Abilify for bipolar 2
The Utility of Low-Dose Aripiprazole for the Treatment of Bipolar II and Bipolar NOS Depression
Save citation to file
Format: Summary (text)PubMedPMIDAbstract (text)CSV
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Add to My Bibliography
- My Bibliography
Unable to load your delegates due to an error
Please try again
Your saved search
Name of saved search:
Search terms:
Test search terms
Email: (change)
Which day? The first SundayThe first MondayThe first TuesdayThe first WednesdayThe first ThursdayThe first FridayThe first SaturdayThe first dayThe first weekday
Which day? SundayMondayTuesdayWednesdayThursdayFridaySaturday
Report format: SummarySummary (text)AbstractAbstract (text)PubMed
Send at most: 1 item5 items10 items20 items50 items100 items200 items
Send even when there aren't any new results
Optional text in email:
Create a file for external citation management software
Full text links
Wolters Kluwer
Full text links
. 2017 Feb;37(1):99-101.
doi: 10.1097/JCP.0000000000000636.
Tammas Kelly 1 , Daniel Z Lieberman
Affiliations
Affiliation
- 1 From the GWU MFA Department of Psychiatry and Behavioral Sciences, George Washington University, Washington, DC.
- PMID: 27977470
- DOI: 10.1097/JCP.0000000000000636
Tammas Kelly et al. J Clin Psychopharmacol. 2017 Feb.
. 2017 Feb;37(1):99-101.
doi: 10. 1097/JCP.0000000000000636.
1097/JCP.0000000000000636.
Authors
Tammas Kelly 1 , Daniel Z Lieberman
Affiliation
- 1 From the GWU MFA Department of Psychiatry and Behavioral Sciences, George Washington University, Washington, DC.
- PMID: 27977470
- DOI: 10.1097/JCP.0000000000000636
Abstract
Background: Despite initial reports of efficacy in bipolar depression, multicenter trials did not show aripiprazole to be better than placebo, possibly because the doses used were too high, leading to lower efficacy and high dropout rates. This study evaluated the effects of low-dose aripiprazole. Extensive clinical experience has suggested that doses beyond 5 mg are rarely efficacious.
This study evaluated the effects of low-dose aripiprazole. Extensive clinical experience has suggested that doses beyond 5 mg are rarely efficacious.
Methods: Data were gathered from patients with bipolar II or bipolar not otherwise specified depression using a retrospective chart review. Efficacy was assessed with the Clinical Global Impression-Improvement score. Patients who had at least 2 trials of aripiprazole were included in a retrospective off-on-off-on experimental design. All patients were on other medications when aripiprazole was started. Patients were treated with doses of 1 to 5 mg.
Findings: On average, patients were rated improved or very much improved compared with baseline. Sixteen of 211 patients worsened or experienced no change. Forty-four patients (21%) discontinued due to adverse effects. The group of patients who underwent off-on-off-on trials experienced statistically significant improvement when they started and restarted aripiprazole, and statistically significant worsening when they discontinued it.
Conclusions: When treating bipolar II or bipolar not otherwise specified depression, low doses of aripiprazole, 5 mg or less, may be more effective and better tolerated than higher ones. Clinicians should start treatment with a very low dose and give patients time to respond.
Similar articles
-
The effectiveness and tolerability of aripiprazole for pediatric bipolar disorders: a retrospective chart review.
Barzman DH, DelBello MP, Kowatch RA, Gernert B, Fleck DE, Pathak S, Rappaport K, Delgado SV, Campbell P, Strakowski SM. Barzman DH, et al. J Child Adolesc Psychopharmacol. 2004 Winter;14(4):593-600. doi: 10.1089/cap.2004.14.593. J Child Adolesc Psychopharmacol. 2004. PMID: 15662152
-
Adjunctive aripiprazole in treatment-resistant bipolar depression.
Ketter TA, Wang PW, Chandler RA, Culver JL, Alarcon AM. Ketter TA, et al. Ann Clin Psychiatry. 2006 Jul-Sep;18(3):169-72. doi: 10.1080/10401230600801176. Ann Clin Psychiatry. 2006. PMID: 16923655
-
Aripiprazole monotherapy in nonpsychotic bipolar I depression: results of 2 randomized, placebo-controlled studies.
Thase ME, Jonas A, Khan A, Bowden CL, Wu X, McQuade RD, Carson WH, Marcus RN, Owen R. Thase ME, et al. J Clin Psychopharmacol. 2008 Feb;28(1):13-20. doi: 10.1097/jcp.0b013e3181618eb4. J Clin Psychopharmacol. 2008. PMID: 18204335 Clinical Trial.
-
Aripiprazole Long-Acting Injectable for Maintenance Treatment of Bipolar I Disorder in Adults.
Aggarwal A, Schrimpf L, Lauriello J.
 Aggarwal A, et al. Clin Schizophr Relat Psychoses. 2018 Jan;11(4):221-223. doi: 10.3371/CSRP.AGSC.010318. Clin Schizophr Relat Psychoses. 2018. PMID: 29341822 Review.
Aggarwal A, et al. Clin Schizophr Relat Psychoses. 2018 Jan;11(4):221-223. doi: 10.3371/CSRP.AGSC.010318. Clin Schizophr Relat Psychoses. 2018. PMID: 29341822 Review. -
A clinical review of aripiprazole in bipolar depression and maintenance therapy of bipolar disorder.
Yatham LN. Yatham LN. J Affect Disord. 2011 Jan;128 Suppl 1:S21-8. doi: 10.1016/S0165-0327(11)70005-2. J Affect Disord. 2011. PMID: 21220077 Review.
See all similar articles
Cited by
-
Is aripiprazole similar to quetiapine for treatment of bipolar depression? Results from meta-analysis of Chinese data.
Tao H, Wang J, Shen D, Sun F, Jin W. Tao H, et al. Front Psychiatry.
 2022 Sep 9;13:850021. doi: 10.3389/fpsyt.2022.850021. eCollection 2022. Front Psychiatry. 2022. PMID: 36159936 Free PMC article.
