How do you diagnose alzheimer's
Alzheimer's disease - Diagnosis and treatment
Diagnosis
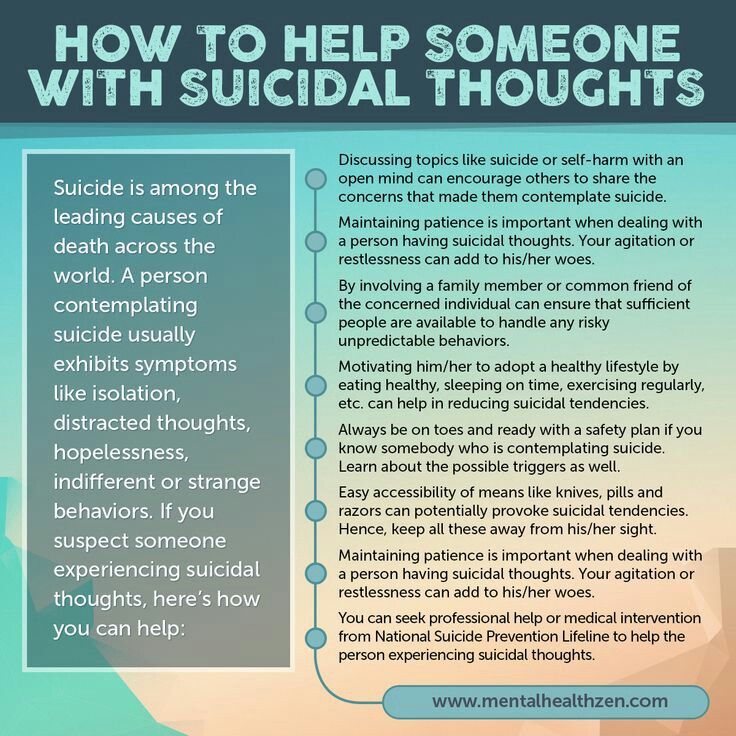
An important part of diagnosing Alzheimer's disease includes being able to explain your symptoms, as well as perspective from a close family member or friend about symptoms and their impact on daily life. Additionally, a diagnosis of Alzheimer's disease is based on tests your doctor administers to assess memory and thinking skills.
Laboratory and imaging tests can rule out other potential causes or help the doctor better identify the disease causing dementia symptoms.
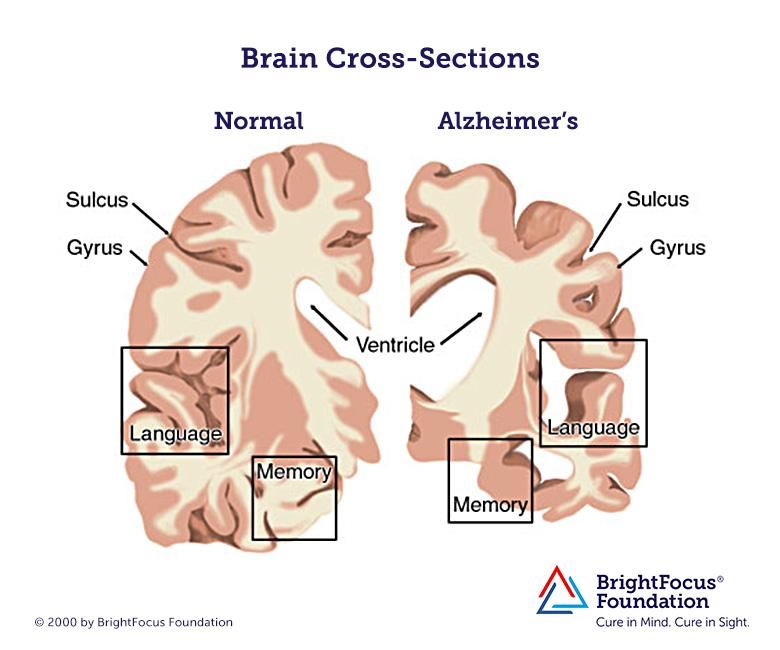
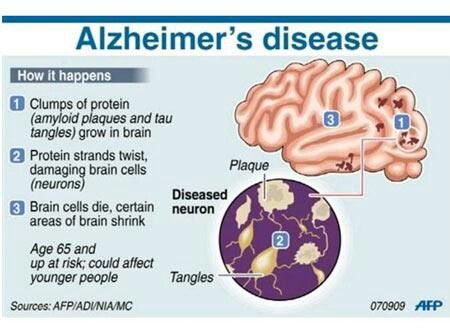
Traditionally, Alzheimer's disease was only diagnosed with complete certainty after death, when examining the brain with a microscope revealed the characteristic plaques and tangles. Clinicians and researchers are now able to diagnose Alzheimer's disease during life with more certainty. Biomarkers can detect the presence of plaques and tangles, such as specific types of PET scans or measuring amyloid and tau proteins in plasma and cerebral spinal fluid.
Tests
A diagnostic work-up would likely include the following tests:
Physical and neurological exam
Your doctor will perform a physical exam and likely assess overall neurological health by testing the following:
- Reflexes
- Muscle tone and strength
- Ability to get up from a chair and walk across the room
- Sense of sight and hearing
- Coordination
- Balance
Lab tests
Blood tests may help your doctor rule out other potential causes of memory loss and confusion, such as a thyroid disorder or vitamin deficiencies.
Mental status and neuropsychological testing
Your doctor may give you a brief mental status test to assess memory and other thinking skills. Longer forms of neuropsychological testing may provide additional details about mental function compared with people of a similar age and education level. These tests can help establish a diagnosis and serve as a starting point to track the progression of symptoms in the future.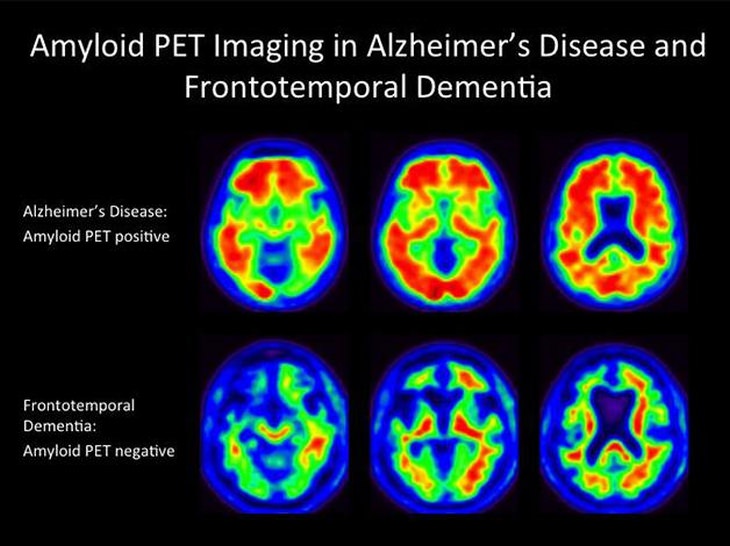
Brain imaging
Images of the brain are now used chiefly to pinpoint visible abnormalities related to conditions other than Alzheimer's disease — such as strokes, trauma or tumors — that may cause cognitive change. New imaging applications — currently used primarily in major medical centers or in clinical trials — may enable doctors to detect specific brain changes caused by Alzheimer's.
Imaging of brain structures include the following:
- Magnetic resonance imaging (MRI). MRI uses radio waves and a strong magnetic field to produce detailed images of the brain. While they may show brain shrinkage of brain regions associated with Alzheimer's disease, MRI scans also rule out other conditions. An MRI is generally preferred to a CT scan for the evaluation of dementia.
- Computerized tomography (CT). A CT scan, a specialized X-ray technology, produces cross-sectional images (slices) of your brain. It's usually used to rule out tumors, strokes and head injuries.
Imaging of disease processes can be performed with positron emission tomography (PET). During a PET scan, a low-level radioactive tracer is injected into the blood to reveal a particular feature in the brain. PET imaging may include the following:
- Fluorodeoxyglucose (FDG) PET scans show areas of the brain in which nutrients are poorly metabolized. Identifying patterns of degeneration — areas of low metabolism — can help distinguish between Alzheimer's disease and other types of dementia.
- Amyloid PET imaging can measure the burden of amyloid deposits in the brain.
 This imaging is primarily used in research but may be used if a person has unusual or very early onset of dementia symptoms.
This imaging is primarily used in research but may be used if a person has unusual or very early onset of dementia symptoms. - Tau PET imaging, which measures the burden of neurofibrillary tangles in the brain, is generally used in the research setting.
In special circumstances, such as rapidly progressive dementia, dementia with atypical features or early-onset dementia, other tests may be used to measure abnormal beta-amyloid and tau in the cerebrospinal fluid.
Future diagnostic tests
Researchers are working to develop tests that can measure biological signs of disease processes in the brain.
