Is ocd bad
The Impact of OCD | OCD-UK
In popular culture and frequently within the media OCD is mistakenly portrayed as a positive trait and personality quirk, but the reality is, for those that suffer with Obsessive-Compulsive Disorder (OCD), it has a devastating impact on their life.
OCD is a treatable condition, but we would be negligent if we didn’t highlight some of the ways that OCD can and does impact on many people.
As mentioned previously, a disproportionately high number of those affected with OCD, about 50% of all cases, fall into the severe category, with less than a quarter being classed as mild cases.
In fact, OCD can be so debilitating and disabling that the World Health Organisation (WHO) ranked OCD in the top ten of the most disabling illnesses of any kind, in terms of lost earnings and diminished quality of life. The same report also said OCD was the fifth leading causes of disease burden for women aged 15-44 in the developed world.
So when people misuse OCD and make reference to being ‘a little OCD’, in addition to failing to understand that OCD is a disorder, they also fail to realise the impact it has on those that suffer. OCD can be so severe that it can seriously impact on some or all areas of a person’s life, sometimes disrupting or completely ruining:
- Education
- Employment
- Career development
- Relationships with partners, parents, siblings and friends
- Starting a family
- Access to own children
- Quality of life (because of social interaction)
Also, some of the behaviour that people do to cope with OCD (including compulsions) can also have devastating affects, including:
- Physical damage from compulsions (red and raw bleeding skin. Eye damage)
- Substance abuse (self-medicating with alcohol or other substances)
- Terminations (some women have felt they had no choice but to have abortions because of OCD)
OCD can affect people in different ways. Some people may spend much of their day carrying out various compulsions and be unable to get out of the house or manage normal activities. Others may appear to be coping with day-to-day life while still suffering a huge amount of distress from obsessive thoughts. Some people with OCD may carry out their rituals and compulsions in secret or make excuses to avoid social interaction so they can complete compulsions.
Some people may spend much of their day carrying out various compulsions and be unable to get out of the house or manage normal activities. Others may appear to be coping with day-to-day life while still suffering a huge amount of distress from obsessive thoughts. Some people with OCD may carry out their rituals and compulsions in secret or make excuses to avoid social interaction so they can complete compulsions.
The severity of OCD differs markedly from one person to another. Some individuals may be able to hide their OCD from their own family. However, the disorder may have a major negative impact on social relationships leading to frequent family and marital discord or dissatisfaction, separation or divorce. It also interferes with leisure activities and with a person’s ability to study or work, leading to diminished educational and/or occupational attainment and unemployment.
It can be particularly difficult for families when the person with OCD has poor insight into the disorder. In these cases the person will have difficulty recognising that their concerns are excessive, that they may have OCD, or indeed that they may need help.
In these cases the person will have difficulty recognising that their concerns are excessive, that they may have OCD, or indeed that they may need help.
There is also frequent reports of a financial burden on the family.
Finally, in some rare cases, the symptoms of a parent with OCD may directly impact on the well-being of family members, for example, when concerns about contamination lead to extreme hygiene measures.
The impact on family members should also not be underestimated. Loved ones, often unwittingly become entwined in OCD compulsions:
- Offering reassurance
- Avoiding objects or places for fear of triggering their loved one’s OCD
- Carrying out actions (compulsions) for their loved one with OCD, i.e. looking after their baby, taking rubbish out, stripping naked at the door to not spread ‘contamination’.
How the family should deal with such requests will be discussed in another chapter.
Whilst we must not dismiss what a devastating impact OCD has, it’s worth noting that with successful treatment, people don’t just improve their quality of life, many move on to recovery.
What to read next:
How common is OCD?
Social and Economic Impact of OCD
Page information
[lastreviewed]
[nextreviewed]
Disclaimer: This article is for information only and should not be used for the diagnosis or treatment of Obsessive-Compulsive Disorder or any other medical condition. OCD-UK have taken all reasonable care in compiling this information, but always recommend consulting a doctor or other suitably qualified health professional for diagnosis and treatment of Obsessive-Compulsive Disorder or any other medical condition.
