;8:e27.
Schizophrenia - American Medical Clinic
US
Medical Clinic
St. Petersburg, Moika river embankment, 78.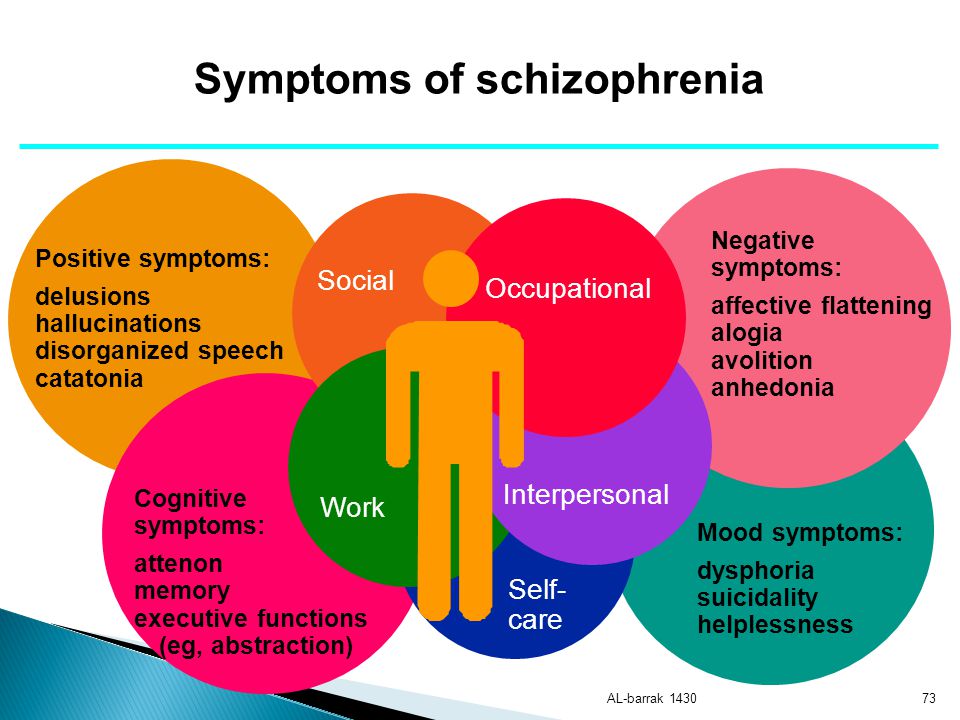
+7 (812) 740-20-90
Contents:
Schizophrenia is a mental disorder in which there is a breakdown of thought processes and emotional reactions. The disease does not cause disturbances in consciousness and does not change many intellectual processes, however, with its prolonged course, perception, memory and attention are disturbed.
Lack of treatment leads to a complete loss of a sense of one's own "I", the loss of the integrity of a person's personality. In order to avoid this, it is necessary to diagnose the signs of schizophrenia in a timely manner and start treatment as soon as possible.
Symptoms of schizophrenia
Schizophrenia develops for a long time and imperceptibly for the patient. The first signs appear when a person is sure that he is completely healthy.
Early symptoms of schizophrenia:
- Isolation from society, unsociableness.
- Indifference to yourself, friends and family.
- Emotional coldness.
- Gradual loss of interest in everything that previously worried.
- Sleep disorders.
Adolescents often experience these symptoms during the transition period. However, in any case, take a closer look at your child and consult a doctor if you suspect.
As the disease progresses, common symptoms and signs of schizophrenia occur:
-
Psychotic (positive):
- Hallucinations - the patient sees and hears what is not there.
- Nonsense - illogical beliefs in which the patient cannot be persuaded.
- Disorderly thinking - the patient either speaks too quickly, then stops in the middle of a thought and at the same time names non-existent words.
- Unnatural movements - a patient with schizophrenia moves slowly and freezes in an unnatural position, or vice versa moves too fast and jerkily.
-
Negative:
- Inability to express emotions - the patient constantly looks depressed and out of touch with reality.
- Impaired thought process - the patient does not absorb information well, cannot concentrate and forgets everything.
- Inability to express emotions - the patient constantly looks depressed and out of touch with reality.
In order to alleviate the situation of the patient, it is necessary to urgently consult a doctor and not push the patient away from himself. Remember that all changes in a person's personality are not his fault, but a manifestation of the disease.
Treatment of schizophrenia
Unfortunately, there is currently no cure for schizophrenia. The doctor can only alleviate the course of the disease. However, this is not a reason to put an end to yourself or your loved one. In the UK, people with schizophrenia even find employment, work successfully and lead a normal life.
From a medical point of view, the ideal solution for the treatment of schizophrenia is the placement of a patient in a hospital. Especially during an exacerbation of the disease. However, it should be borne in mind that hospitalizations are a great stress for a person who is associated with a restriction of freedom.