Intervention for borderline personality disorder
Borderline personality disorder - Diagnosis and treatment
Diagnosis
Personality disorders, including borderline personality disorder, are diagnosed based on a:
- Detailed interview with your doctor or mental health provider
- Psychological evaluation that may include completing questionnaires
- Medical history and exam
- Discussion of your signs and symptoms
A diagnosis of borderline personality disorder is usually made in adults, not in children or teenagers. That's because what appear to be signs and symptoms of borderline personality disorder may go away as children get older and become more mature.
Treatment
Borderline personality disorder is mainly treated using psychotherapy, but medication may be added. Your doctor also may recommend hospitalization if your safety is at risk.
Treatment can help you learn skills to manage and cope with your condition. It's also necessary to get treated for any other mental health disorders that often occur along with borderline personality disorder, such as depression or substance misuse. With treatment, you can feel better about yourself and live a more stable, rewarding life.
Psychotherapy
Psychotherapy — also called talk therapy — is a fundamental treatment approach for borderline personality disorder. Your therapist may adapt the type of therapy to best meet your needs. The goals of psychotherapy are to help you:
- Focus on your current ability to function
- Learn to manage emotions that feel uncomfortable
- Reduce your impulsiveness by helping you observe feelings rather than acting on them
- Work on improving relationships by being aware of your feelings and those of others
- Learn about borderline personality disorder
Types of psychotherapy that have been found to be effective include:
- Dialectical behavior therapy (DBT). DBT includes group and individual therapy designed specifically to treat borderline personality disorder. DBT uses a skills-based approach to teach you how to manage your emotions, tolerate distress and improve relationships.
- Schema-focused therapy. Schema-focused therapy can be done individually or in a group. It can help you identify unmet needs that have led to negative life patterns, which at some time may have been helpful for survival, but as an adult are hurtful in many areas of your life. Therapy focuses on helping you get your needs met in a healthy manner to promote positive life patterns.
- Mentalization-based therapy (MBT). MBT is a type of talk therapy that helps you identify your own thoughts and feelings at any given moment and create an alternate perspective on the situation. MBT emphasizes thinking before reacting.
- Systems training for emotional predictability and problem-solving (STEPPS). STEPPS is a 20-week treatment that involves working in groups that incorporate your family members, caregivers, friends or significant others into treatment. STEPPS is used in addition to other types of psychotherapy.
- Transference-focused psychotherapy (TFP).
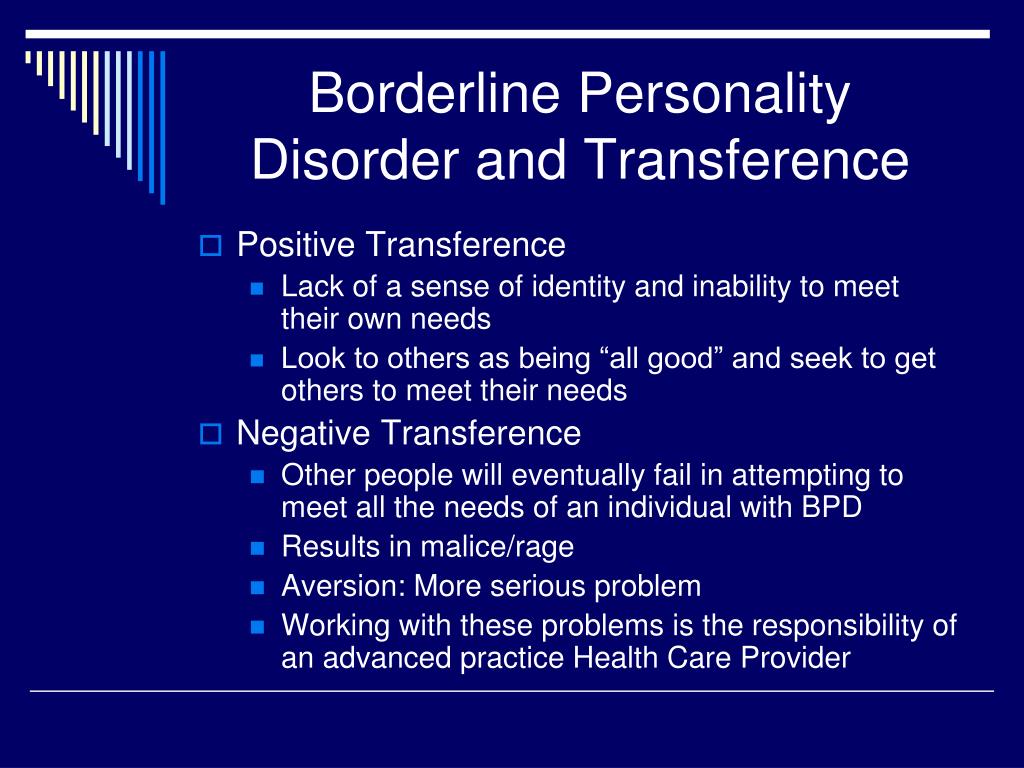 Also called psychodynamic psychotherapy, TFP aims to help you understand your emotions and interpersonal difficulties through the developing relationship between you and your therapist. You then apply these insights to ongoing situations.
Also called psychodynamic psychotherapy, TFP aims to help you understand your emotions and interpersonal difficulties through the developing relationship between you and your therapist. You then apply these insights to ongoing situations. - Good psychiatric management. This treatment approach relies on case management, anchoring treatment in an expectation of work or school participation. It focuses on making sense of emotionally difficult moments by considering the interpersonal context for feelings. It may integrate medications, groups, family education and individual therapy.
Medications
Although no drugs have been approved by the Food and Drug Administration specifically for the treatment of borderline personality disorder, certain medications may help with symptoms or co-occurring problems such as depression, impulsiveness, aggression or anxiety. Medications may include antidepressants, antipsychotics or mood-stabilizing drugs.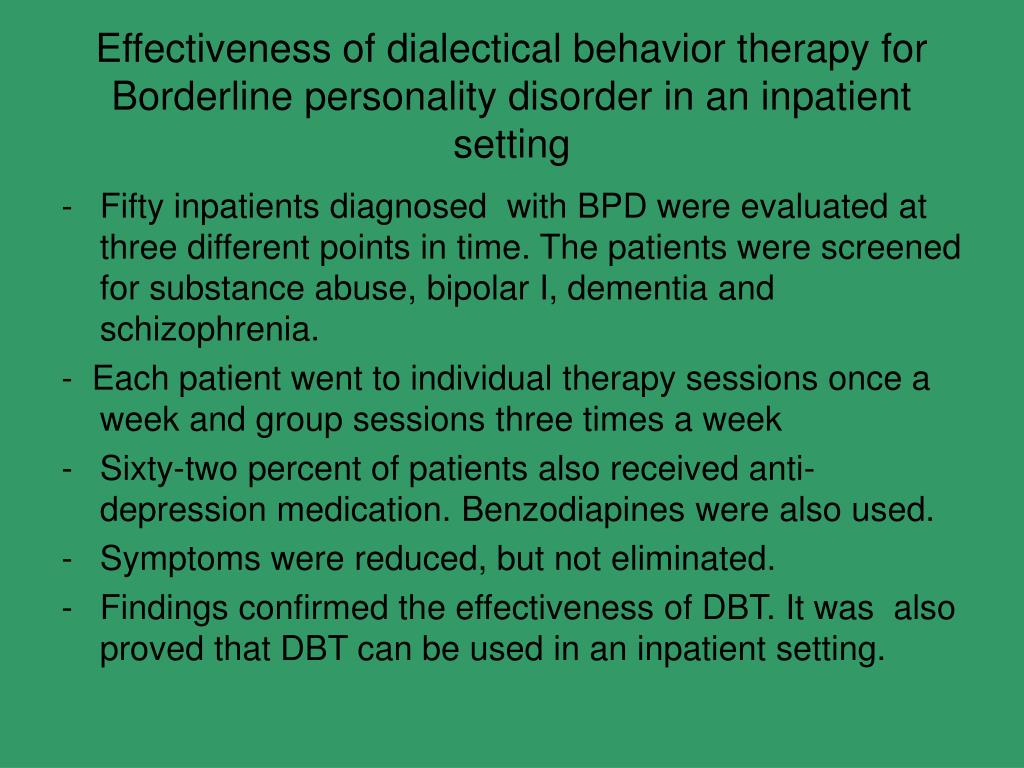
Talk to your doctor about the benefits and side effects of medications.