Obsessive-Compulsive Disorder (OCD) (for Teens)
What Is OCD?
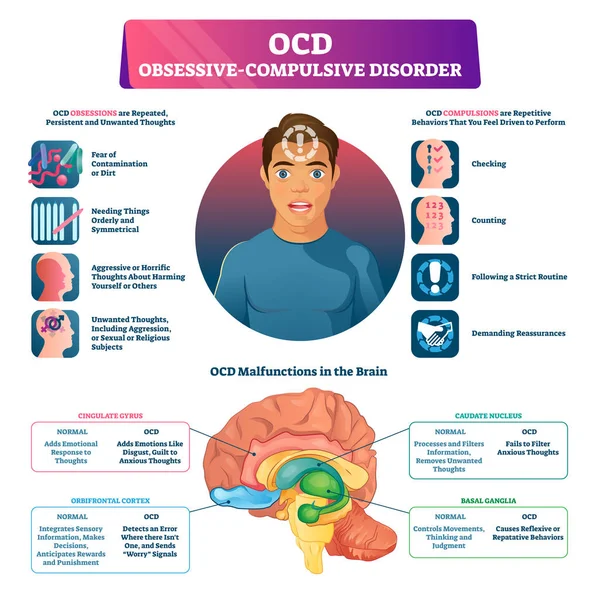
OCD is a mental health condition. It causes thoughts called obsessions, anxiety, and actions called compulsions (also called rituals). People with OCD feel stuck in a stressful cycle of these thoughts and actions.
Cognitive behavioral therapy helps people get past the cycle of OCD. They learn to deal with bothersome thoughts, calm anxiety, and face fears safely without doing rituals. Some people also take medicine for OCD.
If you think you have OCD, talk to a parent or adult in your life. Ask them to help you see a doctor or mental health provider to find out more. If you do have OCD, work with your doctor or therapist to learn and practice the skills that are proven to help OCD get better.
What Are Obsessions?
Obsessions are thoughts that cause anxiety. They can be fear thoughts about bad things that could happen. Or thoughts about how things have to be. They can be nagging doubts about whether things are OK. Or images or ideas about things that seem scary, bad, or wrong.
OCD causes these stressful thoughts to come to mind over and over. They can be about anything, but for many people with OCD, they are thoughts about:
- germs, injury, harm, or illness
- things that seem bad, rude, or wrong
- whether things are even, straight, or placed just as they 'should' be
- colors or numbers that seem bad, unlucky, or have special meaning
- whether something might come true
What Are Compulsions?
Compulsions are behaviors people with OCD feel a strong urge to do. They are also called rituals. To someone with OCD, rituals seem like the way to stop the thoughts, fix things, be safe, or make sure bad things won't happen. Rituals can be actions, or they can be things people say in their head.
They are also called rituals. To someone with OCD, rituals seem like the way to stop the thoughts, fix things, be safe, or make sure bad things won't happen. Rituals can be actions, or they can be things people say in their head.
Here are some examples of rituals. Someone with OCD might feel like they have to:
- wash and clean over and over
- erase, rewrite, or start over a lot
- repeat words, phrases, or questions
- check and re-check if something is closed, locked, clean, right, or finished
- touch, tap, or step in an unusual way or a set number of times
- put things in just the right order, do things a set way
- avoid things, such as numbers or colors that seem unlucky
What's It Like for Someone With OCD?
Most people with OCD can tell that the thoughts and rituals don't make sense. But OCD leads them to feel unsure. They feel a strong urge to do the ritual. They feel if they don't, something bad could happen. At first, rituals give some relief from the bad thoughts and feelings.
At first, rituals give some relief from the bad thoughts and feelings.
But rituals multiply. They take more time and energy. And the worry thoughts keep coming back. This is how OCD becomes a stressful cycle. Instead of stopping OCD, the rituals keep it going.
Someone with OCD will spend more than an hour a day bothered by worry thoughts and rituals. They may check, arrange, fix, erase, count, or start over many times, just to feel that things are OK. They don't want to think about these things. But OCD makes the thoughts hard to ignore. They don't want to do rituals. But OCD makes them feel they have to.