These tests, including blood tests, may improve the accuracy of diagnoses and enable earlier diagnosis before the onset of symptoms. A blood test for Plasma Aβ is currently available and recently received certification in the U.S. by the Centers for Medicare & Medicaid Services to allow distribution on the market.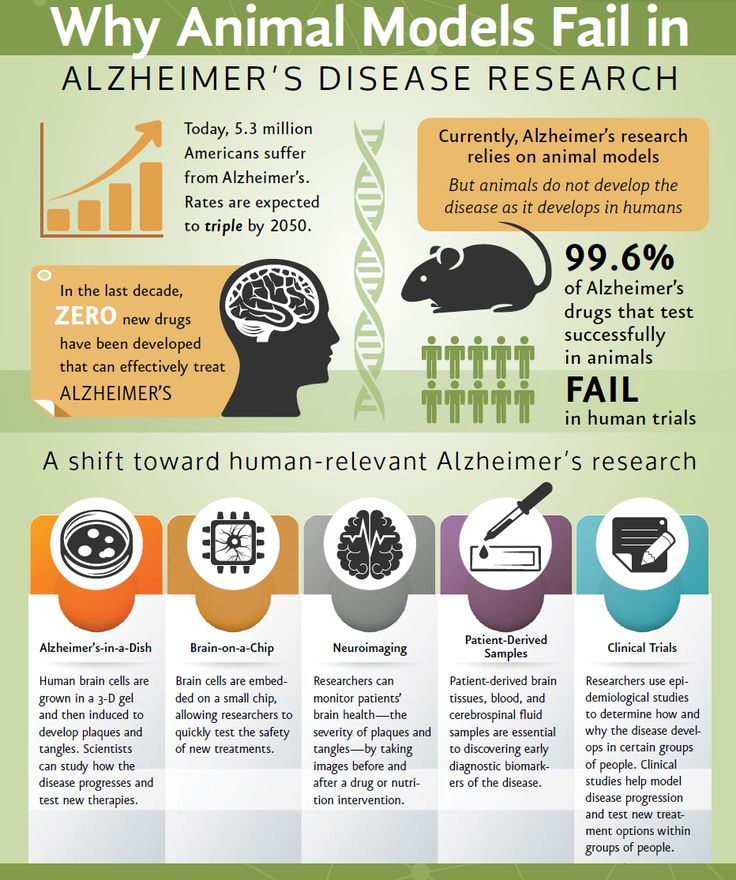
Genetic testing generally isn't recommended for a routine Alzheimer's disease evaluation. The exception is people who have a family history of early-onset Alzheimer's disease. Meeting with a genetic counselor to discuss the risks and benefits of genetic testing is recommended before undergoing any tests.
Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your Alzheimer's disease-related health concerns Start Here
More Information
- Alzheimer's disease care at Mayo Clinic
- Diagnosing Alzheimer's
- CT scan
- MRI
- Positron emission tomography scan
- Mayo Clinic Minute New definition of Alzheimer's changes
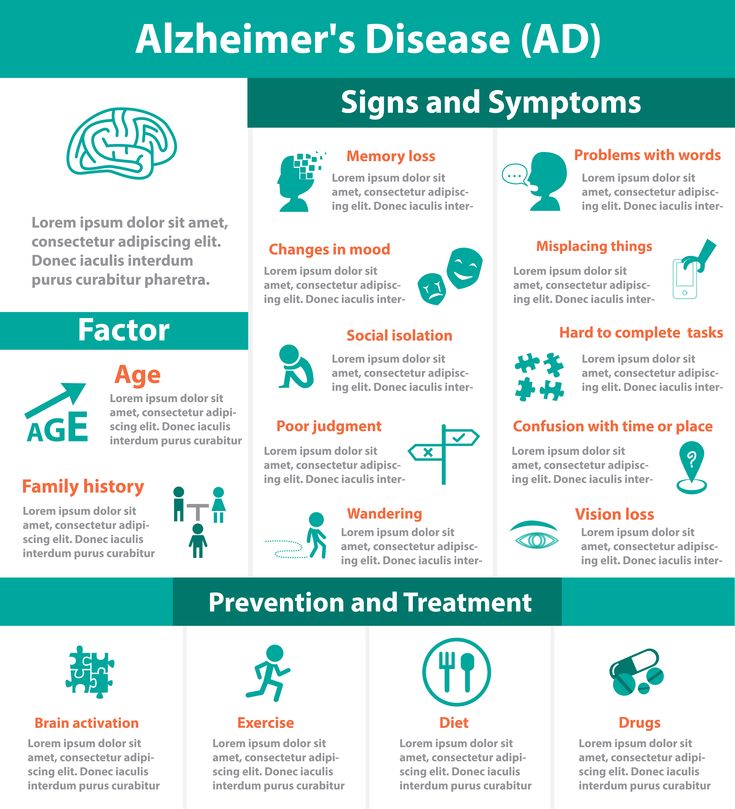
Treatment
Drugs
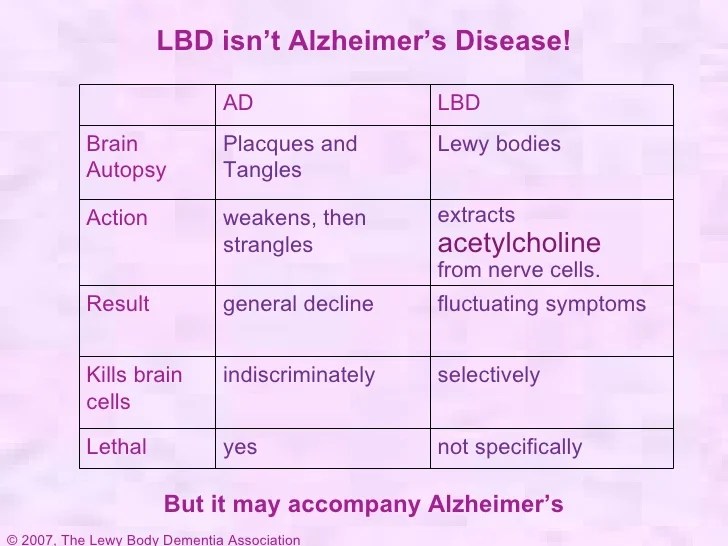
Current Alzheimer's medications can help for a time with memory symptoms and other cognitive changes. Two types of drugs are currently used to treat cognitive symptoms:
-
Cholinesterase inhibitors.
 These drugs work by boosting levels of cell-to-cell communication by preserving a chemical messenger that is depleted in the brain by Alzheimer's disease. These are usually the first medications tried, and most people see modest improvements in symptoms.
These drugs work by boosting levels of cell-to-cell communication by preserving a chemical messenger that is depleted in the brain by Alzheimer's disease. These are usually the first medications tried, and most people see modest improvements in symptoms.Cholinesterase inhibitors may also improve neuropsychiatric symptoms, such as agitation or depression. Commonly prescribed cholinesterase inhibitors include donepezil (Aricept), galantamine (Razadyne ER) and rivastigmine (Exelon).
The main side effects of these drugs include diarrhea, nausea, loss of appetite and sleep disturbances. In people with certain heart disorders, serious side effects may include cardiac arrhythmia.
- Memantine (Namenda). This drug works in another brain cell communication network and slows the progression of symptoms with moderate to severe Alzheimer's disease. It's sometimes used in combination with a cholinesterase inhibitor. Relatively rare side effects include dizziness and confusion.
In June 2021, the Food and Drug Administration (FDA) approved aducanumab (Aduhelm) for the treatment of some cases of Alzheimer's disease. This is the first drug approved in the United States to treat the underlying cause of Alzheimer's by targeting and removing amyloid plaques in the brain. The FDA approved the drug on the condition that further studies be conducted to confirm the drug's benefit. Experts also need to identify which patients may benefit from the drug.
Sometimes other medications such as antidepressants may be prescribed to help control the behavioral symptoms associated with Alzheimer's disease.
Creating a safe and supportive environment
Adapting the living situation to the needs of a person with Alzheimer's disease is an important part of any treatment plan. For someone with Alzheimer's, establishing and strengthening routine habits and minimizing memory-demanding tasks can make life much easier.
You can take these steps to support a person's sense of well-being and continued ability to function:
- Always keep keys, wallets, mobile phones and other valuables in the same place at home, so they don't become lost.
- Keep medications in a secure location. Use a daily checklist to keep track of dosages.
- Arrange for finances to be on automatic payment and automatic deposit.
- Have the person with Alzheimer's carry a mobile phone with location capability so that a caregiver can track its location. Program important phone numbers into the phone.
- Install alarm sensors on doors and windows.
- Make sure regular appointments are on the same day at the same time as much as possible.
- Use a calendar or whiteboard in the home to track daily schedules. Build the habit of checking off completed items.
- Remove excess furniture, clutter and throw rugs.
- Install sturdy handrails on stairways and in bathrooms.
- Ensure that shoes and slippers are comfortable and provide good traction.
- Reduce the number of mirrors. People with Alzheimer's may find images in mirrors confusing or frightening.
- Make sure that the person with Alzheimer's carries identification or wears a medical alert bracelet.
- Keep photographs and other meaningful objects around the house.
More Information
- Alzheimer's disease care at Mayo Clinic
- Alzheimer's drugs
- Alzheimer's: New treatments
- Alzheimer's nose spray: New Alzheimer's treatment?
