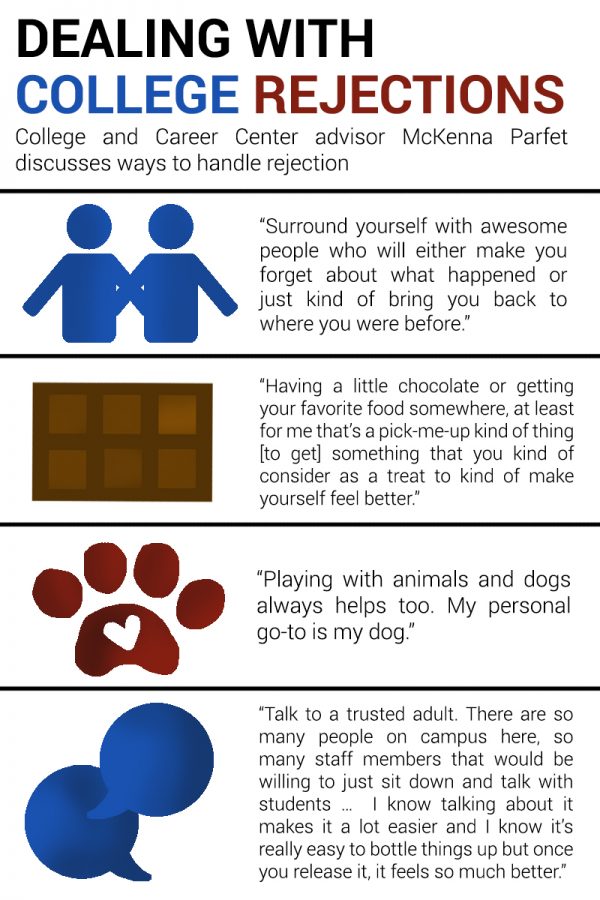
How to help with schizophrenia
Living Well with Schizophrenia - What is Schizophrenia?
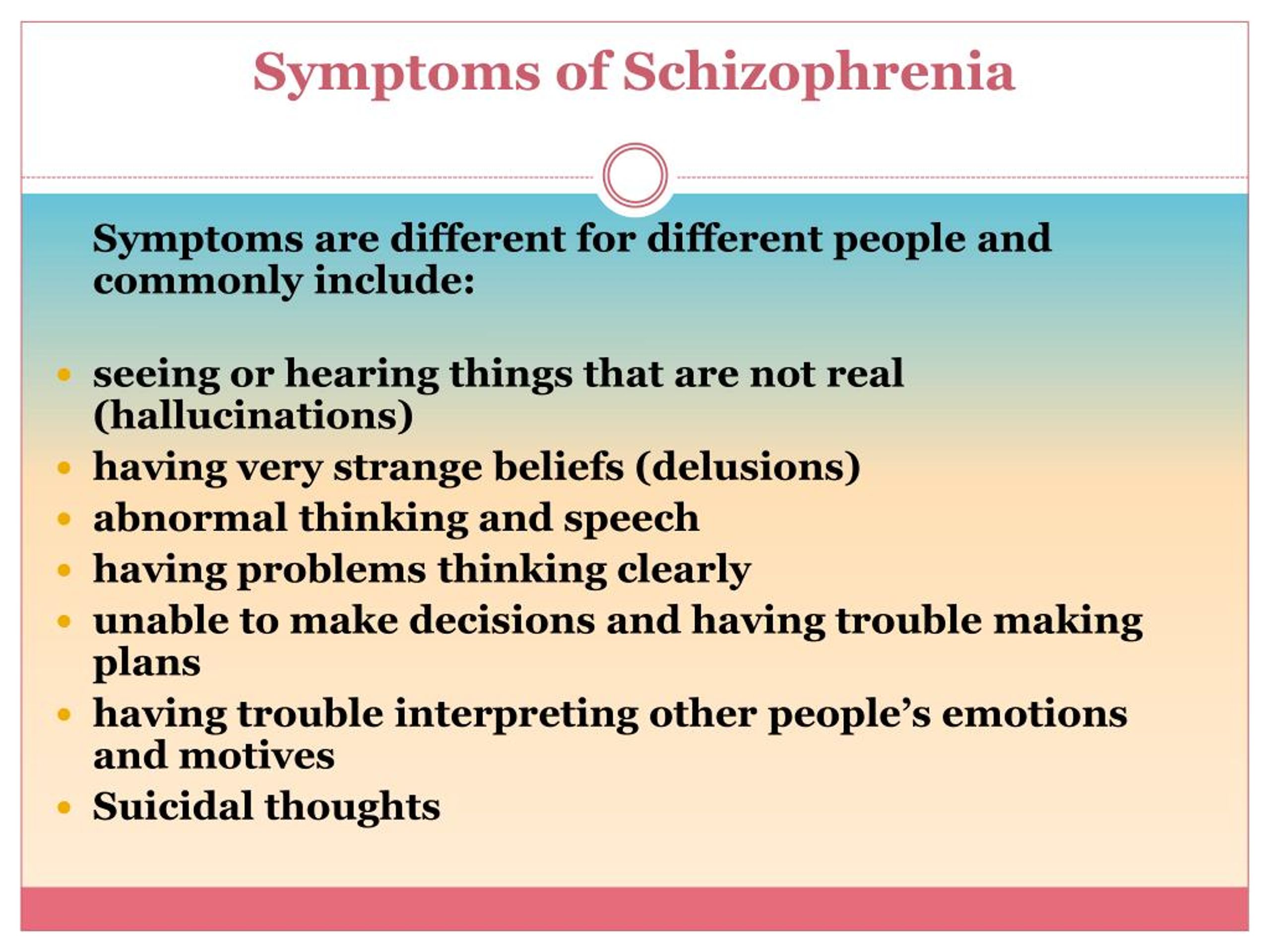
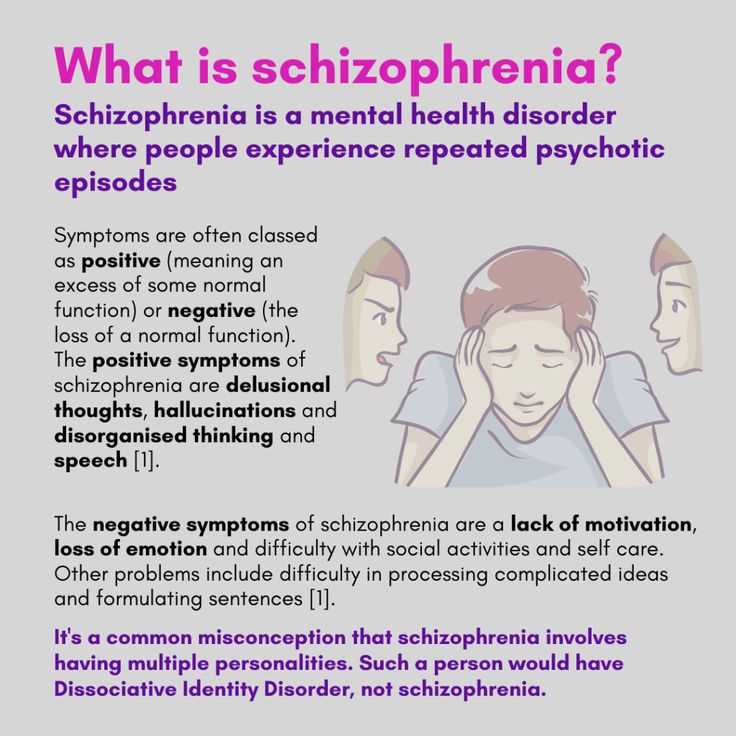
Symptoms of schizophrenia vary from person to person and may change over time. Hospitalization may be needed during a severe episode to ensure a person’s safety, proper nutrition, sufficient sleep, and other factors.
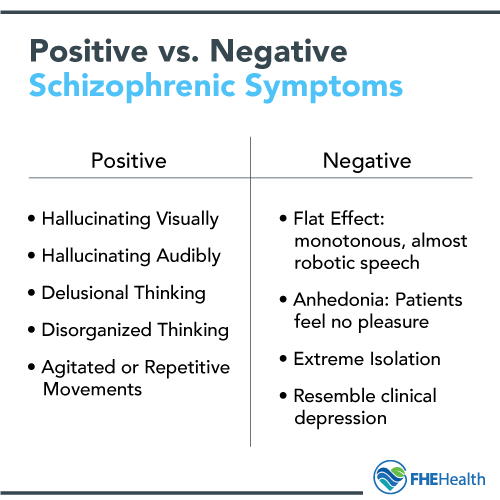
The signs of schizophrenia involve:
- Delusions: false beliefs that a person does not change, even when presented facts.
- Hallucinations: seeing or hearing things that do not exist, such as a voice making commands.
- Disorganized thinking and speech: impaired communication, including shifting from one thought to the next without a logical connection, or speaking in sentences that do not make sense to others.
- Disorganized or abnormal physical behavior: inappropriate or strange actions, a complete lack of movement or talking, acting with a childlike silliness, unpredictable agitation, repetitive or excessive movements.
- Negative symptoms: a reduced or lack of the ability to function normally, such as ignoring personal hygiene or not showing emotion.
Tips for Living Well with Schizophrenia
Some people have one psychotic episode, while others experience many throughout their lives. When treated with medication and therapy, in many cases, people with schizophrenia can pursue their goals, have healthy relationships, keep jobs, and be productive members of their communities.
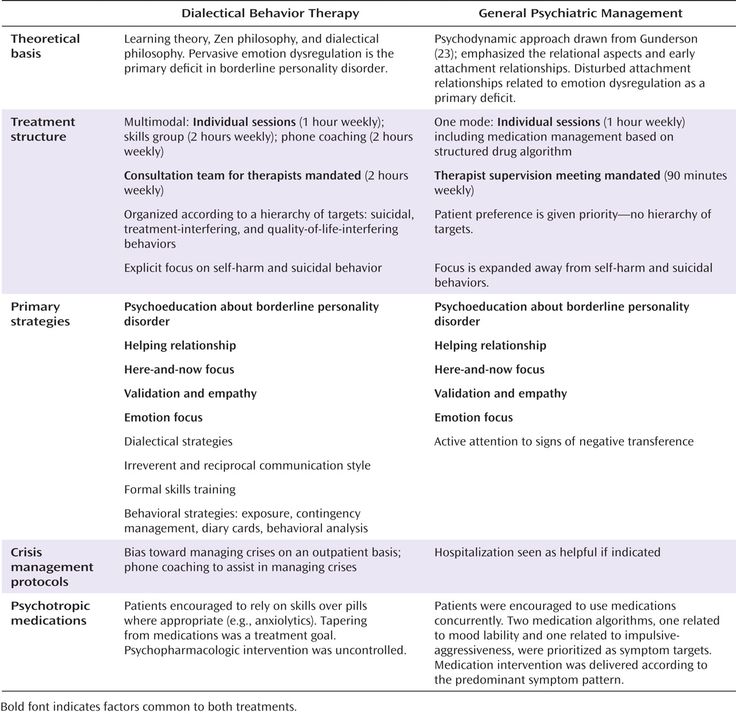
Treatment Options
People with schizophrenia require lifelong treatment. But the earlier treatment begins, the better their chances for recovery and improved quality of life. Medication and therapy can help manage the symptoms of schizophrenia.