Hospitalization
At times, you may need more-intense treatment in a psychiatric hospital or clinic. Hospitalization may also keep you safe from self-injury or address suicidal thoughts or behaviors.
Recovery takes time
Learning to manage your emotions, thoughts and behaviors takes time. Most people improve considerably, but you may always struggle with some symptoms of borderline personality disorder. You may experience times when your symptoms are better or worse. But treatment can improve your ability to function and help you feel better about yourself.
You have the best chance for success when you consult a mental health provider who has experience treating borderline personality disorder.
More Information
- Psychotherapy
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Coping and support
Symptoms associated with borderline personality disorder can be stressful and challenging for you and those around you. You may be aware that your emotions, thoughts and behaviors are self-destructive or damaging, yet you feel unable to manage them.
You may be aware that your emotions, thoughts and behaviors are self-destructive or damaging, yet you feel unable to manage them.
In addition to getting professional treatment, you can help manage and cope with your condition if you:
- Learn about the disorder so that you understand its causes and treatments
- Learn to recognize what may trigger angry outbursts or impulsive behavior
- Seek professional help and stick to your treatment plan — attend all therapy sessions and take medications as directed
- Work with your mental health provider to develop a plan for what to do the next time a crisis occurs
- Get treatment for related problems, such as substance misuse
- Consider involving people close to you in your treatment to help them understand and support you
- Manage intense emotions by practicing coping skills, such as the use of breathing techniques and mindfulness meditation
- Set limits and boundaries for yourself and others by learning how to appropriately express emotions in a manner that doesn't push others away or trigger abandonment or instability
- Don't make assumptions about what people are feeling or thinking about you
- Reach out to others with the disorder to share insights and experiences
- Build a support system of people who can understand and respect you
- Keep up a healthy lifestyle, such as eating a healthy diet, being physically active and engaging in social activities
- Don't blame yourself for the disorder, but recognize your responsibility to get it treated
Preparing for your appointment
You may start by seeing your primary care doctor.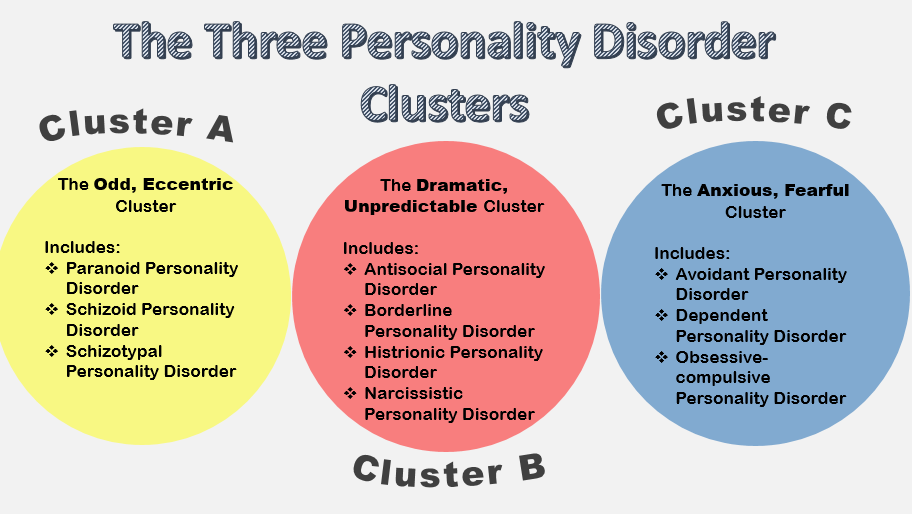 After an initial appointment, your doctor may refer you to a mental health provider, such as a psychologist or psychiatrist. Here's some information to help you prepare for your appointment.
After an initial appointment, your doctor may refer you to a mental health provider, such as a psychologist or psychiatrist. Here's some information to help you prepare for your appointment.
What you can do
Before your appointment, make a list of:
- Any symptoms you or people close to you have noticed, and for how long
- Key personal information, including traumatic events in your past and any current major stressors
- Your medical information, including other physical or mental health conditions
- All medications you take, including prescription and over-the-counter medications, vitamins and other supplements, and the doses
- Questions you want to ask your doctor so that you can make the most of your appointment
Take a family member or friend along, if possible. Someone who has known you for a long time may be able to share important information with the doctor or mental health provider, with your permission.
Basic questions to ask your doctor or a mental health provider include:
- What's likely causing my symptoms or condition?
- Are there any other possible causes?
- What treatments are most likely to be effective for me?
- How much can I expect my symptoms to improve with treatment?
- How often will I need therapy sessions and for how long?
- Are there medications that can help?
- What are the possible side effects of the medication you may prescribe?
- Do I need to take any precautions or follow any restrictions?
- I have these other health conditions. How can I best manage them together?
- How can my family or close friends help me in my treatment?
- Do you have any printed material that I can take? What websites do you recommend?
Don't hesitate to ask questions during your appointment.
What to expect from your doctor
A doctor or mental health provider is likely to ask you a number of questions.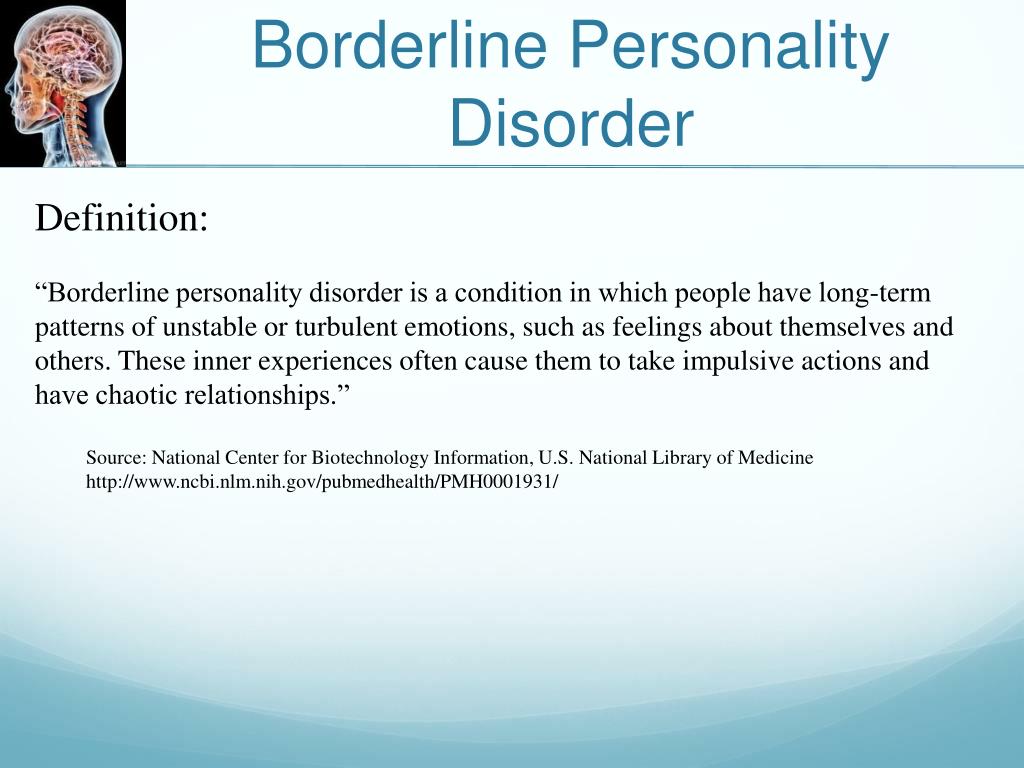 Be ready to answer them to save time for topics you want to focus on. Possible questions include:
Be ready to answer them to save time for topics you want to focus on. Possible questions include:
- What are your symptoms? When did you first notice them?