OCD can show up in many parts of their life. Things like getting dressed, having breakfast, or doing schoolwork seem full of stressful choices. OCD can make it seem like one choice might prevent a bad thing. Or that another choice might make a bad thing happen.
Someone with OCD may not know why they think, feel, and do these things. They may try to hide their fears and rituals.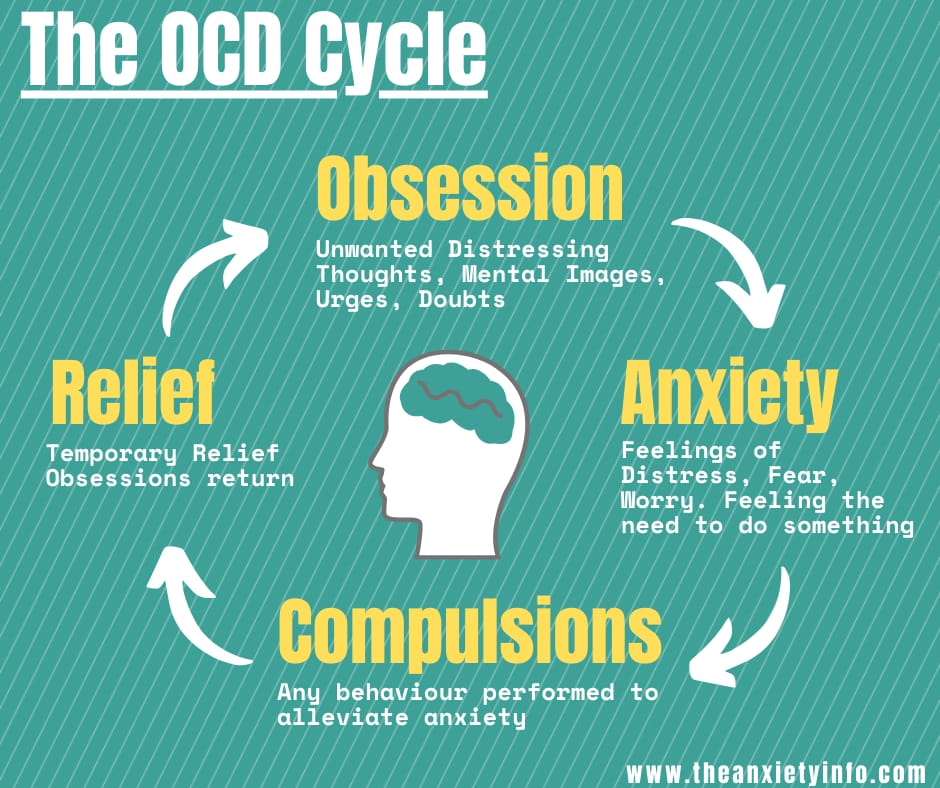 They may worry what others will think. They may even think they are going 'crazy' — but they're not. OCD can cause this to happen.
They may worry what others will think. They may even think they are going 'crazy' — but they're not. OCD can cause this to happen.
Why Do Some People Get OCD but Others Don't?
Like in many health conditions, a person's
genesplay a role in whether they get OCD. That's why OCD often runs in families. Genes can affect the chemistry, structure, and activity in different parts of the brain. With OCD, these differences lead unwanted thoughts to get 'stuck' instead of move on. OCD gets started because someone has genes that make it more likely.
But OCD keeps going because of rituals. The more people do rituals, the stronger OCD gets. This happens because our brains learn to do more of what we practice. Our brains also learn to do more of what gets rewarded. In OCD, rituals 'reward' the brain with a feeling of relief.
What Is the Treatment for OCD?
The treatment for OCD is a type of cognitive behavioral therapy (CBT). In therapy, people meet with a therapist to talk, learn, and practice skills. Along with therapy, some people may take medicine for OCD.
In therapy, people meet with a therapist to talk, learn, and practice skills. Along with therapy, some people may take medicine for OCD.
