How to deal with alcoholism and depression
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. SAMHSA’s 2020 National Survey on Drug Use and Health reports that approximately 19.3 million people aged 18 or older had a substance use disorder in the past year.
Alcohol
Data:
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.
 6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- The 2019 National Survey on Drug Use and Health reports that 139.7 million Americans age 12 or older were past month alcohol users, 65.8 million people were binge drinkers in the past month, and 16 million were heavy drinkers in the past month
- About 2.3 million adolescents aged 12 to 17 in 2019 drank alcohol in the past month, and 1.2 million of these adolescents binge drank in that period (2019 NSDUH)
- Approximately 14.5 million people age 12 or older had an alcohol use disorder (2019 NSDUH)
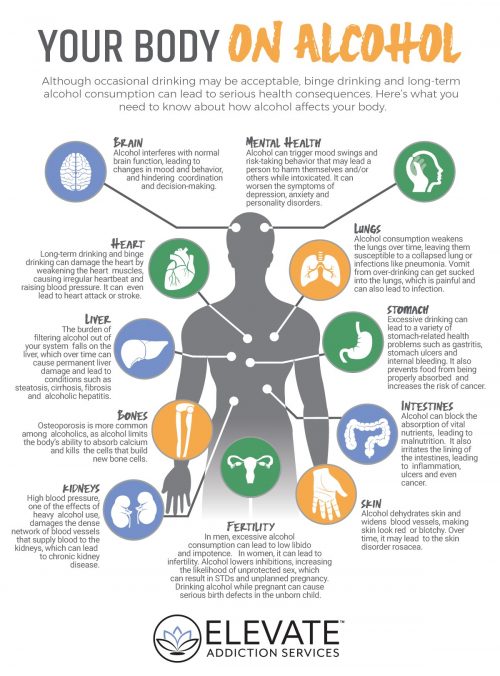
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired.
 The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
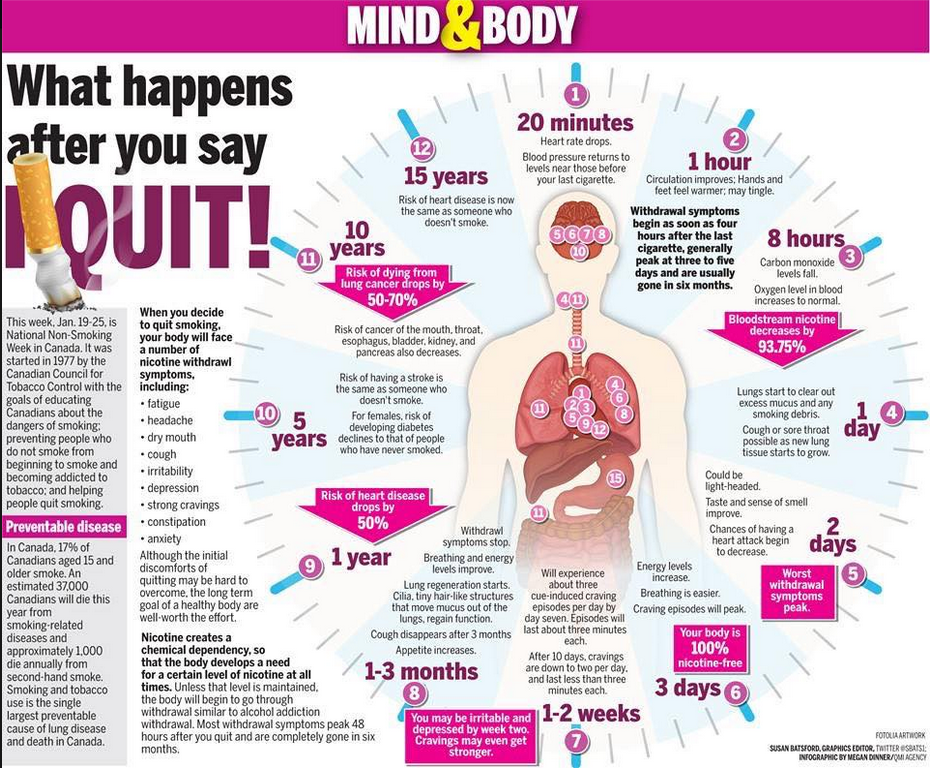
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.
