Working with schizophrenics
What counselors need to know about schizophrenia
The adjective “schizophrenic” needs to be removed from counselors’ vocabulary, says Elizabeth Prosek, a counselor and assistant professor at the University of North Texas (UNT).
Schizophrenia has a great deal of stigma and negative connotations associated with it, and referring to clients in the first person can lessen these, she says.
“I encourage counselors to advocate for what clients with schizophrenia can do rather than [focusing on] the limitations of experiencing psychosis,” says Prosek, who has counseled clients with severe mental health disorders and served on a support team for individuals with schizophrenia living independently. “I once heard someone discuss the ‘aggressive nature’ of those diagnosed with schizophrenia. I could not help but wonder where that perception evolved. In my experience, clients did not demonstrate aggressive behavior or language.”
Counselors, as part of a multidisciplinary treatment team of helping professionals, can play a critical role in the lives of people diagnosed with schizophrenia, say Prosek and Kara Hurt, a licensed professional counselor who works with clients with schizophrenia at an inpatient psychiatric hospital.
Prosek and Hurt, who is also a doctoral student at UNT, recently collaborated to write a practice brief on schizophrenia for the American Counseling Association’s Center for Counseling Practice, Policy and Research (see sidebar below).
In the brief, the duo describes schizophrenia as a lifelong illness characterized by negative symptoms, including “delusions, hallucinations (most commonly auditory), disorganized thinking or speech and disorganized or abnormal motor behavior.” The estimated prevalence rate for schizophrenia is 1 percent of the population in Western, developed countries.
For counselors, empathy should play a big part in therapy – from knowing the many side effects of schizophrenia medications to fully understanding what it is like to live with hallucinations and psychosis, say Prosek and Hurt. Special training and workshops can help counselors understand the nuances of the disorder, as can materials from mental health agencies (see “for more information” below).
Prosek once attended a seminar at which participants sat through the experience – virtually – of living with hallucinations, experiencing paranoia and hearing voices intertwined with the dialogue of another person.
Prosek and Hurt led a course this past year in which they showed videos of clients with schizophrenia explaining their own experiences.
“When the students in the class debriefed after the video, many confirmed that hearing firsthand from a client decreased their misperceptions about the disorder,” says Prosek. “Watching a video of a client with schizophrenia who was articulate and successful in a career reduced stigma of the disorder. Also, I noticed that when person-first language is used when discussing clients with schizophrenia [as opposed to using the term “schizophrenic”], negative connotations are immediately lessened.”
What do counselors need to know about schizophrenia?
Elizabeth Prosek: Living with psychosis can be scary and challenging. When working with those diagnosed with schizophrenia, demonstrating empathic concern is essential to build a therapeutic relationship. In my experience, clients appreciated my willingness to embrace their perspective of psychosis. I think all of the clients I worked with experienced their psychosis uniquely, and it was imperative that I understood their lived experience.
When working with those diagnosed with schizophrenia, demonstrating empathic concern is essential to build a therapeutic relationship. In my experience, clients appreciated my willingness to embrace their perspective of psychosis. I think all of the clients I worked with experienced their psychosis uniquely, and it was imperative that I understood their lived experience.
Kara Hurt: Schizophrenia affects the client’s support system, not just the client. In my experience, it is just as important to provide counseling and support to family members and loved ones of people diagnosed with schizophrenia as it is to provide support and counseling to clients with schizophrenia. All of us counselors can help provide services in some way that help clients diagnosed with schizophrenia and those that love them.
EP: Counselors may provide family members and friends with psychoeducation on the symptoms and treatment options for schizophrenia. Furthermore, counselors may assist family members and friends to build empathy for the experiences of those diagnosed with schizophrenia. There are support groups for family members through the National Alliance on Mental Illness (NAMI). Find a local NAMI support group through nami.org.
There are support groups for family members through the National Alliance on Mental Illness (NAMI). Find a local NAMI support group through nami.org.
For those clients who do not have a familial support system, encouraging the development of a community support network may be essential for the social and emotional well-being of clients diagnosed with schizophrenia. Regardless of diagnosis, humans in general seek “belongingness” in their community, and those diagnosed with schizophrenia are no different.
What advice would you give about working with clients diagnosed with schizophrenia?
EP: Recognizing strengths can be a great first step to creating an appropriate treatment plan. Several of the clients I counseled had creative interests, such as art and music, and we developed interventions to promote participation in those activities.
Also, I recommend communication with all professionals working with the client. In my experience, collaborating with the client’s psychiatrist and case manager allowed for a holistic approach when addressing current therapeutic needs. Having a multidisciplinary team also allows for clients to more easily transition in and out of inpatient psychiatric hospitalization when necessary. With the appropriate releases of information, all professionals involved can be aware of how the client’s psychosis presented, any medication changes and any changes in treatment recommendations after an inpatient hospitalization stay.
Having a multidisciplinary team also allows for clients to more easily transition in and out of inpatient psychiatric hospitalization when necessary. With the appropriate releases of information, all professionals involved can be aware of how the client’s psychosis presented, any medication changes and any changes in treatment recommendations after an inpatient hospitalization stay.
It did not take long after beginning my work with clients diagnosed with schizophrenia for me to recognize the need for socialization. Several of my clients lived in isolation but longed for social relationships. In collaboration with case managers, I organized social outings for clients, which allowed for a more genuine community-living experience. There are several community resources for clients diagnosed with serious mental health disorders, such as supported-work programs. Having knowledge of such programs in the community will serve as great referral sources for clients diagnosed with schizophrenia.
With what other types of issues can clients diagnosed with schizophrenia present?
KH: One of the presenting issues that I had not expected when I started working with clients diagnosed with schizophrenia was substance abuse. One client in particular stands out in my mind because of the extent of his illicit drug use, which worsened his paranoia and other delusions. When working with clients with schizophrenia, you may need to reconsider your assumptions to appreciate that these clients have many of the same kinds of problems as other clients.
EP: I agree. Substance misuse was prevalent among the clients diagnosed with schizophrenia that I worked with as well. I also observed many secondary diagnoses, including anxiety and depression. I connect the anxiety and depressive symptoms back to the potential isolation clients experienced. Furthermore, it seems to me hearing voices and feeling out of touch from reality would lead to feelings of anxiety. Helping my clients accurately explain symptoms to their psychiatrists allowed for more precise medication prescriptions.
Helping my clients accurately explain symptoms to their psychiatrists allowed for more precise medication prescriptions.
What are some common misperceptions about schizophrenia?
EP: One of the common misperceptions I hear frequently when describing a client with schizophrenia is the term “medication noncompliance.” I advocate for this phrase to be removed from counselor language. From my observations, when clients did not take medications regularly or as prescribed, it was not with intentional noncompliance, but rather there was confusion when medication regimens became complex or changed with frequency. Moreover, several antipsychotic medications have uncomfortable side effects. On a bad day, when a client is not feeling well, he or she might not feel inclined to perpetuate the experience by taking medications that may worsen physical symptoms. In counseling sessions, taking time to hear clients’ concerns or complaints about side effects may help clients feel validated in their experience.
What challenges do counselors face in this area?
EP: I think there may be a perception that clients with schizophrenia only need a case manager and psychiatrist. From my perspective, counselors can play a vital role in the treatment team. Never underestimate the power of a space in which a client’s experience is heard and valued.
KH: I think it is absolutely critical to have good supervision when working with a client diagnosed with schizophrenia. I have felt frustrated with my perceptions of clients’ lack of progress or insight, but with supportive supervision, I have been able to be more flexible with my therapeutic expectations and shift my perspective to be a better counselor for my clients. I cannot underestimate the value of good supervision. It can help you gain awareness of potential burnout and the need for regular self-care.
EP: Supervision is helpful. I often felt frustrated with the mental health care system and how clients with schizophrenia became victims of gaps in continuity of care.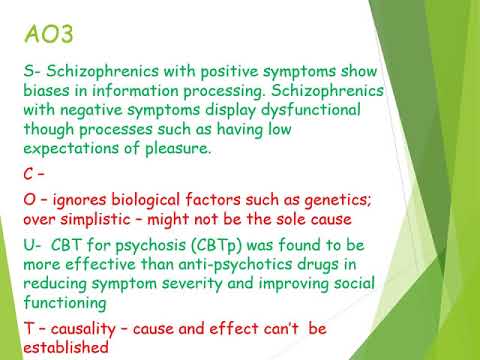 I agree with Kara that there is a greater potential for burnout when working with clients in and out of crisis.
