How to make someone understand depression
SAMHSA’s National Helpline | SAMHSA
Solr Mobile Search
Share Buttons
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Solr Mobile Search
Share Buttons
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers. The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
- Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.
 4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk.
 They Hear You.
They Hear You. - Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
- Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses.
 The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States - The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month. The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
- Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.
 4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH) - Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medications for Substance Use Disorders
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated
Last Updated: 03/22/2023
How to behave with a person with depression. Instructions - Meduza
Depression is one of the most common mental disorders: according to the World Health Organization as of February 2017, more than 300 million people worldwide suffer from it. The scale of the problem in Russia is harder to assess. Experts talk about almost eight million Russians suffering from depression, but specify that, most likely, there are much more of them - people with depression often do not seek help because of shame or unwillingness to admit the seriousness of their condition. Depression can be underestimated not only by the patients themselves, but also by their relatives. At the request of Meduza, the author of the remain_nameless telegram channel about mental health, Daria Chagina, tells how to properly behave with a person suffering from depression, so as not only not to harm him, but also to help.
Depression can be underestimated not only by the patients themselves, but also by their relatives. At the request of Meduza, the author of the remain_nameless telegram channel about mental health, Daria Chagina, tells how to properly behave with a person suffering from depression, so as not only not to harm him, but also to help.
Recognize the importance of the problem
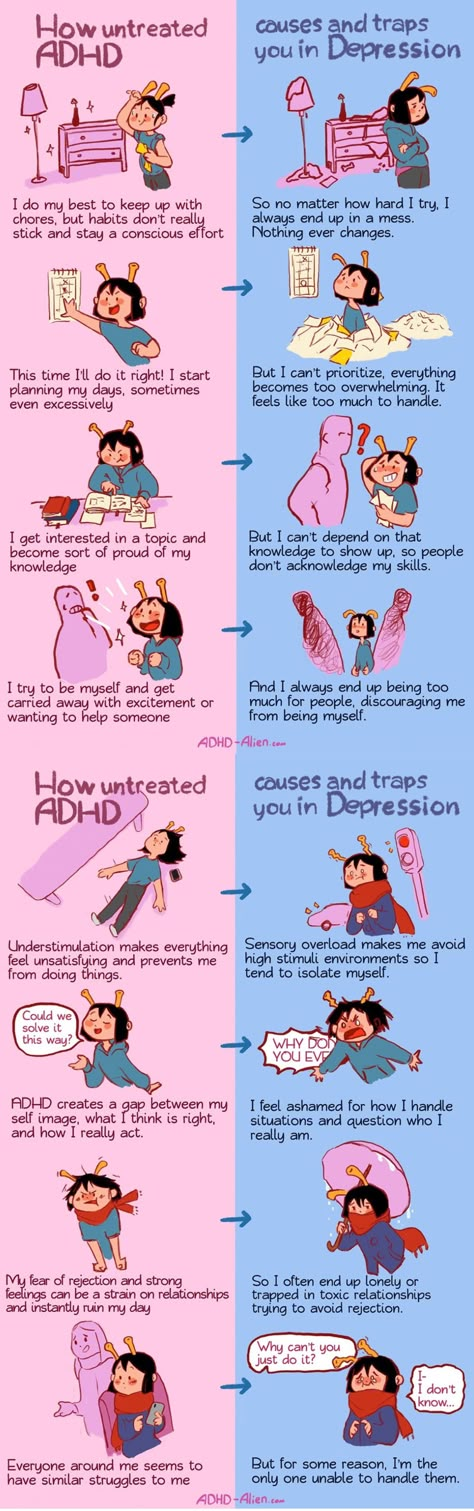
Pop culture has taught us that depression is a kind of seasonal blues: many of us have heard (or said) "I'm depressed today." Of course, any person experiences bouts of melancholy and depression - due to lack of sleep, problems at work, a quarrel with a loved one, and even bad weather. But as soon as the surrounding circumstances change, everything returns to normal. Depression, on the other hand, is arranged differently: its causes can be deeply hidden, it greatly affects a person’s life, and only in 40% of cases goes away on its own - and even then not completely.
Depression is expressed primarily in a constant depressed state, chronic fatigue and loss of interest in things that used to please. In addition, the disease can be accompanied by various somatic manifestations: a person either suffers from insomnia, or, conversely, constantly wants to sleep. Doesn't want sex. He cannot concentrate on anything and loses his ability to work. Loses appetite or, conversely, begins to overeat. Depression can also lead to a complete loss of interest in life, a suicidal state and suicide. The diagnosis is made if the duration of symptoms is at least two weeks - but depression can last for months or even years, and it must be treated.
In addition, the disease can be accompanied by various somatic manifestations: a person either suffers from insomnia, or, conversely, constantly wants to sleep. Doesn't want sex. He cannot concentrate on anything and loses his ability to work. Loses appetite or, conversely, begins to overeat. Depression can also lead to a complete loss of interest in life, a suicidal state and suicide. The diagnosis is made if the duration of symptoms is at least two weeks - but depression can last for months or even years, and it must be treated.
