Healing complex trauma
What Is Complex Trauma? Symptoms, Examples, and How to Heal
Complex trauma has a deep impact on the nervous system. By understanding how it develops, you can better understand how to treat it.
Most of us have a chapter in our lives we’d rather forget. Whether it’s a devastating breakup or the death of a loved one, many of us have felt the sting of heartbreak that comes with being a human.
But for those who live with complex trauma, the memories don’t just live in the past. They live in the present moment, too.
For a long time, complex trauma wasn’t well understood. Now researchers estimate that more than 3% of people meet the criteria for complex trauma, also called complex post-traumatic stress disorder (C-PTSD), in the United States. This is about the same percentage as people with traditional PTSD.
Trauma, the kind you’ve likely heard of, can develop after a distinct traumatic experience. It occurs when the brain and body are so overwhelmed that they have a hard time easing out of “fight, flight, or freeze” mode and coming back into a relaxed state.
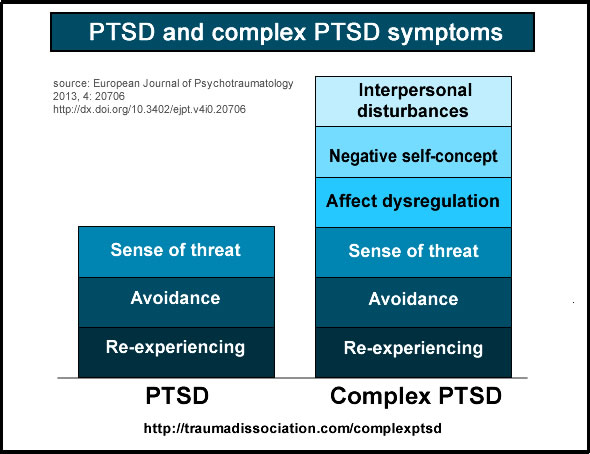
Trauma may refer to a single incident, while complex trauma refers to a series of traumatic events that take place over a long period of time, like months or years.
First introduced in the 1990s by Judith Lewis Herman, PhD, complex trauma has a lot in common with the classic symptoms of PTSD, such as:
- feeling anxious
- having flashbacks
- avoiding circumstances that remind you of the traumatic events
In addition, complex trauma can:
- distort your sense of self
- make it difficult to control your emotions
- cause relationships challenges
When you experience a traumatic event, it activates the limbic system in the brain. This “fire alarm” shuts down all nonessential systems (rest, digestion, sleep) and floods your body with stress hormones, like cortisol, so you can prepare for fight, flight, or freeze.
Once the danger passes, your parasympathetic nervous system provides inner calm, otherwise known as your “rest and digest” mode.
At this point, normal cognitive function returns, and you can go back to your day with relatively few side effects, perhaps only feeling a little jittery for a while, or a bit on edge.
But for people who live with complex trauma, this balance doesn’t quite return all the way.
The limbic system stays engaged most of the time. It’s a coping mechanism to try and stay safe in the face of ongoing adversity. It’s an experience of constantly being in survival mode, or on edge.
Over time, it becomes a “new normal” for the brain and body.
In his book, “The Body Keeps the Score,” trauma expert Bessel van der Kolk, MD, describes how trauma literally becomes trapped in the body and the brain rewires itself. These lasting effects create symptoms of complex trauma.
This bodily state of your nervous system being on “high alert” can affect your thoughts, actions, and relationships.
Some symptoms of complex trauma include:
- flashbacks
- lapses in memory
- difficulty regulating emotions
- hyperarousal, or being “on alert”
- dissociation or lapses in memory
- depersonalization or derealization
- sleep disturbances or nightmares
- struggling in interpersonal relationships
- low self-esteem or negative self-perception
- avoiding people, places, or scenarios that upset you
Somatic (bodily) symptoms, like unexplained headaches or an upset stomach, are also common with complex trauma. Since the body is under chronic stress, it can lower your immune system and lead to a range of chronic health conditions.
Since the body is under chronic stress, it can lower your immune system and lead to a range of chronic health conditions.
Complex trauma can arise in any situation where you feel an ongoing sense of fear, horror, helplessness, or powerlessness over an extended period of time, with the perceived or actual inability to escape.
It usually stems from trauma you experienced in childhood, though it can develop from trauma in adulthood as well.
Some possible causes of complex trauma include:
- sexual abuse or incest
- ongoing physical or emotional abuse
- chronic neglect or abandonment
- medical abuse or medical trauma
- torture or being held captive
- enmeshment or engulfment trauma
- parentification (children taking on adult rules)
- human trafficking
- genocide campaigns
- living in a war zone or area of civil unrest
Everyone’s story is unique — and so is their trauma. What works for one person may not work for another.
Also, keep in mind that what works at one point in time may not work later on down the line.
The great news is, as more is uncovered about complex trauma, more trauma treatment therapies are emerging as well. The goal of each treatment option is to provide a corrective emotional experience for healing.
Here are some effective therapies for complex trauma:
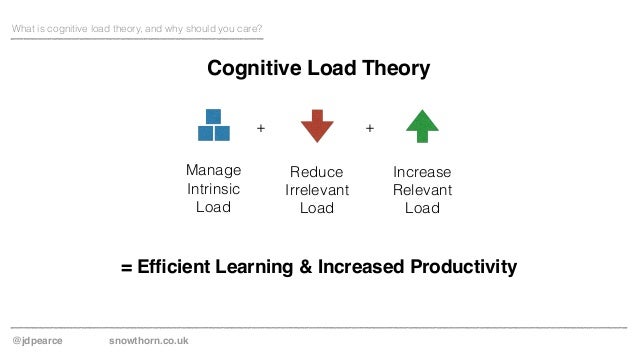
- Cognitive behavioral therapy (CBT). In this form of therapy, you explore the relationship between your thoughts, feelings, and behaviors. Once you become aware of the connections, you may be able to change your actions.
- Eye Movement Desensitization and Reprocessing (EMDR). With this treatment, you’re guided with gentle tapping (or tones) to reprocess traumatic events and form new beliefs around them.
- Internal family systems (IFS).
With this approach, you learn how to integrate the different parts of your personality into one whole “Self” to reprocess traumatic events in a way that can no longer harm you.
