How to help a family member with mental illness
When a family member chooses not to seek help
The Toronto Transit Commission (TTC) is conducting repairs to the streetcar tracks, streetcar platforms and bike lanes along College Street. The repairs are expected to start on September 5, 2022 and end in December 2022.
Learn more
If you are in an emergency, in crisis or need someone to talk to, there is help.
View Crisis Resouces
Skip to content
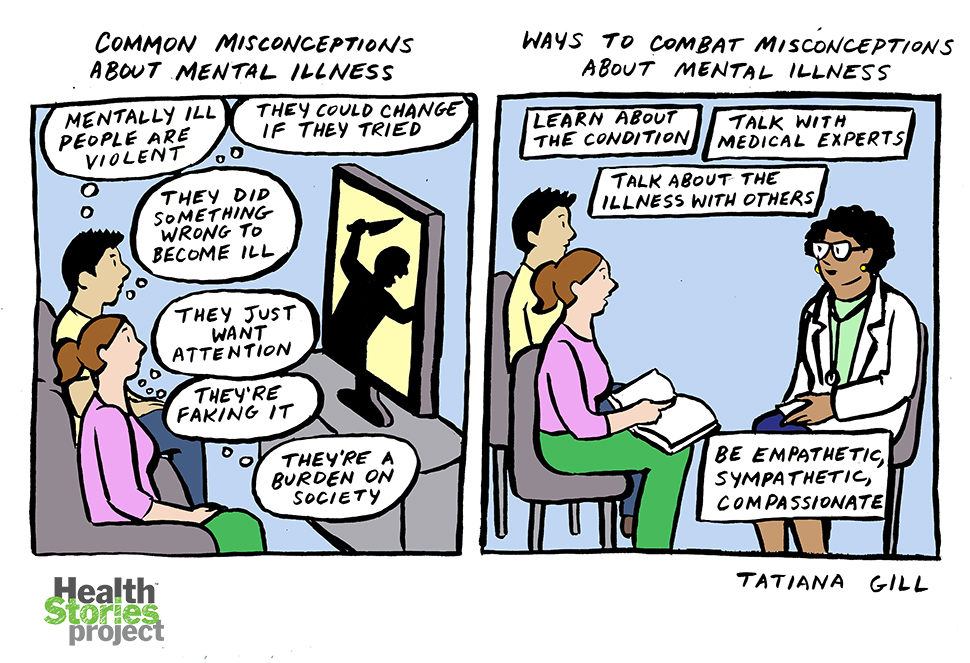
Search results forPeople with mental health or addiction problems are not always willing to seek treatment. They may not believe there is a problem. Or they may feel that they can address the issue on their own, without treatment. The person may also have fears about the mental health system or concerns about the stigma of a mental health or addiction diagnosis. This is a difficult situation for families. While your family member may not see the need for treatment, you are witnessing the situation and feel they need support.
How should I talk to my family member?
You may be tempted to repeatedly urge, plead or even threaten your family member into seeking treatment. Unfortunately, this often results in a breakdown of communication and the person shutting you out.
Try to use “I” statements rather than “you” statements to express your concerns about the importance of treatment. “I” statements focus on your own feelings or beliefs rather than criticizing or directing the other person. This approach may allow you to get your point across without making your family member feel defensive.
For example, instead of saying “You need to get help!” say “When I hear you talking about how unhappy you are, I feel worried. I think it would be really helpful for you to talk with someone about how you’re feeling.”
What can I do?Learn about mental illness and addiction
It can be easier to cope when you feel informed about what your family member is experiencing. Many resources are available, but sometimes it is difficult to know what information is accurate. The “Resources” section in this pamphlet is a good place to start. There may also be education sessions that you can attend.
Many resources are available, but sometimes it is difficult to know what information is accurate. The “Resources” section in this pamphlet is a good place to start. There may also be education sessions that you can attend.
Talk to your family member about your concerns, and encourage them to seek support
Let your family member know you are concerned. Consider how best to express your concerns. See the “How should I talk with my family member?” section for suggestions.
Suggest that the person see their family doctor or make an appointment at a treatment centre. Ask about the referral process and eligibility criteria and about culture-specific or specialized services (e.g., LGBTQ2S+, spiritually focused) to best meet your needs.
Get support for yourself and your family
It is helpful to get connected with family support. This could include attending an education session, meeting with a therapist or joining a support group. There are also peer family supports in the community. See the “Resources” section for suggestions on where you can find support.
See the “Resources” section for suggestions on where you can find support.
Take care of yourself
Supporting a family member with a mental illness or addiction can be overwhelming. It can be a challenge to balance your own needs with being there for them. Take time for yourself and ensure that your own needs are being met—you cannot support your family member effectively if you are not also taking care of yourself.
- Make time for activities that help you cope with stress.
- Make time to see other family members and friends.
- Don’t be afraid to ask friends and family for help.
- Be aware of your boundaries and set limits to make sure they are respected.
- Look after your own physical and mental health, and seek support if necessary.
