Levels of mental health
A guide to understanding mental health levels of care at Rogers Behavioral Health
Posted on 06/09/20 04:26:pm
Share this article:
Understanding the different terms used to describe mental health treatment can be a little confusing at times. Not sure how inpatient is different from residential or which level of care at Rogers is right for you? See our explanations below for each type of treatment.
Inpatient
Inpatient is our highest level of care, which provides mental and physical stabilization during an acute episode. Inpatient care is for people who are in emergency situations and intend to harm themselves, need to regain nutrients or achieve a healthy intake of food, or who need to withdraw from drugs or alcohol. Our multidisciplinary team creates a care plan for each patient to help stabilize symptoms and get through the crisis and a plan for continued treatment.
A typical length of stay in inpatient varies, but the average is three to seven days with a longer stay often required for those with an eating disorder, depending on severity. Once stable, our care team works to transition patients to the appropriate level of care for the next step in their treatment.
Residential
In residential care at Rogers, patients live on campus in our supportive environment while receiving intensive treatment for an average of 30 to 90 days. Patients in residential care are medically stable and focus on building the skills needed for long-term recovery. Residential care at Rogers can be found in Oconomowoc and West Allis, both in the Milwaukee area in Wisconsin.
Partial hospitalization
Patients in our partial hospitalization care (PHP) come in for treatment five days a week typically for six hours each day. This level of care is sometimes referred to as “day treatment.” Patients will often step down from inpatient or residential to partial hospitalization, which is shown to have the best short-term and long-term clinical outcomes with reduced readmission at a future date. PHP is currently also offered virtually through Rogers Connect Care.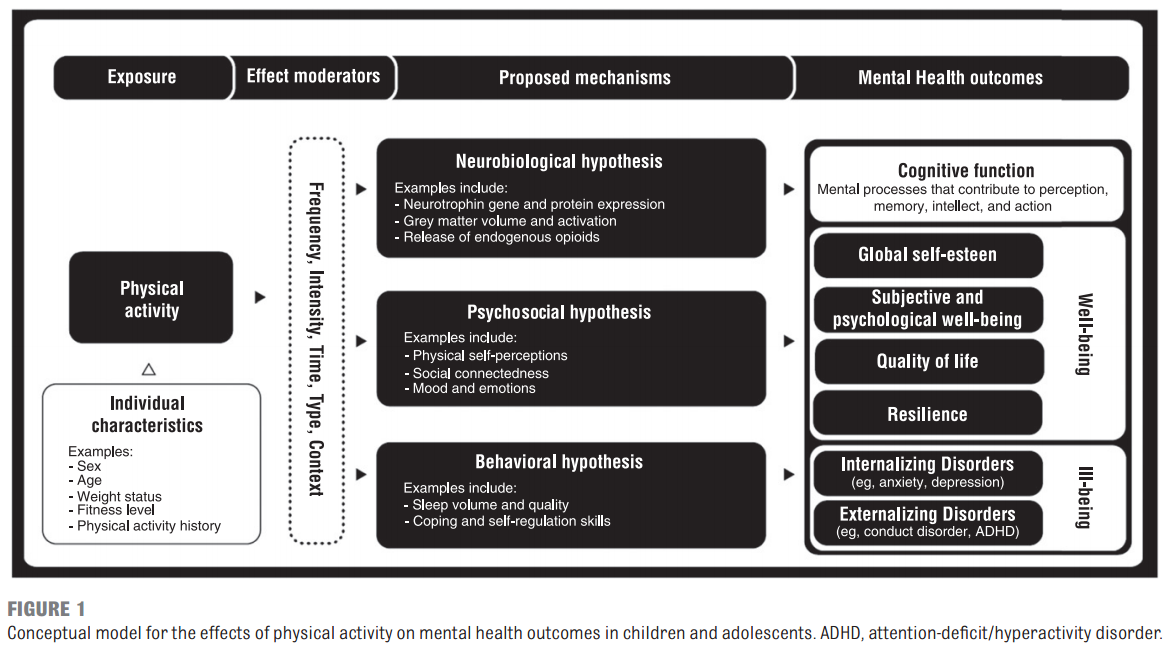 Learn more here.
Learn more here.
Intensive outpatient
Rogers’ intensive outpatient care (IOP) is our lowest level of care where patients come in for treatment five days a week for three hours each day. Patients at this level of care still experience group and individual therapy, meet with psychiatrists, participate in experiential therapy, and other treatment modalities. Virtual treatment is also available for IOP.