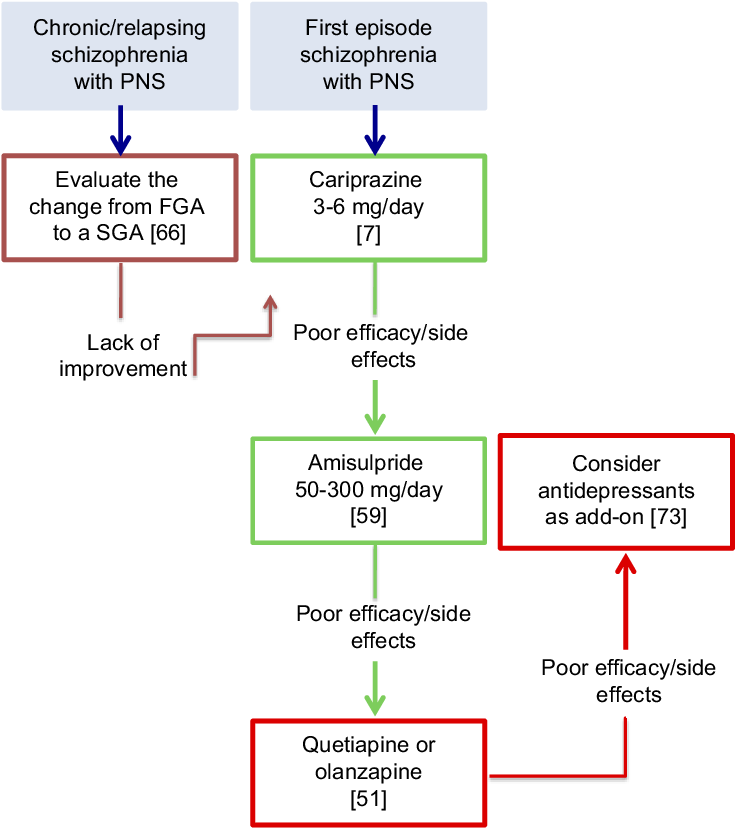
Medication: Antipsychotic medications help get symptoms under control—making them less intrusive and disturbing. A psychiatrist may need to try different medications, at different doses, before finding the most effective medication with the least amount of side effects. It can take several weeks to notice an improvement in symptoms. For people who do no respond to medication, Electroconvulsive therapy (ECT) may be an option. This brain stimulation technique passes small electric currents through the brain to ease the symptoms of schizophrenia.
It can take several weeks to notice an improvement in symptoms. For people who do no respond to medication, Electroconvulsive therapy (ECT) may be an option. This brain stimulation technique passes small electric currents through the brain to ease the symptoms of schizophrenia.
Therapy: In addition to medication, therapy provides guidance and support to people with schizophrenia and their families:
- Individual therapy (“talk therapy”) helps people normalize thought patterns, notice early warning signs of relapse, and handle stress.
- Family therapy offers support, insight, and awareness to families coping with schizophrenia.
What You Can Do: Daily Habits Make a Difference
Once medication and therapy begin to work, these strategies can help ease the challenges of schizophrenia:
- Stay focused on your treatment goals. Tell family members or friends your goals so they can provide support.
- Stick to your treatment plan. Even if symptoms lessen, it is important to go to therapy and take your medication as directed. Use a medication calendar or weekly pillbox to remember to take medications.
- Know your warning signs. Have a plan in place to deal with symptoms as they arise so you can get the right help as soon as possible.
- Take care of yourself. Your physical health is an important part of feeling good, too. Eat nutritious foods, exercise, and follow a regular sleep routine. Do not smoke, or use alcohol, or illegal drugs.
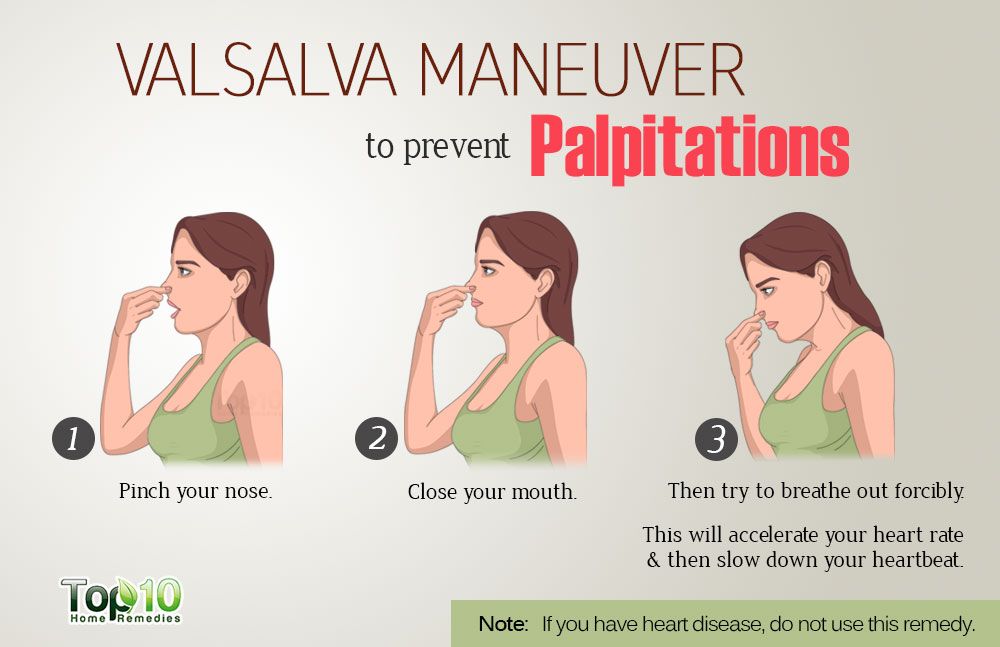
- Incorporate relaxation and stress management techniques into your life. Regularly doing activities such as meditation, or tai-chi, can help reduce stress and avoid triggering an episode.
- Join a support group. Share stories and advice with people who understand what you are going through. It is helpful to connect with – and learn from – others with schizophrenia.
- Educate yourself and others about schizophrenia. Learning about the illness can encourage you to follow your treatment plan and also help your loved ones be more supportive and compassionate.
- Ask about social services assistance. These services help with affordable housing, jobs, transportation, and other daily activities.
Helping Someone with Schizophrenia - HelpGuide.org
schizophrenia
Have a loved one with schizophrenia? Your support can make a huge difference by helping them find the right treatment, cope with symptoms, and build a rich, satisfying life.
When a loved one has schizophrenia
The love and support of family and friends plays an important role in schizophrenia treatment and recovery. If you have a loved one with schizophrenia, you may be struggling with any number of difficult emotions, including fear, guilt, anger, and frustration. You may feel helpless in the face of your loved one’s symptoms, worried about the stigma of schizophrenia, or confused and embarrassed by their strange behaviors.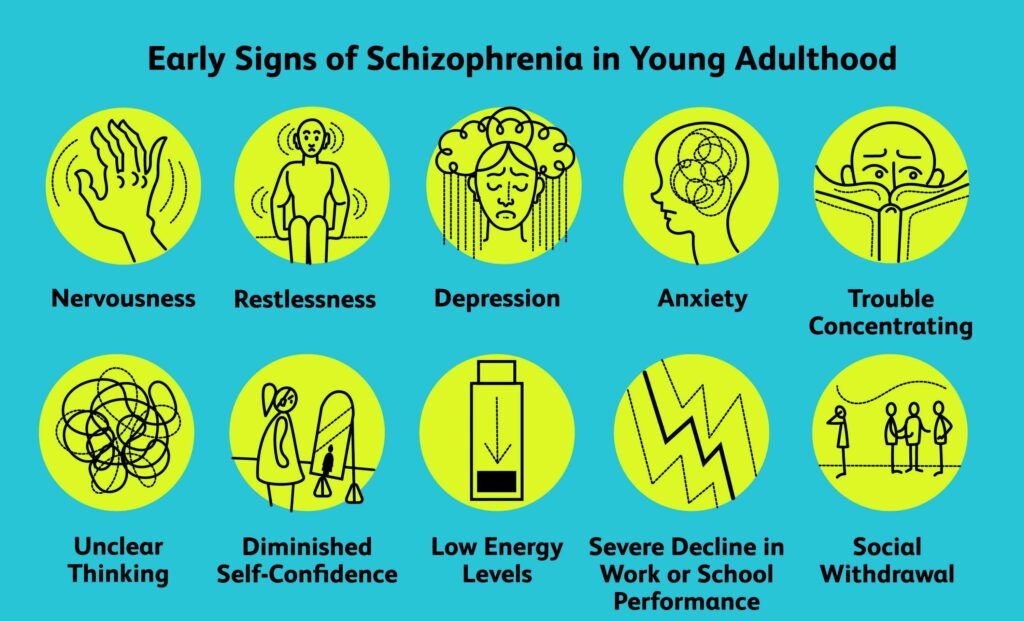 You may even be tempted to hide your loved one’s illness from others.
You may even be tempted to hide your loved one’s illness from others.
But it’s important to remember that a diagnosis of schizophrenia is not a life-sentence. Recovery is possible, especially with your love and support. To help someone with schizophrenia, it’s crucial you:
- Accept the illness and its difficulties.
- Not buy into the myth that someone with schizophrenia can't get better or live a full and meaningful life.
- Do your best to help your loved one feel better and enjoy life.
- Pay attention to your own needs.
- Maintain your sense of humor and remain hopeful.