Support other family members
Mental illness and addiction affect the whole family, as well as the person’s friends. It is important that everyone receives the support they need.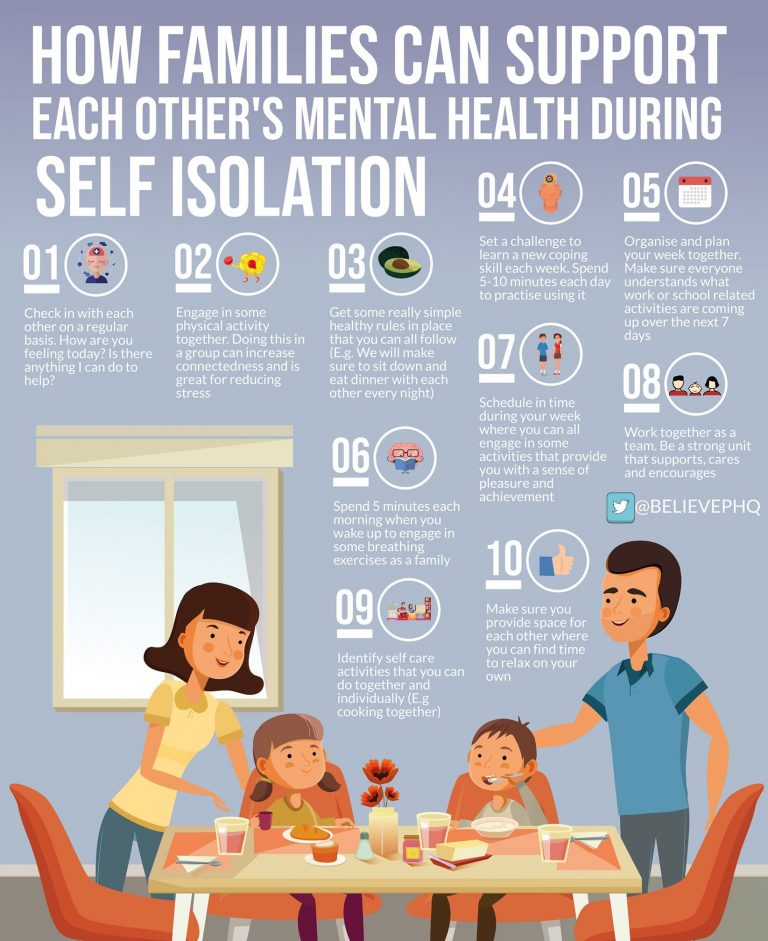 Give what support you can, without overwhelming yourself, and direct others to the resources listed at the end of this pamphlet.
Give what support you can, without overwhelming yourself, and direct others to the resources listed at the end of this pamphlet.
Children in particular may need help to understand what is happening. If you are concerned about how a child is coping, you could speak to their family doctor. Support may also be available from a school social worker or through a community organization.
How do I prepare for a crisis?Try to predict possible crises and plan what you would do. A crisis plan should include contact information for:
- the nearest hospital
- crisis lines
- the local police department
- a treatment provider
- a child care provider, if relevant
- family members or supportive friends.
The CAMH pamphlet When a Family Member Is Thinking about Suicide lists crisis lines and other supports.
What if I think my family member may harm themself or someone else?- If there are immediate concerns for your family member’s safety, take them to the nearest hospital emergency department if you can do so safely.
- If they are unwilling to go to the hospital, call 911. Calling 911 can feel hard. You can explain to the 911 operator that you think your family member is experiencing mental health symptoms, in case a mental health crisis response team is available.
- After calling 911, you might want to access support to help feel connected and know that you are not alone.
- If your family member is agitated, threatening or aggressive, call 911 and make sure you and others are safe.
Everyone has the legally protected right to decide if they want treatment. Treatment is usually most effective when the person has agreed to it. However, in some situations, the Mental Health Act provides ways for people to receive an emergency assessment without their consent.
Form 1
If a physician believes a person is a risk to themself or others, they can write a Form 1.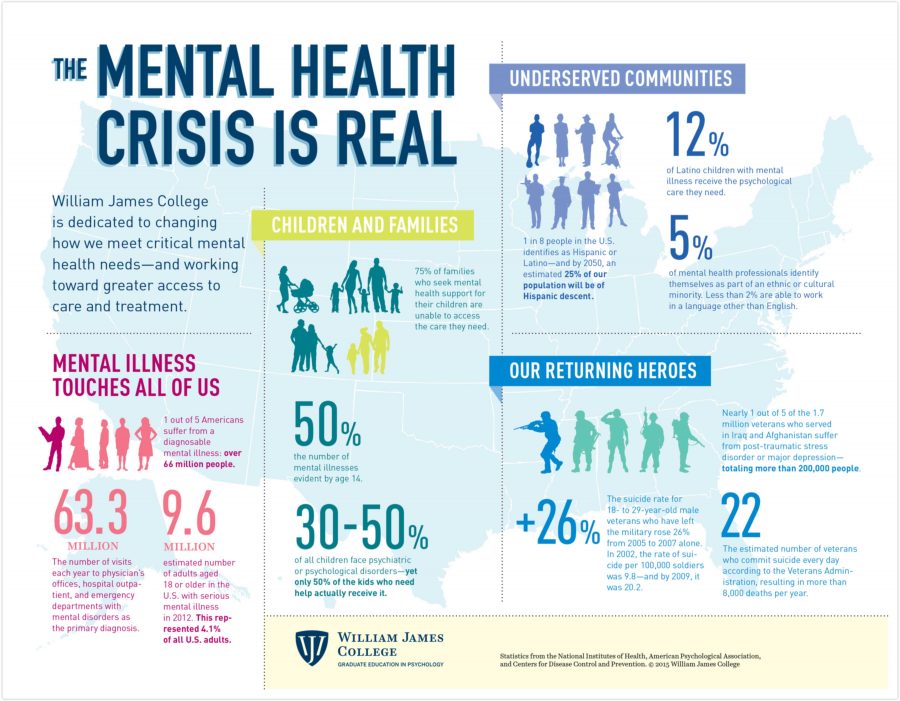 The person may remain in hospital for up to 72 hours while they receive an emergency assessment.
The person may remain in hospital for up to 72 hours while they receive an emergency assessment.
If the person is not found to be a risk to themself or others, they can leave the hospital if they wish, even if it is against medical advice. If the psychiatric team finds that the person is a risk to themself or others, they may be held in hospital under other forms in the Mental Health Act until they are found to be safe to leave.
Form 2
If you are concerned that a family member is a risk to themself or others, you can request a Form 2 from a justice of the peace (www.ontariocourts.ca/ocj). This form allows the police to take the person to a hospital for assessment. At the hospital, a physician will assess
the person to see if they should be put on a Form 1.
Using a Form 2 can negatively affect the relationship you have with your family member. However, the safety of your family member and those around them is the most important consideration.
The police may also take a person to hospital if they, or someone else, have seen the person behaving dangerously as a result of a mental health concern, or if they have a Form 1 or Form 2.
