Inpatient ocd treatment
Residential OCD Treatment – Rogers Behavioral Health
- We want to helpCall 800-767-4411 to request a free screening. Location numbers
- Overview
- Approach
- A Typical Day
- The Team
As part of the comprehensive range of services offered for OCD and anxiety at Rogers Behavioral Health, our 28-bed adult facility anchors our care for OCD. We offer one of the top residential treatment offerings in the world and one of only a handful specializing in OCD in the country.
Here patients benefit from the expertise of a highly trained and caring staff who partner with residents on a personalized plan of care that addresses each person's unique needs, in a setting which provides the comfort and support needed.
With an in-depth, longer-term level of care that averages 45 to 60 days, we work with patients on intensive and challenging treatment for:
- Obsessive-compulsive disorder (OCD)
- OC-spectrum disorders
- Generalized anxiety disorder
- Panic disorder
- Social anxiety disorder
- Trauma (posttraumatic stress disorder)
Led by an internationally recognized clinical psychologist who oversees cognitive behavioral therapy (CBT) at Rogers, we are a team of specialists who are passionate about helping people break free of OCD and related anxiety disorders. Our team provides care that’s proven to work and confirmed by more than a decade of outcomes studies.
Our treatment approach
At Rogers, we base our OCD treatment on a comprehensive, proven effective cognitive behavioral therapy-based approach. Our staff works one-on-one with patients to identify the specific thoughts and situations that create anxiety, and then develop a thorough exposure hierarchy together. Our graduated, manageable treatment approach empowers people to gain control over symptoms and learn effective strategies they can use throughout their life. CBT with an emphasis on exposure and response prevention (ERP) is the foundation of care, in addition to medication management overseen by a board-certified psychiatrist. These skills are gained through both individual and group therapy.
Our graduated, manageable treatment approach empowers people to gain control over symptoms and learn effective strategies they can use throughout their life. CBT with an emphasis on exposure and response prevention (ERP) is the foundation of care, in addition to medication management overseen by a board-certified psychiatrist. These skills are gained through both individual and group therapy.
Additional therapeutic support
Other elements within our care may include:
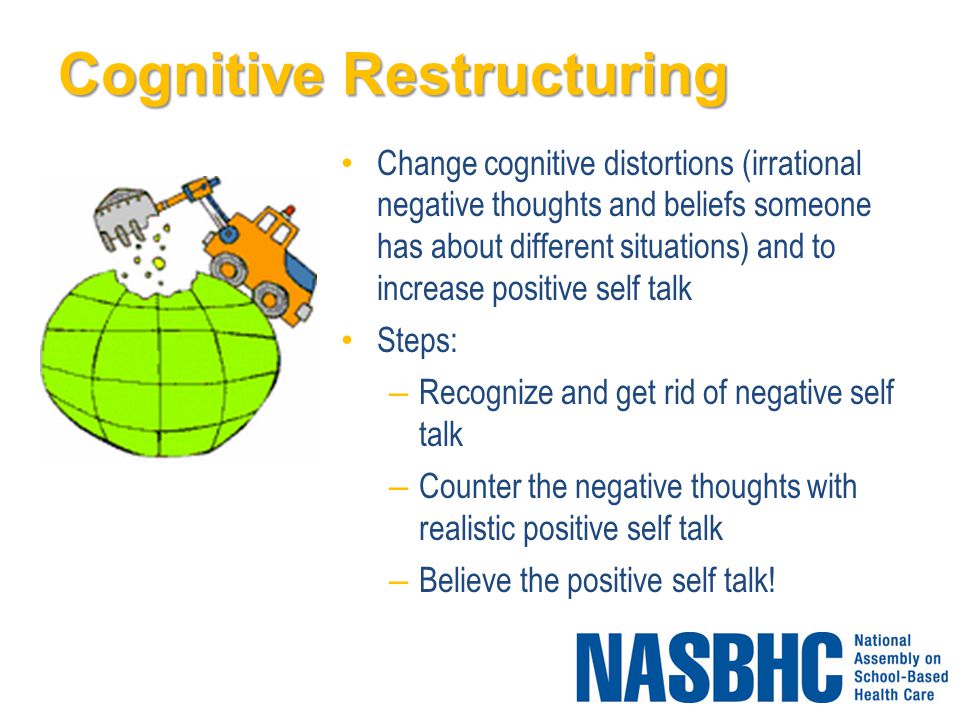
- Cognitive restructuring
- Experiential therapy (art, recreational)
- Personal wellness education
- Spiritual care
- Community meetings and outings
- Family therapy and education
At Rogers, we know it’s hard to change behaviors, and it takes time and effort to replace old thinking patterns and habits with healthier ones. The flexible length of stay allows patients to practice newly acquired skills. We also educate family members on these techniques so they can support a loved one after discharge.
After completing the program, a personal recovery plan for continuing care is created. When appropriate, patients are referred to lower levels of care at Rogers for continued treatment.
A diverse schedule of therapeutic activity helps keep one focused on gaining the skills and understanding to help you cope and manage their OCD and anxiety. The treatment includes structured programming seven days per week. Here’s what a typical weekday looks like:
| Morning | Afternoon | Evening |
|---|---|---|
| Vital/weights; medications | Lunch | Dinner |
| Breakfast | Cognitive restructuring |
Goal review group |
|
Exposure and response prevention |
Experiential therapy |
Supervised assignment work |
|
Supervised assignment work |
Daily living responsibilities or community integration activity |
In addition to the individual sessions with a psychiatrist and other treatment team members scheduled throughout the day and week, patients have access to residential care specialists 24 hours a day for support and help staying on track with their goals.
OCD and Anxiety Adult Residential Care Team
A comprehensive, multidisciplinary team works with residents throughout their stay. A licensed clinical psychologist who specializes in the treatment of OCD and anxiety oversees care, working with a highly trained team which may include:
- Internal medicine physician
- Board-certified psychiatrist
- Licensed clinical psychologist
- Behavioral specialists
- Master’s level therapist
- Registered nurse
- Experiential therapist
- Registered dietitian
- Residential care specialists
Upon admission, we administer an in-depth, detailed series of assessments, which includes the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS). We use this information to develop personalized exposure exercise and a graduated exposure hierarchy care plans.