 3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Data from the 2019 NSDUH reports that 58.1 million people were current (i.e., past month) tobacco users. Specifically, 45.9 million people aged 12 or older in 2019 were past month cigarette smokers (2019 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey.
 Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018 - E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year.
 Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH) - An estimated 745,000 people had used heroin in the past year, based on 2019 NSDUH data
- In 2019, there were 10.1 million people age 12 or older who misused opioids in the past year. The vast majority of people misused prescription pain relievers (2019 NSDUH)
- An estimated 1.6 million people aged 12 or older had an opioid use disorder based on 2019 NSDUH data
- Opioid use, specifically injection drug use, is a risk factor for contracting HIV, Hepatitis B, and Hepatitis C. The CDC reports that people who inject drugs accounted for 9 percent of HIV diagnoses in the United States in 2016
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.
 5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH) - 2019 NSDUH data indicates that 48.2 million Americans aged 12 or older, 17.5 percent of the population, used marijuana in the past year
- Approximately 4.8 million people aged 12 or older in 2019 had a marijuana use disorder in the past year (2019 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 04/27/2022
Alcoholic depression - symptoms, causes, diagnosis and treatment of alcoholic depression
Article reviewed by an expert:
MAKE AN APPOINTMENT
Alcoholic depression is an affective disorder that occurs in people suffering from alcoholism. Usually lasts from 2 weeks to 1 month. The maximum severity of symptoms is usually observed during the development of withdrawal symptoms. This condition often occurs after an exit from alcoholic psychosis, it can also develop during periods of binges and remissions. It is accompanied by a decrease in mood, longing, a feeling of guilt, uselessness and uselessness. Suicidal thoughts and actions are possible. The diagnosis is exposed on the basis of the anamnesis and clinical manifestations. Treatment is drug therapy combined with psychotherapy.
It is accompanied by a decrease in mood, longing, a feeling of guilt, uselessness and uselessness. Suicidal thoughts and actions are possible. The diagnosis is exposed on the basis of the anamnesis and clinical manifestations. Treatment is drug therapy combined with psychotherapy.
Alcoholic depression - what is it?
Depression in alcoholism was described by Bleuler in 1920 under the name "alcoholic melancholia". Subsequent studies have confirmed both the presence of specific depressive and subdepressive conditions in alcoholics, and the complex, diverse links between alcoholism and depressive disorders. The frequency of development of the disease and the severity of symptoms directly correlates with the duration and severity of alcoholism. Middle-aged and elderly patients suffer from a depressive disorder more often than younger ones. Most of the patients are people over 40 years of age.
The average duration of post-alcoholic depression in alcoholism ranges from 2 weeks to 1 month. In severe cases, symptoms may persist for a year or more. The duration of the disease depends on the psycho-emotional characteristics, character traits, features of the constitution and the state of the body of patients. Women suffer more often than men, but in men, depression is more severe and is more often complicated by suicide attempts. The aggravation of male depression is facilitated by the fact that the representatives of the stronger sex rarely seek medical help during the development of the disease. Treatment of depression in alcoholism is carried out by specialists in the field of narcology, psychotherapy and psychiatry.
In severe cases, symptoms may persist for a year or more. The duration of the disease depends on the psycho-emotional characteristics, character traits, features of the constitution and the state of the body of patients. Women suffer more often than men, but in men, depression is more severe and is more often complicated by suicide attempts. The aggravation of male depression is facilitated by the fact that the representatives of the stronger sex rarely seek medical help during the development of the disease. Treatment of depression in alcoholism is carried out by specialists in the field of narcology, psychotherapy and psychiatry.