2022 Sep 9;13:850021. doi: 10.3389/fpsyt.2022.850021. eCollection 2022. Front Psychiatry. 2022. PMID: 36159936 Free PMC article. -
Using Extended-Release Injectable Aripiprazole for the Successful Treatment of Depressive Symptoms in Bipolar I Disorder.
Kuo J, Lin SK. Kuo J, et al. Case Rep Psychiatry. 2020 Feb 21;2020:2615748. doi: 10.1155/2020/2615748. eCollection 2020. Case Rep Psychiatry. 2020. PMID: 32148990 Free PMC article.
-
The Potential Utility of Aripiprazole Augmentation for Major Depressive Disorder with Mixed Features Specifier: A Retrospective Study.
Han C, Wang SM, Bahk WM, Lee SJ, Patkar AA, Masand PS, Pae CU. Han C, et al. Clin Psychopharmacol Neurosci. 2019 Nov 20;17(4):495-502. doi: 10.
 9758/cpn.2019.17.4.495. Clin Psychopharmacol Neurosci. 2019. PMID: 31671486 Free PMC article.
9758/cpn.2019.17.4.495. Clin Psychopharmacol Neurosci. 2019. PMID: 31671486 Free PMC article.
MeSH terms
Substances
Full text links
Wolters Kluwer
Cite
Format: AMA APA MLA NLM
Send To
Aripiprazole (Abilify) | NAMI: National Alliance on Mental Illness
Brand names:
-
- Tablets: 2 mg, 5mg, 10 mg, 15 mg, 20 mg, 30 mg
- Oral disintegrating: 10 mg, 15 mg
- Solution: 1 mg/mL
- Abilify MyCite®
- Tablet with a digestible sensor: 2 mg, 5 mg, 10 mg, 15 mg, 20 mg, 30 mg
- Abilify Maintena®
- Extended-release injectable suspension: 300 mg, 400 mg
- Abilify Aristada® (aripiprazole lauroxil)
- Extended-release injectable suspension: 441 mg, 662 mg, 882 mg, 1064 mg
- Aristada Initio® (aripiprazole lauroxil)
- Extended-release injectable suspension: 675 mg
Generic name: aripiprazole (ay ri PIP ray zole), aripiprazole lauroxil (law rox il)
- Aripiprazole
- Oral tablet: 2 mg, 5mg, 10 mg, 15 mg, 20 mg, 30 mg
- Orally disintegrating tablet: 10 mg, 15 mg
- Oral solution: 1 mg/mL
All FDA black box warnings are at the end of this fact sheet. Please review before taking this medication.
Please review before taking this medication.
What Is Aripiprazole And What Does It Treat?
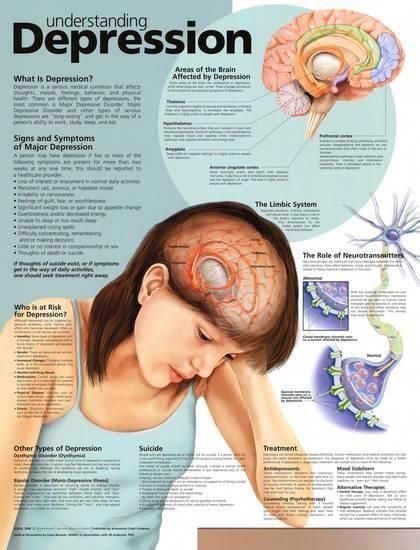
Aripiprazole is a medication that works in the brain to treat schizophrenia. It is also known as a second generation antipsychotic (SGA) or atypical antipsychotic. Aripiprazole rebalances dopamine and serotonin to improve thinking, mood, and behavior.
Symptoms of schizophrenia include:
- Hallucinations — imagined voices or images that seem real
- Delusions — beliefs that are not true (e.g., other people are reading your thoughts)
- Disorganized thinking or trouble organizing your thoughts and making sense
- Little desire to be around other people
- Trouble speaking clearly
- Lack of motivation
Aripiprazole may help some or all of these symptoms.
Aripiprazole is also FDA approved for the following indications:
- Acute treatment of manic or mixed episodes of bipolar disorder (when used alone or with lithium or valproate)
- Maintenance (long-term) treatment of bipolar disorder
- Adjunctive treatment of major depressive disorder.
 This means aripiprazole is used in addition to an antidepressant to help treat depression.
This means aripiprazole is used in addition to an antidepressant to help treat depression. - Irritability associated with autistic disorders
- Tourette's syndrome
This medication sheet will focus primarily on schizophrenia. Find more information about bipolar disorder, depression and autism spectrum disorders here.
Aripiprazole may also be helpful when prescribed “off-label” for borderline personality disorder or drug-induced hyperprolactinemia (elevated prolactin levels caused by other antipsychotics). “Off-label” means that it hasn’t been approved by the Food and Drug Administration for this condition. Your mental health provider should justify his or her thinking in recommending an “off-label” treatment. They should be clear about the limits of the research around that medication and if there are any other options.
What Is The Most Important Information I Should Know About Aripiprazole?
Schizophrenia requires long-term treatment. Do not stop taking aripiprazole, even when you feel better. With input from you, your health care provider will assess how long you will need to take the medicine.
With input from you, your health care provider will assess how long you will need to take the medicine.
Missing doses of aripiprazole may increase your risk for a relapse in your symptoms. Do not stop taking aripiprazole or change your dose without talking to with your health care provider first. For aripiprazole to work properly, it should be taken every day as ordered by your health care provider.
Are There Specific Concerns About Aripiprazole And Pregnancy?
If you are planning on becoming pregnant, notify your health care provider to best manage your medications. People living with schizophrenia who wish to become pregnant face important decisions. This is a complex decision since untreated schizophrenia has risks to the fetus, as well as the mother. It is important to discuss the risks and benefits of treatment with your doctor and caregivers.