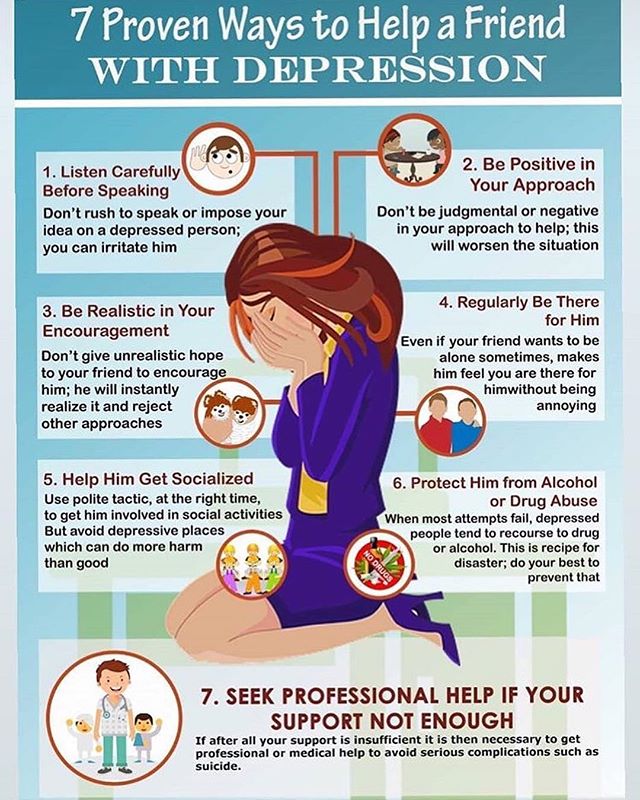
While dealing with a loved one’s schizophrenia can be challenging, the following strategies can help you guide your loved one on the road to recovery without losing sight of your own hopes and dreams.
Tips for helping a loved one with schizophrenia
Educate yourself. Learning about schizophrenia and its treatment will allow you to make informed decisions about how best to cope with symptoms, encourage your loved one to pursue self-help strategies, handle setbacks, and work towards recovery.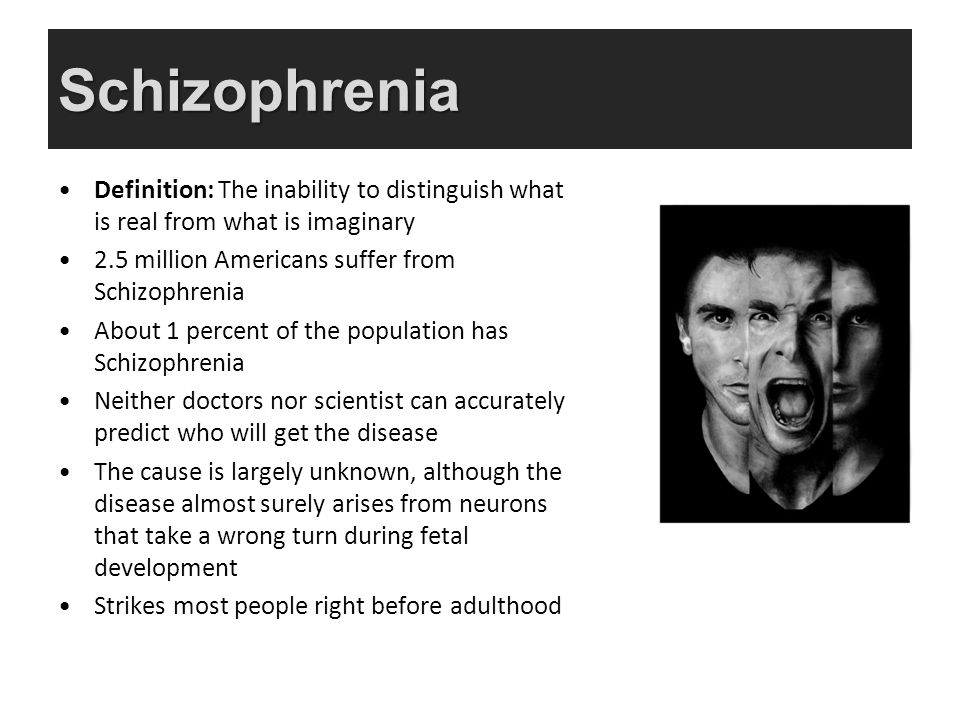
Reduce stress. Stress can cause schizophrenia symptoms to flare up, so it's important to create a structured and supportive environment for your loved one.
Set realistic expectations. It's important to be realistic about the challenges of schizophrenia. Help your loved one set and achieve manageable goals, and be patient with the pace of recovery.
Empower your loved one. Be careful that you're not taking over and doing things for your loved one that they are capable of doing. Support your loved one while still encouraging as much independence and self-help as possible.
Helping someone with schizophrenia tip 1: Encourage treatment and self-help
Encouraging treatment and self-help is a cornerstone of helping a loved one with schizophrenia. While medication is an important element of schizophrenia treatment, your loved one's recovery depends on other factors as well. Self-help strategies such as changing to a healthy diet, managing stress, exercising, and seeking social support can have a profound effect on your loved one's symptoms, feelings, and self-esteem.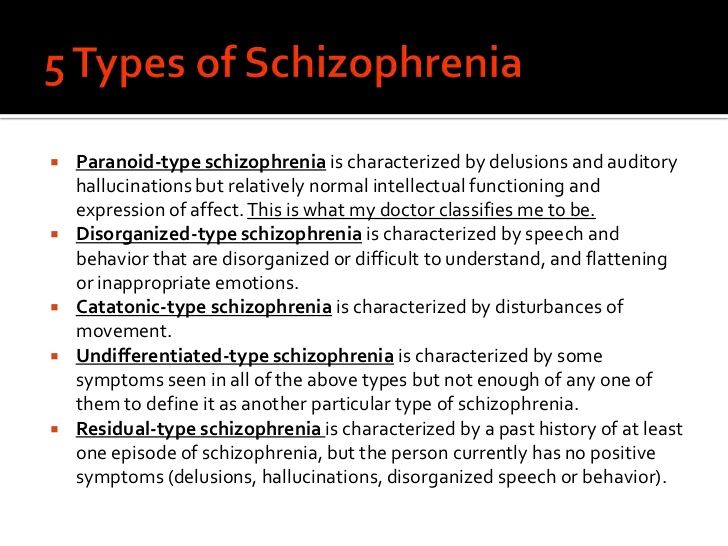 And the more someone does for themselves, the less hopeless and helpless they'll feel, and the more likely their doctor will be able to reduce their medication. Your encouragement and support can be crucial to your loved one starting and continuing a program of self-help.
And the more someone does for themselves, the less hopeless and helpless they'll feel, and the more likely their doctor will be able to reduce their medication. Your encouragement and support can be crucial to your loved one starting and continuing a program of self-help.
[Read: How to Help Someone with Mental Illness Accept Treatment]
Starting treatment
Often, the first challenge of treatment is convincing the person with schizophrenia to see a doctor. To people experiencing delusions, hallucinations, and paranoia, there is no need for medical intervention because the voices and conspiracy theories are real.
If a loved one with schizophrenia is reluctant to see a doctor, try to:
Provide options. Your loved one may be more willing to see a doctor if he or she has some control over the situation. If your relative appears suspicious of you, suggest that another person accompany them to the appointment. You can also give your loved one a choice of doctors.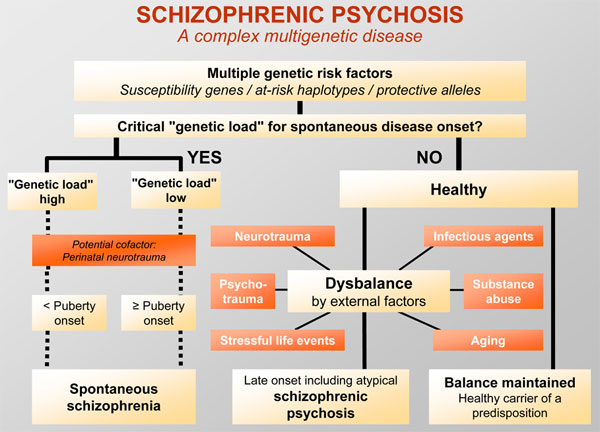
Focus on a particular symptom. Someone with schizophrenia may resist seeing a doctor out of fear of being judged or labeled “crazy.” You can make the doctor less threatening by suggesting a visit in order to deal with a specific symptom such as insomnia or lack of energy.
Tips for supporting a loved one's schizophrenia treatment
Seek help right away. Early intervention makes a difference in the course of schizophrenia, so help your loved one find a good doctor and start treatment.
Be collaborative. When your loved one has a voice in their own treatment, they will be more motivated to work towards recovery.
Encourage self-help. Since schizophrenia is often episodic, periods of remission from the severest symptoms can provide an opportunity for your loved one to employ self-help strategies that may limit the length and frequency of future episodes.
Tip 2: Build your support network
To better support and care for someone with schizophrenia, you need to find help, encouragement, and understanding from others.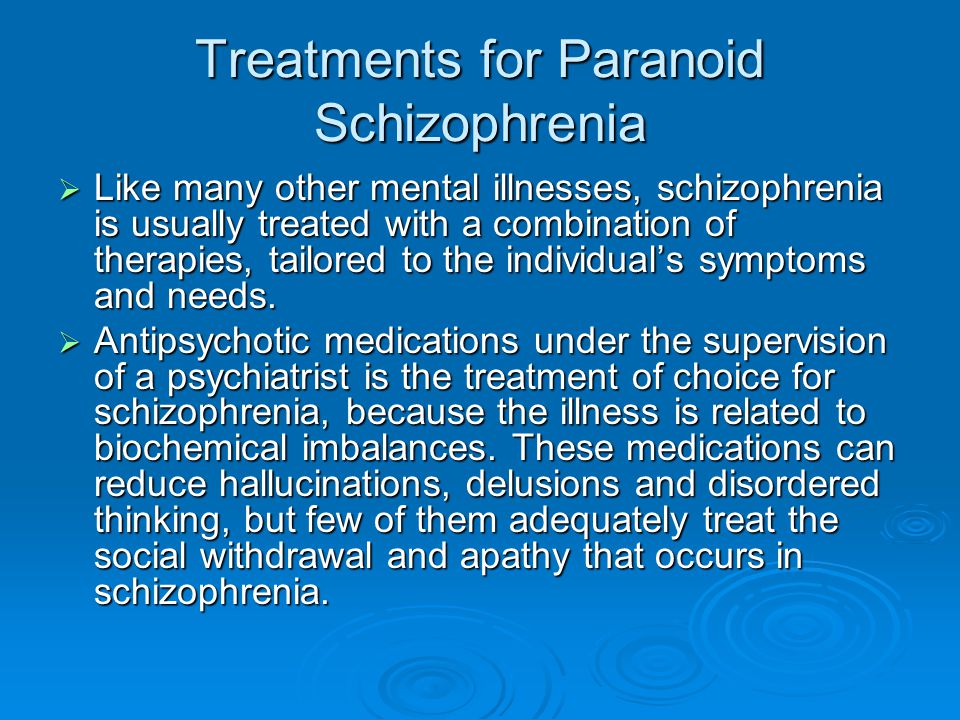 The more support you have, the better it will be for both you and your loved one.
The more support you have, the better it will be for both you and your loved one.
Recognize your own limits. Be realistic about the level of support and care you can provide. You can't do it all, and you won't be much help to a loved one if you're exhausted, so seek help where you can.