In therapy, people might learn:
- how thoughts, feelings, and behaviors affect each other
- how OCD is like a brain 'trick' making it seem like bad things will happen unless people do rituals
- that doing rituals keeps OCD going strong
- that not doing rituals weakens OCD
But even when someone with OCD knows this, it's not easy to just stop doing rituals. That's why therapy teaches skills like:
- coping and calming skills for anxiety
- how to deal with worry thoughts
- how to face fears safely
- how to resist doing rituals
In therapy, people practice using these skills. One by one, they face fears without doing rituals. This can feel uncomfortable at first, but it quickly gets easier with practice. The more people with OCD resist rituals, the more worry thoughts can fade. As the person practices their skills, the brain's activity can change for the better.
As the person practices their skills, the brain's activity can change for the better.
Therapy takes time — how long depends on the person. Most people work with their therapist each week for a few months or more. Some people have therapy more often.
The therapist will teach, support, and encourage along the way. Often, the therapist will work with a parent, too. Parents want to know how to best help when OCD fears or rituals happen at home.
What Should I Do if I Think I Have OCD?
If you think you might have OCD:
- Tell a parent or adult in your life what you're going through. They can take you to your doctor or mental health provider to find out if you have OCD. It can be a relief to know what's causing the symptoms. And to find out there's therapy that works for OCD.
If you find out you have OCD:
- Go to therapy. Learn about OCD. The more you learn, the better you'll understand it.
- Practice the skills you learn in therapy.
 The more you practice, the better and sooner you'll be able to overcome OCD.
The more you practice, the better and sooner you'll be able to overcome OCD. - Get support from people who care. Let a parent help you practice what you learn in therapy. Share your success and progress along the way.
- Be patient with yourself. Dealing with OCD is tiring and stressful. And therapy takes time and practice. But many people like you have overcome OCD. You can, too.
- Make time for good things. Find a little time to relax and do things you enjoy. Be with people who make you laugh and feel good. This helps you through the tough moments and gives you energy to overcome OCD.