Antipsychotic use during the third trimester of pregnancy has a risk for abnormal muscle movements (extrapyramidal symptoms [EPS]) and/or withdrawal symptoms in newborns following delivery.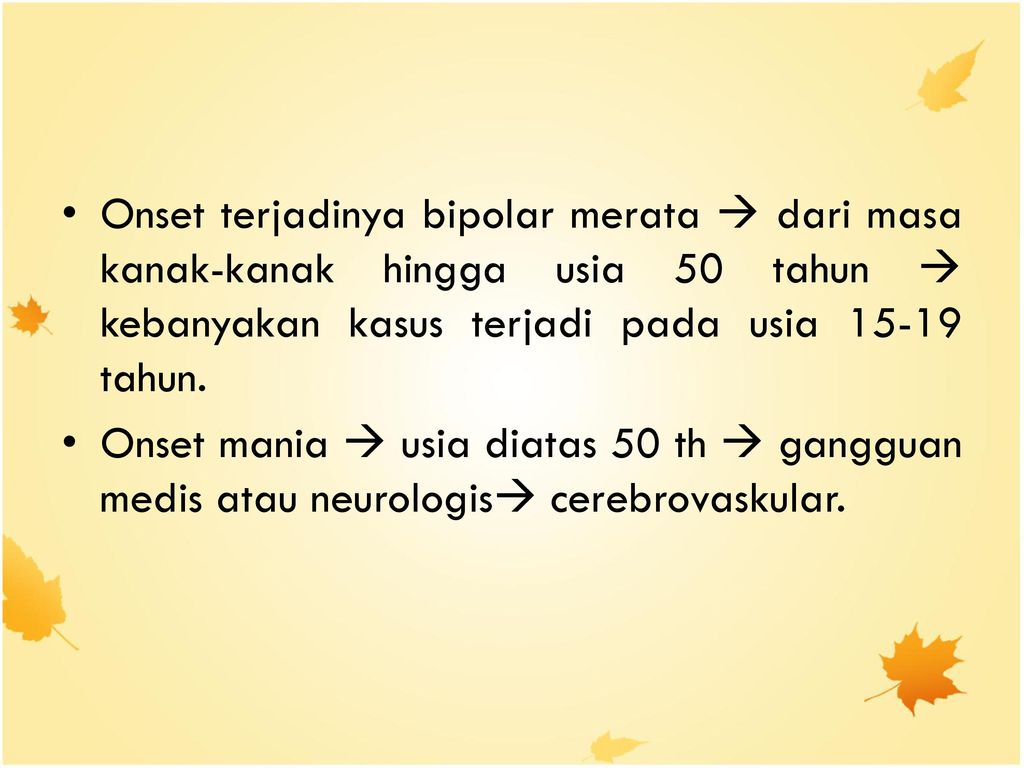 Symptoms in the newborn may include agitation, feeding disorder, hypertonia, hypotonia, respiratory distress, somnolence, and tremor; these effects may be self-limiting or require hospitalization.
Symptoms in the newborn may include agitation, feeding disorder, hypertonia, hypotonia, respiratory distress, somnolence, and tremor; these effects may be self-limiting or require hospitalization.
In general, infants exposed to SGAs via breast milk should be monitored weekly for the first month of exposure for symptoms, such as appetite changes, insomnia, irritability, or lethargy.
Caution is advised with breastfeeding since aripiprazole does pass into breast milk.
What Should I Discuss With My Healthcare Provider Before Taking Aripiprazole?
- Symptoms of your condition that bother you the most
- If you have thoughts of suicide or harming yourself
- Medications you have taken in the past for your condition, whether they were effective or caused any adverse effects
- If you ever had muscle stiffness, shaking, tardive dyskinesia, neuroleptic malignant syndrome, or weight gain caused by a medication
- If you experience side effects from your medications, discuss them with your provider.
 Some side effects may pass with time, but others may require changes in the medication
Some side effects may pass with time, but others may require changes in the medication - Any psychiatric or medical problems you have, such as heart rhythm problems, long QT syndrome, heart attacks, diabetes, high cholesterol, or seizures
- If you have a family history of diabetes or heart disease
- All other medications you are currently taking (including over the counter products, herbal and nutritional supplements) and any medication allergies you have
- Other non-medication treatment you are receiving, such as talk therapy or substance abuse treatment. Your provider can explain how these different treatments work with the medication
- If you are pregnant, plan to become pregnant, or are breast-feeding
- If you smoke, drink alcohol, or use illegal drugs
How Should I Take Aripiprazole?
Aripiprazole tablets and suspension are usually taken 1 time per day with or without food. Typically, patients begin at a low dose of medicine and the dose is increased slowly over several weeks.
The oral dose of aripiprazole usually ranges from 2 mg to 30 mg taken once daily. The dose of aripiprazole maintena extended-release injection ranges from 300 mg to 400 mg given once monthly; the dose of aripiprazole lauroxil extended-release injection ranges from 441 mg to 1064 mg – depending on the dose, it is given once per month, every 6 weeks, or every 2 months. Aripiprazole Maintena requires a two-week oral medication overlap; aripiprazole lauroxil requires a three-week oral overlap. Aripiprazole lauroxil Initio is typically given after an oral dose of aripiprazole along with an aripiprazole lauroxil injection – this allows for a one-day initiation and does not require further oral overlap. Only your health care provider can determine the correct formulation and dose for you.
Use a calendar, pillbox, alarm clock, or cell phone alert to help you remember to take your medication. You may also ask a family member or a friend to remind you or check in with you to be sure you are taking your medication.
What Happens If I Miss A Dose Of Aripiprazole?
If you miss a dose of aripiprazole, take it as soon as you remember, unless it is closer to the time of your next dose. Do not double your next dose or take more than what is prescribed. If you miss an injection, call your doctor or pharmacist right away. Discuss this with your health care provider.
What Should I Avoid While Taking Aripiprazole?
Avoid drinking alcohol or using illegal drugs while you are taking aripiprazole. They may decrease the benefits (e.g., worsen your confusion) and increase adverse effects (e.g., sedation) of the medication.
What Happens If I Overdose With Aripiprazole?
If an overdose occurs call your doctor or 911. You may need urgent medical care. You may also contact the poison control center at 1-800-222-1222.
A specific treatment to reverse the effects of aripiprazole does not exist.
What Are Possible Side Effects Of Aripiprazole?