Outpatient
Traditional outpatient care where someone meets with a therapist or psychiatrist once or twice a week is not offered at Rogers. As symptoms improve, patients will reduce the frequency of appointments until it’s safe to discontinue or only come in occasionally. Patients who leave our care return to their outpatient providers or we can make a referral when needed. Likewise, if an outpatient provider is treating someone who requires a higher level of care, they will refer to Rogers.
If you are still unsure what type of treatment may be right for you, call 800-767-4411 to request a free, confidential screening.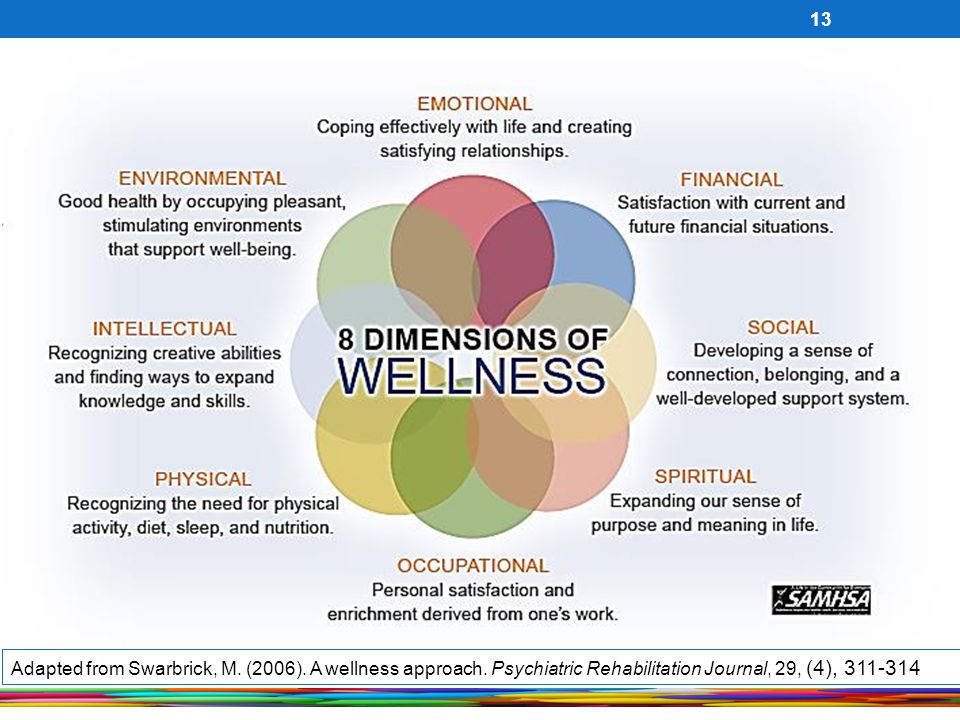 You can also request a screening 24/7 online at https://rogersbh.org/screening-request.
You can also request a screening 24/7 online at https://rogersbh.org/screening-request.
A Guide to Understanding the Levels of Psychiatric Care
As a clinical social worker, I have worked with many patients and families who ask why their outpatient treatment is not working. Is it that the psychiatrist/therapist is incompetent? Is their family member simply “not trying hard enough?” Often, the answer to this question is that the symptoms of the person receiving care are too severe for the level of care that they are engaging with.
The problem is that the people with the most information about the patient, the family, do not always know or understand the different levels of care available to help their loved one. Therefore, their experience is one of helplessness and hopelessness.
Here, we explore the different levels of psychiatric care available in the United States that may help families navigating these difficult situations. Unfortunately, not all the programs described below are available in every part of the country.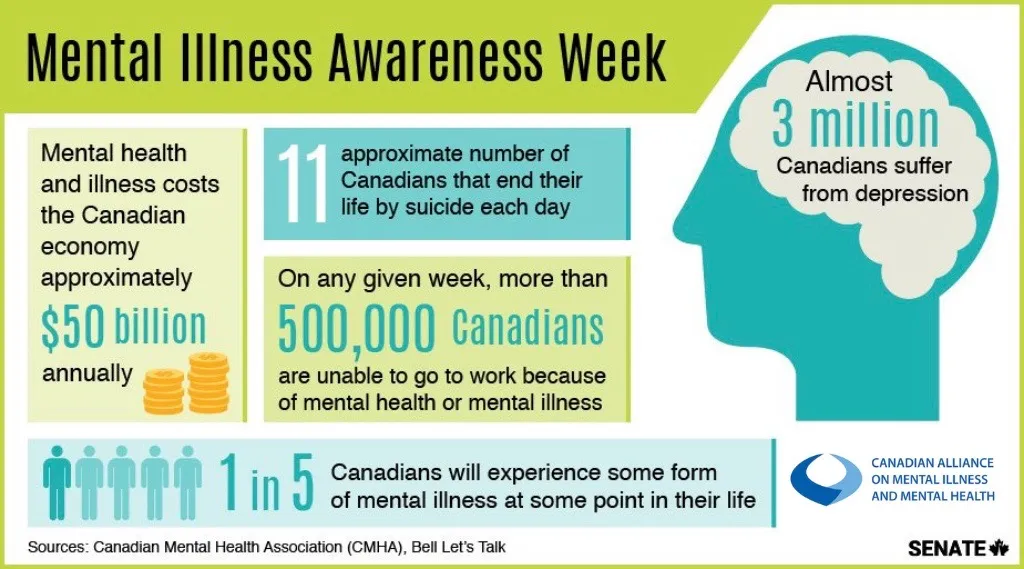 We hope this post is a mini "guide" to understanding different levels of mental health care (see diagram).
