How to tell if antidepressants are working
Is My Depression Medication Working?
How long does it take for an antidepressant to work?
It can take two to three months for the full benefits of an antidepressant to kick in.1 But usually, people start feeling better one to two weeks after they start taking an antidepressant, explains Michael McGee, MD, psychiatrist and Distinguished Life Fellow of the American Psychiatric Association.
“Rarely, it can take up to eight weeks,” he says. “But typically, if the antidepressant is going to work, it starts working in about two weeks.”
If the person feels little or no improvement after several weeks, the doctor may change the dose of the antidepressant or possibly add or substitute another one. It’s important to let the doctor know if a medication is not working or if side effects occur. 1
How do antidepressant drugs work?
It’s thought that depression is caused by an imbalance of certain chemical messengers, known as neurotransmitters, in the brain. The brain’s nerve cells rely on various chemicals to pass on signals. If there is an imbalance, then the signals aren’t passed along the nerves the way they are supposed to. The role of antidepressants is to increase the availability of these chemicals in the brain. 2,3
“Antidepressants change the levels of the neurotransmitter levels in the brain,” Dr. Michael McGee says. A group of antidepressants known as selective serotonin reuptake inhibitors (SSRIs) work by increasing the levels of serotonin, a neurotransmitter, in the brain. When someone takes an SSRI, there is more serotonin available.1
“Serotonin tends to be more calming than some neurotransmitters, but they all interact with one another,” Dr. McGee says.
In terms of how they make a person feel, antidepressants may have a number of positive effects.
“The person taking the antidepressant has increased energy and is calmer,” Dr. McGee says. “They have improved motivation and their sleep and appetite are better regulated. And antidepressants may promote better brain functioning.”
And antidepressants may promote better brain functioning.”
How do I know if my antidepressant works?
When you start taking an antidepressant, you should begin to function better in your daily life before you start feeling better, says Dr. Michael McGee. In other words, you should begin sleeping better, eating better, and having more energy. “Then you should start feeling better,” he says.
Don’t expect to feel sedated, however. Antidepressants are not sedatives or tranquilizers, nor are they “uppers.” And antidepressants are not habit-forming.1
What should I do while I wait for the antidepressant to work?
There are steps you can take to feel better while you are waiting for the antidepressant to start working. If possible, try to stick to a routine, Dr. Michael McGee says.
“Our bodies like routine and it is stressful for the body to change routines,” he says.
It’s not always easy, but try to get up and go to bed around the same times each day. Get some exercise every day, and try to eat a Mediterranean-style diet that is rich in fruits, vegetables, olive oil, beans and legumes, and whole grains, he says.
Get some exercise every day, and try to eat a Mediterranean-style diet that is rich in fruits, vegetables, olive oil, beans and legumes, and whole grains, he says.
And try to get a good night’s sleep. At night, avoid blue light close to bedtime (that means cut down on screen time!) and engage in calm, restful things to do for an hour before bedtime, Dr. McGee advises.
12 Signs Your Antidepressant Isn’t Working
For many people, finding the right depression treatment is a trial-and-error process. An antidepressant may work well for one person but not at all for someone else — and experts don’t yet have ways to predict this.
In other cases, a person may start to feel better on an antidepressant, but the side effects are too bothersome for them to keep taking it.
A review published in February 2018 in the Lancet assessed previous studies of 21 antidepressant medications and concluded that although these drugs are an effective treatment for depression, some work better than others, and some are better tolerated by the body than others.
One way to improve your chances of finding the depression medication that works best for you is to look for the following signs that your antidepressant isn’t working well enough or is no longer working the way it should.
6 Depression Symptoms You Shouldn't Ignore
1. You Feel Better Right Away, but It Doesn’t LastExactly how antidepressants work is still a mystery. The effects are thought to be related to changes in neurochemicals in your brain, such as serotonin, dopamine, and norepinephrine — changes that usually take 2 to 12 weeks to set in, with a peak at 6 to 8 weeks. So, if you feel different immediately after starting a depression treatment, it could be a placebo effect, says the board-certified psychiatrist Joseph Hullett, MD, the senior medical director of OptumHealth Behavioral Solutions in Minnesota.