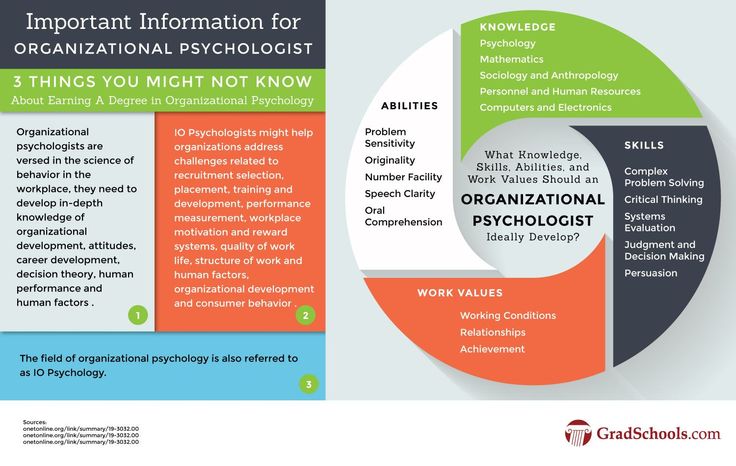
Causes of alcohol depression
Depression in alcoholism is a multifactorial disease. A whole range of circumstances leads to its development, including changes in general metabolism, disruption of brain receptors, personality changes, characteristic mental and somatic disorders, uncontrolled craving for alcohol, withdrawal phenomena when drinking alcohol is stopped, social and domestic problems. Narcologists constantly have to deal with alcoholic depression that develops in various clinical situations.
Narcologists constantly have to deal with alcoholic depression that develops in various clinical situations.
Alcoholic depression is part of the symptom complex of deprivation syndrome, acute alcohol intoxication, binge drinking and uncontrolled craving for alcohol. The most common cause of depressive mental disorder in alcoholics is withdrawal symptoms. Mental suffering of patients is provoked by severe physical and psychological discomfort and social problems, combined with a pathological need for alcohol.
Several bouts of depression occur in patients undergoing treatment for alcoholism in specialized clinics. In the initial stages of therapy, such patients develop a "sobriety phobia" - a pronounced fear of the possibility of life without alcohol. This stage is accompanied by a kind of mourning, due to the loss of alcohol. The second wave of depression is usually observed before the discharge of patients from the hospital, at the stage when the person no longer suffers from the consequences of intoxication. Longing for alcohol and psychological problems come to the fore.
Longing for alcohol and psychological problems come to the fore.
Sometimes depressive disorders develop against the background of remission, when a person feels lost, unable to fit in, “fallen out” of the normal rhythm of life and social environment, suffering from changes in habitual patterns of behavior, forced to solve numerous problems that arose during the period of alcoholism, without having enough external support and internal reserves. Such depressions can cause a breakdown and further alcoholization of the patient.
It should be borne in mind that the premorbid background is of some importance in the development of alcoholism. Even before the start of alcohol consumption, many patients have an increased tendency to mood swings, the development of asthenic conditions, depressive neurosis, subdepression and all kinds of borderline disorders. As alcoholism develops, this tendency is aggravated and aggravated due to secondary psycho-emotional and personality changes. There are also complications and neurosis after a complete rejection of alcohol.
There are also complications and neurosis after a complete rejection of alcohol.
Symptoms and differential diagnosis of alcohol depression
Symptoms of depression in alcoholism are usually mild. Severe affective disorders are relatively rare. The mood is constantly depressed, the patient suffers from a feeling of emptiness and meaninglessness of existence. There is a feeling of loss of colors, the emotional colorlessness of the world, characteristic of depressive disorders. This perception causes depression and anxiety. Anhedonia develops - a person loses the ability to rejoice, cannot enjoy.
