Bipolar 2 criteria
DSM-5 Bipolar 2 Disorder: Criteria, Symptoms, & Treatments
Why is there a bipolar 2 and a bipolar 1? There’s no depression 2 or depression 1. There’s no anxiety 3.0. What makes bipolar disorder (formerly known as manic depression) different? The quick answer is that people with bipolar 2 have enough variation in their symptoms from type 1 bipolar to justify their own unique diagnosis. But the longer answer has to do with how we think about mental illness in general. If you or someone you love is struggling with the symptoms of bipolar 2 disorder, this guide will give you answers to your practical questions as well as some theoretical context for how mental health experts treat bipolar. Let’s get started.
What Is Bipolar 2 Disorder?
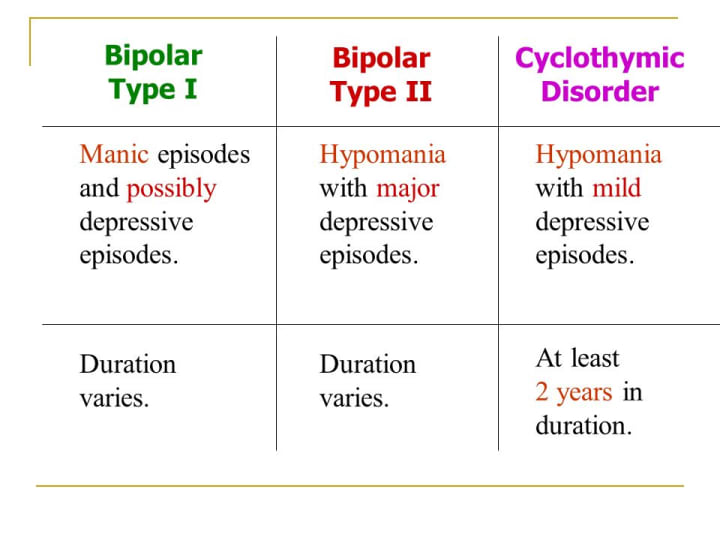
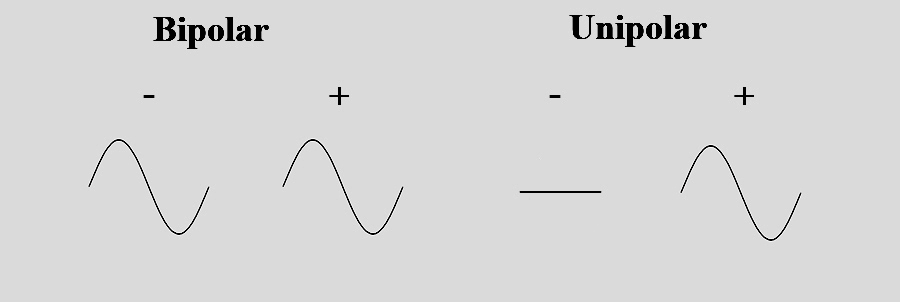
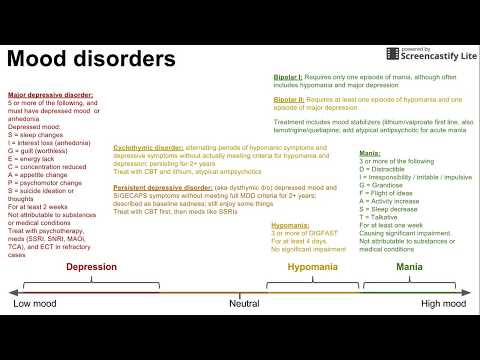
Bipolar 2 disorder is a type of bipolar disorder characterized by major depressive episodes and hypomanias, which are elevated moods that don’t meet the threshold for manias. While manic episodes are often severely debilitating, hypomanic episodes (sometimes called “baby” manic episodes) don’t impair daily living.
They might even be welcomed. But unfortunately they are just one side of a mood swing.
Because bipolar disorder affects emotional states, it’s commonly referred to as a mood disorder. It’s a long-term, chronic mental health condition that usually shows up by the time someone is in their mid-20s. Is bipolar type 2 serious? Yes, it’s serious because it can cause functional impairments and distress. But it can also be successfully treated and managed throughout the lifespan with medication and other interventions. It affects between 0.5 and 1% of the population.
What Is a Bipolar Disorder?
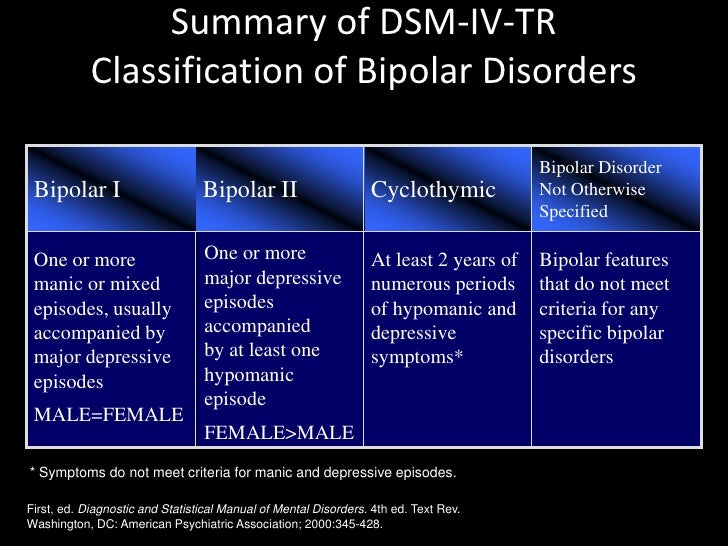
All bipolar disorders are characterized by mood swings of varying intensity. There’s some controversy about why someone can be diagnosed with bipolar 2 or bipolar 1 rather than just land somewhere on a spectrum of a single disorder. In fact, bipolar 2 wasn’t formally recognized by the American Psychiatric Association (APA) until 1994. The debate has to do with the ultimate usefulness and clinical accuracy of bipolar categories.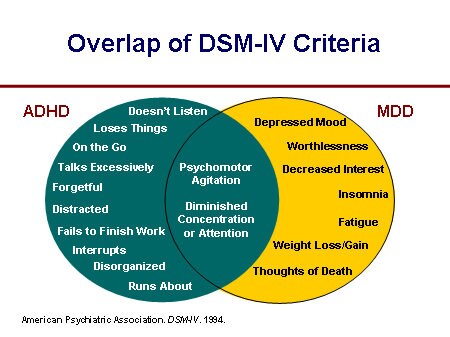 Are bipolar 1 and 2 actually different disorders, or do their symptoms just represent different dimensions of the same disorder?
Are bipolar 1 and 2 actually different disorders, or do their symptoms just represent different dimensions of the same disorder?
Some experts advocate for thinking of bipolar disorder in terms of predominant polarity (PP) rather than different categories (see the different types of bipolar below). For example, someone may have far more depressive episodes than manic episodes, so they would be “depression predominant.” Within this diagnosis clinicians can further specify bipolar disorder by severity and duration of symptoms.
All Types of Bipolar Disorder- Bipolar 1 disorder (aka bipolar I disorder or type I bipolar)
- Bipolar 2 disorder (aka bipolar II disorder or type 2 bipolar)
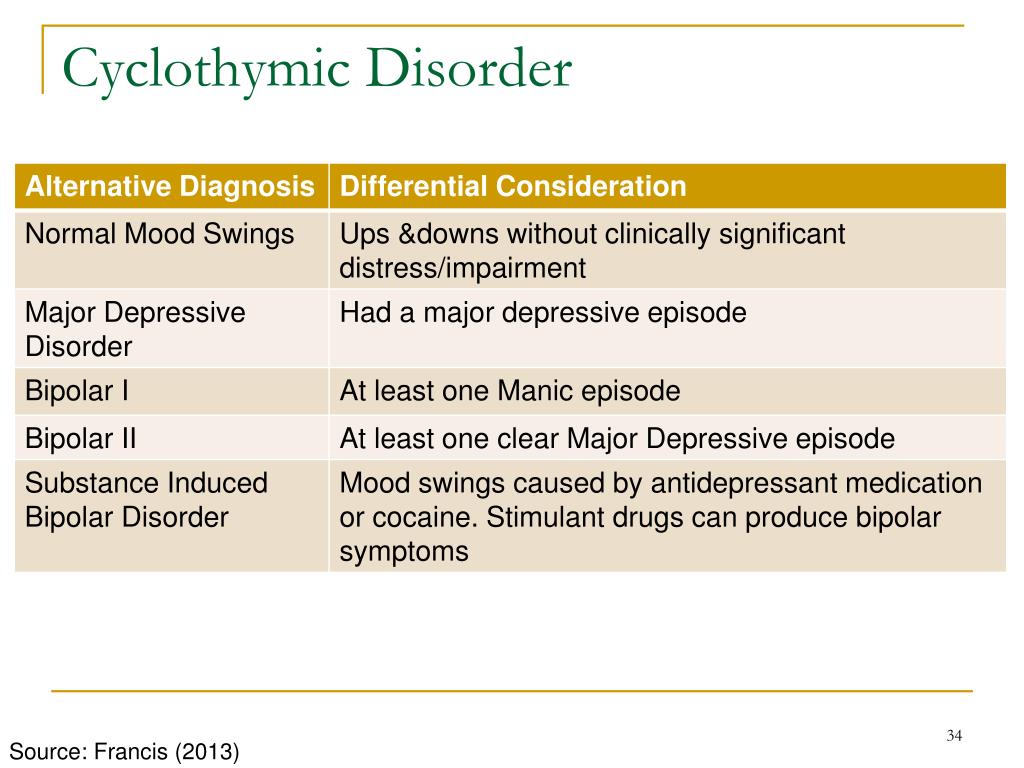
- Cyclothymic disorder
- Substance/medication-induced bipolar and related disorder
- Bipolar and related disorder due to another medical condition (like thyroid disease or multiple sclerosis)
- Other specified bipolar and related disorder
- Unspecified bipolar and related disorder
DSM 5 Bipolar 2 Criteria and Bipolar 2 Symptoms
To be diagnosed with bipolar 2 according to criteria laid out in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), someone must experience A) a hypomanic episode, and B) a major depressive episode.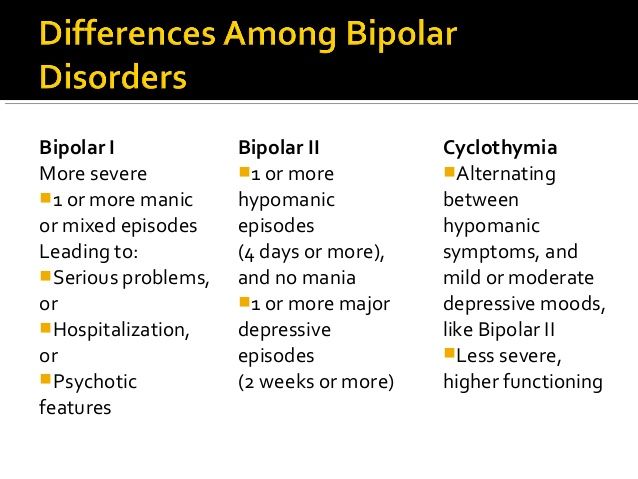 These can occur at any point over the course of a lifetime.