Reviewed by: D'Arcy Lyness, PhD
Date reviewed: July 2021
Obsessive Compulsive Disorder Treatment
Great Thought is an obsessive compulsive disorder treatment program. We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
Symptoms of obsessive-compulsive disorder
- Frightening images and drives
- Compulsive acts (rituals)
- Intrusive check of one's own actions
- Fear of trouble, pollution or infection
- Inexplicable desire to count something
- Excessive organization and pedantry
- Perfectionism in relationships, work and even leisure
- "Stuck", "looping" on one's thoughts
You feel that over time your mood becomes worse: apathy, depression, obsessions increase, and rituals begin to fill all your free time or harm your physical health.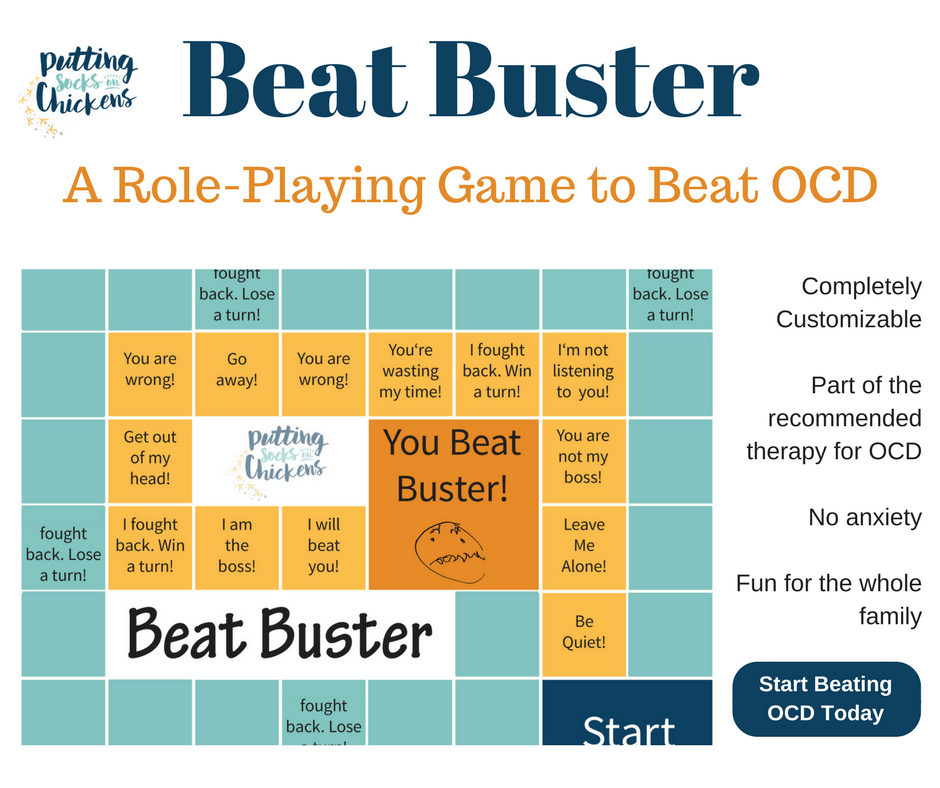
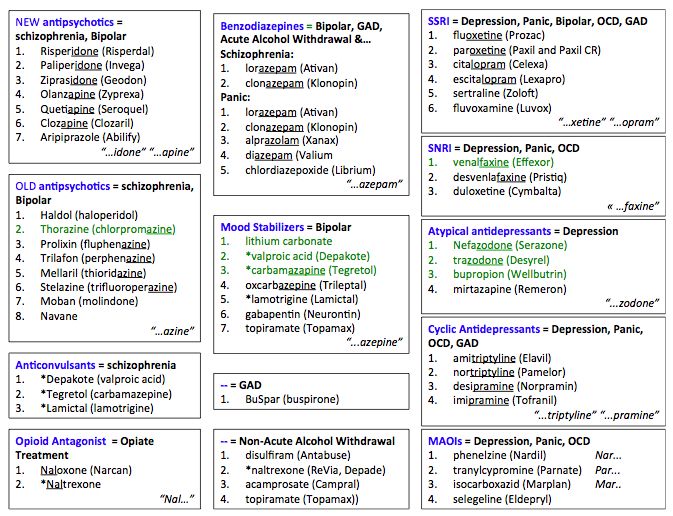
You may have had more than one meeting with psychologists, psychotherapists and psychiatrists. You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder is a syndrome characterized by the presence of obsessive thoughts (obsessions) to which a person reacts with certain actions (compulsions). The causes of the disorder are rarely superficial. The syndrome is also accompanied by the development of obsessive memories and various pathological phobias. May be chronic, episodic or progressive.
Obsession - obsessive thought, persistent desire for something, uncontrollable and accompanied by anxiety and intense anxiety. In an attempt to cope with such thoughts, a person resorts to committing compulsions.
Compulsion - an irresistible need to perform certain actions (rituals), which can be assessed by the person himself as irrational or meaningless, and the internal need to perform them is forced and is the result of obsessive ideas.
Common examples of OCD manifestations
- An exaggerated sense of danger. Fear of the materiality of thoughts:
- "now I will lose control and hurt my loved ones"
- "something terrible is about to happen, I can feel it"
- "I shouldn't think like that, all this will come true because of me"
- Pathological fear of pollution. Thirst for Purity
- Excessive perfectionism, exaggerated responsibility - "everything must be done perfectly", "everything depends on me, mistakes are unacceptable"
How does this painful algorithm work?