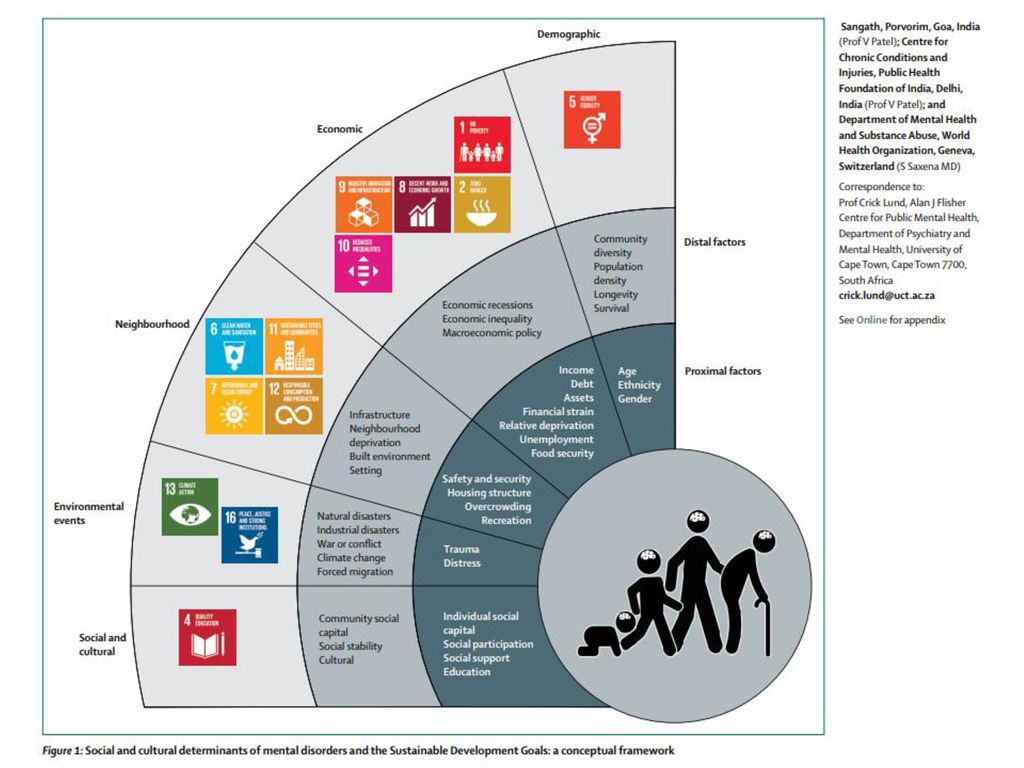
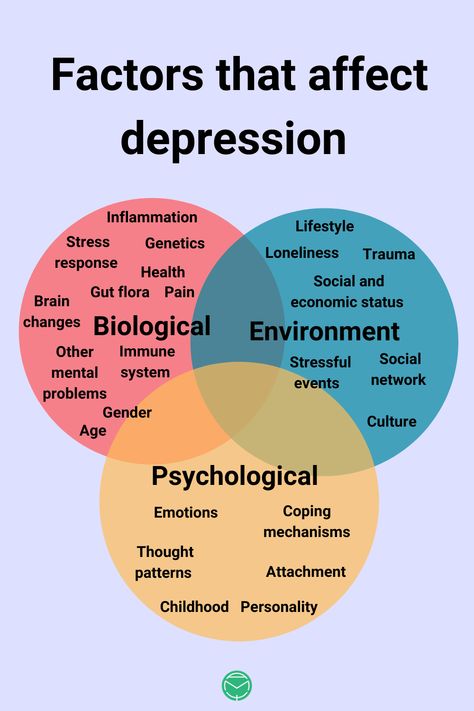
Risk factors for depression can range from psychological shocks or trauma, dysfunctional family situations or lack of parental love, as well as genetic predisposition or various diseases, as well as alcohol or drug use. Moreover, psychogenic depression (caused, for example, by the death of a loved one, divorce or violence) does not necessarily come immediately - people experience difficult events in different ways, and sometimes the reaction to them comes with a delay.
Show that you are there
Depressed people don't just feel lonely, they often feel ashamed and guilty about their feelings and emotions. For fear of being misunderstood, ridiculed, or rejected, they prefer to remain silent about their experiences, do not seek help, or refuse to acknowledge the seriousness of their situation. Left alone with their feelings, many try to suppress and hide them - and only more convinced of their own "abnormality", worthlessness and uselessness. As studies confirm, it is this feeling of separation from other people that can lead to suicidal thoughts - therefore, the support of relatives and friends is especially important for depressed people. Make it clear that you are there no matter what, the person’s condition does not affect your attitude towards him in any way, you understand the depth of his suffering and are ready to help.
Do not discount the feelings and experiences of a depressed person
If you have never had depression, then you are unlikely to be able to fully understand the state of your loved one.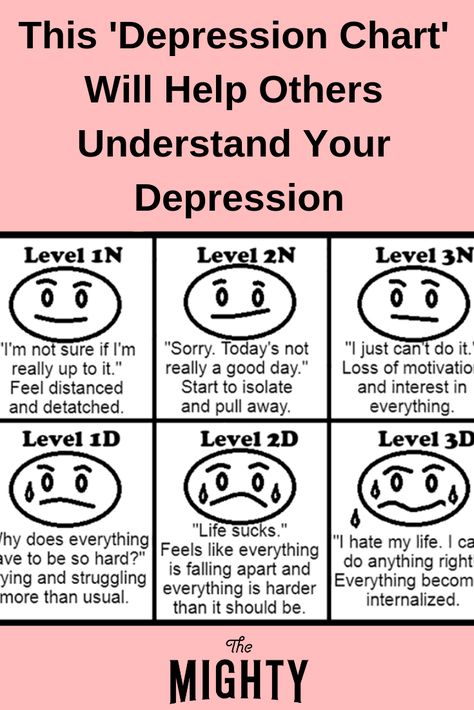 Do not try to compare it to a "bad day" or just a difficult period in life (for example, a session or a job change) and do not offer a person with depression to "pull themselves together" or "tune in to positive." Even if you sincerely want to express support, such advice will only devalue the feelings of a person who is faced with depression, because he knows that everything is not so simple. People in this situation often hear, “Others have worse problems than you”, “It’s all in your head”, “Do something useful”, but all this only causes more shame, guilt or annoyance due to helplessness in the face of illness. Hearing something like this, a person may conclude that you will never understand him, and close up - then it will be much more difficult to help. If you don’t know what to say in such a situation (and this is normal), just hug, say: “I can’t even imagine what you are experiencing right now, but I see that it is very difficult” - and let the person show feelings in the way he it's necessary.