These can occur at any point over the course of a lifetime.
A. What qualifies as a hypomanic episode? An episode of bipolar 2 hypomania requires at least four days of elevated mood change, which might include feelings of increased energy, irritability, and expansiveness. During this time, you must have at least three of the following symptoms. If your mood has been exclusively irritable, you must have four of the following symptoms.
DSM-5 Symptoms of Hypomania- Exaggerated sense of well-being and self-confidence (euphoria), grandiosity
- Decreased need for sleep
- Unusual talkativeness
- Rushed/scattered thinking, racing thoughts
- Attention/focus issues, distractability
- Psychomotor agitation, which is an increase in purposeless physical activity (e.g., restlessness, pacing, tapping fingers or feet, abruptly starting and stopping tasks, rapidly talking, and moving items around without meaning) or increase in “activity toward goals”
- Impulsivity, poor decision-making, and risk-taking
All of these heightened, wired feelings and behaviors can’t be attributed to a substance, and they have to be so uncharacteristic that other people notice.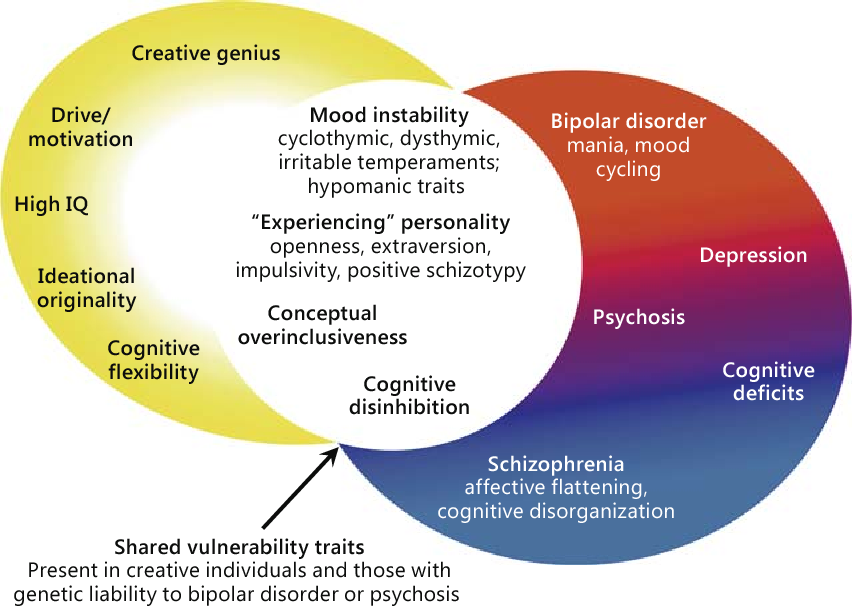 These symptoms don’t, however, cause enough functional impairments to qualify as mania.
These symptoms don’t, however, cause enough functional impairments to qualify as mania.
B. What qualifies as a depressive episode? A major depressive episode requires at least two weeks of major depressive disorder (MDD) symptoms.
DSM-5 Symptoms of Bipolar 2 DepressionA major depressive episode involves depressive symptoms that last at least two weeks and are severe enough to cause significant emotional and occupational distress. An episode of depression must involve a depressed mood or loss of interest and pleasure (anhedonia) in addition to at least four of the following symptoms:
- Significant changes in weight and/or appetite
- Sleeping too much (hypersomnia) or too little (insomnia)
- Restlessness or sluggishness
- Loss of energy
- Feeling extreme worthlessness or guilt
- Attention difficulties, indecisiveness
- Thinking about, planning, or attempting suicide
For people with bipolar 2, moods can fluctuate in different rhythms.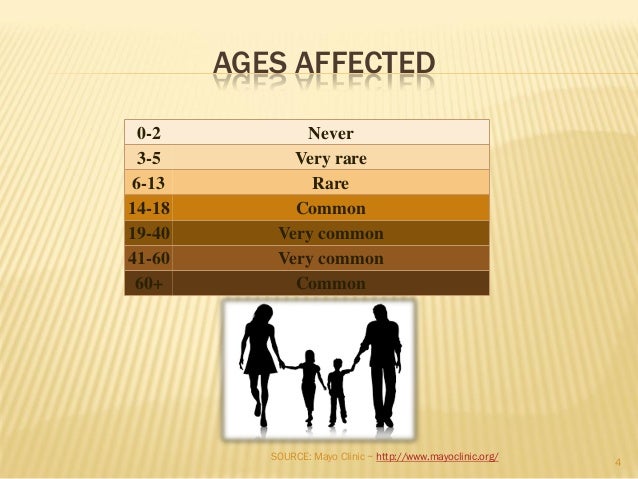 Someone with rapid-cycling bipolar 2 will swing between moods at quicker rates (at least four episodes in a year). To qualify for a bipolar 2 diagnosis, a hypomania episode must last at least four days and a major depressive cycle must last at least 14 days. If someone’s bipolar symptoms last for two years or more and they never meet the full criteria for a hypomanic episode or a major depressive episode, they may be diagnosed with cyclothymic disorder.
Someone with rapid-cycling bipolar 2 will swing between moods at quicker rates (at least four episodes in a year). To qualify for a bipolar 2 diagnosis, a hypomania episode must last at least four days and a major depressive cycle must last at least 14 days. If someone’s bipolar symptoms last for two years or more and they never meet the full criteria for a hypomanic episode or a major depressive episode, they may be diagnosed with cyclothymic disorder.
A bipolar meltdown is the colloquial term for a period of intense emotion that might feel uncontrollable. It can sometimes manifest as rage or aggression.
Bipolar 1 vs Bipolar 2
The most significant contrast between bipolar 1 and bipolar 2 is that the former tends to gravitate toward mania while the latter tends to gravitate toward depression. If someone with bipolar 2 has a single manic episode, they can no longer be diagnosed with bipolar 2. They have another type of bipolar disorder.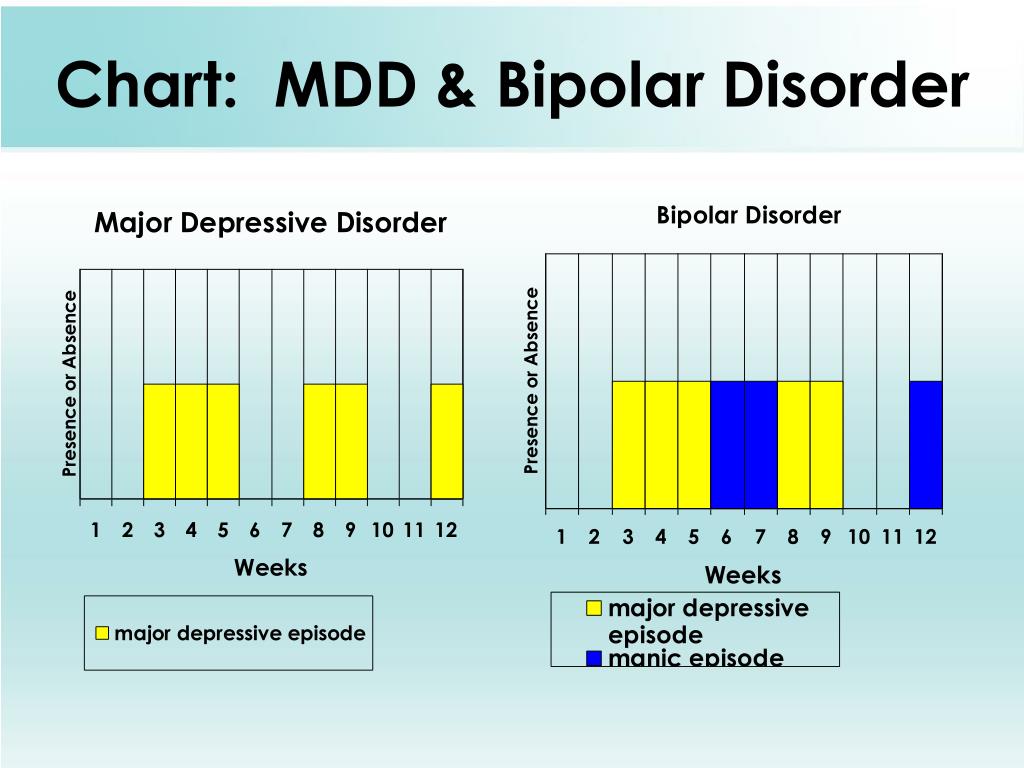
Even though hypomanias are a milder form of mania, it’s not true that bipolar 2 is a milder version of bipolar 1. By definition, hypomanias don’t cause impairment, but the major depressions that characterize bipolar 2 can be brutal. These depressive episodes also tend to happen more frequently than in bipolar 1. And the persistent, unreliable mood swings of bipolar 2 can cause significant harm to someone’s life.
Mania vs HypomaniaMania = at least 7 days of severe functional impairment, great excitement or euphoria, dangerous decision-making, delusions, hallucinations, suicidal thoughts/actions, or even psychosis that could lead to psychiatric hospitalization
Hypomania = at least 4 days of “enhanced” emotion that doesn’t cause significant impairment or extreme personality changes. The DSM-5 also leaves room for a 2-day, “short-duration” hypomania.
What Bipolar Is Worse, 1 or 2?One type of bipolar disorder is not worse than another. They all have their ups and downs, as it were. The worst type of bipolar disorder is untreated bipolar disorder, due to its potential to inflict suffering.
They all have their ups and downs, as it were. The worst type of bipolar disorder is untreated bipolar disorder, due to its potential to inflict suffering.
What Causes Bipolar 2 Disorder?
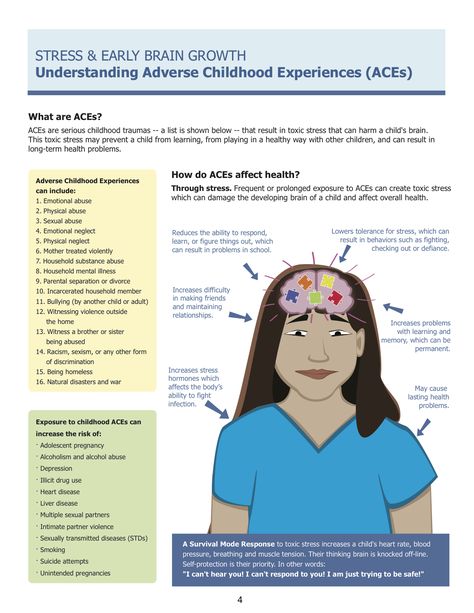
If you have a family member with bipolar 2 disorder, you have a greater risk of having the condition due to genetic factors. Its heritability might be as high as 70%. In fact, researchers recently identified 30 places (loci) on the human genome that are associated with bipolar disorder.
There may be physiological differences in the brains of people with bipolar disorder, but there are currently no biomarkers that can distinguish between bipolar 1 and bipolar 2.