Psychological changes are combined with motor and intellectual retardation. Gait and movements slow down, the voice becomes quiet, monotonous. Mimic diversity disappears, the patient's face almost constantly retains a sad expression. The patient is in a state of inactivity for a significant part of the time, responds to questions with a delay, has difficulty trying to understand someone else's thought or instruction. It is difficult for him to think and formulate statements.
It is difficult for him to think and formulate statements.
Hallucinations and delusions are usually absent. Often there are overvalued ideas of one's own guilt, uselessness, uselessness, fatal inadequacy and inadequacy. There is a tendency to self-abasement and self-accusation. The future looks bleak, hopeless, unpromising. Some patients consider some of their own previous actions as a serious crime. Many patients have thoughts of suicide, suicide attempts are possible. Sometimes (mainly in older patients) alcoholic depression is combined with increased anxiety.
Alcoholic depression is differentiated from other depressive disorders and conditions that include individual symptoms of depression. Unlike a depressive disorder, "drunken grief" is not accompanied by a sense of the colorlessness of the world and the loss of the ability to feel a variety of emotions. This state arises on an "emotional wave" and passes within a few hours, occasionally - several days.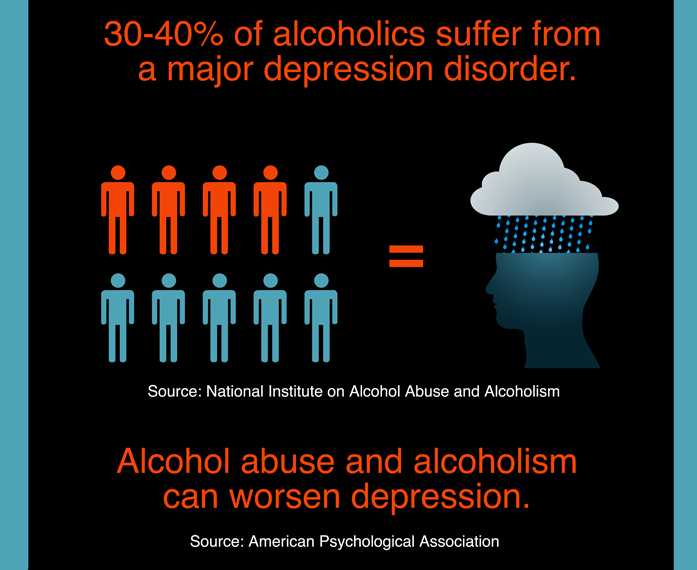
Separate elements of depression are often observed in withdrawal syndrome, but, unlike real alcoholic depression, they disappear after abstinence from drinking alcohol for 1-3 days. Reactive depression on the background of alcoholism in patients develops against the background of severe traumatic events (death of a relative, divorce, etc.); with alcoholic depression, there are no such events in the recent past of patients. Alcohol intake can provoke an exacerbation of other mental illnesses (psychogenic depression, depressive phase of bipolar affective disorder), therefore, when affective symptoms appear in patients with alcoholism, a thorough history taking is necessary.