We hope this post is a mini "guide" to understanding different levels of mental health care (see diagram).
Outpatient Level of Care
This is the level of care most people are familiar with. A patient may go see their psychiatrist a few times per month for medication management. The patient may also go see a therapist (for some patients this may be their psychiatrist) once a week or more depending on their symptoms and overall goals. If a person going into outpatient care has severe symptoms, the providers involved may choose to increase the frequency of visits. If this is not effective, it may be time to consider a higher level of care.
Intensive Outpatient Program (IOP)
In general, an IOP is three days out of the week for at least three hours per day. The programs can vary, possibly being more days and more hours. These programs will focus on group work to help the patient develop additional skills to manage their symptoms. The IOP can include medication management services, although not always.
Partial Hospitalization Program (PHP) or “Day Treatment”
These types of programs are five days out of the week for six to eight hours per day. The program will focus on group work and forming a patient community, as well as psychiatric care. A PHP is normally more days than an IOP and will include psychiatric assessment and care. At this point in their care, patients, their families and their providers have identified that treatment needs to be the primary focus rather than work or other family responsibilities.
Community Integration Program/Extended Care
In this level of care, patients are living in a shared therapeutic space with other patients, but the treatment does not happen in the space where the patients live. At Menninger’s Pathfinder Program, residents live in an apartment setting where there is support from resident advisors; however, group therapy and individual therapy happen in a separate location. This type of care allows the patient to maintain a certain level of independence and to focus on increasing their interaction with the community.
Psychiatric Assertive Community Treatment (PACT)
This level of care can best be described as a hospital without walls. In this model of care, one of the primary goals is to keep a person from being hospitalized. It may work well for people who have had multiple hospitalizations in their past and are trying to break that pattern. In PACT, the patients live in their own home/apartment and the clinicians come to the patient, rather than the other way around. Although the PACT model is becoming better known, this is a level of care that is difficult to find outside of major cities.
Residential Level of Care
In this level of care, patients are living in the place where they are receiving treatment. This type of environment can create a safe environment for patients whose functioning is significantly impacted by their symptoms to the point where they are unable to live at home and make progress in their treatment. Resident advisors provide 24-hour monitoring and support.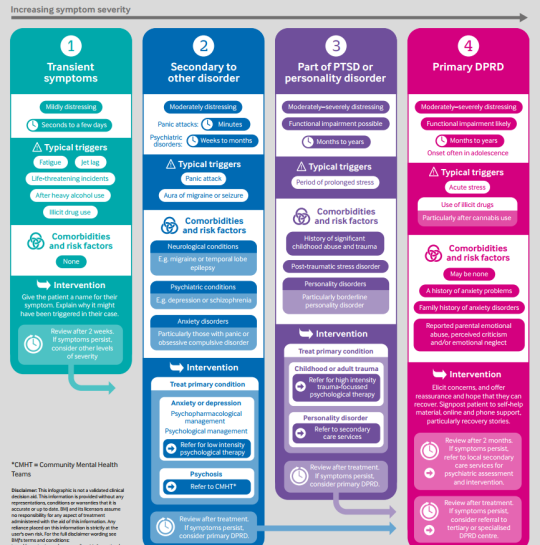
Sub-acute Hospital Care
This is a level of care that is no longer available in most of the country. In this level of care, a patient is hospitalized for a longer period. At the Menninger Clinic, patients stay in most programs for four to six weeks. There are other psychotherapeutic hospitals where patients might stay with the program for much longer, sometimes years. These types of hospital stays are designed to help the patient stabilize their symptoms but also begin to identify and address some of the more significant core issues that have impacted the person's life. Psychiatric nursing staff provide 24-hour care.