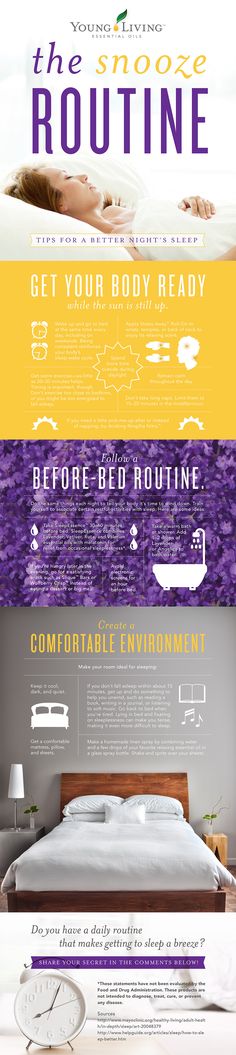
What Can Trigger Bipolar 2?As with many mental health disorders, symptoms of bipolar 2 can be triggered by stress, negative life events, changes in sleep patterns and seasonality (both associated with chronodisruption), substance use, and medications. Childbirth can also trigger hypomanic episodes.
What Is the Impact of Bipolar 2 Disorder?
Unpredictable mood swings and clinical depression can both be incredibly disruptive to someone’s life.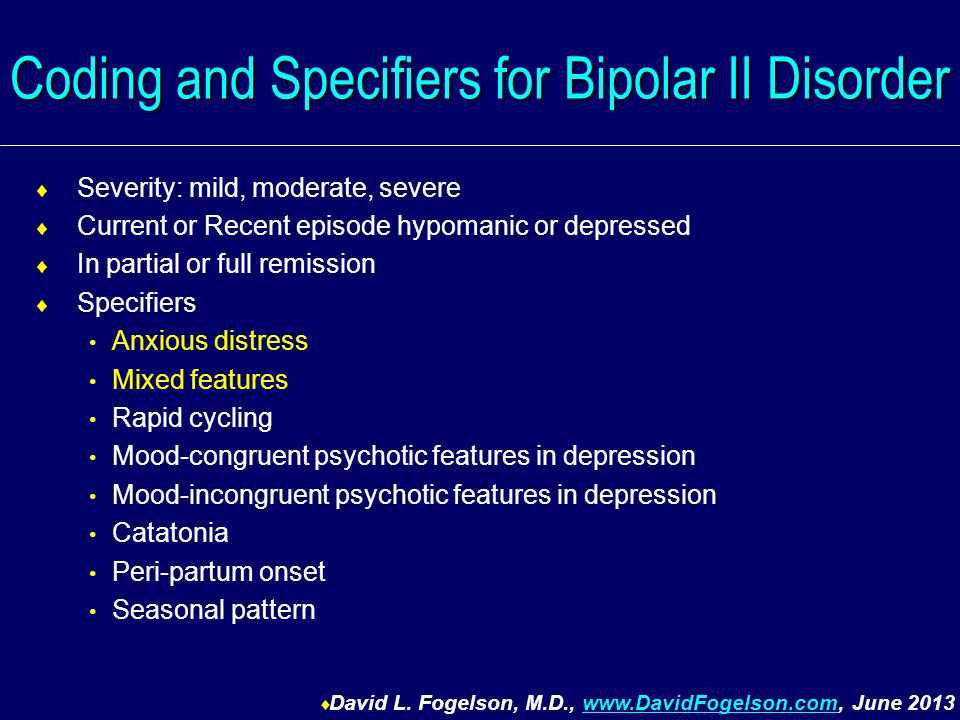 But when bipolar 2 is managed well, people with the disorder can function normally. It’s only when the disorder is left untreated that someone’s biography might take a dark turn or suffer an obstruction. Living with bipolar 2 involves adhering to a treatment plan, recognizing your triggers, and knowing how to get back on your feet if you have a relapse. You can’t cure the disorder, but you can definitely control the impact it has on your life.
But when bipolar 2 is managed well, people with the disorder can function normally. It’s only when the disorder is left untreated that someone’s biography might take a dark turn or suffer an obstruction. Living with bipolar 2 involves adhering to a treatment plan, recognizing your triggers, and knowing how to get back on your feet if you have a relapse. You can’t cure the disorder, but you can definitely control the impact it has on your life.
Many people with bipolar disorder find that a straighter lifestyle can also help flatten the peaks and valleys of their mood swings. This means they stick to a healthy sleep schedule, exercise regularly, eat well, avoid abusing drugs and alcohol, monitor caffeine intake, and try to minimize the stress in their lives.
If their daily habits change, they might start noticing changes in their mood. These can serve as warning signs (aka prodromal symptoms) so the person knows they need to reset their routine or or take other steps to stabilize. This kind of self-awareness and self-monitoring can also lead someone with bipolar 2 to know when they need extra support from friends and family, or from a mental health professional.
This kind of self-awareness and self-monitoring can also lead someone with bipolar 2 to know when they need extra support from friends and family, or from a mental health professional.
How Is Bipolar 2 Diagnosed?
Bipolar 2 can be diagnosed according to the DSM-5 criteria mentioned above, though different mental health professionals may have different perspectives on how to think about the disorder. Some clinicians may mark that distinct boundary between type 1 and type 2, while others may take a more dimensional approach, and think of the diagnostic boundaries as more fluid.
Bipolar 2 is often misdiagnosed as major depressive disorder (MDD). This is because a depressive episode precedes a hypomanic episode, or multiple depressive episodes occur before a hypomanic episode. In addition, people with bipolar 2 and MDD can both have irritability as a symptom. And because hypomanic episodes aren’t extreme or functionally impairing, they may go unrecognized.
Diagnosis can also be challenging because over half of people with bipolar 2 disorder have at least three additional disorders (aka comorbid disorders), particularly anxiety disorders, substance use disorders, personality disorders, and eating disorders.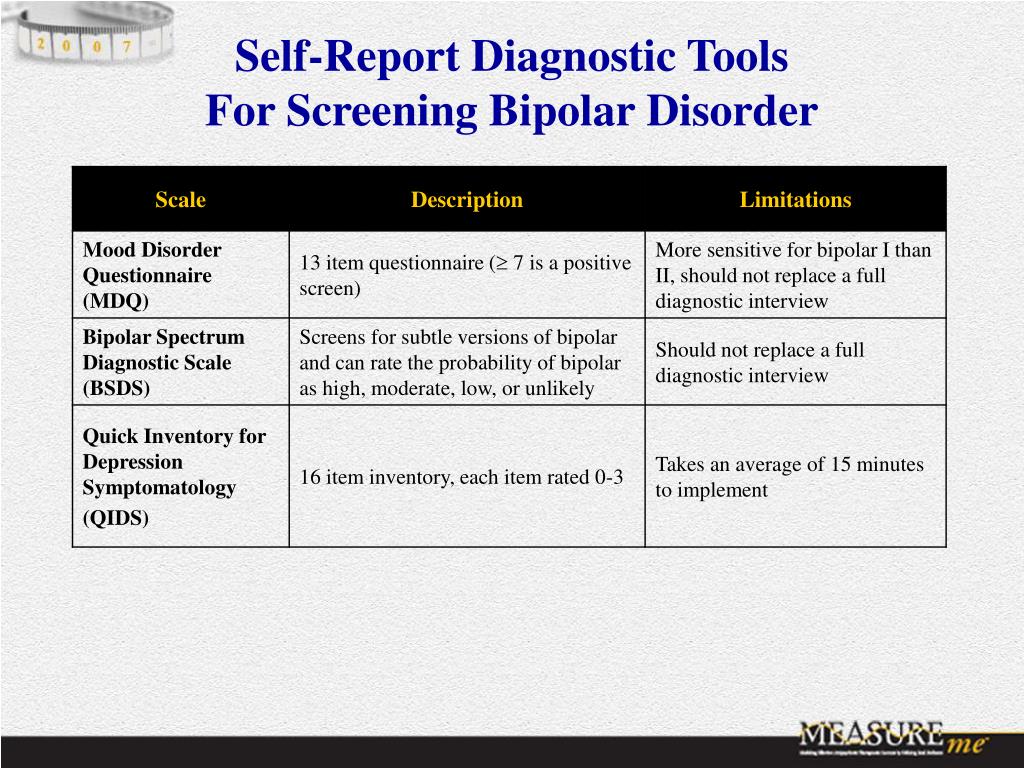
Is there a bipolar 2 test or a bipolar 2 checklist? Mental health professionals will have different ways of evaluating clients for bipolar disorder. A comprehensive test or screening often includes a physical assessment, a family history, a full psychiatric assessment, a mood disorder questionnaire (MDQ), and mood charting, which is when you keep a careful record of your daily emotions.
What Is the First-Line Treatment for Bipolar 2?
The first-line treatment for bipolar 2 is medication. More specifically, the first-line medications prescribed to manage bipolar 2 are often quetiapine (Seroquel), lithium, and lamotrigine (Lamictal). They are all monotherapies, meaning you take them exclusively. The second-line monotherapy treatments for bipolar 2 disorder are often venlafaxine (Effexor), an SNRI, and fluoxetine (Prozac), an SSRI. Anyone starting a new bipolar 2 medication should be monitored closely for side effects and adverse reactions like agitation or hypomania.
According to a comprehensive 2020 analysis, the best medication for an acute bipolar 2 depressive episode is quetiapine. This first-line treatment is followed by the second-line treatments lithium, lamotrigine, sertraline (Zoloft), venlafaxine, and, as an adjunct, buproprion (Wellbutrin). But all this medication guidance is subject to change as clinical knowledge grows. Bipolar 2 simply hasn’t been researched as extensively as bipolar 1.
The same medications that work for mania also seem to work for hypomania (when it requires treatment), namely the mood stabilizers lithium or divalproex (Depakote) and/or atypical antipsychotics.
Nonpharmacological Treatments for DSM-5 Bipolar 2 Disorder
- Psychoeducation and active monitoring
- Cognitive behavioral therapy (CBT)
- Interpersonal psychotherapy
- Behavioral activation
- Family-focused therapy (FFT)
- Complementary and alternative medicine (CAM) therapies
- Interpersonal and social rhythm therapy (IPSRT)
- Peer interventions such as support groups
Final Thoughts on Bipolar 2
Whether you think of bipolar 2 disorder as part of a bipolar spectrum or continuum, or as its own distinct disorder, it’s a serious mental health condition that can exact a high personal cost if left untreated. But people with any bipolar disorder have an excellent chance of thriving if they embrace these three ingredients as part of their experience:
But people with any bipolar disorder have an excellent chance of thriving if they embrace these three ingredients as part of their experience:
1) Consistent, compassionate, and continuous mental health care
2) Psychoeducation, which can help them monitor their moods and prevent relapse
3) Psychopharmacology (medication)
Finally, it’s important to let go of the idea that you can achieve perfect mastery over your illness. Perfectionism, self-criticism, and shaming beliefs are all associated with bipolar symptoms. You can try to protect yourself from these maladaptive feelings by practicing self-compassion. Stigma has no place in mental health care, whether it comes from the outside, or from within.