Resources
ConnexOntario
Tel.: 1 866 531-2600
www.connexontario.ca
Mood Disorders Association of Ontario
www.mooddisorders.ca
Canadian Mental Health Association
www.cmha.ca
Family resources
CAMH
Access CAMH family line
Tel.: 416 535-8501 ext. 2
Family Resource Centre
Tel.: 416 535-8501 ext. 33202
Email: [email protected]
www.camh.ca/families
FAME Reconnect Family and
Caregiver Support Services
Tel.: 416 248-2050
www.reconnect.on.ca
Mood Disorders Association of Ontario
https://mooddisorders.ca
Ontario Caregiver Organization
24/7 helpline: 1 833 416-2273
https://ontariocaregiver. ca
ca
Supports for children and youth
Reconnect FAMEkids
Tel.: 416 248-2050
www.reconnect.on.ca
What Kids Want to Know series (CAMH)
(When a Parent Drinks Too Much Alcohol,When a Parent Has Bipolar Disorder, When a Parent Is Depressed, When a Parent Has Experienced Psychosis)
http://store.camh.ca
Your donation will fund the groundbreaking mental health research that is helping people on the path to recovery.
Give OnceGive Monthly
My gift is in memory or honour of someone
I am donating on behalf of an organization
Other Ways to Give
Coping with Mental Illness in the Family
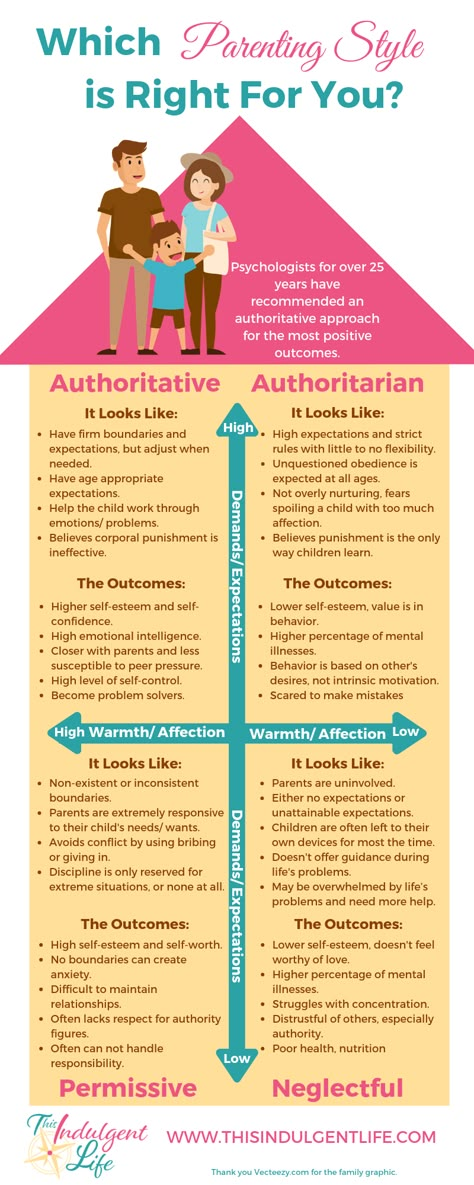
Growing up in any family can be challenging at times. However, there are often unique issues when a family member or family members have a mental illness. Members of these families often have to deal with instability or unpredictability. Often there is confusion in family roles. For example, children or other family members may have to take over many of the parents’ responsibilities, such as taking care of younger siblings or managing household duties usually managed by parents. They may even have the responsibility of taking care of the emotional or physical needs of their parents. Children or other family members in these situations do not always receive the care and nurturing they need. In addition, individuals who have a family member with a mental illness may feel ashamed to talk about their situation with others and consequently may withdraw from relatives or friends who could help them or support them. Oftentimes they may have difficulties to recognize and express their needs to others and even to themselves. As a result, these individuals frequently feel isolated and alone.
However, there are often unique issues when a family member or family members have a mental illness. Members of these families often have to deal with instability or unpredictability. Often there is confusion in family roles. For example, children or other family members may have to take over many of the parents’ responsibilities, such as taking care of younger siblings or managing household duties usually managed by parents. They may even have the responsibility of taking care of the emotional or physical needs of their parents. Children or other family members in these situations do not always receive the care and nurturing they need. In addition, individuals who have a family member with a mental illness may feel ashamed to talk about their situation with others and consequently may withdraw from relatives or friends who could help them or support them. Oftentimes they may have difficulties to recognize and express their needs to others and even to themselves. As a result, these individuals frequently feel isolated and alone.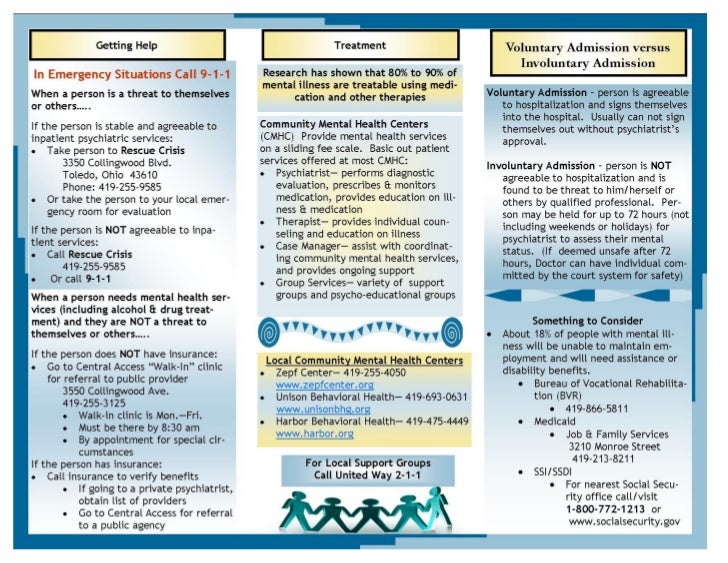
Common Difficulties
Individuals who cope with chronic and severe mental illness in the family may also experience other difficulties outside of their family-of-origin relationships. These may include:
Relationship Difficulties
- Difficulty in relationships and experiencing feelings of isolation.