Sometimes that placebo effect wears off, and the actual effect of the antidepressant kicks in. Other times, the placebo just wears off, and the intended effects of the antidepressant are never felt.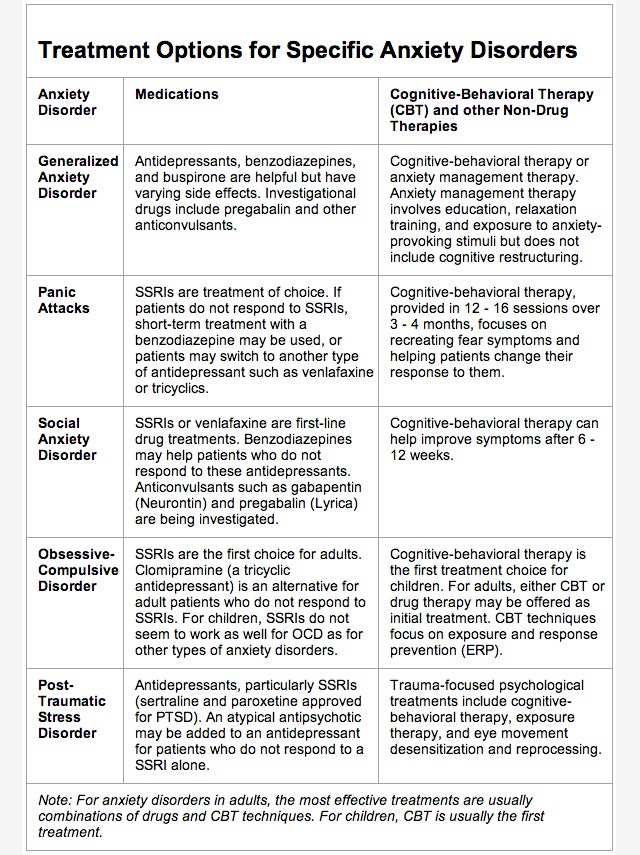 In this second case, it isn’t that the medication stopped working — it’s that the medication (beyond the placebo effect) just didn’t work for you in the first place.
In this second case, it isn’t that the medication stopped working — it’s that the medication (beyond the placebo effect) just didn’t work for you in the first place.
RELATED: 12 Surprising Facts About Depression
2. You Skipped a Dose — or SeveralIt’s a common situation — busy people often miss doses or take their medication at irregular intervals. The trouble is, not taking an antidepressant medication consistently can prevent it from working as well as it should — or prevent it from working at all, Dr. Hullett cautions. This can cause people to abandon what otherwise might be a very effective treatment.
3. You Can’t Sleep Well“Antidepressants can make you feel more sleepy, less sleepy, and affect your libido and sex life, which can affect your sleep,” says Karen Lim, MD, a double board-certified psychiatrist in general and child and adolescent psychiatry at Prairie Health, a telepsychiatry platform based in California.
“Some people are also surprised to know that antidepressants can cause vivid dreams, myoclonus (sudden jerking of limbs especially at night and when tired), and, rarely, seizures,” Dr. Lim adds. She says the following tweaks to your bedtime routine can be enough to correct some of these issues:
- Try relaxation techniques, such as deep breathing.
- Exercise during the day rather than at night.
- Listen to calming sounds and music, or watch calming videos.
- Talk to your doctor about taking an over-the-counter sleep aid like melatonin.