I agree with Kara that there is a greater potential for burnout when working with clients in and out of crisis.
Another challenge for counselors might be understanding the differences in antipsychotic medications most commonly prescribed for clients with schizophrenia. Actually, Kara introduced me to an app (named Epocrates) that provides names, descriptions and side effects for medications. I remember when I first started working with this population, I had a hard time differentiating the medications the clients were prescribed. There are several research studies published outlining effectiveness and common side effects of antipsychotic medications which may be helpful to read.
Going back to one of Kara’s original statements about the importance of family supports, it may be challenging to help family understand the experience of schizophrenia. Counselors can serve as a good source of information to help educate and support family members. Consequently, family members can better support the client diagnosed with schizophrenia.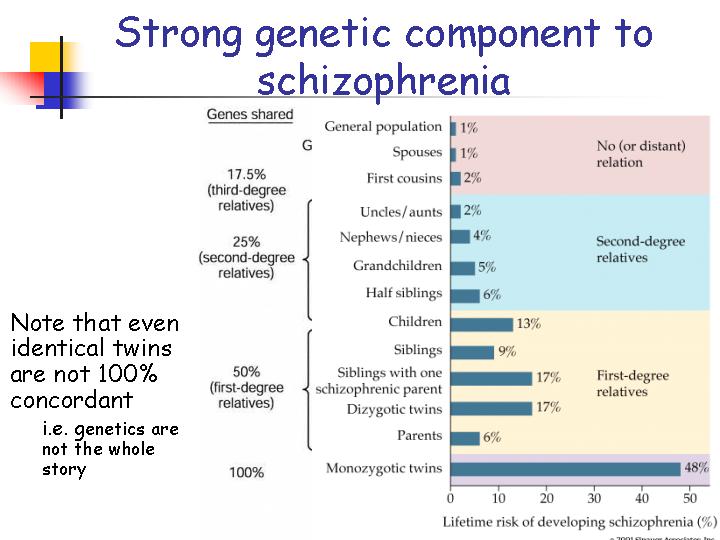
****
For more information
- The ACA Center for Counseling Practice, Policy and Research practice brief on schizophrenia, written by Prosek and Hurt (available only to members of ACA): counseling.org/knowledge-center/center-for-counseling-practice-policy-and-research/practice-briefs
- The National Institute of Mental Health (NIMH) outlines definitions, treatment and potential clinical trials for those diagnosed with schizophrenia: nimh.nih.gov/health/topics/schizophrenia/index.shtml
- The National Alliance on Mental Illness (NAMI) provides training specific to schizophrenia, as well as education, support and advocacy opportunities for individuals diagnosed with mental health disorders and their family members: nami.org
- From the Journal of Counseling & Development: “It’s Time for Counselors to Modify Our Language: It Matters When We Call Our Clients Schizophrenics Versus People With Schizophrenia“
****
ACA Center for Counseling Practice, Policy and Research practice briefs
Prosek and Hurt’s information sheet on schizophrenia is one of 30 practice briefs available to American Counseling Association members through the Center for Counseling Practice, Policy and Research.
The briefs, which range from working with victims of domestic violence to animal-assisted therapy to posttraumatic stress disorder, are written by ACA members who are experts on that particular topic. New practice briefs are being added regularly.
The practice briefs are designed to be practical, evidence-based resources for ACA members, says Victoria Kress, executive editor of the ACA center’s practice briefs project and a professor at Youngstown State University in Ohio.
Counselors can use the practice briefs as a refresher on topics they may not encounter very often, such as schizophrenia, or as a jumping-off point for further research. Each brief contains links to in-depth sources and data on a topic, as well as therapy models and other tools.
Kress says each practice brief is written and edited to be practical and succinct, with focused bursts of information on topics that counselors in all works settings may encounter, from divorce and autism to perfectionism and suicide prevention.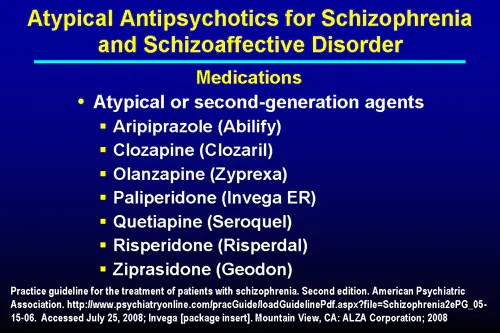
The plan is to post 15 to 20 new briefs each year, Kress says, including on each of the new disorders added to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders.
Kress began soliciting practice briefs from ACA members, then editing and posting the briefs on the ACA website, close to two years ago. The idea grew out of ACA past president Bradley Erford’s focus on counselor use of evidence-based practices, Kress says.
“Counselors don’t always have access to, or the time to read, journal articles,” she says. “We wanted to provide an outlet for ACA members to sit down and get a quick overview. … It was really born out of this idea that counselors should be using evidence-based practices. We know that counselors are busy and have competing demands. … The ultimate idea is that it will improve their practice. It’s better for their clients and the profession.”
- Find the practice briefs, and guidelines on submitting a new brief, here: counseling.
 org/knowledge-center/center-for-counseling-practice-policy-and-research/practice-briefs (Note: ACA member login required to view each brief)
org/knowledge-center/center-for-counseling-practice-policy-and-research/practice-briefs (Note: ACA member login required to view each brief)
****
Bethany Bray is a staff writer for Counseling Today. Contact her at [email protected]
Follow Counseling Today on Twitter @ACA_CTonline and on Facebook: facebook.com/CounselingToday
Helping Someone with Schizophrenia - HelpGuide.org
schizophrenia
Have a loved one with schizophrenia? Your support can make a huge difference by helping them find the right treatment, cope with symptoms, and build a rich, satisfying life.
When a loved one has schizophrenia
The love and support of family and friends plays an important role in schizophrenia treatment and recovery. If you have a loved one with schizophrenia, you may be struggling with any number of difficult emotions, including fear, guilt, anger, and frustration. You may feel helpless in the face of your loved one’s symptoms, worried about the stigma of schizophrenia, or confused and embarrassed by their strange behaviors.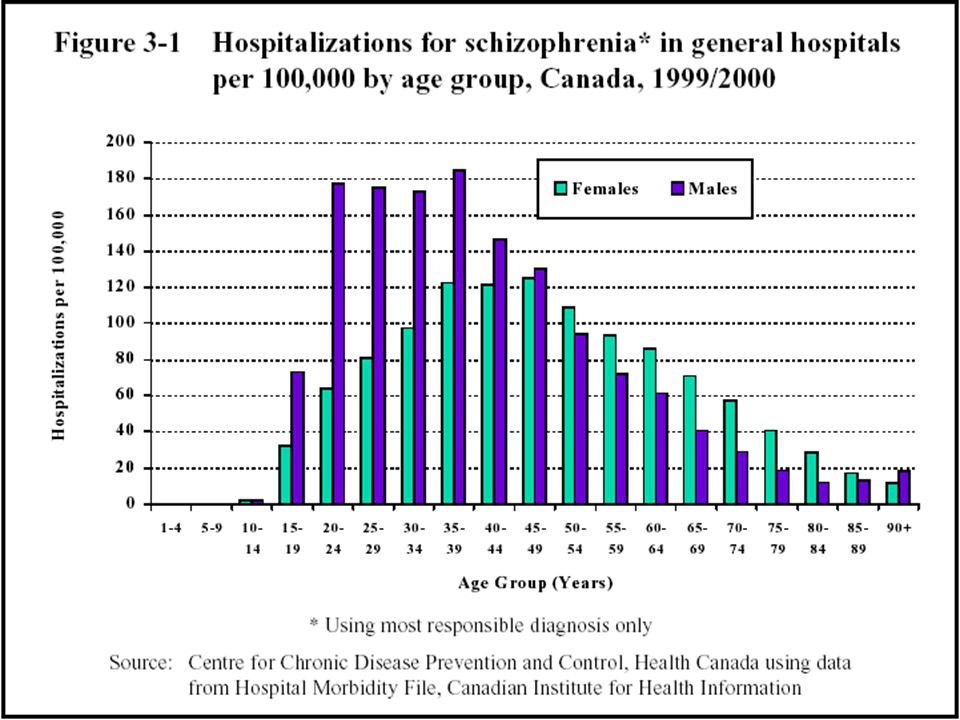 You may even be tempted to hide your loved one’s illness from others.