Join a support group. Meeting others who know first-hand what you're going through can help reduce feelings of isolation and fear. Support groups provide an invaluable venue for the relatives of people with schizophrenia to share experiences, advice, and information.
Turn to trusted friends and family members. Ask loved ones if you can call on them for support. Most people will be flattered by your request.
Seek out new friends. If you don't feel that you have anyone to turn to, it's never too late to build new friendships and improve your support network.
Take advantage of support services. Ask your loved one's doctor or therapist about respite services and other support available in your area, or contact local hospitals and mental health clinics.
With over 25,000 licensed counselors, BetterHelp has a therapist that fits your needs. It's easy, affordable, and convenient.
GET 20% OFF
Online-Therapy.com is a complete toolbox of support, when you need it, on your schedule. It only takes a few minutes to sign up.
GET 20% OFF
Teen Counseling is an online therapy service for teens and young adults. Connect with your counselor by video, phone, or chat.
GET 20% OFF
Tip 3: Monitor medication
Once in treatment, careful monitoring can ensure that your loved one stays on track and gets the most out of medication.
Take side effects seriously. Many people with schizophrenia stop taking their medication because of side effects. Bring any distressing side effects to the attention of the doctor, who may be able to reduce the dose, switch to another antipsychotic, or add medication to counter the side effect.
Encourage your loved one to take medication regularly.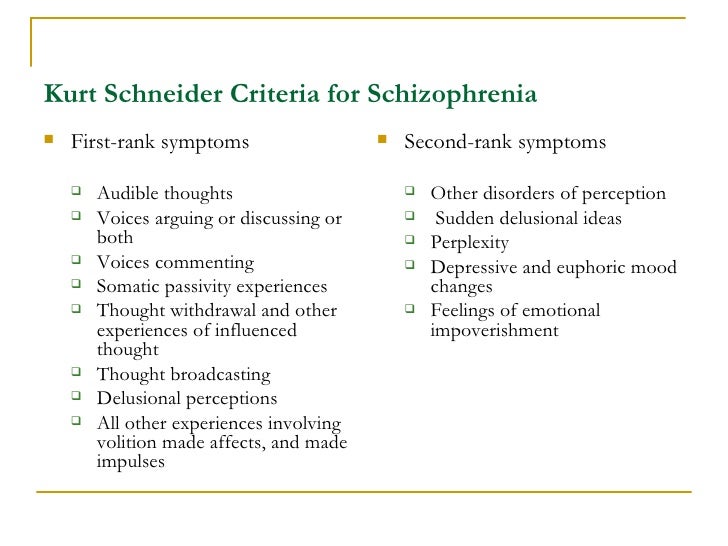 Even with side effects under control, some people with schizophrenia refuse medication or have trouble remembering their daily dose. Medication reminder apps, weekly pillboxes, and calendars can help. Some medications are available as long-lasting weekly or monthly injections instead of daily pills.
Even with side effects under control, some people with schizophrenia refuse medication or have trouble remembering their daily dose. Medication reminder apps, weekly pillboxes, and calendars can help. Some medications are available as long-lasting weekly or monthly injections instead of daily pills.
Be careful to avoid drug interactions. Help your loved one avoid any dangerous drug interactions by giving the doctor a complete list of the drugs and supplements they're taking. Mixing alcohol or illegal drugs with schizophrenia medication is harmful, so talk to the doctor if your relative has a substance abuse problem.
Track your family member's progress. A mood-tracking app, journal, or diary is a good way to track changes in your family member's behavior, outlook, and other symptoms in response to medication.
Stopping medication is the most frequent cause of relapse in schizophrenia, so it's extremely important that your family member continues to take all medication as directed. While relapse can occur even if a person is taking medication as prescribed, you may be able to prevent a full-blown crisis by recognizing the warning signs and taking immediate steps.
While relapse can occur even if a person is taking medication as prescribed, you may be able to prevent a full-blown crisis by recognizing the warning signs and taking immediate steps.
Common warning signs of schizophrenia relapse
- Insomnia
- Social withdrawal
- Deterioration of personal hygiene
- Increasing paranoia
- Hostility
- Confusing or nonsensical speech
- Strange disappearances
- Hallucinations
If you notice any warning signs of relapse or other indications that your family member's symptoms of schizophrenia are getting worse, call the doctor right away.
Tip 5: Prepare for crisis situations
Despite your best efforts to prevent relapse, there may be times when your loved one's condition deteriorates rapidly and hospitalization is required to keep them safe. Having an emergency plan ready for an acute psychotic episode will help you handle the crisis safely and quickly. A good emergency plan for someone with schizophrenia includes:
A good emergency plan for someone with schizophrenia includes:
- Emergency contact information for your loved one's doctor and therapists.
- The address and phone number of the hospital you will go to for psychiatric admission.
- Friends or relatives who will take care of other children or dependents while you deal with the crisis.
It's also wise to go over the emergency plan with your family member. The crisis situation may be less frightening to your loved one if they know what to expect during an emergency.
10 tips for handling a schizophrenia crisis
- Remember that you cannot reason with acute psychosis.
- The person may be terrified by their own feelings of loss of control.
- Don't express irritation or anger.
- Speak quietly and calmly, do not shout or threaten the person.
- Don't use sarcasm as a weapon.
- Decrease distractions by turning off the TV, computer, any fluorescent lights that hum, etc.
- Ask any casual visitors to leave—the fewer people the better.

- Avoid direct, continuous eye contact.
- Avoid touching the person.
- Sit down and ask the person to sit down as well.
Tip 6: Explore housing options
Someone with schizophrenia needs a stable, supportive place to live, but finding the right living situation can be challenging.
- Can your loved one care for themselves?
- How much support do they need with daily activities?
- Does your loved one have a drug or alcohol problem?
- How much treatment supervision does your loved one require?
Living with family
Living with family can be a good option for someone with schizophrenia if their family members understand the illness well, have a strong support system of their own, and are able to provide whatever assistance is needed.
At-home arrangements are less likely to be successful if the person with schizophrenia uses drugs or alcohol, resists taking medication, or is aggressive or uncooperative.
| Choosing the Right Housing Option for Someone with Schizophrenia |
| Living with family works best if: |
|
| Living with family is not advised if: |
|
Try not to feel guilty if you are unequipped to house someone with schizophrenia. If you can't look after your own needs or those of other family members while caring for your loved one, they will be better off elsewhere.
Residential options outside the family home
If an at-home living arrangement isn't the right fit, explore the residential facilities in your community.
Options in your area may include:
Residential treatment facilities or 24-hour care homes. A more structured living environment for those requiring greater assistance or suffering an acute psychotic episode.
Transitional group home. An intensive program that helps individuals transition back into society and avoid relapse after a crisis or hospitalization.
Foster or boarding homes. A group living situation offering a degree of independence, while providing meals and other basic necessities.
Supervised apartments. Residents live alone or share an apartment, with staff members available on-site to provide assistance and support.
Tip 7: Take care of yourself
Taking care of yourself isn't selfish. In fact, it's just as important for your loved one with schizophrenia that you look after your own health needs.
Schizophrenia can place an incredible amount of stress on the family.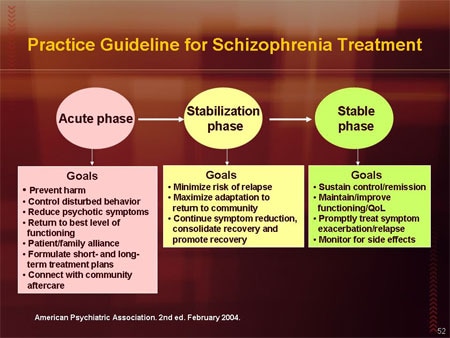 It can take over your life and burn you out. And if you're stressed, you'll make the person with schizophrenia stressed and trigger or exacerbate their symptoms.
It can take over your life and burn you out. And if you're stressed, you'll make the person with schizophrenia stressed and trigger or exacerbate their symptoms.
Since adopting healthy lifestyle habits is also important for your loved one in managing schizophrenia symptoms, by taking care of your own health you can act as a role model. You may even be able to pursue some of these steps together, helping to motivate and encourage each other.
Connect with others. Social interaction with someone who cares about you is the most effective way to relieve stress. It's important for both you and the person with schizophrenia to have other people you can connect with face-to-face—someone you can talk to for an uninterrupted period of time, someone who will listen without judging or continually becoming distracted. That person may be a friend, family member, clergy member, or professional therapist.
Get regular exercise. Physical activity reduces stress and releases endorphins, powerful chemicals in your brain that energize your spirits and make you feel good.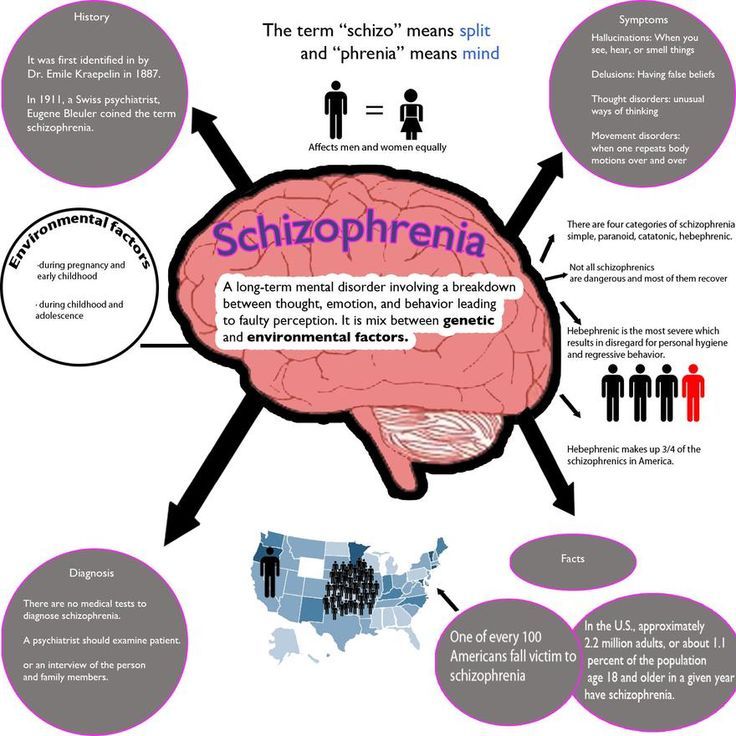 Whether you exercise alone, with a friend, or with your loved one with schizophrenia, aim for 30 minutes of activity on most days, or if it's easier, three 10-minute sessions.
Whether you exercise alone, with a friend, or with your loved one with schizophrenia, aim for 30 minutes of activity on most days, or if it's easier, three 10-minute sessions.