- Difficulty in initiating romantic relationships and friendships.
- Difficulty in maintaining romantic relationships and friendships.
- Difficulty with trusting self and others.
- Difficulty balancing level of intimacy (excessive dependence or excessive avoidance).
- Difficulty balancing taking care of self and taking care of others.
- Difficulty setting and enforcing healthy boundaries with others.
Emotional Difficulties
- Guilt
- Anger or resentment
- Shame or embarrassment
- Depression
- Helplessness
- Tiredness
- Fear of inheriting a family member’s mental illness
- Fear of discovery by others, including one’s partner and friends
Behavioral Difficulties
- Angry outbursts or repressed anger.

- Inability to deal with life unless it is chaotic or in crisis.
- Overly responsible or irresponsible in many areas of life such as commitments, money, alcohol, relationships, etc.
- Self-defeating thoughts, attitudes, and behaviors such as “My needs don’t matter; I’m not worth much; It’s no use trying.”
- Self-defeating themes involving a tendency to equate achievement with worth as a person, such as, “Maybe I can matter if I can excel at something, be perfect in school, my job, or my relationships. But if I fail, I’m worthless and it’s terrible.”
- If you are experiencing any of these difficulties, you are not alone. It is helpful to recognize that these relationship patterns, feelings, and behaviors helped you to cope and survive thus far, and during the more vulnerable years of childhood, they even served a coping function. However, it is also critical to recognize that they may be no longer helpful and functional at this time of your life. Your recognition that these difficulties may limit your life choices as an adult is an important first step towards developing new, rewarding, and functional ways of improving the quality of your life and relating to others better.
How You Can Empower Yourself
Acknowledge that you have a family member with a mental illness and how it affects you. It’s normal to have feelings such as anger, shame, and guilt. Remember that you’re not responsible for causing your family member’s problems or for fixing their condition. It’s also okay to grieve the parental or familial support you never received.
Develop new ways of taking care of yourself. Recognize that you have legitimate needs and stressors and that it’s completely acceptable to take care of yourself. Try to replace negative thoughts with more positive statements: “I am a worthwhile person. This truth does not depend on my successes or failures. My life has ups and downs, but my worth does not change.”
Develop new ways of relating to others. Be mindful of old, unhealthy patterns of communicating and practice new ways of relating to your family members. This may include setting and enforcing new boundaries and being respectful of your own limits.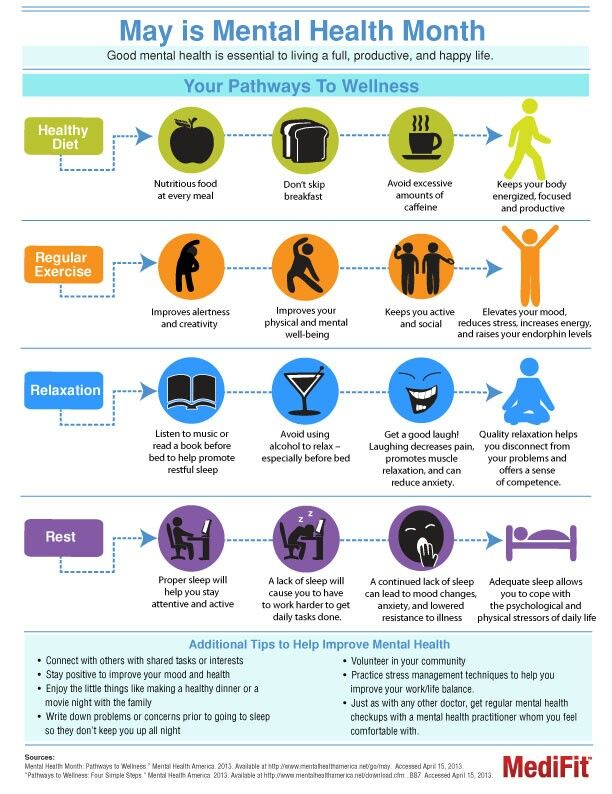 As things shift, appreciate and enjoy the stability in your relationships and recognize that relationships don’t have to be defined by crisis or dependency.
As things shift, appreciate and enjoy the stability in your relationships and recognize that relationships don’t have to be defined by crisis or dependency.
Educate yourself about your family member’s illness. Certainly, this does not mean that you need to know everything about the mental illness of your family member. Your job isn’t to treat or cure your family member, but educating yourself about the illness via reliable online and offline resources can help you understand what your family member is facing and what might have caused problems for your family. It can also help you calm guilt, anger, resentment, embarrassment, shame, and fear.
Consider seeing a mental health professional yourself. You may benefit from seeking assistance—not because you should assume that you are automatically inheriting your family member’s mental illness, but because a mental health professional can help you understand how a family member’s mental illness affects your life and help you explore your unmet or repressed needs and emotions.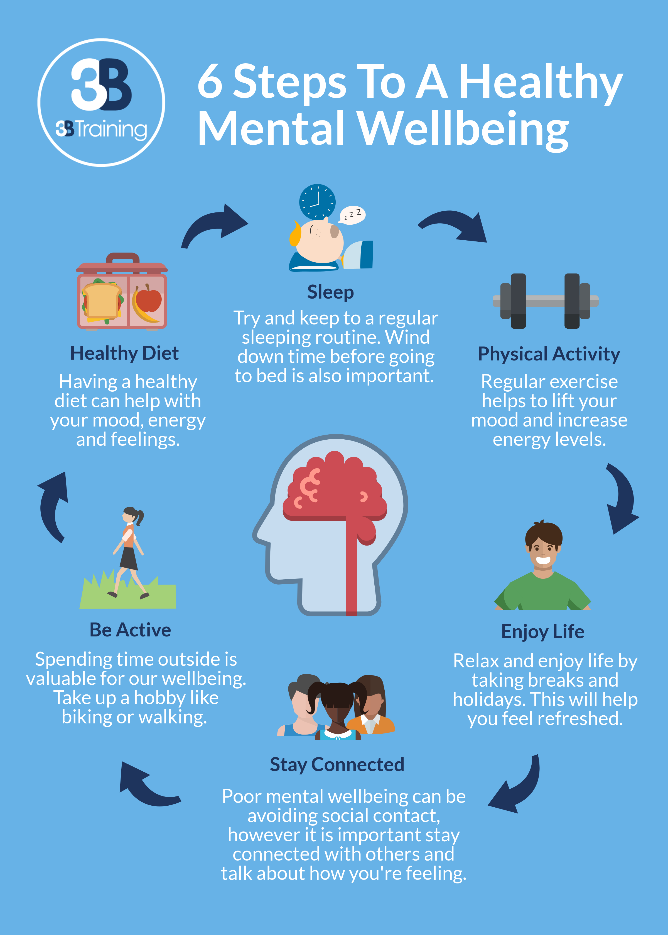 Further, your mental health professional can help you learn and develop healthier ways of caring for yourself, relating to others, and coping with your difficulties in relationships, emotions, and behaviors, if you experience any.
