How to support someone with ptsd
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.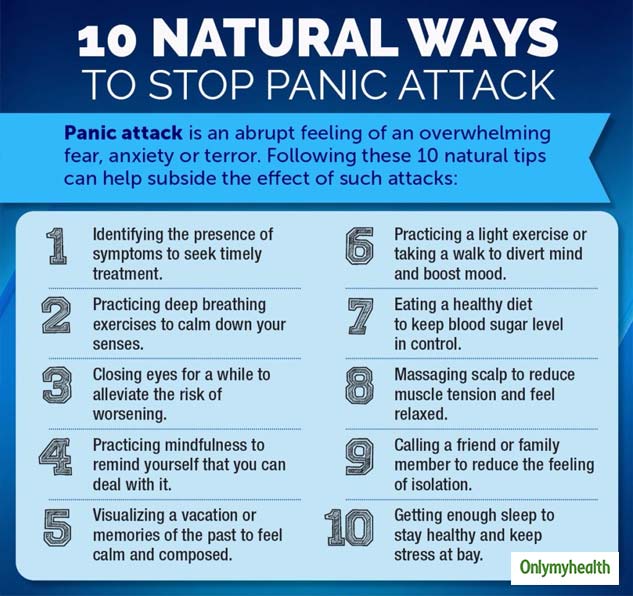
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Recovery and Recovery Support | SAMHSA
Recovery and Resilience
Resilience refers to an individual’s ability to cope with change and adversity. Resilience develops over time and gives an individual the capacity not only to cope with life’s challenges but also to be better prepared for the next stressful situation. Psychological resilience, the ability to cope with adversity and to adapt to stressful life events, varies widely from person to person and depends on environmental as well as personal factors. It refers to positive adaptation, or the ability to maintain mental and physical health despite participating in stressful situations. Resilience is playing up those protective factors so they can outweigh the risk factors. Optimism and the ability to remain hopeful are essential to resilience and the process of recovery.
Because recovery is a highly individualized process, recovery services and supports must be age appropriate and offered over the life course and flexible enough to ensure cultural relevancy. What may work for adults in recovery may be very different for youth or older adults in recovery. For example, the promotion of resiliency in young people, and the nature of social supports, peer mentors, and recovery coaching for adolescents and transitional age youth are different than recovery support services for adults and older adults.
What may work for adults in recovery may be very different for youth or older adults in recovery. For example, the promotion of resiliency in young people, and the nature of social supports, peer mentors, and recovery coaching for adolescents and transitional age youth are different than recovery support services for adults and older adults.
Recovery and Relationships
The process of recovery is supported through relationships and social networks. This often involves family members who become the champions of their loved one’s recovery. They provide essential support to their family member’s journey of recovery and similarly experience the moments of positive healing as well as the difficult challenges. Families of people in recovery may experience adversities in their social, occupational, and financial lives, as well as in their overall quality of family life.
These experiences can lead to increased family stress, guilt, shame, anger, fear, anxiety, loss, grief, and isolation. The concept of resilience in recovery is also vital for family members who need access to intentional supports that promote their health and well-being. The support of peers and friends is also crucial in engaging and supporting individuals in recovery.
The concept of resilience in recovery is also vital for family members who need access to intentional supports that promote their health and well-being. The support of peers and friends is also crucial in engaging and supporting individuals in recovery.
Peer support assists individuals to engage or stay connected to the recovery process through a shared understanding, respect, and mutual empowerment. Peer support extends beyond the reach of clinical treatment into the everyday environment providing non-clinical, strengths-based support. This relationship can help lay the foundation for SAMHSA’s four dimensions of recovery.