Treatment and prognosis for alcoholic depression
Treatment of depression in alcoholism is carried out in a narcological hospital. In the process of treatment, drugs, psychotherapy and non-drug methods are used. Patients are prescribed antidepressants for alcoholism (usually SSRIs, tricyclic antidepressants, or MAO inhibitors).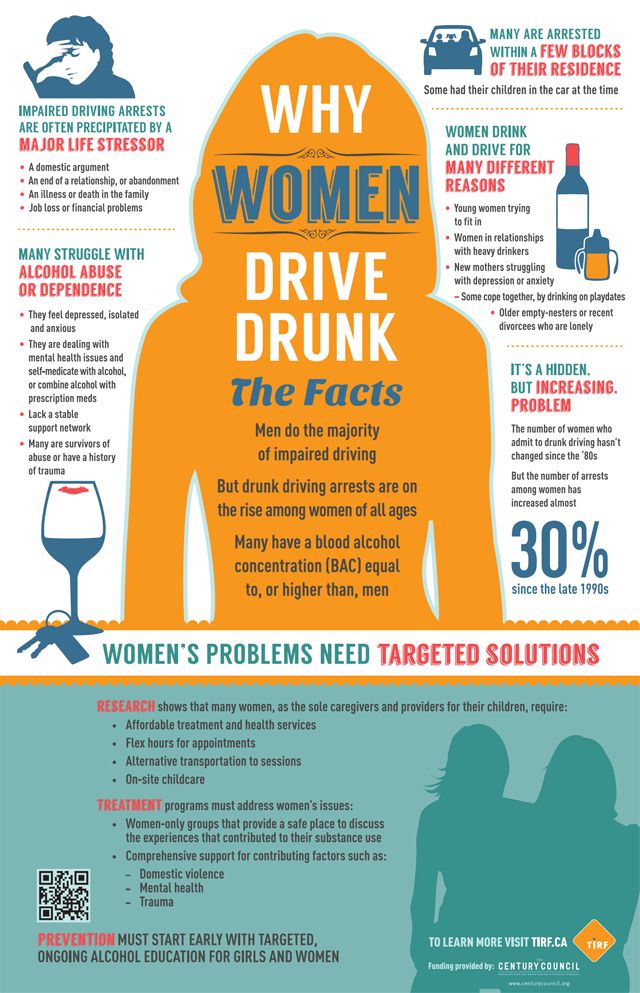 With increased anxiety and sleep disorders, short-term courses of drug therapy and treatment with the use of hypnotics and tranquilizers (diazepam, phenazepam, tazepam, etc.) are carried out. In parallel, they carry out detoxification therapy and provide psychological assistance.
With increased anxiety and sleep disorders, short-term courses of drug therapy and treatment with the use of hypnotics and tranquilizers (diazepam, phenazepam, tazepam, etc.) are carried out. In parallel, they carry out detoxification therapy and provide psychological assistance.
With early detection and timely hospitalization, the prognosis for alcoholic depression in most cases is relatively favorable. Single depressive episodes, as a rule, quickly stop, suicidal intentions disappear, working capacity is restored (if it was not impaired due to other diseases). However, if the patient continues to drink alcohol, these conditions may recur and worsen as alcoholism develops.
is there a way out of the vicious circle? For some, this condition passes quickly, for others it develops into a real illness - depression. In such cases, of course, the help of a specialist is needed, but most people still try to solve the problem on their own, which often only leads to the development of the disease.
Alcohol as a remedy for depression
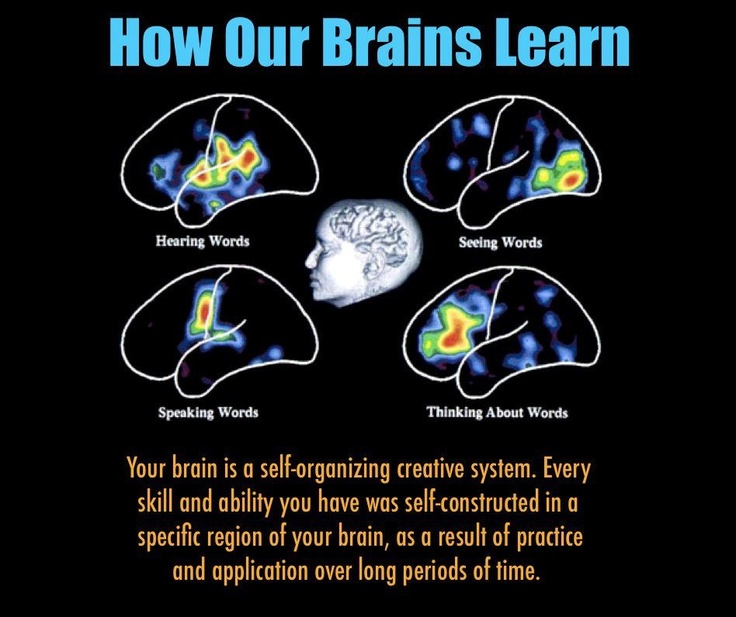
One of the unacceptable treatments for depression is the use of alcohol. Under the influence of alcohol, people forget about all the problems, feel more confident, look at life with different eyes. But it must be remembered that the effect of alcohol ends sooner or later, and the feeling of despair after that only intensifies. In addition, alcohol negatively affects the nervous system, thereby exacerbating depression.