Further, your mental health professional can help you learn and develop healthier ways of caring for yourself, relating to others, and coping with your difficulties in relationships, emotions, and behaviors, if you experience any.
Join a support group. A support group that addresses your specific situation can help reduce feelings of isolation and validate your experience. Seeking support can be especially helpful when other family members are either uncomfortable with or refuse to acknowledge the problem. If an appropriate in-person support group is not available in your community or you are unable to join a group, there may be an online support community available.
Want to Know More?
Sederer, L. I. (2015). The Family Guide to Mental Health Care. W.W. Norton & Company.
Rosalyn, C. (2011). Helping someone with mental illness: A compassionate guide for family, friends, and caregivers. New York: Three Rivers Press.
Glynn, S. M., Kangas, K., & Pickett, S. (July, 2018). How to cope when a loved one has a serious mental illness. Retrieved from: http://www.apa.org/helpcenter/serious-mental-illness.aspx
M., Kangas, K., & Pickett, S. (July, 2018). How to cope when a loved one has a serious mental illness. Retrieved from: http://www.apa.org/helpcenter/serious-mental-illness.aspx
Glynn, S. M., Kangas, K., & Pickett, S. (July, 2018). Supporting a family member with serious mental illness. Retrieved from: http://www.apa.org/helpcenter/improving-care.aspx
Morton, K. (June 7, 2018). How to deal with a mentally ill parents. Retrieved From: https://www.youtube.com/watch?v=hnDE09zumb8 Morton, K. (Aug 4, 2014).
How to deal with family and their mental health. Retrieved From: https://www.youtube.com/watch?v=wbDhkxIh-4INational Alliance on Mental Illness (July, 2018).
Taking care of yourself. Retrieved from: https://www.nami.org/Find-Support/Family-Members-and-Caregivers/Taking-Care-of-Yourself
IF A RELATIVE IS SUFFERING WITH A MENTAL DISORDER…
Vakulchik Irina Sergeevna, Deputy Chief Physician for Medical Affairs of the City Clinical Psychiatric Dispensary
The news that a loved one has a mental disorder can be shocking. At first, confusion and denial are characteristic - "this could not happen to us." The familiar world is collapsing, a new, unclear and frightening reality is approaching, and you have to learn to live in it. Mental illness causes suffering not only to the patient, but also to his relatives, to a greater or lesser extent affecting all family members, changing their lives, plans for the future and relationships between them. In order for life to take place at a higher level of quality, the patient needs the help and support of the whole family. Very often, relatives want to help, but do not know, do not understand how. It has long been known that family relationships can influence the course and outcome of the disease, contribute to both the improvement of the patient's condition and its aggravation.
At first, confusion and denial are characteristic - "this could not happen to us." The familiar world is collapsing, a new, unclear and frightening reality is approaching, and you have to learn to live in it. Mental illness causes suffering not only to the patient, but also to his relatives, to a greater or lesser extent affecting all family members, changing their lives, plans for the future and relationships between them. In order for life to take place at a higher level of quality, the patient needs the help and support of the whole family. Very often, relatives want to help, but do not know, do not understand how. It has long been known that family relationships can influence the course and outcome of the disease, contribute to both the improvement of the patient's condition and its aggravation.
The most general, universal recommendations for dealing with people suffering from mental disorders.
To begin with, try to learn more about the disease that your relative suffers from, about its manifestations. Knowledge will help you deal with their sometimes "strange" behavior and cope more successfully with the problems that arise due to illness.
Knowledge will help you deal with their sometimes "strange" behavior and cope more successfully with the problems that arise due to illness.
A mentally ill person does not quite adequately perceive reality and has deviations in behavior. Communication with such people may also deviate from existing norms. The main thing to remember is that a person is not just behaving abnormally, he is sick. One of the features is that such patients need long-term observation and treatment. During treatment, symptoms may come and go. You, as members of the family, should know what to expect from a relative when doing household chores or interacting with other people. For example: you should not require a patient who has just been discharged from the hospital to immediately go to work or even to look for work. At the same time, there is no need to overprotect your relative, underestimating the requirements for him.
Take part in the treatment . Find out which treatment programs are best for this disease and encourage your relative to take part in these programs; Make sure that he takes his prescribed medications, and if he stops taking them, notify the doctor. Also tell which medications are best for your relative.
Also tell which medications are best for your relative.
Help to avoid stress . After all, people suffering from mental disorders often find it difficult to endure situations when they are shouted at, annoyed, or required to do something that they are not able to do. You can help your relative avoid stress by doing the following:
- talk to him calmly, do not say anything that can piss him off, deservedly praise for good deeds.
- do not argue and do not try to deny the existence of manifestations of the disease that you may not see or hear.
- keep in mind that ordinary events - moving to a new place of residence, marriage, or even a festive dinner - can irritate patients suffering from mental disorders.