Updated Aug 16, 2022, published Jan 27, 2022, 1 min read.
Features 9 cited research articles. 4 comments
Fact-checked Why trust Thriveworks?
Table of contents
What Is Bipolar 2 Disorder?
What Is a Bipolar Disorder?
DSM 5 Bipolar 2 Criteria and Bipolar 2 Symptoms
Bipolar 1 vs Bipolar 2
What Causes Bipolar 2 Disorder?
What Is the Impact of Bipolar 2 Disorder?
How Is Bipolar 2 Diagnosed?
Show all items
What Is the First-Line Treatment for Bipolar 2?
Nonpharmacological Treatments for DSM-5 Bipolar 2 Disorder
Final Thoughts on Bipolar 2
Recent articles
View all
Want to talk to a therapist? We have over 2,000 providers across the US ready to help you in person or online.
Book a session 855-641-1379
- Reviewer
- Author
- 9 sources
- Update history
Medically reviewed by Elizabeth Fiser, PMHNP
Elizabeth Fiser is a Psychiatric Mental Health Nurse Practitioner (PMHNP) who specializes in a range of areas including alcohol use, addiction, anxiety, depression, trauma and PTSD, women’s issues, and more.
Written by Wistar Murray
Wistar Murray writes about mental health at Thriveworks. She completed her BA at the College of William & Mary and her MFA at Columbia University.
We only use authoritative, trusted, and current sources in our articles. Read our editorial policy to learn more about our efforts to deliver factual, trustworthy information.
Goodwin, G. M., Haddad, P.
 M., Ferrier, I. N., Aronson, J. K., Barnes, T., Cipriani, A., Coghill, D. R., Fazel, S., Geddes, J. R., Grunze, H., Holmes, E. A., Howes, O., Hudson, S., Hunt, N., Jones, I., Macmillan, I. C., McAllister-Williams, H., Miklowitz, D. R., Morriss, R., Munafò, M., … Young, A. H. (2016). Evidence-based guidelines for treating bipolar disorder: Revised third edition recommendations from the British Association for Psychopharmacology. Journal of psychopharmacology (Oxford, England), 30(6), 495–553. https://doi.org/10.1177/0269881116636545
M., Ferrier, I. N., Aronson, J. K., Barnes, T., Cipriani, A., Coghill, D. R., Fazel, S., Geddes, J. R., Grunze, H., Holmes, E. A., Howes, O., Hudson, S., Hunt, N., Jones, I., Macmillan, I. C., McAllister-Williams, H., Miklowitz, D. R., Morriss, R., Munafò, M., … Young, A. H. (2016). Evidence-based guidelines for treating bipolar disorder: Revised third edition recommendations from the British Association for Psychopharmacology. Journal of psychopharmacology (Oxford, England), 30(6), 495–553. https://doi.org/10.1177/0269881116636545Gitlin, M., & Malhi, G. S. (2020). The existential crisis of bipolar II disorder. International journal of bipolar disorders, 8(1), 5. https://doi.org/10.1186/s40345-019-0175-7
Carvalho, A. F., McIntyre, R. S., Dimelis, D., Gonda, X., Berk, M., Nunes-Neto, P.
 R., Cha, D. S., Hyphantis, T. N., Angst, J., & Fountoulakis, K. N. (2014). Predominant polarity as a course specifier for bipolar disorder: a systematic review. Journal of affective disorders, 163, 56–64. https://doi.org/10.1016/j.jad.2014.03.035
R., Cha, D. S., Hyphantis, T. N., Angst, J., & Fountoulakis, K. N. (2014). Predominant polarity as a course specifier for bipolar disorder: a systematic review. Journal of affective disorders, 163, 56–64. https://doi.org/10.1016/j.jad.2014.03.035McGuffin, P., Rijsdijk, F., Andrew, M., Sham, P., Katz, R., & Cardno, A. (2003). The heritability of bipolar affective disorder and the genetic relationship to unipolar depression. Archives of general psychiatry, 60(5), 497–502. https://doi.org/10.1001/archpsyc.60.5.497
Stahl, E. A., Breen, G., Forstner, A. J., McQuillin, A., Ripke, S., Trubetskoy, V., Mattheisen, M., Wang, Y., Coleman, J., Gaspar, H. A., de Leeuw, C. A., Steinberg, S., Pavlides, J., Trzaskowski, M., Byrne, E. M., Pers, T. H., Holmans, P. A., Richards, A. L., Abbott, L.
 , Agerbo, E., … Bipolar Disorder Working Group of the Psychiatric Genomics Consortium (2019). Genome-wide association study identifies 30 loci associated with bipolar disorder. Nature genetics, 51(5), 793–803. https://doi.org/10.1038/s41588-019-0397-8
, Agerbo, E., … Bipolar Disorder Working Group of the Psychiatric Genomics Consortium (2019). Genome-wide association study identifies 30 loci associated with bipolar disorder. Nature genetics, 51(5), 793–803. https://doi.org/10.1038/s41588-019-0397-8Koenders, M. A., Giltay, E. J., Spijker, A. T., Hoencamp, E., Spinhoven, P., & Elzinga, B. M. (2014). Stressful life events in bipolar I and II disorder: cause or consequence of mood symptoms?. Journal of affective disorders, 161, 55–64. https://doi.org/10.1016/j.jad.2014.02.036
Jones, I., Chandra, P. S., Dazzan, P., & Howard, L. M. (2014). Bipolar disorder, affective psychosis, and schizophrenia in pregnancy and the post-partum period. Lancet (London, England), 384(9956), 1789–1799. https://doi.org/10.1016/S0140-6736(14)61278-2
Yatham, L.
 N., Kennedy, S. H., Parikh, S. V., Schaffer, A., Bond, D. J., Frey, B. N., Sharma, V., Goldstein, B. I., Rej, S., Beaulieu, S., Alda, M., MacQueen, G., Milev, R. V., Ravindran, A., O’Donovan, C., McIntosh, D., Lam, R. W., Vazquez, G., Kapczinski, F., McIntyre, R. S., … Berk, M. (2018). Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar disorders, 20(2), 97–170. https://doi.org/10.1111/bdi.12609
N., Kennedy, S. H., Parikh, S. V., Schaffer, A., Bond, D. J., Frey, B. N., Sharma, V., Goldstein, B. I., Rej, S., Beaulieu, S., Alda, M., MacQueen, G., Milev, R. V., Ravindran, A., O’Donovan, C., McIntosh, D., Lam, R. W., Vazquez, G., Kapczinski, F., McIntyre, R. S., … Berk, M. (2018). Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar disorders, 20(2), 97–170. https://doi.org/10.1111/bdi.12609Steardo, L., Jr, Luciano, M., Sampogna, G., Zinno, F., Saviano, P., Staltari, F., Segura Garcia, C., De Fazio, P., & Fiorillo, A. (2020). Efficacy of the interpersonal and social rhythm therapy (IPSRT) in patients with bipolar disorder: results from a real-world, controlled trial. Annals of general psychiatry, 19, 15. https://doi.org/10.
 1186/s12991-020-00266-7
1186/s12991-020-00266-7
We update our content on a regular basis to ensure it reflects the most up-to-date, relevant, and valuable information. When we make a significant change, we summarize the updates and list the date on which they occurred. Read our editorial policy to learn more.
Originally published on May 25, 2017
Author: Lenora KM
Updated on January 27, 2022
Author: Lenora KM
Editor: Wistar Murray
Changes: Content added about the efficacy of medication, which is a front-line, evidence-based treatment for bipolar 2 disorder.
Updated on August 16, 2022
Author: Wistar Murray
Reviewer: Elizabeth Fiser, PMHNP
Changes: Added multiple sections and clarified relationship between bipolar 2 and bipolar 1 disorders.
 Clinically/medically reviewed to confirm the accuracy and enhance value.
Clinically/medically reviewed to confirm the accuracy and enhance value.
Are you struggling?
Thriveworks can help.
Browse top-rated therapists near you, and find one who meets your needs. We accept most insurances, and offer weekend and evening sessions.
Book a session 855-641-1379
Rated 4.5 overall from 10,849 Google reviews
Popular articles
Disclaimer
The information on this page is not intended to replace assistance, diagnosis, or treatment from a clinical or medical professional. Readers are urged to seek professional help if they are struggling with a mental health condition or another health concern.
If you’re in a crisis, do not use this site. Please call the Suicide & Crisis Lifeline at 988 or use these resources to get immediate help.
Quick Links
How can we help you?
Bipolar Definition and DSM-5 Diagnostic Criteria
What is Bipolar Disorder?
Bipolar disorders are described by the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-5) as a group of brain disorders that cause extreme fluctuation in a person’s mood, energy, and ability to function.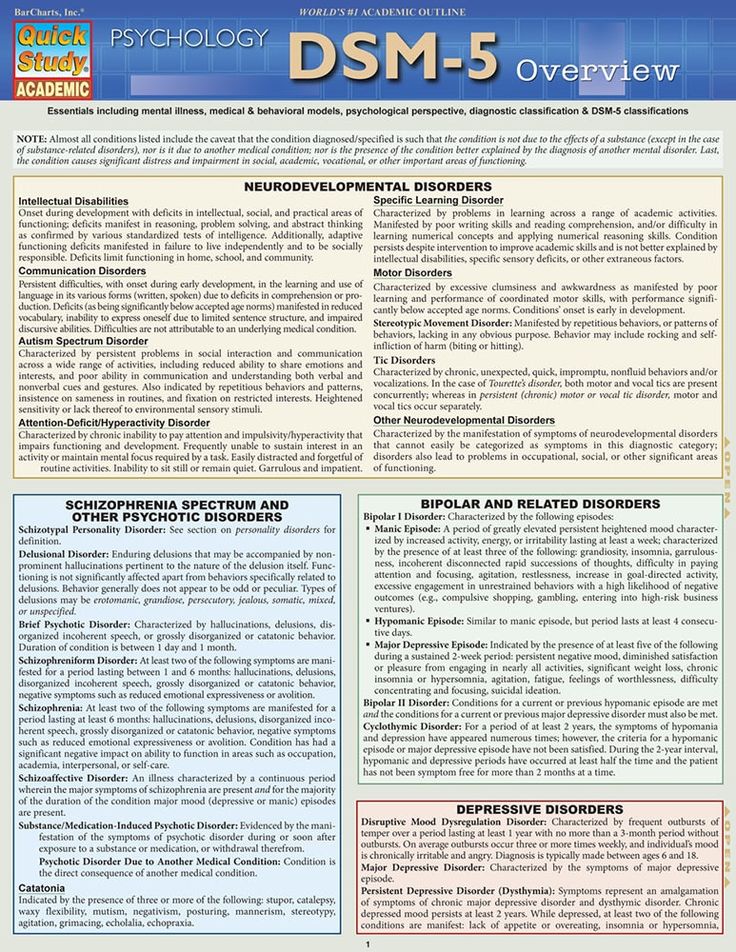
Bipolar disorder is a category that includes three different condition--bipolar I, bipolar II, and cyclothymic disorder.