Recovery Support
SAMHSA advanced recovery support systems to promote partnering with people in recovery from mental and substance use disorders and their family members to guide the behavioral health system and promote individual, program, and system-level approaches that foster health and resilience; increase housing to support recovery; reduce barriers to employment, education, and other life goals; and secure necessary social supports in their chosen community.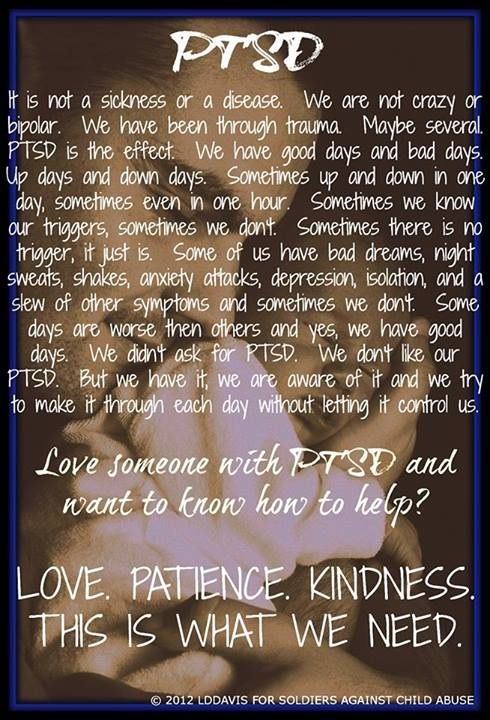
Recovery support is provided in various settings. Recovery support services help people enter into and navigate systems of care, remove barriers to recovery, stay engaged in the recovery process, and live full lives in communities of their choice.
Recovery support services include culturally and linguistically appropriate services that assist individuals and families working toward recovery from mental and/or substance use problems. They incorporate a full range of social, legal, and other services (PDF | 409 KB). that facilitate recovery, wellness, and linkage to and coordination among service providers, and other supports shown to improve quality of life for people (and their families) in and seeking recovery.
Recovery support services may be provided before, during, or after clinical treatment, or may be provided to individuals who are not in treatment but seek support services.
These services, provided by professionals and peers, are delivered through a variety of community and faith-based groups, treatment providers, schools, and other specialized services.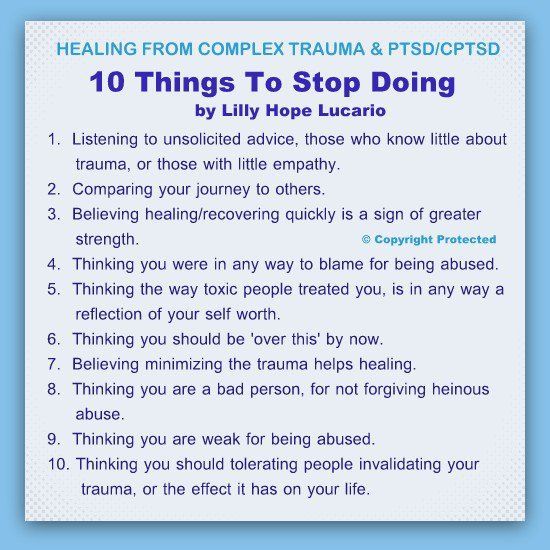 The broad range of service delivery options ensures the life experiences of all people are valued and represented.
The broad range of service delivery options ensures the life experiences of all people are valued and represented.
For example, in the United States there are 34 recovery high schools that help reduce the risk in high school environments for youth with substance use disorders. These schools typically have high retention rates and low rates of students returning to substance use.
Additionally, SAMHSA's Bringing Recovery Supports to Scale Technical Assistance Center Strategy (BRSS TACS) advances effective recovery supports and services for people with mental or substance use disorders and their families.
Find more Publications and Resources on Recovery and Recovery Support.
What is PTSD and how to get rid of it
April 14 Likbez Health
It is possible to maintain a healthy mind even after a disaster. What is PTSD? Initially, the diagnosis was made to those who had been in the war, but PTSD can develop in anyone. nine0003
Most people feel anxious, sad, angry or irritated after a traumatic event.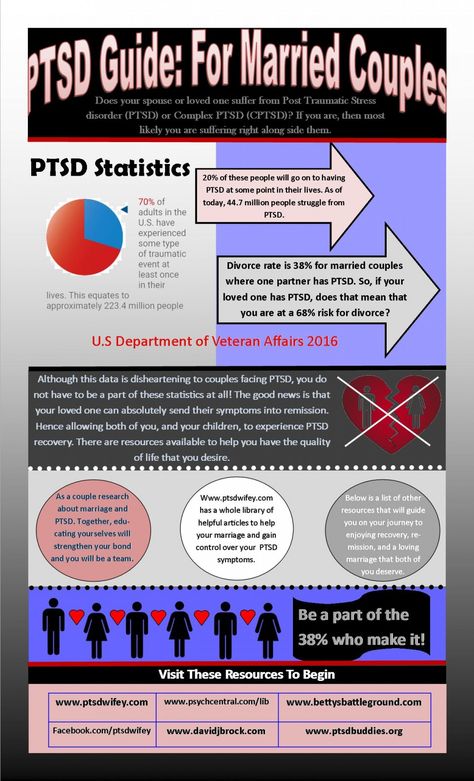 They have insomnia and constant fatigue. This is a normal reaction to a threat to life and health, a feeling of helplessness and loss of control over what is happening. But after a month, these manifestations, as a rule, weaken and people return to normal life.