Most people have unwanted or obsessive thoughts quite often, but all sufferers of the disorder greatly exaggerate their importance.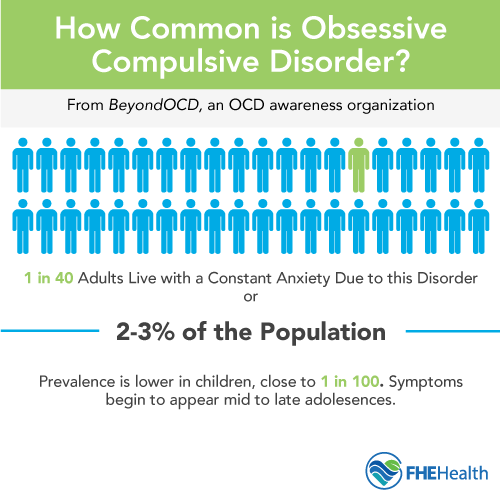 Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
As we noted earlier, repetitive avoidance behavior can "get stuck", "loop", that is, have a tendency to repeat. The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
If you periodically experience over the years:
- Constant or fluctuating anxiety
- The need to perform certain ritualized actions
- A persistent decline in the quality of life due to the need to avoid certain thoughts and actions, places and events
And you are also persecuted:
- Significant problems in studies and career
- Failure to establish a serious relationship
- Constant criticism and pressure from relatives
- Many senseless activities
- Excessive involvement in computer games and the Internet, alcohol
- Loneliness and isolation
We strongly recommend that you do not delay seeking help and that you complete a remedial program.
Consultations and psychotherapeutic sessions according to the program are held several times a week, until the relief of severe symptoms, then the frequency of meetings with specialists is reduced to 2–3 per month. Count on the fact that in the end we will deal with your problem together.
Treatment of obsessive-compulsive disorder in Neuro-Psi
Every day, the specialists of the NEURO-PSI clinic analyze the world practice in the field of psychiatry and psychotherapy. The goal is the impartial selection and implementation of those methods of treatment and psychological assistance, the effectiveness of which has been convincingly proven in independent studies.
We are guided by the principles of evidence-based medicine and use as a basic method of treatment a psychotherapeutic paradigm, the effectiveness of which has been widely recognized by the professional community.
1. What is the essence of the obsessive-compulsive disorder treatment program
Since obsessive thoughts, rituals and conditions are only symptoms of mental dysfunction, the root cause must be treated in order to achieve a stable result. A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
The main emphasis is on teaching the client how to properly respond to his thoughts, emotions, inner feelings and interpretation of external events.
All types of psychotherapeutic and drug treatments serve the same goal: to achieve the best result in the shortest possible time. At the same time, by coordinating the efforts of specialists in various fields, the most complete coverage of all types of mental illnesses, disorders and disorders is possible.
2. What treatments are used
- Priority:
- Cognitive-Behavioral Therapy.
- Schema Therapy.
- Reality Therapy.
- Choice Theory.
- Rational pharmacotherapy.
- Psychopharmacotherapy (if indicated)
- Biofeedback Therapy
- Rational psychocorrection of stress
- Jacobson progressive muscle relaxation.

- Traditional and modern gymnastic systems, relaxation techniques.
- Breathing techniques .
- Stress exposure.
- Self-control training.
- Jacobson progressive muscle relaxation.
- Lifestyle modification
- Work with bad habits.
- Diet correction.
- Professional and social adaptation.
3. How is the treatment under the program
Each treatment program at the NEURO-PSI clinic consists of four stages:
- diagnostics,
- work with disease symptoms,
- work with the causes of the disease,
- consolidation of the achieved results.
Work efficiency is increased by dividing the treatment process into a predetermined number of sessions, at convenient times and without hospitalization. This means that each program is adapted to the problem that the client has addressed.
The program method of treatment is predictable, time-limited, productive, and, most importantly, understandable for the client.
Of course, the treatment takes place in a comfortable mode without interruption from work, study or family. Specialists of various profiles will work with you (team method). This is necessary to minimize the risk of diagnostic errors that could lead to the adoption of a suboptimal treatment plan.
Improvements in well-being and mood (healing) occur in stages: after the decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future.
4. What are the results and prognosis?
Upon completion of the program, you get rid of obsessive thoughts and rituals, fear of pollution, unmotivated fears, panic attacks and multiple vegetative symptoms (sudden jumps in blood pressure, heart palpitations, dizziness, nausea).
According to statistics, the effectiveness of the methods used approaches 100% if all recommendations of specialists are followed.