Do not try to compare it to a "bad day" or just a difficult period in life (for example, a session or a job change) and do not offer a person with depression to "pull themselves together" or "tune in to positive." Even if you sincerely want to express support, such advice will only devalue the feelings of a person who is faced with depression, because he knows that everything is not so simple. People in this situation often hear, “Others have worse problems than you”, “It’s all in your head”, “Do something useful”, but all this only causes more shame, guilt or annoyance due to helplessness in the face of illness. Hearing something like this, a person may conclude that you will never understand him, and close up - then it will be much more difficult to help. If you don’t know what to say in such a situation (and this is normal), just hug, say: “I can’t even imagine what you are experiencing right now, but I see that it is very difficult” - and let the person show feelings in the way he it's necessary.
Don't take the words and actions of a depressed person personally.
People with depression are generally not able to lead the same active lifestyle as before. For example, they stop responding to messages and calls, refuse offers to go out to dinner or to the movies, they may even miss your birthday or wedding. This looks strange and insulting: after all, quite recently everything was in order, and today a person comes up with reasons to avoid a meeting. And if he nevertheless agrees to it, he can behave indifferently and not even try to pretend that he is interested in listening to you.
It's not about you at all - it's just that in a depressed state, most often there is no strength for anything. Even such simple, ordinary things as getting out of bed, taking a shower and preparing breakfast require a lot of effort. It is all the more difficult to go somewhere where there will be a lot of people. In addition, communication with people itself, even if it is not binding, requires a return, for which a depressed person does not have enough emotional resources.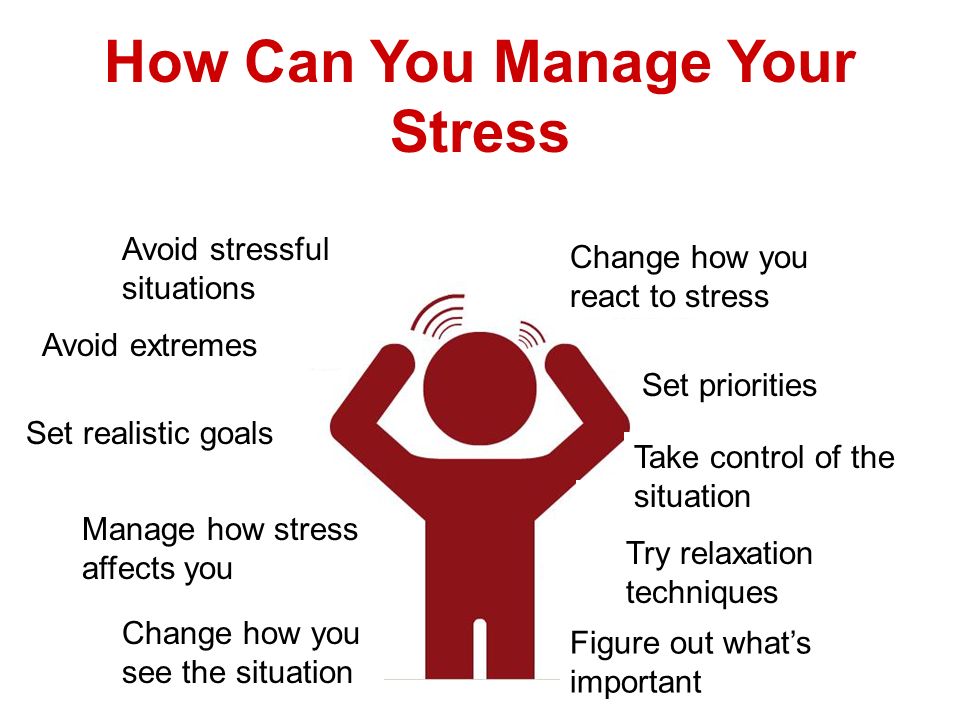 Remember that depressed people feel and appreciate the support of their family and friends, but they simply cannot respond to it in the same way as before.
Remember that depressed people feel and appreciate the support of their family and friends, but they simply cannot respond to it in the same way as before.
Suggest seeking professional help
Depression doesn't often go away on its own—but even if it does, it can come back. According to statistics, 50% of people who have had a depressive episode in their lives have a second one after some time, and 80% of people who have two depressive episodes in their medical history sooner or later have a third. So if you suspect depression, a person should definitely see a specialist - first of all, a psychiatrist who can prescribe drugs if necessary. True, it is also very difficult for many to take this step: going to the doctor is considered something like a “last resort”, an admission of defeat. Antidepressants are also treated with great apprehension, although now there is a large selection of funds - and a competent specialist will be able to choose the right ones in each individual case.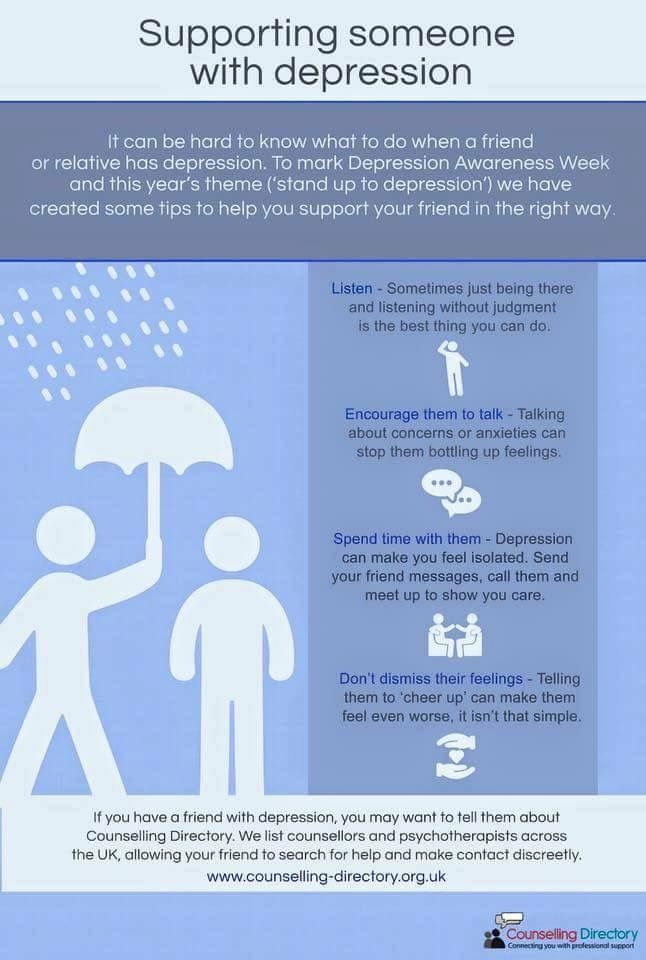 Yes, it doesn’t always work right away, but often you can’t do without medication.