Acute Care Hospital
This level of care offers the highest level of containment. Usually, people who are imminently suicidal or are experiencing acute psychotic/manic symptoms where they pose a safety risk utilize acute hospitalization. The environment is very restrictive as a result. These hospital stays are short, perhaps three to five days.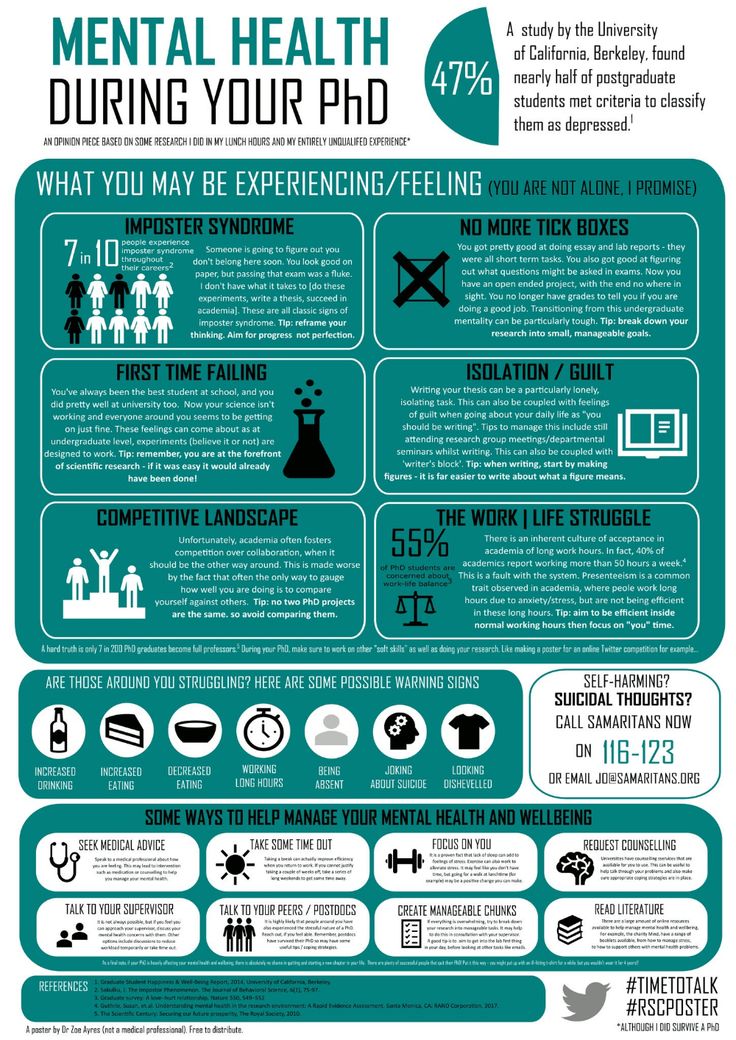 The focus is stabilization and safety. Often, patients and families may feel disappointed in the experience and feel that the core issues were not addressed. An acute hospital stay is not designed to address larger core issues; therefore, outpatient follow-up care is crucial to ensure the best outcome.
The focus is stabilization and safety. Often, patients and families may feel disappointed in the experience and feel that the core issues were not addressed. An acute hospital stay is not designed to address larger core issues; therefore, outpatient follow-up care is crucial to ensure the best outcome.
A patient can move up the continuum of care as needed, or perhaps they end up in acute care and then move down the continuum as they stabilize. It is important to consider an alternative level of care if a patient is not making progress at their current level of care. If someone feels stuck in their mental health, it would be beneficial for them to look at the level of care they are receiving services at and decide if it is what works best for their needs. It is possible a move in the level of care would dramatically help their mental health.
Note: This content first appeared on Mind Matters from Menninger, our blog on PsychologyToday. com.
com.
Mental health levels
09/27/2011
In psychiatry, it is especially clear that the concepts of "mental health" and "mental norm" are not identical. So, S. B. Semichev (1987) identified five degrees of mental health.
1. Ideal norm or reference health - a condition in which the probability of occurrence of mental and behavioral disorders or mental maladaptation is equal to zero. Theoretically, it is assumed that all the numerous indicators characterizing the state of a person’s mental health correspond to the reference norm, there is a complete psychosocial adaptation of the individual, and the personality is harmoniously developed. This hypothetical mental state is akin to an "ideal gas" in physics. “Harmonic natures are for the most part a product of the imagination,” P.B. Gannushkin wrote at the dawn of the 20th century.