You may even be tempted to hide your loved one’s illness from others.
But it’s important to remember that a diagnosis of schizophrenia is not a life-sentence. Recovery is possible, especially with your love and support. To help someone with schizophrenia, it’s crucial you:
- Accept the illness and its difficulties.
- Not buy into the myth that someone with schizophrenia can't get better or live a full and meaningful life.
- Do your best to help your loved one feel better and enjoy life.
- Pay attention to your own needs.
- Maintain your sense of humor and remain hopeful.
While dealing with a loved one’s schizophrenia can be challenging, the following strategies can help you guide your loved one on the road to recovery without losing sight of your own hopes and dreams.
Tips for helping a loved one with schizophrenia
Educate yourself. Learning about schizophrenia and its treatment will allow you to make informed decisions about how best to cope with symptoms, encourage your loved one to pursue self-help strategies, handle setbacks, and work towards recovery.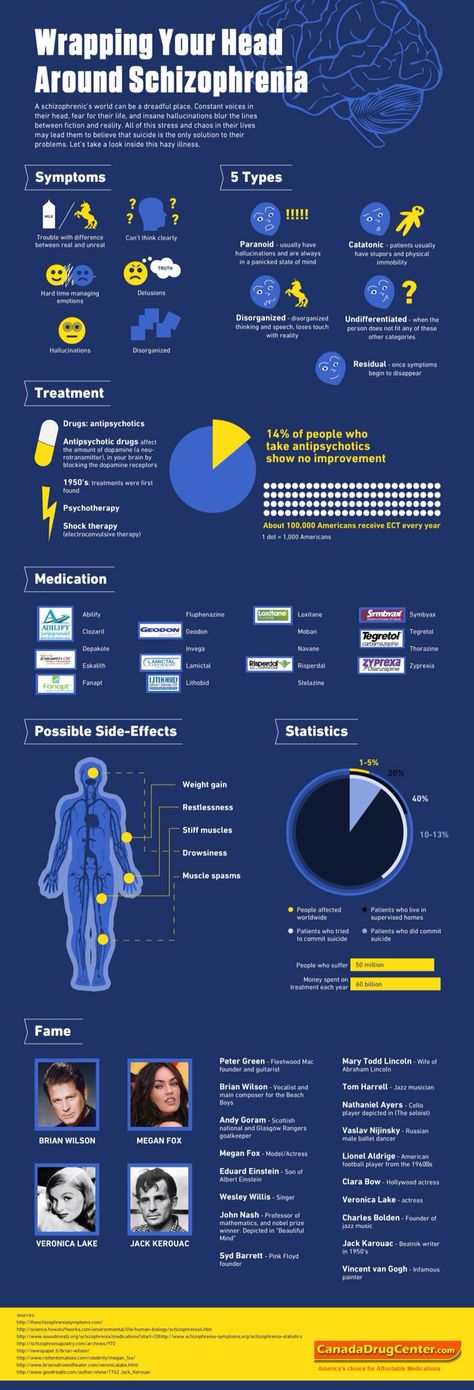
Reduce stress. Stress can cause schizophrenia symptoms to flare up, so it's important to create a structured and supportive environment for your loved one.
Set realistic expectations. It's important to be realistic about the challenges of schizophrenia. Help your loved one set and achieve manageable goals, and be patient with the pace of recovery.
Empower your loved one. Be careful that you're not taking over and doing things for your loved one that they are capable of doing. Support your loved one while still encouraging as much independence and self-help as possible.
Helping someone with schizophrenia tip 1: Encourage treatment and self-help
Encouraging treatment and self-help is a cornerstone of helping a loved one with schizophrenia. While medication is an important element of schizophrenia treatment, your loved one's recovery depends on other factors as well. Self-help strategies such as changing to a healthy diet, managing stress, exercising, and seeking social support can have a profound effect on your loved one's symptoms, feelings, and self-esteem. And the more someone does for themselves, the less hopeless and helpless they'll feel, and the more likely their doctor will be able to reduce their medication. Your encouragement and support can be crucial to your loved one starting and continuing a program of self-help.
And the more someone does for themselves, the less hopeless and helpless they'll feel, and the more likely their doctor will be able to reduce their medication. Your encouragement and support can be crucial to your loved one starting and continuing a program of self-help.
[Read: How to Help Someone with Mental Illness Accept Treatment]
Starting treatment
Often, the first challenge of treatment is convincing the person with schizophrenia to see a doctor. To people experiencing delusions, hallucinations, and paranoia, there is no need for medical intervention because the voices and conspiracy theories are real.
If a loved one with schizophrenia is reluctant to see a doctor, try to:
Provide options. Your loved one may be more willing to see a doctor if he or she has some control over the situation. If your relative appears suspicious of you, suggest that another person accompany them to the appointment. You can also give your loved one a choice of doctors.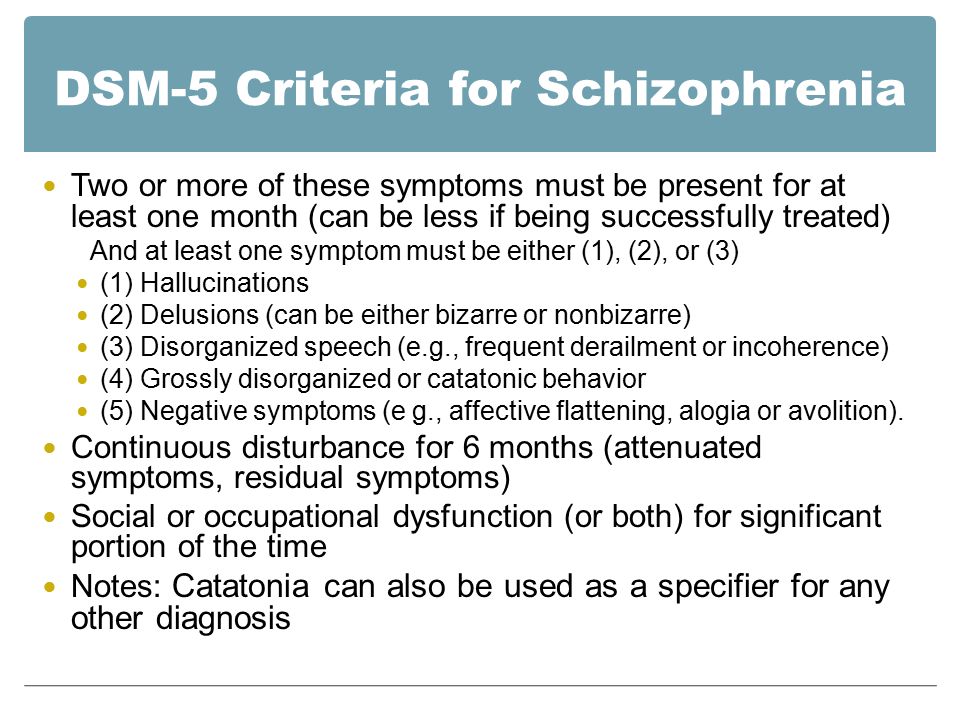
Focus on a particular symptom. Someone with schizophrenia may resist seeing a doctor out of fear of being judged or labeled “crazy.” You can make the doctor less threatening by suggesting a visit in order to deal with a specific symptom such as insomnia or lack of energy.
Tips for supporting a loved one's schizophrenia treatment
Seek help right away. Early intervention makes a difference in the course of schizophrenia, so help your loved one find a good doctor and start treatment.
Be collaborative. When your loved one has a voice in their own treatment, they will be more motivated to work towards recovery.
Encourage self-help. Since schizophrenia is often episodic, periods of remission from the severest symptoms can provide an opportunity for your loved one to employ self-help strategies that may limit the length and frequency of future episodes.