Common side effects
Headache, extrapyramidal symptoms, drowsiness, restlessness, fatigue, sedation, agitation, insomnia, anxiety, weight gain, cholesterol abnormalities, increased glucose, nausea, vomiting, constipation, application site rash (MyCite), tremor
Rare/serious side effects
Rash, dry mouth, muscle aches, seizure, agitation
Aripiprazole may increase the blood levels of a hormone called prolactin.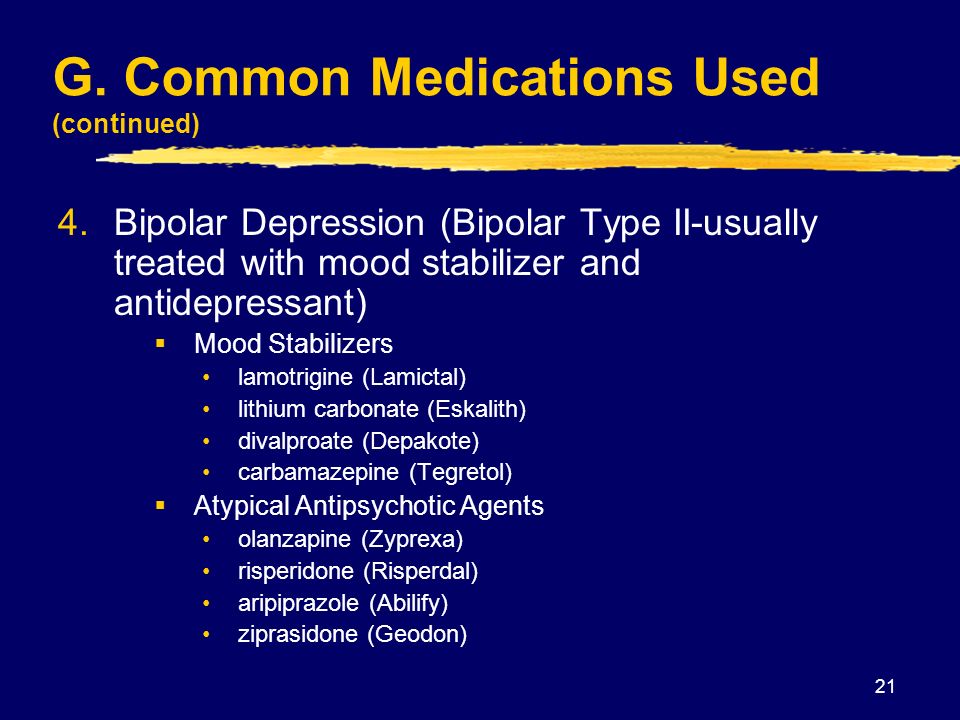 Side effects of increased prolactin levels include females losing their period, production of breast milk and males losing their sex drive or possibly experiencing erectile problems. Long term (months or years) of elevated prolactin can lead to osteoporosis or increased risk of bone fractures.
Side effects of increased prolactin levels include females losing their period, production of breast milk and males losing their sex drive or possibly experiencing erectile problems. Long term (months or years) of elevated prolactin can lead to osteoporosis or increased risk of bone fractures.
Some people may develop muscle-related side effects while taking aripiprazole. The technical terms for these are “extrapyramidal symptoms” (EPS) and “tardive dyskinesia” (TD). Symptoms of EPS include restlessness, tremor, and stiffness. TD symptoms include slow or jerky movements that one cannot control, often starting in the mouth with tongue rolling or chewing movements.
Temperature regulation: Impaired core body temperature regulation may occur; caution with strenuous exercise, heat exposure, and dehydration.
Second generation antipsychotics (SGAs) increase the risk of weight gain, high blood sugar, and high cholesterol. This is also known as metabolic syndrome. Your healthcare provider may ask you for a blood sample to check your cholesterol, blood sugar, and hemoglobin A1c (a measure of blood sugar over time) while you take this medication.
Information on healthy eating and adding exercise to decrease your chances of developing metabolic syndrome may be found at the following sites:
- http://www.helpguide.org/articles/healthy-eating/healthy-eating.htm
- http://www.helpguide.org/home-pages/exercise-fitness.htm
SGAs have been linked with higher risk of death, strokes, and transient ischemic attacks (TIAs) in elderly people with behavior problems due to dementia.
All antipsychotics have been associated with the risk of sudden cardiac death due to an arrhythmia (irregular heart beat). To minimize this risk, antipsychotic medications should be used in the smallest effective dose when the benefits outweigh the risks. Your doctor may order an EKG to monitor for irregular heartbeat.
Neuroleptic malignant syndrome is a rare, life threatening adverse effect of antipsychotics which occurs in <1% of patients. Symptoms include confusion, fever, extreme muscle stiffness, and sweating. If any of these symptoms occur, contact your healthcare provider immediately.
All antipsychotics can cause sedation, dizziness, or orthostatic hypotension (a drop in blood pressure when standing up from sitting or lying down). These side effects may lead to falls which could cause bone fractures or other injuries. This risk is higher for people with conditions or other medications that could worsen these effects. If falls or any of these symptoms occur, contact your healthcare provider.
The U.S. Food and Drug Administration (FDA) is warning that compulsive or uncontrollable urges to gamble, binge eat, shop, and have sex have been reported with the use of aripiprazole. These uncontrollable urges were reported to have stopped when the medicine was discontinued or the dose was reduced. These impulse-control problems are rare, but they may result in harm to the patient and others if not recognized.
Are There Any Risks For Taking Aripiprazole For Long Periods Of Time?
