Switching from effexor to zoloft
What to expect when switching antidepressants
Here’s what you should know about side effects and withdrawal before making the switch
For many, deciding to take an antidepressant medication is a very big deal. You spend a lot of time thinking about it, weighing the pros and cons, and talking to your healthcare provider about options, before deciding to try a prescription medication.
Finding the right antidepressant can require some trial and error, some fine-tuning. You may have to change medications at some point to find one that works well for you. If you’re concerned that your current prescription isn’t as effective as it should be, talk to your doctor about switching antidepressants.
RELATED: List of antidepressants
Common reasons for switching antidepressants
How do you know if you need to change your antidepressant? One of the most common reasons that people switch antidepressants is they feel their current medication isn’t really helping them. Antidepressants can be ineffective in a variety of ways.
1. Time
Antidepressants need time to reach their maximum effectiveness. The length of time can vary.
Six weeks can usually provide insight, one way or another, suggests Gonzalo Laje, MD, MHSc, director at Washington Behavioral Medicine Associates and clinical associate professor at George Washington University.
2. Dosage
If an antidepressant isn’t working after approximately six weeks, it could be that the dose is too low. Consult your healthcare provider, who can slowly and carefully increase the dose. If you’re not feeling better when taking a higher (or even the maximum) dose, it might be time to discuss trying something else—or adding another medication.
3. Side effects
Not everyone experiences side effects, and some people are willing to tolerate certain side effects from medication if it’s helping their depression. But for other people, side effects like a low libido, dry mouth, or nausea are deal breakers. If you’re struggling to cope with the side effects—it may be time to schedule an appointment with your healthcare provider.
If you’re struggling to cope with the side effects—it may be time to schedule an appointment with your healthcare provider.
Don’t try stopping or changing medications on your own. You might experience some withdrawal symptoms, especially if you stop abruptly. “It’s always better to talk to your doctor about (making) these changes,” Dr. Laje says. Withdrawal symptoms of antidepressants typically include:
- Anxiety
- Trouble sleeping
- “Head buzzing”
- Headaches
- Dizziness
- Fatigue
- Flu-like symptoms
- Nausea
- Irritability
Choosing a new antidepressant that is best for you
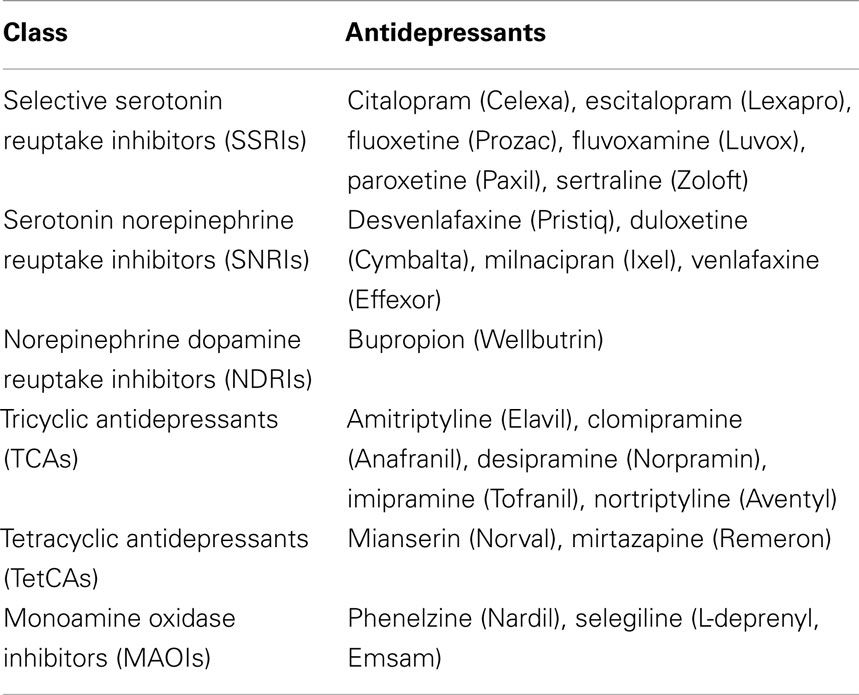
Then the question becomes: What is the best medication to switch to? There are many potential choices from these categories of antidepressants:
- Selective serotonin reuptake inhibitors (SSRIs): This category includes commonly prescribed medications like Prozac (fluoxetine), Celexa (citalopram), Lexapro (escitalopram), Paxil (paroxetine), Zoloft (sertraline), and Viibryd (vilazodone).
- Serotonin and norepinephrine reuptake inhibitors (SNRIs): This category includes Effexor XR (venlafaxine), Pristiq (desvenlafaxine), Cymbalta (duloxetine), and Fetzima (levomilnacipran).
- Tricyclic antidepressants (TCAs): TCAs are an older category of antidepressant with more side effects than newer antidepressants. This class includes drugs such as Tofranil (imipramine), Elavil (amitriptyline), Pamelor (nortriptyline), and Norpramin (desipramine).