Tip 2: Build your support network
To better support and care for someone with schizophrenia, you need to find help, encouragement, and understanding from others.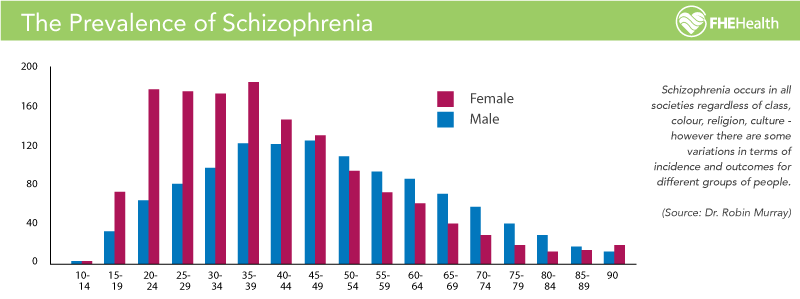 The more support you have, the better it will be for both you and your loved one.
The more support you have, the better it will be for both you and your loved one.
Recognize your own limits. Be realistic about the level of support and care you can provide. You can't do it all, and you won't be much help to a loved one if you're exhausted, so seek help where you can.
Join a support group. Meeting others who know first-hand what you're going through can help reduce feelings of isolation and fear. Support groups provide an invaluable venue for the relatives of people with schizophrenia to share experiences, advice, and information.
Turn to trusted friends and family members. Ask loved ones if you can call on them for support. Most people will be flattered by your request.
Seek out new friends. If you don't feel that you have anyone to turn to, it's never too late to build new friendships and improve your support network.
Take advantage of support services. Ask your loved one's doctor or therapist about respite services and other support available in your area, or contact local hospitals and mental health clinics.
With over 25,000 licensed counselors, BetterHelp has a therapist that fits your needs. It's easy, affordable, and convenient.
GET 20% OFF
Online-Therapy.com is a complete toolbox of support, when you need it, on your schedule. It only takes a few minutes to sign up.
GET 20% OFF
Teen Counseling is an online therapy service for teens and young adults. Connect with your counselor by video, phone, or chat.
GET 20% OFF
Tip 3: Monitor medication
Once in treatment, careful monitoring can ensure that your loved one stays on track and gets the most out of medication.
Take side effects seriously. Many people with schizophrenia stop taking their medication because of side effects. Bring any distressing side effects to the attention of the doctor, who may be able to reduce the dose, switch to another antipsychotic, or add medication to counter the side effect.
Encourage your loved one to take medication regularly. Even with side effects under control, some people with schizophrenia refuse medication or have trouble remembering their daily dose. Medication reminder apps, weekly pillboxes, and calendars can help. Some medications are available as long-lasting weekly or monthly injections instead of daily pills.
Even with side effects under control, some people with schizophrenia refuse medication or have trouble remembering their daily dose. Medication reminder apps, weekly pillboxes, and calendars can help. Some medications are available as long-lasting weekly or monthly injections instead of daily pills.
Be careful to avoid drug interactions. Help your loved one avoid any dangerous drug interactions by giving the doctor a complete list of the drugs and supplements they're taking. Mixing alcohol or illegal drugs with schizophrenia medication is harmful, so talk to the doctor if your relative has a substance abuse problem.
Track your family member's progress. A mood-tracking app, journal, or diary is a good way to track changes in your family member's behavior, outlook, and other symptoms in response to medication.
Stopping medication is the most frequent cause of relapse in schizophrenia, so it's extremely important that your family member continues to take all medication as directed. While relapse can occur even if a person is taking medication as prescribed, you may be able to prevent a full-blown crisis by recognizing the warning signs and taking immediate steps.
While relapse can occur even if a person is taking medication as prescribed, you may be able to prevent a full-blown crisis by recognizing the warning signs and taking immediate steps.
Common warning signs of schizophrenia relapse
- Insomnia
- Social withdrawal
- Deterioration of personal hygiene
- Increasing paranoia
- Hostility
- Confusing or nonsensical speech
- Strange disappearances
- Hallucinations
If you notice any warning signs of relapse or other indications that your family member's symptoms of schizophrenia are getting worse, call the doctor right away.
Tip 5: Prepare for crisis situations
Despite your best efforts to prevent relapse, there may be times when your loved one's condition deteriorates rapidly and hospitalization is required to keep them safe. Having an emergency plan ready for an acute psychotic episode will help you handle the crisis safely and quickly.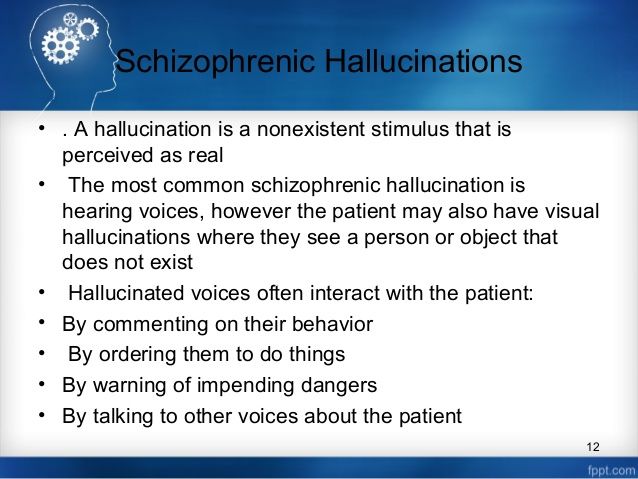 A good emergency plan for someone with schizophrenia includes:
A good emergency plan for someone with schizophrenia includes:
- Emergency contact information for your loved one's doctor and therapists.
- The address and phone number of the hospital you will go to for psychiatric admission.
- Friends or relatives who will take care of other children or dependents while you deal with the crisis.
It's also wise to go over the emergency plan with your family member. The crisis situation may be less frightening to your loved one if they know what to expect during an emergency.
10 tips for handling a schizophrenia crisis
- Remember that you cannot reason with acute psychosis.
- The person may be terrified by their own feelings of loss of control.
- Don't express irritation or anger.
- Speak quietly and calmly, do not shout or threaten the person.
- Don't use sarcasm as a weapon.
- Decrease distractions by turning off the TV, computer, any fluorescent lights that hum, etc.
- Ask any casual visitors to leave—the fewer people the better.

- Avoid direct, continuous eye contact.
- Avoid touching the person.
- Sit down and ask the person to sit down as well.
Tip 6: Explore housing options
Someone with schizophrenia needs a stable, supportive place to live, but finding the right living situation can be challenging.
- Can your loved one care for themselves?
- How much support do they need with daily activities?
- Does your loved one have a drug or alcohol problem?
- How much treatment supervision does your loved one require?
Living with family
Living with family can be a good option for someone with schizophrenia if their family members understand the illness well, have a strong support system of their own, and are able to provide whatever assistance is needed.
At-home arrangements are less likely to be successful if the person with schizophrenia uses drugs or alcohol, resists taking medication, or is aggressive or uncooperative.
| Choosing the Right Housing Option for Someone with Schizophrenia |
| Living with family works best if: |
|
| Living with family is not advised if: |
|
Try not to feel guilty if you are unequipped to house someone with schizophrenia. If you can't look after your own needs or those of other family members while caring for your loved one, they will be better off elsewhere.
Residential options outside the family home
If an at-home living arrangement isn't the right fit, explore the residential facilities in your community.
Options in your area may include:
Residential treatment facilities or 24-hour care homes. A more structured living environment for those requiring greater assistance or suffering an acute psychotic episode.
Transitional group home. An intensive program that helps individuals transition back into society and avoid relapse after a crisis or hospitalization.
Foster or boarding homes. A group living situation offering a degree of independence, while providing meals and other basic necessities.
Supervised apartments. Residents live alone or share an apartment, with staff members available on-site to provide assistance and support.
Tip 7: Take care of yourself
Taking care of yourself isn't selfish. In fact, it's just as important for your loved one with schizophrenia that you look after your own health needs.
Schizophrenia can place an incredible amount of stress on the family. It can take over your life and burn you out. And if you're stressed, you'll make the person with schizophrenia stressed and trigger or exacerbate their symptoms.
It can take over your life and burn you out. And if you're stressed, you'll make the person with schizophrenia stressed and trigger or exacerbate their symptoms.