RELATED: 8 Health Problems Linked to Not Getting Enough Sleep
4. Your Mood Is Still Low After a Few Months“You should see some improvement within three months of starting an antidepressant,” explains Zinia Thomas, MD, a psychiatrist based in St. Louis. “If you have been on an adequate dose of a depression medication for three months and you don’t get results, it’s probably time to try something new.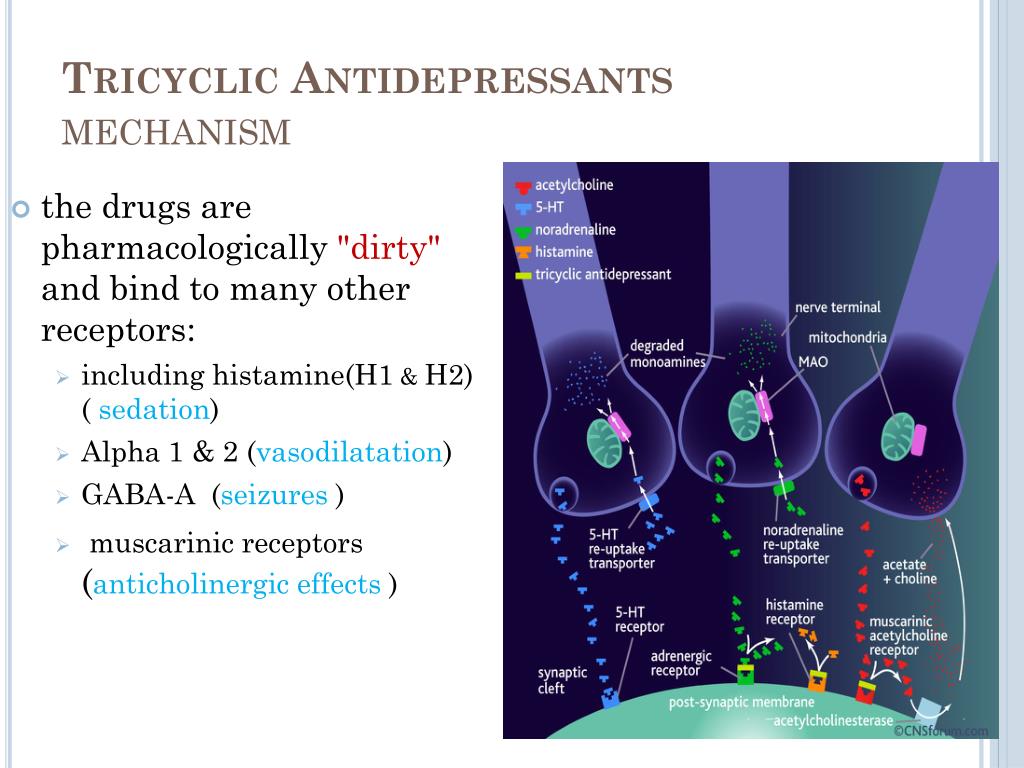 ”
”
“If you feel more physical energy after starting an antidepressant, but you still have depression, that’s good and bad news,” says Gabriela Cora, MD, a psychiatrist in Miami. “It means the depression medication is starting to work, but not in the right way." Increased physical energy combined with depression is a bad combination that can make you act out or increase your risk of suicide, she explains. “So, report these symptoms to your doctor right away,” urges Dr. Cora.
RELATED: 8 Depression Symptoms You Shouldn’t Ignore
6. You’re Experiencing Unpleasant Side EffectsDeciding which depression medication is best for you often comes down to side effects, says Hullett. If you gain weight or have sexual problems on one antidepressant, for example, you may want to switch to one without those side effects, he advises.
Although antidepressants are meant to help you feel better, in some cases an antidepressant may combine with other medications you are taking or foods you are eating and lead to serotonin syndrome, an uncommon condition involving an overabundance of serotonin in the body, the Cleveland Clinic states.
Symptoms to watch out for, Lim says, include fever, aches, shakes, sweats, fatigue, irritability, a bad headache, confusion, agitation, restlessness, dizziness, difficulty seeing or walking, muscle twitching, muscle tension, or jaw clenching.
Typically, serotonin syndrome happens within days or weeks of starting an antidepressant or after a dose increase, says Lim. The most common factors that affect your risk of serotonin syndrome, per the Cleveland Clinic, are:
- Too much of one medication that affects your serotonin levels
- Multiple medications that affect your serotonin levels at the same time
 Your Antidepressant Doesn’t Pack the Same Punch
Your Antidepressant Doesn’t Pack the Same Punch“If you’ve been on an antidepressant for a long time, your body may develop a tolerance,” notes Hullett. As a result, a medication that once worked well at quelling your sadness, anxiety, and other symptom no longer has that power. Sometimes, Hullett says, increasing the dose under supervision by your doctor may help. “If you’ve been taking 10 milligrams (mg) of Prozac (fluoxetine), for example, your physician may increase the dose to 20 mg,” he says. In other cases, trying a different medication or treatment is helpful.