Tardive dyskinesia (TD) is a side effect that develops with prolonged use of antipsychotics.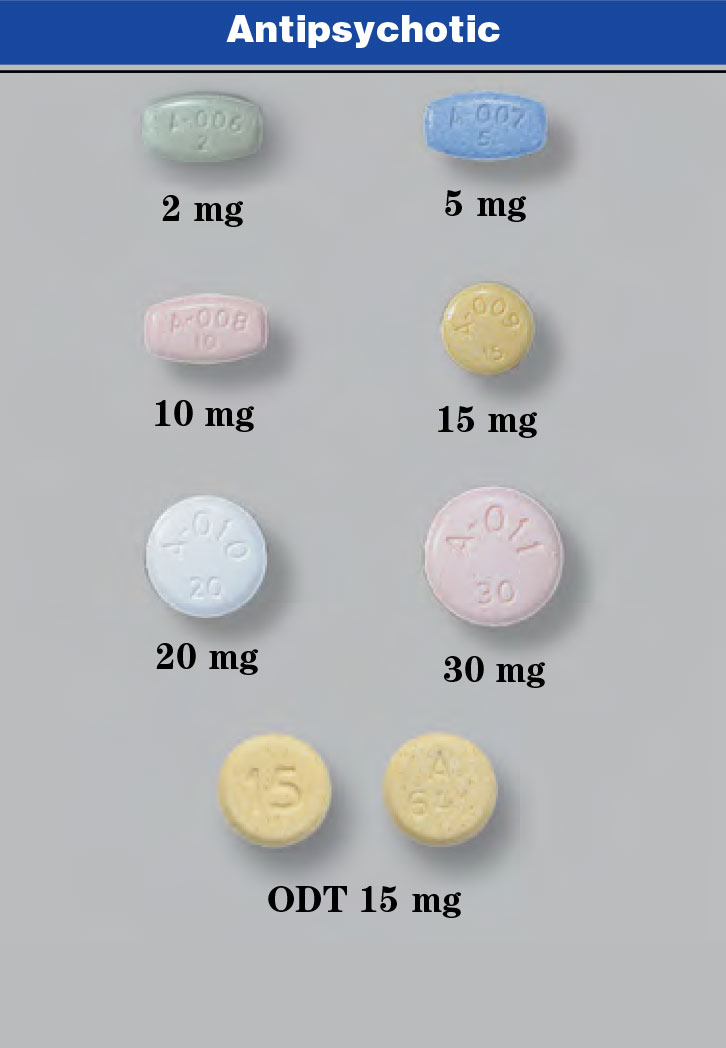 Medications such as aripiprazole have been shown to have a lower risk of TD compared to older antipsychotics, such as Haldol (haloperidol). If you develop symptoms of TD, such as grimacing, sucking, and smacking of lips, or other movements that you cannot control, contact your health care provider immediately. All patients taking either first or second generation antipsychotics should have an Abnormal Involuntary Movement Scale (AIMS) completed regularly by their healthcare provider to monitor for TD.
Medications such as aripiprazole have been shown to have a lower risk of TD compared to older antipsychotics, such as Haldol (haloperidol). If you develop symptoms of TD, such as grimacing, sucking, and smacking of lips, or other movements that you cannot control, contact your health care provider immediately. All patients taking either first or second generation antipsychotics should have an Abnormal Involuntary Movement Scale (AIMS) completed regularly by their healthcare provider to monitor for TD.
Second generation antipsychotics (SGAs) increase the risk of diabetes, weight gain, high cholesterol, and high triglycerides. (See “Serious Side Effects” section for monitoring recommendations).
What Other Medications May Interact With Aripiprazole?
The following medications may increase the levels and effects of aripiprazole:
- The antibiotic clarithromycin (Biaxin®)
- Antidepressants, such as fluoxetine (Prozac®), paroxetine (Paxil®), and nefazodone
- Antifungals, such as fluconazole (Diflucan®), ketoconazole (Nizoral®), and itraconazole (Sporanox®)
- The antiarrhymia agent quinidine
- HIV medications, such as the protease inhibitors indinavir (Crixivan®), ritonavir (Norvir®), saquinavir (Fortovase®, Invirase®), and lopinavir/ritonavir (Kaletra®)
The following medications may decrease the levels and effects of aripiprazole:
- carbamazepine (Tegretol®)
- rifampin (Rifadin®)
How Long Does It Take For Aripiprazole To Work?
It is very important to tell your doctor how you feel things are going during the first few weeks after you start taking aripiprazole. It will probably take several weeks to see big enough changes in your symptoms to decide if aripiprazole is the right medication for you.
It will probably take several weeks to see big enough changes in your symptoms to decide if aripiprazole is the right medication for you.
Antipsychotic treatment is generally needed lifelong for persons with schizophrenia. Your doctor can best discuss the duration of treatment you need based on your symptoms and illness.
- Hallucinations, disorganized thinking, and delusions may improve in the first 1-2 weeks
- Sometimes these symptoms do not completely go away
- Motivation and desire to be around other people can take at least 1-2 weeks to improve
- Symptoms continue to get better the longer you take aripiprazole
- It may take 2-3 months before you get the full benefit of aripiprazole
Summary of FDA Black Box Warnings
Increased mortality in elderly patients with dementia-related psychosis
- Both first generation (typical) and second generation (atypical) antipsychotics are associated with an increased risk of mortality in elderly patients when used for dementia related psychosis.

- Although there were multiple causes of death in studies, most deaths appeared to be due to cardiovascular causes (e.g. sudden cardiac death) or infection (e.g. pneumonia).
- Antipsychotics are not indicated for the treatment of dementia-related psychosis.
Suicidal Thoughts or Actions in Children, Teens, and Young Adults
Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide.
- Patients treated with antidepressants may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking medications. This risk may persist until significant remission occurs.
- Patients, their families, and caregivers should be alert to the emergence of anxiety, restlessness, irritability, aggressiveness and insomnia. If these symptoms emerge, they should be reported to the patient’s prescriber or health care professional.

- All patients being treated with this medication for depression should watch for and notify their healthcare provider for worsening symptoms, suicidality and unusual changes in behavior, especially during the first few months of treatment.
Provided by
(July 2022)
©2022 The College of Psychiatric and Neurologic Pharmacists (CPNP) and the National Alliance on Mental Illness (NAMI). CPNP and NAMI make this document available under the Creative Commons Attribution-No Derivatives 4.0 International License. Last Updated: January 2016.