Since adopting healthy lifestyle habits is also important for your loved one in managing schizophrenia symptoms, by taking care of your own health you can act as a role model. You may even be able to pursue some of these steps together, helping to motivate and encourage each other.
Connect with others. Social interaction with someone who cares about you is the most effective way to relieve stress. It's important for both you and the person with schizophrenia to have other people you can connect with face-to-face—someone you can talk to for an uninterrupted period of time, someone who will listen without judging or continually becoming distracted. That person may be a friend, family member, clergy member, or professional therapist.
Get regular exercise. Physical activity reduces stress and releases endorphins, powerful chemicals in your brain that energize your spirits and make you feel good. Whether you exercise alone, with a friend, or with your loved one with schizophrenia, aim for 30 minutes of activity on most days, or if it's easier, three 10-minute sessions.
Whether you exercise alone, with a friend, or with your loved one with schizophrenia, aim for 30 minutes of activity on most days, or if it's easier, three 10-minute sessions.
Eat a healthy diet. What you eat has a direct impact on the way you feel. Minimize sugar and refined carbs, foods that quickly lead to a crash in mood and energy. Boost your intake of Omega-3 fatty acids from fatty fish, fish oil, walnuts, and flaxseeds to help improve your focus, energy, and outlook. The same diet tips can help manage your loved one's symptoms, too.
Practice acceptance. Instead of dwelling on the unfairness of your loved one's diagnosis, accept your feelings, even the negative ones. It can make a huge difference in your ability to manage stress and balance your moods. See HelpGuide's Emotional Intelligence Toolkit for more.
Seek out joy. Making time for fun isn't indulgent—it's necessary. Schedule time into your day for things you enjoy, whether it's spending time in nature, visiting friends, or reading a good book. Encourage your loved one with schizophrenia to do the same.
Encourage your loved one with schizophrenia to do the same.
Look after your health. Neglecting your health will only add to the stress in your life. Get enough sleep and stay on top of any medical conditions.
Use relaxation techniques. Techniques such as meditation, deep breathing, yoga, or progressive muscle relaxation can put the brakes on stress and bring your mind and body back into balance.
Authors: Melinda Smith, M.A., Lawrence Robinson, and Jeanne Segal, Ph.D.
- References
Schizophrenia Spectrum and Other Psychotic Disorders. (2013). In Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. https://doi.
 org/10.1176/appi.books.9780890425787.x02_Schizophrenia_Spectrum
org/10.1176/appi.books.9780890425787.x02_Schizophrenia_SpectrumPilling, S., P. Bebbington, E. Kuipers, P. Garety, J. Geddes, G. Orbach, and C. Morgan. “Psychological Treatments in Schizophrenia: I. Meta-Analysis of Family Intervention and Cognitive Behaviour Therapy.” Psychological Medicine 32, no. 5 (July 2002): 763–82. https://doi.org/10.1017/s0033291702005895
Lloyd, Joanne, Helen Lloyd, Ray Fitzpatrick, and Michele Peters. “Treatment Outcomes in Schizophrenia: Qualitative Study of the Views of Family Carers.” BMC Psychiatry 17, no. 1 (July 21, 2017): 266. https://doi.org/10.1186/s12888-017-1418-8
Ganguly, Pronab, Abdrabo Soliman, and Ahmed A. Moustafa. “Holistic Management of Schizophrenia Symptoms Using Pharmacological and Non-Pharmacological Treatment.” Frontiers in Public Health 6 (2018): 166. https://doi.org/10.3389/fpubh.2018.00166
Knight, Edward L. “Self-Help and Serious Mental Illness.” Medscape General Medicine 8, no. 1 (March 15, 2006): 68.
 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1681955/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1681955/“Self-Management: The Experiences and Views of Self-Management of People with a Diagnosis of Schizophrenia – Social Care Online.” Accessed November 2, 2021. https://www.scie-socialcareonline.org.uk/self-management-the-experiences-and-views-of-self-management-of-people-with-a-diagnosis-of-schizophrenia/r/a11G00000017tP5IAI
Stępnicki, Piotr, Magda Kondej, and Agnieszka A. Kaczor. “Current Concepts and Treatments of Schizophrenia.” Molecules: A Journal of Synthetic Chemistry and Natural Product Chemistry 23, no. 8 (August 20, 2018): 2087. https://doi.org/10.3390/molecules23082087
Patel, Krishna R., Jessica Cherian, Kunj Gohil, and Dylan Atkinson. “Schizophrenia: Overview and Treatment Options.” Pharmacy and Therapeutics 39, no. 9 (September 2014): 638–45. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4159061/
Biagianti, Bruno, Sophia H. Quraishi, and Danielle A. Schlosser. “Potential Benefits of Incorporating Peer-to-Peer Interactions Into Digital Interventions for Psychotic Disorders: A Systematic Review.
 ” Psychiatric Services 69, no. 4 (April 1, 2018): 377–88. https://doi.org/10.1176/appi.ps.201700283
” Psychiatric Services 69, no. 4 (April 1, 2018): 377–88. https://doi.org/10.1176/appi.ps.201700283
Schizophrenia: The Journey to Recovery (PDF) – Family guide to schizophrenia assessment and treatment. (Schizophrenia Society of Canada)
60 Tips for Helping People who have Schizophrenia – Tips for communicating with someone who has schizophrenia, handling a crisis, and avoiding relapses. (Schizophrenia.com)
Finding a Good Residential Option for Someone with Severe Mental Illness – Provides suggestions for choosing the right living arrangement for someone with schizophrenia. (Schizophrenia.com)
Helplines and support
In the U.S.: Call 1-800-950-6264 or visit NAMI.org
UK: Call 0300 5000 927 or visit Rethink: Schizophrenia
Australia: Call 1800 18 7263 or visit Sane Australia
Canada: Visit Schizophrenia Society of Canada for links to regional societies that offer helplines and local services
India: Call the Vandrevala Foundation Helpline at 1860 2662 345 or 1800 2333 330
Last updated: December 5, 2022
Jobs for people with schizophrenia
Jobs for people with schizophrenia - how to get by Until recently, there was a stereotype that a person with any mental illness is doomed to be isolated from society. But the result of effective treatment from the specialists of the Korsakov Clinic shows that even people with schizophrenia can get a job and live a full life. Unfortunately, the need for independent earnings is relevant for many patients with mental disorders. The level of state assistance does not always allow you to purchase the necessary medicines and take care of yourself. nine0003
But the result of effective treatment from the specialists of the Korsakov Clinic shows that even people with schizophrenia can get a job and live a full life. Unfortunately, the need for independent earnings is relevant for many patients with mental disorders. The level of state assistance does not always allow you to purchase the necessary medicines and take care of yourself. nine0003
If you have schizophrenia, you can work and earn little money. In this article, we will consider optimal and non-rational activities.
Which activities are not suitable for people with mental disorders
Some professions are not suitable for people with disorders of the nervous system. For example, disruption of jet lag while performing work duties can cause complications. This applies to those professions where the main working time falls at night, when the body must sleep and rest. nine0003
Stress and other emotional stress are contraindicated for people with schizophrenia.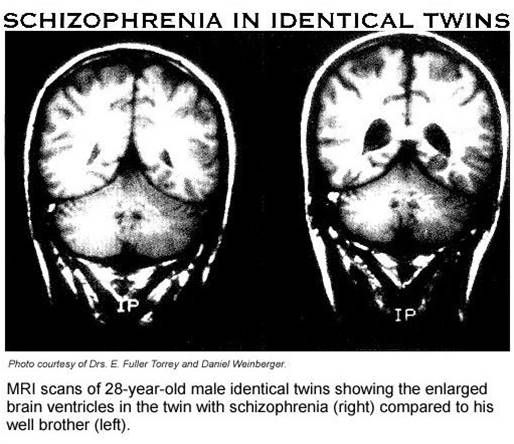 Therefore, it is necessary to avoid any conflicts and stressful situations. This also applies to cases when the patient needs to concentrate his attention. The professions of a driver of any type of transport, driver or operator are not suitable for people with malfunctions in the nervous system.