They have insomnia and constant fatigue. This is a normal reaction to a threat to life and health, a feeling of helplessness and loss of control over what is happening. But after a month, these manifestations, as a rule, weaken and people return to normal life.
If the symptoms do not subside, the person continues to be tormented by memories and nightmares, we can talk about the development of post-traumatic stress disorder. According to the WHO, it needs treatment 9% of those who experienced something terrible. At the same time, women suffer from PTSD 2.5 times more often than men, although men face more dangerous situations.
PTSD cannot be left untreated. The disorder spoils personal, social, work relationships, interferes with daily tasks.
Why PTSD occurs
It is not known exactly why a stress disorder develops in certain people. But there are factors that increase the risks:
- The nature of the injury. The stronger and longer the stress, the higher the likelihood of PTSD.
 nine0022
nine0022 - Previously experienced psychological trauma. For example, childhood abuse.
- Heredity. Those with relatives who have had anxiety disorders or depression are more at risk.
- Work or hobbies associated with constant stress or danger to life.
- Presence of other mental disorders.
- Temperament and how the brain regulates hormones and other chemicals that are released in response to stress.
- Lack of support from loved ones after an injury. nine0022
- Frequent use of alcohol and other psychoactive substances.
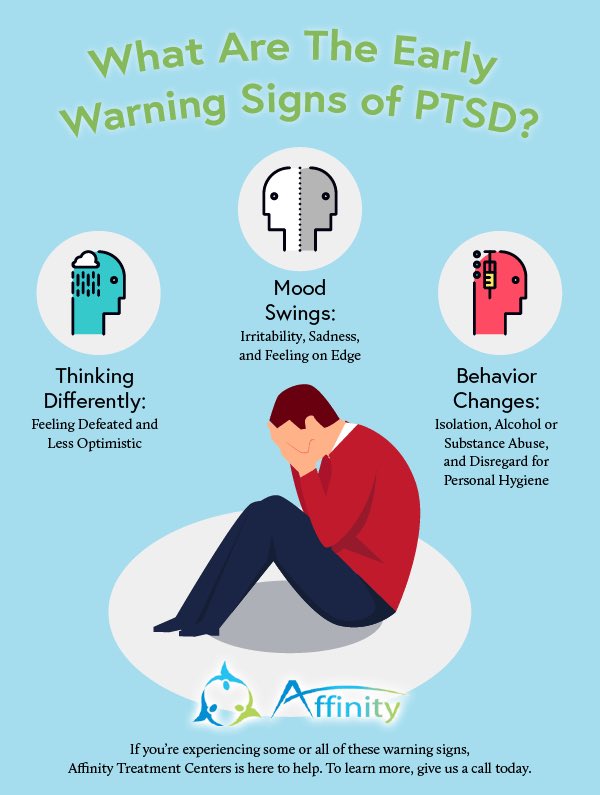
How PTSD manifests itself
Symptoms of PTSD are more often detected within a month after the event, but sometimes they are not noticed until several years later. This can happen against the background of new stress or an accidental reminder of the experience.