- How are these symptoms affecting your life, including your personal relationships and work?
- How often during the course of a normal day do you experience a mood swing?
- How often have you felt betrayed, victimized or abandoned? Why do you think that happened?
- How well do you manage anger?
- How well do you manage being alone?
- How would you describe your sense of self-worth?
- Have you ever felt you were bad, or even evil?
- Have you had any problems with self-destructive or risky behavior?
- Have you ever thought of or tried to harm yourself or attempted suicide?
- Do you use alcohol or recreational drugs or misuse prescription drugs? If so, how often?
- How would you describe your childhood, including your relationship with your parents or caregivers?
- Were you physically or sexually abused or were you neglected as a child?
- Have any of your close relatives or caregivers been diagnosed with a mental health problem, such as a personality disorder?
- Have you been treated for any other mental health problems? If yes, what diagnoses were made, and what treatments were most effective?
- Are you currently being treated for any other medical conditions?
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Intervention for Borderline Personality Disorder
When someone you love has borderline personality disorder (BPD), their behavior and reactions may be unpredictable and may include emotional volatility, impulsivity, a fragile sense of self and difficulty in relationships.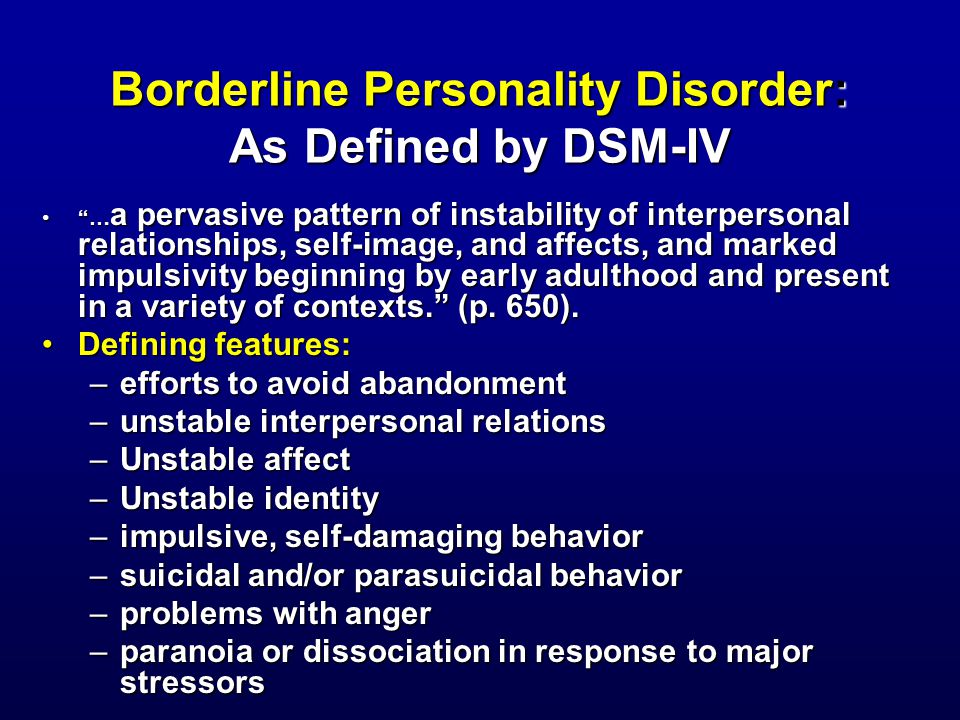 They have trouble managing their emotions and an intense fear of abandonment. Many people with BPD resort to suicidal threats or self-injury.
They have trouble managing their emotions and an intense fear of abandonment. Many people with BPD resort to suicidal threats or self-injury.
For those who care about a person with this condition, it can be difficult to avoid getting caught up in the displays of emotional intensity, inappropriate anger and self-sabotage. BPD is a serious form of mental illness, but it is treatable. Some people with personality disorders don’t recognize that their emotional reactions are quite a bit different than the experiences of most people. How can you support a loved one who has BPD?
For More Information About our Women’s BPD Treatment Center
Call (855) 409-0204 Now
Encouraging Your Loved One with BPD to Get Help
The symptoms of BPD can be intense and can interfere with not only the daily life of the person with the disorder but also the lives of those closest to them. When symptoms of BPD such as impulsivity, fear of abandonment and wide mood swings become apparent, it’s important for your loved one to get help from a mental health provider.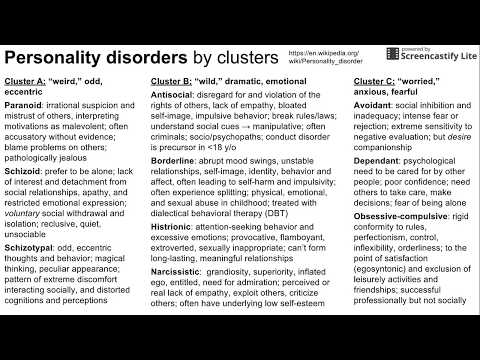
The more you learn about this disorder, the easier it will be for you to understand the behavior of a person with BPD. To be supportive of your loved one, try to avoid getting caught up in emotional conflict. Let them know they are loved and validate the thoughts and feelings they try to share with you. Be prepared that they may give you mixed messages such as hating you one minute and loving you the next.
It’s common for people with this condition to deny they have a problem and try to avoid getting help. They may consider a suggestion that you go together to family therapy or couples therapy. If they continue to refuse to get help, you may need to set boundaries in your relationship while continuing to encourage them to seek treatment from a mental health professional. Communicate to them the behavior you will not tolerate and encourage other family members to participate in trying to get the individual with BPD to get help.
Intervening in a Mental Health Crisis
There are times when a crisis escalates and an individual with BPD threatens suicide or self-harm.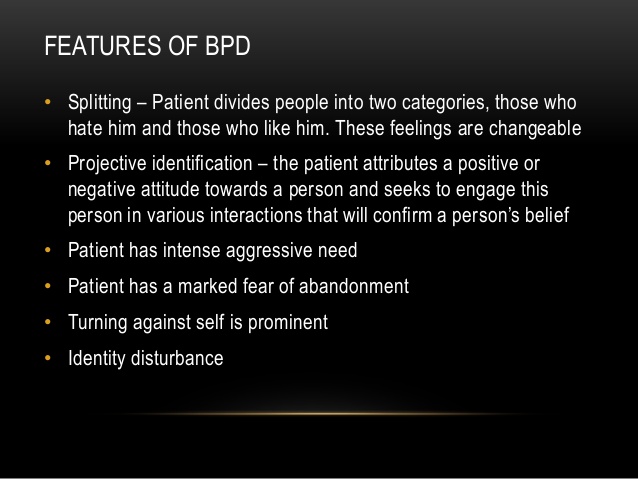 They may show subtle signs of self-harm such as scratching their skin, cutting off their hair, or avoiding others.