Bipolar I disorder is a manic-depressive disorder that can exist both with and without psychotic episodes
Bipolar II disorder consists of depressive and manic episodes which alternate and are typically less severe and do not inhibit function
Cyclothymic disorder is a cyclic disorder that causes brief episodes of hypomania and depression
Bipolar and related disorders are given a chapter of their own in the DSM-5, between depressive disorders and schizophrenia spectrum disorders. People who live with bipolar disorder experience periods of great excitement, overactivity, delusions, and euphoria (known as mania) and other periods of feeling sad and hopeless (known as depression). As such, the use of the word bipolar reflects this fluctuation between extreme highs and extreme lows.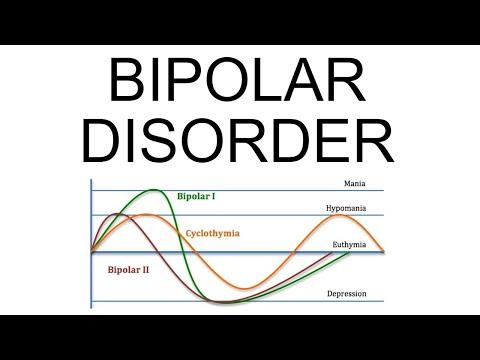 The diagnosis is frequently assigned to young patients presenting with a (first) major depressive episode. In these cases, diagnosis is exclusively based on psychiatric history provided by family and caregivers, not on the current psychopathological assessment by the psychiatrist.
The diagnosis is frequently assigned to young patients presenting with a (first) major depressive episode. In these cases, diagnosis is exclusively based on psychiatric history provided by family and caregivers, not on the current psychopathological assessment by the psychiatrist.
Bipolar disorder occurs in up to 2.5% of the population, but the prevalence is much higher among first-degree relatives of individuals with bipolar or schizophrenia disorder. Individuals with bipolar disorder experience mood swings that are less severe in intensity. During what is known as a hypomanic episode, a person may experience elevated mood, increased self-esteem, and a decreased need for sleep. Unlike a manic episode, these symptoms are not so severe as to impact daily functioning or cause psychotic symptoms.
What’s more, in some cases, a bipolar episode can include symptoms of both mania and depression; this is what’s known as an episode with mixed features. People experiencing an episode with mixed features may feel extreme sadness, guilt, and worthlessness, while at the same experiencing high energy, racing thoughts and speech, and overactivity. It is not uncommon during a mixed episode for a person to go from being exuberantly happy to be expressing suicidal thoughts in a matter of moments.
It is not uncommon during a mixed episode for a person to go from being exuberantly happy to be expressing suicidal thoughts in a matter of moments.
Bipolar Disorder DSM-5 Diagnostic Criteria
Talking with a doctor or mental health professional is the first step in identifying bipolar disorder. Firstly, a doctor may perform a physical evaluation to rule out any other conditions that may be causing symptoms. If no other illnesses are present, the doctor will conduct a comprehensive mental health evaluation to assess the patient’s symptoms in accordance with the specific criteria from the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-5). To be diagnosed with bipolar disorder, a person must have experienced at least one episode of mania or hypomania.
To be considered mania, the elevated, expansive, or irritable mood must last for at least one week and be present most of the day, nearly every day. To be considered hypomania, the mood must last at least four consecutive days and be present most of the day, almost every day.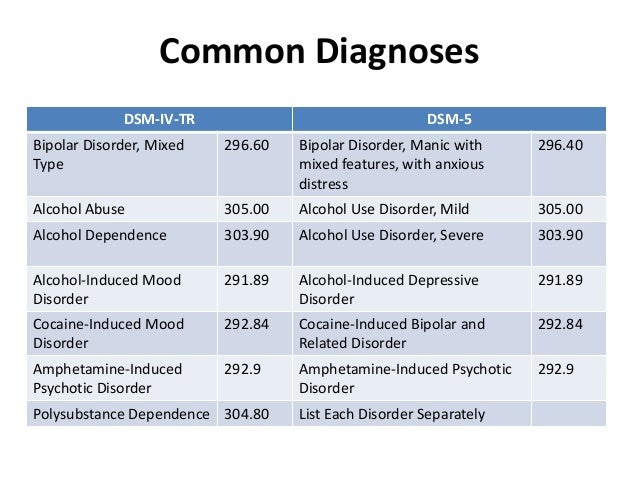
During this period, three or more of the following symptoms must be present and represent a significant change from usual behavior:
Inflated self-esteem or grandiosity
Decreased need for sleep
Increased talkativeness
Racing thoughts
Distracted easily
Increase in goal-directed activity or psychomotor agitation
Engaging in activities that hold the potential for painful consequences, e.g., unrestrained buying sprees
The depressive side of bipolar disorder is characterized by a major depressive episode resulting in depressed mood or loss of interest or pleasure in life. The DSM-5 states that a person must experience five or more of the following symptoms in two weeks to be diagnosed with a major depressive episode:
Depressed mood most of the day, nearly every day
Loss of interest or pleasure in all, or almost all, activities
Significant weight loss or decrease or increase in appetite
Engaging in purposeless movements, such as pacing the room
Fatigue or loss of energy
Feelings of worthlessness or guilt
Diminished ability to think or concentrate, or indecisiveness
Recurrent thoughts of death, recurrent suicidal ideation without a specific plan, or a suicide attempt
Could My Mood Swings Be Bipolar Disorder?
We all have good and bad days –sometimes we feel on top of the world and other days, if we lose a job, go through a bad break-up, or fall out with a friend, we may be down in the dumps.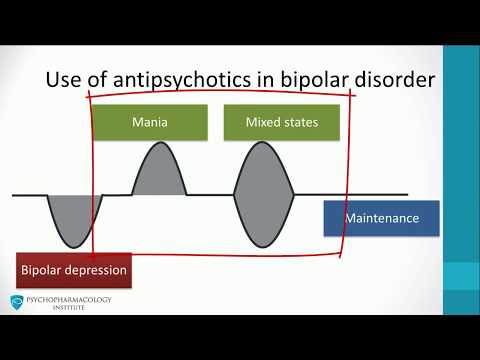 But have you ever gone to bed one night feeling euphoric and woken up the next morning to find you feel empty and hopeless? Have you ever noticed your high-energy levels and racing thoughts suddenly turn to feelings of worthlessness and an inability to experience pleasure doing the same things you once enjoyed? If not, it’s unlikely that you have bipolar disorder.
But have you ever gone to bed one night feeling euphoric and woken up the next morning to find you feel empty and hopeless? Have you ever noticed your high-energy levels and racing thoughts suddenly turn to feelings of worthlessness and an inability to experience pleasure doing the same things you once enjoyed? If not, it’s unlikely that you have bipolar disorder.
Several important features of bipolar disorder allow us to distinguish between the severe mental condition and the occasional mood swing. The first feature is whether the fluctuations in mood are caused by a situation, person, or event, or appear without cause. While the moods of people with bipolar disorder can be affected by situational variables, people with bipolar disorder also frequently become manic or depressed for no apparent reason. In comparison, for most people, moodiness is tied to a situational event, particularly stressful period, or even hormonal changes in the body.
The duration and intensity of high and low moods are also factors to consider when making a judgment on whether you should be concerned about bipolar disorder. Individuals with bipolar experience an elevated or irritable mood for at least four consecutive days, while their depressive episodes last for at least two weeks at a time. If you’re struggling with moodiness, the intensity of the moods you are experiencing is likely significantly higher on the intensity scale than those of people with bipolar disorder.
Individuals with bipolar experience an elevated or irritable mood for at least four consecutive days, while their depressive episodes last for at least two weeks at a time. If you’re struggling with moodiness, the intensity of the moods you are experiencing is likely significantly higher on the intensity scale than those of people with bipolar disorder.
If you’re unsure about whether your mood swings are normal or could be symptomatic of bipolar disorder. You may want to start a mood diary using an app such as "Daylio" to help keep track and monitor your mood fluctuations. Psychologists and therapists suggest that this can be a therapeutic activity. It can also help you to determine whether events or situations in your life cause your mood swings or if they appear seemingly without cause.
If you are concerned about bipolar disorder, we encourage you to make an appointment with your doctor or mental health professional to discuss the specific details of your fluctuating mood.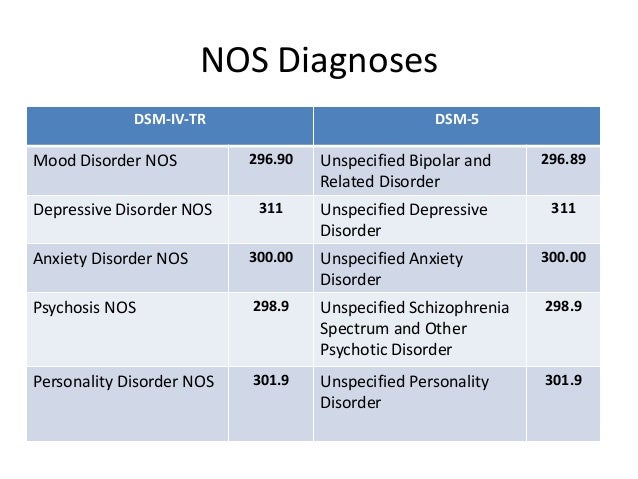
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th Edition. Arlington, VA: American Psychiatric Association; 2013.
Notes: This article was originally published October 13, 2019 and most recently updated September 29, 2020.
classification, epidemiology, diagnosis and treatment
Bipolar disorder (BD) is a fairly widespread severe chronic mood disorder characterized by episodes of mania or hypomania alternating or combined with episodes of depression. BD is often combined with mental and somatic comorbidity and is associated with an increased level of mortality, primarily from suicide. The incidence of suicide in patients with BD is 15 times higher than in the general population [1]. Suicide ends the life of 10-20% of patients with BD [2]. The latter also have increased mortality due to somatic diseases, including cardiovascular, cerebrovascular, and malignant ones [3].
BR has a negative psychosocial impact on patients and their families. Thus, the probability of unemployment in patients with BD is two to three times higher than that of people who do not suffer from this disease, the probability of divorce is two times [4]. 64% of men and 42% of women with BD do not have children [2]. Dissatisfaction with the quality of life in these patients is observed much more often than among healthy people [5].
Thus, the probability of unemployment in patients with BD is two to three times higher than that of people who do not suffer from this disease, the probability of divorce is two times [4]. 64% of men and 42% of women with BD do not have children [2]. Dissatisfaction with the quality of life in these patients is observed much more often than among healthy people [5].
BR is also a heavy economic burden on society. For example, in Australia, BD is the 6th leading cause of disability in the population [4]. At the same time, no more than 25% of patients with BD receive the correct therapy. As a result, individuals with BD use significantly more medical services than patients with unipolar depression or chronic physical illness [6]. At 19In 1999, the direct economic costs of BD were estimated at $60 billion [7], while the indirect costs, mainly associated with a decrease in labor productivity, amounted to about $30 billion per year [8].