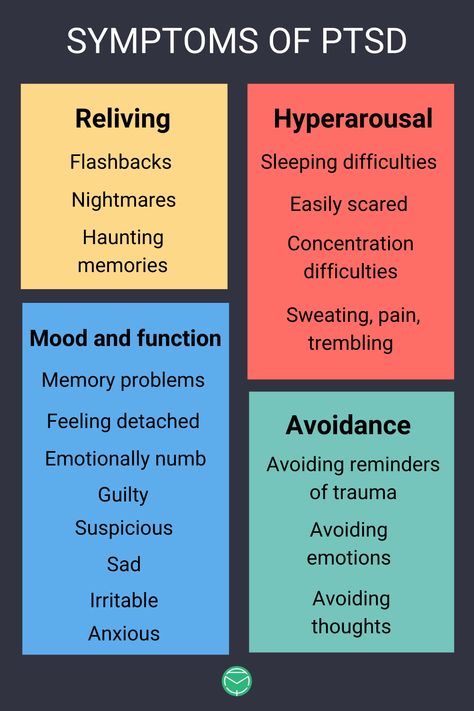
Symptoms can be divided into four main groups.
Obsessive memories and dreams
- A person cannot forget and constantly replays what happened in his head.
 nine0022
nine0022 - He has nightmares that make him afraid to go to bed.
- Any reminder of an event causes strong emotions or physical manifestations. For example, after a car accident, the victim reacts to a car signal with shaking in the hands or a sharp attack of fear.
Avoidance
- The victim is constantly trying to forget about the experience, it takes a lot of strength and energy.
- He diligently avoids places or people that can remind him of something terrible. For example, after the death of a loved one, a person may refuse to meet with other relatives so as not to talk about the deceased. nine0022
- Gives up favorite activities if they have something to do with what happened. A girl who survived an attack in the stairwell may refuse to train after work because she is afraid to return home in the evening.
Changes in mood and thinking
- Negative thoughts about yourself, other people or the world appear.
- Haunted by a feeling of hopelessness.
 There are no goals in life and the desire to change something.
There are no goals in life and the desire to change something. - There are memory problems. Sometimes it is not possible to remember important details of the traumatic event. nine0022
- It becomes difficult to communicate with loved ones, maintain relationships.
- Loss of interest in hobbies or meeting friends.
- The victim is not able to rejoice or grieve, only detachedly observes life from the outside.
Changes in physical and emotional reactions
- A person constantly feels a threat to life and seeks to protect himself by any means.
- Often feels guilty or ashamed. Thinking about how it could have been avoided. nine0022
- Loss of concentration, difficulty working or just reading a book.
- The victim may be short-tempered and aggressive.
- Sleep problems appear.
- Man unconsciously strives for self-destruction. For example, he drinks a lot or ignores traffic rules.
Symptoms may increase or decrease, appear only with new stress or a reminder of a terrible event. The victim himself may not associate problems with sleep or concentration with the trauma experienced, especially if a lot of time has passed. But at the same time, constant stress interferes with a normal life. nine0003
The victim himself may not associate problems with sleep or concentration with the trauma experienced, especially if a lot of time has passed. But at the same time, constant stress interferes with a normal life. nine0003
What to do if you have suicidal thoughts
In this case you should immediately seek help:
- 495 625-06-20). They work around the clock.
- Write to a psychologist on the website of the Ministry of Emergency Situations - this is possible without registration.
- Contact your loved ones for support.
How is PTSD treated? The best place to start is to see a therapist. He will check if there are any physical diseases that can cause changes in the psyche. To do this, the doctor will conduct an examination and prescribe the necessary examinations. This could be a chest x-ray, blood tests, or a CT scan of the brain. nine0003
If everything is in order with the body, the therapist will refer you for a consultation with a specialized specialist.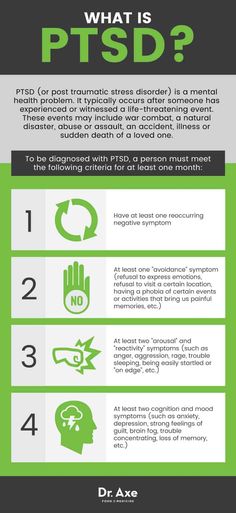 He will determine whether medication is needed or psychotherapy will be enough.
He will determine whether medication is needed or psychotherapy will be enough.