- Somatic (body) therapies. Since trauma lives in the limbic area of the brain and not the frontal cortex (the part of the brain that talks in therapy), somatic therapies or body-centered therapies can teach your body that it does not have to be prepared for trauma all the time.
- Dialectical behavioral therapy (DBT). This approach can be effective for people who live with borderline personality disorder (BPD), which has many overlapping symptoms with complex trauma. In this treatment approach, you learn mindfulness, radical self-acceptance, and distress tolerance.
There’s also a link between complex trauma and substance use as a way to cope with symptoms. If you’d like to cut back on using drugs or drinking alcohol, support is available.
Look for a local 12-step program, like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA), or SMART Recovery.
Here are some additional resources for support:
- Substance Abuse and Mental Health Services Administration (SAMHSA)
- National Council on Alcoholism and Drug Dependence
- National Institute on Alcohol Abuse and Alcoholism
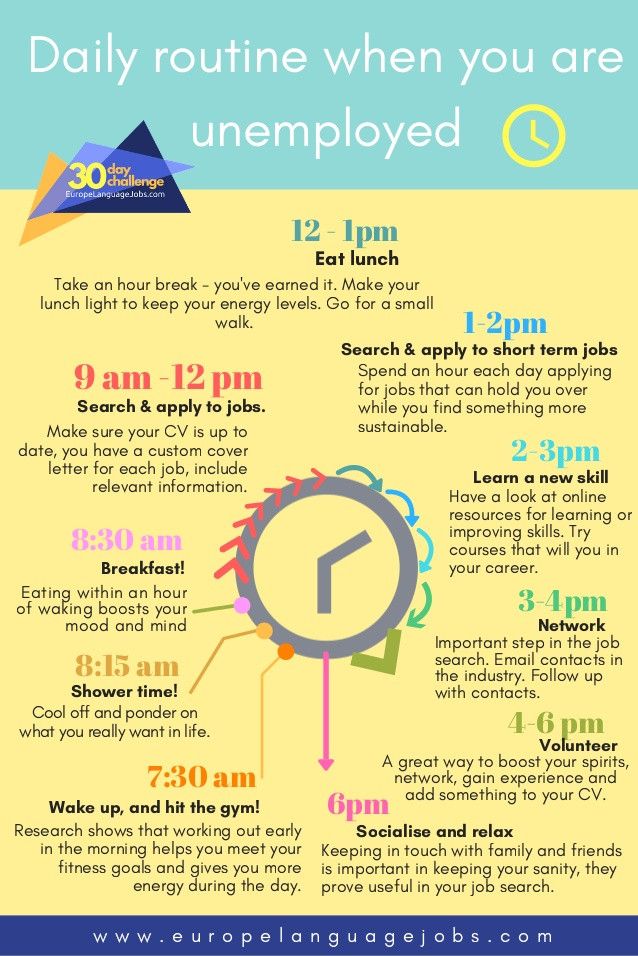
Recovery from complex trauma can be a gradual process.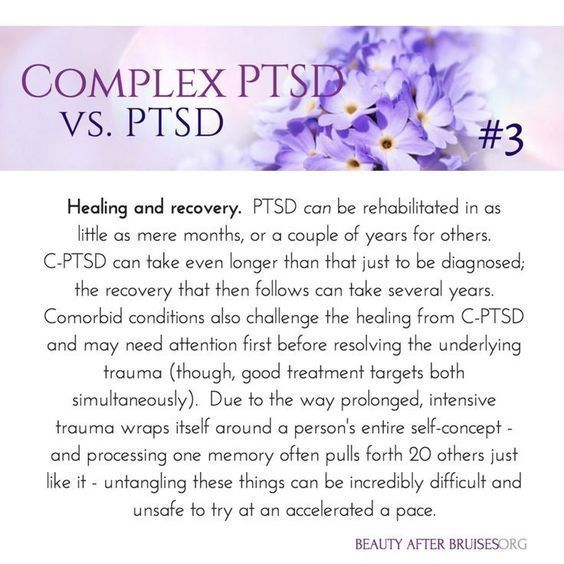 But having a range of tools and self-care strategies can make the process a whole lot easier.
But having a range of tools and self-care strategies can make the process a whole lot easier.
It’s a good idea to keep a few deep breathing exercises up your sleeve for those tough moments. This is a direct way to let your body know that you’re safe. Try these:
- 4-7-8 breathing: Inhale for 4 seconds, hold for 7 seconds, exhale for 8 seconds.
- Box breathing: Inhale for 4 seconds, hold for 4 seconds, exhale for 4 seconds, hold for 4 seconds.
- Alternate nostril breathing: Place your right thumb over your right nostril. Inhale and exhale eight times through your left nostril. Repeat on the other side.
A consistent mindfulness practice can help too. A 2018 study involving veterans with PTSD found that a regular meditation practice can reduce symptoms of trauma. Yoga has shown similar results, showing that both can be an effective complement to talk therapy.
It might help to access trauma-informed yoga sessions, where the yoga instructor is aware that trauma can be stored in the body, and that some body movements can trigger emotional reactions. They can help you navigate these reactions in a healing way.
They can help you navigate these reactions in a healing way.
Here are some lifestyle adjustments that can make complex trauma more manageable:
- do tai chi or dance
- journal your feelings
- spend time in nature
- eat a nutritious, balanced diet
- sleep around 8 hours a night
- “shake off” tough emotions by literally shaking your arms or your body to release tension
- talk through your triggers with loved ones
- practice progressive relaxation techniques
- exercise five times a week, even if only a few minutes a day
- try using the flashback halting protocol to manage flashbacks
Complex trauma may feel like it’s taking over your life. Perhaps you feel alone in your experience, wondering if it will ever feel like less of a big deal.
Two thoughts: You’re not alone, and it will get better.
One of the best things you can do is to continue to educate yourself about complex trauma. You may be able to find a healing book club or support group in your area.
You can also join one online, like this one through the C-PTSD Foundation.
Here are some books to add to your reading list:
- “The Body Keeps the Score” by Bessel van der Kolk, MD
- “Healing the Fragmented Selves of Trauma Survivors: Overcoming Internal Self-Alienation” by Janina Fisher, PhD
- “Trauma & Recovery” by Judith Lewis Herman, MD
- “The Complex PTSD Workbook” by Arielle Schwartz, PhD
- “Waking the Tiger” by Peter Levine, PhD
- “Trauma and the Body” by Pat Ogden, PhD
- “The Body Heals Itself” by Emily Francis
- “What Happened to You? Conversations on Trauma, Resilience, and Healing” by Bruce D. Perry, MD, PhD, and Oprah Winfrey
Also, here’s a great TED Talk on how childhood trauma affects health over a lifetime.
