How to cure mental illness
Mental illness - Diagnosis and treatment
Diagnosis
To determine a diagnosis and check for related complications, you may have:
- A physical exam. Your doctor will try to rule out physical problems that could cause your symptoms.
- Lab tests. These may include, for example, a check of your thyroid function or a screening for alcohol and drugs.
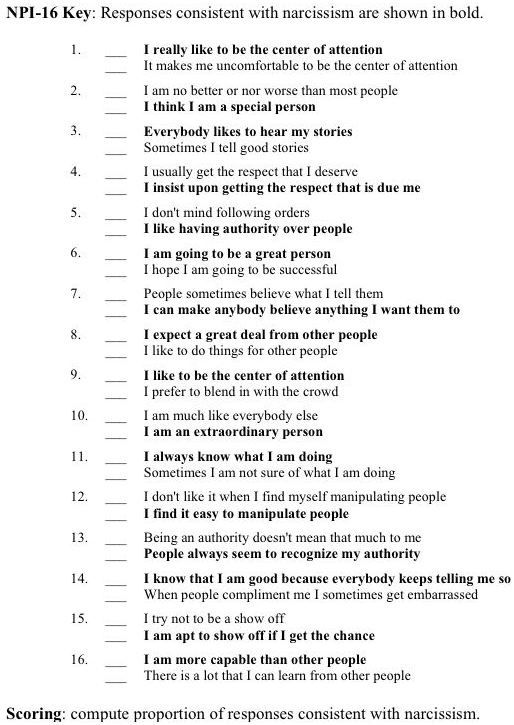
- A psychological evaluation. A doctor or mental health professional talks to you about your symptoms, thoughts, feelings and behavior patterns. You may be asked to fill out a questionnaire to help answer these questions.
Determining which mental illness you have
Sometimes it's difficult to find out which mental illness may be causing your symptoms. But taking the time and effort to get an accurate diagnosis will help determine the appropriate treatment. The more information you have, the more you will be prepared to work with your mental health professional in understanding what your symptoms may represent.
The defining symptoms for each mental illness are detailed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association. This manual is used by mental health professionals to diagnose mental conditions and by insurance companies to reimburse for treatment.
Classes of mental illness
The main classes of mental illness are:
- Neurodevelopmental disorders. This class covers a wide range of problems that usually begin in infancy or childhood, often before the child begins grade school. Examples include autism spectrum disorder, attention-deficit/hyperactivity disorder (ADHD) and learning disorders.
- Schizophrenia spectrum and other psychotic disorders. Psychotic disorders cause detachment from reality — such as delusions, hallucinations, and disorganized thinking and speech. The most notable example is schizophrenia, although other classes of disorders can be associated with detachment from reality at times.
- Bipolar and related disorders. This class includes disorders with alternating episodes of mania — periods of excessive activity, energy and excitement — and depression.
- Depressive disorders. These include disorders that affect how you feel emotionally, such as the level of sadness and happiness, and they can disrupt your ability to function. Examples include major depressive disorder and premenstrual dysphoric disorder.
- Anxiety disorders. Anxiety is an emotion characterized by the anticipation of future danger or misfortune, along with excessive worrying. It can include behavior aimed at avoiding situations that cause anxiety. This class includes generalized anxiety disorder, panic disorder and phobias.
- Obsessive-compulsive and related disorders. These disorders involve preoccupations or obsessions and repetitive thoughts and actions. Examples include obsessive-compulsive disorder, hoarding disorder and hair-pulling disorder (trichotillomania).
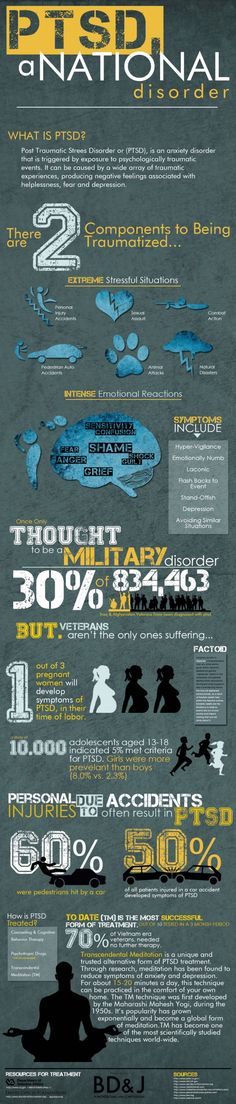
- Trauma- and stressor-related disorders. These are adjustment disorders in which a person has trouble coping during or after a stressful life event. Examples include post-traumatic stress disorder (PTSD) and acute stress disorder.
- Dissociative disorders. These are disorders in which your sense of self is disrupted, such as with dissociative identity disorder and dissociative amnesia.
- Somatic symptom and related disorders. A person with one of these disorders may have physical symptoms that cause major emotional distress and problems functioning. There may or may not be another diagnosed medical condition associated with these symptoms, but the reaction to the symptoms is not normal. The disorders include somatic symptom disorder, illness anxiety disorder and factitious disorder.
- Feeding and eating disorders. These disorders include disturbances related to eating that impact nutrition and health, such as anorexia nervosa and binge-eating disorder.
- Elimination disorders. These disorders relate to the inappropriate elimination of urine or stool by accident or on purpose. Bed-wetting (enuresis) is an example.
- Sleep-wake disorders. These are disorders of sleep severe enough to require clinical attention, such as insomnia, sleep apnea and restless legs syndrome.
- Sexual dysfunctions. These include disorders of sexual response, such as premature ejaculation and female orgasmic disorder.
- Gender dysphoria. This refers to the distress that accompanies a person's stated desire to be another gender.
- Disruptive, impulse-control and conduct disorders. These disorders include problems with emotional and behavioral self-control, such as kleptomania or intermittent explosive disorder.
- Substance-related and addictive disorders. These include problems associated with the excessive use of alcohol, caffeine, tobacco and drugs.
 This class also includes gambling disorder.
This class also includes gambling disorder. - Neurocognitive disorders. Neurocognitive disorders affect your ability to think and reason. These acquired (rather than developmental) cognitive problems include delirium, as well as neurocognitive disorders due to conditions or diseases such as traumatic brain injury or Alzheimer's disease.
- Personality disorders. A personality disorder involves a lasting pattern of emotional instability and unhealthy behavior that causes problems in your life and relationships. Examples include borderline, antisocial and narcissistic personality disorders.
- Paraphilic disorders. These disorders include sexual interest that causes personal distress or impairment or causes potential or actual harm to another person. Examples are sexual sadism disorder, voyeuristic disorder and pedophilic disorder.
- Other mental disorders. This class includes mental disorders that are due to other medical conditions or that don't meet the full criteria for one of the above disorders.

Treatment
Your treatment depends on the type of mental illness you have, its severity and what works best for you. In many cases, a combination of treatments works best.
If you have a mild mental illness with well-controlled symptoms, treatment from your primary care provider may be sufficient. However, often a team approach is appropriate to make sure all your psychiatric, medical and social needs are met. This is especially important for severe mental illnesses, such as schizophrenia.
Your treatment team
Your treatment team may include your:
- Family or primary care doctor
- Nurse practitioner
- Physician assistant
- Psychiatrist, a medical doctor who diagnoses and treats mental illnesses
- Psychotherapist, such as a psychologist or a licensed counselor
- Pharmacist
- Social worker
- Family members
Medications
Although psychiatric medications don't cure mental illness, they can often significantly improve symptoms. Psychiatric medications can also help make other treatments, such as psychotherapy, more effective. The best medications for you will depend on your particular situation and how your body responds to the medication.
Psychiatric medications can also help make other treatments, such as psychotherapy, more effective. The best medications for you will depend on your particular situation and how your body responds to the medication.
Some of the most commonly used classes of prescription psychiatric medications include:
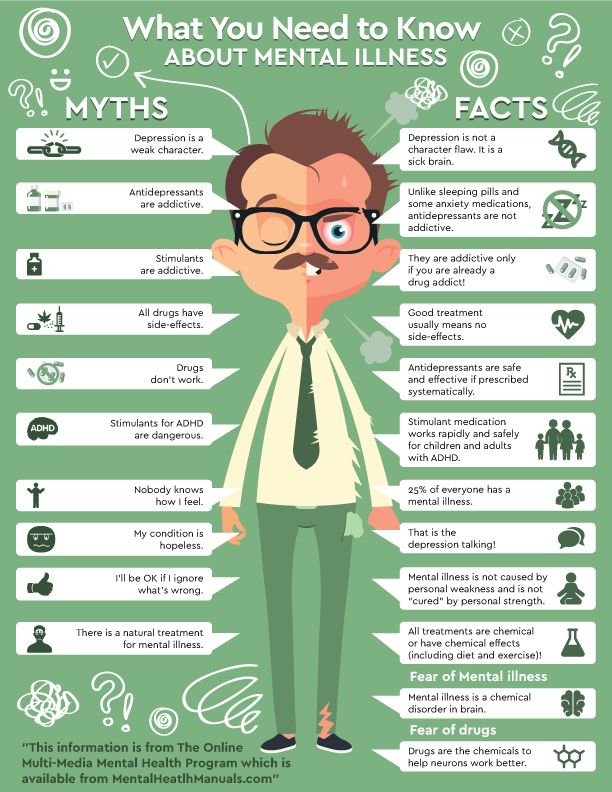
- Antidepressants. Antidepressants are used to treat depression, anxiety and sometimes other conditions. They can help improve symptoms such as sadness, hopelessness, lack of energy, difficulty concentrating and lack of interest in activities. Antidepressants are not addictive and do not cause dependency.