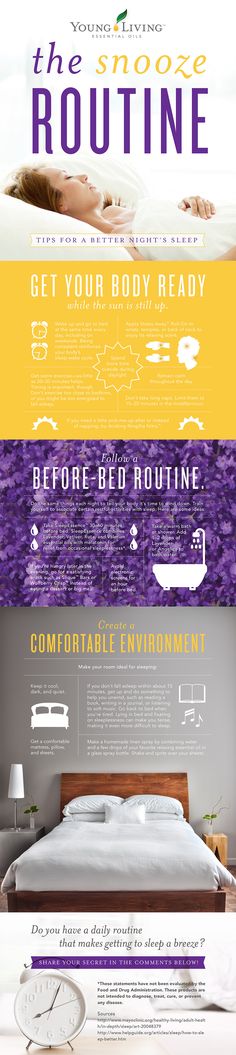
Habitual routine . An important point that stabilizes the condition of a sick person is the preservation of the usual, simple life routine in the house, for example, a stable time to get up in the morning, sleep time, and meal hours. It is necessary to create a calm, consistent, predictable life as much as possible. This will enable the sick person to cope with anxiety, confusion, to understand what and at what time you expect from him and what to expect from you in turn. Try to make the life of a sick person as ordered as possible, this will protect you from chaos!
It is necessary to create a calm, consistent, predictable life as much as possible. This will enable the sick person to cope with anxiety, confusion, to understand what and at what time you expect from him and what to expect from you in turn. Try to make the life of a sick person as ordered as possible, this will protect you from chaos!
Try to be calm . You must keep in mind that a person suffering from a mental illness may experience strong feelings, his thoughts may be confused, flow too slowly, or, on the contrary, quickly, and his feelings may be very strong and contradictory. Communicating with a sick person, especially during periods of deterioration in his condition, it is important to learn to behave calmly and with restraint. Such behavior contributes to the stabilization of the mental state, and in some cases even helps the patient to calm down and cope with anxiety.
Learn how to respond correctly to the manifestations of the disease.
| Symptom or characteristic | What to do. |
| Difficulty concentrating | Be brief, repeat what has been said. |
| Irritability, anger | Do not argue, do not aggravate the discussion, limit communication. |
| Inadequate judgments, statements | Do not rely on rational discussion, do not try to convince. |
| Delusional beliefs | Do not argue, but do not support crazy statements. |
| Little empathy for others, emotional coldness | Treat as a symptom of mental illness. |
| Closed | Be the first to start a conversation, try to involve in communication. |
| Fear | Keep calm yourself, try to calm the sick person. |
| Self-doubt | Treat with love and understanding. |
| Low self-esteem | Be respectful, maintain a positive attitude |
Celebrate and encourage even small successes, manifestations of improvement. It is important to set really realistic goals. Get out of bed, get dressed, brush your teeth, wash the dishes, it's not so little. Celebrate even such successes, because self-esteem is built from these bricks. You need to learn to find certain positive signs, and sometimes just words of support and approval in difficult, crisis periods of the disease. And if a sick person himself paid attention to the approaching symptoms of an exacerbation of the condition and decided to go to the hospital, it would be very useful to support him, express approval and say that the ability to independently recognize the approaching exacerbation of the condition is the key to successful prevention of attacks of the disease in the future.
You need to learn to find certain positive signs, and sometimes just words of support and approval in difficult, crisis periods of the disease. And if a sick person himself paid attention to the approaching symptoms of an exacerbation of the condition and decided to go to the hospital, it would be very useful to support him, express approval and say that the ability to independently recognize the approaching exacerbation of the condition is the key to successful prevention of attacks of the disease in the future.
Do not lose hope for recovery, maintain an optimistic attitude. It is very important and at the same time very difficult not to lose hope for recovery. Often a chronically ill person has a hard time, a painful condition can last for months and years, taking away hope for recovery, or at least for a significant relief of the condition. Friends, peers have gone far ahead in life, got a profession, have their own families. It may so happen that it will never be available to a sick person. Therefore, encourage the activity of a sick person, his independence, desire for activity, try to build relationships in such a way that he does not take a passive role in life, declaring himself an invalid and refusing to perform his duties. It is very important that a person suffering from a mental disorder strive for the most independent life.
Therefore, encourage the activity of a sick person, his independence, desire for activity, try to build relationships in such a way that he does not take a passive role in life, declaring himself an invalid and refusing to perform his duties. It is very important that a person suffering from a mental disorder strive for the most independent life.
Show love and respect for your relative. Remember that he often gets into unpleasant situations and sometimes treats himself badly because of illness. By your daily behavior, show that he, no matter what, remains a respected and beloved family member for you. Treat a sick person with respect and love, even if you remind the sick person several times a morning to brush their teeth, sweep the room, change clothes, and clean up the dishes. Never insult the dignity of a sick person!
Healthy family members should remember that their own well-being is fundamentally important: the better they feel, the better not only for themselves, but also for the sick person. Therefore, you should protect yourself from "burnout". The more care the patient needs, the more support the immediate family members need. You can try to distribute the care of the patient among several relatives. You can find help in support groups - to communicate and share experiences with other families who have encountered similar difficulties.
Therefore, you should protect yourself from "burnout". The more care the patient needs, the more support the immediate family members need. You can try to distribute the care of the patient among several relatives. You can find help in support groups - to communicate and share experiences with other families who have encountered similar difficulties.
The optimal behavior of the family in relation to the patient involves maintaining a balance between the necessary help and care, on the one hand, and providing the patient with sufficient autonomy and independence, on the other. Such a balance must be based on a good understanding of the possibilities and limitations that the disease imposes. Patience, gradually acquired knowledge about the disease and treatment, support from specialists and others can help in this family.
what can help the family in overcoming the disease (in reduction), (end...) » GBUZ RB Sterlitamak Psychiatric Hospital
T. A. Solokhina, L.S. Shevchenko
A. Solokhina, L.S. Shevchenko
lecture 1 mental health professionals consider drug treatment to be the mainstay of management of patients with schizophrenia and other serious mental illnesses. Therefore, in both areas it is widely believed that the solution to the problem lies in the correct selection of drugs. However, the modern approach to the treatment of mental and behavioral disorders involves a balanced combination of its three main components: pharmacotherapy (drugs), psychotherapy and psychosocial rehabilitation. The features of each of them will be discussed in detail in other lectures. And here we will focus only on their definition.