- Monoamine oxidase inhibitors (MAOIs): MAOIs are another older category of medication not used as first-line treatments anymore, and include Nardil (phenelzine), and Parnate (tranylcypromine)
- Other antidepressants: This category includes medications that may not fit precisely into another category, such as Wellbutrin (bupropion), which is a norepinephrine-dopamine reuptake inhibitor (NDRI), and Desyrel (trazodone), which is known as a serotonin antagonist and reuptake inhibitor (SARI).
All antidepressants come with benefits and downsides, so it may become a question of what works well for you. “We usually go for something that has the least amount of side effects in general,” says psychiatrist Samuel Mowerman, MD, faculty member at the University of Miami Miller School of Medicine.
According to Dr. Mowerman, the features of your particular kind of depression will also affect the choice. For example, if you also live with anxiety, your doctor might recommend an antidepressant with a success rate for addressing anxiety, too.
Your doctor may choose to switch you from one category of antidepressant to another. Or your doctor might suggest that you stick with a medication from the same category of drug that you’ve been taking. For example, if you’re already taking one SSRI, your doctor might suggest trying another one, like switching from Prozac to Zoloft or switching from Lexapro to Zoloft.
How to switch antidepressants
When you do make the switch, there are several possible processes for doing it:
- Cross tapering: You decrease the original medication dose while starting the new medication at a low dose and gradually increasing it.

- Direct switch: This could involve stopping the old drug and then starting the new one on the following day.
- Taper down and stop, before starting the new drug: You gradually decrease the amount of your original antidepressant, then start taking the new medication immediately after stopping the original medication.
- Taper, washout, and switch. You gradually decrease the amount of your original antidepressant, then stop taking it altogether. Your healthcare provider will advise a “washout period” of days or weeks to wait before starting the new medication.
“MAOIs and tricyclics are two classes of antidepressants that should be tapered off first with time for the blood levels to go to zero before starting a new antidepressant,” Dr. Israel says.
More about cross-tapering
Cross-tapering is a standard approach in many cases, says psychiatrist Lindsay Israel, MD, chief medical officer at Success TMS. For example, it’s often used when you switch an SSRI to a drug in another class. Why? Because it takes time for the original medication to leave your system, just as it takes a while for the new medication to take effect.
For example, it’s often used when you switch an SSRI to a drug in another class. Why? Because it takes time for the original medication to leave your system, just as it takes a while for the new medication to take effect.
A cross-taper allows you to gradually ramp up the new med while slowly decreasing the original one, which should help to minimize any symptoms of what Israel calls “discontinuation syndrome” due to any overlap, especially if the medications have similar properties, says Dr. Israel.
Common symptoms of discontinuation syndrome include fatigue, nausea, insomnia, vertigo, dizziness, and fogginess.
How long does it take to adjust to a new antidepressant?
It depends in part on the dosage you have been taking. A higher dose may take a little longer. “Depending on the half-life of the medications in question and the current dosage, this cross taper can take anywhere from one week to four-to-six weeks,” Dr. Israel says.
Side effects of switching antidepressants
As previously mentioned, you may experience symptoms of withdrawal or discontinuation syndrome.
It’s also important to note symptoms of serotonin syndrome, which is a life-threatening condition that can happen when you take more than one antidepressant medication (or more than one medication, antidepressant or other) that affects serotonin levels. Serotonin syndrome requires emergency medical attention. Symptoms of serotonin syndrome include:
- Mood changes, agitation, or anxiety
- Restlessness
- Confusion
- Muscle changes, such as lack of coordination, stiffness, rigidity, or muscle jerks (especially in the legs)
- Sweating, shivering, flushed skin, fever, or hyperthermia
- Increased heart rate or blood pressure
- Nausea, vomiting, diarrhea
- Tremor
- Hyperactive reflexes
- Dilated pupils
You should also be aware of the side effects to expect from your new antidepressant, as they may differ from those of the original antidepressant.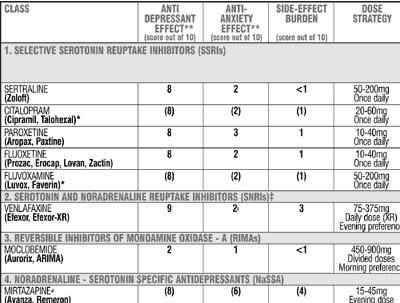 Ask your healthcare provider or pharmacist for a complete list of side effects associated with the new medication.
Ask your healthcare provider or pharmacist for a complete list of side effects associated with the new medication.
Are antidepressants worth switching?
Ultimately, the goal of switching antidepressants is to find a medication that works for you.
Dr. Mowerman’s advice: “Give it time.” Let the new medication work, he adds. It may take some time to ramp up to the dose that’s most effective for you, or to find the right medication. Don’t give up if you don’t feel great right away or have to try a few prescriptions.
And don’t be afraid to speak up. If you have any questions or concerns about side effects, be sure to ask. For example, don’t be embarrassed to raise any concerns about the effect of an antidepressant on your sex drive, Dr. Mowerman says. They’re real, and valid concerns.
Switching and stopping antidepressants - PMC
A number of strategies are available for switching between antidepressants ().6,8 Close clinical observation and caution is required with all approaches, as some patients may respond idiosyncratically and serious complications can occur. Individual patient factors and illness factors may require considerable modification of a switching strategy.
Individual patient factors and illness factors may require considerable modification of a switching strategy.