- Anti-anxiety medications. These drugs are used to treat anxiety disorders, such as generalized anxiety disorder or panic disorder. They may also help reduce agitation and insomnia. Long-term anti-anxiety drugs typically are antidepressants that also work for anxiety. Fast-acting anti-anxiety drugs help with short-term relief, but they also have the potential to cause dependency, so ideally they'd be used short term.
- Mood-stabilizing medications. Mood stabilizers are most commonly used to treat bipolar disorders, which involves alternating episodes of mania and depression. Sometimes mood stabilizers are used with antidepressants to treat depression.
- Antipsychotic medications. Antipsychotic drugs are typically used to treat psychotic disorders, such as schizophrenia. Antipsychotic medications may also be used to treat bipolar disorders or used with antidepressants to treat depression.
Psychotherapy
Psychotherapy, also called talk therapy, involves talking about your condition and related issues with a mental health professional. During psychotherapy, you learn about your condition and your moods, feelings, thoughts and behavior. With the insights and knowledge you gain, you can learn coping and stress management skills.
There are many types of psychotherapy, each with its own approach to improving your mental well-being. Psychotherapy often can be successfully completed in a few months, but in some cases, long-term treatment may be needed. It can take place one-on-one, in a group or with family members.
Psychotherapy often can be successfully completed in a few months, but in some cases, long-term treatment may be needed. It can take place one-on-one, in a group or with family members.
When choosing a therapist, you should feel comfortable and be confident that he or she is capable of listening and hearing what you have to say. Also, it's important that your therapist understands the life journey that has helped shape who you are and how you live in the world.
Brain-stimulation treatments
Brain-stimulation treatments are sometimes used for depression and other mental health disorders. They're generally reserved for situations in which medications and psychotherapy haven't worked. They include electroconvulsive therapy, repetitive transcranial magnetic stimulation, deep brain stimulation and vagus nerve stimulation.
Make sure you understand all the risks and benefits of any recommended treatment.
Hospital and residential treatment programs
Sometimes mental illness becomes so severe that you need care in a psychiatric hospital.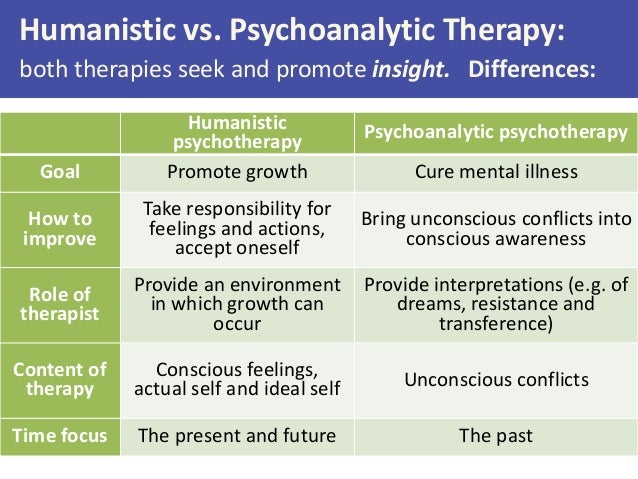 This is generally recommended when you can't care for yourself properly or when you're in immediate danger of harming yourself or someone else.
This is generally recommended when you can't care for yourself properly or when you're in immediate danger of harming yourself or someone else.
Options include 24-hour inpatient care, partial or day hospitalization, or residential treatment, which offers a temporary supportive place to live. Another option may be intensive outpatient treatment.
Substance misuse treatment
Problems with substance use commonly occur along with mental illness. Often it interferes with treatment and worsens mental illness. If you can't stop using drugs or alcohol on your own, you need treatment. Talk to your doctor about treatment options.
Participating in your own care
Working together, you and your primary care provider or mental health professional can decide which treatment may be best, depending on your symptoms and their severity, your personal preferences, medication side effects, and other factors. In some cases, a mental illness may be so severe that a doctor or loved one may need to guide your care until you're well enough to participate in decision-making.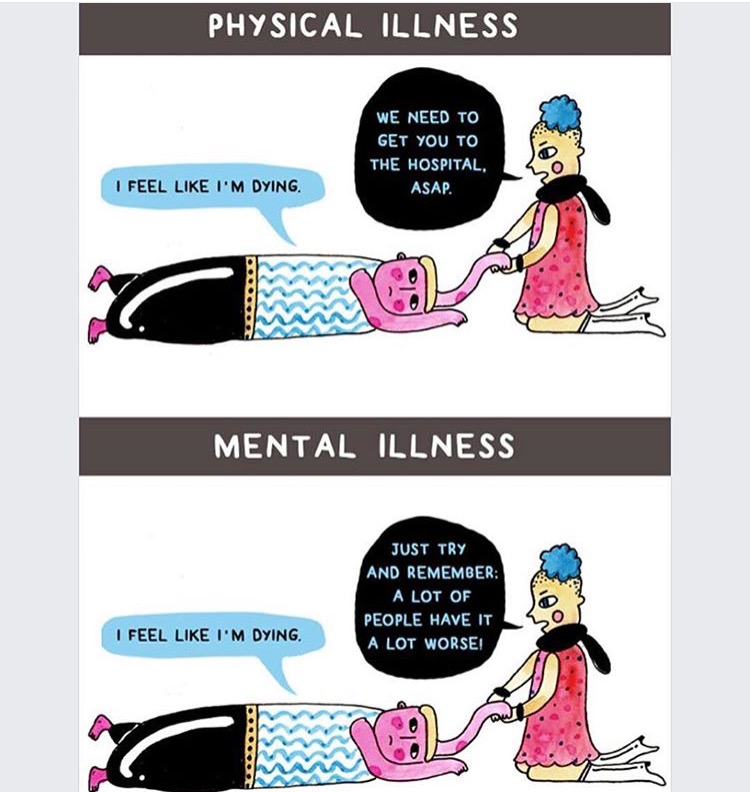
More Information
- Mental health providers: Tips on finding one
- Deep brain stimulation
- Electroconvulsive therapy (ECT)
- Psychotherapy
- Transcranial magnetic stimulation
- Vagus nerve stimulation
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
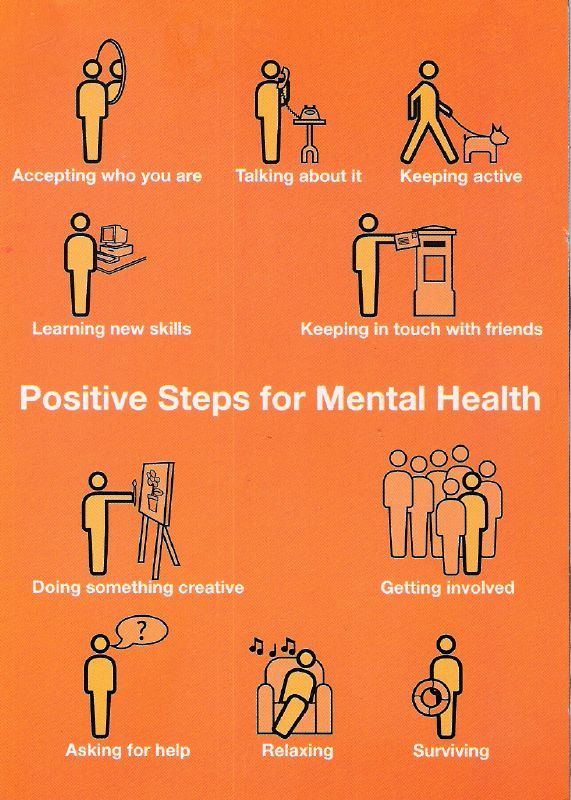
Lifestyle and home remedies
In most cases, a mental illness won't get better if you try to treat it on your own without professional care. But you can do some things for yourself that will build on your treatment plan:
- Stick to your treatment plan. Don't skip therapy sessions. Even if you're feeling better, don't skip your medications. If you stop, symptoms may come back. And you could have withdrawal-like symptoms if you stop a medication too suddenly. If you have bothersome drug side effects or other problems with treatment, talk to your doctor before making changes.
- Avoid alcohol and drug use. Using alcohol or recreational drugs can make it difficult to treat a mental illness. If you're addicted, quitting can be a real challenge. If you can't quit on your own, see your doctor or find a support group to help you.
- Stay active. Exercise can help you manage symptoms of depression, stress and anxiety. Physical activity can also counteract the effects of some psychiatric medications that may cause weight gain. Consider walking, swimming, gardening or any form of physical activity that you enjoy. Even light physical activity can make a difference.
- Make healthy choices. Maintaining a regular schedule that includes sufficient sleep, healthy eating and regular physical activity are important to your mental health.
- Don't make important decisions when your symptoms are severe. Avoid decision-making when you're in the depth of mental illness symptoms, since you may not be thinking clearly.
- Determine priorities. You may reduce the impact of your mental illness by managing time and energy. Cut back on obligations when necessary and set reasonable goals. Give yourself permission to do less when symptoms are worse.