Pharmacotherapy of mental disorders is determined by the use of mainly three classes of psychotropic drugs, the action of which is aimed at alleviating the symptoms of the disease. These drugs include antipsychotics (antipsychotics), which affect psychotic symptoms, antidepressants, used for depression, and tranquilizers, which are most commonly used for anxiety. We emphasize once again: these medicines are not focused on eliminating the cause of the disease, but on weakening its symptoms or preventing relapses.
We emphasize once again: these medicines are not focused on eliminating the cause of the disease, but on weakening its symptoms or preventing relapses.
Psychotherapy refers to interventions aimed at changing behavior, mood, emotional reactions through verbal (verbal) and non-verbal psychological means.
Psychosocial rehabilitation is a package of interventions that enables people with impaired mental health or mental disabilities to achieve an optimal level of independent functioning in society.
The volume of each component of the therapeutic process (pharmacotherapy, psychotherapy, psychosocial rehabilitation) depends not only on the main diagnosis, but also on the stage of the disease, the age of the patient, his living conditions. This means that the treatment should be as close as possible to the individual needs of the patient in a certain period of time. However, even an ideally selected treatment regimen does not always provide good results.
The best result is achieved when the patient and his immediate environment are not passive participants in the complex healing process, but active partners in providing care along with professionals.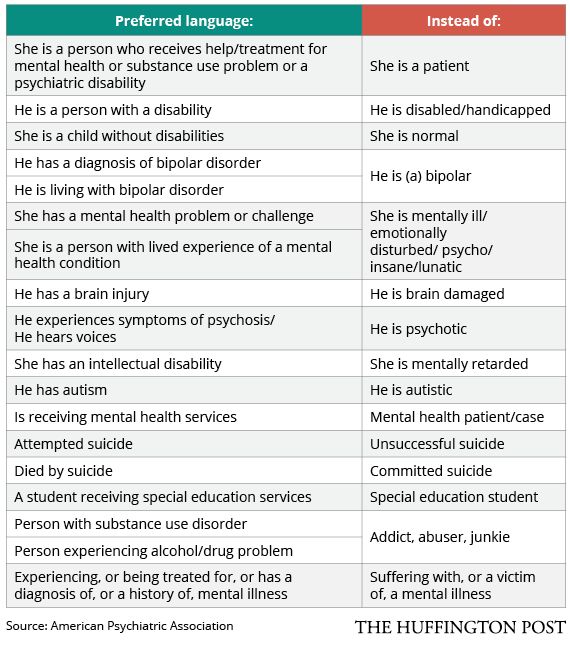
Conditions for the formation of partnerships are:
• the patient and his immediate environment have knowledge about the nature of mental illness and their treatment, style of communication and behavior in the family;
• Skills for solving disease-specific problems;
• Possession of ways to control the symptoms of the disease.
In most families, such knowledge and skills are minimal, and it is unrealistic to demand their acquisition by oneself. Relatives of patients should have access to the necessary information, as well as the opportunity to communicate with each other to share experiences reflecting their successes and failures, as well as to develop ways to solve the most common problems.
The following forms of work with families have been proven effective:
•psychiatric education;
•support groups.
Psychiatric education as a form of information and socio-psychological support for relatives of patients and the patients themselves began to be actively introduced in our country. In a number of foreign countries, the educational approach to helping families has been used for more than a decade. The results of scientific research have proved that psychiatric education is the basis for:
In a number of foreign countries, the educational approach to helping families has been used for more than a decade. The results of scientific research have proved that psychiatric education is the basis for:
•early treatment for yu during an exacerbation of the disease;
• prevention of exacerbations and repeated hospitalizations;
•understanding the mental world of a sick person.
The educational approach is based on the belief in the positive influence of the family on the relative's recovery process. However, back in the 1950s, there was an idea among doctors of the family as one of the main causes of mental disorder due to the incorrect attitude of its members towards the patient. The therapeutic effect consisted in using certain techniques to change the behavior of family members and thereby save the patient from the disease. This approach turned out to be a "failure" because the relatives did not agree that they were involved in the disease, and the patients still could not get rid of its symptoms.
Despite the fact that the nature of mental illness remains unclear, the development of biological psychiatry has changed the idea of their occurrence. This prompted a reconsideration of the view on the role of the family in its occurrence and the launch of educational programs in psychiatry, teaching proper communication with the patient, convincing relatives that their attitude towards the patient, knowledge of the nature of the disease, long-term participation in treatment can contribute to recovery. In other words, the enormous contribution of the help of relatives to the treatment of a sick family member was recognized. The results of many studies prove that psychiatric education helps to reduce the frequency of relapses of the disease.
It also happens, of course, that relatives of patients perceive training as an attempt to shift the entire responsibility for treatment onto their shoulders. This is not true, since training makes it easier for people close to the patient to interact with him and with professionals.
The results of a survey of family members of the mentally ill who participated in the psychiatric education program show that almost everyone uses the knowledge gained in the classroom, especially regarding the symptoms of the disease, communication skills with a sick person, and techniques for reducing their own stress. Many relatives began to look more optimistically into the future, some noted that, thanks to the classes, their relations with medical personnel improved, emotional stress in the family decreased, and they feel less lonely.
Here are some testimonials from parents participating in the family mental health education program.
“I have been in a psychiatric education program for several months now and I realized that the feelings I was experiencing were a normal reaction to my daughter's illness: I was very worried that I myself might be sick. Now I have someone to talk to, they understand me, I don't feel as lonely as before. And most importantly, every time I come to class, I learn something important and new for myself. ”
”
(I.G., aged 62).
“The neighbors don't understand me and are afraid of my son. Now I sometimes tell them about psychiatry, about how people like my sick son are treated in England. They are surprised and even once, when my son fell ill again, they asked how to help me.”