Finally, know that you will get through this. You’ve survived 100% of your worst days so far and, just like the other tough times, this will pass too.
You’re stronger than you know.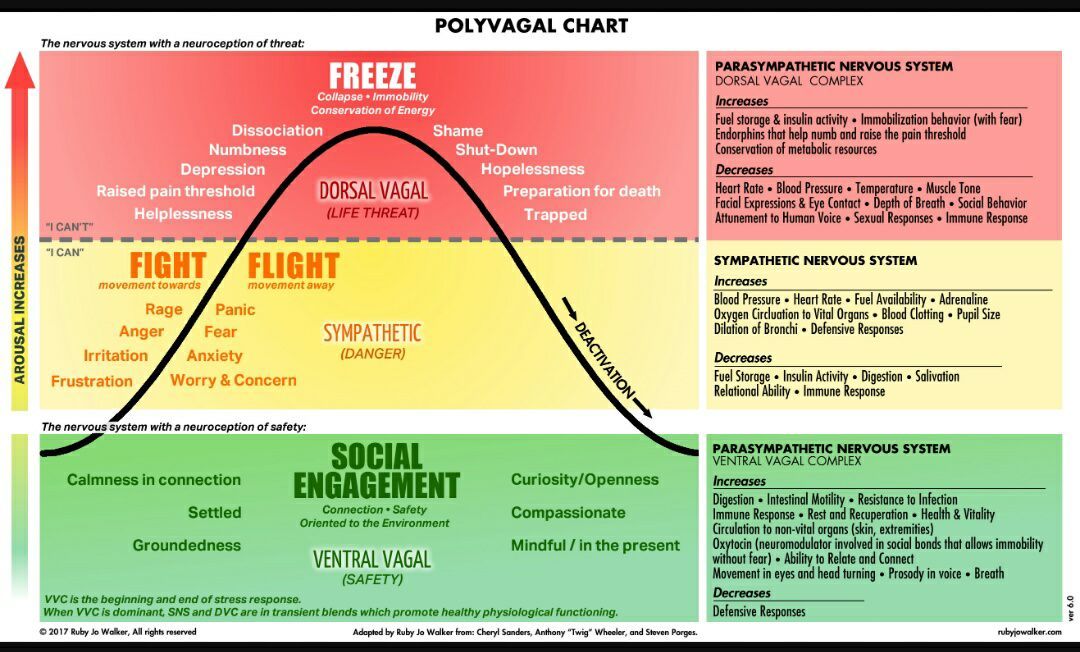
Suicide prevention
Complex trauma may increase your risk of self-harm. If you’re considering self-harm or suicide, help is available right now:
- Call a crisis hotline, such as the National Suicide Prevention Lifeline at 800-273-8255.
- Text HOME to the Crisis Text Line at 741741.
What Is Complex Trauma? Symptoms, Examples, and How to Heal
Complex trauma has a deep impact on the nervous system. By understanding how it develops, you can better understand how to treat it.
Most of us have a chapter in our lives we’d rather forget. Whether it’s a devastating breakup or the death of a loved one, many of us have felt the sting of heartbreak that comes with being a human.
But for those who live with complex trauma, the memories don’t just live in the past. They live in the present moment, too.
For a long time, complex trauma wasn’t well understood. Now researchers estimate that more than 3% of people meet the criteria for complex trauma, also called complex post-traumatic stress disorder (C-PTSD), in the United States. This is about the same percentage as people with traditional PTSD.
This is about the same percentage as people with traditional PTSD.
Trauma, the kind you’ve likely heard of, can develop after a distinct traumatic experience. It occurs when the brain and body are so overwhelmed that they have a hard time easing out of “fight, flight, or freeze” mode and coming back into a relaxed state.
Trauma may refer to a single incident, while complex trauma refers to a series of traumatic events that take place over a long period of time, like months or years.
First introduced in the 1990s by Judith Lewis Herman, PhD, complex trauma has a lot in common with the classic symptoms of PTSD, such as:
- feeling anxious
- having flashbacks
- avoiding circumstances that remind you of the traumatic events
In addition, complex trauma can:
- distort your sense of self
- make it difficult to control your emotions
- cause relationships challenges
When you experience a traumatic event, it activates the limbic system in the brain. This “fire alarm” shuts down all nonessential systems (rest, digestion, sleep) and floods your body with stress hormones, like cortisol, so you can prepare for fight, flight, or freeze.
This “fire alarm” shuts down all nonessential systems (rest, digestion, sleep) and floods your body with stress hormones, like cortisol, so you can prepare for fight, flight, or freeze.
Once the danger passes, your parasympathetic nervous system provides inner calm, otherwise known as your “rest and digest” mode.
At this point, normal cognitive function returns, and you can go back to your day with relatively few side effects, perhaps only feeling a little jittery for a while, or a bit on edge.
But for people who live with complex trauma, this balance doesn’t quite return all the way.
The limbic system stays engaged most of the time. It’s a coping mechanism to try and stay safe in the face of ongoing adversity. It’s an experience of constantly being in survival mode, or on edge.
Over time, it becomes a “new normal” for the brain and body.
In his book, “The Body Keeps the Score,” trauma expert Bessel van der Kolk, MD, describes how trauma literally becomes trapped in the body and the brain rewires itself. These lasting effects create symptoms of complex trauma.
These lasting effects create symptoms of complex trauma.
This bodily state of your nervous system being on “high alert” can affect your thoughts, actions, and relationships.
Some symptoms of complex trauma include:
- flashbacks
- lapses in memory
- difficulty regulating emotions
- hyperarousal, or being “on alert”
- dissociation or lapses in memory
- depersonalization or derealization
- sleep disturbances or nightmares
- struggling in interpersonal relationships
- low self-esteem or negative self-perception
- avoiding people, places, or scenarios that upset you
Somatic (bodily) symptoms, like unexplained headaches or an upset stomach, are also common with complex trauma. Since the body is under chronic stress, it can lower your immune system and lead to a range of chronic health conditions.