 You may find it helpful to make a list of daily tasks or use a planner to structure your time and stay organized.
You may find it helpful to make a list of daily tasks or use a planner to structure your time and stay organized. - Learn to adopt a positive attitude. Focusing on the positive things in your life can make your life better and may even improve your health. Try to accept changes when they occur, and keep problems in perspective. Stress management techniques, including relaxation methods, may help.
Coping and support
Coping with a mental illness is challenging. Talk to your doctor or therapist about improving your coping skills, and consider these tips:
- Learn about your mental illness. Your doctor or therapist can provide you with information or may recommend classes, books or websites. Include your family, too — this can help the people who care about you understand what you're going through and learn how they can help.
- Join a support group. Connecting with others facing similar challenges may help you cope.
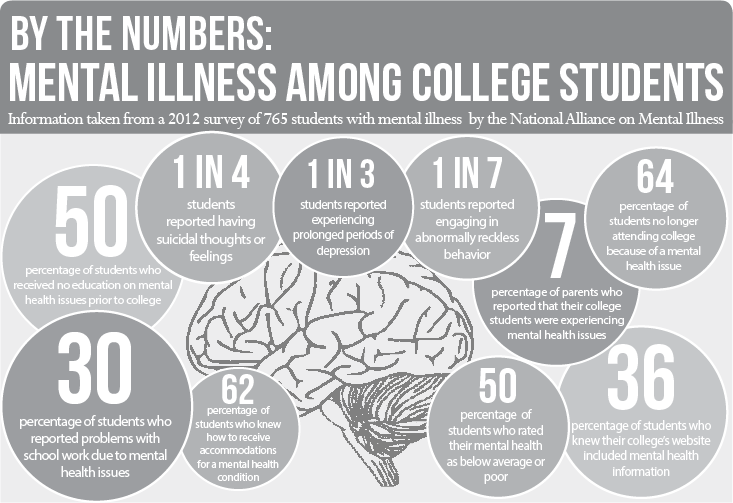
 Support groups for mental illness are available in many communities and online. One good place to start is the National Alliance on Mental Illness.
Support groups for mental illness are available in many communities and online. One good place to start is the National Alliance on Mental Illness. - Stay connected with friends and family. Try to participate in social activities, and get together with family or friends regularly. Ask for help when you need it, and be upfront with your loved ones about how you're doing.
- Keep a journal. Or jot down brief thoughts or record symptoms on a smartphone app. Keeping track of your personal life and sharing information with your therapist can help you identify what triggers or improves your symptoms. It's also a healthy way to explore and express pain, anger, fear and other emotions.
Preparing for your appointment
Whether you schedule an appointment with your primary care provider to talk about mental health concerns or you're referred to a mental health professional, such as a psychiatrist or psychologist, take steps to prepare for your appointment.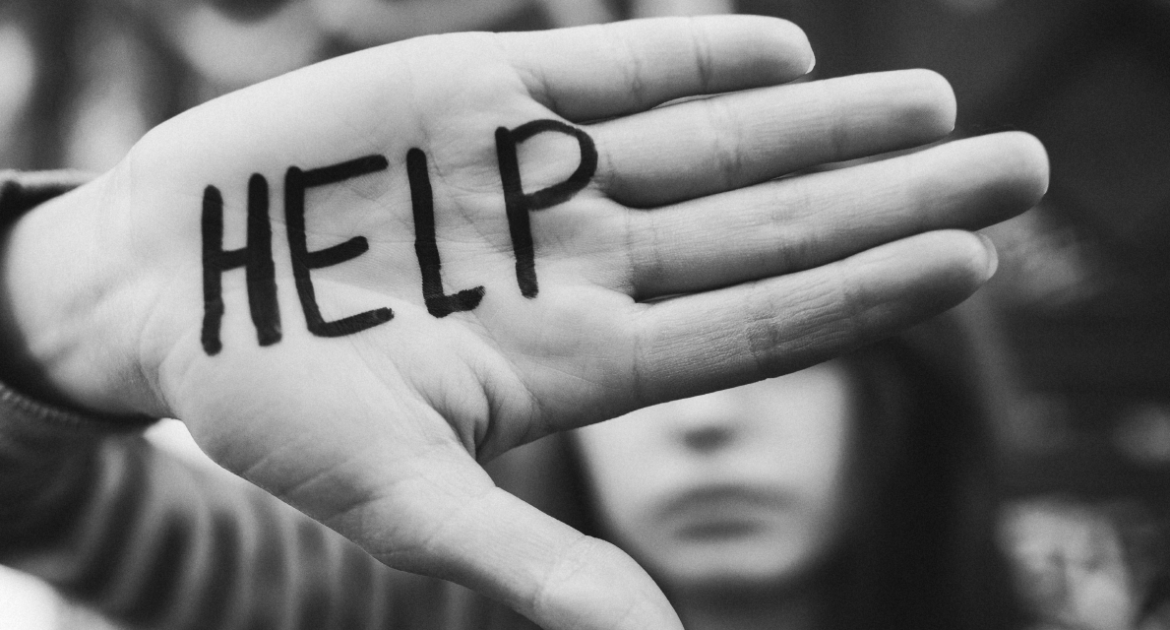
If possible, take a family member or friend along. Someone who has known you for a long time may be able to share important information, with your permission.
What you can do
Before your appointment, make a list of:
- Any symptoms you or people close to you have noticed, and for how long
- Key personal information, including traumatic events in your past and any current, major stressors
- Your medical information, including other physical or mental health conditions
- Any medications, vitamins, herbal products or other supplements you take, and their dosages
- Questions to ask your doctor or mental health professional
Questions to ask may include:
- What type of mental illness might I have?
- Why can't I get over mental illness on my own?
- How do you treat my type of mental illness?
- Will talk therapy help?
- Are there medications that might help?
- How long will treatment take?
- What can I do to help myself?
- Do you have any brochures or other printed material that I can have?
- What websites do you recommend?
Don't hesitate to ask any other questions during your appointment.
What to expect from your doctor
During your appointment, your doctor or mental health professional is likely to ask you questions about your mood, thoughts and behavior, such as:
- When did you first notice symptoms?
- How is your daily life affected by your symptoms?
- What treatment, if any, have you had for mental illness?
- What have you tried on your own to feel better or control your symptoms?
- What things make you feel worse?
- Have family members or friends commented on your mood or behavior?
- Do you have blood relatives with a mental illness?
- What do you hope to gain from treatment?
- What medications or over-the-counter herbs and supplements do you take?
- Do you drink alcohol or use recreational drugs?
Your doctor or mental health professional will ask additional questions based on your responses, symptoms and needs. Preparing and anticipating questions will help you make the most of your time with the doctor.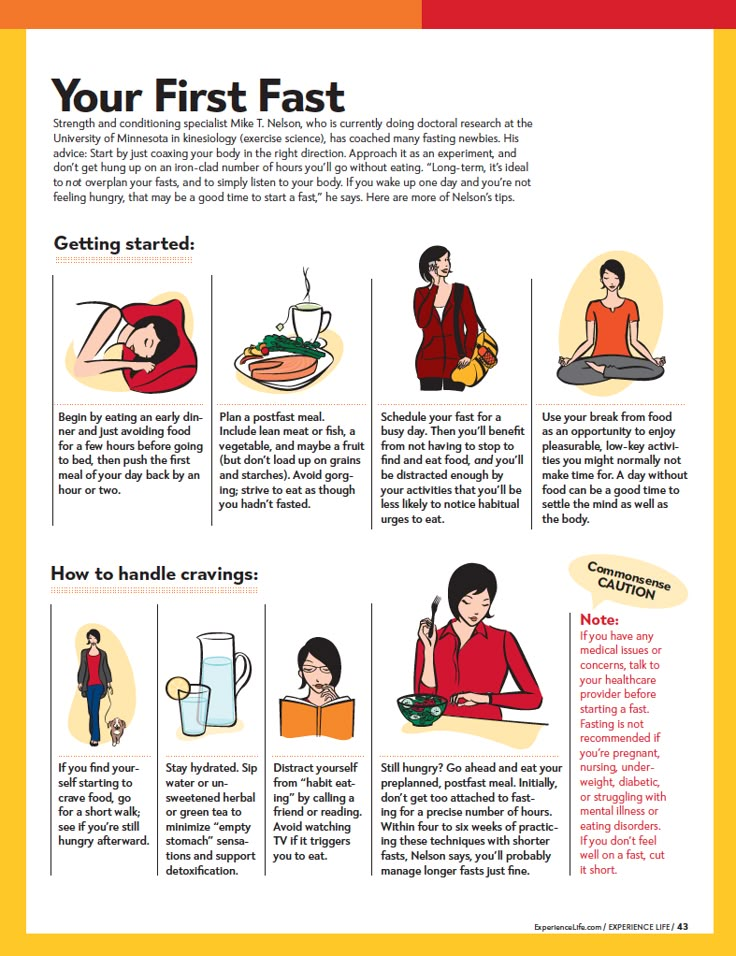
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Medication | Mental Health America
Researchers believe that the symptoms of mental illness come from chemical imbalances in a person's brain. A medication works on these imbalances to reduce your symptoms, or sometimes, to relieve them completely.
It is important to know the benefits of prescribed medications, as well as their potential side effects, and to talk to your doctor about any concerns that you may have. As you consider your options, it may help to know some basic facts about medication.