Eat a healthy diet. What you eat has a direct impact on the way you feel. Minimize sugar and refined carbs, foods that quickly lead to a crash in mood and energy. Boost your intake of Omega-3 fatty acids from fatty fish, fish oil, walnuts, and flaxseeds to help improve your focus, energy, and outlook. The same diet tips can help manage your loved one's symptoms, too.
Practice acceptance. Instead of dwelling on the unfairness of your loved one's diagnosis, accept your feelings, even the negative ones. It can make a huge difference in your ability to manage stress and balance your moods. See HelpGuide's Emotional Intelligence Toolkit for more.
Seek out joy. Making time for fun isn't indulgent—it's necessary. Schedule time into your day for things you enjoy, whether it's spending time in nature, visiting friends, or reading a good book.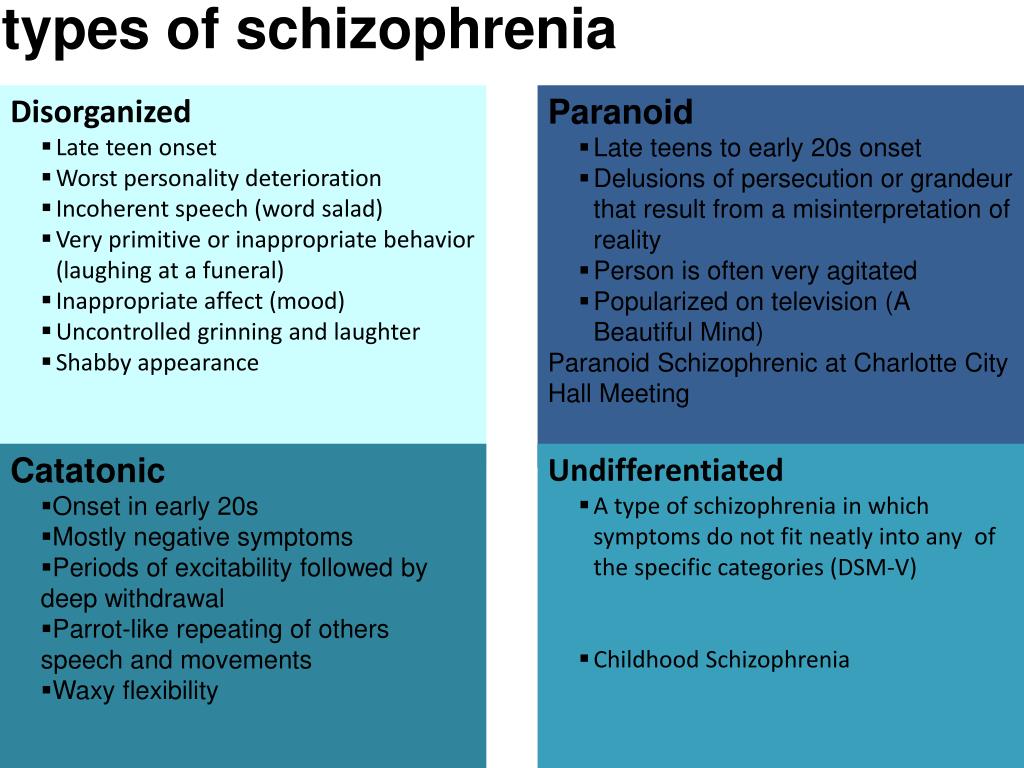 Encourage your loved one with schizophrenia to do the same.
Encourage your loved one with schizophrenia to do the same.
Look after your health. Neglecting your health will only add to the stress in your life. Get enough sleep and stay on top of any medical conditions.
Use relaxation techniques. Techniques such as meditation, deep breathing, yoga, or progressive muscle relaxation can put the brakes on stress and bring your mind and body back into balance.
Authors: Melinda Smith, M.A., Lawrence Robinson, and Jeanne Segal, Ph.D.
- References
Schizophrenia Spectrum and Other Psychotic Disorders. (2013). In Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. https://doi.
 org/10.1176/appi.books.9780890425787.x02_Schizophrenia_Spectrum
org/10.1176/appi.books.9780890425787.x02_Schizophrenia_SpectrumPilling, S., P. Bebbington, E. Kuipers, P. Garety, J. Geddes, G. Orbach, and C. Morgan. “Psychological Treatments in Schizophrenia: I. Meta-Analysis of Family Intervention and Cognitive Behaviour Therapy.” Psychological Medicine 32, no. 5 (July 2002): 763–82. https://doi.org/10.1017/s0033291702005895
Lloyd, Joanne, Helen Lloyd, Ray Fitzpatrick, and Michele Peters. “Treatment Outcomes in Schizophrenia: Qualitative Study of the Views of Family Carers.” BMC Psychiatry 17, no. 1 (July 21, 2017): 266. https://doi.org/10.1186/s12888-017-1418-8
Ganguly, Pronab, Abdrabo Soliman, and Ahmed A. Moustafa. “Holistic Management of Schizophrenia Symptoms Using Pharmacological and Non-Pharmacological Treatment.” Frontiers in Public Health 6 (2018): 166. https://doi.org/10.3389/fpubh.2018.00166
Knight, Edward L. “Self-Help and Serious Mental Illness.” Medscape General Medicine 8, no. 1 (March 15, 2006): 68.
 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1681955/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1681955/“Self-Management: The Experiences and Views of Self-Management of People with a Diagnosis of Schizophrenia – Social Care Online.” Accessed November 2, 2021. https://www.scie-socialcareonline.org.uk/self-management-the-experiences-and-views-of-self-management-of-people-with-a-diagnosis-of-schizophrenia/r/a11G00000017tP5IAI
Stępnicki, Piotr, Magda Kondej, and Agnieszka A. Kaczor. “Current Concepts and Treatments of Schizophrenia.” Molecules: A Journal of Synthetic Chemistry and Natural Product Chemistry 23, no. 8 (August 20, 2018): 2087. https://doi.org/10.3390/molecules23082087
Patel, Krishna R., Jessica Cherian, Kunj Gohil, and Dylan Atkinson. “Schizophrenia: Overview and Treatment Options.” Pharmacy and Therapeutics 39, no. 9 (September 2014): 638–45. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4159061/
Biagianti, Bruno, Sophia H. Quraishi, and Danielle A. Schlosser. “Potential Benefits of Incorporating Peer-to-Peer Interactions Into Digital Interventions for Psychotic Disorders: A Systematic Review.
 ” Psychiatric Services 69, no. 4 (April 1, 2018): 377–88. https://doi.org/10.1176/appi.ps.201700283
” Psychiatric Services 69, no. 4 (April 1, 2018): 377–88. https://doi.org/10.1176/appi.ps.201700283
Schizophrenia: The Journey to Recovery (PDF) – Family guide to schizophrenia assessment and treatment. (Schizophrenia Society of Canada)
60 Tips for Helping People who have Schizophrenia – Tips for communicating with someone who has schizophrenia, handling a crisis, and avoiding relapses. (Schizophrenia.com)
Finding a Good Residential Option for Someone with Severe Mental Illness – Provides suggestions for choosing the right living arrangement for someone with schizophrenia. (Schizophrenia.com)
Helplines and support
In the U.S.: Call 1-800-950-6264 or visit NAMI.org
UK: Call 0300 5000 927 or visit Rethink: Schizophrenia
Australia: Call 1800 18 7263 or visit Sane Australia
Canada: Visit Schizophrenia Society of Canada for links to regional societies that offer helplines and local services
India: Call the Vandrevala Foundation Helpline at 1860 2662 345 or 1800 2333 330
Last updated: December 5, 2022
The brain of a person suffering from schizophrenia: how the disease manifests itself and how scientists fight it
The brain of a person suffering from schizophrenia: how the disease manifests itself and how scientists fight it
Even if there are no people suffering from schizophrenia among your acquaintances, most likely, you have an idea about its symptoms.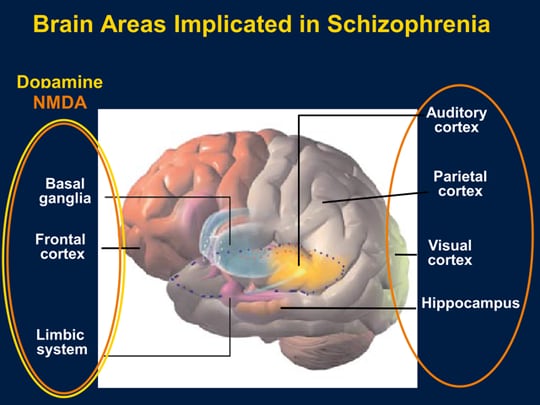
The disorder may manifest as hallucinations, delusions, and paranoia, as well as difficulty concentrating, organizing thoughts, and performing basic daily tasks. nine0003
For many years doctors knew little about this disease, except for the symptoms reported by the patients themselves. The causes of schizophrenia and how it affects the brain have for the most part remained a mystery due to the extreme difficulty scientists have had in trying to understand the most complex—and least accessible—organ in the human body.
But today, thanks to new technologies, the veil of secrecy is beginning to be covered.
“Over the past few years, we have seen tremendous advances in the understanding and treatment of schizophrenia,” says MD Husseini Manji, MD, Global Head of Neurology Therapeutics at Janssen. “This area of medicine is going through an exciting period.” nine0003
The possibility of developing new treatments for people with schizophrenia was one of the reasons that attracted Dr.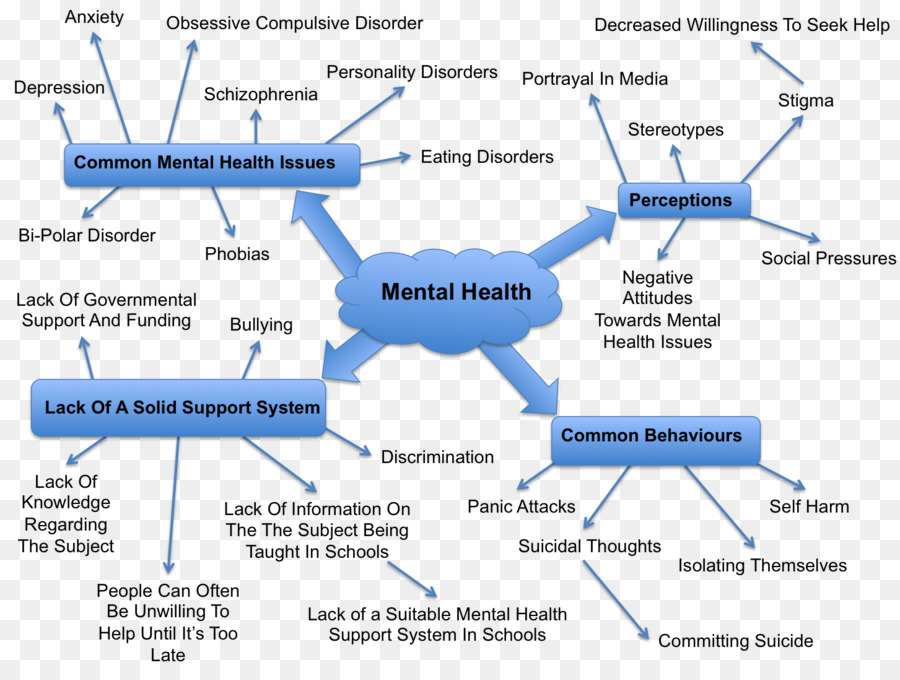 Manji to the company. Then, in 2008, he was director of the National Institute of Mental Health and director of the Mood and Anxiety Disorders Program.