Complex trauma can arise in any situation where you feel an ongoing sense of fear, horror, helplessness, or powerlessness over an extended period of time, with the perceived or actual inability to escape.
It usually stems from trauma you experienced in childhood, though it can develop from trauma in adulthood as well.
Some possible causes of complex trauma include:
- sexual abuse or incest
- ongoing physical or emotional abuse
- chronic neglect or abandonment
- medical abuse or medical trauma
- torture or being held captive
- enmeshment or engulfment trauma
- parentification (children taking on adult rules)
- human trafficking
- genocide campaigns
- living in a war zone or area of civil unrest
Everyone’s story is unique — and so is their trauma. What works for one person may not work for another.
Also, keep in mind that what works at one point in time may not work later on down the line.
The great news is, as more is uncovered about complex trauma, more trauma treatment therapies are emerging as well. The goal of each treatment option is to provide a corrective emotional experience for healing.
Here are some effective therapies for complex trauma:
- Cognitive behavioral therapy (CBT). In this form of therapy, you explore the relationship between your thoughts, feelings, and behaviors. Once you become aware of the connections, you may be able to change your actions.
- Eye Movement Desensitization and Reprocessing (EMDR). With this treatment, you’re guided with gentle tapping (or tones) to reprocess traumatic events and form new beliefs around them.
- Internal family systems (IFS). With this approach, you learn how to integrate the different parts of your personality into one whole “Self” to reprocess traumatic events in a way that can no longer harm you.
- Somatic (body) therapies. Since trauma lives in the limbic area of the brain and not the frontal cortex (the part of the brain that talks in therapy), somatic therapies or body-centered therapies can teach your body that it does not have to be prepared for trauma all the time.
- Dialectical behavioral therapy (DBT). This approach can be effective for people who live with borderline personality disorder (BPD), which has many overlapping symptoms with complex trauma. In this treatment approach, you learn mindfulness, radical self-acceptance, and distress tolerance.
There’s also a link between complex trauma and substance use as a way to cope with symptoms. If you’d like to cut back on using drugs or drinking alcohol, support is available.
Look for a local 12-step program, like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA), or SMART Recovery.
Here are some additional resources for support:
- Substance Abuse and Mental Health Services Administration (SAMHSA)
- National Council on Alcoholism and Drug Dependence
- National Institute on Alcohol Abuse and Alcoholism
Recovery from complex trauma can be a gradual process. But having a range of tools and self-care strategies can make the process a whole lot easier.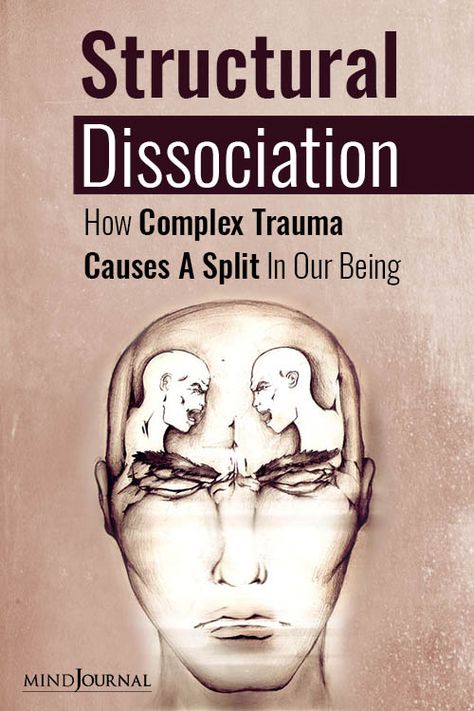
It’s a good idea to keep a few deep breathing exercises up your sleeve for those tough moments. This is a direct way to let your body know that you’re safe. Try these:
- 4-7-8 breathing: Inhale for 4 seconds, hold for 7 seconds, exhale for 8 seconds.
- Box breathing: Inhale for 4 seconds, hold for 4 seconds, exhale for 4 seconds, hold for 4 seconds.
- Alternate nostril breathing: Place your right thumb over your right nostril. Inhale and exhale eight times through your left nostril. Repeat on the other side.
A consistent mindfulness practice can help too. A 2018 study involving veterans with PTSD found that a regular meditation practice can reduce symptoms of trauma. Yoga has shown similar results, showing that both can be an effective complement to talk therapy.
It might help to access trauma-informed yoga sessions, where the yoga instructor is aware that trauma can be stored in the body, and that some body movements can trigger emotional reactions. They can help you navigate these reactions in a healing way.
Here are some lifestyle adjustments that can make complex trauma more manageable:
- do tai chi or dance
- journal your feelings
- spend time in nature
- eat a nutritious, balanced diet
- sleep around 8 hours a night
- “shake off” tough emotions by literally shaking your arms or your body to release tension
- talk through your triggers with loved ones
- practice progressive relaxation techniques
- exercise five times a week, even if only a few minutes a day
- try using the flashback halting protocol to manage flashbacks
Complex trauma may feel like it’s taking over your life. Perhaps you feel alone in your experience, wondering if it will ever feel like less of a big deal.
Two thoughts: You’re not alone, and it will get better.
One of the best things you can do is to continue to educate yourself about complex trauma. You may be able to find a healing book club or support group in your area.
You can also join one online, like this one through the C-PTSD Foundation.
Here are some books to add to your reading list:
- “The Body Keeps the Score” by Bessel van der Kolk, MD
- “Healing the Fragmented Selves of Trauma Survivors: Overcoming Internal Self-Alienation” by Janina Fisher, PhD
- “Trauma & Recovery” by Judith Lewis Herman, MD
- “The Complex PTSD Workbook” by Arielle Schwartz, PhD
- “Waking the Tiger” by Peter Levine, PhD
- “Trauma and the Body” by Pat Ogden, PhD
- “The Body Heals Itself” by Emily Francis
- “What Happened to You? Conversations on Trauma, Resilience, and Healing” by Bruce D. Perry, MD, PhD, and Oprah Winfrey
Also, here’s a great TED Talk on how childhood trauma affects health over a lifetime.
Finally, know that you will get through this. You’ve survived 100% of your worst days so far and, just like the other tough times, this will pass too.
You’re stronger than you know.
Suicide prevention
Complex trauma may increase your risk of self-harm. If you’re considering self-harm or suicide, help is available right now:
- Call a crisis hotline, such as the National Suicide Prevention Lifeline at 800-273-8255.