They may show subtle signs of self-harm such as scratching their skin, cutting off their hair, or avoiding others.
Threats of suicide should always be taken seriously, and your loved one shouldn’t be left alone if they’re threatening suicide. You may need to call 911 if you believe they’re in danger of harming themselves or if their behavior becomes violent. In some cases, you may be able to deescalate a crisis by talking calmly and encouraging them to accompany you to the emergency room or call a mental health professional.
Taking Care of Your Own Mental Health When Living with BPD
When you care for a person with BPD, it’s easy to get caught up in their actions and negative emotions, but whether or not your loved one agrees to get help, you’ll need to take care of yourself and your own mental health. If you’re dealing with one crisis after another, it can be tempting to isolate, but you’ll need the support of loved ones or a support group for family members of people with BPD to help you feel less overwhelmed.
Taking care of yourself includes getting enough sleep along with regular exercise and choosing healthy foods. Learn techniques to manage stress and practice staying calm in a crisis. Be as supportive as you can of your loved one, but also give yourself permission to participate in other activities you enjoy rather than making the person with BPD the complete focus of your life.
If you or a loved one are struggling with a borderline personality disorder or another mental health disorder, please contact us at (855) 409-0204 or submit the form below and a treatment specialist will contact you.
Borderline personality disorder: what it is, symptoms and signs of BPD
Borderline personality disorder is characterized by emotional instability, impulsive behavior and low self-control. Forbes Life figured out what causes this disease, how to diagnose borderline personality disorder and how to help people who have experienced it
Mental personality disorders differ from other types of disorders in their intensity.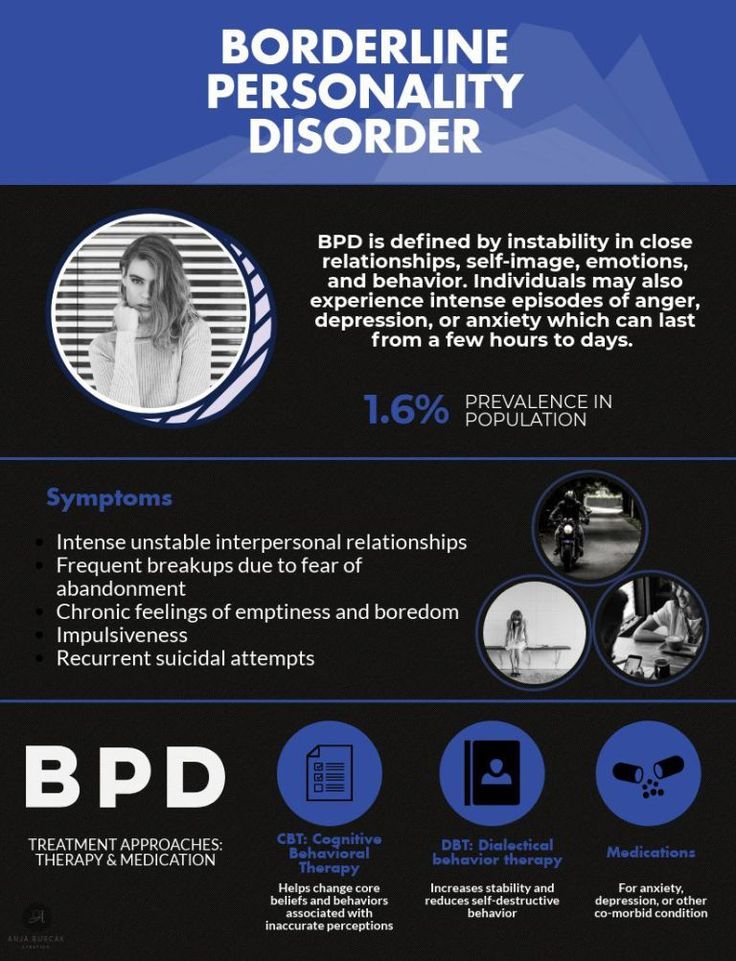 They cannot be treated like an ordinary illness, as a temporary mental disorder, because personality disorders affect a set of personal characteristics formed in childhood. There are a number of problems with diagnosing such diseases: their symptoms are quite individual, although there are a number of common signs. For borderline personality disorder (BPD), these may include difficulties with self-image, extreme mood swings, risky behavior, and self-harm. The good news is that personality disorders can still be managed—there is a cure.
They cannot be treated like an ordinary illness, as a temporary mental disorder, because personality disorders affect a set of personal characteristics formed in childhood. There are a number of problems with diagnosing such diseases: their symptoms are quite individual, although there are a number of common signs. For borderline personality disorder (BPD), these may include difficulties with self-image, extreme mood swings, risky behavior, and self-harm. The good news is that personality disorders can still be managed—there is a cure.
Now officially: BPD is a diagnosis
Borderline personality disorder is one of ten types of personality disorders in modern psychotherapy, which is expressed in problems of awareness and formation of personal identity. Psychologist, Gestalt therapist Valentin Oskin notes that this mental illness is associated with strong, uncontrollable and often painful emotions that lead to a distorted sense of self and unstable interpersonal relationships.
People with BPD are reverse solipsists: they are convinced of the inviolability of the surrounding world, but doubt the reality of their own existence - their image of the inner “I” is so mobile and unstable. In addition to depersonalization, "borderguards" are characterized by impulsiveness, dependence on other people, unstable behavior, a tendency to a chaotic life, and even a need to harm themselves and injure themselves. "Border guards" are characterized by chronic suicidality: 75% of people with BPD try to commit suicide, of which about 10% die as a result of suicide. Moreover, a third of all completed suicides were committed by those suffering from borderline personality disorder.
Despite the statistics, until 2022 the diagnosis of BPD in Russia could not be officially diagnosed - borderline personality disorder in psychiatry was defined as a disease only in foreign classifications of diseases. It was often called impulsive personality disorder or generally diagnosed as sluggish schizophrenia: the diseases are similar in symptoms, among the signs of BPD there are no hallucinations and delusions. BPD also resembles bipolar affective disorder (up to 40% of "border guards" get an erroneous diagnosis of bipolar disorder), only periods of depressive and elated mood are replaced with bipolar disorder less often. The transition to the International Classification of Diseases of the 11th revision will finally allow doctors to make an accurate diagnosis for Russian citizens and prescribe the appropriate treatment.
BPD also resembles bipolar affective disorder (up to 40% of "border guards" get an erroneous diagnosis of bipolar disorder), only periods of depressive and elated mood are replaced with bipolar disorder less often. The transition to the International Classification of Diseases of the 11th revision will finally allow doctors to make an accurate diagnosis for Russian citizens and prescribe the appropriate treatment.
Diagnosis is not a sentence, the boundary between the norm and pathology is very flexible: “Each of us has borderline responses. For some, they are deeply hidden and appear only in crises, traumas, stressful situations. And for some, life as such is stressful, and therefore the ways of responding turn into what psychologists could call the borderline organization of the personality,” notes Irina Mlodik, Candidate of Psychological Sciences, in the book “House of Cards. Psychotherapeutic assistance to clients with borderline disorders.