Manji to the company. Then, in 2008, he was director of the National Institute of Mental Health and director of the Mood and Anxiety Disorders Program.
“Several pharmaceutical companies tried to persuade me to join them, but at Johnson & Johnson they were focusing on neuroscience just as many were moving away from the field,” he explains. “The science of mental illness has reached a point of maturity where existing knowledge can be translated into advanced treatments for illnesses like schizophrenia.” nine0003
The nearly 2.5 million people with schizophrenia—one percent of the US adult population—are looking forward to progress in understanding and treating this complex disease.
Dr. Husseini Manji,
Head of Global Therapeutic Area Neurology at Janssen
Schizophrenia is one of the most severe mental illnesses. It usually manifests itself in late adolescence or after 20 years of age. Its consequences can be catastrophic: people with schizophrenia are at increased risk of becoming unemployed, homeless and incarcerated.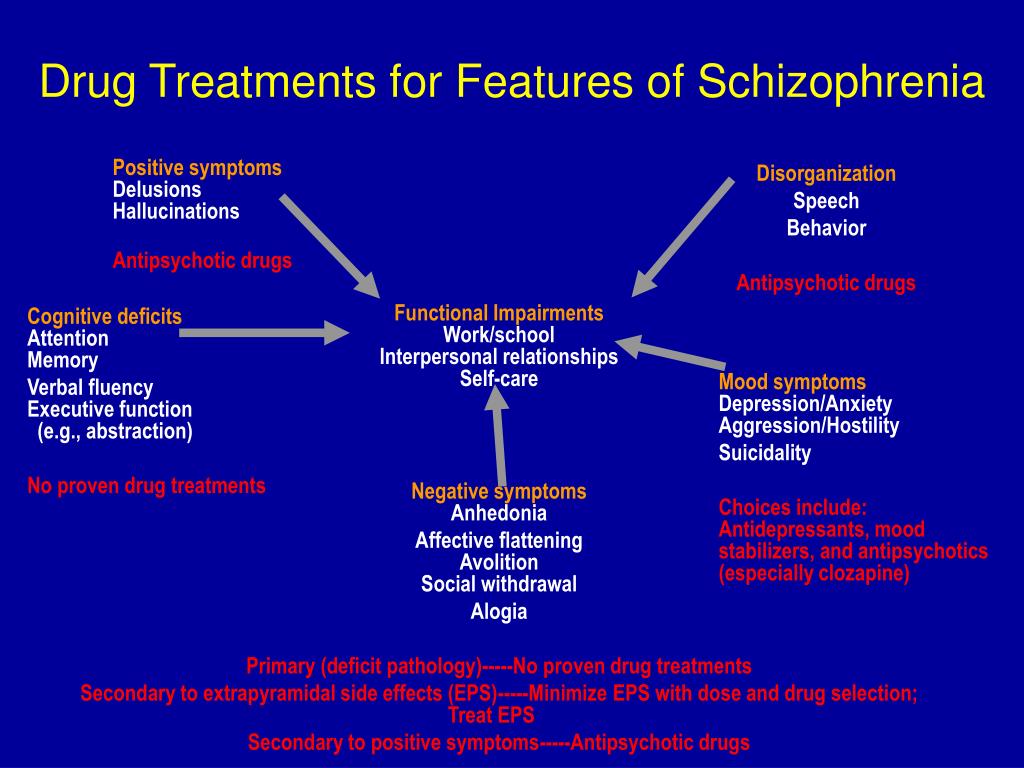 About a third of patients attempt to commit suicide, and about one in ten eventually succeeds. nine0003
About a third of patients attempt to commit suicide, and about one in ten eventually succeeds. nine0003
Researchers know that schizophrenia is largely hereditary, but they know less about the biological basis of the disease. However, thanks to advanced brain imaging technologies, scientists such as Dr. Manji are beginning to gain a clearer picture of the changes taking place in the brain of a person with schizophrenia. It turns out that these changes occur even before the onset of clinical symptoms.
Study of the brain of a patient with schizophrenia
Over the past decade, several brain imaging studies have provided evidence that structural abnormalities are present in the brains of patients with schizophrenia. This gave scientists clues to the biological causes of the disease and how it progresses.
In one 15-year study funded in part by Janssen and described in the American Psychiatric Journal ( American Journal of Psychiatry ), it was found that during the first attack of psychosis, patients had less brain tissue than healthy people. Although losses stabilized over time, long-term relapses of psychosis were associated with additional volume reductions.
Although losses stabilized over time, long-term relapses of psychosis were associated with additional volume reductions.
“We knew from earlier post-mortem studies of the brains of schizophrenic patients that they have fewer synapses and neural branches that allow neurons to communicate,” explains MD Scott W. Woods, Professor of Psychiatry and Director of the Research Clinic prodromal period of psychosis PRIME at Yale University. “We think this explains the reduction in brain tissue seen on the scans.” nine0003
During adolescence, everyone experiences a normal loss of a certain amount of gray matter, which contains neurons and their short processes, but experts believe that in people at high risk of developing schizophrenia, this process may proceed too quickly or actively, causing psychosis.
Imaging results indicate a lack of gray and white matter in the brains of people with schizophrenia. In adolescence, everyone experiences a normal loss of a certain amount of gray matter, which contains neurons and their short processes, but experts believe that in people at high risk of developing schizophrenia, this process may proceed too quickly or actively, causing psychosis.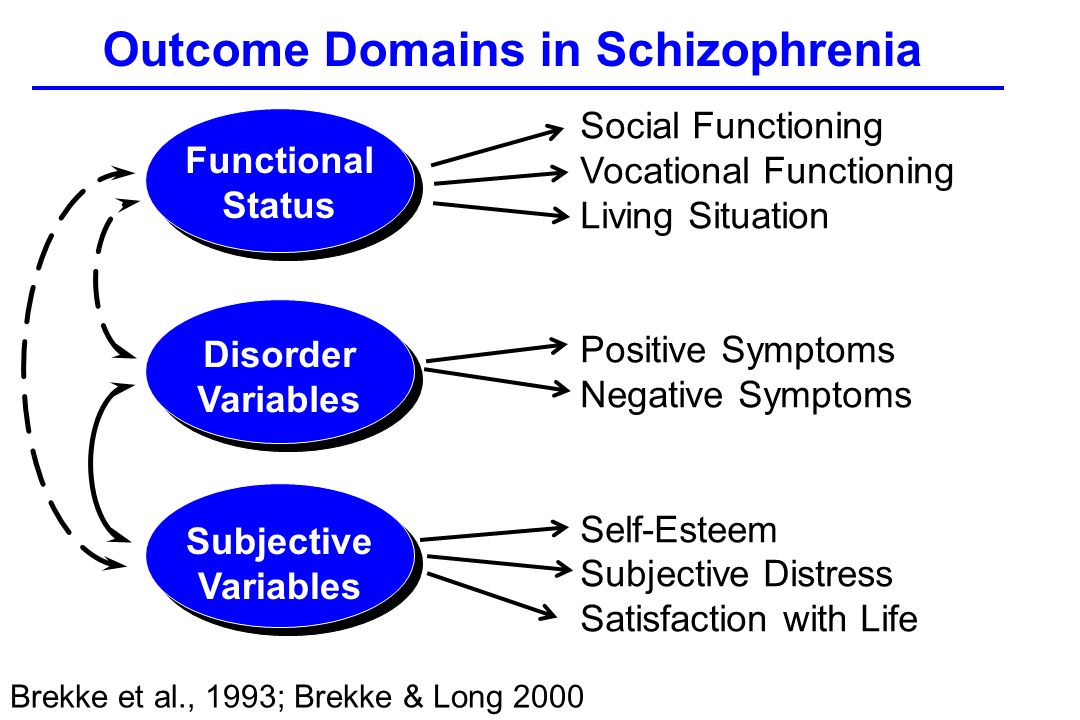 nine0003
nine0003
The abnormal development of white matter, which contains long, myelinated nerve fibers that connect the four lobes of the brain, can also be a tipping point for some people who are predisposed to this disease. The authors of the study, published in the journal Clinical Neuroimaging ( NeuroImage: Clinical ), suggest that this may be related to cognitive symptoms in patients with schizophrenia, including cognitive and memory impairments, apathy, and low motivation. nine0003
What causes these losses is still unknown, but a common theory is that inflammation contributes to the progression of many diseases. Two years ago, British researchers discovered increased activity of immune cells in the brains of schizophrenic patients and people at risk. It is not clear what exactly can serve as a stimulus for the onset of the inflammatory process, but in the course of previous studies it was possible to establish a link between infections at an early age and cases of schizophrenia. nine0003
nine0003
"Inflammation is one of the mechanisms leading to the destruction of synapses and neuronal branches in the brain, so severe inflammation could explain the loss," says Dr. Woods.
Advanced Brain Protection
By learning about these brain anomalies, Janssen scientists understand the importance of treating people at the earliest stage of schizophrenia and discovering new ways to minimize the damage caused by multiple relapses.
One of Janssen's major areas of research is finding ways to improve treatment adherence. This problem is faced by any doctor who treats chronic diseases, but it is especially difficult when working with patients suffering from schizophrenia. Only about half of patients are taking prescribed medications. Failure to adhere to the regimen sets off a cycle of relapse and return of symptoms that is difficult to break and weakens the response to treatment.