Yes, it doesn’t always work right away, but often you can’t do without medication.
Your loved one may be seriously afraid of going to the doctor because of the fear that he will be labeled as "mentally ill", "registered" or even "put in a fool". In fact, psychiatric registration was canceled back in the early 90s, and a person can be placed in a hospital against their will only by a court decision - or if a person poses a threat to himself and is not able to take care of himself. But if your loved one is still haunted by the fear of free medicine, advise him to contact a private specialist - if possible.
Tell the person with depression that more and more people are going to therapy and it really helps. After all, with a fracture, your friend would go to the surgeon - so in this case, you need to see a doctor. Offer help in finding a psychiatrist, offer to give a ride to an appointment or just see them off. But in no case do not shame and do not force.
Help with the simplest things (but in moderation)
When a person close to you cannot do some things due to illness, there is a desire to take everything upon yourself. You really can help, but here you need to know when to stop.
You really can help, but here you need to know when to stop.
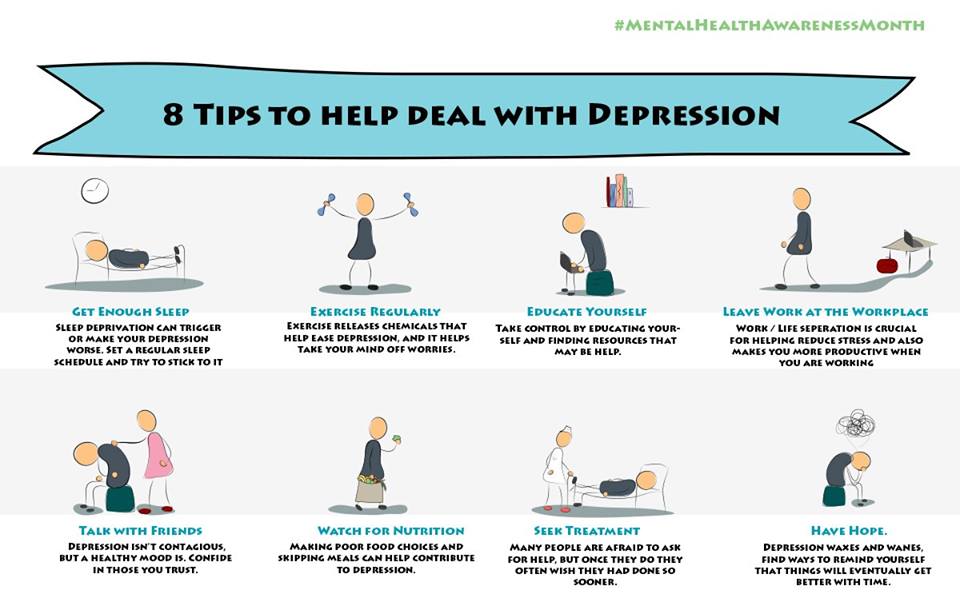
If you live together, help with daily chores: waking up and going to bed on time, remembering to take a shower or soak in the bath, eat well, and remember to take medication if prescribed. The correct daily routine helps to maintain some kind of balance even in the most difficult condition. You can try to involve a person in physical exercises - studies confirm that sports help in the treatment and prevention of depression. Moreover, it is the regularity of classes, and not their intensity, that plays the key role - you need to exercise for at least three months and for 45-60 minutes. Workouts on a pulse of 120-130 beats per minute are best suited: running, walking, swimming, cycling, tennis, dancing.
Offer useful applications
When depressed, it is useful to monitor how your mood changes over time - there are many paid and free mobile applications in Google Play and the App Store for this. For example, Moodnotes. When creating the application, the developers relied on the method of cognitive behavioral therapy, so in it you can not only note what you think about and how you feel today, but also track what causes certain thoughts and moods. You can also keep a mood diary through the How Are You and MoodPanda apps.
When creating the application, the developers relied on the method of cognitive behavioral therapy, so in it you can not only note what you think about and how you feel today, but also track what causes certain thoughts and moods. You can also keep a mood diary through the How Are You and MoodPanda apps.
Mindfulness meditation apps can also be useful. It forms the basis of Mindfulness-Based Cognitive Therapy (MBCT), which is now gaining popularity in the United States. The main goal is to help get rid of the tendency to automatically respond to thoughts, emotions and life events. Perhaps the best mobile app for this is Headspace; it's available on both iOS and Android, but it's a paid subscription for $12.99 a month (I must say it's loved by many who don't have a depression problem, too). A free alternative to it could be Stop, Breathe & Think. But, of course, we must remember that neither meditation nor a mood diary can replace treatment, but can only be a help (well, it doesn’t hurt to discuss these practices with your doctor).