Related material
Ghost hints
Most people with BPD are unaware of their diagnosis and do not seek medical attention.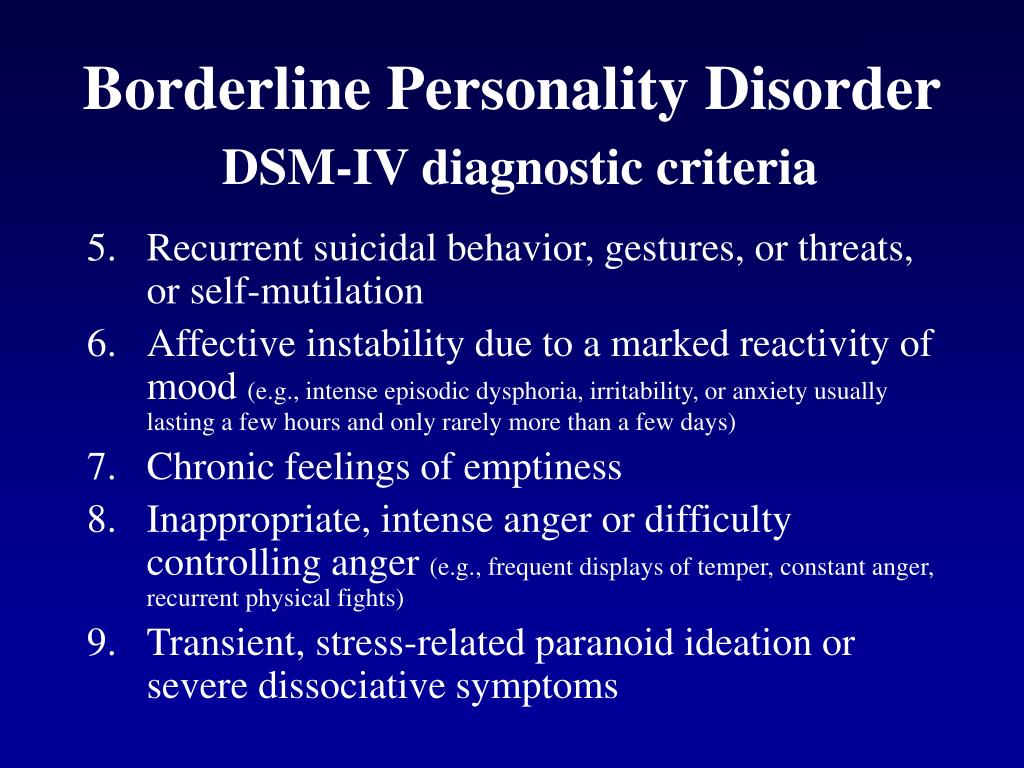 And it's not just that BPD in psychology does not have a clear definition. The disease does not allow you to objectively assess your mental state and understand that the indomitable monster inside is raging not because of the permanent retrograde Mercury and the fatal force of circumstances. The absence of obvious mental abnormalities like hallucinations makes it possible to attribute emotional behavior to character traits. Colleagues, friends and relatives often believe that behind the disgusting behavior of such a person is hysteria and selfishness. Therefore, systematic treatment of borderline personality disorder begins in most cases after a suicide attempt.
And it's not just that BPD in psychology does not have a clear definition. The disease does not allow you to objectively assess your mental state and understand that the indomitable monster inside is raging not because of the permanent retrograde Mercury and the fatal force of circumstances. The absence of obvious mental abnormalities like hallucinations makes it possible to attribute emotional behavior to character traits. Colleagues, friends and relatives often believe that behind the disgusting behavior of such a person is hysteria and selfishness. Therefore, systematic treatment of borderline personality disorder begins in most cases after a suicide attempt.
The most striking and obvious sign of borderline personality disorder is a craving for auto-aggression, or self-harm. This is not only the infliction of bodily harm (cuts, blows or burns), but also the intention to deprive oneself of sleep, nutrition. This practice is not necessarily a consequence of suicidal behavior: physical pain serves as a way to drown out inner pain, to switch attention from uncontrollable emotions to those that have become the result of an effort of will.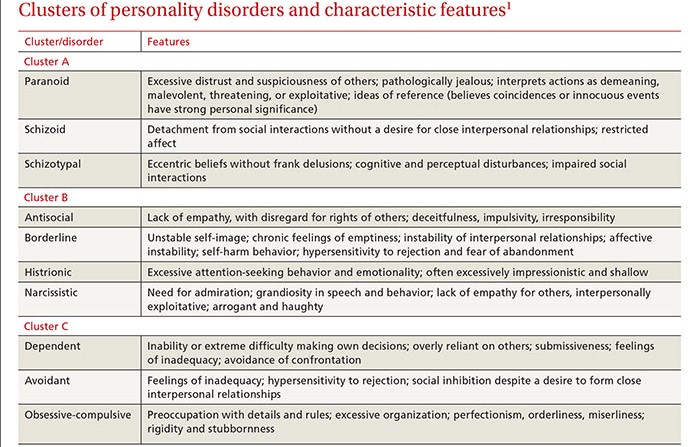 The problem is that self-harm is either carefully hidden by people with BPD because it is not normal in our culture, or they perceive it as controlled behavior (eg, exhausting workouts in the gym, striving to do work tasks in their free time).
The problem is that self-harm is either carefully hidden by people with BPD because it is not normal in our culture, or they perceive it as controlled behavior (eg, exhausting workouts in the gym, striving to do work tasks in their free time).
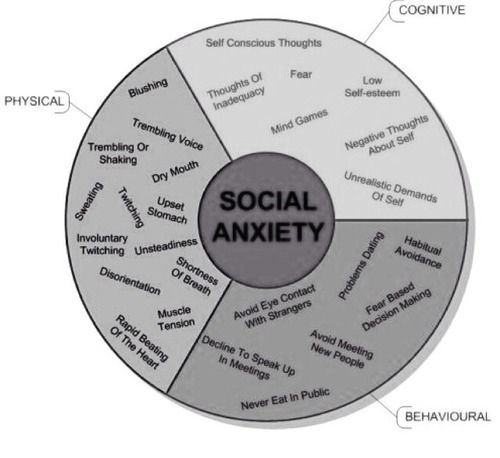
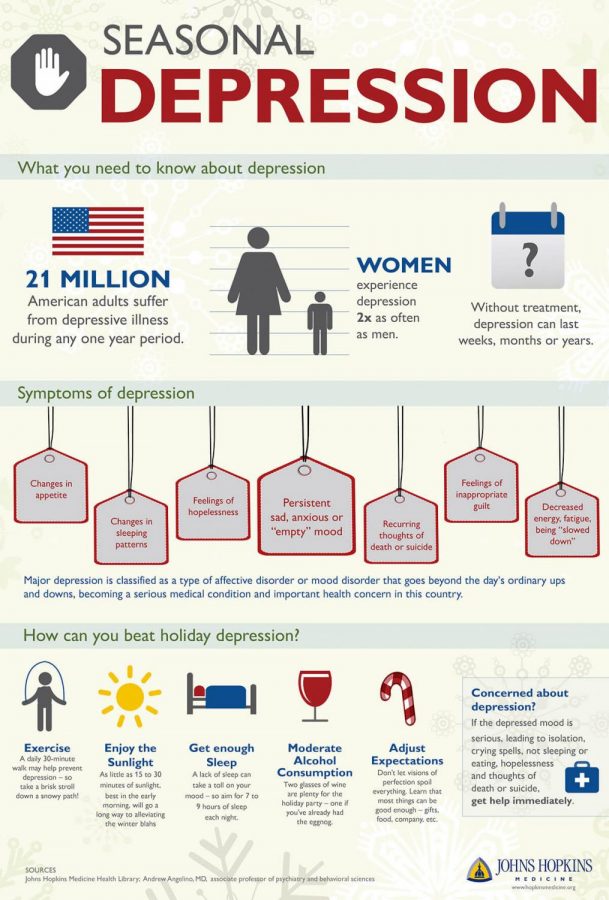
Borderline personality disorder may be accompanied by alcohol, drug, gambling and a number of other diseases. “For example, depression, anxiety disorders, eating disorders are common in people with BPD. Often, a history of PTSD or CPTSD is found, ”notes Valentin Oskin. That is, constant panic attacks or overeating in the evenings can be a sign of more serious mental disorders than just a reaction to stress.