- Medications are not cures. Medications only treat symptoms, so if you stop taking them, your symptoms can return. Ask your health care provider how long you might expect to take medication.
- Every medicine has its benefits and its risks. Deciding to take medication is all about balancing possible benefits against possible side effects.
 Sometimes, it's hard to know how a medicine will affect you until you try it.
Sometimes, it's hard to know how a medicine will affect you until you try it. - Medications often help the most when they're part of an overall treatment program. Your plan may include psychotherapy, peer programs and rehabilitative services to help with problems that medication alone can't treat.
- It can take time to feel better. Some medications take a few weeks to work. And sometimes a medication's side effects may start before its benefits. You also may have to try more than one medication before you get the right fit, but many people find it's worth the wait.
Types of Medication
Medication Decisions
Brand vs. Generic vs. Authorized Generic Medications
Pharmacogenomics
Talk to Someone Now - Pharmacy Chat
Getting the Most Out of Medication
Staying Safe
Types of Medications
Learning about your medication options can help you have a more meaningful conversation with your doctor. You also can be more fully involved in taking care of your health. Medications for mental health conditions fall into the following types:
You also can be more fully involved in taking care of your health. Medications for mental health conditions fall into the following types:
Antipsychotic medications can help reduce or, in some cases, eliminate hearing unwanted voices or having very fearful thoughts. They can promote thinking clearly, staying focused on reality, and feeling organized and calm. They also can help you sleep better and communicate more effectively. These medications can come in pill form, which are taken daily, or in an injectable form that lasts between 3 and 6 weeks depending on the specific drug.
Possible side effects include: drowsiness, upset stomach, increased appetite and weight gain, blurred vision, constipation, dry mouth, dizziness, low blood pressure, restlessness, weakness, shakes and twitches, and muscle stiffness. Rare side effects include seizures and problems controlling internal body temperature.
Antidepressants help reduce such feelings as sadness or depressed mood and anxiety as well as suicidal thoughts. They do not, however, make people "happy" or change their personalities. The oldest form of antidepressants are called tricyclic antidepressants, but they are not prescribed as often as newer antidepressants like SSRIs or SNRIs because they have more side effects.
They do not, however, make people "happy" or change their personalities. The oldest form of antidepressants are called tricyclic antidepressants, but they are not prescribed as often as newer antidepressants like SSRIs or SNRIs because they have more side effects.
Possible side effects include: drowsiness or insomnia, constipation, weight gain, sexual problems, tremors and dry mouth.
For people whose depression is resistant to treatment and do not experience relief from antidepressants alone, esketamine may be taken in addition to antidepressants. Esketamine is derived from the drug ketamine and works on different chemical receptors in the brain than antidepressant pills. It is administered by a doctor as a nasal spray.
Mood stabilizers help reduce or eliminate extremes of high and low moods and related symptoms. They shouldn't keep you from experiencing the normal ups and downs of life, though. These medications are also used to treat depression that lasts for a long time, that goes away but comes back or that isn't treated well enough with an antidepressant alone.
Possible side effects include: stomach problems, drowsiness, weight gain, dizziness, shaking, blurred vision, lack of coordination or confusion.
Tranquilizers and sleeping pills can reduce anxiety and insomnia and help you feel more relaxed. Although some of them are used mostly to help with sleep, they all might cause drowsiness. Usually, these medications are used only briefly because longer use can cause dependency.
These medicines are generally safe when used as prescribed and have relatively few serious side effects. As with any medicine, though, some people may have difficulties. You should call your doctor right away if you experience headaches, slurred speech, confusion, dizziness, nausea or increased nervousness or excitability.
Stimulants and related medicines can have a calming effect and help improve concentration and attention span in both children and adults. They also can improve a person's ability to follow directions and reduce hyperactivity and impulsiveness.
Possible side effects include: trouble falling asleep, decreased appetite and weight loss. Less common side effects can include headaches, stomachaches, irritability, rapid pulse or increased blood pressure. These often go away within a few weeks after ending use or if your health care provider lowers your dose.
Medication Decisions
When you're feeling overwhelmed or confused, it's understandable that you might want to let others make medication decisions for you. But it's becoming clearer to researchers, providers and mental health consumers themselves that being actively involved in your treatment can make a real difference in your recovery. Talking honestly with your doctor is a big part of that process. If you discuss your concerns and learn about your options, you are much more likely to come up with a plan that works well for you and for the life you want to create.
The following tips can help you decide about taking a medication:
- Get information.
 Ask your provider how the medication is supposed to help with your specific concerns. Also find out about any possible side effects. You might consider taking notes, since it can be hard to remember a lot of information, especially when you aren't feeling well. You also might ask a friend or relative to go with you for emotional support and to help keep track of important information.
Ask your provider how the medication is supposed to help with your specific concerns. Also find out about any possible side effects. You might consider taking notes, since it can be hard to remember a lot of information, especially when you aren't feeling well. You also might ask a friend or relative to go with you for emotional support and to help keep track of important information. - Talk with others with similar experiences. Self-help groups and peer specialists-people with mental health conditions who are trained to help-can provide great first-hand information. Local Mental Health America affiliate offices, the National Alliance on Mental Illness, Depression and Bipolar Support Alliance and Children and Adults with Attention-Deficit/Hyperactivity Disorder are good sources for this kind of support. Remember that every person is different, but you can learn from the experiences of others.
- Think about your priorities and goals. Is relief from symptoms extremely important? If not, maybe you're willing to live with some symptoms to avoid side effects.
 What are your main life goals? How might medication help?
What are your main life goals? How might medication help? - Sometimes the only way to know if a medication is right for you is to try it. You may find that it helps you feel much better. If not, you can decide to stop later.
Medications are often prescribed by their brand name. This was the name they were given by the company that first created them. Once these medications are no longer “on patent” other companies may start making them and offering them as generic medications. These go by chemical names. For instance, Zoloft is a brand name antidepressant, and its generic name is sertraline. Brand name drugs and generic drugs must have the same active ingredient, but they may have different inactive ingredients used to make them. Inactive ingredients can be things like coloring agents, preservatives, and fillers. The FDA requires generic drug makers to prove that their products are just as effective as the brand name drug before people are allowed to buy them. Your insurance company will often require that you be given the less expensive, generic version of medication (if one is available) unless your doctor determines that the brand name version is medically necessary.
Your insurance company will often require that you be given the less expensive, generic version of medication (if one is available) unless your doctor determines that the brand name version is medically necessary.
When a doctor determines that a brand name medication is medically necessary for you or if you are seeking a generic that is identical to the brand but you have trouble affording the higher cost of the brand name medication, a third option may be available. This third option is an authorized generic. An authorized generic medication is a medication made by the original creator of the drug, using the exact same formula (including inactive ingredients) as the original drug. It is manufactured by the maker of the brand name medication and distributed by a special generics division of the drug company. An authorized generic medication will cost the same as a generic medication. But you may have to specially request it from your pharmacy because they may not keep it in stock. Not all medications are available in authorized generic form, but you can check to see if yours is at www.authorizedgenericmedicines.org/product-finder.
Not all medications are available in authorized generic form, but you can check to see if yours is at www.authorizedgenericmedicines.org/product-finder.
Pharmacogenomics is the study of how a person’s genes impact their reaction to drugs. It is a relatively new field that holds promise for developing effective medications and dosages based on a person’s genetic makeup.
When working with a clinician to start medication for a mental health condition, there are a number of factors that play into deciding which medicine is a good fit for you – this includes things like your physical and mental health history, family history, cost, and side effects. Pharmacogenomic testing can be an extra tool in your clinician’s toolbox to help inform medication selection.
Pharmacogenomic testing is conducted by your doctor with a simple cheek swab. By analyzing the genetic variations in your DNA, the test can provide information about genes that may impact how you break down or react to certain medications.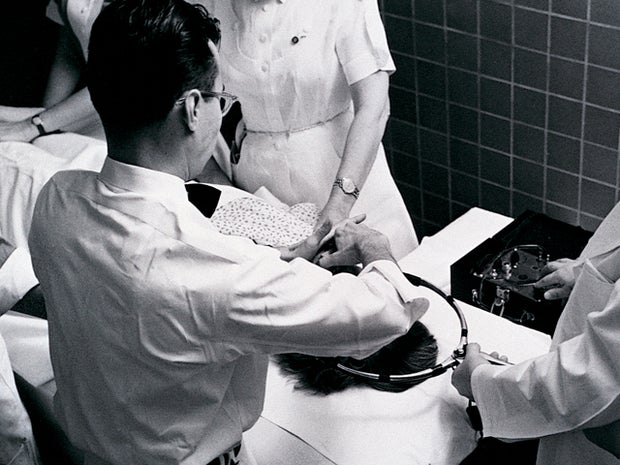 This can help your doctor predict which medications will be effective for you.
This can help your doctor predict which medications will be effective for you.
The cost of testing varies depending on which test is ordered and your health insurance. Not all insurance companies cover it, though some may depending on the reasons for testing – like if you have tried other medications that haven’t worked. If you’re concerned about cost and coverage, contact your insurance provider prior to testing so you can know what to expect.
Learn more about pharmacogenomic testing here.
Talk to Someone Now
MHA has a partnership with Walgreens and together we want to help if you have extra questions. Visit their Pharmacy Chat and speak to someone today for extra help.