9. Your Depression Worsens“If your depression symptoms get worse as soon as you start taking an antidepressant, or they get better and then very suddenly get worse, it’s a sign that the depression medication isn’t working properly, and you should see your healthcare professional right away,” Hullett says. Specific warning signs to watch for include feeling agitated or restless, pacing or constant movement, hand wringing, or feeling generally out of control.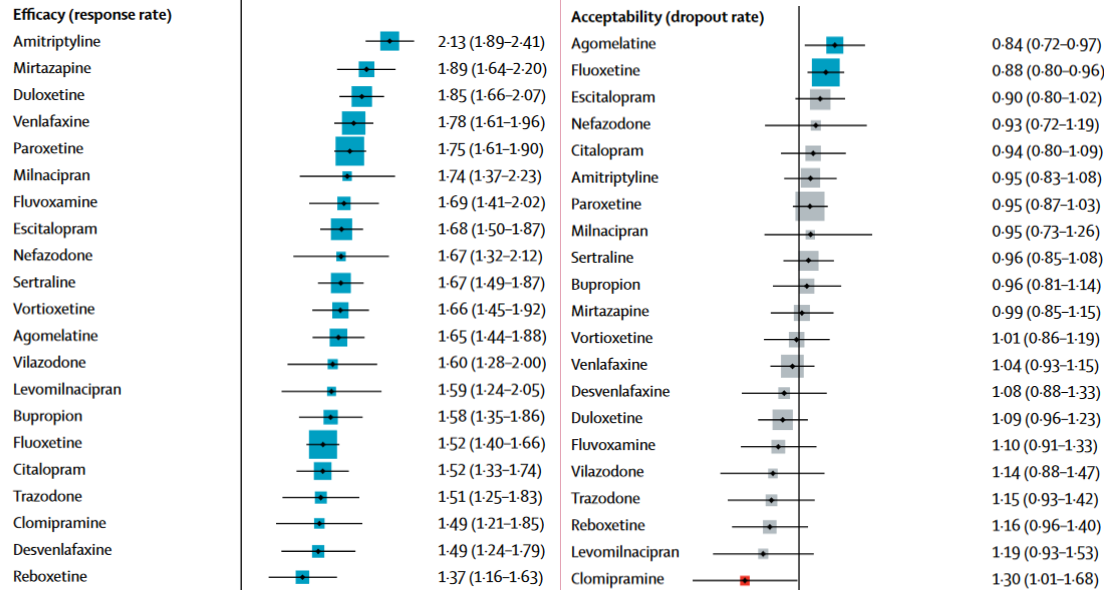
If you experience some relief on an antidepressant, but it’s not the relief you hoped for, it may be time to try something new, Dr. Thomas says. Options include another depression medication or the addition of counseling, psychotherapy, mood-boosting cardio exercise, or light therapy to your treatment regimen. The combination of medication and other mood-brightening treatments can speed your recovery and reduce your overall time on antidepressants, she says.