Mind, a British mental health resource, highlights the following symptoms that may indicate borderline personality disorder. If they last long enough and have a negative impact on your life, it makes sense to consult a psychotherapist or psychiatrist:
- Fear of being alone.
 You constantly worry about people leaving you and are ready to do everything to prevent this from happening.
You constantly worry about people leaving you and are ready to do everything to prevent this from happening. - Impulsivity and affectivity. You are overcome by strong emotions that last from several hours to several days and can change quickly (for example, from feelings of happiness and confidence to sudden depression and sadness). This is especially evident in a state of anger, which is difficult to control. In a state of severe stress, you may also experience paranoia or dissociation (as if everything is not happening to you, but to someone else).
- Depersonalization. There is no clear idea of who you really are: the sense of self and behavior changes radically depending on where and with whom you are. As an option - a constant feeling of emptiness inside, boredom, misunderstanding of one's true desires and values.
- Communication problems. It is very difficult for you to create and maintain stable relationships, you are prone to masochistic communication, cyclically idealize and devalue even the closest people, and do not always correctly interpret the motives of the actions of others.
“Borderline personality disorder can manifest itself in a wide range of signs,” says Valentin Oskin, “the symptoms of borderline personality disorder are most fully described in the DSM-5 and ICD-11 reference books. If grouped together, the symptoms will reflect a lack of control in the emotional, behavioral, cognitive spheres, as well as a distortion of the sense of self and a violation of interpersonal relationships. According to the psychologist, it is extremely difficult for people with BPD to break off relationships, even those that need to be broken off. Instead, they may go to great lengths to keep the people who matter to them around them.
At the same time, “border guards” tend to involuntarily throw out their emotions on those who are dear to them: “Often this ends with an interruption in communication, because not everyone is able to endure such a bolt from the blue. And even more so if this thunder rumbles once every couple of months, ”Ksenia Ivanenko notes in her Telegram channel, where she describes her personal experience in dealing with BPD.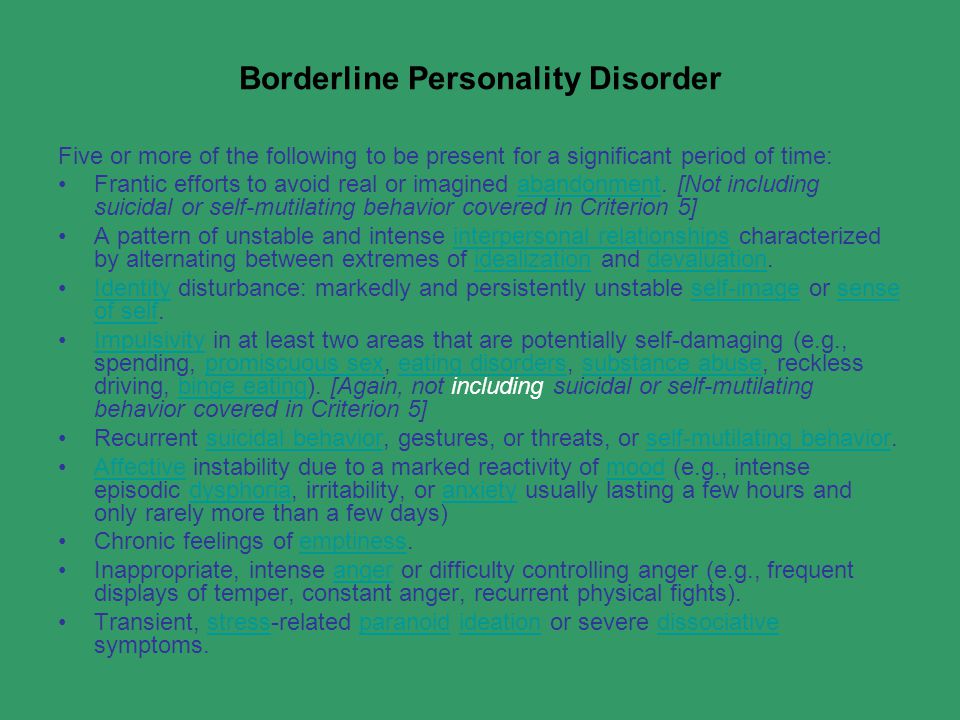
Related material
To determine if you are at risk, you can take several tests for borderline personality disorder that are publicly available. It is important to understand that the result obtained is not a final diagnosis, it can only be made by a qualified doctor after analyzing the symptoms.
The Root of the Problem: What Causes Borderline Personality Disorder
Effective treatment for most mental illnesses requires identifying the cause. Borderline personality disorder is problematic in that it arises from a number of factors and affects the basic components of the personality. That is, there is simply no specific reason that triggers the PRL processes. “While BPD is one of the most researched personality disorders, there is no consensus on what exactly causes it. Severe stresses experienced by children and adolescents, such as neglect, prolonged painful separation, loss of a parent, violence, are common in people with BPD. There is also evidence of a genetic predisposition: among first-line relatives of a person with borderline disorder, the likelihood of developing a similar disorder is 3-5 times higher when compared with the general population,” notes Valentin Oskin.
There is also evidence of a genetic predisposition: among first-line relatives of a person with borderline disorder, the likelihood of developing a similar disorder is 3-5 times higher when compared with the general population,” notes Valentin Oskin.
Any person can be at risk, especially if he is going through a difficult stressful situation. It is known that this diagnosis is made more often in women than in men, and that in almost all cases of BPD it is driven by a deep emotional shock. Most researchers agree that the development of BPD is promoted by a combination of two groups of factors:
- Stress and traumatic life situations. For example, sexual, physical or emotional abuse, persistent feelings of fear or abandonment in childhood, family problems, repressed feelings of anger, anxiety, and sadness. Stress or trauma in adulthood can trigger the onset of borderline personality disorder.
- Genetic predisposition and environmental influences.
 The disease can be inherited, but more often borderline occurs as a pattern of behavior unconsciously borrowed from parents or close people, reactions to external stimuli.
The disease can be inherited, but more often borderline occurs as a pattern of behavior unconsciously borrowed from parents or close people, reactions to external stimuli.