Getting the Most Out of Your Medication
Some people get relief from their symptoms immediately, others after a few days or weeks; for others it may take even longer. Medications differ widely in how quickly they take effect. After a short time on the medication, it's important to share with your doctor or therapist how you are doing with the treatment.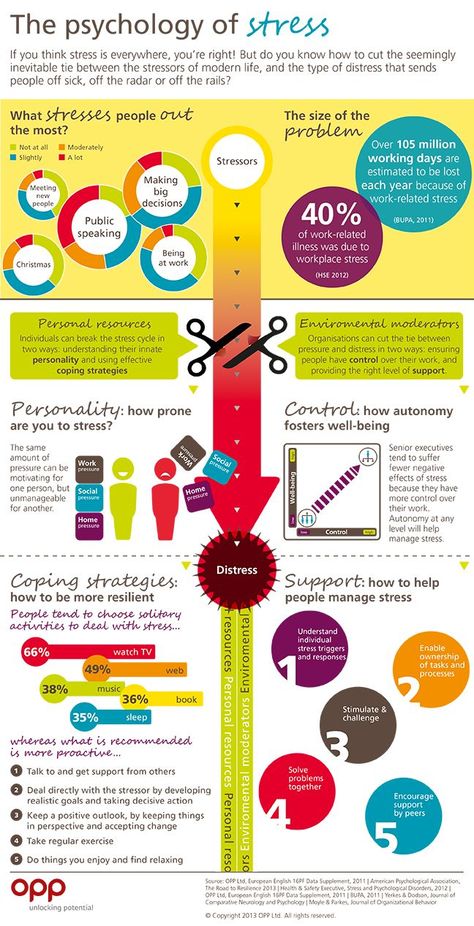
Remember to be honest with your provider. Tell him or her about your symptoms. Also make sure to tell the provider about any drugs, alcohol, over-the-counter or prescription medicines and herbal supplements you've been taking. That way you'll get the most appropriate treatment.
Dealing with side effects
If you're having trouble with a medication, or experiencing unpleasant side effects, don't suffer in silence. Your doctor or pharmacist will likely have suggestions that can help. You can use a side-effect checklist to keep track and quickly share information with your provider.
Sometimes side effects can be addressed easily. If you have:
- Dry mouth...Try sugarless gum or mints
- Constipation...Drink plenty of water and eat lots of fruits and vegetables. Ask your doctor or pharmacist about over-the-counter remedies.
- Nausea...Take your medication with a meal.
- Feeling sleepy.
 ..Ask about changing when you take the medication.
..Ask about changing when you take the medication. - Problems with sexual functioning...Talk with your doctor about changing or adding medicines. Talk with your partner about what's happening.
Try to keep track of your progress
- Keep a chart of your medications and how you're feeling. That way you can make sure you're taking your medicines at the right times, and you can see how they affect your progress. You also might want to share your chart with your health care providers. It's very important that your providers have all your recent information so they can figure out how best to support your recovery.
- If you have any questions, consider putting them in your chart. It can be hard to remember everything you want to discuss with your doctor, especially if your appointment is short or you feel somewhat stressed about it.
- Hold on to your records. If a doctor suggests a particular medicine, you can check your records to see if you've taken it in the past and how well it worked.

- Keep track of who can help. Ask your doctor whom to call if you suddenly have troubling side effects. Pharmacists can be of tremendous help in understanding medications, how to use them safely, possible side effects and other treatment options. Give a list of your medications to a friend or family member in case of emergency. Carry one in your wallet too. Include the names of your pharmacy and your health care providers.
If you are thinking about stopping your medication...
There are many reasons people consider stopping their medication. Some people dislike the side effects, feel that there's stigma about medication or worry about the expense. If these or other concerns are bothering you, know that you are not alone. Still, quitting is a big decision and can seriously affect your health, so think it through carefully.
Some possible steps if you're thinking about stopping include:
- Take a look at your situation. Consider whether changes in your life or your body may be affecting how well the medication is working.
 Ask your doctor if switching or adding medications might help. And ask whether stopping a medication creates a risk that means it won't work as well if you decide you want to go back on it later.
Ask your doctor if switching or adding medications might help. And ask whether stopping a medication creates a risk that means it won't work as well if you decide you want to go back on it later. - Talk honestly with your health care provider. Some people feel uncomfortable raising concerns with their providers. Remember that it's your right to ask questions and make decisions. To help the conversation go smoothly, make sure you both have enough time to talk. State your concerns calmly, and try to agree on some reasonable next steps for promoting your recovery.
- Talk to the people who support you. They may be able to help you decide. Even if you don't want help with the decision, people close to you should know that you haven't been feeling well. That way they can provide extra support if you need it.
Staying Safe
Following some basic guidelines will protect your health while taking medication:
- Avoid using street drugs or drinking alcohol while taking psychiatric medications.
 The combination can be dangerous and even deadly.
The combination can be dangerous and even deadly. - Be careful while driving or using machinery, especially if your medicine makes you sleepy.
- Women who may become pregnant, are pregnant, or are breast-feeding should talk with their doctor about possible special concerns related to medications.
- Stopping medications abruptly may cause you to feel ill - and possibly could even cause a seizure. They should be stopped gradually and according to your doctor's instructions.
- If taking a medicine causes you to feel sick, have a fever, skin reaction or anything else that worries you, contact your doctor or pharmacist as soon as possible.
Ask Important Questions
To protect your health, be sure to ask your doctor or pharmacist the following questions:
- What is the name of the medication? Is it known by other names too? Is it a "brand name" or generic?
- When will the medication begin to work?
- What is the recommended dosage? How many times a day will I take it?
- Should I take the medication with food?
- What are the side effects that commonly occur with this medication?
- What are the less common but more serious side effects that can occur?
- Is this medication addictive? Can it be abused?
- Are there any laboratory tests that I need before beginning this medication or while I'm taking it?
- Are there any medications, foods or supplements I should avoid while taking this medication?
- How long will I be taking this medication? If I stop taking it, what are the chances of my symptoms returning?
- Is there any chance my symptoms will be worse once I stop?
- How soon will I see results?
Learn more about how medications can affect you here.
Help for a loved one with a mental disorder
Basic concepts
There is a lot of talk these days about the rise in the number of mental disorders in society, but many people have very vague ideas about this very vague concept. Despite the fact that now psychiatrists are doing everything possible to inform the population as best as possible about stress, depression, anxiety, neurosis, more severe mental disorders, there is very little literature written by experts for the average layman, and on the Internet there is an abundance of information written either difficult language, or simply illiterate. All this ultimately leads to the fact that such information is not only contrary to reality, but also harmful.
It is impossible to sort everything out in one article and give clear instructions on the relationship between the patient and his relatives, but it is possible to bring to a holistic picture the idea of this complex group of diseases (the terms "disease" and "disorder" from a medical point of view are largely close, but not identical*).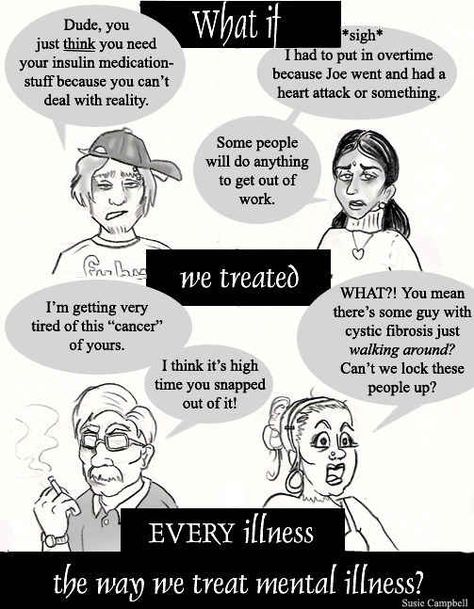 Therefore, my task is to acquaint the reader with this complex problem, primarily related to relationships and assistance to those suffering from severe mental illnesses.
Therefore, my task is to acquaint the reader with this complex problem, primarily related to relationships and assistance to those suffering from severe mental illnesses.
* It is desirable to know the most basic terms, then it will be easier for the doctor to help both the patient himself and his relatives. In addition, you should not use terms that are not well known to you, it is better to describe the situation or condition as you understand it.
So, mental (or mental, because psyche - translated from Greek means the soul ) disorders - are painful conditions of a person with psychopathological (i.e., with mental disorders) and behavioral (i.e., they do not always appear, for example, in case of neurosis, when a person by willpower keeps himself within the limits of cultural society up to a certain point) manifestations due to the influence of biological, psychological, social and other factors.
Let's not confuse with psychosis (or psychotic) disorders, which are characterized by gross and contradictory environmental disorders of thinking, perception and behavior (delusions, in a medical, not philistine view; hallucinations; psychomotor agitation; suicidal behavior, etc. ).
).
It is important to note that the problem of mental disorders is interdisciplinary and even interdepartmental, social. Rehabilitation is needed, not just treatment.
As for the diagnosis. Diagnosis - definition and recognition, an indication of the disease. In medicine, and especially in psychiatry, diagnosis does not always imply treatment in strict accordance with the diagnosis. Diagnosis is often a statistical category necessary to understand, roughly speaking, how the condition of one patient is similar to another.