The WHO defines an ideal norm as a behavior supported by a cultural group because it is desirable or optimal.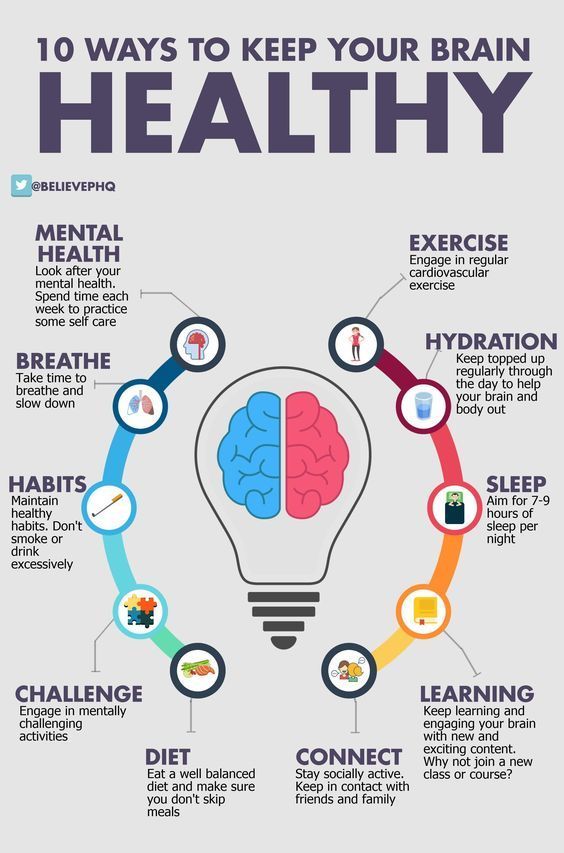 It is a socially prescribed pattern of behavior.
It is a socially prescribed pattern of behavior.
2. Average statistical norm is the state of psychological and psychiatric characteristics that reflect the norm for a certain population. These characteristics are distinguished when studying a specific population (taking into account gender, age, social status, sociocultural characteristics of the region of residence, etc.). In this state, there is a likelihood of mental and behavioral disorders, as well as mental maladaptation, which increases dramatically during times of historical transformation and during periods of crisis in a person’s life and during macrosocial upheavals.
It should be noted that the condition, which for one population can be qualified as an average statistical norm, for another is an indicator of a mental or behavioral disorder. For example, unexpressed intellectual-mnestic disorders in the elderly fit into the indicators of the average statistical norm of this age group and indicate a disorder in young people.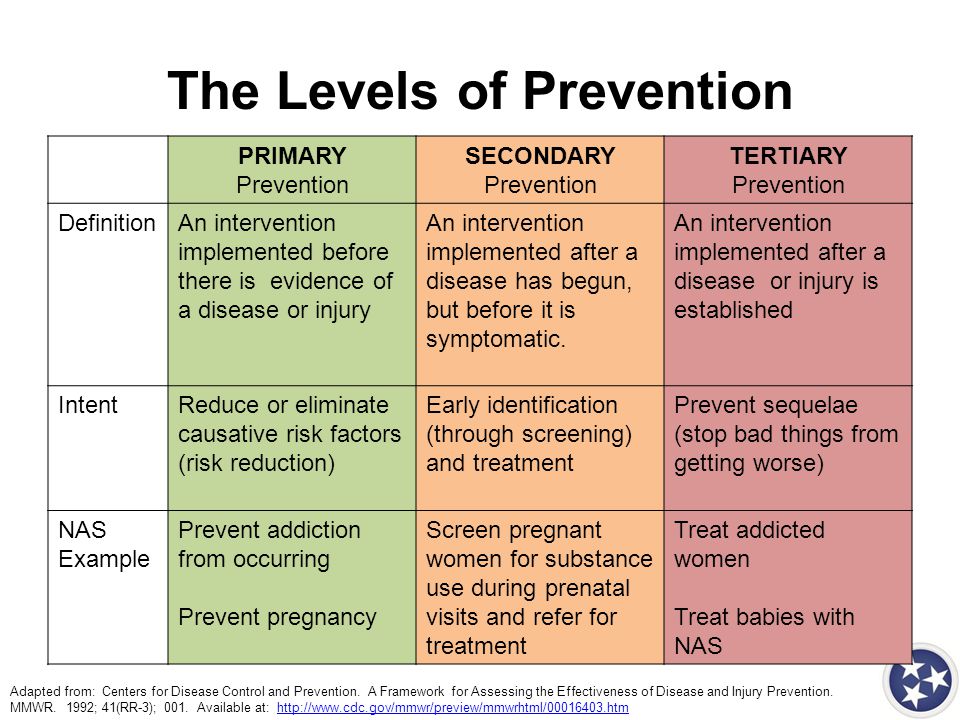
3. Constitutional norm . Each constitutional type is predisposed to a certain type of psychological response and to a certain range of mental and behavioral disorders. For each type, there are specific pathogenic factors against which it is most vulnerable. Thus, persons with a schizoid constitution are characterized by coldness, rationalism, and hypersensitivity; persons with a cyclothymic constitution - a change of mood from fun to depression.