Table 2
Techniques for switching from one antidepressant to another 6
| Method | Comment |
|---|---|
| Conservative switch: • the first antidepressant is gradually reduced and stopped • there follows a drug-free washout interval of five half-lives of the first antidepressant • the new antidepressant is started according to its dose recommendation | Most appropriate for general practice. The risk of drug interactions is very low but discontinuation symptoms may occur. |
| Moderate switch: • the first antidepressant is gradually reduced and stopped • there follows a drug-free washout interval of 2–4 days • the new antidepressant is started at a low dose | Also recommended for use in general practice. The risk of drug interactions is low but discontinuation symptoms may occur.
The risk of drug interactions is low but discontinuation symptoms may occur. |
| Direct switch: • the first antidepressant is stopped • the second antidepressant is started the next day at the usual therapeutic dose | Quick and simple but discontinuation symptoms are likely depending on the second antidepressant. The risk of drug interactions is substantial, depending on the second antidepressant. Method requires clinical expertise and is only feasible in selected instances, such as swapping from one short half-life SSRI to another. |
| Cross-taper switch: • the first antidepressant is gradually reduced and stopped • the second antidepressant is introduced at a low dose at some stage during the reduction of the first antidepressant, so that the patient is taking both antidepressants simultaneously • the dose of the second antidepressant is increased to the therapeutic dose when the first antidepressant has been stopped | Frequently used for patients with high risk from illness relapse but there is risk of drug interactions and increased adverse effects from combined medications. Only feasible in selected instances. Requires clinical expertise. Only feasible in selected instances. Requires clinical expertise. |
Open in a separate window
Note: Above strategies do not apply to monamine oxidase inhibitors, for which strict recommendations must be followed ()
SSRI selective serotonin reuptake inhibitor
Adapted from reference 6
The most conservative strategy, with the lowest risk of drug interactions, is to gradually taper the dose of the first antidepressant to minimise withdrawal symptoms then start a washout period equivalent to five half-lives of the drug (). This does not apply to irreversible monoamine oxidase inhibitors where a specified long period of washout is mandatory (see ). Five half-lives equates to about five days for most SSRIs except fluoxetine, which can still be significantly active five or more weeks after cessation. The second antidepressant is then introduced according to the starting dose recommendations.
Table 3
Guidelines for switching between specific antidepressants 2,8-10
| TO → ↓ FROM | citalopram escitalopram paroxetine sertraline (SSRIs) | fluoxetine | fluvoxamine | vortioxetine | agomelatine | desvenlafaxine duloxetine venlafaxine (SNRIs) | mianserin mirtazapine | reboxetine | amitriptyline imipramine nortriptyline doxepin dothiepin trimipramine (TCAs) | clomipramine | moclobemide | phenelzine tranylcypromine (MAOIs) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| citalopram escitalopram paroxetine sertraline (SSRIs) | taper drug, start alternative SSRI at low dose* | taper and stop drug, then start fluoxetine at 10 mg§ | taper and stop drug, then start fluvoxamine at 50 mg§ | taper drug, start vortioxetine at 5 mg* | taper drug, start agomelatine* | taper drug, then start SNRI at low dose* | taper drug, then start above drug at low dose* | taper drug, start reboxetine* | taper SSRI, start above drug at low dose (usually 25 mg)* | taper and stop drug, then start clomipramine at 25 mg§ | taper and stop drug for 7 days washout before starting moclobemide at low dose§ | taper and stop drug for 7 days washout before starting MAOI at low dose§ |
| fluoxetine | stop fluoxetine (or taper if dose >40 mg/day), wait 7 days for washout, then start above SSRI at low dose†§ | stop fluoxetine (or taper if dose >40 mg/day), wait 14 days for washout, then start fluvoxamine at 50 mg†§ | stop fluoxetine (or taper if dose >40 mg/day), wait 7 days for washout, then start vortioxetine at 5 mg†§ | stop fluoxetine (or taper if dose >40 mg/day), start agomelatine | taper and stop fluoxetine, wait 7 days for washout, then start SNRI at low dose†§ | stop fluoxetine (or taper if dose >40 mg/day), start above drug at low dose | stop fluoxetine (or taper if dose >40 mg/day), start reboxetine at 4 mg | stop fluoxetine (or taper if dose >40 mg/day), wait 14 days for washout, then start above drug at 25 mg and continue low dose for further 3 weeks‡ | stop fluoxetine (or taper if dose >40 mg/day), wait 14 days for washout, then start clomipramine at 25 mg and continue this dose for further 3 weeks‡ | stop fluoxetine (or taper if dose >40 mg/day), then wait 5–6 weeks for washout before cautiously commencing low-dose moclobemide§ | stop fluoxetine (or taper if dose >40 mg/day), then wait 5–6 weeks for washout before cautiously commencing low-dose MAOI§ | |