As a rule, if you do not control the dose of alcohol you drink, the “treatment” with alcohol will not be limited to one drink. Suffering once again from a hangover syndrome, complaining of weakness, malaise, headache, a depressed person tries to draw attention to himself, arouse pity and sympathy from the people around him. Not receiving, as it seems to him, due attention, he will again flood his suffering from misunderstanding with alcohol. Thus, a vicious circle is obtained, a way out of which can only be found by a specialist, that is, a psychologist.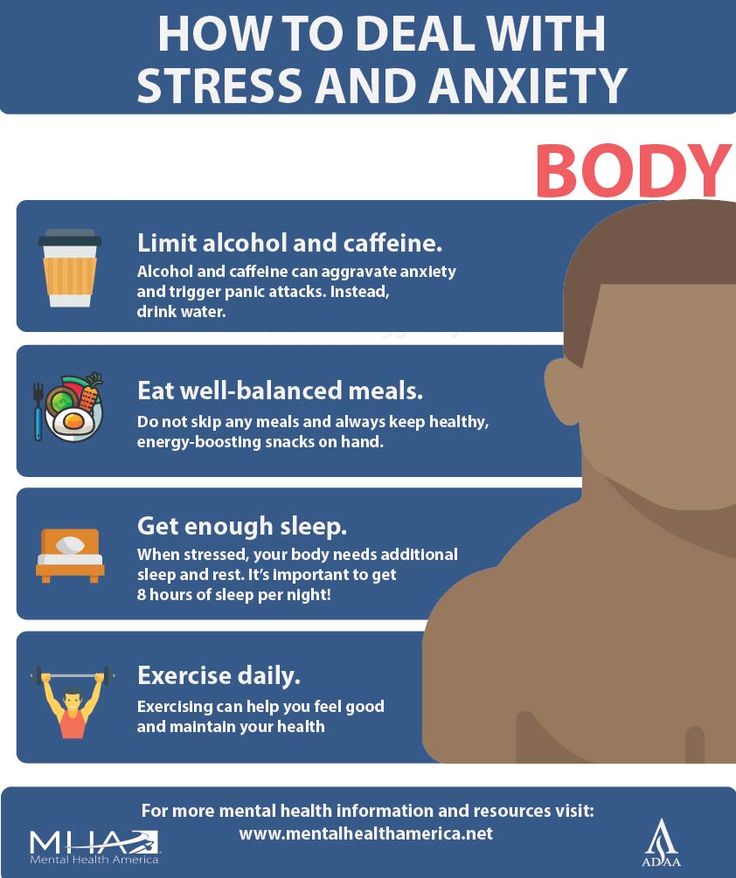
In some cases, alcohol during depression can lead to tragic consequences. A drunken "sea is knee-deep", therefore a person who has had suicidal thoughts more than once in his head is capable of committing suicide while intoxicated.
Alcohol as a cause of depression
But is there an inverse relationship between alcohol and depression? Yes, alcohol also affects the occurrence of depression, as depression affects the development of alcoholism treatment. It is known that alcohol changes the chemical composition of the brain, and this contributes to the onset of depression. It is also known that people who regularly take high-grade drinks often have conflicts in the family and at work, memory deteriorates, problems appear in their sexual life, and all this is accompanied by stress, which in turn leads to depression.
It must be remembered that alcohol is not a solution. By encouraging yourself with alcoholic beverages, you not only run the risk of becoming addicted to alcohol, but also completely losing your taste for life.
There are many causes of depression: bad weather, problems at work or in your personal life, dissatisfaction with your figure, lack of creativity, etc.