Therefore, it is necessary to avoid any conflicts and stressful situations. This also applies to cases when the patient needs to concentrate his attention. The professions of a driver of any type of transport, driver or operator are not suitable for people with malfunctions in the nervous system.
Many safety regulations prohibit people with schizophrenia from accessing weapons of any type (cold, pneumatic, gas and firearms). Therefore, this limits the range of professions available to patients in a psychiatric clinic. nine0003
What professions are allowed if you have a diagnosis of schizophrenia
Quiet professions, without physical and emotional stress, are suitable for people with some mental disorders. For example, working as a librarian, janitor, yard keeper, repairman, artist, or craftsman. Serving specialties in this case should involve a slight contact of a person with people who can cause irritable emotions. nine0003
What difficulties arise when looking for a job
A big problem is the negative stereotypical perception of a person with a certificate of schizophrenia.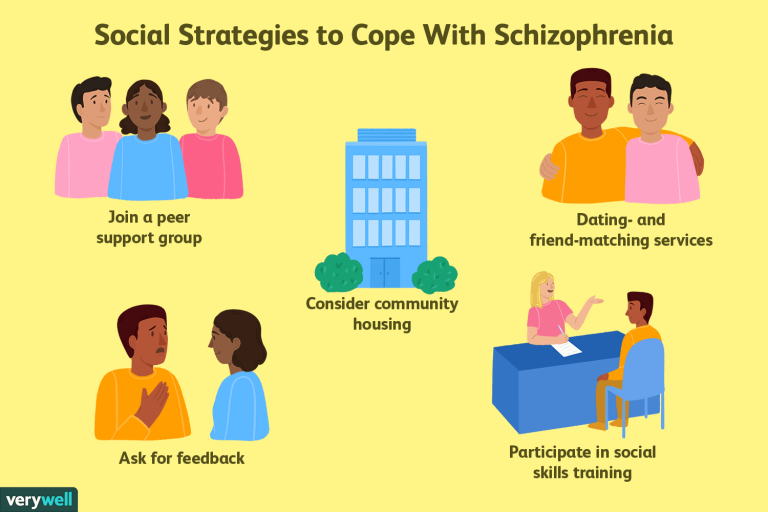 You should immediately look for a job that allows people with disabilities. Usually on the Internet, on job sites, such vacancies are marked with a special sign. And at the labor exchange it is necessary to request a choice of advertisements in which the employer allows the involvement of people with certain deviations.
You should immediately look for a job that allows people with disabilities. Usually on the Internet, on job sites, such vacancies are marked with a special sign. And at the labor exchange it is necessary to request a choice of advertisements in which the employer allows the involvement of people with certain deviations.
It is important to understand that mild schizophrenia, in which a person is not protected from society, allows working with people. People with this diagnosis can freely communicate with others, listen and hear them, and perform their duties. If the problem in the psyche is accompanied by non-standard behavior, then you should choose a profession with a distance from society. For example, a cleaner or caretaker of the territory. Despite the low status of such a position, a person with a disability can receive a stable salary. nine0003
There are many examples of people with schizophrenia becoming famous and rich people who were respected and revered.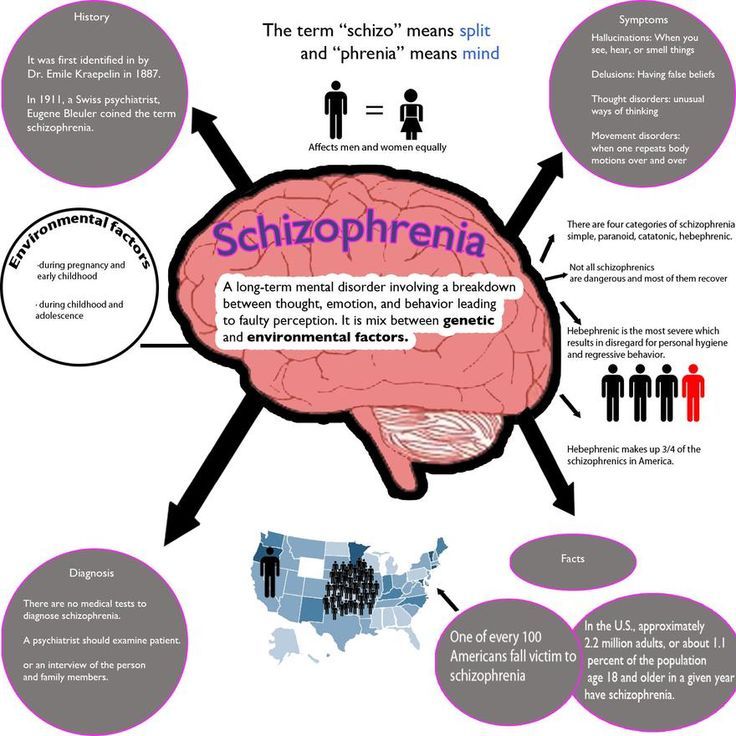 The most striking example is the artist Vincent van Gogh, as well as the mathematician John Forbes Nash, who was awarded the Nobel Prize.
The most striking example is the artist Vincent van Gogh, as well as the mathematician John Forbes Nash, who was awarded the Nobel Prize.
The main thing is to start treatment in a timely manner and strive for work that will bring benefits and financial support.
Reviews
Pavel nine0003
is now in a similar situation! need to look for a job!
reply to feedback
Nadezhda Anatolyevna
My son is diagnosed with ordinary schizophrenia. He is registered. How can he get a job without having a certificate of disability? . Disability removed in 2013 before that was on disability since 2001. Disabled since childhood.
Disabled since childhood.
reply to feedback nine0003
Popular articles
2020-01-29 11:28:03
How to stop feeling sorry for yourself
One of the most common questions for a psychotherapist is how to stop feeling sorry for yourself and learn to live "to the fullest"....
More nine0003
2018-07-25 10:24:34
How to deal with postpartum depression?
Many mistakenly believe that a joyful event never leads to depression.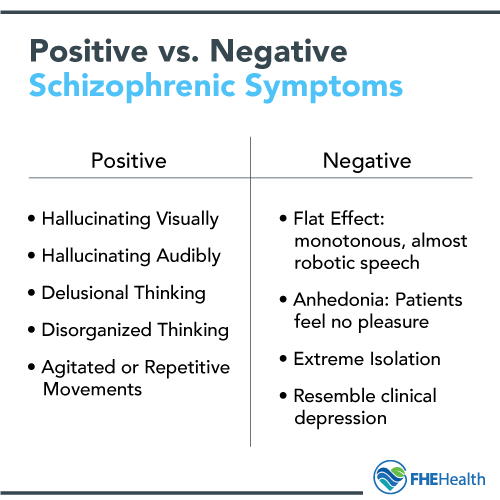 Official statistics say: from 10 to 15% of newly minted m...
Official statistics say: from 10 to 15% of newly minted m...
More nine0003
2020-11-12 11:41:29
What is procrastination
Often, a modern person, regardless of age, gender and social status, postpones the solution of important tasks on the back burner, reassuring ...
More nine0003
X
Reply to review
give feedback
Make an appointment
Ask a Question
X
Ask a question
X
Enroll
X
Leave a review
Schizophrenia and work: who can and cannot work with such a diagnosis?
Schizophrenia imposes certain limitations on a person, as it is chronic, and there is always a risk of relapse.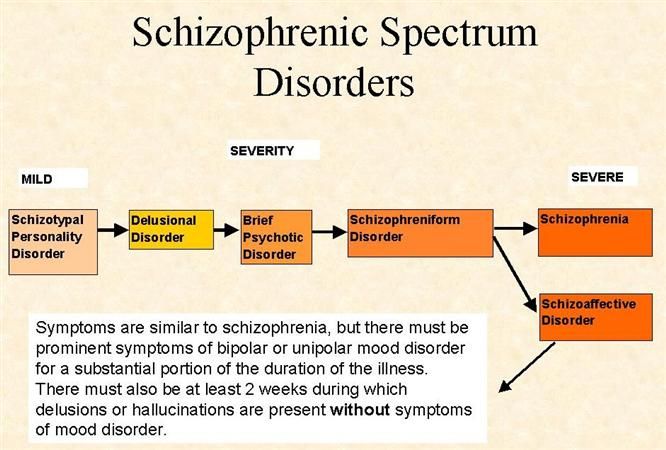 Even if it was possible to stop symptoms for a long time, the diagnosis remains. During the period of exacerbation, a person can be dangerous to himself and others. But at the same time, you can’t put an end to it. He has a high chance of living a fulfilling life. We will find out how compatible schizophrenia and work are, and what type of activity to choose for a patient with such a disease. nine0096
Even if it was possible to stop symptoms for a long time, the diagnosis remains. During the period of exacerbation, a person can be dangerous to himself and others. But at the same time, you can’t put an end to it. He has a high chance of living a fulfilling life. We will find out how compatible schizophrenia and work are, and what type of activity to choose for a patient with such a disease. nine0096
In this article
- About schizophrenia
- Employment problem
- Main contraindications
- Who can work
- Employment as a teacher
- Disability removal
- Why you need to work
About schizophrenia
There are about 500 million people with mental disorders worldwide. Approximately 60 million of them have endogenous diseases of the schizophrenic spectrum. Their prevalence in different countries is the same and amounts to 1% with slight deviations in one direction or another. This means that 1 in 100 people have schizophrenia.