- Video: Alzheimer's drug shows early promise
Request an Appointment at Mayo Clinic
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Alternative medicine
Various herbal remedies, vitamins and other supplements are widely promoted as preparations that may support cognitive health or prevent or delay Alzheimer's.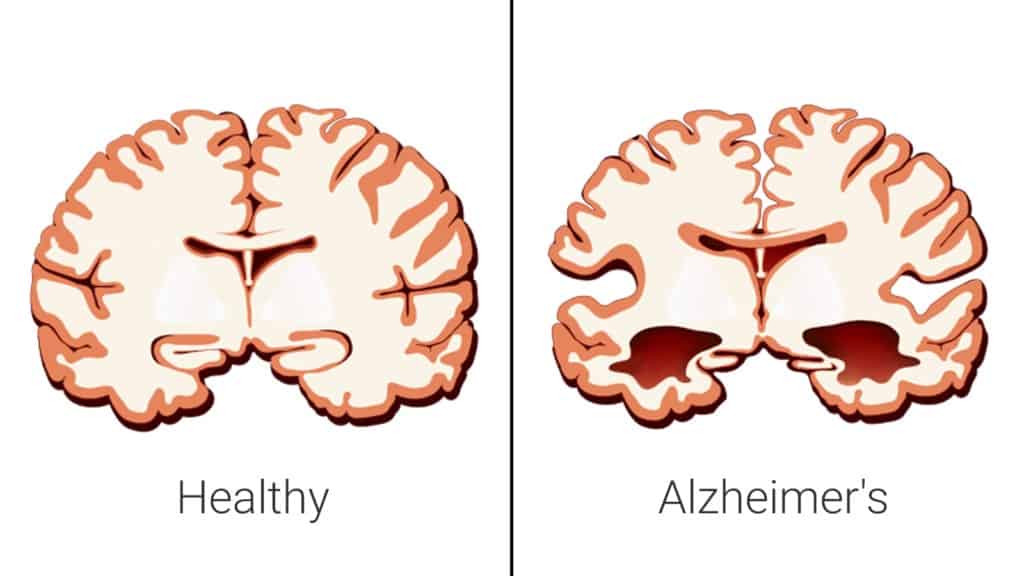 Clinical trials have produced mixed results with little evidence to support them as effective treatments.
Clinical trials have produced mixed results with little evidence to support them as effective treatments.
Some of the treatments that have been studied recently include:
-
Vitamin E. Although vitamin E doesn't prevent Alzheimer's, taking 2,000 international units daily may help delay the progression in people who already have mild to moderate disease. However, study results have been mixed, with only some showing modest benefits. Further research into the safety of 2,000 international units daily of vitamin E in a dementia population will be needed before it can be routinely recommended.
Supplements promoted for cognitive health can interact with medications you're taking for Alzheimer's disease or other health conditions. Work closely with your health care team to create a safe treatment plan with any prescriptions, over-the-counter medications or dietary supplements.
- Omega-3 fatty acids. Omega-3 fatty acids in fish or from supplements may lower the risk of developing dementia, but clinical studies have shown no benefit for treating Alzheimer's disease symptoms.

- Curcumin. This herb comes from turmeric and has anti-inflammatory and antioxidant properties that might affect chemical processes in the brain. So far, clinical trials have found no benefit for treating Alzheimer's disease.
- Ginkgo. Ginkgo is a plant extract containing several medicinal properties. A large study funded by the National Institutes of Health found no effect in preventing or delaying Alzheimer's disease.
- Melatonin. This supplement of a hormone that regulates sleep is being studied to determine if it offers benefits managing sleep in people with dementia. But some research has indicated that melatonin may worsen mood in some people with dementia. More research is needed.
Lifestyle and home remedies
Healthy lifestyle choices promote good overall health and may play a role in maintaining cognitive health.
Exercise
Regular exercise is an important part of a treatment plan.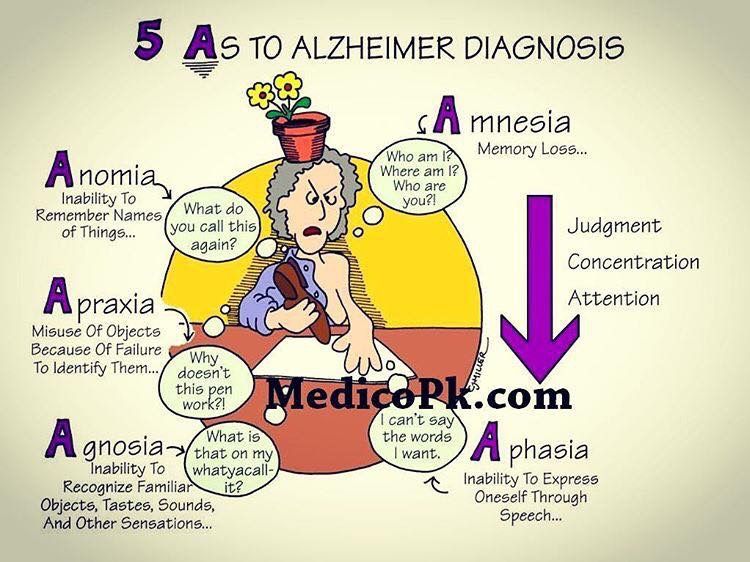 Activities such as a daily walk can help improve mood and maintain the health of joints, muscles and the heart. Exercise can also promote restful sleep and prevent constipation — and it's beneficial for care partners, too.
Activities such as a daily walk can help improve mood and maintain the health of joints, muscles and the heart. Exercise can also promote restful sleep and prevent constipation — and it's beneficial for care partners, too.
People with Alzheimer's who develop trouble walking may still be able to use a stationary bike, stretch with elastic bands or participate in chair exercises. You may find exercise programs geared to older adults on TV or on DVDs.
Nutrition
People with Alzheimer's may forget to eat, lose interest in preparing meals or not eat a healthy combination of foods. They may also forget to drink enough, leading to dehydration and constipation.
Offer the following:
- Healthy options. Buy favorite healthy food options that are easy to eat.
- Water and other healthy beverages. Encourage drinking several glasses of liquids every day. Avoid beverages with caffeine, which can increase restlessness, interfere with sleep and trigger a frequent need to urinate.
- High-calorie, healthy shakes and smoothies. Supplement milkshakes with protein powders or make smoothies featuring favorite ingredients, especially when eating becomes more difficult.
Social engagement and activities
Social interactions and activities can support the abilities and skills that are preserved. Doing things that are meaningful and enjoyable are important for the overall well-being of a person with Alzheimer's disease. These might include:
- Listening to music or dancing
- Reading or listening to books
- Gardening or crafts
- Social events at senior or memory care centers
- Planned activities with children
Coping and support
People with Alzheimer's disease experience a mixture of emotions — confusion, frustration, anger, fear, uncertainty, grief and depression.
If you're caring for someone with Alzheimer's, you can help them cope with the disease by being there to listen, reassuring the person that life can still be enjoyed, providing support, and doing your best to help the person retain dignity and self-respect.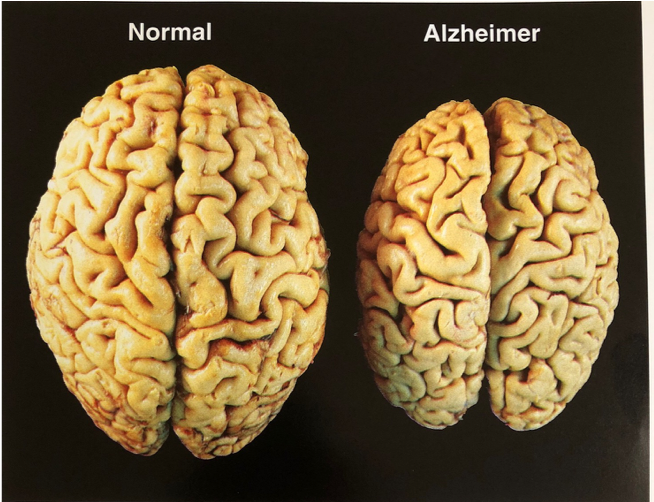
A calm and stable home environment can help reduce behavior problems. New situations, noise, large groups of people, being rushed or pressed to remember, or being asked to do complicated tasks can cause anxiety. As a person with Alzheimer's becomes upset, the ability to think clearly declines even more.
Caring for the caregiver
Caring for a person with Alzheimer's disease is physically and emotionally demanding. Feelings of anger and guilt, stress and discouragement, worry and grief, and social isolation are common.
Caregiving can even take a toll on the caregiver's physical health. Paying attention to your own needs and well-being is one of the most important things you can do for yourself and for the person with Alzheimer's.
If you're a caregiver for someone with Alzheimer's, you can help yourself by:
- Learning as much about the disease as you can
- Asking questions of doctors, social workers and others involved in the care of your loved one
- Calling on friends or other family members for help when you need it
- Taking a break every day
- Spending time with your friends
- Taking care of your health by seeing your own doctors on schedule, eating healthy meals and getting exercise
- Joining a support group
- Making use of a local adult day center, if possible
Many people with Alzheimer's and their families benefit from counseling or local support services.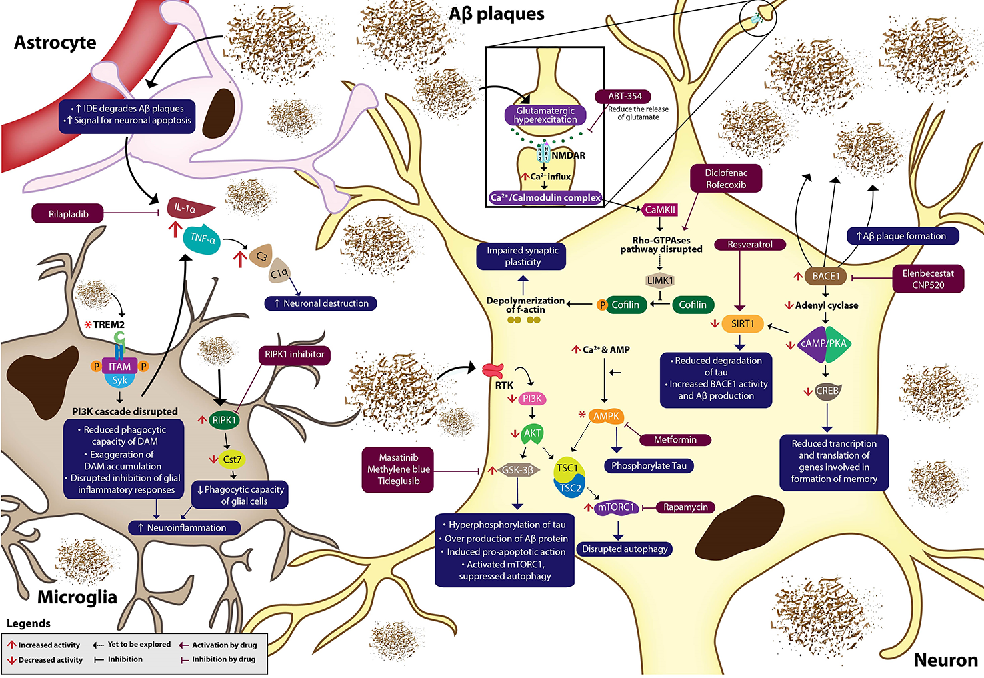 Contact your local Alzheimer's Association affiliate to connect with support groups, doctors, occupational therapists, resources and referrals, home care agencies, residential care facilities, a telephone help line, and educational seminars.