OCD and Anxiety Adult Residential Care setting and tour
Nestled in the woods on a peninsula where Lower Nashotah and Upper Nemahbin lakes converge, our OCD and Anxiety adult residential care facility offers a quiet, secluded setting about a mile down the road from Rogers’ main Oconomowoc, Wisconsin, campus. The lodge-like facility is surrounded by therapeutic landscaping, walking trails, a gazebo, and an outdoor patio. Comfortable treatment and therapy areas, home-like community spaces, a dining hall and living areas with semi-private bedrooms create a supportive environment.
The lodge-like facility is surrounded by therapeutic landscaping, walking trails, a gazebo, and an outdoor patio. Comfortable treatment and therapy areas, home-like community spaces, a dining hall and living areas with semi-private bedrooms create a supportive environment.
CLICK ON THE IMAGES TO VIEW LARGER.
CRext2.jpg
CRext1.jpg
Solarium
Dining
Entry
Corridor
Group Room
Bedroom
Wondering if you could benefit from residential treatment?
Contact us to request a free confidential screening and learn more.
Call 800-767-4411
Free Screening
Denise's Story
Real people sharing what they have overcome and how Rogers helped through their process.
Hear Denise's joy in recovery with OCD ... Read More
Share your Rogers experience
Have you or a loved one spent time at Rogers? We’d like to hear about your experience with us. Share your story.
Call 800-767-4411 or go to rogersbh.org to request a free screening.
OCD Institute at McLean Hospital
Compassionate OCD care for children and adults. Call us today to talk to our admission staff about treatment options.
Obsessive compulsive disorder (OCD) is a debilitating illness consisting of unwanted thoughts and time-consuming rituals that can significantly limit a person’s ability to function in daily life.
In 1997, we opened our doors as the country’s first residential treatment program for this condition. Since then, the Obsessive Compulsive Disorder Institute (OCDI) has served as a leader in the advancement of clinical care and research for OCD and related disorders in children and adults. Our experts are ready to help you.
Our experts are ready to help you.
For more information or to make a referral, please call 877.203.3232 (adults) or 877.244.4476 (children).
Watch Now!
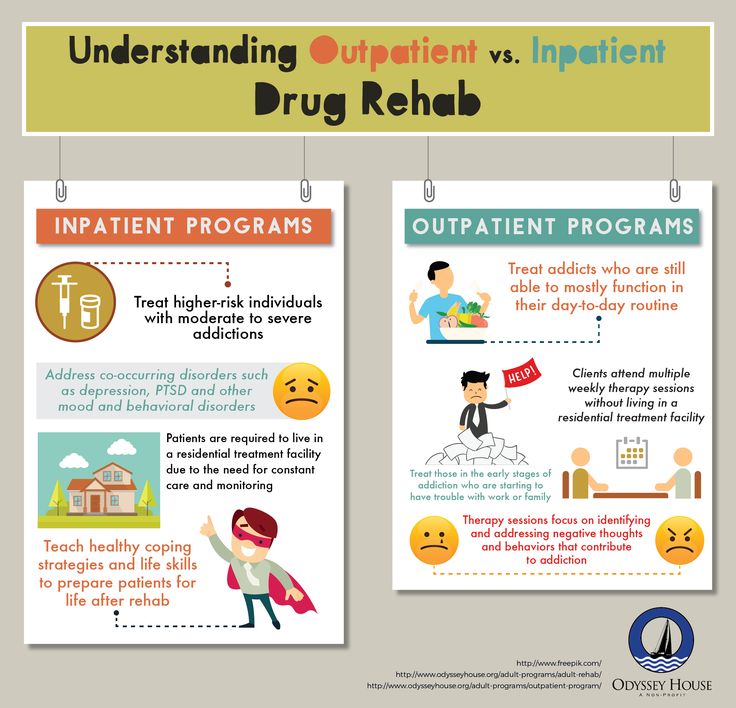
Our programs are ideal for individuals with moderate to severe or treatment-resistant OCD and its most common co-occurring disorders such as major depression and anxiety disorders.
Our adult program is most appropriate for individuals ages 18 and older. Our program for children and adolescents, OCDI Jr., is best suited for ages 10 to 18.
Adult residents’ average length of stay is between 30 and 90 days. At OCDI Jr., most commonly, youth stay for 2 months in residential care. The OCDI is covered by most health insurance providers, but self-pay is possible.
The OCDI is covered by most health insurance providers, but self-pay is possible.
We primarily use two methods to treat OCD. Exposure and response prevention (ERP) therapy allows individuals to gradually face their obsessional cues in order to build confidence with triggers and ultimately inhibit future compulsive responses.
Acceptance and commitment therapy (ACT) promotes a willingness to accept and address, rather than avoid, difficult thoughts and emotions and may reduce barriers to other forms of treatment. These treatment approaches are proven to help individuals struggling with OCD, anxiety, and related disorders.
“It was life-changing being at the OCDI. The staff, along with my parents, changed my life. I have an entirely different perception of my emotions and believe that the classes and groups will vastly reduce the re-occurrence of major depressive episodes.”– Patient treated at the OCDI
Educational services are also available for children and teens to help our young patients keep up with schoolwork during their time at the program.
The OCDI is located on McLean’s historic Belmont campus. The programs offer a pleasant and peaceful environment that is conducive to helping patients focus on their treatment.
Our expert staff specialize in OCD and related mental health disorders and are devoted to improving the quality of life of patients and their families. Our 24-hour care also includes available emergency psychiatric and medical personnel.
McLean OCDI Houston
Looking for OCD care or treatment options closer to home? This McLean-affiliated program offers cutting-edge treatment children and adults with OCD, anxiety, and related disorders.
About the Program
Treatment Approach
The Obsessive Compulsive Disorder Institute takes a robust approach to patient care. We use evidence-based models, family-focused therapy, and cutting-edge treatments.