I am sometimes puzzled by the desire of a person to look at the records of a doctor. After all, a special interpretation, justification of the diagnosis, terminology can not only frighten and offend an unprepared person, but cause unreasonable distrust of a specialist and, even worse, aggravate disturbed mental balance, upset not only the patient, but also relatives.
It is much more important to trust each other (the doctor, the patient, his relatives), to ask questions of interest.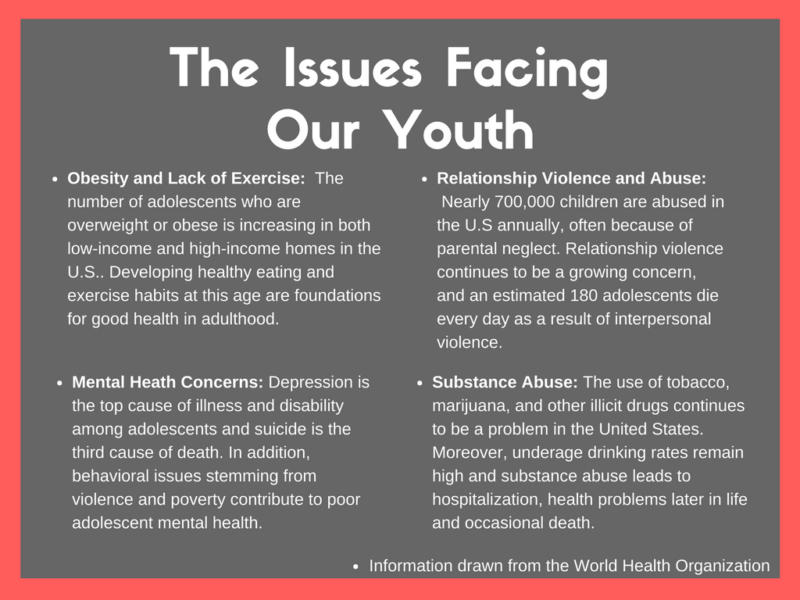 It is on trust that the desired result is achieved - a cure or a stable remission, if the disorder is chronic.
It is on trust that the desired result is achieved - a cure or a stable remission, if the disorder is chronic.
I will not decipher concepts and terms much in this article. Let's talk about the topic corresponding to the title. We will talk about such diseases as schizophrenia, dementia, severe depression, drug addiction (alcoholism, drug addiction), etc. I will try to give basic, a kind of "universal" recommendations.
Recommendations
1 situation: a relative (both a 16-year-old child and an old grandfather, a researcher in the past or present) became “somehow not like that”, began to withdraw, get annoyed for no apparent reason, although “he had never been aggressive before ', to talk, to talk to oneself.
Usually, such behavior is first perceived as a joke, then surprise, then a discussion with a sick person begins, which can lead to serious conflicts and distrust. If you suspect that a person close to you has a mental disorder (we do not take emergency situations, for example, in case of severe aggression, the police and medical workers are already intervening here), you cannot argue.
It is also desirable not to support the painful delusions of a person, to try to be patient and caring, to persuade a loved one to seek medical help. Unfortunately, in our society, when it comes to psychiatry, in most cases it causes a smile, fear, surprise, but not sympathy and a desire to help a sick person, especially if it refers to a relative. Only later, when a sick person can feel and even understand that the help of a psychiatrist is for his benefit, will he himself reach out to her.
At the initial stage, it is worth trying to persuade a person to calm down, assess his degree of adequacy (if he used to trust you, but now he doesn’t groundlessly, whether he understands you or is completely in his experiences, etc.), to understand whether there are threats to him and surrounding.
It is impossible to forcibly help a person (involuntary hospitalization in a psychiatric hospital is carried out only by a court decision), but everything possible must be done: to involve relatives who will correctly understand and support people who are authoritative for the patient, consult a doctor.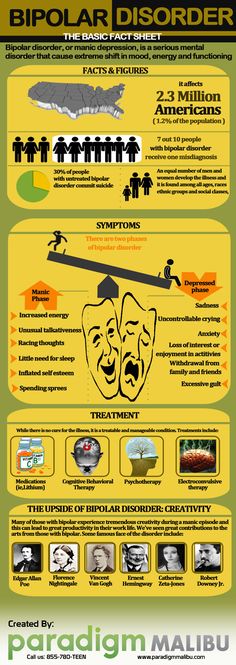
Situation 2: patients were brought to a psychiatrist. There can be 2 ways here. The doctor will help to understand the situation, make a diagnosis, prescribe treatment, give recommendations. Everything here is very individual. But it may also be that the doctor gives a recommendation, but not only the patient (due to inadequacy), but also a relative does not want to follow it.
I can give an example. A mother brings her 20-year-old daughter to a psychotherapist. The daughter has painful sensations in her body: the bones, according to her, “go back and forth, fall through and hurt.” All specialists were examined, all studies were carried out, including MRI, no diseases were found, the symptoms do not correspond to the alleged physical pathology.
A mental illness was diagnosed, drugs were prescribed, and after a couple of months there was a significant improvement. The patient stops taking the medicine, after a while she comes to the doctor with her mother, complains about the deterioration, assures that the medicines do not help, refuses help, runs out of the office, rushes about, says that she does not want to live. Hospitalization is proposed, since adequate dosages of drugs can only be prescribed in a hospital, in response - a categorical refusal.
Hospitalization is proposed, since adequate dosages of drugs can only be prescribed in a hospital, in response - a categorical refusal.
With difficulty he manages to calm down, persuade him to give an injection, agrees to resume taking medications. The doctor suggests that the mother call a psychiatric team to resolve the issue of hospitalization, in connection with the suicidal risk, to which he receives the answer: “Well, she will kill herself, then this is her fate, I will not put her in a psychiatric hospital.” On receipt released home. The mother calls the next day, the daughter gets a little better, then disappears for six months. Another call to the doctor's personal phone: the daughter lies in bed, does not want to get up, complains about "movements in the body of some creatures" that cause severe pain.
Recommendations were given, the patient was finally hospitalized in a psychiatric hospital with schizophrenia. She was discharged with improvement, criticism of her condition appeared, adequate therapy was selected.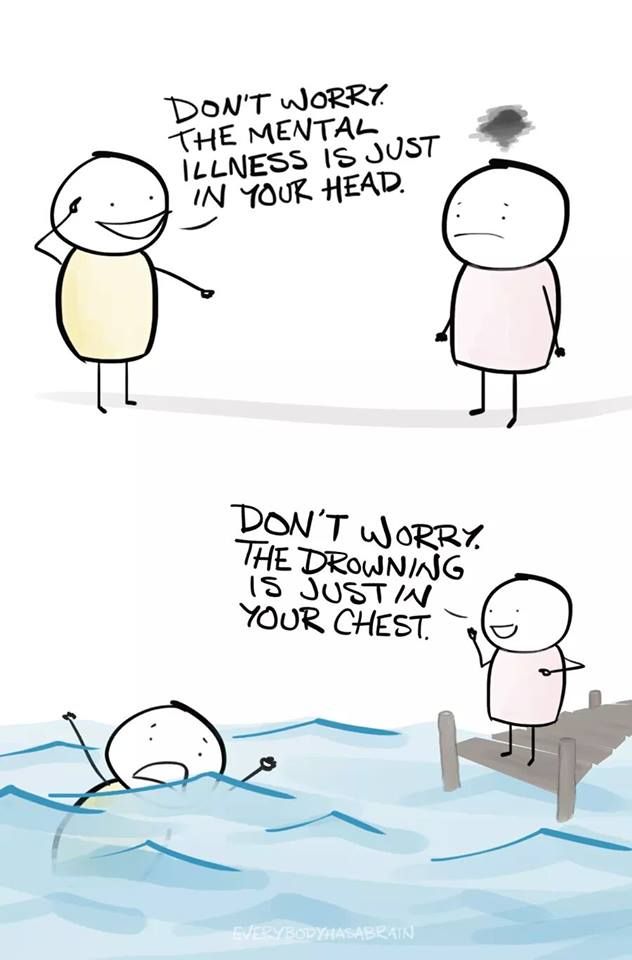
Bottom line: fortunately, this story ended happily, but the patient suffered for several months, while the mother believed in the need for hospitalization; I had to prescribe heavier drugs, the treatment was delayed.
There is nothing wrong if the patient refuses this doctor (for example, the patient has included the doctor in his delusional system) or the doctor himself understands that he will not be able to provide adequate assistance. Then it is necessary to attract colleagues, send them to a hospital, together with relatives, think over options for assistance and choose the best one. It happens that the patient returns after treatment, apologizes for his behavior, because he did not understand the pain and inadequacy at that time.
You should not change specialists (sometimes people come to me with dozens of recommendations from different doctors of the same specialty, which is puzzling). Well, 2-3 opinions is understandable, but more than 10!? The most common reason is that medications do not immediately help, side effects.
Some patients soon stop taking their medications, and many diseases are chronic and require many months or even years of maintenance therapy. A natural deterioration sets in, the new doctor does not yet know the specifics of the course of the disorder in this patient, experiments with treatment begin, a new selection of medicines begins, resistance to treatment is formed, and previously effective drugs cease to work.