Classification of bipolar disorders and their episodes
The classification of the American Psychiatric Association (4th edition - DSM-IV) distinguishes:
Type I BR - the presence of at least one manic or mixed episode.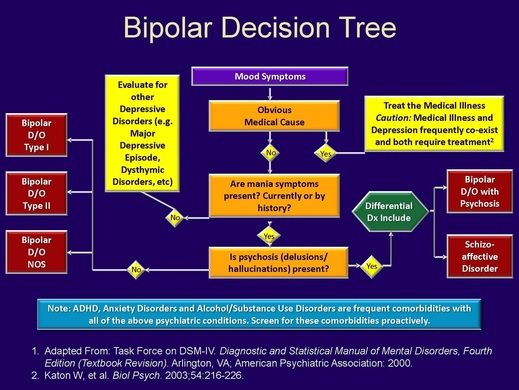 Episodes of major depressive disorder are often observed, but they are not mandatory;
Episodes of major depressive disorder are often observed, but they are not mandatory;
BD type II - the presence of at least one hypomanic and one depressive episode. There are no manic or mixed episodes;
BR without additional clarifications [9].
The course of the disease in many patients does not fully meet the criteria for BR-I or BR-II, therefore, the concept of bipolar spectrum disorders is often used to describe course variants. These include borderline BR-II, affective temperament (hyperthymic, dysthymic, cyclothymic, irritable), BR-III (cyclothymia), BR-IV, BR-V and BR-VI (including patients with a hereditary burden of BD, the so-called. unipolar mania, mania caused by antidepressants, hyperthymic depression, etc.) [10].
The DSM-IV classification distinguishes the following current episodes of BD:
episodes of mania;
episodes of hypomania;
episodes of major depressive disorders;
mixed episodes;
cyclothymia;
fast cycling.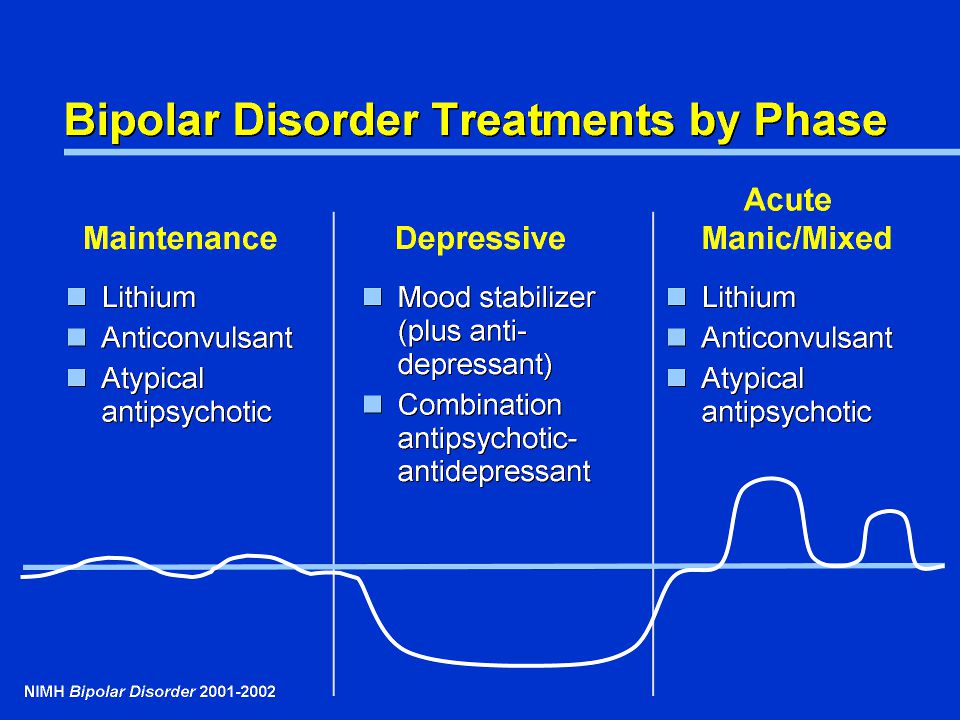
A manic episode is characterized by elevated mood and increased volume and pace of physical and mental activity. The most common symptoms of mania include: increased energy, activity, and restlessness; excessively good, euphoric mood; excessive excitability; a significant number of plans and ideas, quick switching from one idea to another; jumping thoughts and fast speech; absent-mindedness, the impossibility of a good concentration of attention; low need for sleep; unrealistic faith in one's own abilities and strength; low level of criticism; prodigality; increased sexual interest; abuse of alcohol and other pharmacologically active substances; provocative, obsessive or aggressive behavior.
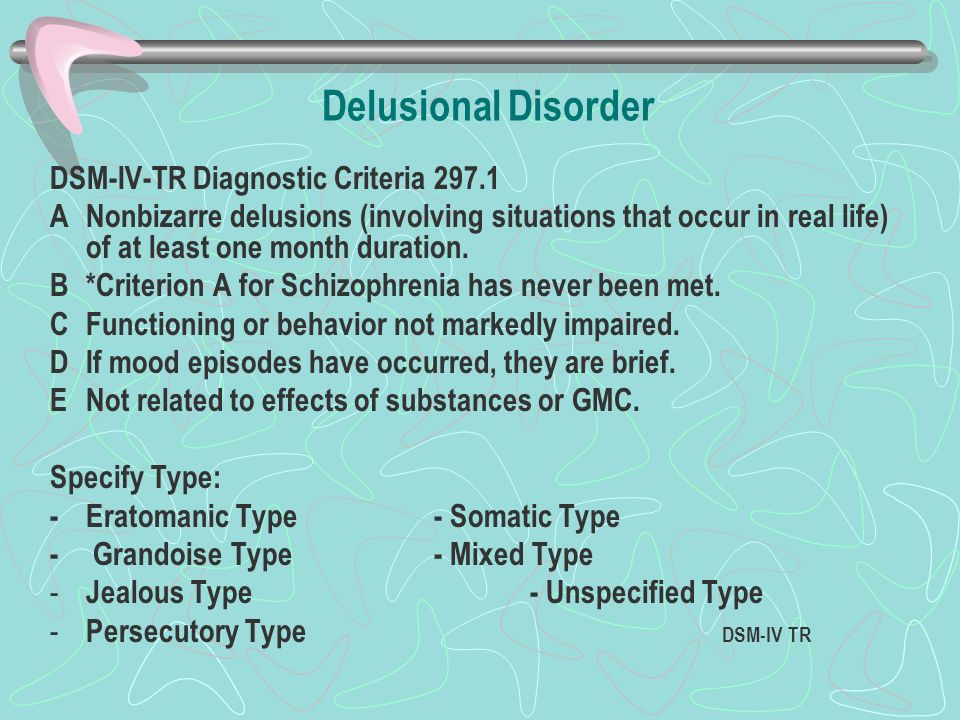
Up to 86% of BD patients experience psychotic symptoms (delusions, hallucinations) throughout their lives [2].
Hypomania is defined as mild mania without psychotic symptoms (delusions or hallucinations). According to the DSM-IV, to diagnose mania, it is necessary that its symptoms have been observed for at least seven days, hypomania - four days. Signs and symptoms of depression in BD are summarized in Table 1. 1. (see full article)
Signs and symptoms of depression in BD are summarized in Table 1. 1. (see full article)
Patients with BD experience both minor and major depressive disorders during the course of their illness. The question of the presence of specific signs of bipolar depression remains unresolved.
Most patients are depressed most of the time. The latter is more likely to be the first episode of BD, especially in women. Patients with BR-I are depressed on average 32% of the time and 9% are manic or hypomanic, while patients with BR-II are depressed 50% of the time and only 1% are hypomanic [12]. About 80% of all suicides in patients with BD occur during the depression phase [1].
Mixed manic-depressive episodes are states that meet the criteria for both mania and depression and last more than 7 days. Mixed episodes can occur at any stage of the disease and are associated with worse short- and long-term prognosis.
Cyclothymia is characterized by the presence of prolonged subdepressive and hypomanic symptoms in the absence of severe depressive disorders or mania.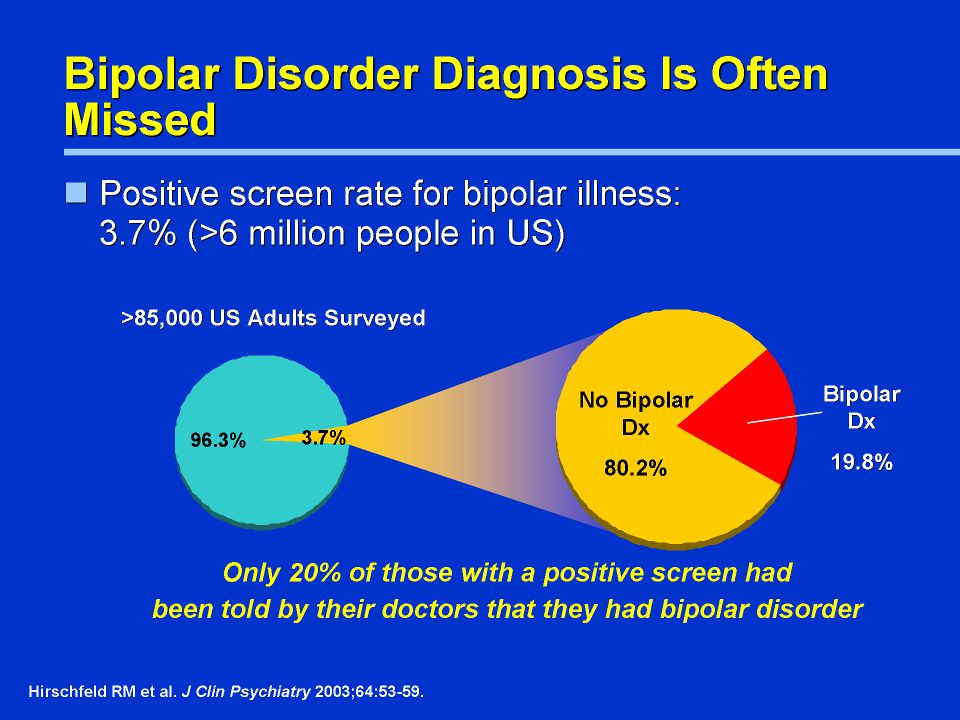 It is often compared to unipolar depression dysthymia and is diagnosed when a patient has had frequent bouts of depressed mood, including anhedonia, alternating with bouts that meet some of the criteria for a hypomanic state for at least two years. Some patients with cyclothymia subsequently develop typical BR.
It is often compared to unipolar depression dysthymia and is diagnosed when a patient has had frequent bouts of depressed mood, including anhedonia, alternating with bouts that meet some of the criteria for a hypomanic state for at least two years. Some patients with cyclothymia subsequently develop typical BR.