We use evidence-based models, family-focused therapy, and cutting-edge treatments.
Staff focus on creating a customized treatment plan for each individual based on his or her specific symptoms, the severity of the symptoms, and other coexisting psychiatric diagnoses. We work in close partnership with patients and their families and emphasize patient self-motivation.
Treatment plans regularly include a combination of individual and group therapies, a variety of behavioral therapies, and medication that help patients manage their symptoms and transition back to their daily lives.
Our primary treatment is exposure and response prevention (ERP) therapy—a behavioral therapy that allows patients to engage directly with obsessional cues in a manner that builds confidence and competence with OCD triggers and ultimately leads to inhibition of future fear responses.
In order to customize the best program for each individual to help ensure success, we also incorporate other approaches, tools, and techniques that enhance motivation. These can include elements of dialectical behavior therapy (DBT) and acceptance and commitment therapy (ACT), two behavioral therapies that focus on thoughts and actions.
These can include elements of dialectical behavior therapy (DBT) and acceptance and commitment therapy (ACT), two behavioral therapies that focus on thoughts and actions.
Upon admission, each patient receives a diagnostic assessment and completes an array of objective measures. These assessments are administered by our OCDI Office of Clinical Assessment and Research.
We use the information to establish a treatment plan that incorporates the best therapies and strategies for addressing the patient’s symptoms, meeting challenges, and setting goals.
By establishing a critical baseline of symptoms, we can also track progress throughout the duration of treatment and even after patients have returned home. OCD takes many forms. Consistent reevaluation allows us to monitor our patients’ gains.
With permission from the patient, we make use of the data we collect clinically to answer important questions about OCD and how to best treat it.
Having a team devoted entirely to clinical assessment and research is invaluable, as it helps us better serve our patients and continually improve our program while we search for new and innovative ways to treat OCD.
Residents and partial hospital (day program) patients follow the same structured schedule, a combination of group, family, and individual therapy targeted at reducing the severity of the patient’s symptoms and providing the individual with tools to prevent relapse.
The schedule is designed to engage patients in their treatment. Each day is carefully planned with ample time for self-focus and group work and to maintain the important balance between work and leisure.
At the Intersection of Compassion and Innovation
Learn why McLean’s world-class approach to obsessive compulsive disorder treatment is considered a life changer for those with OCD
Each patient works with a behavioral therapist (a licensed psychologist or social worker) several times a week. The therapist develops a plan that serves as a guideline for staff to ensure quality and consistency in treatment. The plan identifies obsessions, compulsions, and avoidance behaviors, provides a menu of exposures for staff to implement, and recommends special instructions for each patient.
The therapist develops a plan that serves as a guideline for staff to ensure quality and consistency in treatment. The plan identifies obsessions, compulsions, and avoidance behaviors, provides a menu of exposures for staff to implement, and recommends special instructions for each patient.
Patients meet with a psychiatrist weekly, or more frequently if required, for medication management. The nursing and counseling staff are also certified in medication administration.
In general, group therapy focuses on helping patients become more open and willing to participate in treatment. Groups also include topics like decreasing behavioral symptoms; increasing normalized family, work, and social functioning; and improving access to education and support.
Through group therapy we teach skills in areas where people with OCD typically have deficits, including becoming more fully engaged in treatment by learning mindfulness, scheduling, social skills, and goal setting.
There are also a wide assortment of groups pertaining to specific symptoms that allow patients to learn key interventions for their individual diagnoses.
The specifics of the day’s schedule vary from day to day so that on a weekly basis group therapy covers a wide range of topics including mindfulness, motivation, cognitive behavior therapy, expressive therapies, and more. We also incorporate both didactic and skills-based groups, as well as activity therapies.
Research shows that expressive therapies such as music and art improve clinical and behavioral outcomes, reduce stress and anxiety, and give patients a better sense of well-being.
We offer a holistic balance of yoga and mindfulness as well as music and art therapy classes, run by a team of expressive therapists who specialize in mental health care.
As a component of treatment, we take our residents on community outings, such as outdoor recreation, movie theaters, shopping, and museums to practice newly acquired skills.
The OCDI leads the way in the advancement of clinical care, education, and research to help patients, families, and health care providers understand and more effectively treat OCD.
Our care for children and adolescents also extends to academics. Certified teachers who are extensively trained in mental health settings work with the children and teens’ local school districts for two hours of tailored instruction per day.
Through this service, we create a supportive learning environment in which children can continue their studies and earn school credit during their stay.
The priority of family therapy is to provide education about OCD that best supports the patient’s home life. This can mean working to stop accommodating behaviors, which are very common in the families of people with OCD.
Families also learn more helpful responses to a patient’s symptoms in the home environment. This close alliance and education of the family system significantly helps the patient transition back home successfully once treatment is over, and also helps to reduce the likelihood of relapse.
Each patient is assigned to one of the program’s independently licensed family therapists who facilitates weekly family sessions and works with the patient and family to create an aftercare plan.
It is the expectation that incoming adult patients identify at least one person in their life to engage in the treatment, be it a family member or a friend.
Parents and caregivers of OCDI Jr. patients are required to be active partners in treatment.
Therapists meet with parents to help them become coaches in their child’s treatment to assist with applying skills and the transition to home and school environments. Sessions are conducted over the phone with family or significant friends who don’t live in the area.
Toward the end of treatment, parents are invited to come and spend a week at OCDI Jr. to learn needed skills to help their children transition home and maintain the gains they have made.