| fluvoxamine | taper and stop fluvoxamine, then start above SSRI at low dose§ | taper and stop fluvoxamine, then start fluoxetine at 10 mg§ | taper and stop fluvoxamine, start vortioxetine at 5 mg§ | taper and stop fluvoxamine, wait 7 days for washout, then start agomelatine§ | taper and stop fluvoxamine, then start SNRI at low dose§ | taper and stop fluvoxamine, then start above drug at low dose§ | taper fluvoxamine, start reboxetine at 4 mg* | taper fluvoxamine, start above drug at 25 mg* | taper and stop fluvoxamine, start clomipramine at 25 mg§ | taper and stop fluvoxamine, wait 7 days for washout before cautiously commencing low-dose moclobemide§ | taper and stop fluvoxamine, wait 7 days for washout before cautiously commencing low-dose MAOI§ | |
| vortioxetine | taper vortioxetine, start above SSRI at low dose* | taper and stop vortioxetine, start fluoxetine at 10 mg§ | taper and stop vortioxetine, start fluvoxamine at 50 mg§ | taper vortioxetine, start agomelatine at 25 mg* | taper vortioxetine, start SNRI at low dose* | taper vortioxetine, start above drug at low dose* | taper vortioxetine, start reboxetine* | taper vortioxetine, start above drug at low dose (usually 25 mg)* | taper and stop vortioxetine, start clomipramine at 25 mg§ | taper and stop vortioxetine for 14 days washout before starting moclobemide at low dose§ | taper and stop vortioxetine for 21 days washout before starting MAOI at low dose cautiously§ | |
| agomelatine | stop agomelatine, then start above SSRI | stop agomelatine, then start fluoxetine | stop agomelatine, then start fluvoxamine* | stop agomelatine, then start vortioxetine | stop agomelatine, then start SNRI | stop agomelatine, then start above drug | stop agomelatine, then start reboxetine | stop agomelatine, then start above drug at low dose (usually 25 mg)* | stop agomelatine, then start clomipramine | stop agomelatine, then start moclobemide | stop agomelatine, then start MAOI | |
| desvenlafaxine duloxetine venlafaxine (SNRIs) | taper SNRI, start above SSRI at low dose* | taper and stop SNRI, start fluoxetine at 10 mg§ | taper and stop SNRI, start fluvoxamine at 50 mg§ | taper SNRI, start vortioxetine at 5 mg* | taper SNRI, start agomelatine* | taper SNRI, start alternative SNRI at low dose* | taper SNRI, start above drug at low dose* | taper SNRI, start reboxetine at 4 mg* | taper SNRI, start above drug at 25 mg* | taper SNRI, start clomipramine at 25 mg* | taper and stop SNRI, wait 7 days for washout before cautiously commencing low-dose moclobemide§ | taper and stop SNRI, wait 7 days for washout before cautiously commencing low-dose MAOI§ |
| mianserin mirtazepine | taper drug, start above SSRI* | taper drug, start fluoxetine* | taper drug, start fluvoxamine* | taper drug, start vortioxetine* | taper drug, start agomelatine* | taper drug, start SNRI* | taper drug, start drug above at low dose* | taper drug, start reboxetine at 4 mg* | taper drug, start above drug at 25 mg* | taper drug, start clomipramine at 25 mg* | taper and stop drug, wait 7 days for washout before cautiously commencing low-dose moclobemide§ | taper and stop drug, wait 14 days for washout before cautiously commencing low-dose MAOI§ |
| reboxetine | taper reboxetine, start above SSRI* | taper reboxetine, start fluoxetine* | taper reboxetine, start fluvoxamine at 50 mg* | taper reboxetine, start vortioxetine at 5 mg* | taper reboxetine, start agomelatine* | taper reboxetine, start SNRI at low dose* | taper reboxetine, start above drug* | taper reboxetine, start above drug at 25 mg* | taper reboxetine, start clomipramine at 25 mg* | taper and stop reboxetine, then wait 7 days for washout before cautiously commencing low-dose moclobemide§ | taper and stop reboxetine, then wait 7 days for washout before cautiously commencing low-dose MAOI§ | |
| amitriptyline imipramine nortriptyline doxepin dothiepin trimipramine (TCAs) | taper first drug and start above drug at low dose* | taper and stop first drug before starting fluoxetine§ | taper drug, start fluvoxamine at 50 mg* | taper drug, start vortioxetine at 5 mg* | taper drug, start agomelatine* | taper drug, start SNRI at low dose* | taper drug, start above drug at low dose* | taper drug, start reboxetine at 4 mg* | taper first drug, start alternative TCA at 25 mg* | taper drug, start clomipramine cautiously at 25 mg* | taper and stop drug, then wait 7 days for washout before starting moclobemide§ | taper and stop drug, then wait 14 days (21 days for imipramine) before starting MAOI§ |