4. Accentuation is a variant of the mental norm, which is characterized by a special severity or sharpening of certain character traits, which determines the specifics of a person's vulnerability to certain mental and behavioral disorders. As a rule, these are conduct disorders, narcotic and psychogenic disorders.
5. Pre-illness is a condition in which there are already some symptoms of mental disorders (usually neurotic and affective levels), but social adaptation is still preserved or partially impaired.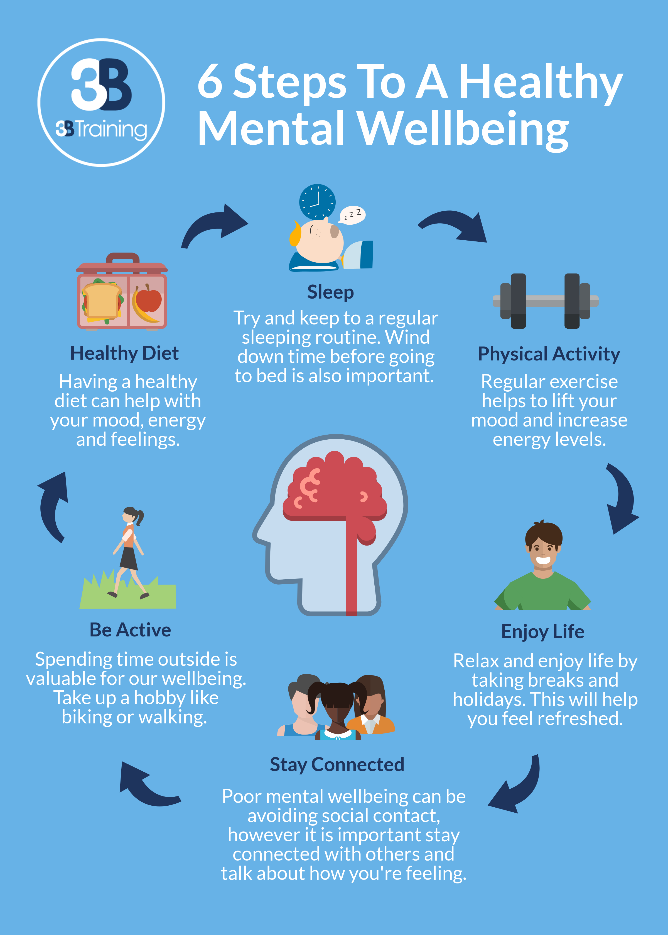 According to various epidemiological studies, it has been established that the premorbid state in the population reaches 22% -89%. The most common are asthenic disorders (headache, sleep disorders, fatigue, irritability, irascibility) and affective disorders (emotional lability, anxiety, dysphoria). The probability of illness in this case tends to 100%.
According to various epidemiological studies, it has been established that the premorbid state in the population reaches 22% -89%. The most common are asthenic disorders (headache, sleep disorders, fatigue, irritability, irascibility) and affective disorders (emotional lability, anxiety, dysphoria). The probability of illness in this case tends to 100%.
It should be noted that in the ICD - 10 there is no concept " mental illness ". The definition of "mental disorder" has been introduced into the conceptual apparatus of modern psychiatry. In ICD-10 and DSM-IV, "mental disorder" means:
“a morbid condition with psychopathological or behavioral manifestations associated with impaired functioning of the body as a result of exposure to biological, social, psychological, genetic or chemical factors. It is determined by the degree of deviation from the concept of mental health taken as the basis.
It can be seen from the definition that the presence or absence of a mental disorder is ultimately determined by those ideas about mental health that exist in a certain historical period with its inherent sociocultural characteristics, as well as the concepts that dominate in this historical period in the field of psychiatry and related disciplines. Renowned psychologist and suicidologist Karl Menninger at 1964, reflecting on the problem of diagnosis in psychiatry, he wrote:
Renowned psychologist and suicidologist Karl Menninger at 1964, reflecting on the problem of diagnosis in psychiatry, he wrote:
"Diagnoses change because we change our concepts of illness and mental disorder."
A third of a century later, in 1990, the president of the Royal College of Psychiatrists of Great Britain, Jim Burley, completed the thought expressed by K. Meninger in this way: “ The patient suffers from an illness, the doctor suffers from the concept of ”.