Contact your local Alzheimer's Association affiliate to connect with support groups, doctors, occupational therapists, resources and referrals, home care agencies, residential care facilities, a telephone help line, and educational seminars.
Preparing for your appointment
Medical care for the loss of memory or other thinking skills usually requires a team or partner strategy. If you're worried about memory loss or related symptoms, ask a close relative or friend to go with you to a doctor's appointment. In addition to providing support, your partner can provide help in answering questions.
If you're going with someone to a doctor's appointment, your role may be to provide some history or your thoughts on changes you have seen. This teamwork is an important part of medical care for initial appointments and throughout a treatment plan.
Your primary care doctor may refer you to a neurologist, psychiatrist, neuropsychologist or other specialist for further evaluation.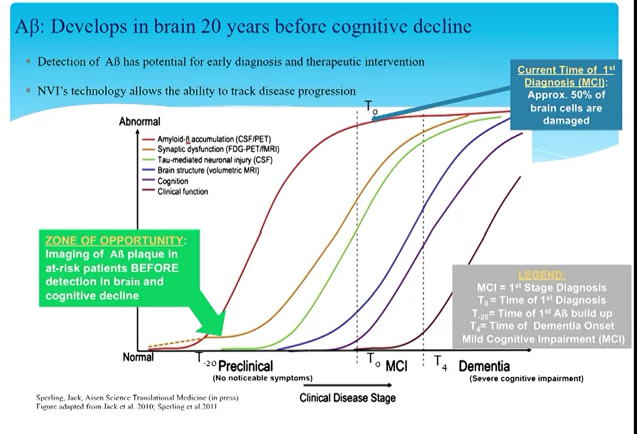
What you can do
You can prepare for your appointment by writing down as much information as possible to share. Information may include:
- Medical history, including any past or current diagnoses and family medical history
- Medical team, including the name and contact information of any current physician, mental health professional or therapist
- Medications, including prescriptions, over-the-counter drugs, vitamins, herbal medications or other dietary supplements
- Symptoms, including specific examples of changes in memory or thinking skills
What to expect from your doctor
Your doctor will likely ask a number of the following questions to understand changes in memory or other thinking skills. If you are accompanying someone to an appointment, be prepared to provide your perspective as needed. Your doctor may ask:
- What kinds of memory difficulties and mental lapses are you having? When did you first notice them?
- Are they steadily getting worse, or are they sometimes better and sometimes worse?
- Have you stopped doing certain activities, such as managing finances or shopping, because these activities were too mentally challenging?
- How is your mood? Do you feel depressed, sadder or more anxious than usual?
- Have you gotten lost lately on a driving route or in a situation that's usually familiar to you?
- Has anyone expressed unusual concern about your driving?
- Have you noticed any changes in the way you tend to react to people or events?
- Do you have more energy than usual, less than usual or about the same?
- What medications are you taking? Are you taking any vitamins or supplements?
- Do you drink alcohol? How much?
- Have you noticed any trembling or trouble walking?
- Are you having any trouble remembering your medical appointments or when to take your medication?
- Have you had your hearing and vision tested recently?
- Did anyone else in your family ever have memory trouble? Was anyone ever diagnosed with Alzheimer's disease or dementia?
- Do you act out your dreams while sleeping (punch, flail, shout, scream)? Do you snore?
By Mayo Clinic Staff
How Is Alzheimer's Disease Diagnosed?
Symptoms and Diagnosis of Alzheimer’s Disease
Doctors use several methods and tools to help determine if a person with thinking or memory problems has Alzheimer’s disease.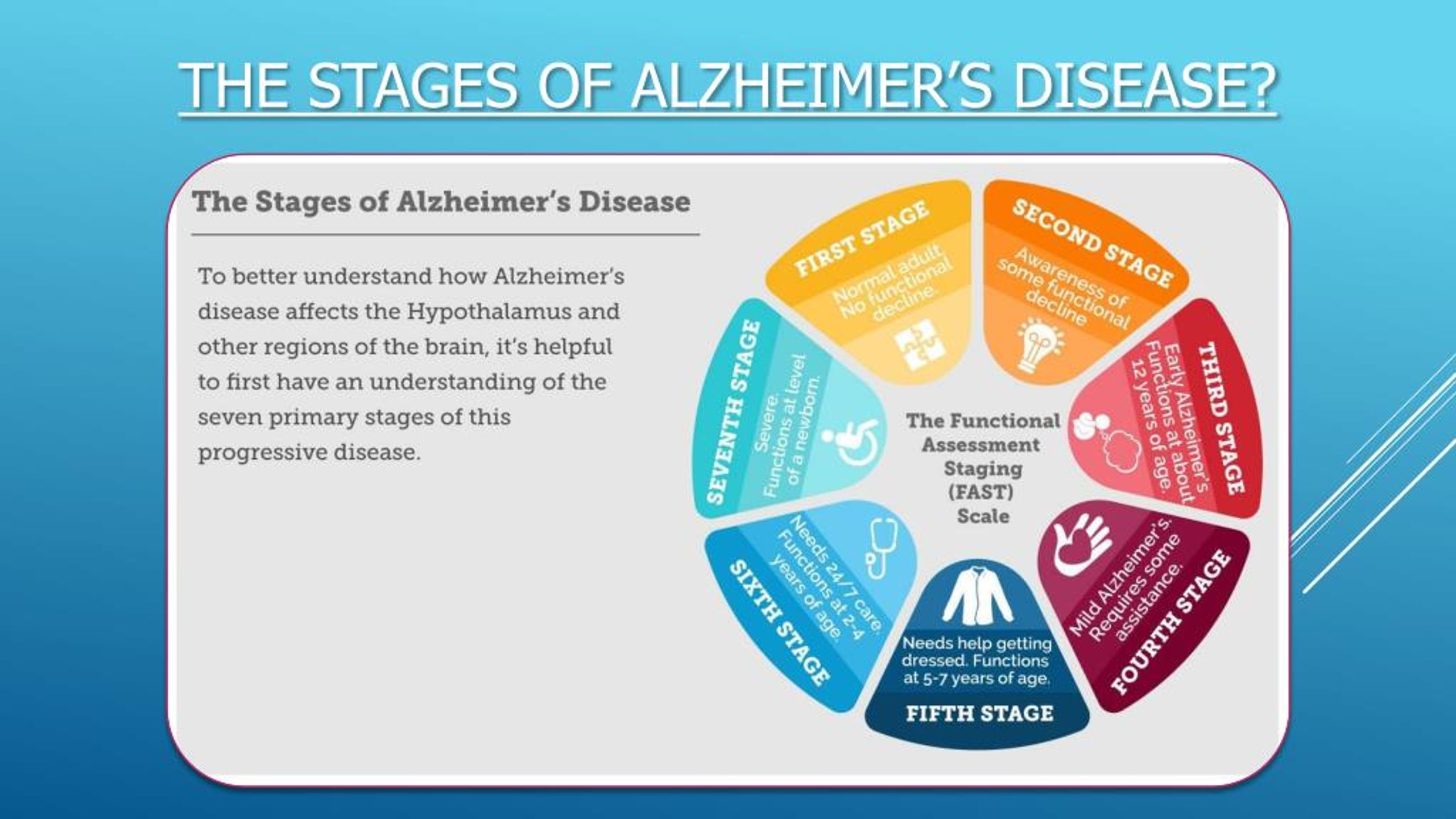 To diagnose Alzheimer’s, doctors may:
To diagnose Alzheimer’s, doctors may:
- Ask the person experiencing symptoms, as well as a family member or friend, questions about overall health, use of prescription and over-the-counter medicines, diet, past medical problems, ability to carry out daily activities, and changes in behavior and personality.
- Administer a psychiatric evaluation to determine if depression or another mental health condition is causing or contributing to a person's symptoms.
- Conduct tests of memory, problem solving, attention, counting, and language.
- Order blood, urine, and other standard medical tests that can help identify other possible causes of the problem.
- Perform brain scans, such as computed tomography (CT), magnetic resonance imaging (MRI), or positron emission tomography (PET), to support an Alzheimer’s diagnosis or rule out other possible causes for symptoms.
Doctors may want to repeat these tests to help best determine how the person’s memory and other cognitive functions are changing over time. The tests can also help diagnose other causes of memory problems, such as stroke, tumor, Parkinson’s disease, sleep disturbances, side effects of medication, an infection, or another type of dementia. Some of these conditions may be treatable and possibly reversible.
The tests can also help diagnose other causes of memory problems, such as stroke, tumor, Parkinson’s disease, sleep disturbances, side effects of medication, an infection, or another type of dementia. Some of these conditions may be treatable and possibly reversible.
People with memory problems should return to the doctor every six to 12 months.