Before meeting with a psychotherapist, prepare a list of symptoms, behavioral changes, or lifestyle changes. At the appointment, ask the specialist about the experience of working with post-traumatic stress syndrome and the number of patients who have overcome it. It is important to ask all the exciting questions at once, because the success of treatment largely depends on the trusting relationship between the patient and the psychotherapist. nine0003
What psychotherapy can be like
According to experts, only psychotherapy can get rid of PTSD. Medicines can only relieve acute manifestations and temporarily improve the quality of life.
Several methods are used to treat PTSD:
- Cognitive therapy . The doctor will analyze the thinking errors and stereotypes that prevent you from returning to normal life after an injury. For example, the thought "I'm bad because they did this to me" will gradually turn into "They did this to me, but that doesn't make me bad.
" The patient will keep a diary and describe in it his condition and reactions to different situations. Gradually, a person will learn to solve problems that were previously beyond his power. nine0022
- Behavioral or exposure therapy . The meaning of the method is to return to a traumatic situation under the control of a psychotherapist. The patient is immersed in the past with the help of video, sounds or verbal description, but the specialist teaches to cope without panic and horror. Over time, memories cease to frighten, it becomes possible to live on without looking back at the trauma.
- EMDR, or EMDR - eye movement desensitization and processing. This method was developed specifically for the treatment of post-traumatic disorders. It is believed that the brain cannot cope with the processing of a stressful event and therefore memories do not go away. In an EMDR session, the patient briefly focuses on the past and at the same time on eye movements or other stimuli: pats, sounds.
 This synchronizes the activity of both hemispheres and helps the brain process painful memories. If the injury was mild, four or five sessions may be enough. nine0022
This synchronizes the activity of both hemispheres and helps the brain process painful memories. If the injury was mild, four or five sessions may be enough. nine0022
What drugs can be prescribed by a doctor
Medications are prescribed at the same time as psychotherapy, if you need to remove the most striking manifestations of the disorder and improve the quality of life before psychotherapy works.
Several groups of drugs are used:
- Antidepressants . May reduce symptoms of anxiety and depression, improve sleep, memory and concentration.
- Mood stabilizers . They are used to reduce impulsivity, anger attacks and to reduce irritability. nine0022
- Antipsychotics . They are prescribed if the shock was too severe and memories and emotions interfere with life.
- Benzodiazepines . Used to reduce severe anxiety and improve sleep. But now they are rarely appointed.
What else can you do
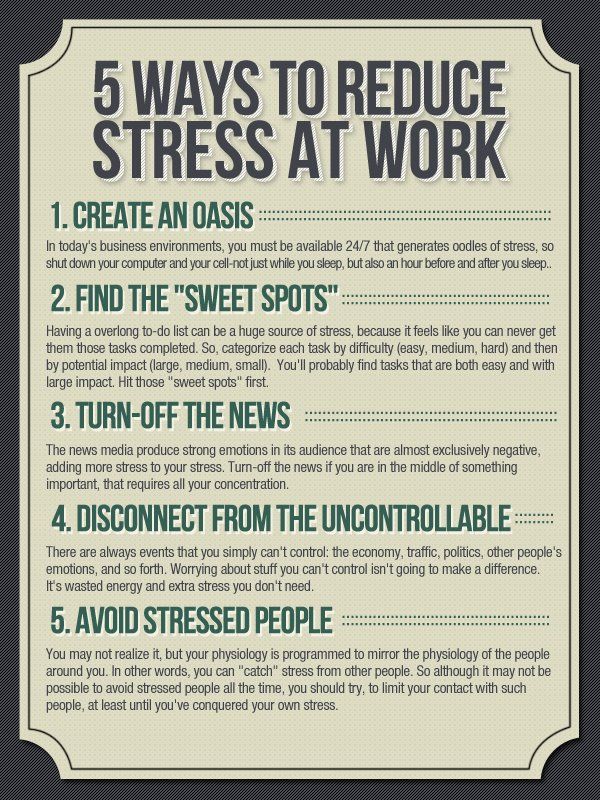
Taking care of yourself helps you get back to normal life faster and easier. For this it is worth:
- Follow the treatment plan, even if it seems that psychotherapy and medications do not help. It takes time to get easier. nine0022
- Find an opportunity for good rest and sports or walks. Physical activity and healthy sleep relax and help to recover.