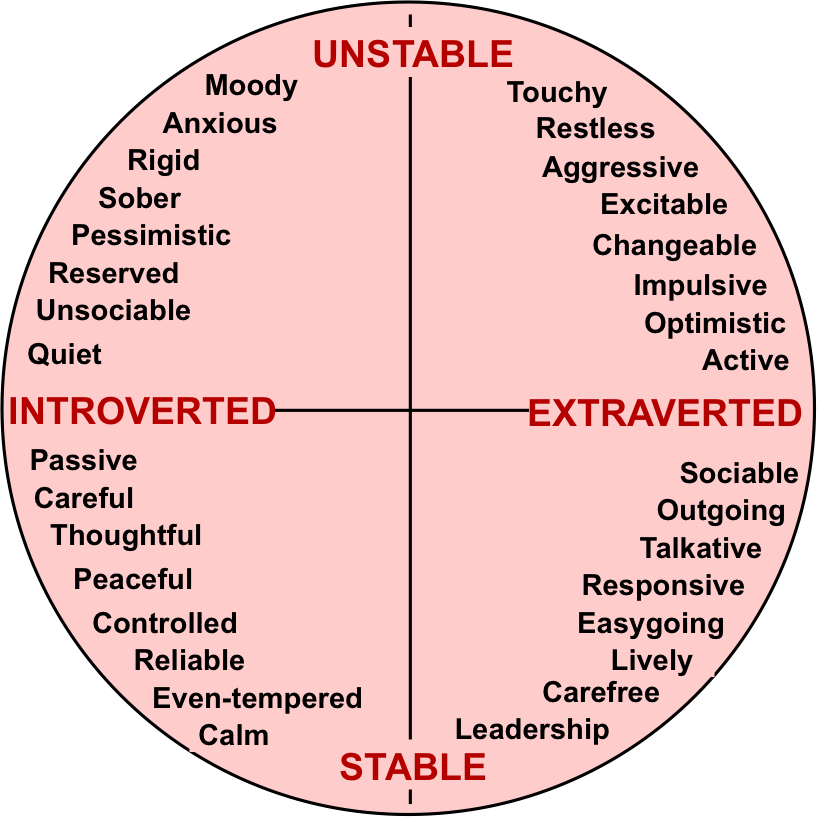
11. Your Mood or Energy Improves — but Too Much“Depression medications can sometimes cause mood swings, especially in people who have a tendency toward bipolar disorder — depression and mania,” Hullett says. If you feel unusually elated or you become very terse with your spouse, feel noticeably more irritable, or have an uncharacteristic bout of road rage, you probably need to change your antidepressant, he advises.
RELATED: 9 Different Types of Depression
12. Your Depression Is GoneIf you’ve been taking an antidepressant for at least six months and you’ve achieved remission, it’s important to slowly taper off your depression medications with the help of your physician. “Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), can produce physical symptoms of withdrawal if you stop taking them suddenly,” he says. “So, you need to reduce the dosage of depression medication slowly, usually over a few weeks.”
You may experience some depressive symptoms when discontinuing antidepressants, but this does not mean the depression is returning. Unfortunately, some people stay on their antidepressants longer than needed because the symptoms of discontinuing SSRIs can be mistaken for signs of returning depression.
Work with your doctor to distinguish between the two. You may need to go even slower than a few weeks when tapering off your antidepressant to prevent these withdrawal symptoms.
While taking an antidepressant can be very helpful for managing depression, you might not find the right one for you on the first try.
If your medication isn’t meeting your expectations, don’t give up. Consider talking to a doctor who specializes in treating mood disorders if you aren’t already seeing one. And be on the lookout for any worrisome symptoms while you're taking any antidepressant, Lim advises. Manic episodes, serotonin syndrome, and seizures, for example, need to be evaluated by a doctor ASAP.
Additional reporting by Michelle Pugle.
Is the antidepressant working - how can you tell?
There are standards for understanding how antidepressants work, the so-called "therapeutic response" or "therapeutic response".
Doctors know and warn the patient to expect a quick effect from any antidepressant (if this is not a side effect - excessive sedation and drowsiness, when after taking a certain antidepressant he is already asleep, on the first night, this does not mean that the antidepressant works exactly as antidepressant He realized the possibility, for example, to sleep. nine0005
nine0005
The antidepressant effect of the drug appears after at least 10 days, and the first antidepressant effect is evaluated only after 2 weeks. Doctors evaluate the patient's condition and say: "Let's see, you will take, we will evaluate together what happened during these 2 weeks."
This is the first estimate. The side effect of the drug is evaluated, you can stop at the selected dose, reduce it, or stop if the side effect is excessive. Evaluate the first therapeutic signs, whether the drug works or not. nine0005
But this is not a reason to change the drug if a therapeutic response is not achieved after 2 weeks. A reliable assessment of the action of an antidepressant occurs within a month, you need to wait until all the mechanisms that are embedded in the drug itself work.