Key words: Psyche, Health
Source: Yurieva LN, History. Culture. Mental and behavioral disorders
| Related materials |
|---|
| Health psychology and mental norm in children Isaev DN, Childhood psychiatry: developmental psychopathology: a textbook for universities. — St. Petersburg. |
| Mental health states of the individual ... |
| Mental health and family Yurieva LN, History. Culture. Mental and behavioral disorders |
| Mental health criteria Isaev D.N. - Emotional stress, psychosomatic and somatopsychic disorders in... |
| Playing and learning activities in children with mental retardation Psychology of children with mental retardation / O. V. Zashchirinskaya - "St.... |
| Levels of mental reflection Zavalova N.D., Image in the system of mental regulation |
| Development of mental disorders by periods after traumatic brain injury ... |
| The concept of health, the main indicators of health MN Misyuk, VV Maksimenko. |
Mental health - what it is, criteria, levels
Mental health in psychology is a concept that determines the harmonious development of a person who is able to be independent and responsible in almost any conditions. The term "mental health" was introduced by the World Health Organization to clarify the definition of health in general and includes the absence of mental illness and the healthy development of the nervous system in general.
Content
- What is mental health
- Criteria for mental health of personality
- Mental health levels
- Mental health factors
- Portrait of a mentally healthy person
- Mental health of children and adolescents
- METHODS IN Prevention of mental health
- Conclusion
What is mental health
Human mental health, according to WHO, is a state of a person in which he does not have any mental disorders, and also successfully realizes his own potential, successfully performs the necessary activities and contributes to the development of society.
Criteria of a person's mental health
In a narrow sense, mental health should be characterized by the absence of a person's signs of mental disorders, among which, according to the German psychiatrist E. Kraepelin, are psychoses, psychopathy, dementia and neuroses.
In a broader sense, according to the WHO concept, the criteria for mental health of a person include the following indicators:
- awareness of the uniqueness and constancy of one's own "I";
- constancy and identity of the reactions of the psyche to similar situations;
- criticality to one's own mental activity and its results;
- adequacy of reactions to the frequency and strength of environmental influences on the psyche;
- the ability to manage one's own behavior in accordance with the rules established in society;
- the ability to set goals, build an action plan and bring the work started to the result;
- the ability to change one's behavior depending on the changing situation.
Levels of mental health
The World Health Organization also defines the main levels of mental health.
Thus, the first and highest level is the ideal mental and physical health of a person. Harmonious development, in the presence of all the criteria for mental health, the absence of prerequisites for the development of mental illness.
The second level is the average. This, one might say, is the “norm”, which is characteristic of the population, age group, gender, social status and conditions in which a person is located.
The third level is the level of accentuations. These are pointed traits of temperament and character that border on the norm and, under very unfavorable conditions, can flow into mental illness.
The fourth level is predisease. A person begins to show point symptoms of mental disorders.
Mental health factors
When assessing mental health, it is necessary to take into account the conditions in which a person is and what surrounds him.
So, one of the main factors influencing the mental health of a person can be called a favorable socio-economic situation in the place where he lives. If an individual feels safe, has enough money to live on, and is relatively free in his life and work, then his state of mind is likely to be about normal.
Another factor is a high level of intelligence. Here, mental health is seen as a factor in effective performance. A person must understand the causes and consequences of various events, be able to make predictions of what is happening depending on the situation, think about decisions and analyze the results.
The level of upbringing is also a significant factor. The more social rules a person learned in childhood, the more stable his psyche will be.
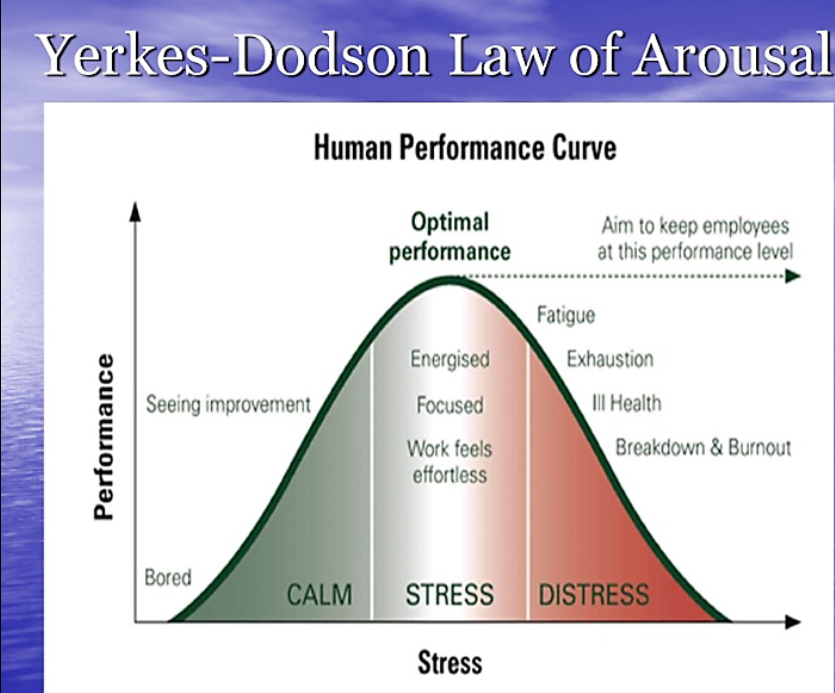
Individual personality traits are determined by the speed of transmission of impulses along nerve fibers and determine a person's behavior in stressful situations.