Partial Hospital Program
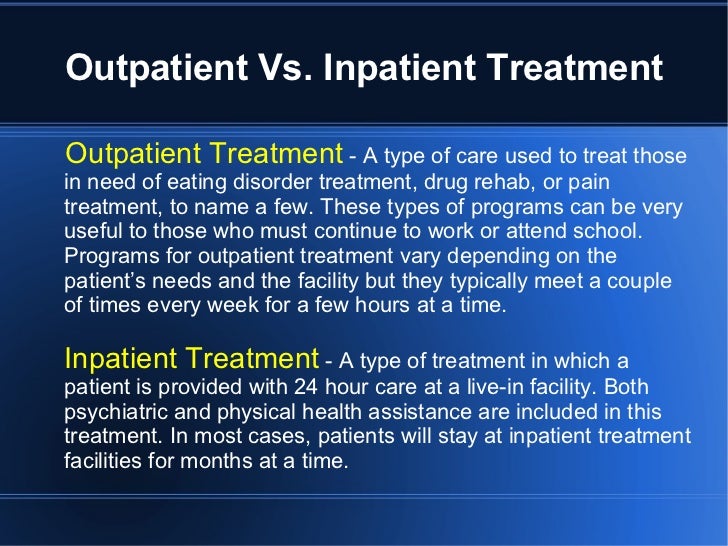
The OCDI offers a day (partial hospital) program for individuals who do not require 24-hour care yet need more structure than is available in outpatient treatment.
This level of care is appropriate for patients whose symptoms do not interfere with their ability to travel to the program and who are able to successfully manage their symptoms while at home.
Many of our adult partial hospital patients have completed our residential program and are in need of less intensive treatment.
At OCDI Jr., we use partial hospital care as a step-down at the end of residential treatment. This allows us to gradually transition patients and prepare them to leave the program. Parents are invited to attend the program for 1-4 weeks, depending on their child’s progress, to ensure adequate transitional care.
Patients within the partial hospital program attend the same structured schedule and individual and group therapy sessions as residents while spending their evenings at home practicing the skills they have learned during the day.
The emphasis of the day program is to provide a sufficient level of stability for the patient to be able to gradually leave treatment.
The partial hospital program operates daily, Monday through Friday.
Articles, Videos, and More
More About OCD
Everything You Need To Know About OCD
Patient Perspective: Reflections 20 Years After Seeking Treatment
Everything You Need To Know About OCD in Kids and Teens
Research
The OCDI research program aims to improve treatments for OCD and related conditions. Founded in 1997, the program was renamed the Office of Clinical Assessment and Research (OCAR) in 2013.
Founded in 1997, the program was renamed the Office of Clinical Assessment and Research (OCAR) in 2013.
The OCDI’s treatment program is a rich environment for informing clinical practice. Research is driven by the complex questions and practical issues faced in the daily effort to help patients overcome their OCD.
By design, OCAR includes a diverse staff of clinical researchers. The team examines OCD and its treatments using observation of patient behaviors and self-report data. They combine this with other factors, such as genetics, brain imaging, and biology.
The Office of Clinical Assessment and Research studies OCD to improve current and future patient careThe gold standard for treating OCD is exposure and response prevention (ERP) therapy. OCAR aims to improve the lives of current and future patients by advancing the science and practice of exposure therapy.
OCAR focuses on understanding why ERP works. They help tailor treatment to the individual by examining responses and their underlying processes in the brain and body. The team also evaluates innovative treatments and improvements to them. This includes tools such as acceptance and commitment therapy and computerized cognitive trainings.
The team also evaluates innovative treatments and improvements to them. This includes tools such as acceptance and commitment therapy and computerized cognitive trainings.
In addition, OCAR examines other areas to help improve OCD treatments and outcomes. Current research at the adult program includes studying sleep phases, family accommodations, identity status, and more.
As digital methods advance, OCAR is looking into the benefits of technology interventions and tools. The use of computer tests and data collection through devices like smartphones and fitness trackers may prove invaluable for both research and treatments.
At OCDI Jr., our clinician-researchers are examining family factors that influence treatment outcomes and exploring support systems for parents raising children with OCD.
Though patients at the OCDI may be asked to take part in OCAR research, participation is not required and does not affect access to care.
Learn more about the OCDI’s Office of Clinical Assessment and Research
Admission & Cost
Admission
The OCD Institute is suitable for children, teens, and adults ages 10 and older with moderate to severe or treatment-resistant OCD and its most common coexisting disorders. This includes major depression and anxiety disorders, such as social anxiety, specific phobias, panic attacks, and separation anxiety.
This includes major depression and anxiety disorders, such as social anxiety, specific phobias, panic attacks, and separation anxiety.
The OCDI is appropriate for those who could benefit from intensive residential or partial hospital (day program) care.
Our program may not be appropriate for individuals who have certain active co-occurring difficulties:
- Eating disorders: Individual must be medically stable and at a stable, healthy weight and
- Substance addictions: Individual must be sober for 3 months; If using alcohol or THC excessively, the individual must refrain prior to admission; drug/alcohol use, including medical marijuana, is not permitted while in program
- Suicidality and self-harm: Individuals are assessed on a case by case basis, but may require a period of stability prior to treatment if they are exhibiting suicidal or self-injuring behaviors
For further information about our program or to make a referral, please contact our admission staff:
Adults
Phone: 877. 203.3232
203.3232
Email: @email
Children and Adolescents
Phone: 877.244.4476
Email: @email
Cost
The OCDI is covered by most insurance providers. Self-pay is also accepted at OCDI Jr.
We understand that navigating the insurance system can be challenging, which is why we assist prospective patients to help determine eligibility. We welcome your questions and concerns and have a dedicated staff to help you.
McLean Hospital accepts Medicare, Massachusetts Medicaid, and many private insurance and managed care plans. More information on insurance providers accepted by McLean Hospital may be found on the Mass General Brigham website. You may also find it beneficial to review McLean’s patient billing and financial assistance information.
Treatment Team
Program Leadership
Staff and Associates
Working in close partnership with patients and families, our clinicians create and provide tailored treatment plans and high-quality care that meets each patient’s needs. Our expert clinical team includes board-certified psychiatrists, licensed psychologists and family therapists, registered nurses, certified teachers, and expressive therapists.
Our expert clinical team includes board-certified psychiatrists, licensed psychologists and family therapists, registered nurses, certified teachers, and expressive therapists.
Our clinicians have experience working with patients from diverse cultural and socioeconomic backgrounds from across the country and around the world.