Be attentive and patient
The process of treating depression is long and hard. How much time and effort it will take depends on the severity of depression (mild, moderate, severe), and on the chosen treatment method (only taking pills, only psychotherapy, or both), and on how quickly it turned out to pick up the right pills and their dosage and, finally, whether it was possible to find a suitable psychotherapist. It also happens that a psychotherapist is good, but not suitable. Even if you have done everything you could and the healing process has begun, you should not expect an immediate result. Don't ask, "Are you feeling better?" - It may seem to a depressed person that progress in his treatment does not meet your expectations.
Instead, ask delicately from time to time if he remembers to take his pills, if he misses psychiatric and/or psychotherapist appointments, and if so, try to carefully find out why. For example, in psychotherapy there is such a thing as "resistance" - the patient's subconscious opposition to the process of psychotherapy. This phenomenon is associated with the fear of change, because it is far from always easy and painless to come to a cure. Resistance in psychotherapy can be expressed in many ways, including just missing meetings or refusing to continue psychotherapy in principle. Dealing with this is the work of a psychotherapist, but a careful, confidential conversation with a loved one can also help.
This phenomenon is associated with the fear of change, because it is far from always easy and painless to come to a cure. Resistance in psychotherapy can be expressed in many ways, including just missing meetings or refusing to continue psychotherapy in principle. Dealing with this is the work of a psychotherapist, but a careful, confidential conversation with a loved one can also help.
Take care of yourself
Being around a depressed person can be exhausting. Especially if this is a person close to you, to whose condition you cannot be indifferent. Nevertheless, do not forget the main rule from the instructions for behavior in emergency situations: you must first put on the oxygen mask. You may feel like you have to stay strong for your loved one, but you don't have to sacrifice your comfort and convenience. Don't forget that you have your own worries and feelings. If you make it your goal to get your loved one out of depression at all costs and forget about everything else, there is a risk that you will undermine your own health.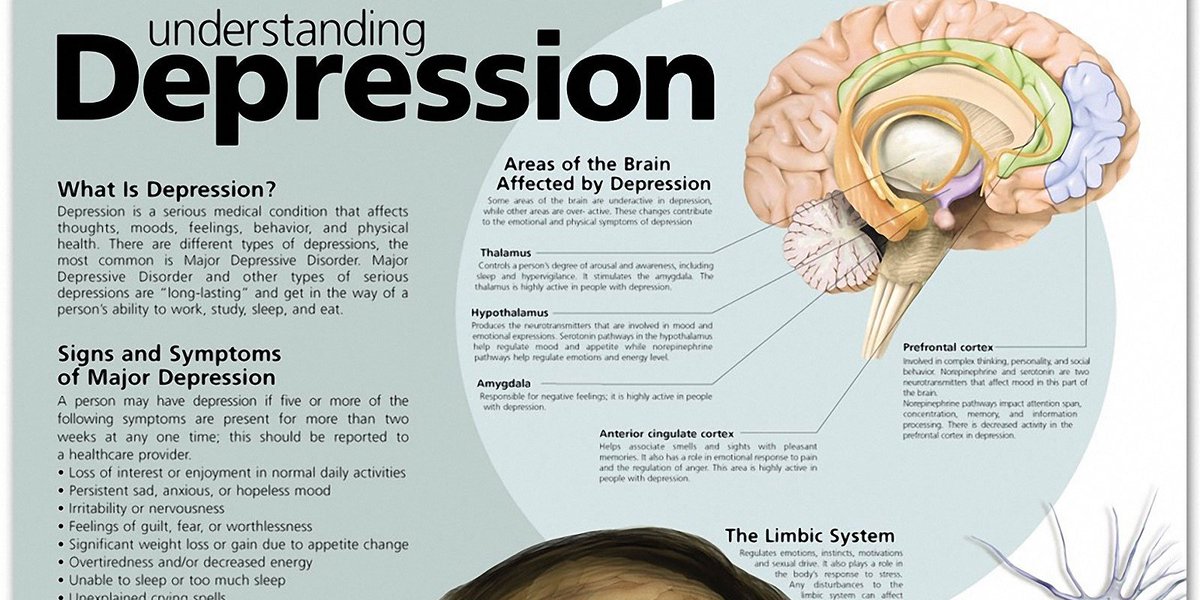 To avoid this, try to clearly define what you are ready and able to do and what you are not. Listen to your feelings and emotions and seek support if you need it (including from a psychotherapist). After all, you can do little to help a depressed person if you yourself are not okay.
To avoid this, try to clearly define what you are ready and able to do and what you are not. Listen to your feelings and emotions and seek support if you need it (including from a psychotherapist). After all, you can do little to help a depressed person if you yourself are not okay.
Daria Chagina
Perhaps you know or guess that someone close to you suffers from a mental illness. If a person is not feeling well, he needs communication and support, even if it seems that this is not so. We have collected recommendations: what alarming bells you should pay attention to and how to support a person so that he does not get even worse.