This information is being provided as a community outreach effort of the College of Psychiatric and Neurologic Pharmacists. This information is for educational and informational purposes only and is not medical advice. This information contains a summary of important points and is not an exhaustive review of information about the medication. Always seek the advice of a physician or other qualified medical professional with any questions you may have regarding medications or medical conditions.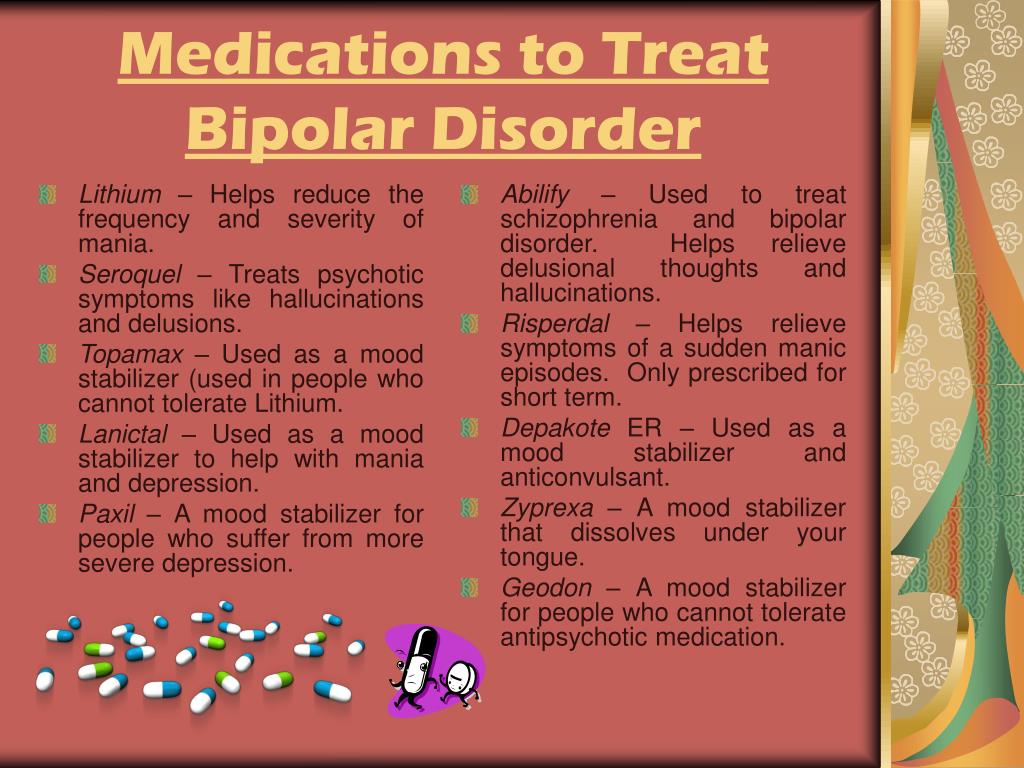 Never delay seeking professional medical advice or disregard medical professional advice as a result of any information provided herein. The College of Psychiatric and Neurologic Pharmacists disclaims any and all liability alleged as a result of the information provided herein.
Never delay seeking professional medical advice or disregard medical professional advice as a result of any information provided herein. The College of Psychiatric and Neurologic Pharmacists disclaims any and all liability alleged as a result of the information provided herein.
what they are and what effects they have
Psychiatrists usually recommend medication as the initial treatment to control symptoms as quickly as possible.
Once your symptoms are under control, you will receive supportive care to reduce your risk of relapse.
Supportive care also reduces the chance that minor mood changes turn into mania or depression.
Several types of drugs are used to treat bipolar disorder.
These include mood stabilizers, antidepressants and anti-anxiety drugs. Your doctor may prescribe one or a combination of medications for maximum effect.
Finding the right remedy or combination of remedies will require trial and error.
You may need to change your medications because of side effects.
Each drug may take up to eight weeks to see the full effect.
Usually only one drug is changed at a time.
This helps your doctor better monitor and determine which one is not working.
The following types of drugs are used to treat bipolar disorder
Lithium
Lithium (such as Lithobid) is a mood-stabilizing drug that has been used since the 1970s.
It helps control the symptoms of acute mania.
It is also effective in preventing the recurrence of periods of mania and depression.
Common side effects include weight gain and digestive problems.
The drug may also affect the thyroid and kidneys. Periodic blood tests are needed to monitor the condition of the thyroid gland and kidneys.
Lithium is a category D drug that should be avoided during pregnancy if possible.
However, in some cases the benefits may outweigh the potential risks.
Anticonvulsants
Anticonvulsants are mood stabilizers used to treat bipolar disorder.
They have been in use since the mid-1990s. A
Anticonvulsants include:
- divalproex sodium (Depakot)
- lamotrigine (lamiktal)
- valproic acid (Depaken)
Common side effects of anticonvulsants include weight gain, drowsiness and inability to sit still.
Anticonvulsants are also associated with an increased risk of suicidal thoughts and behavior.
Valproic acid is known to cause birth defects.
Lamictal is known to cause a dangerous rash.
Tell your doctor about any new rash that develops while taking Lamictal.
Antipsychotics
Antipsychotics are another treatment option. Some commonly prescribed antipsychotics include:
- olanzapine (Zyprexa)
- risperidone (Risperdal)
- Quetiapine (Seroquel)
- lurasidone (Latuda)
- aripiprazole (Abilify)
- Azenapine (Saphris)
Common side effects include weight gain, drowsiness, dry mouth, decreased libido and blurred vision.
Antipsychotics may also affect memory and attention.
They are also known to cause involuntary movements of the face or body.
Antidepressants
These include serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), monoamine oxidase inhibitors (MAOIs), and tricyclics.
Antidepressants may be added to help manage depression in bipolar disorder, but they can sometimes cause manic episodes.
To reduce the risk of a mixed or manic episode, they are often given with mood stabilizers or antipsychotics.
As with any medication, talk to your doctor about the risks and benefits of taking antidepressants for bipolar disorder.