| clomipramine | taper and stop clomipramine, then start above SSRI at low dose§ | taper and stop clomipramine, then start fluoxetine at 10 mg§ | taper and stop clomipramine, then start fluvoxamine at 50 mg§ | taper and stop clomipramine, then start vortioxetine at 5 mg§ | taper clomipramine, start agomelatine* | taper and stop clomipramine, then start SNRI at low dose§ | taper clomipramine, then start above drug at low dose* | taper clomipramine, then start reboxetine at 4 mg* | taper clomipramine, then start drug at 25 mg* | taper and stop clomipramine, then wait 7 days for washout before starting moclobemide§ | taper and stop clomipramine, then wait 21 days for washout before starting MAOI§ | |
| moclobemide | taper and stop moclobemide, then wait 24 hours for washout before starting above drug§ | taper and stop moclobemide, then wait 24 hours for washout before starting fluoxetine§ | taper and stop moclobemide, then wait 24 hours for washout before starting fluvoxamine§ | taper and stop moclobemide, then wait 24 hours for washout before starting vortioxetine§ | taper moclobemide, start agomelatine | taper and stop moclobemide, then wait 24 hours for washout before starting SNRI§ | taper and stop moclobemide, then wait 24 hours for washout before starting above drug§ | taper and stop moclobemide, then wait 24 hours for washout before starting reboxetine§ | taper and stop moclobemide, then wait 24 hours for washout before starting above drug§ | taper and stop moclobemide, then wait 24 hours for washout before starting clomipramine§ | taper and stop moclobemide, then wait 24 hours for washout before starting MAOI§ | |
| phenelzine tranylcypromine (MAOIs) | taper and stop MAOI, then wait 14 days for washout before starting above drug§ | taper and stop MAOI, then wait 14 days for washout before starting fluoxetine§ | taper and stop MAOI, then wait 14 days for washout before starting fluvoxamine§ | taper and stop MAOI, then wait 14 days for washout before starting vortioxetine§ | taper and stop MAOI, start agomelatine* | taper and stop MAOI, then wait 14 days for washout before starting SNRI§ | taper and stop MAOI, then wait 14 days for washout before starting above drug§ | taper and stop MAOI, then wait 14 days for washout before starting reboxetine§ | taper and stop MAOI, then wait 14 days for washout before starting above drug§ | taper and stop MAOI, then wait 21 days for washout before starting clomipramine§ | taper and stop MAOI, start moclobemide while maintaining MAOI dietary restrictions for 14 days§ | taper and stop MAOI, wait 14 days for washout before starting other MAOI§ |
Open in a separate window
Taper means gradual dose reduction, with lowering by increments every few days, usually over a period of 4 weeks, modified by patient experience, drug, illness and other factors.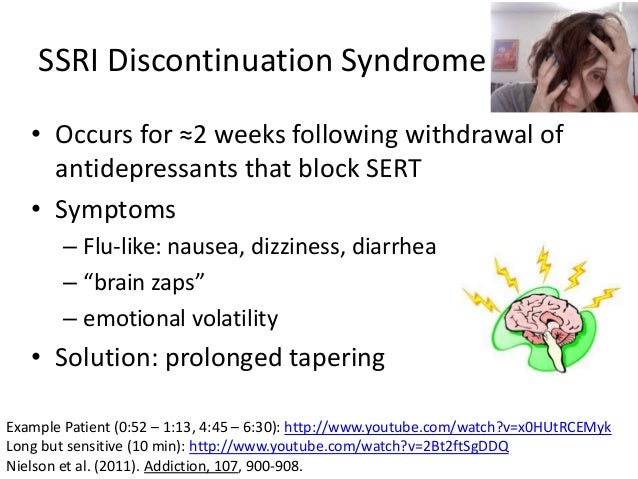
All switches from one antidepressant to another may result in serious complications. Switches must be undertaken cautiously and under close observation.
The recommendations in this table are based on clinical experience, product information, empirical evidence and recommendations from other guidelines. It may be necessary to modify the switching process depending on patient, illness and interacting drug variables, determined by the patient’s clinical progress. In appropriate circumstances expert prescribers may use less conservative switch strategies if justified by harm–benefit considerations arising from factors such as illness severity.
MAOI monoamine oxidase inhibitor
SNRI serotonin noradrenaline reuptake inhibitor
SSRI selective serotonin reuptake inhibitor
TCA tricyclic antidepressant
* A washout period of 2–5 half-lives (most frequently 2–5 days) between cessation of previous drug and the introduction of a new drug is the safest switching strategy from the point of view of drug interactions.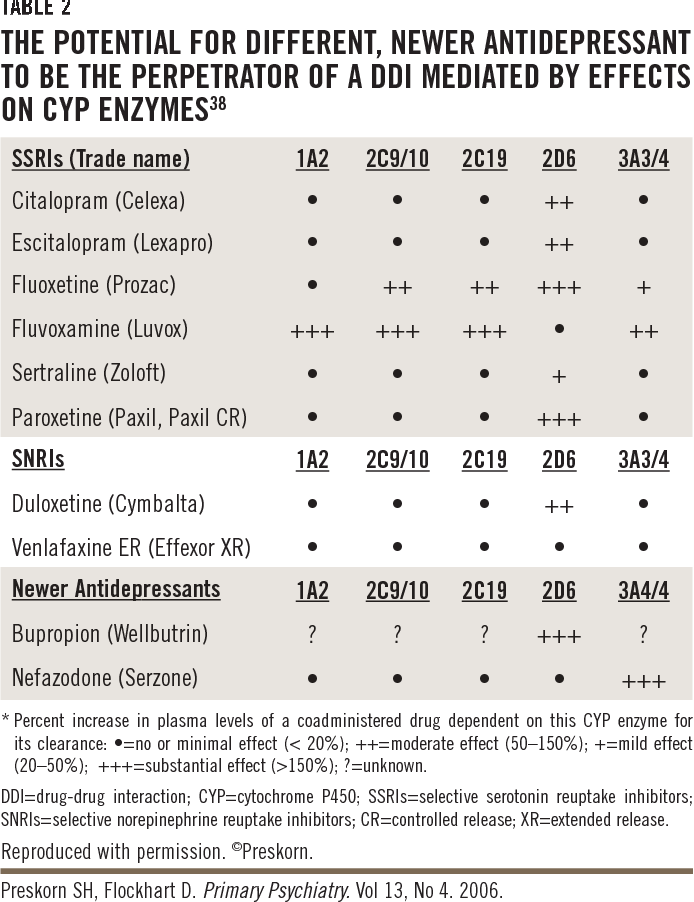 In the indicated instances a washout period is not essential if switching is carried out cautiously and under close observation, and clinical considerations such as illness severity support harm–benefit considerations. Cautious cross taper (when the dose of the first drug is being reduced and the dose of the second drug is being increased at the same time so that the patient is taking both antidepressants) may be used in the indicated instances if appropriate and safe.