If there is no effect, the doctor decides to increase the dose of the same drug. No need to quickly "jump" to another antidepressant. After all, it can be a wonderful drug that just has not yet begun to work. And you can jump on antidepressants like a jumping horse and achieve nothing but a toxic effect on the liver. nine0005
And you can jump on antidepressants like a jumping horse and achieve nothing but a toxic effect on the liver. nine0005
So, waiting for a higher dose, and only if there is no response to the higher dose, usually 2 times the initial dose, it is a question of changing the antidepressant group, because there are many groups of antidepressants.
to the video listFind a doctor
Recommended on this topic:
November 7, 2022
Timely treatment of depression reduces the risk of developing dementia
Studying the relationship between clinical depression and further risk of dementia has been a challenging task for researchers from different countries. However, they have successfully shown that the presence of depression at different ages is a factor that increases the likelihood of developing various forms of dementia in older people. nine0005
October 21, 2022
Post-COVID-19 depression: a danger not to be ignored
Post-COVID-19 depression is common.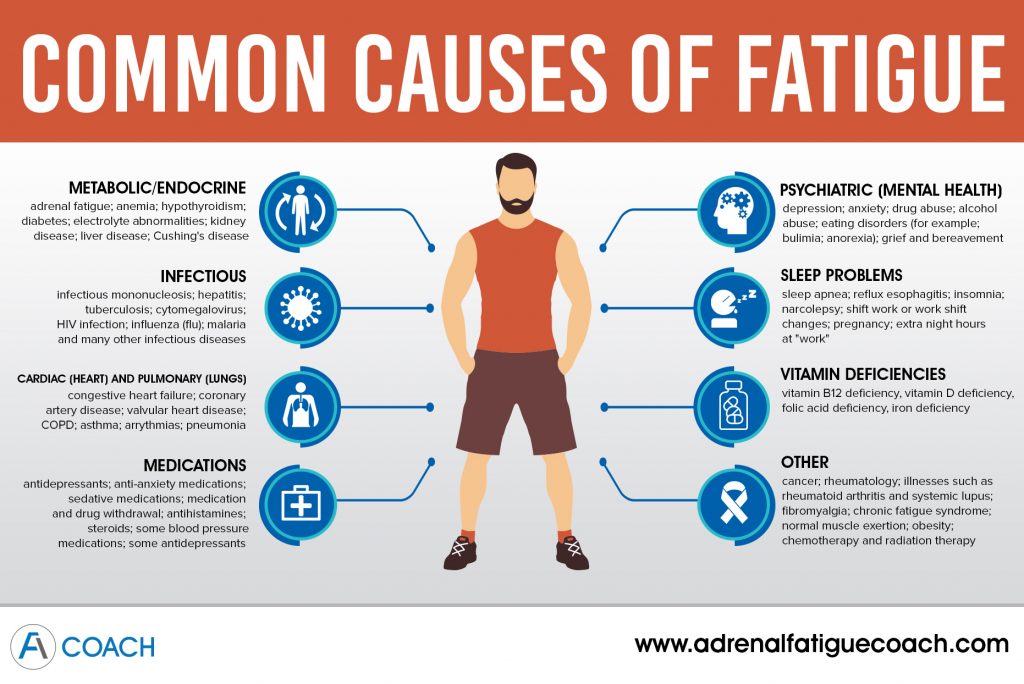 In this case, biological, psychological and environmental factors may contribute to the onset of a mental disorder. In people who have recovered from COVID-19, depression may occur after hospitalization, due to stress during a pandemic, or as a symptom of post-COVID syndrome. nine0005
In this case, biological, psychological and environmental factors may contribute to the onset of a mental disorder. In people who have recovered from COVID-19, depression may occur after hospitalization, due to stress during a pandemic, or as a symptom of post-COVID syndrome. nine0005
August 16, 2022
Risk factors for depression and factors that reduce the risk of depression
Most of the scientific literature on clinical depression usually contains information on risk factors for the development of this severe mental disorder. And a recent study by American scientists also identified factors that can reduce the likelihood of developing depression. Awareness of both types of factors can be useful to the people of Ukraine in today's difficult conditions and help prevent depression. nine0005
June 21, 2022
War and depression: what you need to know
The physical and mental suffering of the civilian population during hostilities can trigger both new cases of depression and exacerbations / relapses in people who had episodes of this disease in the past, even before start of the war. In this case, depression threatens not only those civilians who find themselves in the war zone, but also those located in the territory of the country that was attacked, which the war did not directly affect. nine0005
In this case, depression threatens not only those civilians who find themselves in the war zone, but also those located in the territory of the country that was attacked, which the war did not directly affect. nine0005
Antidepressants don't work: how to treat depression the right way
The right antidepressants can be a real elixir for anxiety, depression and even suicidal thoughts. Unfortunately, doctors do not always manage to find the perfect drug the first time. It is very important to understand in time that your antidepressants are not working as they should.