Skills you acquire during the program:
- self-control and self-regulation
- constructive analysis of the state of the body
- understanding one's own mental and emotional sphere
- ability to control one's attention
- ability to act consciously in stressful situations
Significantly improves the emotional and physical condition, gains self-confidence, in the future.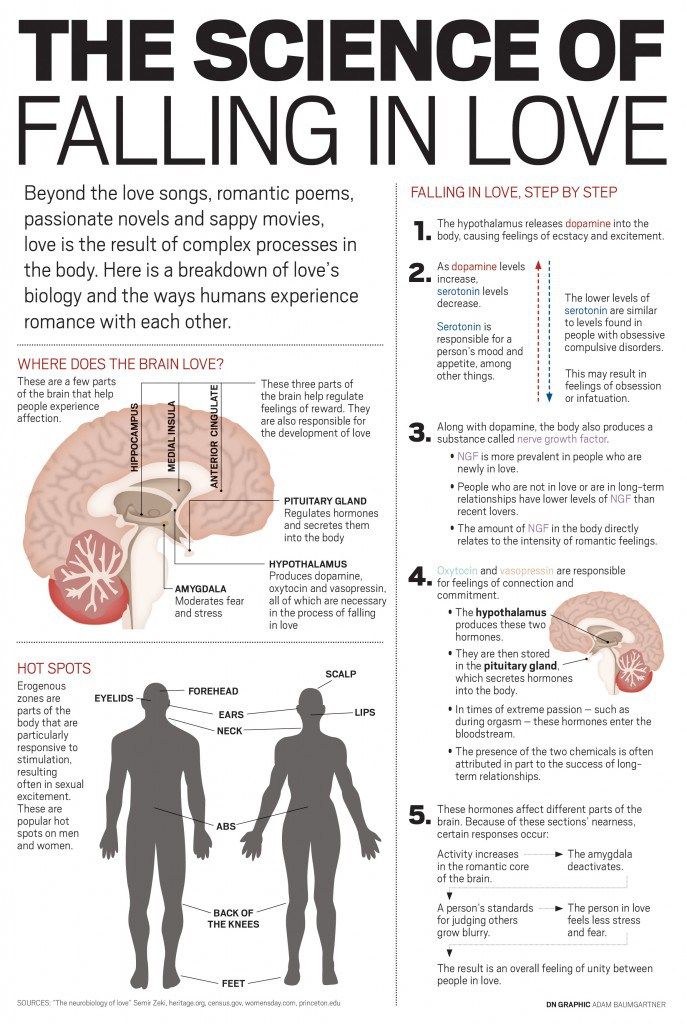 Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
5. Where to start taking the course
In order for you to know the treatment plan, we recommend signing up for a diagnostic (first) consultation.
Obsessive Compulsive Disorder Treatment
Great Thought is an obsessive compulsive disorder treatment program. We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
Symptoms of obsessive-compulsive disorder
- Frightening images and drives
- Compulsive acts (rituals)
- Intrusive check of one's own actions
- Fear of trouble, pollution or contamination
- Inexplicable desire to count something
- Excessive organization and pedantry
- Perfectionism in relationships, work and even leisure
- "Stuck", "looping" on one's thoughts
You feel that over time your mood becomes worse: apathy, depression, obsessions increase, and rituals begin to fill all your free time or harm your physical health.
You may have had more than one meeting with psychologists, psychotherapists and psychiatrists. You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder is a syndrome characterized by the presence of obsessive thoughts (obsessions) to which a person reacts with certain actions (compulsions). The causes of the disorder are rarely superficial. The syndrome is also accompanied by the development of obsessive memories and various pathological phobias. May be chronic, episodic or progressive.
Obsession - obsessive thought, persistent desire for something, uncontrollable and accompanied by anxiety and intense anxiety. In an attempt to cope with such thoughts, a person resorts to committing compulsions.
Compulsion - an irresistible need to perform certain actions (rituals), which can be assessed by the person himself as irrational or meaningless, and the internal need to perform them is forced and is the result of obsessive ideas.
Common examples of OCD manifestations
- An exaggerated sense of danger. Fear of the materiality of thoughts:
- "now I will lose control and hurt my loved ones"
- "something terrible is about to happen, I can feel it"
- "I shouldn't think like that, all this will come true because of me"
- Pathological fear of pollution. Thirst for Purity
- Excessive perfectionism, exaggerated responsibility - "everything must be done perfectly", "everything depends on me, mistakes are unacceptable"
How does this painful algorithm work?