The hereditary factor is the basis of mental health: the more stable it is in parents, the stronger it is in the child.
Portrait of a mentally healthy person
A healthy person is excellent at building relationships with people, regardless of differences in interests or social status. He accepts people with all their advantages and disadvantages, knows how to maintain a balance between "take" and "give" in relations with others.
Such a person wants and can work, engage in professional activities and be successful in it. He knows how to play with children and adults, in serious and playful games, knows how to play with words and metaphors. This is a creative person with his own hobbies and interests.
A mentally healthy person is autonomous - his actions do not depend on anyone, he is critical of value judgments, he is independent and responsible in what he does. He understands ethical and moral norms, is emotionally stable and has a strategy for the flexible use of the protective mechanisms of the psyche. Such a person is capable of reflection, has adequate self-esteem and a high level of awareness.
Mental health of children and adolescents
Children, and especially adolescents, are characterized by an unstable psyche and the presence of character accentuations. Depending on the type of accentuation, children and adolescents may experience various mental health problems. For example, with the schizoid type, excessive isolation and obsession with something often manifests itself, with the cycloid type - a constant movement in a circle of emotions from euphoria to apathy and vice versa, with the hysteroid type - an excessive need for attention from others. With growing up and gaining life experience, the corners of character are most often smoothed out, but in an unfavorable situation, for example, emotional violence in the family or due to serious traumatic shocks for the psyche, mental illness can occur.
Signs of a decline in mental health in adolescents include excessive isolation, aggressiveness, tearfulness, irritability, a tendency to deviant behavior or delinquency, and the presence of various kinds of addictions.
Ways to maintain mental health: my advice
How to maintain a person's mental health? To do this, it is important to follow simple rules that affect not only mental, but also somatic health.
First, eat right. Too sweet and fatty foods in excessive quantities leads to a change in the functioning of the hormonal system. As a result, the state of the psyche also changes. Also, it is affected by the lack of useful trace elements and vitamins.
The second is to be active on the physical plane. During physical education and sports, the brain is saturated with oxygen, useful hormones are produced and negative thoughts are eliminated.
The third is to strive for self-knowledge. Accept your strengths and weaknesses, work on the latter; learn to control your emotions, identify new talents and abilities.
Overcome addictions. This item includes both chemical and psychological species. Getting rid of alcohol, cigarettes, dependence on the opinions and behavior of other people, you can greatly strengthen the state of your psyche due to the emergence of a new sense of freedom.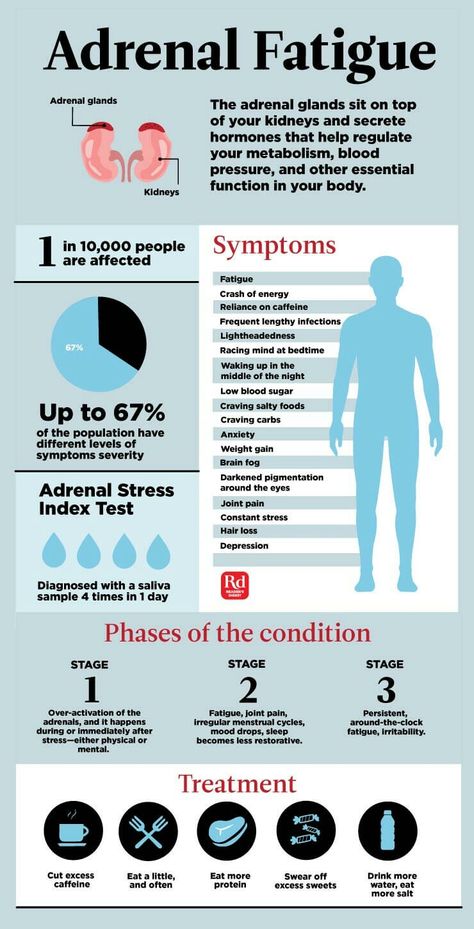
 ..
..  Fundamentals of medical knowledge: Educational and methodological complex for...
Fundamentals of medical knowledge: Educational and methodological complex for...