The criterion for rapid cycling is the presence of at least four episodes of the disease per year with partial or complete remission between them or a direct switch from one polarity to another (from mania to depression or vice versa). In some patients, phase inversion can occur very quickly (within hours) and can reach four episodes per day. Rapid cycling is typical for approximately 10-15% of patients. In contrast, the "average" BD patient has four episodes of mood disorders in the first 10 years after diagnosis. Rapid cycling is more common in the late stages of the disease and is associated with female sex and BR-II [13]. Secondary causes of rapid cycling are hypothyroidism (including lithium-induced), alcohol and other substance abuse, comorbid somatic diseases such as sleep apnea, multiple sclerosis, and head trauma [14]. In 30-40% of cases, a rapid phase change is preceded by the use of antidepressants [12]..........
In 30-40% of cases, a rapid phase change is preceded by the use of antidepressants [12]..........
Download the full article
Ushkalova A.V.
Department of Psychiatry and Medical Psychology, Peoples' Friendship University of Russia, Moscow
Published in: Pharmateka, 2007, No. 7 (142) Neurology, Psychiatry
Bipolar affective disorder (BAD), its signs, types and methods of treatment from the outside. However, when these changes are excessive, often unexpected and for no apparent reason, emotions get out of control, or a person remains in a radically positive or negative mood for a long time, it is very likely that bipolar disorder can be diagnosed. This disease was first described at the end of 19century, the famous German psychiatrist Emil Kripelin, calling it manic-depressive psychosis. Many world famous personalities such as Vincent van Gogh, Isaac Newton, Ludwig van Beethoven, Abraham Lincoln suffered from this disease.
 The pronounced form of this disease, which in the international classification of diseases is called bipolar affective disorder (BAD), is detected in 3% of the world's population.
The pronounced form of this disease, which in the international classification of diseases is called bipolar affective disorder (BAD), is detected in 3% of the world's population. TABLE OF CONTENTS
- 1. Bipolar Personality Disorder - Overview
- 2. Symptoms and signs
- 3. Types of Bipolar Disorder
- 4. Phases of Bipolar Disorder
- 5. Bipolar disorder in women
- 6. Treatment of Bipolar Personality Disorder
It is not uncommon for women to be treated with a combination of drug therapy and cognitive behavioral or interpersonal therapy with a psychotherapist.
Bipolar personality disorder - general information
According to statistics, bipolar disorder affects people between 14 and 44 years of age. Unlike adults, children and adolescents experience more frequent mood swings from mania to depression, sometimes several times a day. 90% of young people make their debut precisely from the phase of depression or melancholy. Another feature of bipolar disorder is that, due to the low level of diagnosis, the patient can live with this disease for 5-10 years without knowing the cause of the painful symptoms.
Another feature of bipolar disorder is that, due to the low level of diagnosis, the patient can live with this disease for 5-10 years without knowing the cause of the painful symptoms.
Most often, bipolar disorder is diagnosed in people whose immediate family members have had a similar problem. The causes of this disease are unknown, but stress, overstrain, and various diseases can provoke the manifestation of its symptoms. However, having fenced off a person from the influence of these factors, it is impossible to get rid of the problem, you need to seek help from a psychotherapist.
Bipolar disorder is a disease that cannot be completely cured. But with properly selected medication and psychotherapy, the quality of life is significantly improved and the periods between phases are lengthened. The person remains socialized and able to work.
Symptoms and signs
From the name it is clear that we are talking about two different poles of affective manifestations, that is, mood manifestations.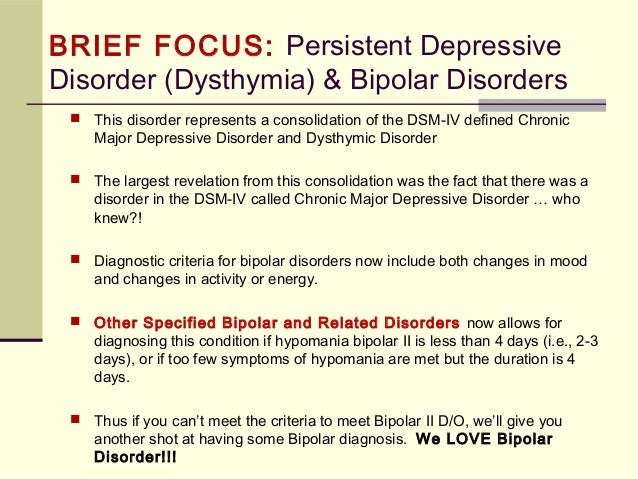 One of these conditions is depression. Depression in bipolar disorder is pronounced, with vivid symptoms. It can last up to a year and is manifested not only by low mood, lack of ability to enjoy and interest in ongoing events, but also by psychosis, when ideas of self-accusation arise, the patient feels inferior, unnecessary, poisoning the life of others. There are also nihilistic thoughts about suffering from some kind of severe illness, despite medical evidence to the contrary. There may be delusional thoughts, as well as suicidal thoughts and even attempts.
One of these conditions is depression. Depression in bipolar disorder is pronounced, with vivid symptoms. It can last up to a year and is manifested not only by low mood, lack of ability to enjoy and interest in ongoing events, but also by psychosis, when ideas of self-accusation arise, the patient feels inferior, unnecessary, poisoning the life of others. There are also nihilistic thoughts about suffering from some kind of severe illness, despite medical evidence to the contrary. There may be delusional thoughts, as well as suicidal thoughts and even attempts.
The other pole of bipolar disorder is a hypomanic state or hypomania, the characteristic features of which are an increased euphoric emotional background, the patient is constantly on the move, hyperactive, and is distinguished by very fast, associative speech. The patient is constantly cheerful, often hypersexual, almost always awake or sleeping 2-3 hours a day.
Hypomania is often followed by a manic bipolar state with psychotic manifestations.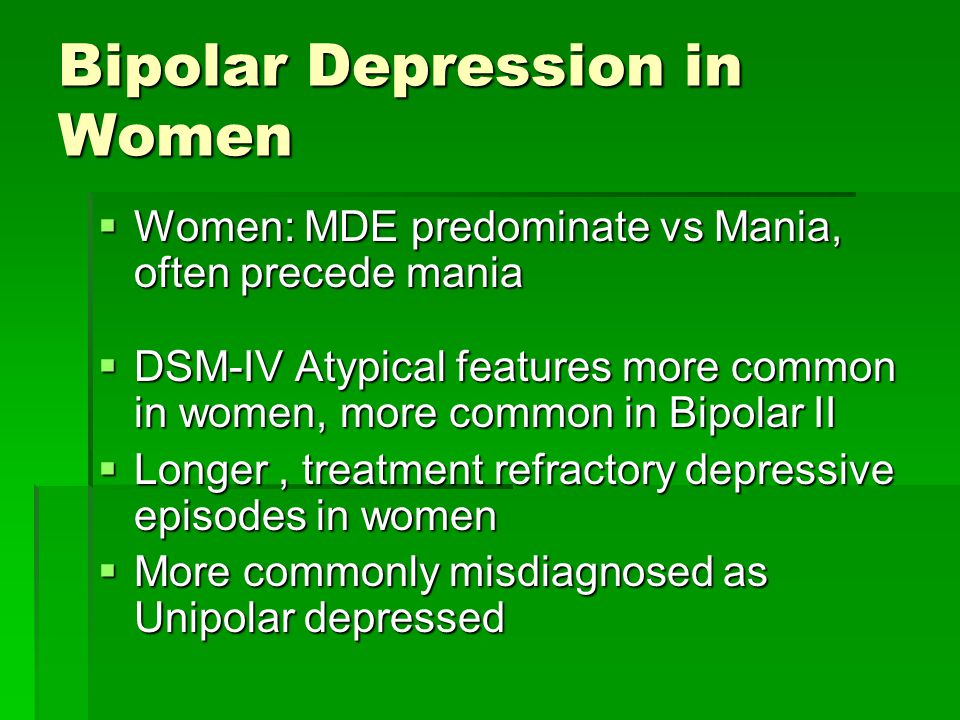 The patient develops convictions in his own greatness, he believes that he is capable of anything, feels that he has a special calling in this world or that he is a descendant of great people. In extended manic episodes of mania with psychotic manifestations, anger, irritability, and direct aggression often occur. This condition leads the patient into extremely unpleasant and sometimes dangerous situations.
The patient develops convictions in his own greatness, he believes that he is capable of anything, feels that he has a special calling in this world or that he is a descendant of great people. In extended manic episodes of mania with psychotic manifestations, anger, irritability, and direct aggression often occur. This condition leads the patient into extremely unpleasant and sometimes dangerous situations.
In addition to the typical symptoms of the disease, there are a large number of comorbid mental disorders. Comorbid mental disorders are those that accompany the underlying disease. The most common disorder of this kind is anxiety, which is manifested, among other things, by nonspecific autonomic symptoms, including sweating, palpitations, tremors of the limbs, various disorders of the gastrointestinal tract, dizziness, headaches, suffocation, and many others. In the case when these symptoms occur suddenly, mainly in public places, they are called panic attacks.
Types of bipolar disorder
Bipolar disorder can be of Ι and ΙΙ types.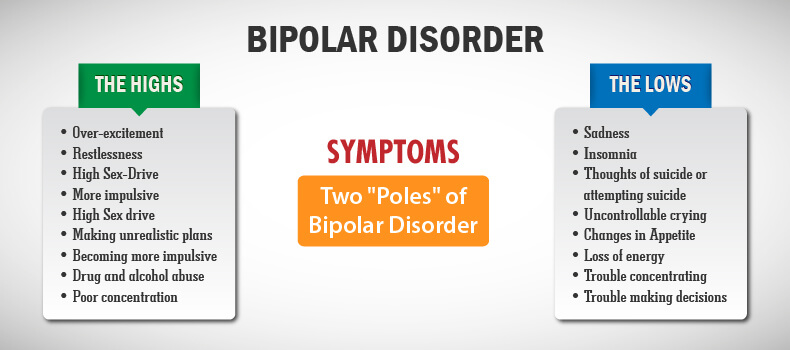
Bipolar I disorder is a condition in which the patient has persistent manias, i.e. overexcitation, enthusiastic inappropriate behavior, manic psychosis, as well as severe depressions. Symptoms of this type are more severe, so hospitalization is indicated in most cases.
Bipolar I disorder is characterized by short periods of hypomania followed by periods of deep depression. Hypomania is a pre-manic state with less active manifestations. Hypomania lasts a very short period of time - from several days to several hours, so sometimes patients do not even notice them and do not inform the doctor about it. Only careful, painstaking work with the patient makes it possible to identify hypomania, make the correct diagnosis and prescribe treatment.
Phases of bipolar disorder
There are several phases of bipolar personality disorder:
- Depressive (unipolar depression). People experience a depressed mood, despair and despondency, complain of a lack of energy and mental concentration, they can either eat too much or too little and sleep.

Depersonalization and derealization may occur at the peak of bipolar depressive disorder. The boundaries of their own "I" and the world around them become blurred, patients experience difficulties in perceiving what is happening. Familiar places seem new, the colors of the surrounding world change, the patient constantly experiences a feeling of "déjà vu". Sounds become muffled, even if someone is talking very close, it seems to the patient that the voice is coming from afar.