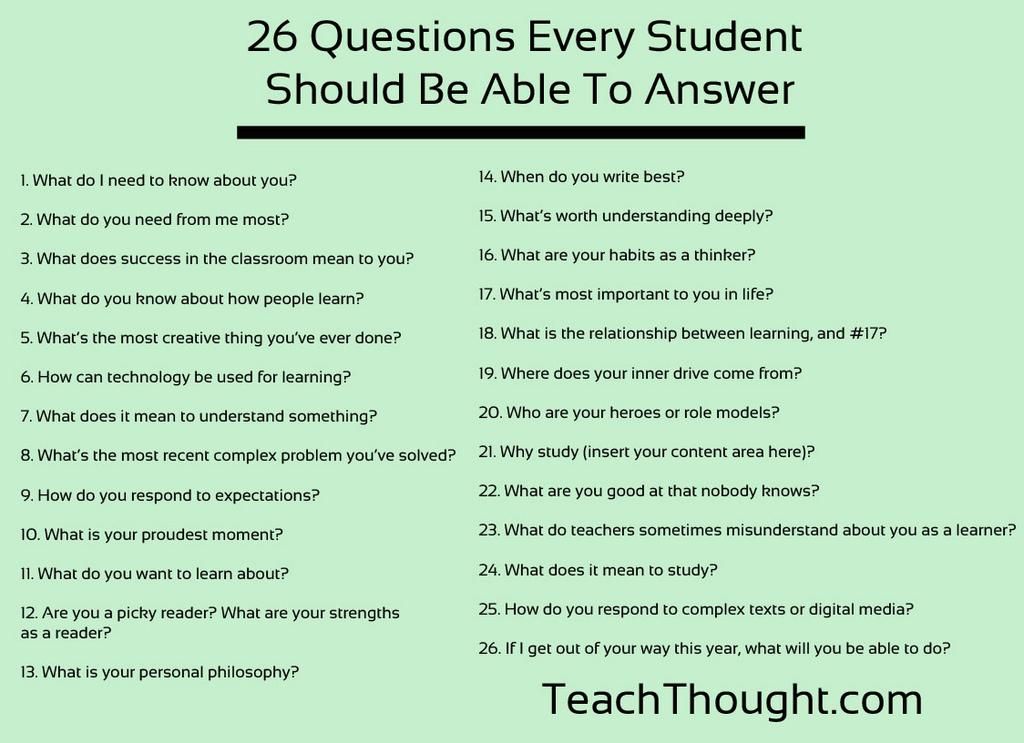
- How to understand that a person is not just sad or tired?
- Early wake-up calls
- Everything seems to be serious. How to talk about it?
- Phrases to avoid
- How can I help a loved one in such a situation?
- Don't try to guess
- Specify help
- Stay in touch
- spend time together
- Separate symptoms from personality
- Celebrate even the smallest victories
- Agree on feedback
- What to do if a loved one refuses to talk about the problem?
- "I don't know what to tell you"
- "I don't have any problems"
- "I'll deal with it myself"
- "It's not so bad"
- "You will not understand anyway"
- Everything seems to be really bad.
 How to persuade a person to seek professional help?
How to persuade a person to seek professional help? - I try to support, but for me it is very hard. Am I a bad friend?
How to understand that a person is not just sad or tired?
Sadness, anxiety, irritability, restlessness or sleep problems are very common. But if these sensations become very intense, do not go away for a long time, and begin to interfere with relationships or work, this may be a sign of mental illness.
It's like a cold: in most cases, it can be tolerated relatively easily without breaking away from the usual activities, but sometimes there are complications. For example, everything can end with pneumonia - then just sleeping will obviously not help, you will have to take more serious measures.
If you know the person well, you may notice complications in his condition and behavior that say that this is not "just sadness."
Early warning signs
- A person sleeps too much or too little
- Too much energy or vice versa, no strength at all
- Alcohol abuse
- Suddenly lost interest in what used to please loved ones avoiding quarrels, quarrels with communication
- Frequent and severe mood swings
- Difficulties with daily activities, taking care of yourself (for example, you notice that the person has become less likely to leave the house or has almost stopped preparing food for himself)
Also be alert if the person mentions: feelings disappeared
Everything seems to be serious.
 How to talk about it?
How to talk about it? It can be scary or embarrassing to talk about such a topic, and this is absolutely normal. Try to choose the right moment when you are alone and no one is in a hurry.
The following phrases can help start a conversation:
✅ “I'm worried about you. If you're feeling down, can we talk about what you're going through?"
✅ “I care about you and am ready to listen. Would you like to tell me how you feel?"
✅ “Looks like you're having a hard time right now. Would you like to talk about it?"
It is better to ask open-ended questions that cannot be answered with a simple "yes" or "no". This will give more chances that a loved one will be able to express what is on his mind. Give the person time to respond and don't bombard them with questions. You are not necessarily expected to give advice or solve a problem - the fact that you listen to him is already important in itself.
Let the person tell exactly as much as they want. Try not to push or ask for details that he is not yet ready to share. Remember that talking about mental problems is usually very difficult, it requires a lot of trust and courage.
Try not to push or ask for details that he is not yet ready to share. Remember that talking about mental problems is usually very difficult, it requires a lot of trust and courage.
It is important that the person feels heard, that their experiences are respected and taken seriously. Many people who suffer from mental illness blame themselves for what they are going through. It may seem to them that all this is “only in their head” and unworthy of attention. Even if you may not fully understand how your loved one feels, it is important to validate their feelings and experiences. This can be expressed, for example, with the phrase “It sounds really difficult, I really sympathize with you.”
Phrases to avoid
⛔️ “It's okay, you're depressed”
Don't try to diagnose or question the person's feelings. Many mental illnesses have similar symptoms. Most likely, you are not an expert, so try not to draw conclusions and conclusions. You are expected to support, not "home psychotherapy. "
"
⛔️ “It is even worse for others now than you”
This does not help, but devalues the person's experiences. You seem to be saying, “You have no right to feel what you feel. It has to be earned."
⛔️ “Everyone is feeling bad and anxious now”
It is also better not to use such phrases. On the one hand, this normalizes the experience of a person, and on the other hand, it can have an undesirable effect in the form of depreciation and a call to do nothing about the problem.
⛔️ “After all, nothing terrible has happened to you, how can you be sad?”
Mental illnesses often have a biochemical basis - that is, a person feels bad literally “for no reason”. This can frighten and torment him: after all, if he understood the reason, he could cope with it. Therefore, it is better not to emphasize it once again.