And one more thing: it is desirable, at the initial visit to the doctor, to bring, if not all, then the main examinations, extracts, and tests. A psychiatrist is a doctor like everyone else, and the more information about the patient, the easier it is to understand the diagnosis. For example, if a person has a pathology of the thyroid gland, it is advisable to bring the last tests for hormones, since when the hormonal background changes, the state of mind also changes (irritability, sleep disturbances, mood swings, etc.).
In some cases, antidepressants are not only not needed, but can be harmful, it may be worth limiting yourself to the appointments of an endocrinologist and psychotherapy.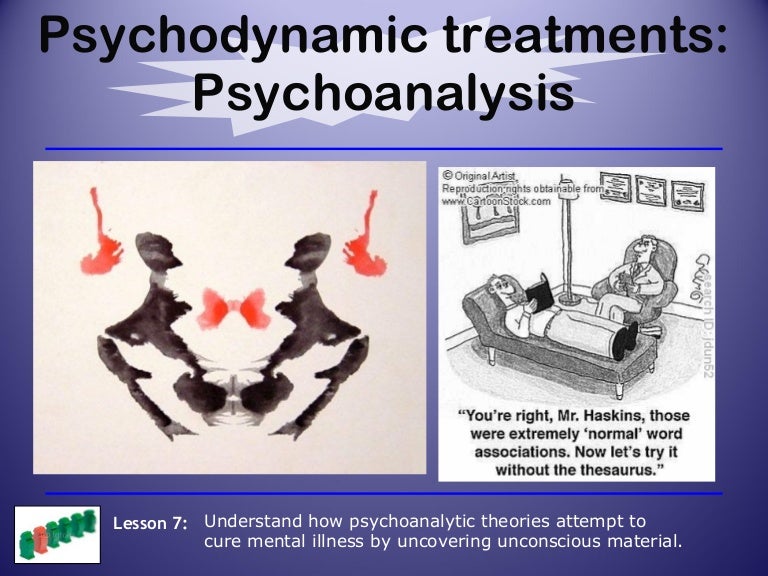 Elderly people with diabetes can confuse events and even behave inappropriately with an increase in blood glucose, here prescribed antipsychotics are also not always necessary.
Elderly people with diabetes can confuse events and even behave inappropriately with an increase in blood glucose, here prescribed antipsychotics are also not always necessary.
3 situation: the patient has been examined for a long time, the diagnosis is known, but the disease is progressing. Relatives begin to "look for a miracle": consult the patient with leading specialists, go to the main scientific centers, someone is looking for help abroad.
I have had a number of cases where patients have returned from the US, Europe, Israel, etc. with complaints that the prescription of drugs selected in Russia was refused, or that the treatment was simply ineffective, worsened. Here I would advise you to find a specialist you trust and coordinate your actions with him. Only together can we help sick people provide adequate assistance and, if not cured, then improve the quality of life as much as possible.
4 situation: terminally ill patient in the final stage. There is an opinion, or rather another myth, that one does not die from mental illness, however, mental illness is the same as somatic (i.e. body diseases), only the brain is sick, regardless there is a visible focus there (for example, as a result of a craniocerebral injury to the damaged part of the brain) or not. For example, severe progressive dementia, the final stage of alcoholism with multiple organ disorders, the terminal stage in malignant forms of schizophrenia, and others. Here it is necessary to decide individually, depending on the specific case.
There is an opinion, or rather another myth, that one does not die from mental illness, however, mental illness is the same as somatic (i.e. body diseases), only the brain is sick, regardless there is a visible focus there (for example, as a result of a craniocerebral injury to the damaged part of the brain) or not. For example, severe progressive dementia, the final stage of alcoholism with multiple organ disorders, the terminal stage in malignant forms of schizophrenia, and others. Here it is necessary to decide individually, depending on the specific case.
“If a person cannot be cured, this does not mean that he cannot be helped.”
If you are destined to die, it is easier to do this among loving relatives on your bed, even if a person does not understand anything and does not recognize anyone. But he FEELS the attitude towards him. How a small child feels the caress of his mother, smiles or cries when his mother is gone. You will say - there is no comparison, children are our future, and here is a dying person who does not understand anything. Yes, this is true, but we must understand that any of us can, God forbid, be in the place of this person ...
Yes, this is true, but we must understand that any of us can, God forbid, be in the place of this person ...
Nursing staff
Well, a few words about help for those who care for the sick. It is difficult to give specific recommendations here, only one thing is clear: you cannot take the position of either a rescuer or a victim, you just need to fulfill your human duty to the best of your ability and ability. Don't forget yourself.
Any person who lives with a sick person, and even more so caring for him, experiences enormous personal and emotional stress. Therefore, you should think about how you will cope with the disease in the future. By understanding your own emotions properly, you will be able to deal more effectively with both the patient's problems and your own problems. You may have to experience emotions such as grief, shame, anger, embarrassment, loneliness and others.
For some people who care for the sick, the family is the best helper, for others it brings only grief. It is important not to reject the help of other family members if they have enough time, and not to try to bear the sometimes difficult burden of caring for the sick alone.
It is important not to reject the help of other family members if they have enough time, and not to try to bear the sometimes difficult burden of caring for the sick alone.
If family members upset you with their unwillingness to help, or criticize your work because of the lack of information about this disorder, you can form a family council to discuss care problems. In particular, make a decision to involve an employee, at least for the period of time necessary for your rest and recuperation, and, if necessary, treatment.
And the last. Don't keep problems to yourself. Feeling that your emotions are a natural reaction in your position, it will be easier for you to cope with your problems. Don't reject the help and support of others, even if you feel like you're making it difficult. Even psychotherapists themselves (seemingly knowing how to minimize stress as much as possible) often have their own psychotherapist, and it is bad for the doctor who neglects the help of his colleagues.
Prepared information for you:
Aronov Pavel Vladimirovich - psychiatrist, psychotherapist, narcologist, doctor of the highest category, candidate of medical sciences, associate professor. The doctor conducts an appointment in the building of the clinic on Baumanskaya.
Is it possible to cure a mental disorder and how to understand that you are already healthy - Knife
Author Elena Leontyeva
regular author of The Knife, clinical psychologist, gestalt therapist, host of a telegram channel about family therapy and author of books "About Psychos" and "Private Practice"
The answer to this question greatly depends on the place and time.
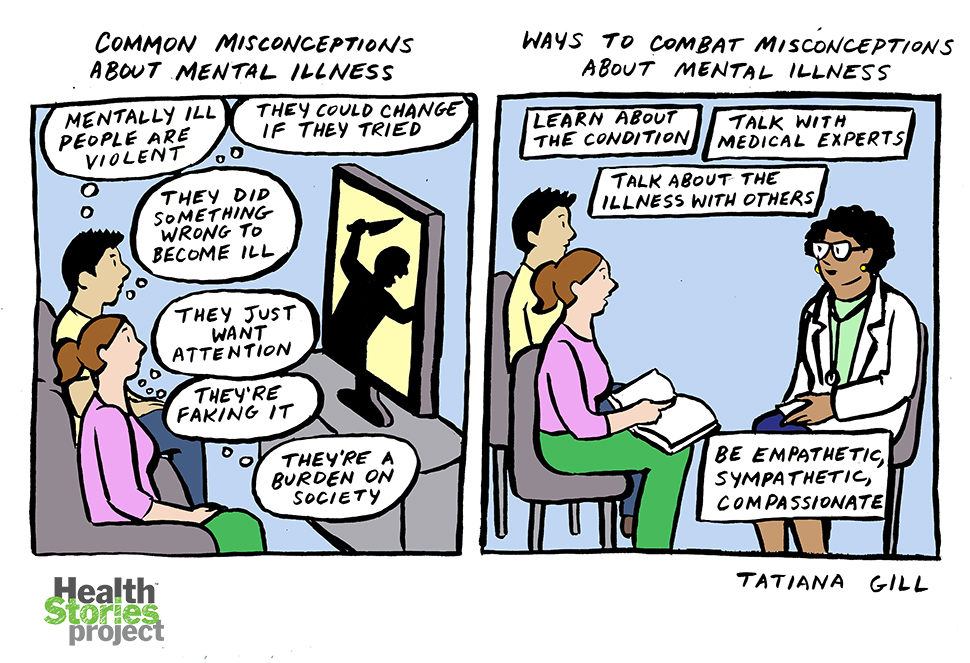
More recently, the underlying mental illness, schizophrenia, was considered incurable and therefore had a very bad reputation compared to other disorders. The horror stories of everyday consciousness scare people with dangerous, unpredictable people who commit shameful and unpleasant deeds and who should preferably be kept in prison-type special institutions for life.
Now we can control conception, live twice as long and transplant new organs - so what prevents us from curing such an ephemeral substance as the psyche? Mental disorders are no longer perceived as fatal, and some are now even considered indicators of originality or talent. The role of the media and social networks is important here: the legalization of mental problems has become a growing trend.
See also
Antipsychiatry: how the protest against punitive psychiatry led the world to revise the norm
Antipsychiatry: how the protest against punitive psychiatry led the world to revise the norm
The truth, as usual, lies somewhere in between.
In fact, many will never take the chance to be cured. There are cases when medicine is completely powerless: drugs may not help, and mental disorders that start in childhood and have a strong impact on development are difficult to treat or not treated at all.
But for those who are fortunate enough to be helped by medications, with rehabilitation professionals working with them, it is important to understand what it means to "cure" a disorder.