Our staff members are trained in assessing and treating complex OCD and related conditions through exposure and response prevention (ERP) therapy and acceptance and commitment therapy (ACT).
All counselors receive specific training in working with patients who live with OCD and other anxiety disorders. They are also trained in general crisis prevention/intervention, CPR, and group leadership skills. Our team of well-trained and compassionate clinicians foster an environment to help our patients to succeed.
The OCDI operates within the Division of Depression and Anxiety Disorders, led by Chief Scientific Officer Kerry J. Ressler, MD, PhD. OCDI Jr. is also supported by the Simches Division of Child and Adolescent Psychiatry, led by Daniel P. Dickstein, MD, FAAP.
is also supported by the Simches Division of Child and Adolescent Psychiatry, led by Daniel P. Dickstein, MD, FAAP.
Accommodations
The adult residential and day program is located in East House, one of several historic buildings on McLean’s Belmont campus. The program offers a pleasant and peaceful environment that helps patients focus on their treatment.
For our residential patients, accommodations and amenities are designed to provide a home-like environment. This allows patients the chance to work on real-life challenges.
Our facilities offer comfortable bedrooms, a fully-equipped kitchen, common areas for groups, a laundry area, and access to a fitness facility with state-of-the-art equipment and certified staff.
The programs are located on and near McLean’s historic Belmont campusFor adults that desire luxury accommodations, our Lincoln Residence is located near the Belmont campus in Lincoln, Massachusetts.
This residence offers private rooms, full baths, catered meals, and a kitchen stocked with snacks and beverages. There is a tennis court and exercise room, health club membership, and transportation services to and from the OCDI.
There is a tennis court and exercise room, health club membership, and transportation services to and from the OCDI.
Please note that while treatment at the OCDI is covered by insurance, the Lincoln Residence is a self-pay option. Please inquire about this alternative living situation when contacting our admissions staff.
OCDI Jr. is also located at East House. At our dorm-like facility, we provide cutting-edge treatment delivered in a sensitive and nurturing manner. Amenities include wireless internet access, fitness and recreation, and comfortable, light-filled rooms.
Frequently Asked Questions
Where is the OCD Institute located?
The OCDI is located on McLean’s Belmont campus, in East House. For more information on directions, parking, and local accommodations, please visit our Maps & Directions page.
Who benefits most from the OCD Institute?
The OCDI focuses on treating adults and children who have not had adequate access to proper treatments for OCD and other severe anxiety disorders or who have tried outpatient treatment for OCD but found that they need more intensive treatment.
The program is ideal for individuals who are willing and motivated for treatment and are able to engage in a rigorous treatment program.
Is family involved in treatment?
Family and/or other supports are expected to be actively involved in treatment via weekly meetings and/or conference calls with our licensed family therapists. This allows families the chance to learn about OCD and how to best support their loved ones.
In addition, OCDI Jr. educates and coaches families to continue the work as the child transitions out of the program.
Is smoking permitted?
For adult residents, smoking is allowed in designated outdoor areas only. No smoking is allowed inside any of our buildings. OCDI Jr. is a smoke-free program and medical marijuana is not allowed.
When are visiting hours?
Adult residents may have visitors—around treatment expectations—until 10pm daily. Visitation takes place in common areas only.
Visitation takes place in common areas only.
Visiting hours at OCDI Jr. take place daily around dinner time, with extended hours during the evening and on weekends.
Are cell phones allowed?
Adult patients are allowed to have cell phones as long as they abide by program cell phone policies, including guidelines to prevent disruption of the program and other patients.
At OCDI Jr., tablets owned by McLean are available during admission as a means of video communication with family and to facilitate exposure treatment. Personal cell phones and tablets are not permitted while in the program. Portable music players (e.g., iPods) with no other functionality may be permitted.
Are academics offered?
While our first priority is treatment, we recognize the importance of education for our younger patients.
Certified teachers extensively trained in mental health settings work with the children and adolescents’ local school districts in order to provide two hours of tailored instruction per day. Through this service, we create a supportive learning environment in which children can continue their studies and earn school credit during their stay.
Through this service, we create a supportive learning environment in which children can continue their studies and earn school credit during their stay.
Is aftercare planning a part of the program?
The treatment team works closely with the individual as well as with family, significant friends, and outside providers to develop a personalized aftercare plan. Recommendations by staff are made based upon clinical needs, progress made during treatment, and long-term treatment goals.
Can former patients access their medical records?
All requests for medical records should be directed to McLean’s Health Information Management Department.
Are support groups offered?
To complement our programs’ services and encourage individuals’ initiatives in their own treatment course, many self-help groups are hosted by McLean.
Is research conducted?
Since the Obsessive Compulsive Disorder Institute (OCDI) opened its doors in 1997, research has played an integral role in helping to develop innovative treatment approaches to OCD.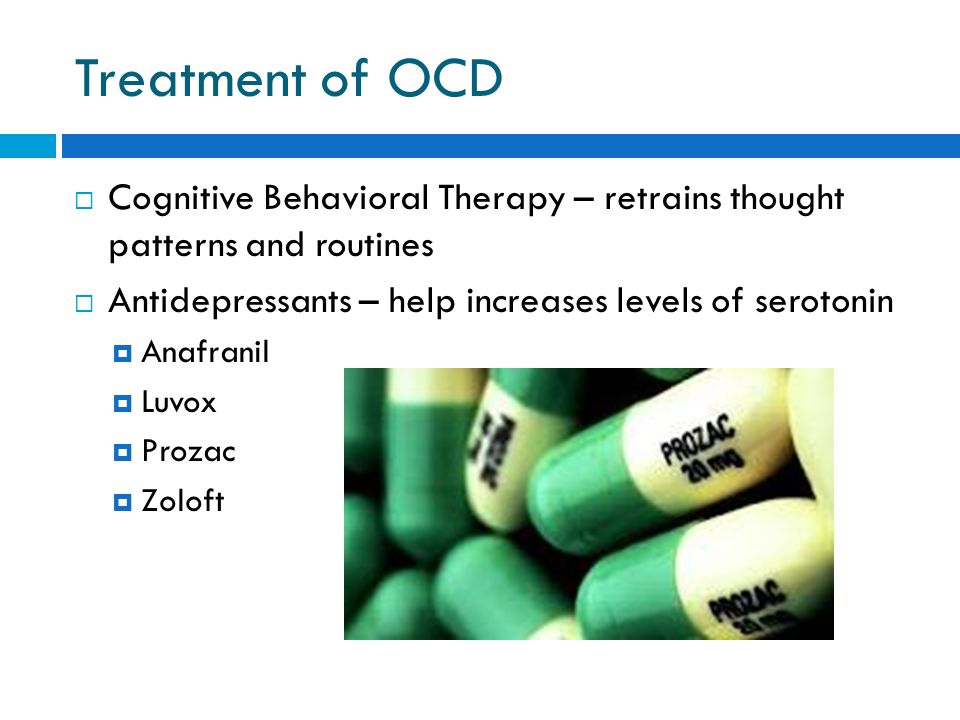 With permission, patients and families may be asked to participate in clinical research conducted by the OCDI Office of Clinical Assessment and Research.