Related material
No reason to break ties
If there is a “border guard” in your environment, you can build constructive communication with him, although this will require a lot of effort. “It is important to understand that a person with borderline personality disorder takes criticism extremely hard, for him it sounds like rejection, which he is terribly afraid of. At the same time, emotional jumps do not allow him to get the desired intimacy. Relations with such a person are usually like a swing between the poles "I love you, don't leave me - I hate you, I'll leave you." It is important to understand that with borderline personality disorder it is impossible to consciously change your behavior, thinking, emotional reactions and response patterns to certain situations, ”says Valentin Oskin.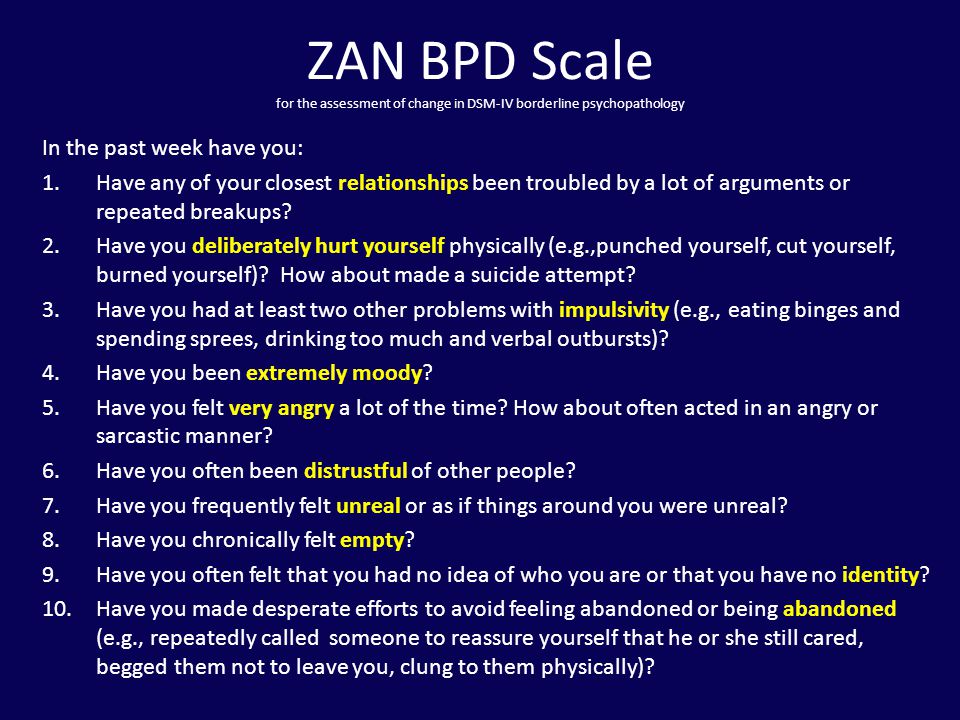
Many "border guards" live with a constant oppressive feeling of guilt, they feel broken, bad and unworthy of normal communication, which they badly need. They are unable to correctly read the reactions of others and the motives of their actions. This determines their strange behavior and repels potential partners and friends. Often, people with borderline personality disorder have a Favorite Person - a person on whom the "borderguard" is extremely dependent and who replaces not only everyone around him, but also himself. If this person is busy or there is a conflict with him, the “border guard” literally collapses the world: he drowns in a storm of emotions, reflects on death and looks for thousands of reasons why he was rejected.
There are a number of rules that psychologists have developed for those who seek to communicate as "border guards", minimizing chaos, conflicts and the possibility of a tragic denouement: could end in disaster.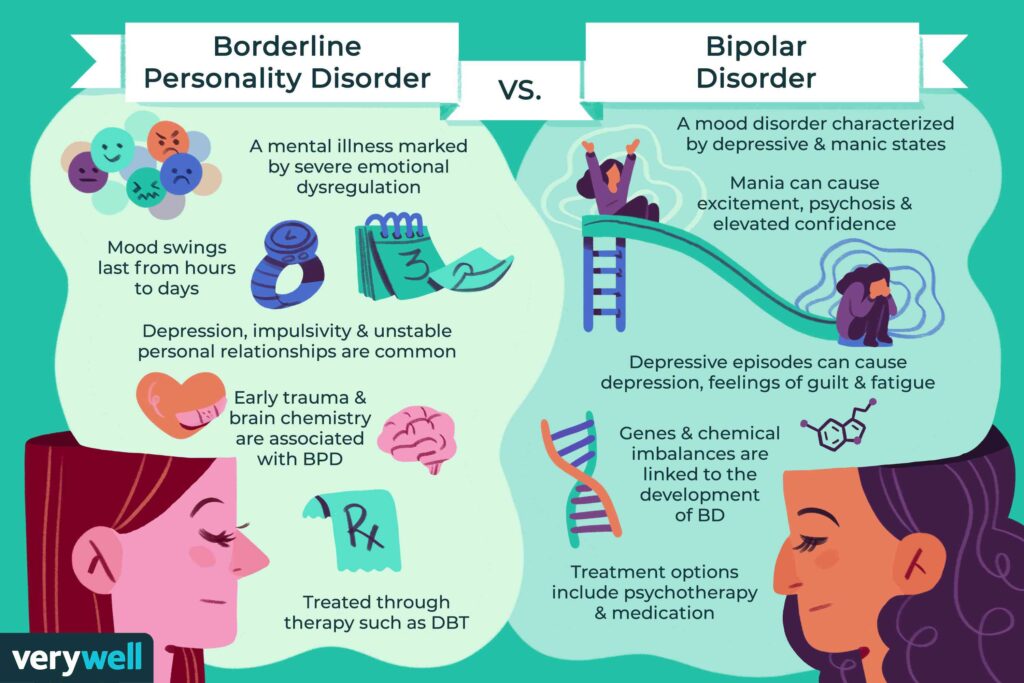
Related material
How to get rid of BPD
The main way to deal with borderline personality disorder is psychotherapy, in which work is done on the accompanying manifestations of an unstable mental state (depression, addictions, eating disorders, etc.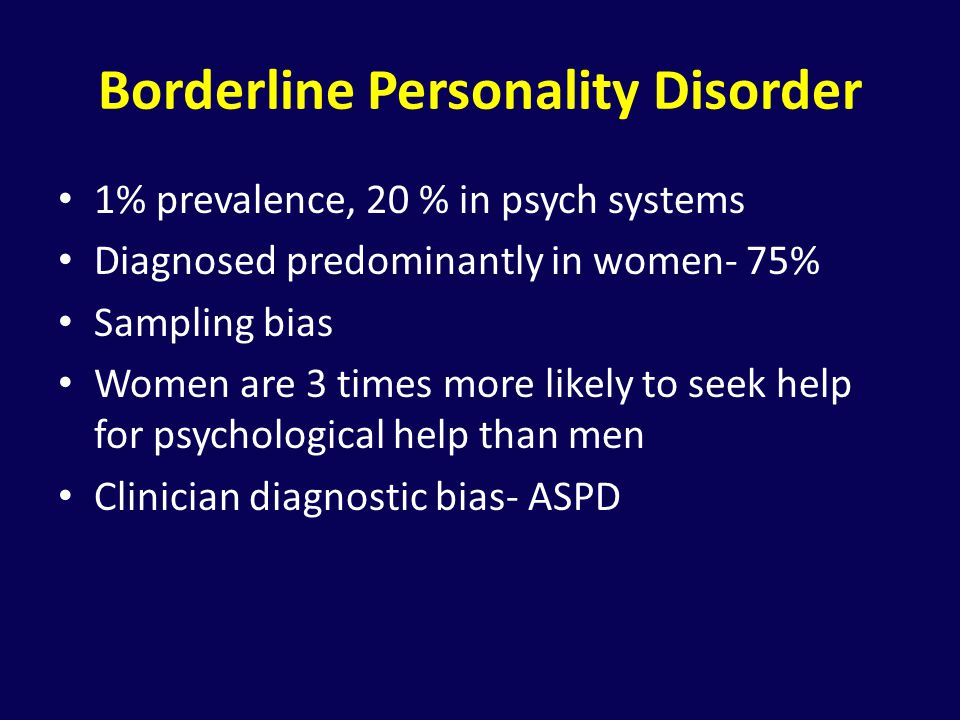 ) and syndromes (it is often necessary to treat alcohol withdrawal symptoms). syndrome). This is a long and complicated process, but statistics show that 70% of the “border guards” get rid of the main symptoms during therapy within six years, and remission occurs in a third of patients after two years.
) and syndromes (it is often necessary to treat alcohol withdrawal symptoms). syndrome). This is a long and complicated process, but statistics show that 70% of the “border guards” get rid of the main symptoms during therapy within six years, and remission occurs in a third of patients after two years.