- Text HOME to the Crisis Text Line at 741741.
Rehabilitation after complex injuries and operations. Center "ZARTA" Kyiv
Vadim Konovalenko
I want to say thank you to the Zart Center and personally to each employee for their invaluable help in my treatment! I had a knee injury, an unsuccessful operation (to put it mildly), more than a year of agony with my knee! I turned to Vladimir Anat...
01/29/2020
Taras Sobkiv
Experts of the appropriate level, fans of their work, team approach, constant growth. Respect!
03.11.2019
Htc Bolt
High professionalism of employees.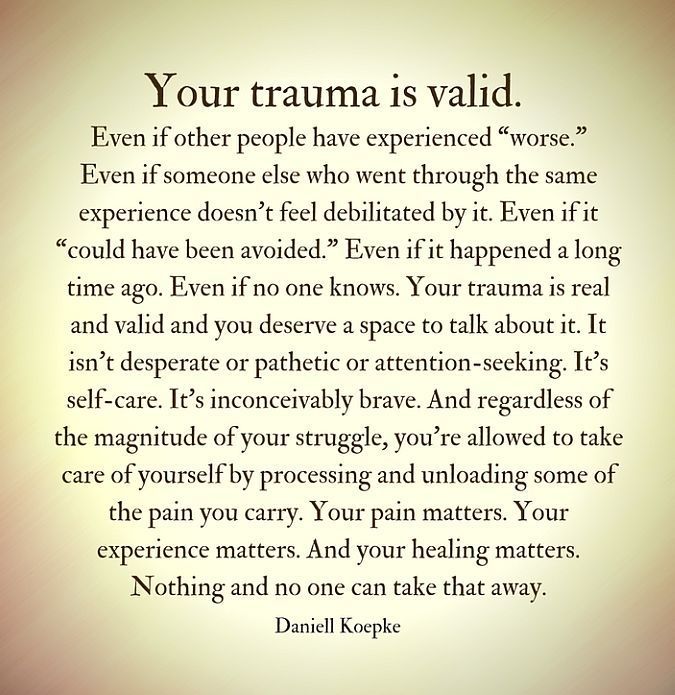 The use of evidence-based medicine methods.
The use of evidence-based medicine methods.
24.10.2019
Lyubov Titenko
Super team. Painless!
08/30/2019
Olga Dobryanskaya
Helped the whole family! Thanks to Ivan Andreevich and his team, people get not only hope, but also results in a really short time at any age! A very pleasant and decent doctor who can really be trusted...
06/13/2019
Max Gladyshko
Yuzva Dmitry is the best thing that can happen to you in this area.
05/14/2019
Artur Filatov
If Zasadnyuk Ivan works here, then you should go to him, a very good orthopedic surgeon 🔥🔥🔥, operated on my knee.
04.05.2019
Dudar V. I.
I want to share with everyone my impressions of the treatment of a damaged medial meniscus, a defect in the articular cartilage - I could not walk.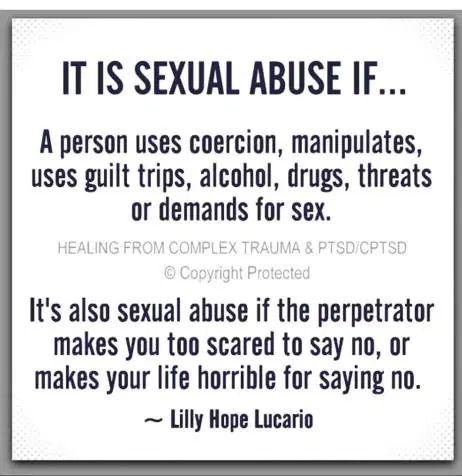 I was looking for recommendations, consultations, reviews. The hospital said I needed a prosthesis. Only in c...
I was looking for recommendations, consultations, reviews. The hospital said I needed a prosthesis. Only in c...
03/28/2019
Olena Stefanska
Highly professional team of rehabilitation specialists, modern equipment, attentive attitude to each patient, individual programs and approach. With Ivan Ses and Andrei Sorokin, kinesiotherapy restored movement ...
03/22/2019
Alina Pilipenko
Great atmosphere, pleasant, polite staff, everything is clean and stylish, always greeted with a smile. Many thanks to Ivan Andreevich, after the procedures I can finally walk without pain! And of course, thanks to Maxim, competently...
26.02.2019
Lena G.
Exemplary Clinic with a good aura. You come there when you feel bad, and you are surrounded by delicate attention and care, and it becomes warmer in your soul and you understand that you are in good hands. Doctor Zasadnyuk I.A. professional, he d...
Doctor Zasadnyuk I.A. professional, he d...
21.02.2019
Tanya Podebejko
I want to express HUGE thanks to the specialists of the ZARTA center. It is very comfortable to work with a team of professionals. Individual approach and customer care, in my opinion, is the motto of the center. Special thanks to Ivan Andreevich....
21.02.2019
Evgeny Sharokhin
After an intense run, he could not walk at all - he overloaded his knee and severely damaged the cartilage. Passed a series of PRP procedures and magnetic laser procedures. He also went through rehabilitation. Worked with rehabilitation specialist Ivan. Very do...
21.02.2019
Elena Desyatnik
Good afternoon! I want to thank Ivan Ses - a wonderful master of his craft! He sees the problem, solves it comprehensively and feels the human body with his hands, like a sorcerer! My toes were numb, my colleagues advised me to “drink vitamin. ..
..
12/18/2018
Larion Babych
Exceptional qualifications of specialists at all stages of treatment and modern equipment will make the recovery process quick and enjoyable.
12/10/2018
Vlad Kozak
I want to say a very big thank you to Ivan Andreevich for professional treatment and attitude!!! The staff is very friendly and sincere, they are always ready to help and give useful advice. I especially want to thank Nat...
05.12.2018
Vladyslav Lebedynets
I want to express my gratitude to everyone in Zart for their care and help, and especially to Ses Ivan for rehabilitation. Even such a lazy person as I tried to get fired up with the desire to play sports. During training, Ivan constantly watched ...
11/25/2018
Anatoly Sovailo
My wife came to the ZARTA clinic with severe pain in the shoulder joint, which caused suffering. After 3 weeks, the wife was unrecognizable. She just returned to a full life. Irina talked about modern methods of l...
After 3 weeks, the wife was unrecognizable. She just returned to a full life. Irina talked about modern methods of l...