⛔️ "Find something to do and there will be no time for suffering"
Sometimes the symptoms of mental illness are apathy, lack of energy and loss of interest in things that a person used to love.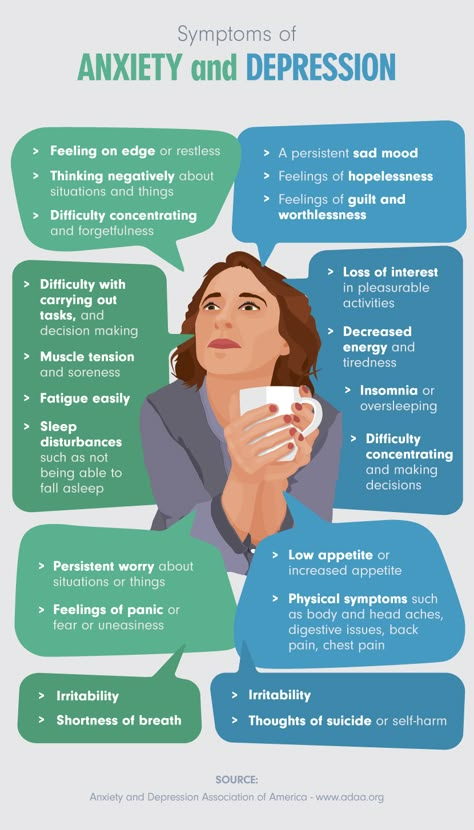 In this state, it is difficult to find something to do and get distracted - in addition, the problem will not disappear from this.
In this state, it is difficult to find something to do and get distracted - in addition, the problem will not disappear from this.
How can I help a loved one in such a situation?
Don't try to guess
It's important to remember that support means different things to each of us. It is enough for someone to be simply listened to and not condemned, another needs help in deed. Instead of wondering how you can help, ask directly: “How can I support you?” or “What would be good for you right now?”
Specify help
Sometimes it can be difficult for a person to formulate exactly what they need. Instead of the general phrase "I'm there, if anything," try to be specific about what kind of help you are ready to provide. Often help is needed in daily activities. A person who suffers from a mental illness may be overwhelmed by even the simplest decisions or actions. For example, it may be difficult to choose what to eat or wash the dishes. If you are visiting, offer to help with household chores. For example, order food or go to the pharmacy. Or, if the person is comfortable with such help, you can offer to remind them when to eat, take their medication, or go to bed.
For example, order food or go to the pharmacy. Or, if the person is comfortable with such help, you can offer to remind them when to eat, take their medication, or go to bed.
Keep in touch
Try to keep in touch regularly. The person is most likely embarrassed to waste someone else's time and energy. It is important to remind that you are there and love him. Even a simple “How are you?” is enough for a person to feel that he is not alone, and he has someone to rely on.
Spend time together
Support can come in the form of doing something together that brings you both joy. Even with a mental illness, it's still the same person - the loved one you love. It may be difficult for him to answer the question "What do you want to do?". Remind him what you usually like to do together - cooking, watching TV shows, going out.
Even a simple “How are you?” is enough to make a person feel that he is not alone, and that he has someone to rely on.

Separate symptoms from personality
Try not to take your loved one's behavior personally. Often people with mental illness behave unpredictably. They can be either talkative or withdrawn, and sometimes, as if for no reason, to postpone a meeting or call. You may feel uncomfortable and hurt, but try not to look in these actions for a reflection of how the person treats you. Instead, try to indicate that you accept the person. Show understanding if he canceled joint plans due to the fact that the day turned out to be especially difficult, or adapt them. Instead of going to the cinema, you can offer to watch a movie in bed if it is difficult for a loved one to get out of bed today.
Celebrate even the smallest victories
For someone suffering from mental illness, every day can be full of trials. So it is worth welcoming even the smallest achievements of a loved one. It helps to restore and strengthen self-confidence. You can rejoice with a person if he managed to pull himself out for a walk, or thank him for having the courage to share his experiences with you.
Negotiate feedback
Your support will not always work the way you expected. It may be that it is difficult for a person in his condition to show emotions or notice that he has become easier. Therefore, try to discuss with your loved ones: how it will be easier for you to understand what you support correctly.
What to do if a loved one refuses to talk about the problem?
If the person brushes off talking, try not to take it personally. It most likely says nothing about you or your relationship. There are many reasons why a person does not want to talk about what they are going through, or are not ready to seek help.
“I don't know what to tell you”
If your loved one finds it difficult to talk about what is bothering him, he may not yet fully understand it himself. If he has difficulty processing and expressing his feelings, talking about his condition can be anxious and uncomfortable.
How to act: perhaps if you yourself are the first to share difficult experiences, it will be easier for your loved one to open up to you.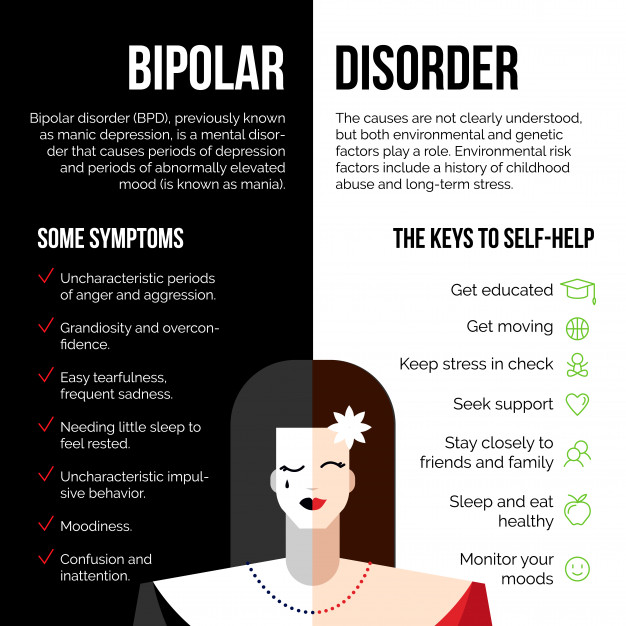
"I don't have any problems"
If your loved one gets irritated when you try to discuss their condition, they may be in denial right now. This is a common reaction when a person is faced with mental difficulties that interfere with the normal course of his life.