“In therapy, people with BPD are primarily trained in emotional control, responsibility, and interpersonal skills. Dialectico-behavioral psychotherapy, a specially developed method for the treatment of BPD based on cognitive behavioral therapy, is well suited for this. No less effective is schema therapy, which also has special developments for the treatment of BPD. In the course of treatment, pharmacotherapy can also be prescribed, for example, for the treatment of associated depression or anxiety disorder, ”says Valentin Oskin.
Comprehensive treatment may include the following therapies:
- Dialectical Behavioral Therapy (DBT).
 Allows the "border guard" to realize that problems can be viewed from different angles, eliminates black and white thinking.
Allows the "border guard" to realize that problems can be viewed from different angles, eliminates black and white thinking. - Mentalization (MBT). It helps to explain to oneself the behavior of other people, logically argue their motives and work to improve interpersonal interaction.
- Transference Psychotherapy (TFP) teaches to perceive positive and negative qualities simultaneously, to get out of the "deification/devaluation" paradigm.
- Cognitive Behavioral Therapy helps to change the way of thinking, reactions to stress and correct affective patterns of behavior.
- Schematic therapy is a complex treatment based on psychoanalysis and gestalt therapy. It changes the behavioral patterns laid down in childhood or adolescence.
- Self help. It consists in tracking the dynamics of emotions, asking yourself questions like “how do I feel now?”, “What does he (a) specifically want from me?”, “Is this reality or my fiction?”.
To improve their inner state, people with BPD are advised to start meditating, exercising, walking more often in the fresh air, trying to rationalize their own mood swings, learning self-soothing techniques and training willpower in order to stop emotional breakdowns in time.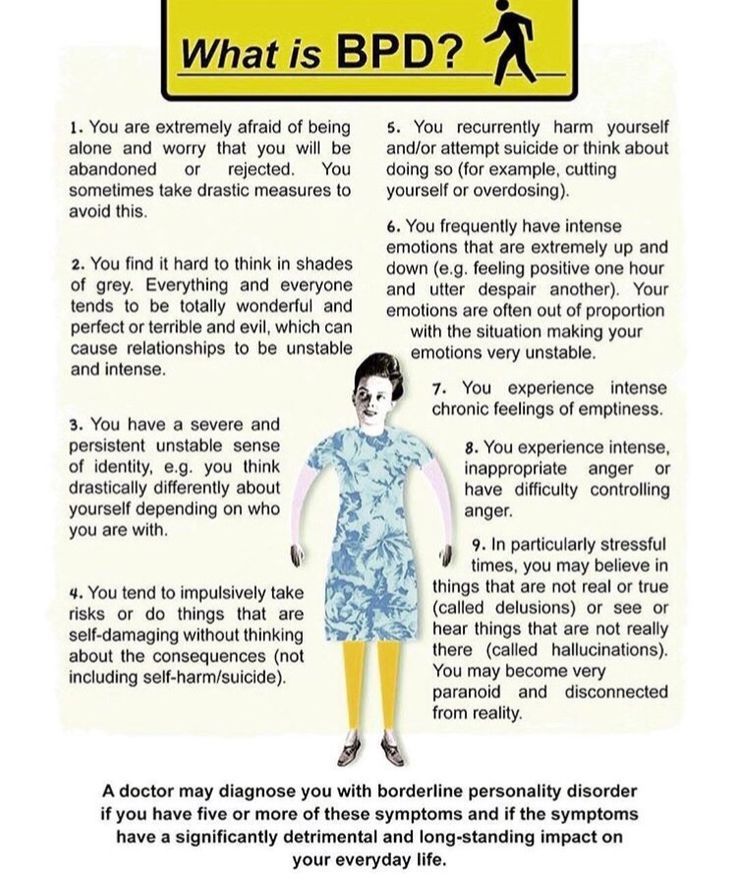
Related material
Borderline personality disorder
Olga Vladimirovna Plotnikova
psychiatrist
Borderline personality disorder (hereinafter referred to as BPD) is characterized by increased anxiety, emotional instability, and a tendency to impulsive actions. All these components greatly affect the quality of life. In addition, antisocial behavior, self-harm and an increased risk of suicide are common in borderline personality disorder.
Causes:
Genetics BPD has an evident hereditary factor. It would be more correct to say - predisposition. Like schizophrenia, BPD does not have a single gene that is responsible for the development of the disorder, but the influence of genetics is undeniable.
Neurophysiology or how does it work? Numerous neuroimaging studies (fMRI) have compared patients with BPD and healthy controls. Anomalies were found: a decrease in the level of serotonin, a decrease in the volume of the hippocampus, amygdala and other areas of the medial temporal lobe of the brain. The behavior of patients and their symptoms are a product of the special structure of their brain.
Anomalies were found: a decrease in the level of serotonin, a decrease in the volume of the hippocampus, amygdala and other areas of the medial temporal lobe of the brain. The behavior of patients and their symptoms are a product of the special structure of their brain.
Environmental influence There are a lot of myths here. And, despite the appearance of neuroimaging data, for some reason they are still alive. The most common myth is the influence of childhood trauma on the occurrence of BPD. Indeed, studies of people with BPD show that they have a history of domestic violence, but again, not everyone is without exception. A case of childhood trauma can only provoke and awaken a hereditary predisposition to BPD, but this is not the cause of its development. It's all about the structure of the brain.
Why is this important? When we talk about diabetes, we don't think that willpower can change insulin levels. BPD is not a whim and cannot be cured by “education”, you need to learn to live with it.
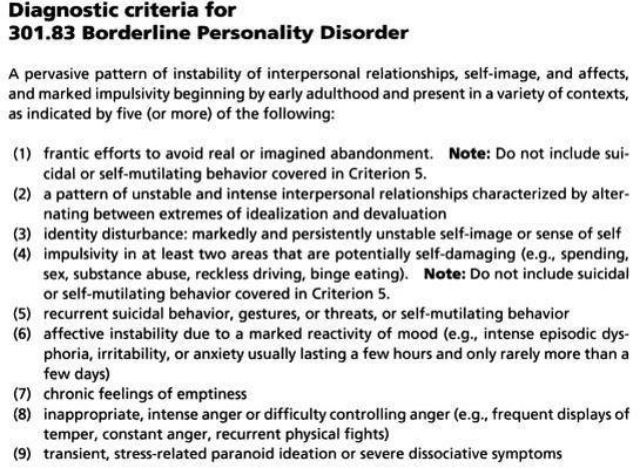
Diagnostic criteria for borderline personality disorder:
- Tendency to make excessive efforts to avoid the real or imagined fate of being abandoned.
- Tendency to engage in intense, tense, and unstable relationships characterized by alternating extremes of idealization and devaluation.
- Identity disorder: marked and persistent instability of the image or feeling of the self.
- Impulsivity in at least two areas that involve self-harm (eg, spending money, substance abuse, traffic violations, habitual overeating).
- Recurrent suicidal behavior, hints or threats of suicide, acts of self-harm.
- Affective instability, very changeable mood (for example, periods of intense irritability or anxiety, usually lasting from several hours to several days).
- Constantly experienced feeling of emptiness.
- Inappropriate manifestations of intense anger or difficulty in controlling anger (eg, frequent irritability.
- Paranoid ideas.
How to treat?
The first line is the psycho-education of the patient and his relatives. This is very important, as it helps to understand what is happening with the patient and outline the tactics of further actions.
Schema therapy patients learn how to respond to their symptoms and then control them.
Medications help manage the severity of symptoms and give strength to fight BPD.
Special considerations to consider when selecting therapy
-Second generation antipsychotics should be used in patients with thought disorder, paranoia, identity disorder.
- In patients with mood disorders, outbursts of aggression, mood stabilizers (normotimics) should be used, and not antidepressants.
SUMMARY:
BPD is an anomaly in the structure of the brain, and not a bad upbringing and a complex character.