“Unfortunately, the nature of schizophrenia limits patients' understanding of the disease,” says Dr.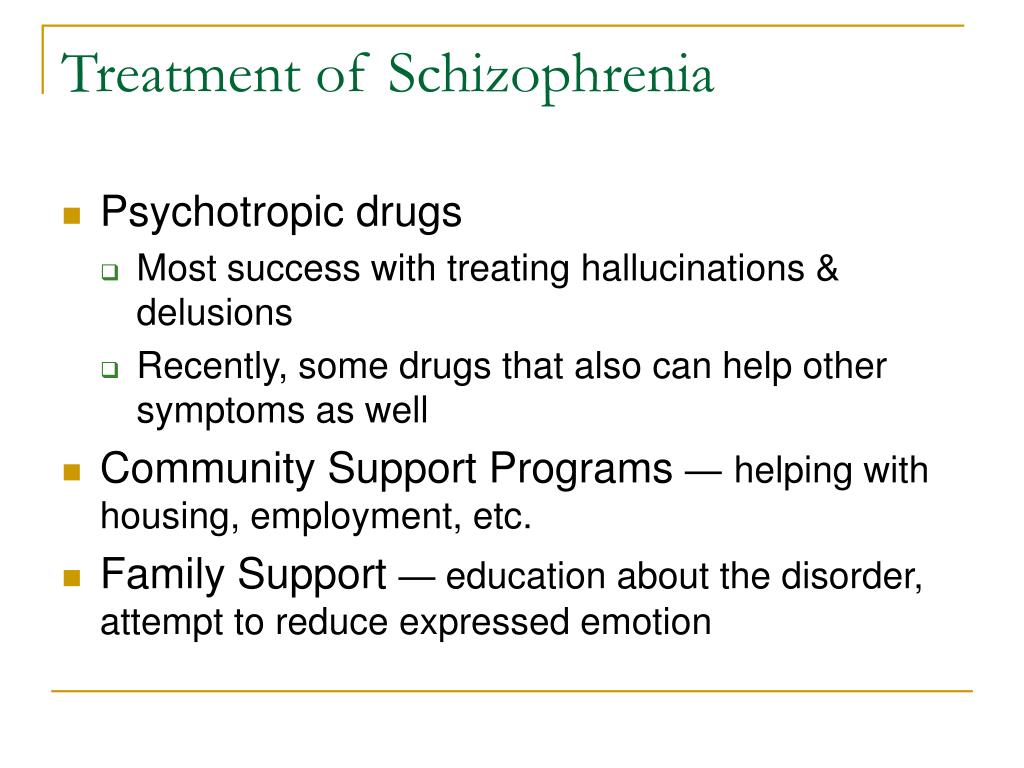 Manji. “In many cases, when they feel a little better, they stop taking the medication. However, unlike, for example, patients with diabetes, who feel the effects of missing a dose of insulin after only a few hours, patients with schizophrenia who stop taking antipsychotic drugs may not experience symptoms of relapse for several weeks. nine0003
Manji. “In many cases, when they feel a little better, they stop taking the medication. However, unlike, for example, patients with diabetes, who feel the effects of missing a dose of insulin after only a few hours, patients with schizophrenia who stop taking antipsychotic drugs may not experience symptoms of relapse for several weeks. nine0003
Janssen scientists have attempted to help reverse this severe cycle of relapse by developing long-acting injectable antipsychotics that are administered to patients less frequently than other drugs.
To further protect patients from the damaging effects of multiple relapses, Janssen is exploring ways to identify patients at high risk of relapse using data collected from smartphones, medical trackers and body sensors. nine0003
Long-acting injectables are administered by physicians, so if a patient misses a dose, the attending physician will know and take action.
To further protect patients from the damaging effects of multiple relapses, Janssen is exploring ways to identify patients at high risk of relapse using data collected from smartphones, medical trackers and body sensors.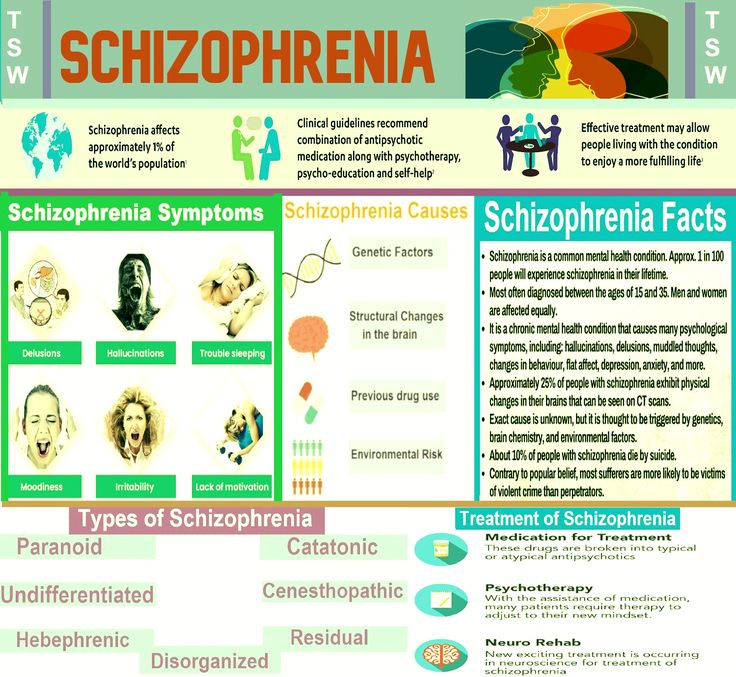
“We want to know if, by tracking factors such as sleep, activity levels, interactions with other people and other biomarkers, we can provide doctors with early information about an impending relapse,” explains Dr. Manji. “This would give them the ability to identify patients who are deteriorating and get in touch with them, instead of waiting for them to come to the appointment themselves.” nine0003
Among other things, incorporating medical technology into a patient's treatment plan would help clinicians gain more objective data about how a person is actually feeling. Practice shows that when patients are asked about their well-being for several weeks, they remember only the last day or two. With more long-term, measurable data, clinicians could not only have a relatively clear picture of how a patient is feeling, but also be more constructive in their appointments. nine0003
“If patients are stable and you don't have to spend so much time just dealing with psychotic symptoms, you can focus on finding constructive ways to help them get back to normal,” says Dr.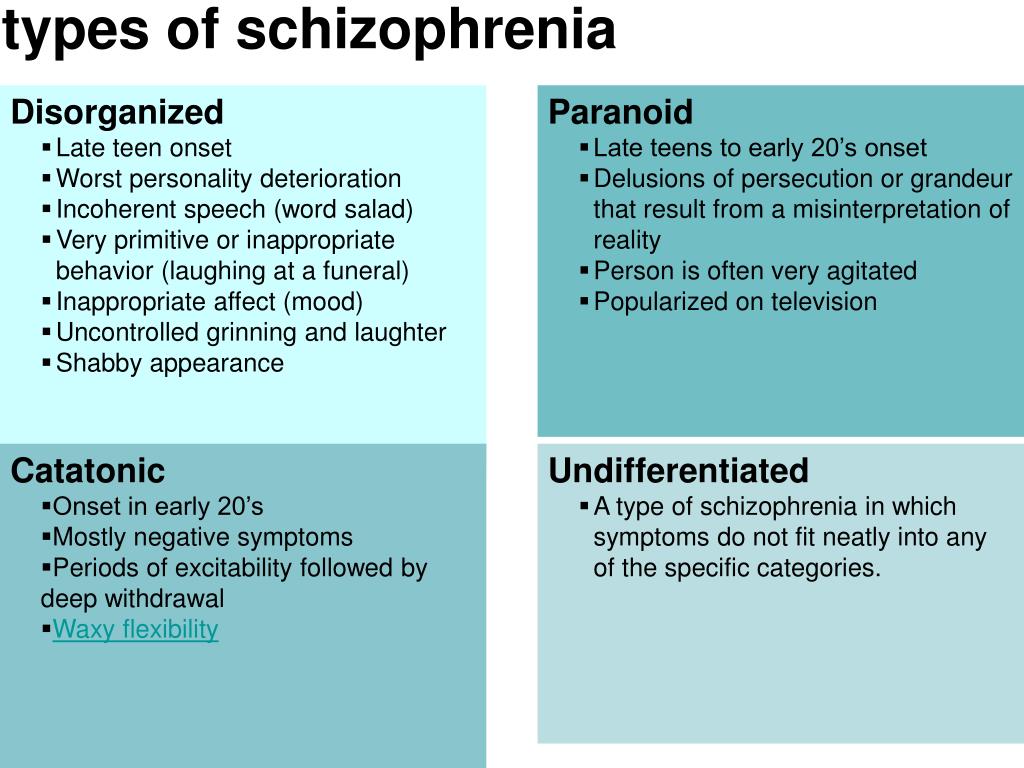 Manji.
Manji.
More than just symptom relief, it's a comprehensive treatment
To truly improve the lives of people with schizophrenia, scientists are not only developing new drugs, but also promoting the principles of integrative care. Dr. Manji said he was drawn to work at Johnson & Johnson because the company shares his belief that medicine must go beyond pills to provide the best possible outcome for patients with schizophrenia. nine0003
“We want people to understand that the best way to treat schizophrenia in the long term is through a more holistic, integrated model of care,” he explains. Mental illness has a big impact on every aspect of a person's life: their physical health, behavior and relationships. Patients require several types of correction, and not just medication.”
One of Janssen's research focuses on the vital role of caregivers and the challenges they face in treating and caring for people with schizophrenia. Patients are currently being recruited for a one-year clinical trial called Family Intervention in Recent Onset Schizophrenia Treatment (FIRST). The scientists plan to evaluate the overall impact that caregivers can have on patients by participating in a program of psychological education and training for caregivers. Perhaps such programs will help reduce the number of treatment failures, such as psychiatric hospitalization and suicide or attempted suicide. nine0003
The scientists plan to evaluate the overall impact that caregivers can have on patients by participating in a program of psychological education and training for caregivers. Perhaps such programs will help reduce the number of treatment failures, such as psychiatric hospitalization and suicide or attempted suicide. nine0003
The company's sincere commitment to improving the lives of patients is reflected in its projects in partnership with academia, government and the biotechnology industry. “This disease is so complex that we need to come together to make progress in research,” says Dr. Manji.
In 2015, Janssen Research & Development launched the Open Translational Science in Schizophrenia (OPTICS), a forum for collaborative analysis of Janssen clinical trial data and publicly available information on schizophrenia provided by the National Institutes of Health. nine0003
In addition, the company is an industry partner in a recently formed consortium led by the Johns Hopkins University School of Medicine and the Salk Institute for Biological Research. The consortium aims to improve the quality of induced pluripotent stem cell technology, a tool that allows scientists to harvest skin cells from mentally ill patients and convert them into neurons. By building a neural model of schizophrenia using patient cells, scientists hope to gain new insights into the underlying mechanisms of the disease in order to develop more targeted treatments. nine0003
The consortium aims to improve the quality of induced pluripotent stem cell technology, a tool that allows scientists to harvest skin cells from mentally ill patients and convert them into neurons. By building a neural model of schizophrenia using patient cells, scientists hope to gain new insights into the underlying mechanisms of the disease in order to develop more targeted treatments. nine0003
Dr. Manji believes that such innovative projects will not only lead to new treatments for schizophrenia, but also approaches to delay and possibly even prevent the disease.