Before the early 2000s, the only sure way to know whether a person had Alzheimer’s disease was through autopsy, a procedure that is performed after death. Thanks to advances in research, lab and imaging tests are now available to help a doctor or researcher see biological signs of the disease, or biomarkers, in a living person. For example, it is now possible for doctors to order a blood test to measure levels of beta-amyloid, a protein that accumulates abnormally in the brains of people with Alzheimer’s. Several other blood tests are in development. However, the availability of these diagnostic tests is still limited. NIA-supported research teams continue to study options for faster, less-expensive, and less-invasive ways to diagnose Alzheimer’s.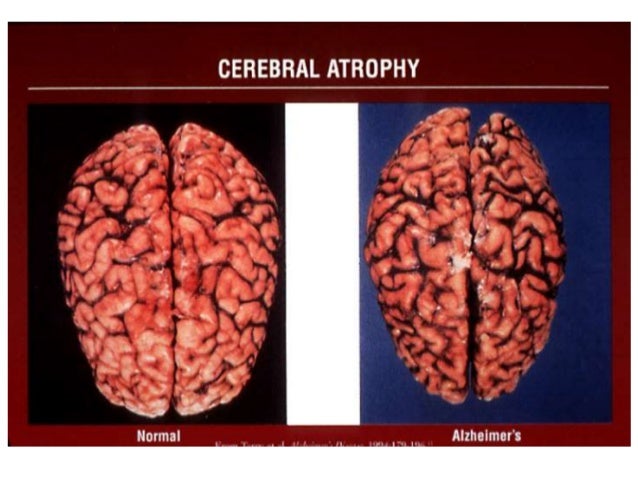
Learn more about biomarkers and Alzheimer’s detection and research.
What happens if a doctor thinks it's Alzheimer's disease?
If a primary care doctor suspects Alzheimer’s, he or she may refer the patient to a specialist who can provide a detailed diagnosis or further assessment. Specialists include:
- Geriatricians, who manage health care in older adults and know how the body changes as it ages and whether symptoms indicate a serious problem.
- Geriatric psychiatrists, who specialize in the mental and emotional problems of older adults and can assess memory and thinking problems.
- Neurologists, who specialize in abnormalities of the brain and central nervous system and can conduct and review brain scans.
- Neuropsychologists, who can conduct tests of memory and thinking.
Memory clinics and centers, including Alzheimer’s Disease Research Centers, offer teams of specialists who work together to diagnose the problem. In addition, these specialty clinics or centers often have access to the equipment needed for brain scans and other advanced diagnostic tests.
What are the benefits of an early Alzheimer's diagnosis?
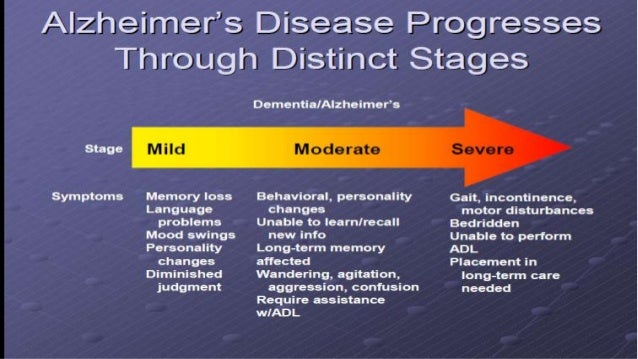
Alzheimer’s disease slowly worsens over time. People living with this disease progress at different rates, from mild Alzheimer’s, when they first notice symptoms, to severe, when they are completely dependent on others for care.
Early, accurate diagnosis is beneficial for several reasons. While there is no cure, there are several medicines available to treat Alzheimer’s, along with coping strategies to manage behavioral symptoms. Beginning treatment early in the disease process may help preserve daily functioning for some time. Most medicines work best for people in the early or middle stages of the disease. Learn more about Alzheimer’s medications.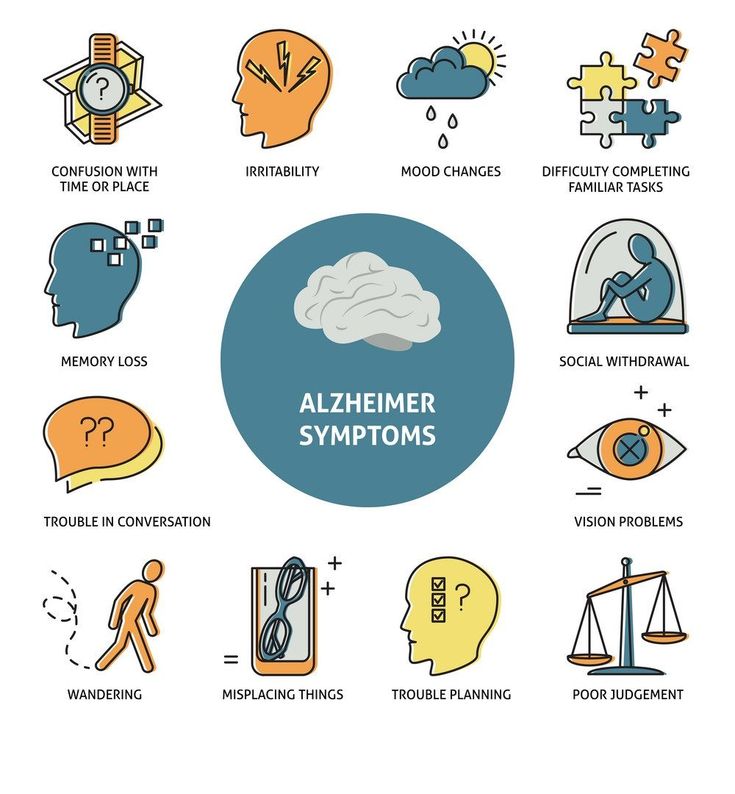
In addition, having an early diagnosis helps people with Alzheimer’s and their families:
- Plan for the future
- Take care of financial and legal matters
- Address potential safety issues
- Learn about living arrangements
- Develop support networks
An early diagnosis also provides people with more opportunities to participate in clinical trials or other research studies testing possible new treatments for Alzheimer’s.
For more information about Alzheimer's
NIA Alzheimer’s and related Dementias Education and Referral (ADEAR) Center
800-438-4380
[email protected]
www.nia.nih.gov/alzheimers
The NIA ADEAR Center offers information and free print publications about Alzheimer’s and related dementias for families, caregivers, and health professionals. ADEAR Center staff answer telephone, email, and written requests and make referrals to local and national resources.
Alzheimers.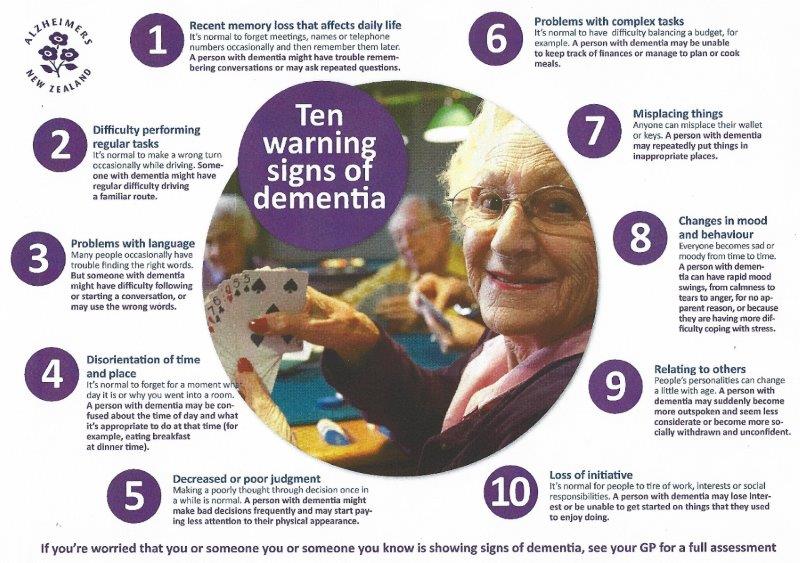 gov
gov
www.alzheimers.gov
Explore the Alzheimers.gov portal for information and resources on Alzheimer’s and related dementias from across the federal government.
Eldercare Locator
800-677-1116
[email protected]
https://eldercare.acl.gov
MedlinePlus
National Library of Medicine
www.medlineplus.gov
This content is provided by the NIH National Institute on Aging (NIA). NIA scientists and other experts review this content to ensure it is accurate and up to date.