With permission, patients and families may be asked to participate in clinical research conducted by the OCDI Office of Clinical Assessment and Research.
Does McLean gather patient feedback?
McLean is dedicated to maintaining high-quality and effective patient care. To ensure that those standards remain at the highest level, we use a number of feedback instruments and quality indicators.
Among these tools are the Perceptions of Care survey which monitors patient satisfaction and BASIS-24™, a psychiatric outcomes measurement tool created at McLean and widely used in the U.S. and around the world, which delivers feedback on the patient care experience.
McLean Is Here to Help
Let us help you find the OCD care that’s right for you or your loved one. Call us today to talk to our admission staff:
877.203.3232 (Adults) or 877.244.4476 (Children)
Topics
- OCD
- Anxiety
- Child & Adolescent
- Diane Davey
Not Found (#404)
hide menu
Issues of the current year
-
7-8 (136)
-
5-6 (135)
-
3-4 (134)
-
2 (133)
-
1 (132)
7-8 (136)
Issue content 7-8 (136), 2022
- nine0009
War Wikis: help in crisis situations
-
Ethical and legal problems of mental health: Ukraine at the focus of international respect
Yu.
 A. Kramar
A. Kramar -
Screening, diagnosis and treatment of diabetic sensorimotor polyneuropathy: consensus recommendations
-
Influx of mass information on delinquent behavior
R. І. Isakov
-
Stopping programs for rukhovo's rehabilitation for the normalization of the psychoemotional sphere of patients with Parkinson's disease
N.P. Voloshin, I.V. Bogdanova, I.K. Voloshin-Gaponov, S.V. Fedosiev, L.P. Tereshchenko, T.V. Bogdanova
-
Trauma management algorithm
-
Type of neuropathic pain according to the International classification of orofacial pain
-
Management of patients with dementia: key provisions for diagnosis, examination and observation for example of life
-
Significant Pre-Raphaelism: John Ruskin and Effi Gray
5-6 (135)
3-4 (134)
2 (133)
1 (132)
Other projects of the Health of Ukraine publishing house
Specialization medical portal
nine0009 Child doctorMedical aspects of women's health
Clinical Immunology, Allergology, Infectology
Rational pharmacotherapy
nine0000 OCD Treatment | Psychological help for obsessive-compulsive disorderSummary:
- Causes of illness
- Main symptoms of obsessive-compulsive disorder
- Misophobia
- Obsessive doubts
- Contrast obsessions
- Intrusive actions
- Drug treatment of obsessive-compulsive disorder
- Psychotherapy of obsessive-compulsive syndrome
- Licenses and certificates
- Photo clinic
- Our specialists
- Our promotions
Such a syndrome is observed infrequently, but according to experts, such statistics, as a rule, are due to the fact that most patients carefully hide the symptoms of obsessive-compulsive personality disorder. Many either do not go to the doctor at all, or begin treatment 7-10 years after the manifestation of signs of pathology. The disease is characterized by constant obsessive thoughts, images, ideas (they are called obsessions), obsessive movements and actions (compulsions). nine0004
Many either do not go to the doctor at all, or begin treatment 7-10 years after the manifestation of signs of pathology. The disease is characterized by constant obsessive thoughts, images, ideas (they are called obsessions), obsessive movements and actions (compulsions). nine0004
Doctors of the specialized medical center "Dependence 24" offer a comprehensive treatment for obsessive-compulsive disorder. The combination of drug therapy and an individually designed program of sessions with a psychologist allows you to achieve remission in more than 90% of cases.
Causes of illness
Although the exact etiology of obsessive-compulsive personality disorder is not fully understood, most doctors believe that the disease is caused by genetic factors (they suggest that the risk of inheritance is as high as 7-10%). nine0004
According to clinical studies, an important role in the development of pathology is played by:
- cerebral anomalies;
- neurological diseases;
- organic lesions of the brain (congenital abnormalities, trauma, surgery, stroke, etc.
 ).
).
Some doctors tend to psychoanalytic theory, considering the appearance of signs of obsessive-compulsive disorder as a consequence of the “turning on” of a psychological defense mechanism. Many patients with this diagnosis have suffered severe emotional trauma in childhood, which has led to a fear of punishment and an almost irresistible desire for isolation. As they grow older, these habits become fixed and take the form of a mental disorder. nine0004
Main symptoms of obsessive-compulsive disorder
The syndrome is characterized by repetitive thoughts and actions that are perceived by the patient himself as something alien and absurd. In addition to the will, obsessive ideas and images appear (at the initial stages of the disease, a person tries to resist them).
There are several clinical forms of obsessive-compulsive syndrome:
- mysophobia:
- obsessive doubts;
- contrast obsessions; nine0011
- obsessive actions.
Mysophobia
Accompanied by obsessive ideas of soil pollution, physiological secretions, fear of infection with a viral or bacterial infection, ingestion of poisons or any foreign elements (needles, fragments, etc.). Outwardly, a similar form of obsessive-compulsive disorder is manifested by a pathological tendency to cleanliness.