05.11.2018
Alena Egorova
Modern clinic with modern equipment and methods. Thanks to Ivan Andreevich for consultations, to the medical staff and rehabilitation specialist Evgenia for the quick recovery and professional work, and in general, everything is ...
03/29/2018
Anastasia Tolochnaya
She underwent rehabilitation in Zart after cruciate ligament plasty. Started 3 months after surgery. For those who doubt whether or not to go to a rehabilitologist… go without fail!!! Set the gait correctly...
03/05/2018
Inna Gavrilova
Super professionals! The best orthopedic center in Kyiv, from my extensive experience this confidence. No need for Israel and Europe.
03/05/2018
Julia Samorodova
Thanks to Ivan Andreevich for the perfect foot surgery. After only 6 weeks, I was already able to fly to the North. Cyprus with a group of children, to successfully implement our active-educational project there. Children of Cyprus and Ukraine thanks...
After only 6 weeks, I was already able to fly to the North. Cyprus with a group of children, to successfully implement our active-educational project there. Children of Cyprus and Ukraine thanks...
28.02.2018
Viktor Rezvyi
I highly recommend a consultation on any issues of this profile with Ivan Andreevich, as well as a trial workout with a rehabilitologist Dmitry! I promise you will want to come back because it restores all parts of the body back to normal!
09.02.2018
Alina Pilipenko
There is a great team and good atmosphere. Always greeted with a smile) Special thanks to Ivan Andreevich, the doctor knows his stuff. I miraculously came to you! 100% recommend to anyone with problems. Thank you for your help!
09.02.2018
Tatiana Goliaka
Thank you very much and low bow to Ivan Andreevich and Alexander Ivanovich for high-quality operations and quick recovery. Good luck and prosperity!
Good luck and prosperity!
12/22/2017
Larisa Ivashko
Very good clinic, doctors are masters of their craft, nurses are responsive, attentive and responsible. I wish you good health and patience
12/22/2017
Svetlana Yurievna
I turned to Antonyuk Alexander Ivanovich on the recommendations of many of my friends, as a wonderful surgeon, traumatologist, orthopedist, a practitioner with extensive experience, with my painful problem, I had to be operated on, ...
12.12.2017
Sergey Tyutyunenko
During the treatment, I had to go through many specialists and clinics, for almost a year the fracture did not heal. Ivan Andreevich and Svetlana performed a miracle! For 1.5 months I was able to step on my foot. And for 3 more to get off the crutches. The only o...
07. 12.2017
12.2017
Knysh Sergey
Was a patient of this medical center. Only pleasant impressions, without exception: modern equipment and conscientiousness in work, qualified recommendations, everything is on time from diagnosis to treatment. Team p...
08/26/2017
Yuri Zheleznyak
Cool clinic, professionals work, I wish you success, keep it up!!!
08.08.2017
Zoryana Knysh
I recommend ZARTA to everyone! Here I received highly qualified assistance using modern technologies, complete comfort and friendly attitude of the staff! Many thanks to the doctor Ivan Andreevich Zasadnyuk, who is not only...
08.08.2017
Galina Novosad
I want to express my gratitude to the doctor Ivan Andreevich for his help and professionalism. As they say "doctor from God". I recommend to everyone. Special thanks to the staff of the clinic for their hospitality and kindness.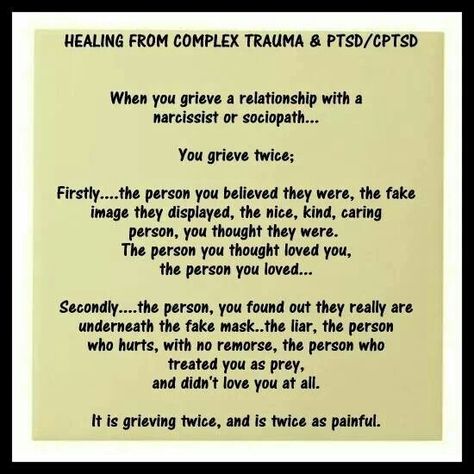
07/27/2017
Lyubov Gerasimova
A very good doctor Ivan Andreevich and a wonderful team of nurses.
25.07.2017
Tatyana Novosad
I used the services of the clinic and my family members. The clinic provides a wide range of services from initial consultation to various types of rehabilitation procedures. The staff is always friendly and open, ready to...
07/18/2017
Oksana Savchuk
Services at a high level. I regularly go to presotherapy. The staff is welcoming and friendly. I recommend!
06/26/2017
Oksana Zayats
I want to thank doctor Ivan Andreevich and his team at the ZARTA orthopedic center. Always friendly, courteous and most importantly professional. I wish Ivan Andreevich and the whole team the most important...
19. 02.2016
02.2016
Lena Nesterovych
Thank you, Ivan Andreevich, for your help! Perfect cleanliness, a clear work schedule, high professionalism of the staff - this is how you can characterize the work of the medical center. And since such conditions are created for patients,...
10.10.2015
Rupture (damage) of the rotator cuff of the shoulder joint
Large loads on the shoulder can cause various injuries and degenerative changes. With repeated loads on the shoulder joint, its stability is lost, and performance problems arise. A more serious problem is a partial or complete tear of the rotator cuff. Such an injury requires urgent medical intervention and, often, surgical treatment.
The shoulder joint is one of the most mobile joints in the human body. The structure of this joint makes it possible to carry out various movements of the upper limbs in a wide range: rotational, flexion, abduction, extension and adduction actions.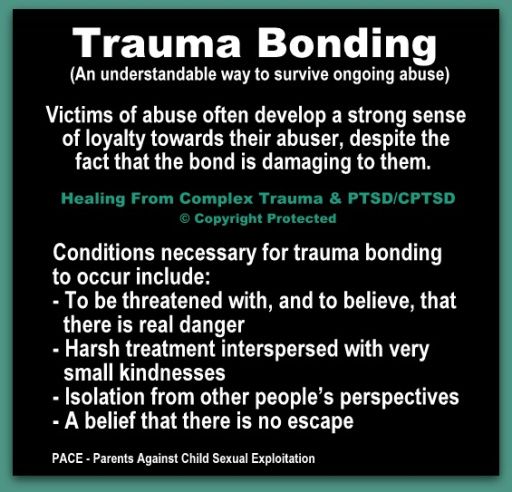
Disease description
Rotator Cuff - Anterior outer portion of the shoulder joint capsule. It combines the tendons of the supraspinatus, infraspinatus, small round muscles. Despite the difference in their functions, such an anatomically close place of muscle fixation allowed traumatologists to identify them in a common group (rotator cuff of the shoulder).