Most people have unwanted or obsessive thoughts quite often, but all sufferers of the disorder greatly exaggerate their importance. Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
As we noted earlier, repetitive avoidance behavior can "get stuck", "loop", that is, have a tendency to repeat. The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
If you periodically experience over the years:
- Constant or fluctuating anxiety
- The need to perform certain ritualized actions
- Persistent decline in quality of life due to the need to avoid certain thoughts and actions, places and events
And you are also persecuted:
- Significant problems in studies and career
- Failure to establish a serious relationship
- Constant criticism and pressure from relatives
- Many senseless activities
- Excessive involvement in computer games and the Internet, alcohol
- Loneliness and isolation
We strongly recommend that you do not delay seeking help and that you complete a remedial program.
Consultations and psychotherapeutic sessions according to the program are held several times a week, until the relief of severe symptoms, then the frequency of meetings with specialists is reduced to 2–3 per month. Count on the fact that in the end we will deal with your problem together.
Treatment of obsessive-compulsive disorder in Neuro-Psi
Every day, specialists of the Neuro-Psi clinic analyze the world practice in the field of psychiatry and psychotherapy. The goal is the impartial selection and implementation of those methods of treatment and psychological assistance, the effectiveness of which has been convincingly proven in independent studies.
We are guided by the principles of evidence-based medicine and use as a basic method of treatment a psychotherapeutic paradigm, the effectiveness of which has been widely recognized by the professional community.
1. What is the essence of the obsessive-compulsive disorder treatment program
Since obsessive thoughts, rituals and conditions are only symptoms of mental dysfunction, the root cause must be treated in order to achieve a stable result. A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
The main emphasis is on teaching the client how to properly respond to his thoughts, emotions, inner feelings and interpretation of external events.
All types of psychotherapeutic and drug treatments serve the same goal: to achieve the best result in the shortest possible time. At the same time, by coordinating the efforts of specialists in various fields, the most complete coverage of all types of mental illnesses, disorders and disorders is possible.
2. What treatments are used
- Priority:
- Cognitive-Behavioral Therapy.
- Schema Therapy.
- Reality Therapy.
- Choice Theory.
- Rational pharmacotherapy.
- Psychopharmacotherapy (if indicated)
- Biofeedback Therapy
- Rational psychocorrection of stress
- Jacobson progressive muscle relaxation.

- Traditional and modern gymnastic systems, relaxation techniques.
- Breathing techniques .
- Stress exposure.
- Self-control training.
- Jacobson progressive muscle relaxation.
- Lifestyle modification
- Work with bad habits.
- Diet correction.
- Professional and social adaptation.
3. How is the treatment under the program
Each treatment program at the NEURO-PSI clinic consists of four stages:
- diagnostics,
- work with disease symptoms,
- work with the causes of the disease,
- consolidation of the achieved results.
Work efficiency is increased by dividing the treatment process into a predetermined number of sessions, at convenient times and without hospitalization. This means that each program is adapted to the problem that the client has addressed.
The program method of treatment is predictable, time-limited, productive, and, most importantly, understandable for the client.
Of course, the treatment takes place in a comfortable mode without interruption from work, study or family. Specialists of various profiles will work with you (team method). This is necessary to minimize the risk of diagnostic errors that could lead to the adoption of a suboptimal treatment plan.
Improvements in well-being and mood (healing) occur in stages: after the decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future.
4. What are the results and prognosis?
Upon completion of the program, you get rid of obsessive thoughts and rituals, fear of pollution, unmotivated fears, panic attacks and multiple vegetative symptoms (sudden jumps in blood pressure, heart palpitations, dizziness, nausea).
According to statistics, the effectiveness of the methods used approaches 100% if all recommendations of specialists are followed.
Skills you acquire during the program:
- self-control and self-regulation
- constructive analysis of the state of the body
- understanding one's own mental and emotional sphere
- ability to control one's attention
- ability to act consciously in stressful situations
Significantly improves the emotional and physical condition, gains self-confidence, in the future.