A distinctive symptom is the almost constant washing of hands, and sometimes it even comes to damage to the skin. The manic desire for cleanliness in the house is also typical: a person can wash already clean clothes and linen several times a day, clean, and again and again treat door handles, countertops, etc. with disinfectant solutions. nine0004
Libido gradually decreases, apathy and general dissatisfaction with one's life increase. When examining a patient, doctors pay attention to skin irritation caused by too frequent use of toxic antiseptics. Possible diseases of the respiratory tract due to inhalation of toxic fumes of chlorine and other disinfectants.
Possible diseases of the respiratory tract due to inhalation of toxic fumes of chlorine and other disinfectants.
Obsessive doubts
The patient is tormented by constant thoughts about the correctness of the actions taken (this condition is usually called retrospective anxiety). The patient thinks all the time about what he could not do or do wrong. This type of obsessive-compulsive syndrome is characterized by uncertainty about the correctness of the actions performed and the desire to act in a completely opposite direction. nine0004
For example, a person can go on vacation to the sea, and then constantly think that it was worth staying at home or choosing another vacation option. Any exit to the street is accompanied by compulsive checks to see if the water, electrical appliances, etc. are turned off.
Patients with this form of obsessive-compulsive disorder are pedantic, carefully perform any daily work, obsessively keep order - every thing should be in a strictly designated place. With the progression of the disease, there may be a tendency to accumulate various, unnecessary items, broken household appliances, papers - the patient is sure that this will definitely come in handy. nine0004
With the progression of the disease, there may be a tendency to accumulate various, unnecessary items, broken household appliances, papers - the patient is sure that this will definitely come in handy. nine0004
Contrast obsessions
This subtype of obsessive-compulsive disorder is manifested by intrusive thoughts, fear of losing self-control and harming oneself and/or loved ones. Panic attacks are typical, accompanied by severe somatovegetative symptoms (sweating, redness of the skin, shortness of breath, tachycardia). Constant anxiety leads the patient to do his best to prevent possible suicide or aggression against family members.
He removes piercing and cutting objects from the house (stationery and kitchen knives, needles, etc.), ropes - everything that can be used for suicide or crime. The patient tries to leave the house less often. In severe cases, there is confidence that the act of violence has already occurred, and the person is constantly looking for traces of blood, scraps of clothing and other "evidence". nine0004
nine0004
Intrusive actions
For the syndrome, compulsive actions are typical - constantly repeating the same type of movements (turning off / on the light, opening / closing doors, etc.). The patient performs them until there is a feeling that the action is performed exactly as needed. So-called "rituals" are possible - a special form of behavior, often associated with phobias (for example, with mysophobia, the patient clearly builds an algorithm of actions for disinfecting the house).
Drug treatment of obsessive-compulsive disorder
Therapy is indicated in cases where the disease has a significant impact on the patient's daily life, his communication in society. The following drugs are prescribed for treatment:
- anxiolytics (adaptol, pregabalin): they are preferred for severe anxiety, panic attacks
- benzodiazepines (diazepam, alprazolam): treatment is carried out with a short course to relieve acute symptoms; nine0011
- neuroleptics: drugs of this group are necessary for pronounced compulsive movements, psychomotor agitation;
- antidepressants.

Psychotherapy of obsessive-compulsive syndrome
As a rule, drug treatment brings only a short-term effect. Therefore, the doctors of the Addiction 24 clinic pay great attention to psychotherapy. Psychological consultations are necessary to relieve anxiety, correct behavior. The specific method of treatment is selected depending on the clinical picture. nine0004
For example, with the predominance of phobic symptoms, preference is given to behavioral therapy, relaxation techniques, and Ericksonian hypnosis is practiced. A good effect is given by rational psychotherapy, aimed at understanding and awareness by the patient of his own illness, the need to take medications prescribed by the doctor. After achieving remission, supportive and family psychotherapy is indicated.
Our consultants will talk in detail about the treatment of obsessive-compulsive personality disorder. Call us around the clock at 8 (495) 182-66-66.
Call us around the clock at 8 (495) 182-66-66.