Damage to the rotator cuff can be considered a rupture of one or a group of tendons included in its composition. Most often it is caused by trauma, dislocation or a previous chronic inflammatory process.
What causes a rotator cuff injury?
As mentioned above, the most common cause of rotator cuff injury is trauma. Most often, ruptures occur in the elderly, but in young people, a rupture can also occur due to serious injuries, such as a fracture of part of the humerus or dislocations.
-
A fairly common cause of rotator cuff injury is permanent tendon injury chronic.
 Basically, this applies to people whose professional activities are associated with heavy physical labor. Tension and heavy stress on the joints, accompanied by repeated movement operations, leads to chronic inflammation and pain.
Basically, this applies to people whose professional activities are associated with heavy physical labor. Tension and heavy stress on the joints, accompanied by repeated movement operations, leads to chronic inflammation and pain. -
Spontaneous rupture or injury of the tendons, as a rule, is preceded by a period of degenerative-dystrophic changes . Lack of blood supply is the main cause of tissue degeneration or tendopathy. Another possible reason for the development of degeneration, many doctors also include a genetic predisposition.
-
Another reason may be individual anatomy . Sometimes insufficient space between the head of the humerus and the tip of the scapula leads to constant friction and injury to the tendons of the rotator cuff. In addition, the hook-shaped form of the acromial process and the presence of an additional bone at the tip of the scapula, damaging the tendons, are anatomically determined.
Rotator cuff tear symptoms
A rupture is always accompanied by a sharp attack of pain localized in and around the shoulder joint. The pain often radiates to the hand, neck and forearms. A characteristic symptom is an increase in pain when you try to make a certain movement with your hand, for example, raise it or take it to the side. In some cases, patients are completely deprived of the ability to move their hand. The individuality of symptoms and the degree of their severity depends on whether the rotator cuff rupture was complete or partial. Patients also very often complain of the inability to sleep on the side where the joint is damaged.
The pain often radiates to the hand, neck and forearms. A characteristic symptom is an increase in pain when you try to make a certain movement with your hand, for example, raise it or take it to the side. In some cases, patients are completely deprived of the ability to move their hand. The individuality of symptoms and the degree of their severity depends on whether the rotator cuff rupture was complete or partial. Patients also very often complain of the inability to sleep on the side where the joint is damaged.
The place where the center of pain is localized directly depends on the location of the damaged tendon. The most common in clinical practice is supraspinatus tendon rupture. You can diagnose such a case by asking the patient to take his hand to his side. If we are dealing with just such damage, the patient will not be able to perform this task. If, however, abduction of the arm is possible, but pronounced pain is felt, it is most likely that the tendon is not completely torn, but only severely damaged.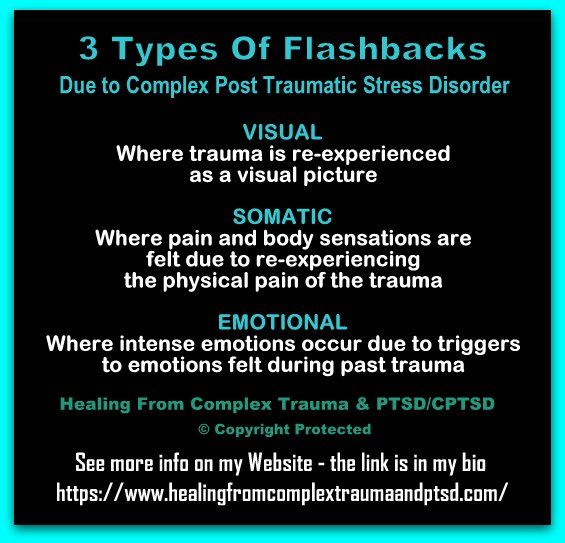
Diagnosis of rotator cuff injuries of the key joint
In order to make a correct diagnosis, the doctor conducts a set of measures to establish the clinical picture.
-
The first method is questioning the patient : the doctor needs to establish the circumstances under which the pain appeared, to establish how long the patient experienced discomfort in this area and ask about the nature of the professional activity.
-
Then a thorough examination is required using specific tests . Thus, the level, severity of the pain syndrome, the degree of weakness of the motor function and the condition of the adjacent muscles are determined. Usually, a complete rupture has a number of pronounced symptoms, so it can be diagnosed without difficulty.
Below are a few diagnostic tests to help your doctor understand the nature of your shoulder injury.
Dawburn's painful arch
The arm is passively and actively retracted from the initial position along the body.
Score . Pain in abduction between 70° and 120° is symptomatic of a supraspinatus tendon injury that is being compressed between the greater tubercle of the humerus and the acromial process during this phase of movement (“subacromial impingement”).
Zero Position Abduction Test
The patient is standing with arms down and relaxed. The doctor covers the distal third of each forearm of the patient with his hands. The patient tries to spread his arms, while the doctor resists.
Estimated. Abduction of the arm is performed by the supraspinatus and deltoid muscles. Pain and especially weakness during abduction and deviation of the arm strongly support a rotator cuff tear.
The eccentric location of the head of the shoulder in the form of its upper displacement during a rupture of the rotator cuff occurs due to an imbalance in the muscles surrounding the shoulder joint. Partial ruptures, which can be functionally compensated, disrupt function to a lesser extent with the same severity of pain. Complete tears are invariably characterized by weakness and loss of function.
Complete tears are invariably characterized by weakness and loss of function.
Jobe supraspinatus test
This test can be performed with the patient standing or sitting. With the forearm extended, the patient's arm is placed in 90° abduction, 30° horizontal flexion, and internal rotation. The doctor resists this movement by applying pressure to the proximal shoulder.
Estimated. If this test causes significant pain and the patient is unable to hold the arm abducted to 90° against gravity on its own, this is referred to as a positive falling arm symptom. The upper portions of the rotator cuff (supraspinatus) are evaluated mainly in the position of internal rotation (the first finger points down), and the condition of the anterior portion of the cuff is in the position of external rotation.