How to proceed: be there, wait until he is ready to admit that there is a problem, and then gently re-talk that you are worried about him.
"I'll deal with it myself"
Your loved one may believe that he or she should handle everything on their own. Perhaps he is ashamed of the difficulties that he is experiencing, or for him to ask for help means to show weakness.
How to act: try to accept the person's desire to show inner strength and cope with everything on your own. But also remind him that accepting help is also a strong act, and not at all a sign of weakness.
“It's not so bad”
Perhaps a person feels like a burden to loved ones, especially if they are also experiencing difficulties now. So you might want to downplay how hard it is for him right now.
So you might want to downplay how hard it is for him right now.
Action: Remind your loved one that their feelings, worries and concerns are important to you - no matter how hard it is for you or the other eight billion people on the planet.
"You still won't understand"
In an acute state, it may seem to your loved one that no one will understand his experiences. Remember that many mental illnesses exacerbate feelings of loneliness and isolation, and this experience can be very painful.
How to act: tell the person that even if you have not experienced this yourself, this does not mean that you are indifferent to his condition. If you have had a similar experience, please share it.
Everything seems to be really bad. How to persuade a person to seek professional help?
When you see someone you love suffer, it can be very difficult to suppress the urge to take matters into your own hands and “do good” by force. But in this way you will take away agency from a person - his independence, the ability to make decisions himself and influence his life. You are trying to support the person, not control them, so avoid taking ultimatums about what your loved one should or shouldn't do.
But in this way you will take away agency from a person - his independence, the ability to make decisions himself and influence his life. You are trying to support the person, not control them, so avoid taking ultimatums about what your loved one should or shouldn't do.
⛔️ “Come on, see a psychologist quickly”
⛔️ “You need urgent treatment”
✅ “You can count on my support, but I'm not a specialist. Maybe we should look for a therapist together?”
Even if you are sure that therapy will help your loved one, it may be that he is not ready for it yet. Of course, this is hard to understand and accept, but remember that asking for help can be very scary and embarrassing. In addition, if a person is not ready for therapy, even the best specialist will not be able to help him.
If your loved one refuses to see a specialist, try to understand what is behind their refusal. When you understand the reason, you can try to carefully discuss the beliefs behind it. Often a person simply does not have enough information about how and on what the therapeutic work is built. For example, many are afraid that a psychologist will force you to take pills (and he can only recommend). It also happens that a person lacks confidence that he can really be helped. And sometimes a person simply does not have the strength to choose a specialist, and then make an appointment with him and go to an appointment. What seems to you a simple, understandable and uncomplicated plan, a person with a mental illness may seem an unbearably difficult “long-term construction” that he will never endure.
Often a person simply does not have enough information about how and on what the therapeutic work is built. For example, many are afraid that a psychologist will force you to take pills (and he can only recommend). It also happens that a person lacks confidence that he can really be helped. And sometimes a person simply does not have the strength to choose a specialist, and then make an appointment with him and go to an appointment. What seems to you a simple, understandable and uncomplicated plan, a person with a mental illness may seem an unbearably difficult “long-term construction” that he will never endure.
You cannot force a person, but you can motivate them to seek help. If you already had experience working with a psychologist, then offer to return to him or find another. If the person has never sought psychological help before, encourage them to try. Share how therapy has helped you yourself: for example, how you coped with anxiety and began to feel more confident. Explain that a psychologist does not “teach you how to live”, but helps you better understand yourself, look at the situation in a new way and see ways to solve problems. Explain how the appointments work, how the therapy is structured, what can be expected. Offer to help you find a specialist or make an appointment with one.
Explain how the appointments work, how the therapy is structured, what can be expected. Offer to help you find a specialist or make an appointment with one.
I try to be supportive, but it's very hard for me. Am I a bad friend?
In any situation, you need to remember first of all about yourself. It is within your power to support a loved one, but it is not an obligation. Empathy must be shown first of all to yourself - only in this way you can provide support without burning out and without sacrificing yourself.
You may feel responsible for the condition of a loved one, worried about what might happen to him if you are not around. These experiences can be painful and embarrassing, both for you and your loved one.
Compassion must be shown to yourself first of all - this is the only way you can provide support without burning out and without sacrificing yourself.
So that you and he can feel more independent, do not forget:
- Rest.

If you feel that you "do not take it out", it is better to rest and return to the person with renewed vigor than to scold yourself for being tired and burn out.
- Set boundaries.
Defining boundaries does not mean rejecting a loved one in difficult times. It's about being realistic about how much support you're willing to provide and what you can no longer do. This is how you take care of yourself and those around you. In addition, if you encourage a person to cope without you at some points, this will help him build confidence in his abilities.
- Enlist the support of others.
Do not try to be the only support for your loved one. You can arrange with his friends or relatives to create a support network together. If you know that others can support your loved one, this will relieve you of unnecessary pressure.
- Share your feelings.
Of course, you should not dump all your emotions on the loved one you support. But from the fact that you keep everything to yourself, no one will definitely benefit. Try to talk about your feelings, problems and experiences. That way you can feel supported too.
But from the fact that you keep everything to yourself, no one will definitely benefit. Try to talk about your feelings, problems and experiences. That way you can feel supported too.
Remember that, as a rule, the solution of mental health problems is not a quick process. You may feel helpless when you see a loved one suffering. But you can still make it easier to experience these difficulties. Your loved one doesn't expect you to find a magic pill that will heal them. He just needs you to be around.
An urgent desire to “fix everything” in the state of a loved one may indicate that this is how you are trying to cope with your own discomfort or anxiety. Try to listen to yourself. It is important not to suppress these feelings, but to try to figure out what is behind them. Maybe this is how you are trying to cope with feelings of helplessness, or maybe the difficulties of a loved one are too much like your own.
If your mental condition worsens, make sure that you yourself have someone to talk to and get support and, if necessary, professional help.