This means that 1 in 100 people have schizophrenia.
Pathology is manifested, as a rule, at a young age, and sometimes in early childhood. But often it manifests between the ages of 15 and 25. The incidence in men and women is the same, but in the latter, symptoms appear somewhat later than in the former - 5-7 years after the onset of the disease.
Schizophrenia is one of the most unusual and mysterious psychopathologies. Scientists have not yet established its true causes and are not able to give a 100% forecast regarding its development. The disease is very insidious and unpredictable. In some patients, it causes a complete disintegration of the personality, as a result of which they completely lose touch with reality, while others can live with this pathology and lead a normal life. nine0003
This is due to the fact that schizophrenia can take different forms, each of which has its own symptoms.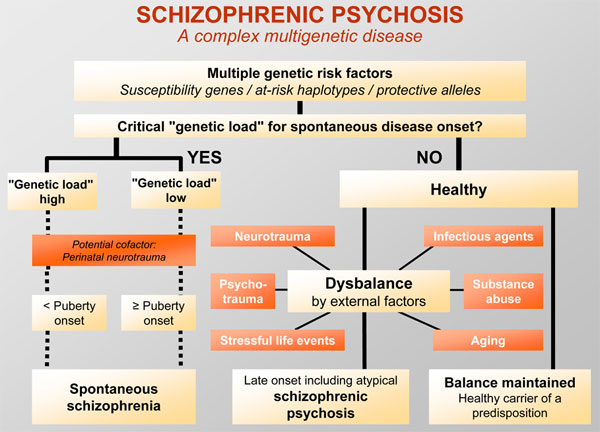 In general, they are divided into two groups: negative and positive. The first are characterized by the passivity of the psyche. A person in this state is apathetic, lack of initiative and indifferent. He strives for loneliness, breaking off social contacts and silence.
In general, they are divided into two groups: negative and positive. The first are characterized by the passivity of the psyche. A person in this state is apathetic, lack of initiative and indifferent. He strives for loneliness, breaking off social contacts and silence.
Productive symptoms are accompanied by mental activity, when patients see hallucinations and crazy ideas come to their minds. Such periods are called attacks or exacerbations, during which a person can be dangerous to himself and others. nine0003
Employment problem
The complexity of the course and the consequences of the pathology are determined by the form of the course. So, paranoid and hebephrenic develop rapidly and lead to a persistent schizophrenic defect. Sluggish or neurosis-like develop over the years and does not always cause changes in personality.
Sometimes patients recover quickly and return to normal. Others need long-term rehabilitation. Moreover, some have long remissions, and some relapse almost every year. The problem is that any factor can provoke an attack, including a conflict at work, an industrial injury or dismissal. nine0003
Moreover, some have long remissions, and some relapse almost every year. The problem is that any factor can provoke an attack, including a conflict at work, an industrial injury or dismissal. nine0003
In some cases, a person, after going into remission, returns to normal life. Severe patients are assigned a disability of the second or third degree. At the same time, the issue of employment is a priority for many patients. Benefits are not so big, and therefore it is almost impossible to feed yourself at the expense of the state. Therefore, work is important for schizophrenics no less than for other people.
However, there are stereotypes in society regarding people with mental disorders. They are perceived as inadequate, uncontrollable, and most importantly, dangerous. Not every employer is willing to hire a person with schizophrenia. It should be borne in mind that it can develop at the age when the patient has already managed to learn and get a profession. nine0003
nine0003
Approximately 65% of patients with schizophrenic disorders have higher education.
People with schizophrenia, as well as their relatives, should be aware that this diagnosis does not always interfere with work. Moreover, under favorable circumstances, a schizophrenic can earn good money and lead a decent lifestyle.
Major contraindications
First of all, you need to remember about legal restrictions. People with mental disabilities of any type are prohibited from working as security guards and military personnel, as they are not allowed to use weapons. Also, people with schizophrenia are not hired by firefighters, police officers, bailiffs, etc. Usually, to get such a job, you need to go through a medical commission, which will include a visit to a psychiatrist. Since the diagnosis is made for life and it is impossible to erase it from the medical history, the doctor will not give access to production.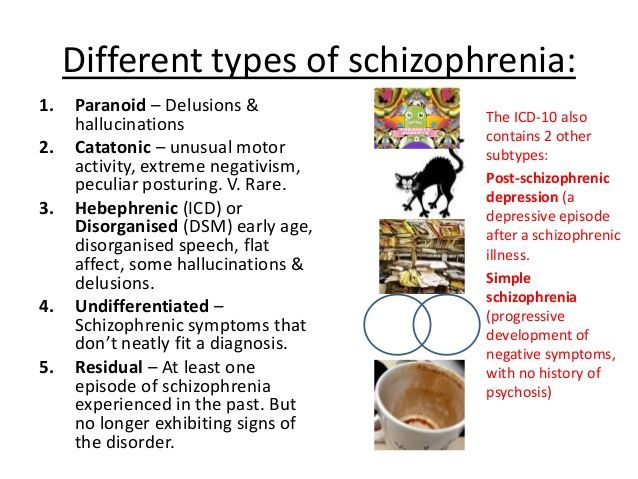 nine0003
nine0003
The following activities are also not recommended for people with schizophrenia:
- Work with a floating schedule and night shifts. Confused biorhythms are potentially dangerous for schizophrenics. They are not even recommended to travel across multiple time zones. It is advisable to sleep at night for 7.5 hours a day.
- Work with high physical or emotional stress. In an enterprise in which activities take place in a rush mode, there is usually too much fuss and conflict. It is better for a person with schizophrenia to avoid this, otherwise the psyche will begin to get tired and sooner or later will fail. nine0102
- Work with a large number of social contacts. Schizophrenics are often reserved people. As a rule, this disease develops in schizoids who do not like to communicate a lot. But after the diagnosis is made, it is not contraindicated to communicate with society. Moreover, a secluded lifestyle is more likely to be harmful to the patient.
 However, it will be difficult for the psyche to withstand a huge number of contacts, so it is advisable to choose a job that is calm and without a large flow of people.
However, it will be difficult for the psyche to withstand a huge number of contacts, so it is advisable to choose a job that is calm and without a large flow of people. - Work related to teaching. A person with schizophrenia cannot teach children. If a pathology is detected in a teacher, he will have to retrain. nine0102
- Work that is associated with danger - electricity, gas, oil, etc. Such activities, in principle, are traumatic even for healthy people. A schizophrenic, hypothetically, can create a dangerous situation not only for himself, but also for others.
- Work related to the plot of the patient's delusional ideas, if during the attack he had systematized delirium. For example, a person worked in the subway and it seemed to him that aliens were hiding underground. It is clear that it is better for him not to go down to the "subway" at all, especially for work. nine0102
It is difficult to list all the professions for schizophrenics within the framework of the article. In addition, you need to build on each specific case. It must be understood that a person with schizophrenia cannot take responsibility for other people. First, not the fact that he is able to withstand it. Secondly, it is unlikely that an employer will entrust his employees to a patient with a schizophrenic disorder.
In addition, you need to build on each specific case. It must be understood that a person with schizophrenia cannot take responsibility for other people. First, not the fact that he is able to withstand it. Secondly, it is unlikely that an employer will entrust his employees to a patient with a schizophrenic disorder.