In the indicated instances a washout period is not essential if switching is carried out cautiously and under close observation, and clinical considerations such as illness severity support harm–benefit considerations. Cautious cross taper (when the dose of the first drug is being reduced and the dose of the second drug is being increased at the same time so that the patient is taking both antidepressants) may be used in the indicated instances if appropriate and safe.
† Fluoxetine may still cause interactions 5 or 6 weeks after cessation (especially from higher doses) due to long half-life of drug and active metabolite.
‡ Fluoxetine is likely to continue to elevate TCA concentrations for several weeks.
§ Co-prescription of the two antidepressants in this instance is not recommended.
Adapted from references 2, 8–10
The dose is usually tapered over four weeks, similar to the minimum period required for antidepressant discontinuation. However, the time frame may need to be modified depending on patient factors.
However, the time frame may need to be modified depending on patient factors.
As the conservative switch can take quite a long time and usually includes at least several days where the patient is not on an antidepressant, a compromise strategy is the moderate switch. Here the washout period can generally be shortened to about two days. The risk of drug interactions is increased with this approach, but is still quite low. The conservative and moderate switch techniques are both suitable for general practice.
Direct and cross-taper switch methods can also be used but considerable expertise is necessary (). Some patients will require admission to hospital. A direct switch – one drug is stopped and another drug is commenced the next day at the usual therapeutic dose – can be used when switching between some SSRIs, SNRIs and tricyclic antidepressants. However, there will be a considerable risk of withdrawal symptoms and drug interactions. A cross-taper strategy, where the first antidepressant dose is reduced while the second antidepressant is introduced at a low dose and gradually increased, can be done safely with only some antidepressants ().
Zoloft withdrawal syndrome - Center for Healthy Youth
Zoloft - what is this drug? The active substance of the drug is sertraline. It belongs to the pharmacological group of antidepressants and is prescribed to patients with the following symptoms: depression, OCD, panic disorders, PTSD, social phobia. Zoloft is a powerful serotonin reuptake inhibitor in human brain cells.
More than 1/3 of people face the dangerous consequences of abrupt withdrawal of Zoloft. In narcology, this phenomenon is called withdrawal syndrome or withdrawal syndrome. The time of onset of symptoms of withdrawal syndrome when used is directly proportional to the half-life of the drug from the body. A drug such as Zoloft is addictive with systematic irregular use, therefore, there is also a Zoloft withdrawal syndrome, which usually occurs 3-5 days after the last use of the drug. The symptoms of Zoloft withdrawal syndrome are quite difficult to recognize, so people think that the disease has returned and start using the medicine again.
-
Can't
persuade
to get treatment?
-
We will help you with motivation for treatment. As a rule, it is difficult for close people to persuade or force an addict to be treated. World experts have developed EFFECTIVE motivation schemes, using which you can lead the addict to the decision to seek help.
8 (800) 333-20-07
How to reduce the dose of Zoloft correctly?
The course of treatment with Zoloft usually lasts no more than 8 weeks (about two months). As with the use of other antidepressants, an unreasonable increase in the duration of its use leads to negative consequences for human health. However, even before the period prescribed by the doctor, it is not recommended to stop taking the drug, since the gradual disappearance of symptoms is not a reason to complete the course. How long can I take Zoloft?
How much Zoloft can I take?
Many patients wonder how much Zoloft should be taken? Naturally, the duration of the course is strictly individual. So, how long can you take Zoloft? Only the attending physician, depending on the symptoms present, will be able to tell you how much Zoloft should be taken in your case. A specialist can prescribe a medication for 6-12 months, but this happens in exceptional cases.
The risk of developing withdrawal symptoms is increased in the following cases:
- abrupt drug withdrawal and removal from the body;
- regular intake over two months;
- excessive anxiety;
- Combination with antihypertensives, allergies, and antipsychotics.
Do you want to know the cost of services?
8 (800) 333-20-07 - call our specialist
How to cancel and stop drinking Zoloft?