(T.S., aged 52).
“I take advice. As it seemed to me before, nothing changes in my wife's illness. And now, looking back, as I was taught, I compare what was before and what is now, I see improvements - small, but they are.
(P.G., 48 years old).
Support groups and public organizations are an effective form of socio-psychological and informational support for families of mentally ill patients, helping themselves and their loved ones.
The number of such groups and public (non-governmental) organizations in developed countries is in the thousands.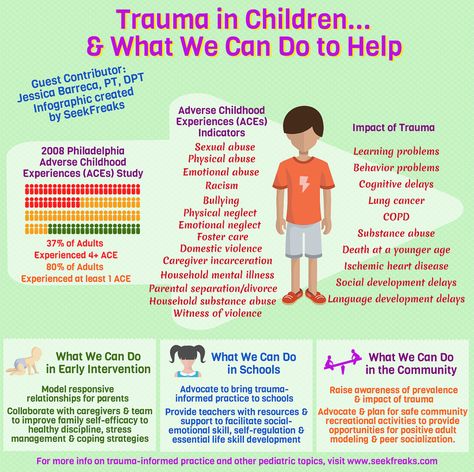 In Russia, the social movement in psychiatry is still gaining strength, but even now, as already mentioned, significant positive experience has been accumulated.
In Russia, the social movement in psychiatry is still gaining strength, but even now, as already mentioned, significant positive experience has been accumulated.
Over the past few years, the authors of the book have not only analyzed the activities of a number of public organizations and self-help groups operating in Moscow, but they themselves initiated the creation of such a public organization and we can confirm with full confidence their enormous role in the socio-psychological support of families with special needs. needs. Meetings of families united by one problem are invaluable in alleviating the burden of suffering associated with a severe mental illness of a loved one.
The work of support groups and public organizations created by the relatives of patients is aimed not only at their psychiatric education, but also at protecting the interests of the patients themselves and their families. Specialists can understand families and help them, but it is difficult for professionals to achieve such a healing effect, which gives mutual understanding of families, discussion of their problems in them.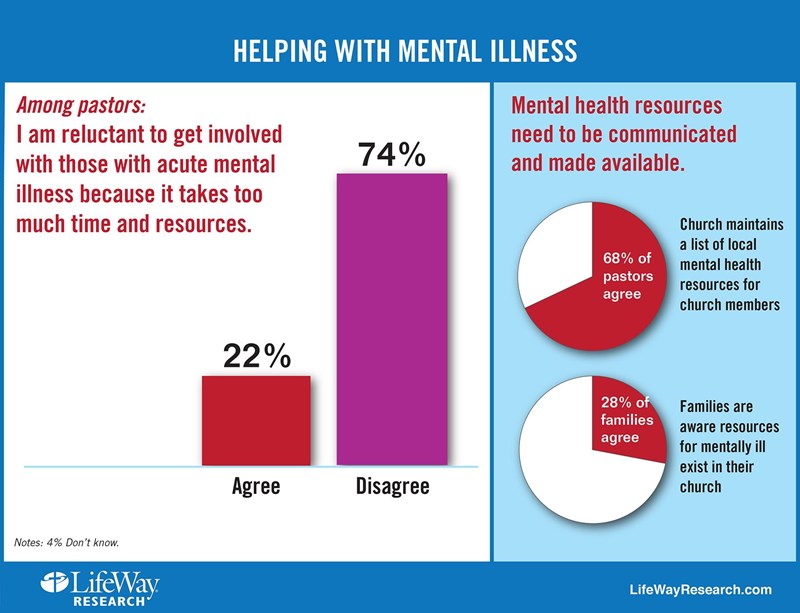 Evidence can be provided by the mother of a sick son attending a support group.
Evidence can be provided by the mother of a sick son attending a support group.
“It took me 20 years before I could talk to someone other than the local psychiatrist and openly say that my son has schizophrenia”
(E.P., 65 years old).
Concluding the introductory lecture, we consider it necessary to give the relatives of patients recommendations developed by leading experts in the field of psychiatric education of families.
Advice to family members
1. No need to rush. The recovery process can be lengthy. It is very important to get more rest. Everything will fall into place in time.
2. Remain calm. Being overly enthusiastic is a normal reaction. Try to moderate it. Disagreement is also normal. Try to take it easy as well.
3. Let each other rest: everyone needs a break. You are tired of something - this is normal. It's also okay to say "no" sometimes.
4. Set limits. Everyone must know the rules. A few simple rules can put everything in its place.
Set limits. Everyone must know the rules. A few simple rules can put everything in its place.
5. Don't think about what you can't change. Some things need to be left as they are. Pay attention to manifestations of cruelty.
6. Keep it simple. Say what you intended to say clearly, calmly, confidently.
7. Follow your doctor's instructions. It is necessary to take medicines as prescribed by the doctor, and only those that he prescribed.
8. Go about your business as usual. Restore the normal routine of housework. Keep in touch with your family and friends.
9. No drugs or alcoholic drinks: they aggravate the symptoms of the disease.
10. Pay attention to any changes in the well-being of a loved one, record them. Consult with your doctor.
11. Solve problems step by step. Make changes gradually. Work on one thing.
12. Temporarily lower expectations. Use your own characteristics and impressions about the state of your loved one. Compare the results of the current and previous months.
Compare the results of the current and previous months.
These simple recommendations are in fact patterns of behavior with the patient. It is important that they take into account the biological, psychological and social components of mental illness. They help in maintaining a calm atmosphere in the family, are aimed at reducing stress among its members and help prevent the recurrence of the disease. Reading the material below. You will also learn about other recommendations that will help you in communicating with the patient and in his treatment.
And a few more things to pay attention to.
The burden of illness, its painful impact on the patient and his family can be mitigated if:
• the disease is recognized as such;
• all interested persons received the necessary information about the disease and its treatment;
• drug therapy is carried out sequentially;
• medical supervision is carried out regularly;
• The family managed to avoid isolation.