Falling hand test (symptom of falling flag, chess clock)
The patient is seated, the physician passively abducts the patient's extended arm approximately 120°.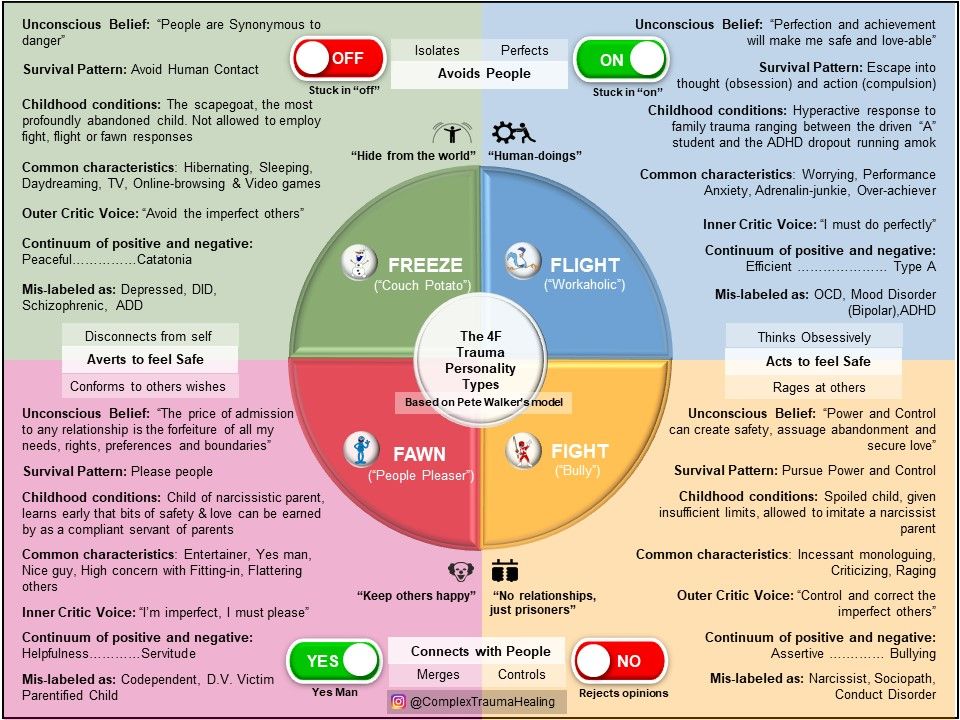 The patient is asked to independently hold the arm in this position, and then gradually lower it.
The patient is asked to independently hold the arm in this position, and then gradually lower it.
Estimated. Failure to hold the arm in this position with or without pain, or a sudden fall of the arm, confirms rotator cuff injury. The most common cause is a defect in the supraspinatus muscle. With pseudoparalysis, the patient cannot independently raise the injured arm. This is the main symptom confirming the pathology of the rotator cuff.
External rotation abduction test for infraspinatus tendon rupture
The patient's arm is placed in 90° abduction and 30° flexion. In this position, the action of the deltoid muscle as an external rotator is excluded. The patient is then asked to begin external rotation, which is prevented by the physician.
Estimated. Decreased active external rotation in abducted arm position is consistent with clinically significant infraspinatus tendon injury.
Further, without fail, the patient receives a referral for an x-ray. With the help of an X-ray examination, the doctor receives a picture typical of a particular case. Unfortunately, it is the gap that is not clearly defined; only a number of indirect signs can indicate it. The most informative diagnostic method today is magnetic resonance imaging. It can be used to visualize the tendons, muscles and ligaments of the shoulder joint. This method provides the most clear and vivid picture of the condition of the patient's soft tissues.
With the help of an X-ray examination, the doctor receives a picture typical of a particular case. Unfortunately, it is the gap that is not clearly defined; only a number of indirect signs can indicate it. The most informative diagnostic method today is magnetic resonance imaging. It can be used to visualize the tendons, muscles and ligaments of the shoulder joint. This method provides the most clear and vivid picture of the condition of the patient's soft tissues.
Treatments for a rotator cuff tear
The very first action of the doctor will be measures to relieve pain: usually, these are anti-inflammatory painkillers and ointments. Complete rest of the injured hand and fixation with a bandage or abduction splint is recommended. The application of cold, such as an ice pack, will help to remove swelling.
Surgical treatment
A complete rupture of the cuff will not be able to heal on its own, and therefore, immediate surgical intervention is required so as not to lose the motor function of the joint. In this case, it is important to perform the operation as early as possible, because an old injury leads to a shortening of the muscle and the impossibility of stretching it to its original length. In such cases, it is very difficult to return the tendon to its place and will require a lot of effort from the surgeon. The optimal period for the execution of the operation is several months from the moment of rupture.
In this case, it is important to perform the operation as early as possible, because an old injury leads to a shortening of the muscle and the impossibility of stretching it to its original length. In such cases, it is very difficult to return the tendon to its place and will require a lot of effort from the surgeon. The optimal period for the execution of the operation is several months from the moment of rupture.
During the surgical intervention, the damaged tendon is stretched, attaching it to its original position, and also sutured, if necessary. All lifeless tissues that have undergone degeneration are removed in order for the tendon to better adhere to the place of artificial attachment. Anchors are mainly used to attach the tendon. The anchor is screwed into the part of the bone where the soft tissues will subsequently be connected. Threads attached to the anchor are passed through the rotator cuff and pulled up to the bone with interrupted sutures. Thus, the sutures hold the tissues until the rupture sites are completely healed. The operation to restore the functions of the rotator cuff can be called quite complex, and it is performed by incision.
The operation to restore the functions of the rotator cuff can be called quite complex, and it is performed by incision.
Arthroscopic treatment
Arthroscopy is the most advanced method of surgical treatment of rupture of the rotator cuff. It is performed without an incision by creating a special puncture with a diameter of 1-2 centimeters. Through the puncture cavity, a camera is introduced into the joint - an arthroscope, thanks to which the surgeon sees a clear picture of the internal space of the joint. The image obtained from the surface of the arthroscope is transmitted to the screen, looking at which the surgeon performs all the necessary manipulations and simultaneously controls them.
An operation performed in this way is most preferable, since healing is much faster, and the tissues surrounding the joint are practically not damaged during the intervention. After surgery, the patient's arm is immobilized for several weeks by splinting. This will protect against the possibility of re-rupture and allow the tissues to heal after the operation.