- Diverse and tasty food. The lack of useful elements can worsen the mental state.
- Reduce or eliminate possible sources of stress. New causes for concern lengthen the treatment.
- Avoid coffee, alcohol and cigarettes. They can increase anxiety.
- Connect with loved ones and meet friends who can support and listen. nine0022
- Find interesting hobbies that will distract from experiences and memories.
How successful is the treatment of PTSD
Everything is individual. The result will depend on the severity of the symptoms, as well as the efforts of the patient and the support of loved ones.
But if you follow all the doctor's recommendations, sooner or later you can be cured and return to normal life.
Moreover, new preparations and methods are constantly appearing. For example, the US Food and Drug Administration recently approved an app to interrupt nightmares. nine0003
How to help a loved one with PTSD
If a relative or friend has PTSD, the most important thing is to help them seek professional help. After all, the victim may inadequately perceive the situation and believe that everything will pass by itself.
Also important:
- Recognize that avoidance and withdrawal are symptoms of a disorder. Do not insist on your help if the person rejects it. Just explain that you are there.
- Be willing to listen. Let your loved one know that you can talk about what happened whenever they want. But do not press, do not force to talk about the injury against your will. nine0022
- Walking together or doing interesting things.
- Plan more meetings, celebrate holidays.
- Take care of yourself. Being close to someone who has experienced something terrible can be difficult. You may experience constant stress, guilt, powerlessness. Therefore, do not forget to restore your resources: rest, eat right, play sports.
- Prepare a safe place to hide if a loved one becomes aggressive. nine0022
Read also 😟🚑💊
- How to recognize hysterical personality disorder and what to do about it
- What is catatonia and why is it dangerous
- How to stop borderline personality disorder from ruining your life
- 12 signs of an anxiety disorder
- 8 tips for those who take everything to heart
Tips on how to help a person with post-traumatic stress syndrome
After the events on Euromaidan, many participants experience post-traumatic stress disorder (PTSD). And this is quite natural, because people lived for three months in suspense, worried about their loved ones, for the country, slept little, worked hard, overcame fear. After that, they experienced shock, saw death very close, lost friends. Were forced to “turn off” feelings in an emergency in order to act and help others. All this does not go unnoticed. Unfortunately, in our countries the system of assistance to people with PTSD is not sufficiently developed and often they are left alone with their painful condition. nine0003
We would like to give some simple tips on how to help people who are survivors and need help. Signs of post-traumatic syndrome: - sleep and appetite disorders, - impaired contact with needs, you do not remember when you last ate, slept, do not notice injuries, cold, dirt, - feeling of tension, anxiety, the body does not relax even in sleep, - flashbacks (pictures of the experience, flashing in the mind against will), - irritability, intolerance to the slightest difficulty, disagreement,
— bouts of guilt, constant replaying of options in the head of what could be done to save the dead — sharp, hard-to-control bouts of anger or despair — dullness, apathy, depression, desire to forget, unwillingness to live
Now watching
In especially severe cases, psychotic episodes may occur, with a loss of adequate perception of reality, as well as suicidal attempts.