Who can work
Where a patient with schizophrenia can find a job depends on the presence or absence of a disability and its group. There are two of them - the second and the third. The third is the easiest, as it is characterized by a stable remission. Any activities other than those previously listed are available. However, you still have to consult a psychiatrist to discuss the nuances. Perhaps he himself will offer the patient certain professions. nine0003
In the second group of disability, it is recommended to choose a quiet job. It is desirable that it be monotonous or even manual. Quite often, patients are arranged at neuropsychiatric dispensaries to keep them under observation.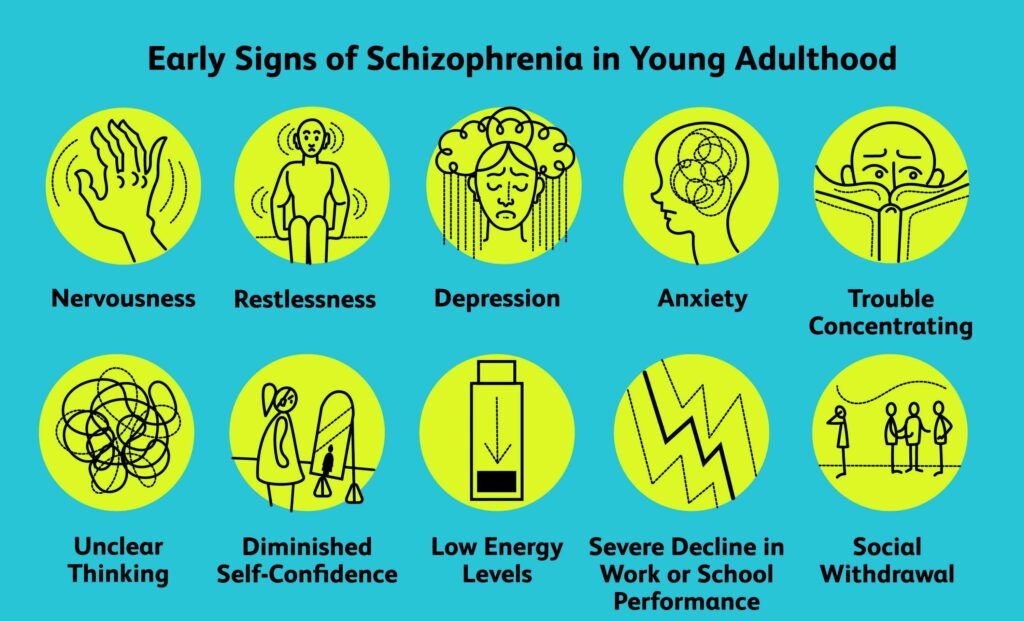 Salaries, of course, are small, but a person earns money himself, which psychologically helps to better cope with the disease.
Salaries, of course, are small, but a person earns money himself, which psychologically helps to better cope with the disease.
Wherever a person with schizophrenia works, he will have to follow the rules: both those prescribed by the doctor and those prescribed by the employer. nine0145
Disability is not assigned to all people with schizophrenia. This has both pluses and minuses. Among the disadvantages is the lack of a pension, and the advantage is that the list of professions is more diverse. Suitable for this case:
- librarian;
- archive worker;
- secretary;
- accountant;
- shoemaker;
- editor; nine0101 gardener, etc.
Today, many people choose to work from home, especially professionals who do not need to communicate with people offline.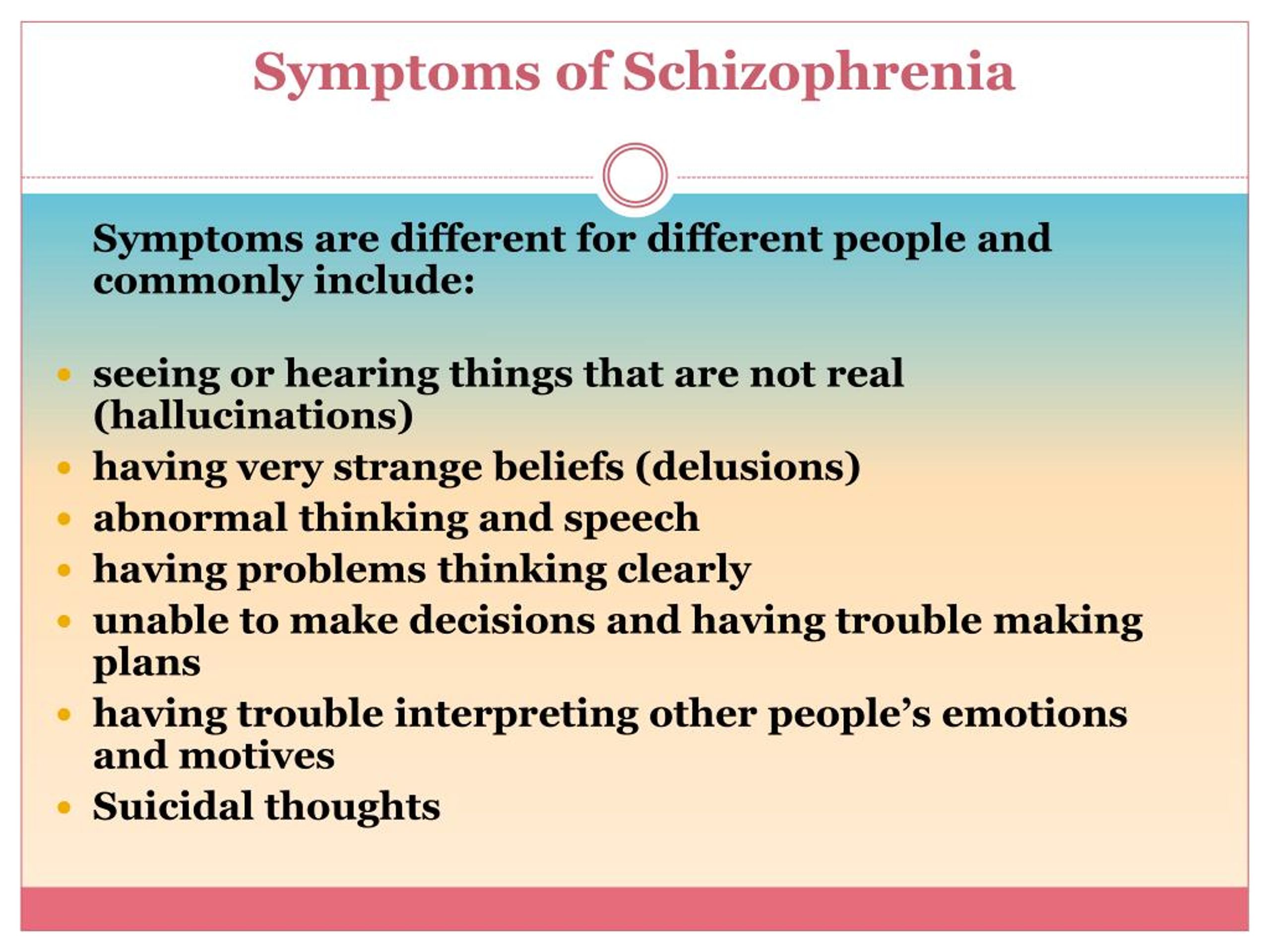 With schizophrenia, you can remotely engage in almost any legal activity. There are restrictions, but they are more related to the daily routine, workload and other organizational issues. Appropriate recommendations should also be given by the attending physician.
With schizophrenia, you can remotely engage in almost any legal activity. There are restrictions, but they are more related to the daily routine, workload and other organizational issues. Appropriate recommendations should also be given by the attending physician.
Work as a teacher
A common question in this context is related to the possibility of teaching in schizophrenia. A person with such a diagnosis cannot go to school, since any teacher undergoes a medical examination, including a psychiatrist. In universities and colleges, the employment system is much simpler. Hypothetically, you can get a job as a teacher in a vocational school, but only by hiding your illness. This will be considered as an offense entailing certain liability. nine0003
Removal of disability
With a stable remission, the patient can submit documents to a medical institution for the removal of disability. You will have to go to the hospital for a full examination, and for several weeks.