What does it mean to be cured?
Usually people think that being cured means never getting sick again. By this logic, almost all diseases are incurable: there are no guarantees that an attack of gastritis will not happen to you in forty years. But if there was no gastritis for forty years, did you have it all this time, or did you not?
Physicians have been arguing furiously about the nature of schizophrenia for more than a century and have not come to a consensus. The idea of incurability is also supported by the fact that some patients need treatment and government support all their lives: registration rules, regular monitoring, free medicines and opportunities for hospitalization and rehabilitation. If a person is recognized as cured, then he must be deprived of this help - and such a level of risk and responsibility of state medicine is almost inaccessible.
Therefore, a complete “legal” recovery: discontinuation of medication, withdrawal of a psychiatric diagnosis and deregistration, requires a lot of effort from the patient and a willingness to take serious risks from the doctor.
However, the more optimistic patients and specialists themselves are in dire need of hope for a cure. Otherwise, stigmatization (“psychos are dangerous and cannot be cured”) and self-stigmatization (“I am a sick person - a psycho for life”) destroy life and impose fatal restrictions, which, as a rule, concern family, children and profession.
Russian psychiatrists I. Ya. Gurovich and A. B. Shmukler cite data from numerous studies, according to which at least 20-25% of patients with schizophrenia recover, and this also applies to severe hospital patients. And the psychiatrists of the National Medical Research Center for Psychiatry and Narcology named after V.P. Serbsky A.B. Shmukler and O.S. Bochkareva showed that 44% of patients after the first psychotic state had a stable remission that lasted at least 5 years.
These data look optimistic and outline a large circle of patients who can be helped by psychological rehabilitation, and the episode of the disease will remain the only one in a lifetime.
What is mental health
What can we rely on when answering the question: “Am I mentally healthy”?
Today, the concepts of “mental health” and “quality of life”, which are considered normal in the opinion of the majority, are at the forefront. These criteria for mental health are available, but if they are followed, on the entire planet we will barely scrape together a handful of "normal" people. And after the pandemic - and no one at all. Therefore, based on my many years of practice and experience, I will single out only three points that I consider important.
1. Critical view of the disease
To be critical of the disease means to know about yourself that you were sick and needed medical help or are sick now and you need treatment. You can have many versions about the reasons for this, resentment against relatives and doctors - all this is not fundamental. The main thing is that you know for sure that you were sick and needed help (or so it is now).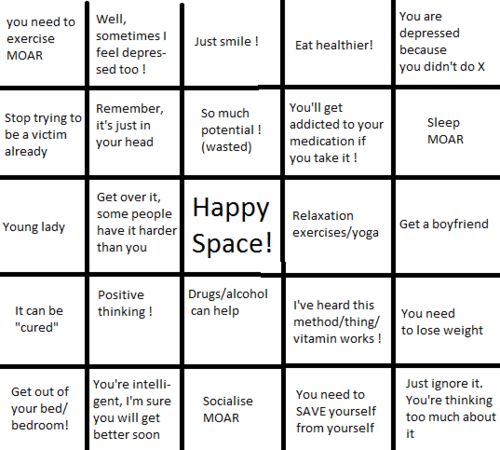 This fact is no longer a zone of psychological conflict for you.
This fact is no longer a zone of psychological conflict for you.
2. Mental symptoms ended
You made contact with specialists and received treatment, after which the symptoms of a mental disorder ended or stopped bothering you. You have already restored your usual way of life and now you are responsible for yourself. You have successfully completed family and labor rehabilitation. You know how to help yourself and where to turn for help if you need it.
If you check the box next to these two items, then you are cured and you can be considered a mentally healthy person. And there are no guarantees that "there will never be anything else". Just like with gastritis.
The third point is controversial and very exciting for everyone.
3. Refusal of drug therapy
It is controversial because there are thousands of cases where people have been drinking antipsychotics for decades and thus avoiding exacerbations. Just like many people take dietary supplements or cholesterol-lowering drugs for half their lives.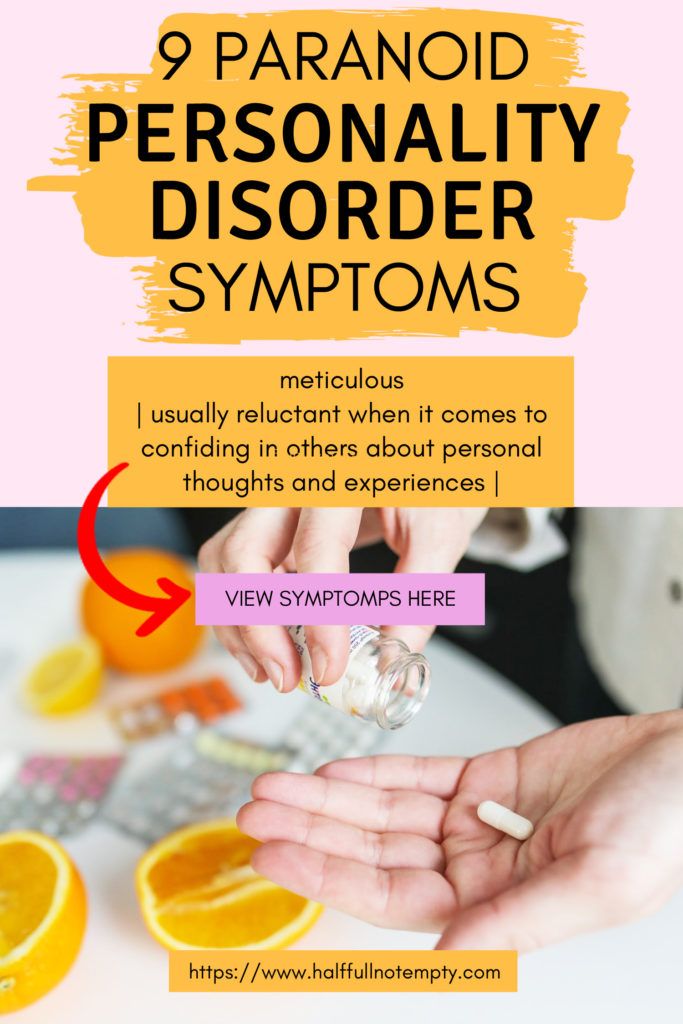
Patients withdraw from medication because when symptoms go away, normal life takes over. And then the little things become important, including how we feel every day.
Medicines often dull the senses and emotions. Unfortunately, in the perception of some people, they also reduce the joy of simple things: the sun outside the window, delicious food, sex, communication, and so on.
By canceling medications, patients regain their usual level of emotions before the illness: “It’s as if you are starting to live normally again,” and, of course, this is very attractive.
The problem is that until the patient learns to independently control the strong fluctuations of his emotions, an exacerbation of a mental disorder is almost inevitable. A month, two or a year without drugs - and all over again.
Specialists need to warn patients about this, and people with diagnoses need to look for a way out of this situation together with their doctor, and not behind his back. And this is often helped by working with a psychologist who responds in a timely manner to changes in the state of his patient. This helps to track the symptoms and their relationship with the patient's psychological problems and develop an adequate attitude towards oneself and one's health.
And this is often helped by working with a psychologist who responds in a timely manner to changes in the state of his patient. This helps to track the symptoms and their relationship with the patient's psychological problems and develop an adequate attitude towards oneself and one's health.
Maybe interesting
Psychosis: is it possible to prevent it, how to recognize it, how to treat it - and what to do if your loved one has a psychotic disorder
In addition, there is a specific Russian phenomenon - pharmacophobia , when people believe that the harm from drugs is greater than from the disease. Now we are seeing how people are more afraid of vaccinations, and not of the virus. As in the case of a mental disorder, here we are dealing with psychological defense - denial and displacement, that is, we are not afraid of what is really scary.
Sometimes it takes a lot of effort and time to make patients and relatives understand that, without treatment, a mental disorder leads to irreparable losses: the disintegration of the personality and a profound impairment of thinking.
And psychoses often have devastating consequences for the psyche, after which a person can become disabled. Therefore, pills are always the lesser of evils.
Restoring an adequate internal picture of the disease and answering the difficult question "What happened to me and why?" and most of the psychological rehabilitation is devoted.
Who conducts rehabilitation?
Participating in the rehabilitation process:
- medical institution (hospital, day hospital, neuropsychiatric clinic),0226
- attending doctor,
- clinical psychologist or psychotherapist,
- social worker,
- support groups,
- the patient himself and his family.
Psychosocial rehabilitation begins at the first visit to mental health care. The role of this episode is very important: the patient's future attitude to his illness depends on the initial experience of the patient.
Unfortunately, in our country, a psychological culture is just beginning to take shape: people turn to a psychologist and doctors mainly when “thunder is already thundering” and the storm of disorder has already begun.
Therefore, the initial treatment often immediately ends with hospitalization, since the person is already in a completely inadequate condition - in the acute phase of the disease, which requires immediate medical treatment and observation.
Often, patients and their relatives seek help not from specialists, but in circles alternative to psychological ones: in the church, shamans, personal growth trainings or some non-specialized events where the peculiarities of their mental state can clearly manifest themselves.
By themselves, these activities are not to blame for the deterioration of the mental state of a person, and are not the cause of disorders, as one might think. The state of a mental patient would still worsen in due time without treatment, but there is a trigger.