If you observe these signs (there may not be all, but only some) in yourself or your loved ones, pay close attention to this. This condition is not only very painful, but also quite harmful to health and to the situation as a whole. Do not tolerate or ignore the problem, ask for help and provide assistance. How can you help a person with PTSD: - Basic care: feed, persuade to rest and sleep, it is very important - warmth, warm food, drink, bed, clothes, bath. - Body contact: hold the hand, hug, stroke, be near, but do not disturb. - Contact with nature: sit in the sun, look at water, fire, sky, smell grass, earth, touch wood, stone. - Simple, familiar activity, best with a specific clear result and with the content of "putting things in order, reconnecting, taking care of yourself and others": cleaning, working on the ground, doing housework, taking apart, sorting something. - Participate in rituals, especially joint rituals, farewell to the dead, commemoration, in the creation of commemorative signs, in joint prayers.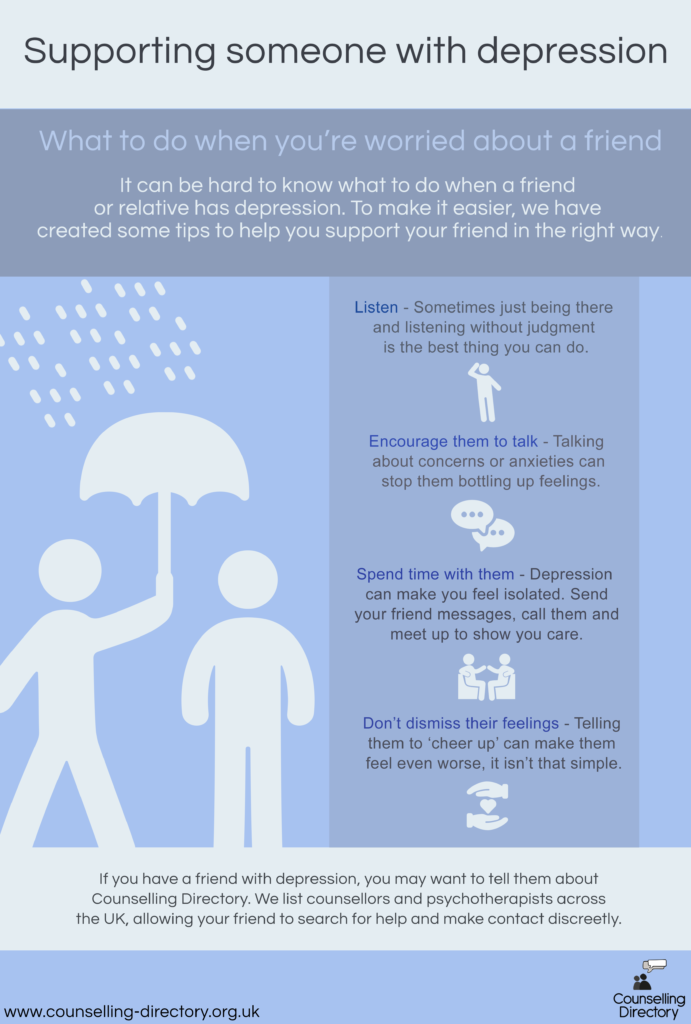 - Do not be silent, do not restrain your feelings: cry if you want, write, speak, complain, tell about your experience to everyone who is ready to listen, and, accordingly, listen if they tell you. In no case should you go straight to consolations or calls to “do not get upset, pull yourself together”, do not freeze grief with formulas like “heroes do not die”. They are dying, it hurts, and the pain must have an outlet. - If right now there is no opportunity to speak, cry, receive support, it is better on the contrary, to consciously block memories and thoughts about the experience, not to allow yourself to be “pulled” into the funnel of trauma, be distracted, switch, do something, sing, pray - but later give the will to feelings, as soon as there are conditions for support, close people are nearby. - Be extremely careful with such "sedatives" as alcohol. Small doses taken once can help to relax, but alcohol is a depressant, it depletes an already exhausted psyche, with regular use it worsens the course of the syndrome - Seek help from psychologists and doctors (an ordinary neuropathologist or therapist will do), in severe conditions take sedative drugs, this is not weakness, but self-care.
- Do not be silent, do not restrain your feelings: cry if you want, write, speak, complain, tell about your experience to everyone who is ready to listen, and, accordingly, listen if they tell you. In no case should you go straight to consolations or calls to “do not get upset, pull yourself together”, do not freeze grief with formulas like “heroes do not die”. They are dying, it hurts, and the pain must have an outlet. - If right now there is no opportunity to speak, cry, receive support, it is better on the contrary, to consciously block memories and thoughts about the experience, not to allow yourself to be “pulled” into the funnel of trauma, be distracted, switch, do something, sing, pray - but later give the will to feelings, as soon as there are conditions for support, close people are nearby. - Be extremely careful with such "sedatives" as alcohol. Small doses taken once can help to relax, but alcohol is a depressant, it depletes an already exhausted psyche, with regular use it worsens the course of the syndrome - Seek help from psychologists and doctors (an ordinary neuropathologist or therapist will do), in severe conditions take sedative drugs, this is not weakness, but self-care.