You may also be interested
Need help? Call us!
8 (495) 182-66-66
90% of addicts do not admit that they are sick
- Our clinical psychologists will convince the patient of the need for treatment
- In case of treatment in the clinic - consultation of a narcologist - psychiatrist free of charge + annual service nine0008 We transport the patient to the hospital if necessary
Licenses and certificates
(to enlarge any image just click on it)
Photo clinic
Our specialists
Kazantsev Alexey Vladimirovich
Experience: 30 years
Head physician of the clinic, psychiatrist-narcologist of the highest category, psychotherapist
Portnov Alexander Sergeevich
Experience: 22 years
Psychiatrist-narcologist
Brynzar Konstantin Sergeevich
Experience: 6 years
Psychiatrist-narcologist
All specialists
Expert opinion
Gamaev Anton Evgenievich
Resuscitator-anaesthesiologist
Work experience 30 years
As a narcologist with many years of experience, I want to note the seriousness of the problem of beer alcoholism. The risk of developing dependence on beer is no less than on strong alcohol. With the systematic use of beer, the body adapts to the toxic effect and begins to require larger portions for pleasure. The disease develops gradually, so the addict himself does not notice the changes and does not consider himself an alcoholic. We know how to help you, how to cope with beer alcoholism. Therapy in our clinic is possible in a hospital or at home, with a guarantee of anonymity. nine0004
The risk of developing dependence on beer is no less than on strong alcohol. With the systematic use of beer, the body adapts to the toxic effect and begins to require larger portions for pleasure. The disease develops gradually, so the addict himself does not notice the changes and does not consider himself an alcoholic. We know how to help you, how to cope with beer alcoholism. Therapy in our clinic is possible in a hospital or at home, with a guarantee of anonymity. nine0004
Aleksey Vladimirovich Kazantsev
Head physician of the clinic, psychiatrist-narcologist of the highest category, psychotherapist
Work experience 30 years
I want to address the relatives of patients undergoing treatment for alcoholism at home. Do not need self-activity. Trying to "strengthen" the therapeutic effect, family members often use folk remedies that allegedly relieve cravings for alcohol. The effectiveness of non-traditional methods is not confirmed by medical research. The safety of the interaction of decoctions and tinctures with medicines has not been proven. An incorrect combination can cause severe intoxication, confusion, and an allergic reaction. Outpatient treatment of alcoholism in our clinic does not need an imaginary reinforcement of folk recipes. We conduct patients according to a personal program, making every effort for a successful result. nine0004
An incorrect combination can cause severe intoxication, confusion, and an allergic reaction. Outpatient treatment of alcoholism in our clinic does not need an imaginary reinforcement of folk recipes. We conduct patients according to a personal program, making every effort for a successful result. nine0004
Portnov Alexander Sergeevich
Psychiatrist-narcologist
Work experience 22 years
Based on professional experience, I believe that one of the reasons for the breakdown after coding is the patient's deliberately false consent. Agreeing under pressure from relatives, a person does not understand and does not accept his illness, and therefore sooner or later returns to his former way of life. To avoid relapse, the duration of the encoding must be used to motivate treatment. The main thing is to convince them to ask for help. We will help you deal with addiction. Our psychotherapy sessions will help you strengthen your sobriety mindset and get sincere consent to a full course of treatment for alcoholism.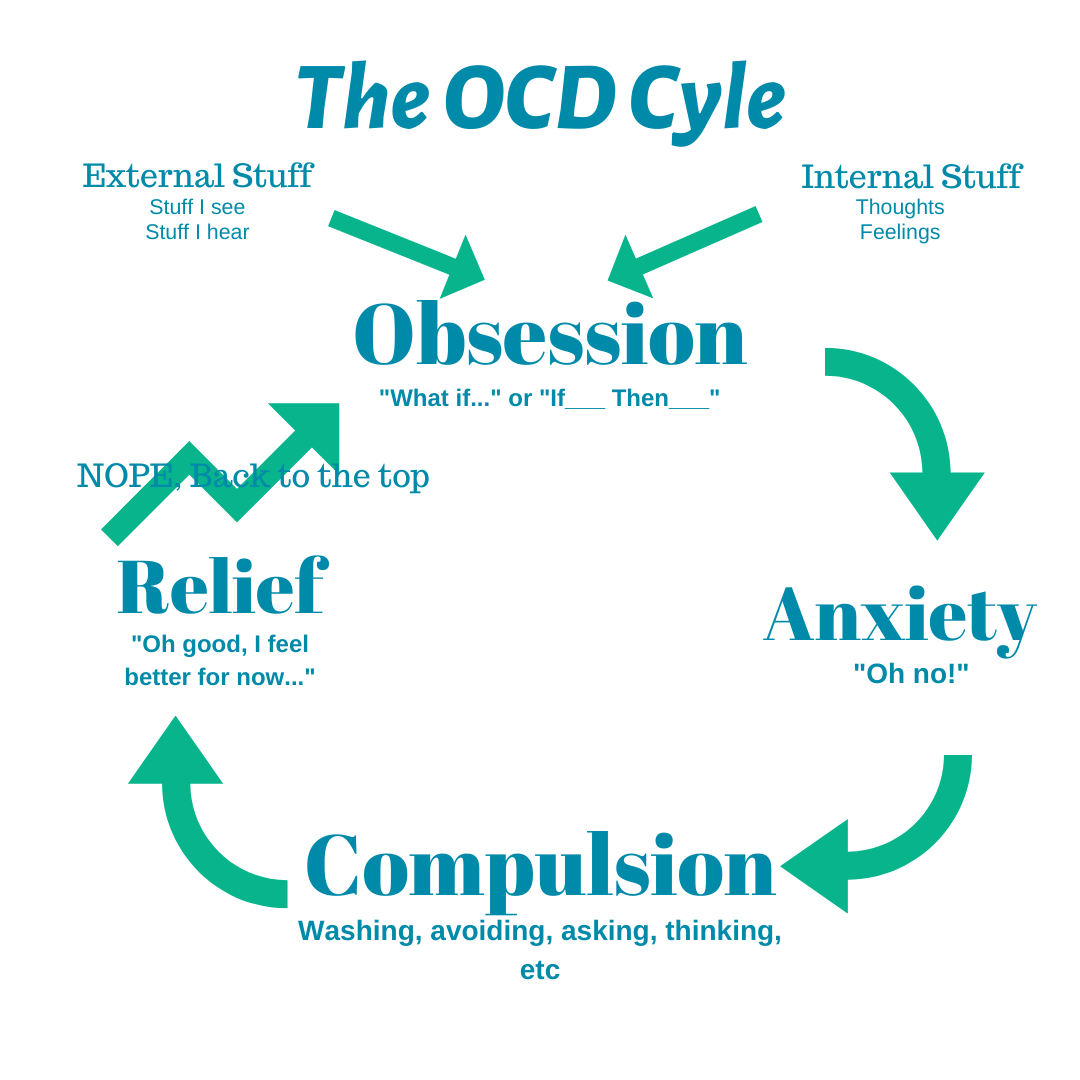 nine0004
nine0004
Zhanna Viktorovna Makhobey
I would like to draw attention to the problem of female alcoholism. The weaker sex is more prone to psychological dependence on alcohol due to vegetative lability, emotional instability, and increased sensitivity to traumatic events. At the same time, it is more difficult for a woman to admit dependence and trust a doctor. Therefore, the problem requires a delicate approach to the solution. Patients of our clinic can count on understanding and support. We will keep treatment confidential from the employer, colleagues, friends and relatives. nine0004
Zdanovich Aleksey Anatolyevich
As a family psychologist, I want to remind you that alcoholism is not a problem of an individual, but of the whole family. Life with an alcoholic person turns into a nightmare for his loved ones. The illness of one family member leads to co-dependence of relatives, destroys fundamental family foundations and values. A chance to change the situation is given by family psychotherapy and family counseling.