Content reviewed: September 09, 2021
Related Articles
Alzheimer's disease: symptoms, stages, prevention and treatment, symptoms, diagnosis and treatment | Alpha
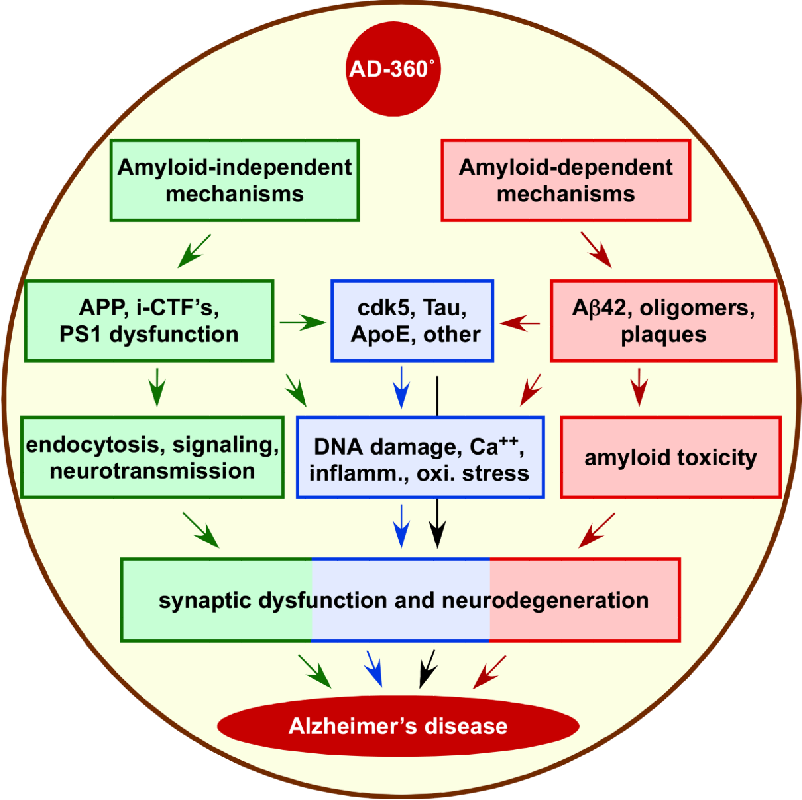
Alzheimer's disease is a neurodegenerative pathology with progressive senile dementia. It is characterized by the development of cognitive disorders, dementia. Neurological disorders in Alzheimer's disease are caused by the formation of insoluble rigid amyloid proteins (senile plaques) that envelop and destroy functional brain cells.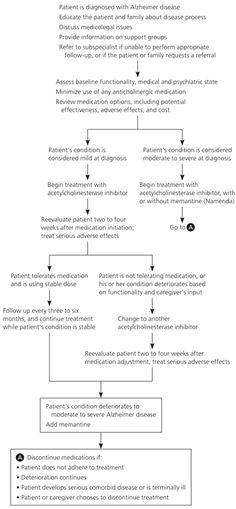 Gradually, the process spreads, captures new areas.
Gradually, the process spreads, captures new areas.
Modern medicine can only offer palliative care. Complex therapy and proper care can significantly slow down the destructive processes, increase the duration and maintain the quality of life of patients with Alzheimer's disease.
Causes of disease
According to statistics, the symptoms of Alzheimer's disease develop in 5-8 people per 1000 population. Every second case of dementia is caused by this pathology. In the last decade, there has been an increase in the incidence, but doctors still find it difficult to name the exact causes of neurodegenerative processes. An increase in risk has been proven in the age group over 65 years. After 9By 5 years, almost 70% of older people develop characteristic symptoms. Women get sick more often than men, but this may be due to their higher life expectancy, especially in European countries.
Most experts agree that the main factor triggering neurodegenerative processes is the natural aging of the body. The slowdown of metabolic processes contributes to the accumulation of amyloids.
The slowdown of metabolic processes contributes to the accumulation of amyloids.
Genetic studies have proven a hereditary predisposition to Alzheimer's disease. Mutations in several chromosomes lead to disruption of protein metabolism in cerebral tissues. Genetics most often causes the early debut of the disease, when the first signs of dementia appear at the age of 30-40 years.
The following factors can accelerate the development of pathology:
- Poor nutrition.
- Living in areas with poor ecology.
- Bad habits.
- Chemical poisoning, heavy metals.
- Chronic stress.
- Past neuroinfections: meningitis, encephalitis.
- Tumors of the brain.
Symptoms of Alzheimer's disease
Pathology is characterized by a long and subtle onset. In the early stages, Alzheimer's disease may not have any symptoms at all. Plaques begin to form in the brain tissues several years before the first manifestations.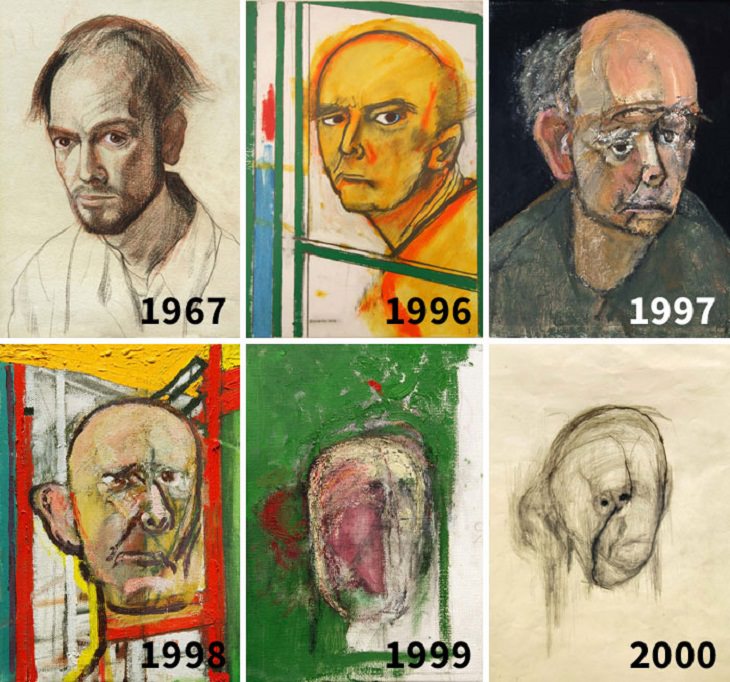
As the area of the lesion increases, the first nervous disorders are observed:
- Decreased memory and attention.
- Violation of orientation in space and time.
- Difficulty in building logical chains.
A person becomes distracted, forgetful, for example, often loses keys or forgets where he put the phone. It is difficult for the patient to master new activities; in speech, he begins to pause in order to find the right words. The progression of the pathology is steady, without periods of remission.
There are four stages of Alzheimer's disease according to the severity of symptoms:
- Prementation. The initial form of pathology. Changes in the patient's condition can only be noticed by close people or a doctor during neurocognitive testing. The predementia stage can last up to 8 years. Of the main symptoms, there is usually a disorder of short-term memory, absent-mindedness, difficulty planning activities.
 Alzheimer's disease in the elderly in the first manifestations is always accompanied by detachment, apathy - this is one of the typical signs.
Alzheimer's disease in the elderly in the first manifestations is always accompanied by detachment, apathy - this is one of the typical signs. - Early dementia. Memory loss is progressive. Changes in the patient's behavior are strongly pronounced, and it is no longer possible to attribute them to old age. A person remembers well the events of many years ago, but he cannot always say whether he dined today or not yet. Disorders of hearing, vision, tactile perception develop. In early dementia, speech impairment is possible. The patient's vocabulary is significantly reduced, he cannot understand some new expressions. Doing things that require fine motor skills takes longer than usual. It is difficult for a person to thread a needle, fasten buttons on clothes, or write anything.
- Moderate dementia. It is difficult for the patient to carry out daily activities. A person becomes slovenly, poorly combed, he may not notice the mess in the room. Memory and spatial orientation are impaired - older people with moderate dementia are often lost.
 It is difficult for the patient to remember his name, name the address or say which side he came from. Neuropsychiatric symptoms intensify: a person becomes irritable, whiny, aggressive. Many patients resist caring for them and show a tendency to wander. Writing and reading skills are almost completely lost. Possibly urinary incontinence.
It is difficult for the patient to remember his name, name the address or say which side he came from. Neuropsychiatric symptoms intensify: a person becomes irritable, whiny, aggressive. Many patients resist caring for them and show a tendency to wander. Writing and reading skills are almost completely lost. Possibly urinary incontinence. - Severe dementia. The patient is incapable of self-care. He needs help to get dressed, wash, eat. Speech is limited to a few words or sounds. Many patients in the stage of severe dementia can still maintain contact with loved ones and perceive the environment, but complete apathy gradually sets in. The patient stops moving, does not recognize relatives. Muscles atrophy, there are complications of immobility, which usually become the cause of death.
Alzheimer's diagnostics
Patients are not always able to notice and understand changes in their body, so relatives need to bring a loved one to the doctor at the first manifestations of pathology.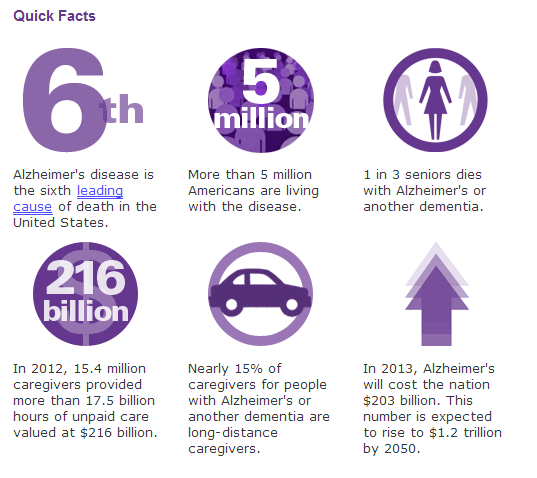 Alzheimer's disease is diagnosed by a neurologist. During the examination, he determines the level of the patient's reflexes, conducts a series of tests to assess cognitive functions, establishes an anamnesis, the presence of provoking factors.
Alzheimer's disease is diagnosed by a neurologist. During the examination, he determines the level of the patient's reflexes, conducts a series of tests to assess cognitive functions, establishes an anamnesis, the presence of provoking factors.
The complex of surveys includes:
- General blood analysis. The results provide information about the presence of concomitant diseases, inflammatory processes in the body. It is recommended to do a detailed clinical analysis for the content of folic acid and vitamin B12.
- Biochemical blood test. Dementia can be caused not only by Alzheimer's disease, but also by a number of endocrine disorders, thyroid dysfunction.
- Blood test for HIV, syphilis, other infections. The pathogen in the body worsens the patient's condition, accelerates the course of neurodegenerative processes.
- Electroencephalography (EEG). The essence of Alzheimer's disease is the destruction of neurons and impaired conduction of nerve impulses.
 The EEG will show diffuse slowing of the signal.