- Manic (hypomanic). In this state, patients are full of energy, overly happy or optimistic, euphoric, and have extremely high self-esteem. At first glance, these are positive signs, but when a person experiences large-scale manic episodes, these symptoms and such an emotional state can reach dangerous extremes. A patient in this phase may indiscriminately spend huge amounts of money or behave carelessly, not realizing the full danger. In conversation, people may choke on words, speak at a high speed, or jump from one thought to another.
 These episodes may also be accompanied by delusions of grandeur or the adoption of serious decisions without thinking about the further consequences.
These episodes may also be accompanied by delusions of grandeur or the adoption of serious decisions without thinking about the further consequences.
In the development of the manic phase, the following stages of development can be distinguished:
- Hypomania - increased excitement, emotional upsurge.
- Mania - all signs are more pronounced, aggression, irritability, irascibility and rage are possible.
- Peak phase. The patient constantly experiences nervous excitement, he cannot relax. All his emotions are "heated" to the limit, coordination of movements is disturbed, thoughts are illogical and abrupt, in speech he constantly jumps from one sentence to another.
- Relief of symptoms. The patient gradually calms down. Movement disorders are on the decline. The speed of thinking and increased emotional mood remain unchanged.
- Return to normal.
- Mixed. Sometimes people have complaints that are characteristic of both depression and mania at the same time.
 They may also experience frequent phasing—4 or more episodes in one year.
They may also experience frequent phasing—4 or more episodes in one year.
In the intervals between depressive and manic phases in bipolar disorder, there is a light period during which the general background of mood becomes relatively stable, the person continues to adequately respond to certain events, the emotional sphere is under his control. This is the main criterion for remission of bipolar disease.
Bipolar disorder in women
According to statistics, bipolar Ι disorder occurs with the same frequency in men and women, and type ΙΙ disease is more often diagnosed in women. It is also known that the female course of the disease is characterized by rapid cycles and mixed episodes. Comorbidities often include eating disorders, borderline personality disorder, alcohol or drug addiction, and psychotropic drug abuse. Women are more susceptible to such somatic diseases as migraine (intense headaches), thyroid pathologies, diabetes, and obesity.
For women, a special technique is being developed to alleviate this disorder, since from adolescence to menopause there are specific changes in hormonal levels that must be taken into account.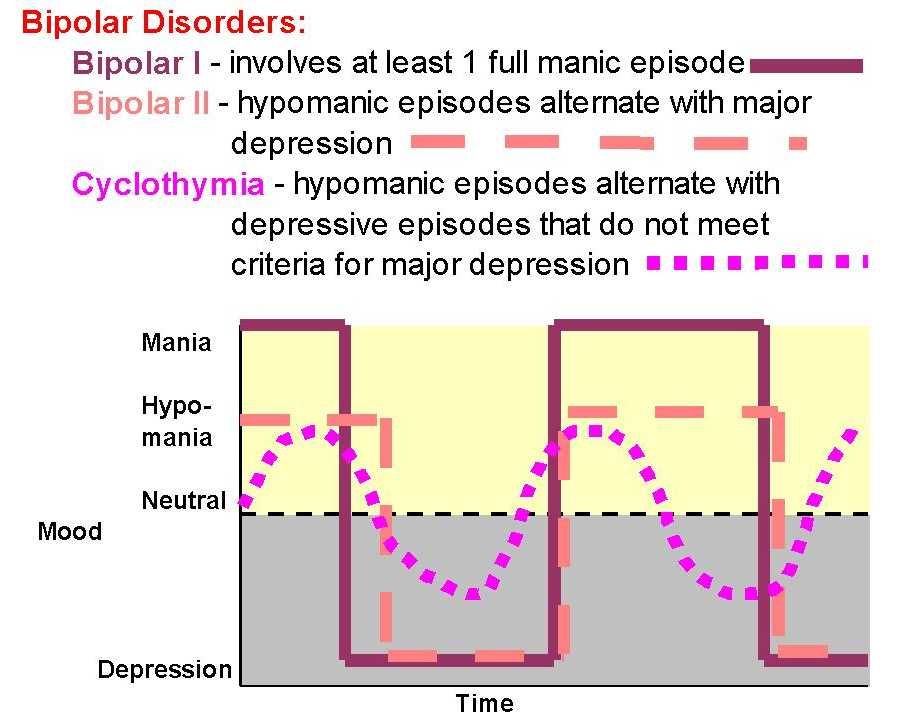 In addition, psychotropic substances, which are supposed to stabilize the condition, can adversely affect the intrauterine development of the fetus if the woman is in position. It is noted that in the first trimester of pregnancy this disorder is milder, but after childbirth they often have to deal with postpartum depression. Thus, at each stage of the development of the female body, a competent doctor must review and adjust the treatment regimen. Often in the treatment of women, a complex method is used that combines drug therapy and cognitive-behavioral or interpersonal therapy with a psychotherapist. This approach gives the fastest results.
In addition, psychotropic substances, which are supposed to stabilize the condition, can adversely affect the intrauterine development of the fetus if the woman is in position. It is noted that in the first trimester of pregnancy this disorder is milder, but after childbirth they often have to deal with postpartum depression. Thus, at each stage of the development of the female body, a competent doctor must review and adjust the treatment regimen. Often in the treatment of women, a complex method is used that combines drug therapy and cognitive-behavioral or interpersonal therapy with a psychotherapist. This approach gives the fastest results.
Treatment for bipolar disorder
Attempts to get rid of bipolar disorder on your own do not bring the desired result and, ultimately, lead to an aggravation of the situation, including the development of drug or alcohol dependence. In the diagnosis of the disease, keeping a mood diary can help, where the patient records all his thoughts, emotions, feelings, changes in mood.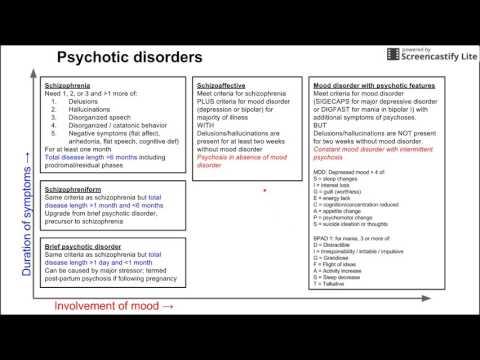 Such records will help the doctor to assess the mental state in detail and make the correct diagnosis. If you suspect bipolar disorder, you should consult a doctor, and the sooner a person realizes that he has a disease and comes to the clinic for help, the sooner professional help will be provided to him and painful symptoms will be replaced by a stable condition. It is impossible to get rid of the disease on your own, since a person cannot fully adequately assess not only his actions, but also the alternation of the phases of the disease.
Such records will help the doctor to assess the mental state in detail and make the correct diagnosis. If you suspect bipolar disorder, you should consult a doctor, and the sooner a person realizes that he has a disease and comes to the clinic for help, the sooner professional help will be provided to him and painful symptoms will be replaced by a stable condition. It is impossible to get rid of the disease on your own, since a person cannot fully adequately assess not only his actions, but also the alternation of the phases of the disease.
Bipolar disorder is one of the few mental disorders in which medication is indicated in 100% of cases, and psychotherapy is an auxiliary tool. This disease is incurable, but its diagnosis and treatment is extremely important. Treatment can reduce the number of episodes, their severity and intensity, as well as prevent negative life events, help prevent relationship breakups, job loss, and even suicidal attempts. Thus, the quality of life of a patient with bipolar disorder who is undergoing treatment will be several times higher than that of a person who neglects treatment.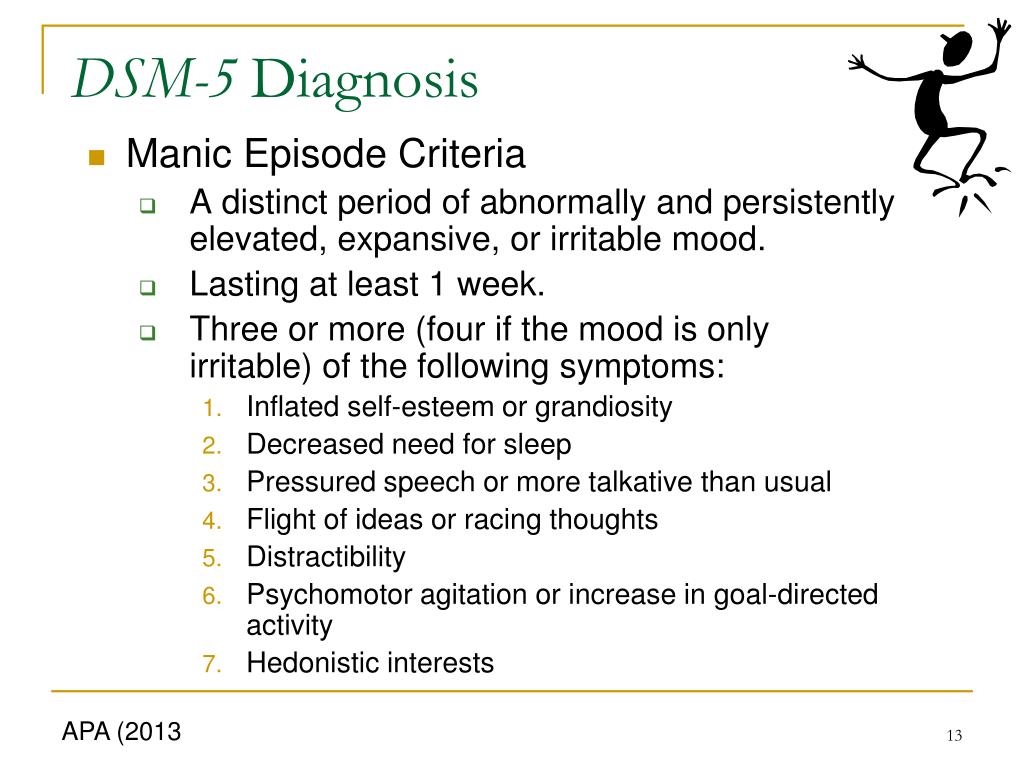 If the patient loses touch with reality and harms himself and others, he is subject to hospitalization, outpatient treatment in this case is not permissible.
If the patient loses touch with reality and harms himself and others, he is subject to hospitalization, outpatient treatment in this case is not permissible.
If you have a disease, it is recommended to exclude coffee, strong tea, alcoholic and energy drinks from your diet in order not to provoke an overexcited state. If possible, you should stop smoking and in no case should you take even soft drugs. It is also very important to establish a sleep pattern, sleep at least 8 hours a day and try to go to bed at about the same time. You should learn to recognize mood swings and notice the early manifestations of new episodes.
If you suspect that you have bipolar personality disorder, there is no need to panic, only a doctor can diagnose the disease, so you need to make an appointment with a psychotherapist with extensive experience in managing such patients at our MedAstrum clinic. If the diagnosis is confirmed, the doctor will make the necessary medication, if necessary, prescribe psychotherapeutic sessions and give recommendations for further lifestyle adjustments.