Some of the most commonly prescribed antidepressants are:
- SNRIs
- desvenlafaxine (Pristiq)
- duloxetine (Cymbalta, Yentreve)
- venlafaxine (Effexor)
- SSRIs
- citalopram (Celexa)
- escitalopram (Lexapro)
- fluoxetine (Prozac, weekly Prozac)
- paroxetine (Paxil, Paxil CR, Pekseva)
- sertraline (Zoloft)
- Tricyclics
- amitriptyline
- desipramine (Norpramine)
- imipramine (Tofranil, Tofranil-PM)
- nortriptyline (pamelor)
- IMAO
- phenelzine (nardil)
- tranylcypromine (parnate)
In general, MAOIs are rarely prescribed unless the patient has a poor response to SNRIs or SSRIs.
Common side effects include decreased sex drive, disturbed sleep, increased appetite, dry mouth, gastrointestinal disturbances, and menstrual problems.
While taking an MAOI, it is important to avoid other drugs and foods, such as wine and cheese, which can cause a rare but dangerous condition known as serotonin syndrome.
Benzodiazepines and Bipolar Disorder
This is a group of drugs with anti-anxiety properties. Benzodiazepines include:
- alprazolam (Xanax)
- chlordiazepoxide (librium)
- clonazepam (Klonopin)
- diazepam (Valium)
- lorazepam (ativan)
Side effects may include drowsiness, decreased muscle coordination, and problems with balance and memory.
These drugs should be used with caution due to the risk of dependence.
Symbiax
This medication is a combination of fluoxetine and the antipsychotic olanzapine. Symbyax has both antidepressant and mood stabilizer properties.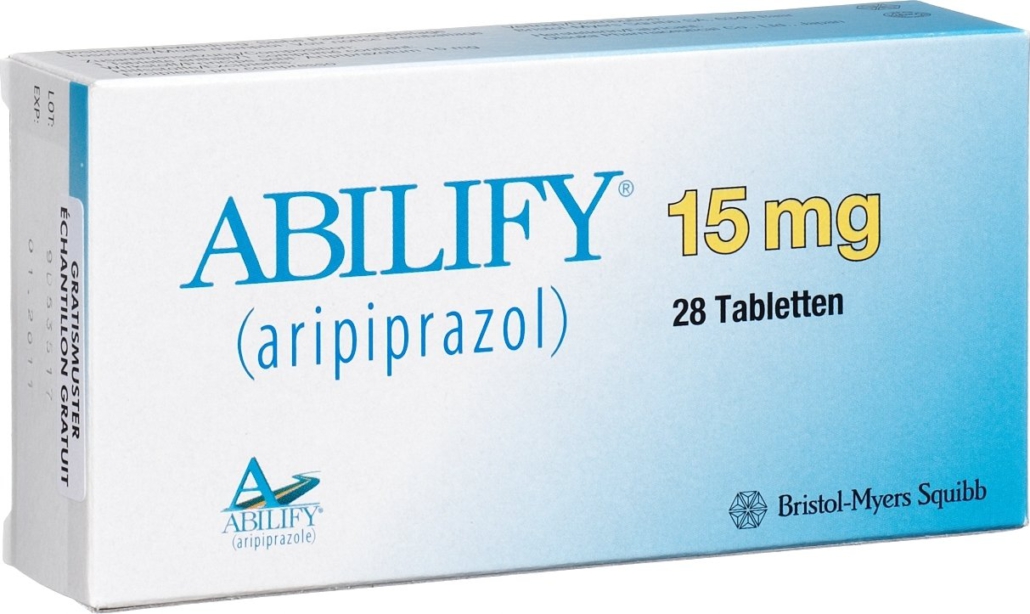
Side effects may include increased appetite, sexual problems, drowsiness, fatigue, and dry mouth.
If your doctor prescribes this medicine, ask if separate prescriptions for the two ingredients are cheaper.
There is nothing special about the combination tablet. It's just a new formulation of two existing drugs.
References:
- Bipolar disorder. (2016).
nimh.nih.gov/health/topics/bipolar-disorder/index.shtml - FDA pregnancy categories (2017).
chemm.nlm.nih.gov/pregnancycategories.htm - Mayo Clinic staff. (2017). serotonin syndrome.
mayoclinic.org/diseases-conditions/serotonin syndrome/symptoms-causes/syc-20354758 - Mayo Clinic staff. (2018). Bipolar disorder.
mayoclinic.org/diseases-conditions/bipolar disorder/symptoms-causes/syc-20355955
Read also:
Emergency Live More. .. Live: download your newspaper's new free app for IOS and Android
.. Live: download your newspaper's new free app for IOS and Android
What you need to know about substance use disorder
Seasonal depression can happen in the spring: why and how to deal with it
Don’t ban ketamine: the real promise of this anesthetic in prehospital medicine from Lancet
Intranasal ketamine for treating patients with acute pain in ED
Delirium and dementia: what's the difference?
Prehospital Ketamine Use - VIDEO
Ketamine can be an emergency deterrent for people at risk of suicide
Everything you need to know about bipolar disorder
Source:
Health Line
Sanofi-Aventis and Bristol-Myers Squibb merger is controversial
It can be said without exaggeration that the global pharmaceutical community is following the situation around Sanofi-Aventis and Bristol-Myers Squibb with great attention. According to foreign media, these companies have signed a preliminary agreement on the merger. And although no official statements have been made yet, and the company's management refuses to comment on the reports that have appeared in the press, a possible deal causes a lot of speculation.
And although no official statements have been made yet, and the company's management refuses to comment on the reports that have appeared in the press, a possible deal causes a lot of speculation.
As a result of a possible deal, a company with a market capitalization of 175 billion US dollars (135 billion euros) will appear on the world pharmaceutical market, which will allow it to come close to the leader in this indicator - Pfizer (188 billion US dollars). However, in terms of sales, the new company will overtake Pfizer and take a leading position. In addition, it will be able to become the world's No. 1 R&D spender, slightly outperforming Pfizer and outperforming GlaxoSmithKline by more than 2x.
In an environment where the development of one drug costs the manufacturer $ 800 million, the largest companies have undeniable advantages. However, many market participants still agree that strategic mergers / acquisitions are needed for success, and not mega-deals between pharmaceutical giants. But in this case, the situation is special - both companies have been cooperating for a long time in the field of sales of two drugs - the antihypertensive Avapro and the anticoagulant Plavix. By the way, regarding the latter, the companies got stuck in a lawsuit against the Canadian manufacturer of generic drugs - Apotex.