The EEG will show diffuse slowing of the signal. - Computed or magnetic resonance imaging. The pictures show areas of atrophy of the cerebral cortex, senile plaques. According to the results of MRI, differential diagnosis of such pathologies as hematomas, neoplasms, and strokes is carried out.
- Liquor analysis. In Alzheimer's disease, an increased content of amyloid is determined.
- Genetic analysis. The presence of a mutation in the ApoE gene, the defect of which causes dementia, is detected.
Treatment of Alzheimer's disease
Drug treatment
The doctor prescribes symptomatic therapy. It is important to alleviate the patient's condition as much as possible, to help him retain memory and attention longer, to increase life expectancy.
Drug treatments for Alzheimer's disease include:
- Cholinesterase inhibitors: rivastigmine, donepezil, gaoantamine.
- NMDA-glutamate receptor blockers: akatinol-memantine.

Drugs are included in the list of vital drugs, their purchase is financed from the budget. When prescribed at an early and middle stage, drugs help to stop the development of the disease.
For the treatment of concomitant disorders, the doctor prescribes antipsychotics, antidepressants,
Social rehabilitation
It is important to maintain the habitual way of life of the patient as long as possible. Intellectual regression will be steady, but doing what you love and hanging out with friends helps slow it down. A person with Alzheimer's disease often lives "in the past", so relatives are advised to discuss current events with him as much as possible, to remind him of some facts. If the patient was painting or playing a musical instrument before the diagnosis, let him continue. Active intellectual activity and movement stimulate the formation of new connections between neurons, use brain reserves, which helps to resist dementia.
In many large cities "schools for relatives" are open.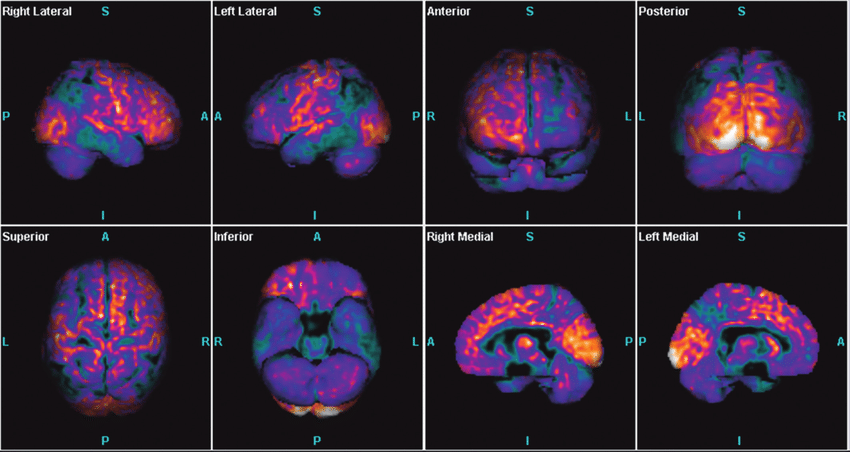 The essence of the classes is largely reduced to psychological support, but as part of the training they provide a lot of valuable information on caring for people with Alzheimer's disease. The attention of relatives is an important aspect of the social rehabilitation of each patient.
The essence of the classes is largely reduced to psychological support, but as part of the training they provide a lot of valuable information on caring for people with Alzheimer's disease. The attention of relatives is an important aspect of the social rehabilitation of each patient.
Some tips for caring for someone with dementia:
- As memory deteriorates, teach the patient to use simple paper notes. Everything in the room must be signed. Post detailed instructions for daily tasks, lists with meal times, and more in prominent places.
- Set a clear daily routine. Breakfast, lunch, dinner, hygiene procedures - everything should be done at the same time. This contributes to the formation of "muscle" memory when a person acts automatically.
- Find something for the patient to do. Many elderly people like to knit, read newspapers, and do crossword puzzles.
- Remain calm in communication. You can not scream at the patient, swear, use physical force.
 With severe dementia, the character and personality of a person change greatly, but he does not behave this way on purpose, but because of his illness.
With severe dementia, the character and personality of a person change greatly, but he does not behave this way on purpose, but because of his illness. - Let the patient take care of himself as much as possible. It is important for a person to feel his independence, independence. You don't have to do all the household chores for him. The patient can wash the dishes or make up the bed himself, even if it takes twice as long as usual.
- Make the environment safe. It is worth removing cutting and piercing objects from the room, leaving a minimum number of electrical appliances. As Alzheimer's disease progresses, patients tend to act rashly.
An integrated approach to treatment allows patients to maintain a fairly clear mind and the ability to self-service until old age. Life expectancy after diagnosis reaches 14 years or more. Relatives are advised to use the services of specialists, especially in the later stages of Alzheimer's disease. Professional care for a patient in a boarding house or hospice will significantly improve his well-being and allow the family to return to work, to their usual way of life.
Prevention of Alzheimer's disease
It is impossible to predict and prevent neurodegenerative changes in the brain in advance. But you can reduce the risk of their development. It has been proven that people engaged in intellectual work are less likely to suffer from dementia. A good prevention of Alzheimer's disease are special gymnastics, exercises for the mobility of the mind. It is recommended to read books, solve crossword puzzles, engage in scientific activities as far as possible until old age.
Maintaining mental balance is one of the most effective methods of preventing dementia. Stress and nervous strain should be avoided. Physical activity, frequent walks in the fresh air, and proper nutrition help to strengthen overall health.
Diagnosis and treatment of Alzheimer's disease in Nizhny Novgorod
The doctors of the Alfa Health Center clinic have extensive experience in treating patients with dementia. We have modern equipment for diagnosing Alzheimer's disease, conduct medical procedures, and work with relatives of patients. Call us to make an appointment with a doctor at a convenient time.
Call us to make an appointment with a doctor at a convenient time.
Alzheimer's disease: causes, diagnosis, treatment
Views: 17681 Published: / Updated:
- hereditary diseases
General
Alzheimer's disease is a form of dementia or dementia that cannot be reversed. The disease is accompanied by a progressive loss of memory, a decrease in intellectual abilities, a deterioration in language and speech skills. All these symptoms together lead to a change in human behavior and a decrease in the quality of his life, the result is complete social maladaptation.
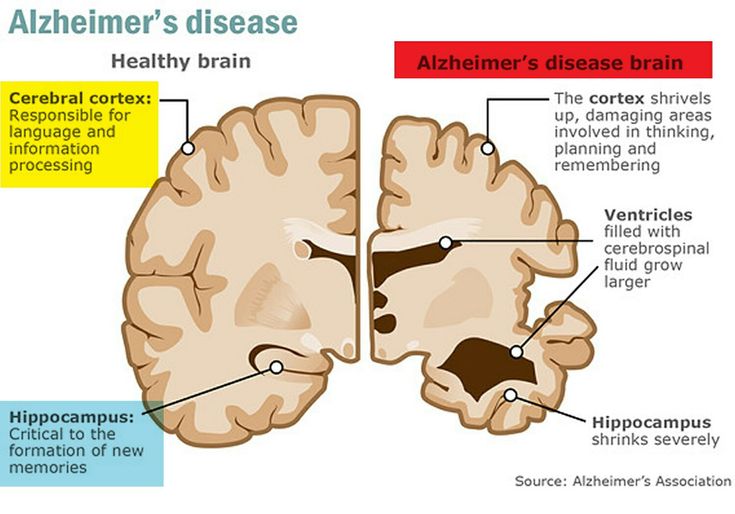
In Alzheimer's disease, damage to brain tissue is primary. The pathological process is associated with the accumulation of amyloid protein in the interstitial substance of the brain and the formation of senile plaques, tau protein in the cells of the nervous tissue and the formation of typical structures called neurofibrillary tangles.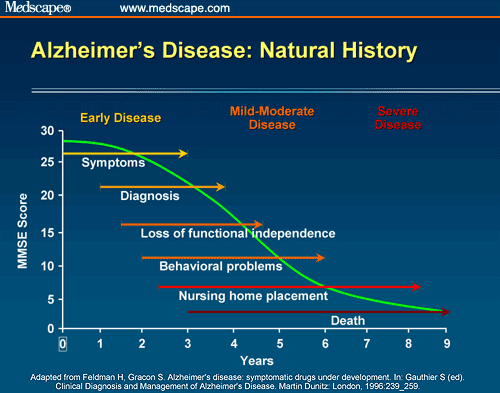 The formation of pathological structures leads to damage and death of nerve cells, a decrease in the level of neurotransmitters, and a deterioration in the interaction between brain regions.
The formation of pathological structures leads to damage and death of nerve cells, a decrease in the level of neurotransmitters, and a deterioration in the interaction between brain regions.
Alzheimer's disease begins with minor memory problems as the temporal cortex is the first to be affected. A person forgets where he put the thing, what this cutlery is for, what he went to the store for, what time he should come to work, etc. A person may not remember the date of birth, his address of residence, the names of his own children, he may get lost in simple questions, for example, what day it is, what time it is, where and by whom he works. Later, speech disorders join, the patient cannot remember the right word, orientation disorders are observed, the person cannot find his way home.