Alla Rezyapova
am JD / Unsplash
"Each person's brain and body reacts and processes drugs differently," said Melissa Shepard, board certified psychiatrist and assistant professor, "but it's not always clear why that happens." However, doctors in an interview with HuffPost named seven sure signs that your treatment needs to be adjusted. nine0005
Contents of article
Do not self-medicate! In our articles, we collect the latest scientific data and the opinions of authoritative health experts. But remember: only a doctor can diagnose and prescribe treatment.
But remember: only a doctor can diagnose and prescribe treatment.
You feel an immediate improvement, but it is followed by a rollback
Doctors have no exact answer as to why rapid progress is lost over time, but there are several suggestions. The fact is that with mood disorders and anxiety, serotonin and dopamine drop. The drug raises the levels of these substances, but stabilizing the "chemistry" of the brain by itself may not be enough. For example, for patients with bipolar disorder, mood stabilizers are also required. Taking concomitant medications or alcohol can affect the effect of antidepressants. nine0005
And if the cause of the mood disorder or anxiety is caused by diseases - for example, the thyroid gland - then antidepressants may not be effective at all. In addition, the reason for the short-term improvement may be the placebo effect: the patient expects the drugs to help, and they do. But, of course, an incorrectly selected antidepressant will not give a long-term and stable effect.
But, of course, an incorrectly selected antidepressant will not give a long-term and stable effect.
To cure depression, it is important not only to take medication, but also to adjust your lifestyle in general: less psychoactive substances, including alcohol, more activities, more time outdoors. nine0005
Side effects come and go
During the first 12 weeks of use, the body gradually adjusts and gets used to the drug. During this time, side effects may occur. Some people are more sensitive to the components of the medicine. “For some patients, side effects may be due to the fact that they absorb drugs more slowly, so they tend to accumulate in the body,” says Eric Vanderlip, a certified psychiatrist and family doctor. nine0005
You may experience:
- nausea,
- headache,
- fatigue,
- diarrhea.
But these side effects should go away after a few days. If you feel that the unpleasant effects outweigh the benefits of treatment, contact your doctor for a course adjustment.
If you feel that the unpleasant effects outweigh the benefits of treatment, contact your doctor for a course adjustment.
Your symptoms are coming back
Depression is an insidious disease. Sometimes even a patient who conscientiously takes the medicine can relapse. The reason may be increased stress, additional negative factors in life: not only private, but also global events can also affect your condition. However, if nothing has changed in your life and environment, and you feel a "rollback", a return of depression symptoms, this may signal that your medication has stopped working. nine0005
Depressive and anxiety symptoms get worse
The doctor usually starts with the mildest drug that fits the patient's disease profile. Maximum positive effect, minimum side effects. Then the psychiatrist adjusts the course, changes the dosage, adds or removes some drugs. But sometimes, right after you start taking antidepressants, you may not feel better, but worse. “It means the drug is not right for you,” says Shili Gandhi, Vice President of SingleCare Clinic. nine0005
“It means the drug is not right for you,” says Shili Gandhi, Vice President of SingleCare Clinic. nine0005
You don't notice the difference
Many people have only a partial response to their medications—for example, they may stop having panic attacks but still experience high levels of anxiety that interferes with daily life. “In fact, we rarely get complete remission of symptoms with the first drug, the first dose,” says Vanderlip. "For many, a couple of dosage adjustments is not unusual." And sometimes the drug just doesn't work—it doesn't work for your type of depression. If you have not noticed an improvement in your well-being within a month, contact your doctor for a course adjustment. nine0005
You notice severe mood swings
It can be difficult for doctors to immediately tell the difference between unipolar depressive disorder and bipolar manic episodes. If the drug is not properly chosen, and a patient with bipolar disorder takes an antidepressant instead of a mood stabilizer, he may experience unpleasant mood swings.