Zoloft causes a withdrawal syndrome when it is stopped abruptly. This drug affects the processes occurring in the human brain, so you should take the medicine only with a doctor's prescription. How to stop taking the drug and "get off" from Zoloft? To avoid the withdrawal syndrome, the dosage of the medication according to the medical plan is reduced by 25 mg every 14 days.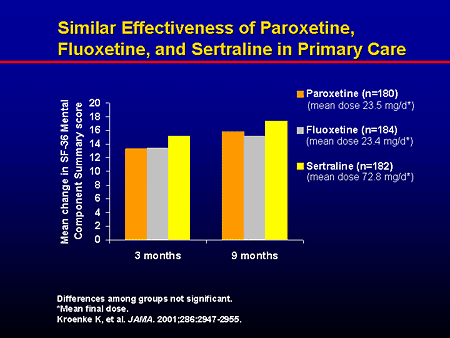 If a stable remission is achieved after a course of treatment, the doctor will stop taking the drug. However, the specialist will cancel the drug if the patient experiences side effects, insomnia and headache from Zoloft are not uncommon.
If a stable remission is achieved after a course of treatment, the doctor will stop taking the drug. However, the specialist will cancel the drug if the patient experiences side effects, insomnia and headache from Zoloft are not uncommon.
In which case the doctor can cancel the medication:
- the patient has a headache;
- causeless sadness, anxiety;
- feeling of devastation;
- nervousness, irritability;
- weakness;
- suicidal tendencies;
- sleep and appetite disorders;
- decrease in concentration.
If a person has lost their appetite or has regular headaches, the doctor begins a gradual process of reducing the dosage. The therapeutic dose is reduced over several weeks, and sometimes months.
Symptoms of withdrawal after taking
Is it possible to abruptly stop taking the medicine? Abrupt withdrawal of the drug threatens the occurrence of withdrawal or withdrawal. The human body, accustomed to a certain dose of the drug, will respond without an adaptation period. Most often, a deterioration in the patient's health is noted within 2-4 days after the last use. Depending on the individual characteristics and the state of the central nervous system, withdrawal symptoms may be different.
The human body, accustomed to a certain dose of the drug, will respond without an adaptation period. Most often, a deterioration in the patient's health is noted within 2-4 days after the last use. Depending on the individual characteristics and the state of the central nervous system, withdrawal symptoms may be different.
Symptoms and signs of withdrawal
- nervousness;
- irritability;
- irritability;
- insomnia;
- nausea, vomiting;
- headaches;
- incoordination, balancez.
In some cases, a person will not even feel dangerous signs, and sometimes you may need to call an ambulance for narcological help from the Center for Healthy Youth. Therefore, if you feel a deterioration in the condition, it is worth contacting a doctor who will help reduce the dose and improve overall well-being.
How long does Zoloft withdrawal last?
Withdrawal symptoms can persist without drug treatment for quite a long time, for several weeks. While taking antidepressants, the activity of neurons changes, so after stopping the drugs, the body needs time to rebuild and adapt to new conditions. The longer the course of treatment was, the longer the rehabilitation period will be. Withdrawal symptoms will not disappear until the active substance of the drug is excreted from the body. If general weakness lasts for a month, you should contact your doctor or specialists from the Healthy Youth Center.
While taking antidepressants, the activity of neurons changes, so after stopping the drugs, the body needs time to rebuild and adapt to new conditions. The longer the course of treatment was, the longer the rehabilitation period will be. Withdrawal symptoms will not disappear until the active substance of the drug is excreted from the body. If general weakness lasts for a month, you should contact your doctor or specialists from the Healthy Youth Center.
When does Zoloft start to act and help?
It is important to understand that Zoloft does not begin to act immediately, but after a certain period of time. How long does Zoloft take to work? As a rule, the first positive dynamics begins to be noticeable to the patient only after 2-3 weeks of regular use. The maximum effect is noticeable after 2-3 months of admission.
Discontinuation considerations
When choosing antidepressants, it is important to know which medications the patient has previously taken and which medications they are currently taking. Before prescribing an effective remedy that normalizes the work of the central nervous system, the doctor conducts a number of necessary examinations, identifies existing contraindications and prevents side effects. If Zoloft is not recommended for you, the specialist will offer you a wide range of analogues of this drug, including Cipralex, Prozac, Paxil, Cipramil and other equally effective drugs. The drug Velaksin, Amitriptyline, etc. has a similar effect.
If you experience withdrawal symptoms after taking Zoloft, contact the Healthy Youth Drug Treatment Center for help. We have been treating addictions for over 15 years.
Video about the treatment of drug addiction and alcoholism in the CZM
Changing first-line antidepressants | Attending Doctor is a professional medical publication for physicians. Science articles.
| To achieve the targeted clinical effect of antidepressants, it is recommended to switch from tricyclic antidepressants to drugs with a similar mechanism of action, in particular venlafaxine, a modern serotonin and norepinephrine reuptake inhibitor | |
partners Keywords / keywords: Antidepressants, Velaxin, Venlafaxine, Depression, Noradrenergic system, Neuropsychiatry, Serotonergic system, Thymoanaleptic therapy
VEL 25. 09.2020/7
09.2020/7
Thymoanaleptic therapy is a dynamic process, the scenario of which depends on the characteristics of the disease and the response to treatment. According to the current recommendations, the clinical effect of an antidepressant (BP) of more than 50% within 3-4 weeks is considered sufficient [1]. According to statistics, such effectiveness is not achieved in 30-50% of patients with initial therapy with the first-line drug [1]. In such cases, it is recommended to increase the dose of blood pressure to the maximum, and in some cases, especially with the use of SSRIs, improvement still develops: a full effect can be achieved at 4-6 or even 8 weeks of treatment [1]. If this does not happen, and also in cases where increasing the dose is impractical (for example, in case of poor tolerance), it is recommended to change the blood pressure to a drug within the same pharmacological class or with a different mechanism of action [1]. In this case, a special algorithm should be followed.