“We now know that schizophrenia, like many other diseases, does not strike people overnight,” he explains. “It matures before a person develops full-blown psychosis, and the sooner treatment is started, the better the long-term prognosis will be.
If we learn to identify people at high risk of developing schizophrenia and learn what happens to them at the earliest stages, then in the long run we can change the entire trajectory of the disease. ” nine0107
” nine0107
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- Newsletter
- The facts are clear nine0106 b
- s
- b
- e
- u
- i
- WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements nine0107
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO Data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Highlights "
- About WHO »
- General director
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
nine0172 - Main page/
- Media Center /
- Newsletters/
- Read more/
- Schizophrenia
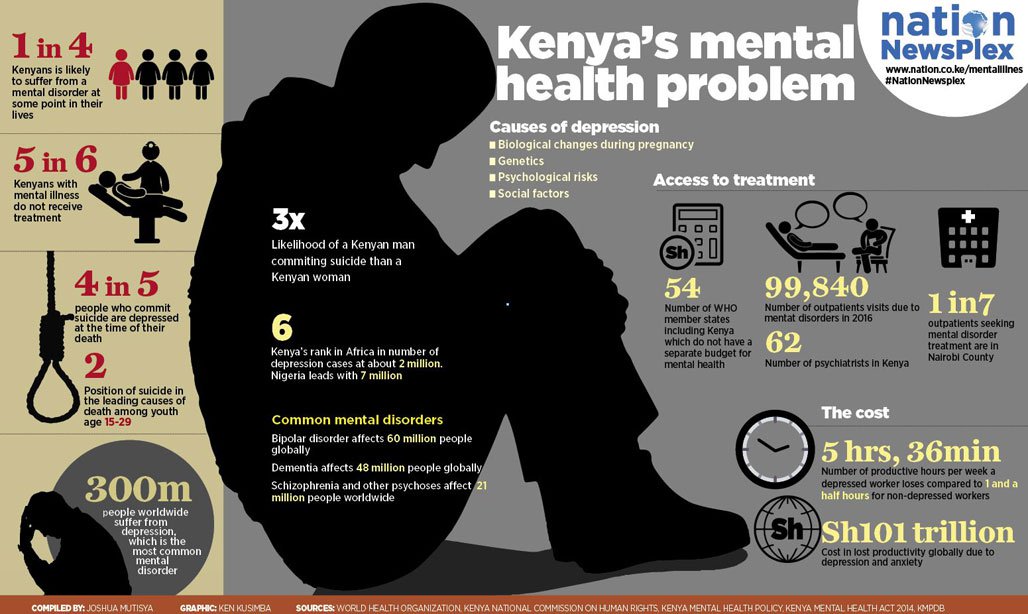
- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.
- Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life. nine0030
- People with schizophrenia are often subject to stigma, discrimination and human rights violations.
- Worldwide, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective options for helping patients with schizophrenia, which can lead to a complete recovery of at least one in three patients.
Key Facts
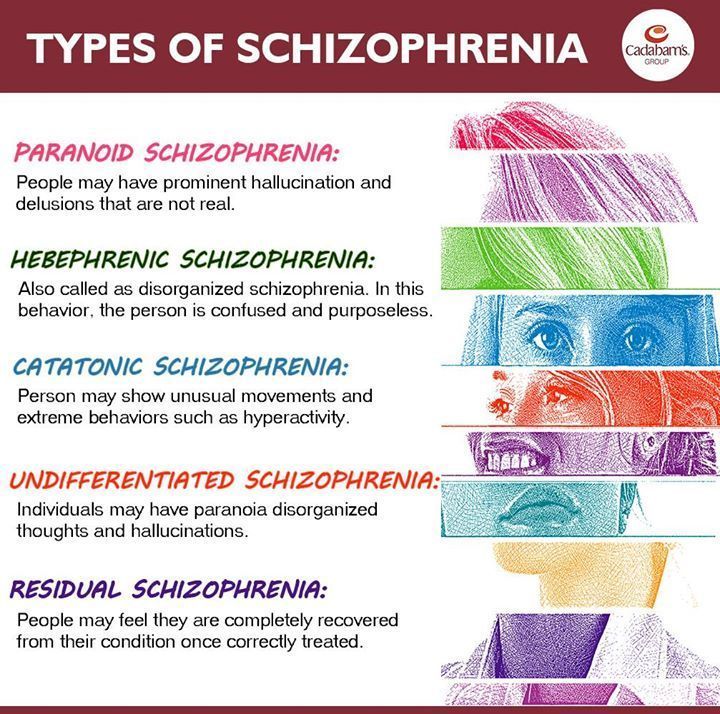
Symptoms
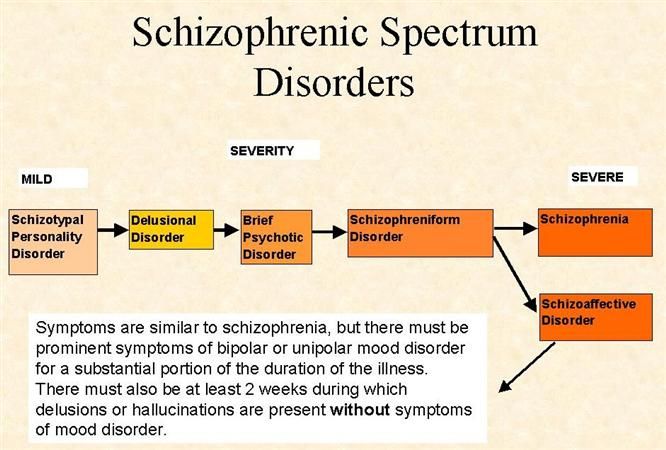
Schizophrenia is characterized by significant disturbances in the perception of reality and behavioral changes, such as:
- persistent hallucinations: the patient hears, sees, touches non-existent things and smells non-existent smells;
- feeling of external influence, control or passivity: the presence in the patient of the feeling that his feelings, impulses, actions or thoughts are dictated from outside, put in or disappear from consciousness at the will of others, or that his thoughts are broadcast to others; nine0107
- disorganized thinking, often expressed in incoherent or pointless speech;
- significant disorganization of behavior, such as the patient performing actions that may seem strange or meaningless, or an unpredictable or inappropriate emotional response that prevents the patient from organization of their behavior;
- "negative symptoms" such as extreme poverty of speech, flatness of emotional reactions, inability to feel interest or pleasure, social autism; and/or
- Extreme agitation or, on the contrary, slowness of movements, freezing in unusual postures.
People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms. nine0003
Magnitude of the problem and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease. nine0003
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.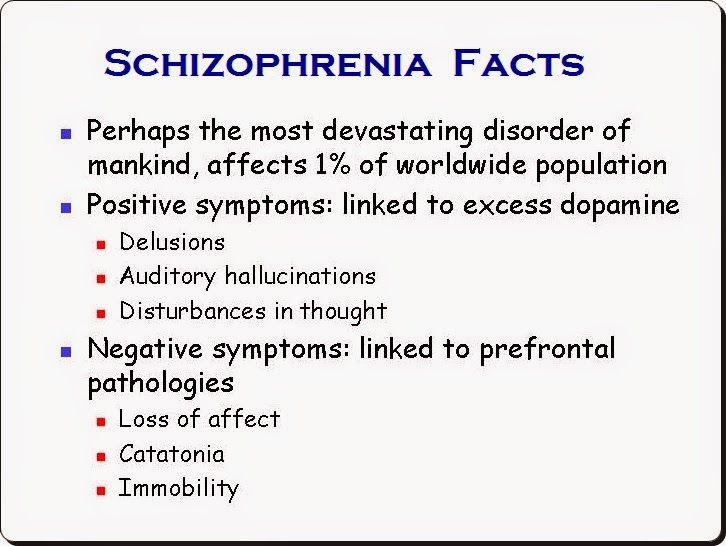
Individuals with schizophrenia are 2-3 times more likely to die early than the population average (2). It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment. nine0003
Humanitarian emergencies and health crises can cause intense stress and fear, disrupt social support mechanisms, cause isolation and disrupt health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease.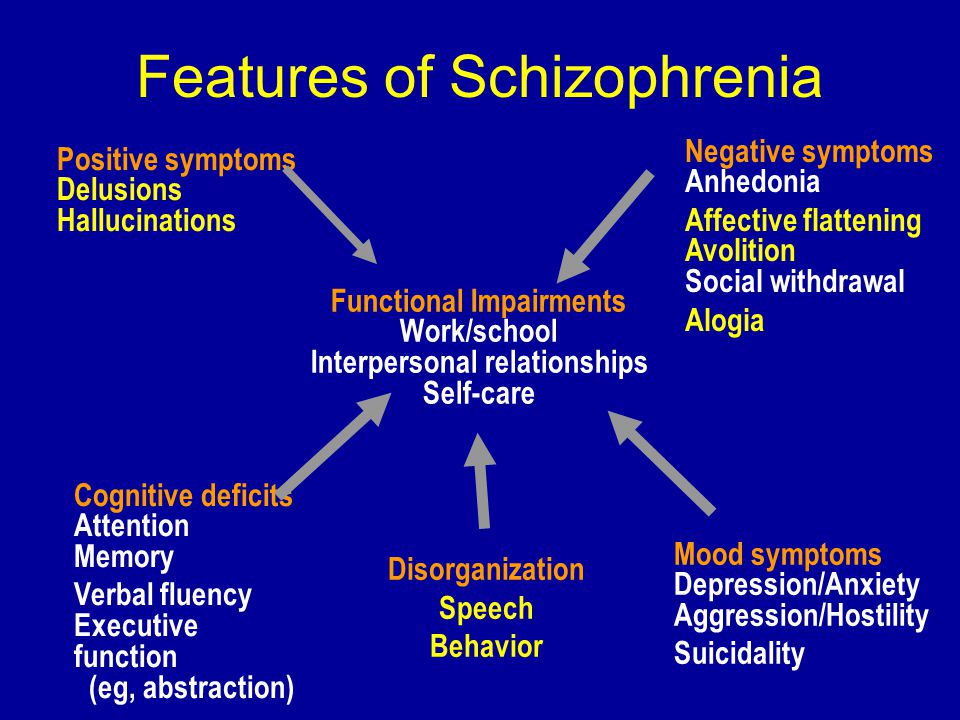 People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion. nine0003
People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion. nine0003
Causes of schizophrenia
Science has not established any one cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.
Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective way of providing care for mental disorders and is regularly associated with the violation of the basic rights of patients with schizophrenia. Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is important the patient with schizophrenia, his family members and members of local communities. nine0003
nine0003
Schizophrenia management and care
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg, life skills education). The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care. nine0003
WHO activities
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care. nine0003
nine0003
The WHO Mental Health Gap Action Program (mhGAP) is developing evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings. The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States. nine0003
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services.