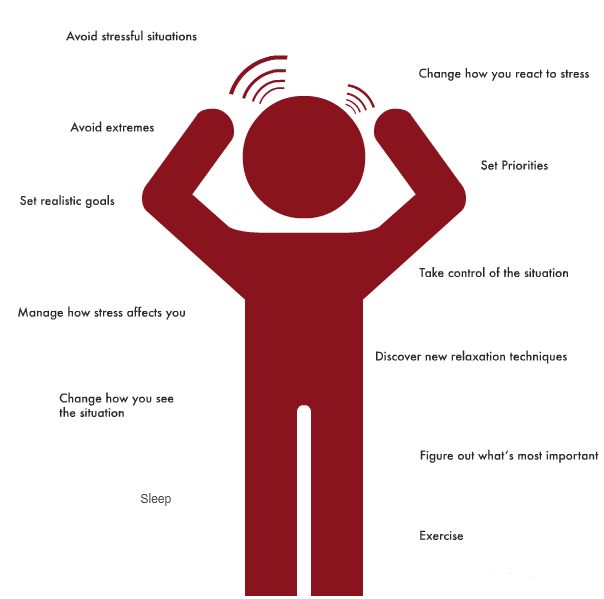
It is best to prevent depression at the very beginning of its inception. First you need to believe that you control your emotions, not they control you.
Recipes for depression
How can you keep your spirits high and not become discouraged? Here are some recipes for depression:
- Good lighting. Most often, depression catches us in the fall or winter. This is not at all strange: it is at these times of the year that we experience a lack of sunlight, which affects the mood. So do not save on light, try to make it brighter at work and at home.
- Meeting with friends. A good company has never bothered anyone, the main thing is that it should be cheerful and be able to distract you from negative thoughts, setting you on a positive one. In the circle of close people you will not be sad and lonely.
- Favorite occupation. Each of us has a favorite pastime: some like to draw, others like to read, others prefer to watch movies. Your main task is to escape from boredom and monotony. Therefore, feel free to pick up a pencil, your favorite book or sit down to watch your favorite movie. Just remember one thing - the movie or book must be fun (horror, dramas and thrillers are cancelled).
- Change of scenery. It's never too late to try something new: rearrange your home or start a renovation. Believe me, even minor changes can help you look at life with different eyes. This applies to new activities, and even to a change in daily routine.
- Physical activity. Go in for sports or just try to move more, even ordinary walking will do. As you know, small physical activity contributes to raising the mood and improving the figure.
- Gift for yourself. Give yourself a nice gift, like treating yourself to your favorite food or shopping for clothes.
- Another attitude to life.
 Try to look at life from the other side: take some things with humor, try to find something good in every situation, do not be vindictive and vindictive, do not envy, believe in yourself and remember that you are worthy of happiness.
Try to look at life from the other side: take some things with humor, try to find something good in every situation, do not be vindictive and vindictive, do not envy, believe in yourself and remember that you are worthy of happiness.
There are so many interesting things in life that it is just a shame to waste it on despondency and sadness. Therefore, find joy in the little things more often, and do not forget that your happiness is in your hands.
The editors would like to thank the specialists of the medical center "AlcoMed" for their help in preparing the material.
References
- Ng SY., Soh BS., Rodriguez-Muela N., Hendrickson DG., Price F., Rinn JL., Rubin LL. Genome-wide RNA-Seq of Human Motor Neurons Implicates Selective ER Stress Activation in Spinal Muscular Atrophy. // Cell Stem Cell - 2015 - Vol17 - N5 - p.569-84; PMID:26321202
- Wang L., Wei F., Liu S., Wan Y., Chen N., Cui S., Zhong R., Huang Y. Can Modified Kurokawa's Double-Door Laminoplasty Reduce the Incidence of Axial Symptoms at Long-term Follow -up?: A Prospective Study of 152 Patients With Cervical Spondylotic Myelopathy.