The classical scheme suggests the gradual withdrawal of the initially prescribed drug, and after a washout period, the appointment of a new one with the selection of its therapeutic dose [2]. This method is used if there is a likely risk of an unwanted interaction that occurs when switching from drugs with a long half-life (such as fluoxetine), if the activity of the liver enzyme systems is reduced in the patient, or if the drugs differ radically in the mechanism of action (for example, when switching from mirtazapine or mianserin to milnacipran).
Both the patient and the doctor are much more comfortable with the one-time method of “switching” between drugs with a similar mechanism of action, when one day the first drug is canceled, and the second is prescribed immediately in a therapeutic dose. In this context, it seems convenient to switch patients from tricyclic antidepressants, fluvoxamine, sertraline, paroxetine, and milnacipran to a modern serotonin and norepinephrine reuptake inhibitor (SSRI) venlafaxine ( Velaxin ® [3]).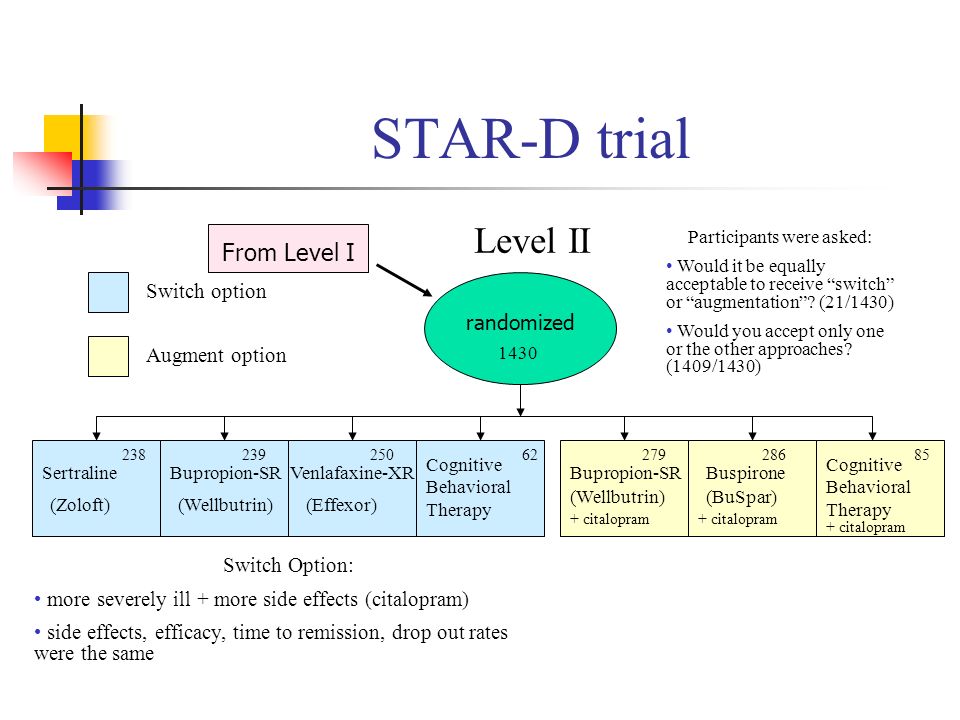 The need for such a transition arises in clinical practice, because. the efficacy of venlafaxine is somewhat higher than that of SSRIs due to a broader spectrum of neurochemical action [1]. The drug acts immediately on three types of neurotransmitters: serotonin (improves mood), norepinephrine (promotes activation) and dopamine (improves motivation for action) [3]. In addition, the advantage of Velaksin ® is a special form of release in capsules. It provides a prolonged action of the active molecule of the drug [3], a more harmonious distribution in the corresponding synaptic sections of the CNS, which, in turn, reduces the risk of adverse events in the process of simultaneous administration or gradual achievement of a therapeutic dose [4].
The need for such a transition arises in clinical practice, because. the efficacy of venlafaxine is somewhat higher than that of SSRIs due to a broader spectrum of neurochemical action [1]. The drug acts immediately on three types of neurotransmitters: serotonin (improves mood), norepinephrine (promotes activation) and dopamine (improves motivation for action) [3]. In addition, the advantage of Velaksin ® is a special form of release in capsules. It provides a prolonged action of the active molecule of the drug [3], a more harmonious distribution in the corresponding synaptic sections of the CNS, which, in turn, reduces the risk of adverse events in the process of simultaneous administration or gradual achievement of a therapeutic dose [4].
It should be taken into account that the transition from fluoxetine to Velaxin ® should be gradual due to the aforementioned long half-life of fluoxetine, in order to avoid unwanted interactions.