But in this case, the situation is special - both companies have been cooperating for a long time in the field of sales of two drugs - the antihypertensive Avapro and the anticoagulant Plavix. By the way, regarding the latter, the companies got stuck in a lawsuit against the Canadian manufacturer of generic drugs - Apotex.
Sanofi-Aventis has 17 drugs in the final stages of clinical trials (CTs), while BMS has 6. And while any merger inevitably attracts the attention of antitrust authorities (in this case, the US and the EU), according to experts, the analysis of the generalized portfolio of potential drugs both companies shows that regulators are unlikely to be required to diversify individual drugs.
Both companies are developing new drugs for the prevention of thrombosis and the treatment of diabetes mellitus, but the main therapeutic area where the companies' portfolios overlap the most is oncology.
Some analysts say the deal may not make sense in the long run, especially for BMS. In their opinion, it will at best achieve certain short-term goals. The black streak that has been chasing Bristol-Myers Squibb for the past 5 years is ending. Companies need to be revived. One of the positive steps taken by P. Dolan as an executive director (we recall that he was dismissed by decision of the Board of Directors in September 2006) was that he was able to reorient the company to the markets of specialized drugs, in particular, for the treatment of rheumatic and oncological diseases, which do not require an army of medraps to advance. In addition, BMS has a good relationship with the FDA - since 2006, 6 drugs of the company have been approved, incl. Abilify for schizophrenia and bipolar disorder, the antiretroviral drug Reyataz, Orenica for rheumatoid arthritis, and Sprycel for chronic myelogenous leukemia. Revenues from these new drugs cannot yet compensate for losses resulting from the expiration of patents for some drugs. But this period may soon end. Analysts, who advised investors to sell BMS shares before P.
In their opinion, it will at best achieve certain short-term goals. The black streak that has been chasing Bristol-Myers Squibb for the past 5 years is ending. Companies need to be revived. One of the positive steps taken by P. Dolan as an executive director (we recall that he was dismissed by decision of the Board of Directors in September 2006) was that he was able to reorient the company to the markets of specialized drugs, in particular, for the treatment of rheumatic and oncological diseases, which do not require an army of medraps to advance. In addition, BMS has a good relationship with the FDA - since 2006, 6 drugs of the company have been approved, incl. Abilify for schizophrenia and bipolar disorder, the antiretroviral drug Reyataz, Orenica for rheumatoid arthritis, and Sprycel for chronic myelogenous leukemia. Revenues from these new drugs cannot yet compensate for losses resulting from the expiration of patents for some drugs. But this period may soon end. Analysts, who advised investors to sell BMS shares before P.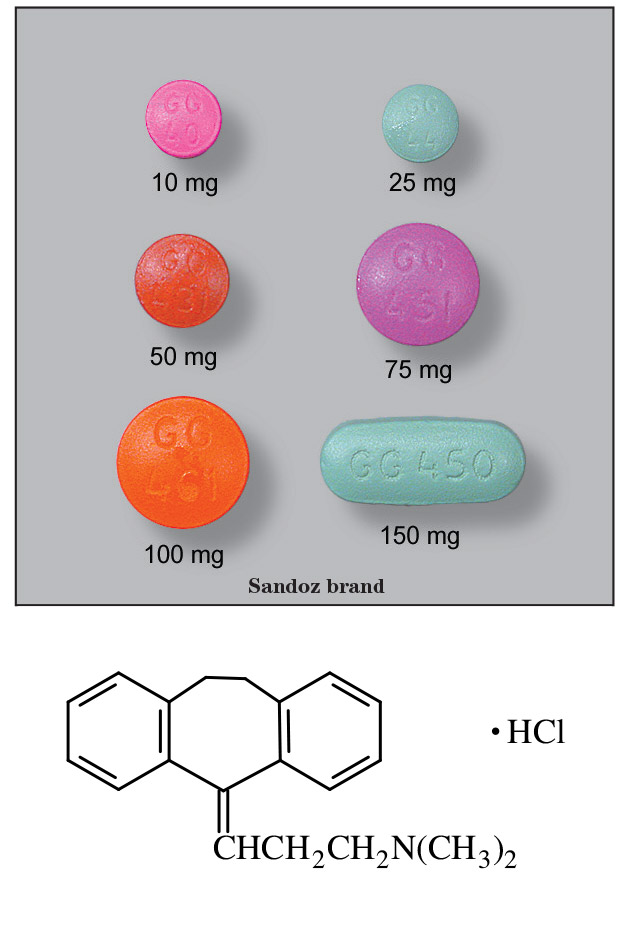 Dolan's departure, are now recommending buying. There are all prerequisites for optimism: until the end of the decade there is no threat from generic companies, and the existing drugs on the market are enough to maintain the company's shares at the proper level. Experts warn that the takeover of the company may have a negative impact on the process of bringing it out of the crisis. As experience shows, they say, mergers in the pharmaceutical industry do not always have a positive effect on the expansion of research and development activities. An example is given of Pfizer, which intends to close the laboratory in which the most popular drug in the world, Lipitor, was developed. This does not mean that the merged companies do not stimulate research and produce more drugs, but the opposite is too often the case.
Dolan's departure, are now recommending buying. There are all prerequisites for optimism: until the end of the decade there is no threat from generic companies, and the existing drugs on the market are enough to maintain the company's shares at the proper level. Experts warn that the takeover of the company may have a negative impact on the process of bringing it out of the crisis. As experience shows, they say, mergers in the pharmaceutical industry do not always have a positive effect on the expansion of research and development activities. An example is given of Pfizer, which intends to close the laboratory in which the most popular drug in the world, Lipitor, was developed. This does not mean that the merged companies do not stimulate research and produce more drugs, but the opposite is too often the case.
The most important factor behind the deal between Sanofi-Aventis and Bristol-Myers Squibb is Plavix, the world's second most popular drug after Lipitor. Its annual sales volume is 6 billion US dollars.