Disease stages
There are three stages in the course of Alzheimer's disease. At the first stage, the patient can serve himself on his own, at the second stage he cannot do without the help of loved ones.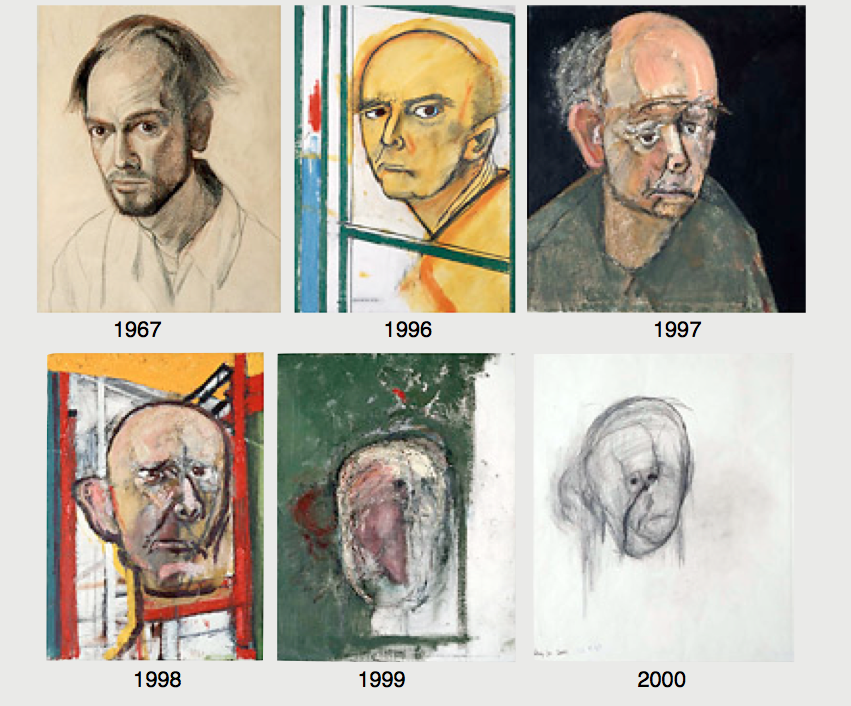 A person cannot dress himself, take a shower, wash dishes, etc. During the third stage, dependence on the presence of a loved one becomes total: the patient cannot perform a single daily action without outside help.
A person cannot dress himself, take a shower, wash dishes, etc. During the third stage, dependence on the presence of a loved one becomes total: the patient cannot perform a single daily action without outside help.
Disease and age
The risk of Alzheimer's disease and other forms of dementia increases significantly with age. Isolated cases of the disease are observed after 40 years, in people aged 65 years the disease is detected in 10-12%, over the age of 85 in 30-40% of cases.
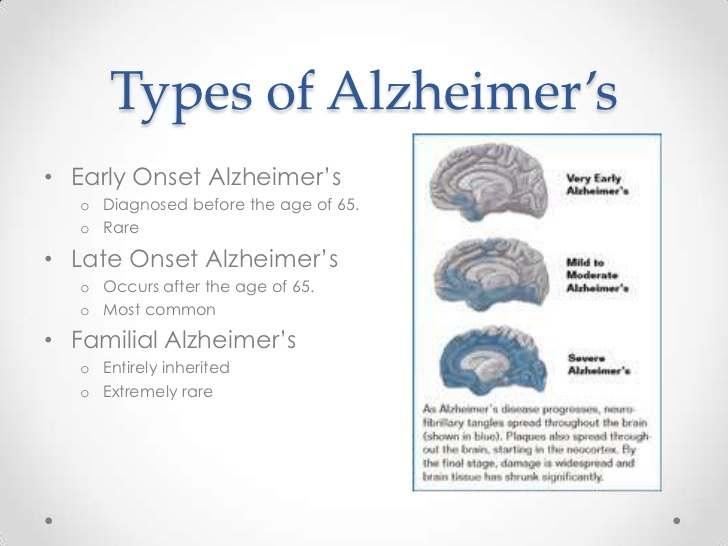
Distinguish between early and late onset Alzheimer's disease. Early onset is manifested by the manifestation of the disease before the age of 65 and is characterized by rapid progression. A number of assumptions have been made about the genetic component of the disease. "Late onset" Alzheimer's disease appears after 65 years of age, is not considered inherited, its course is smoother.
Genetic predisposition
Alzheimer's disease is caused by many factors that are not yet well understood.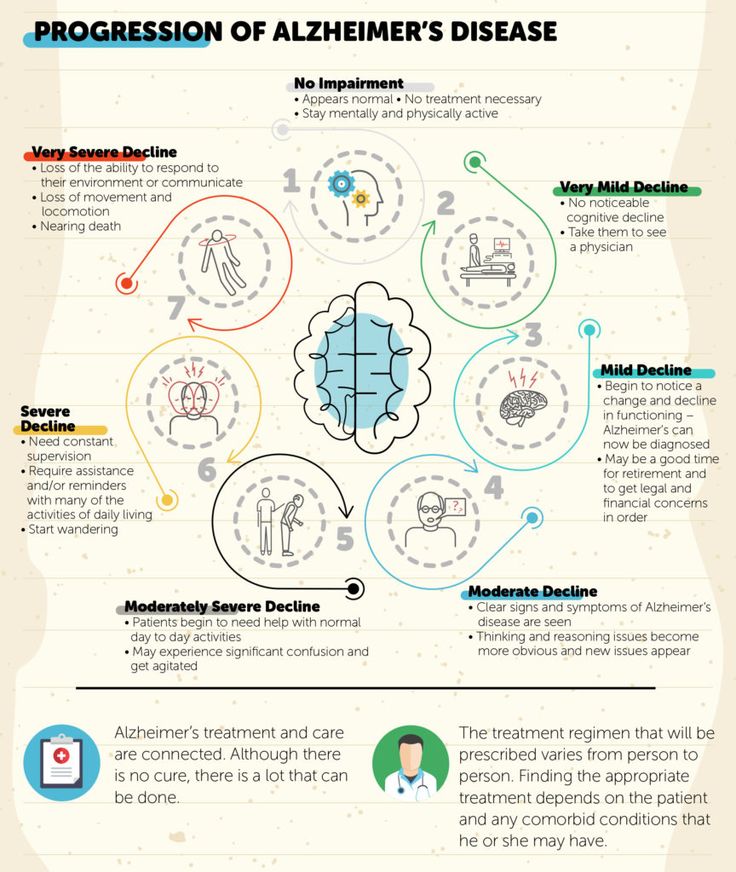 Three genes have been identified, mutations in which are associated with rare early familial forms of the disease. They account for 5% of all cases. Genes PSEN 1 , PSEN 2 and AP, located on chromosomes 14, 1 and 21, are responsible for the synthesis of abnormal protein structures that are the pathomorphological substrate of Alzheimer's disease. There is a 50% chance that the gene mutation will be passed on to each of the children of the carrier of the pathological gene.
Three genes have been identified, mutations in which are associated with rare early familial forms of the disease. They account for 5% of all cases. Genes PSEN 1 , PSEN 2 and AP, located on chromosomes 14, 1 and 21, are responsible for the synthesis of abnormal protein structures that are the pathomorphological substrate of Alzheimer's disease. There is a 50% chance that the gene mutation will be passed on to each of the children of the carrier of the pathological gene.
Other genes are associated with late onset Alzheimer's disease. They are not considered a direct cause of the pathological process, although they may explain why there is an increased risk of developing a late onset in individuals whose families have had cases of the disease. The APOE gene is one of them. The APOE gene is responsible for the production of apolipoprotein E, a lipid (fat and cholesterol) carrier protein in the blood. The APOE gene exists in three different forms (alleles): E 2 , E 3 and E 4 .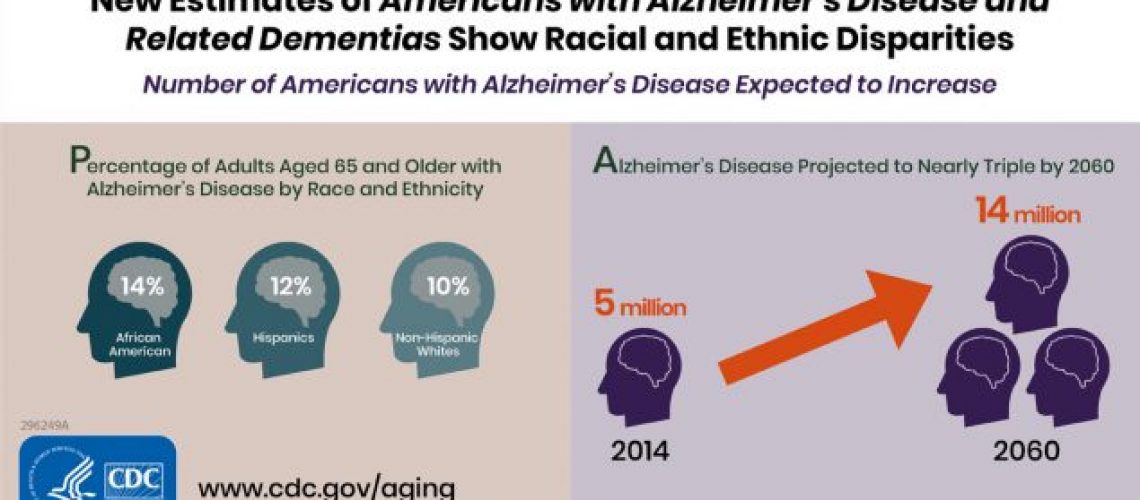 Each person inherits two APOE alleles, which are a combination of these three. E 3 is the most common allele in the population, found in 60% of the general population. The presence of the E 4 APOE allele is associated with the majority of family cases and an increased risk of developing Alzheimer's disease, therefore, it is considered an unfavorable combination prognostically.
Each person inherits two APOE alleles, which are a combination of these three. E 3 is the most common allele in the population, found in 60% of the general population. The presence of the E 4 APOE allele is associated with the majority of family cases and an increased risk of developing Alzheimer's disease, therefore, it is considered an unfavorable combination prognostically.
Risk factors
Along with genetic factors, there are other risk factors for Alzheimer's disease. These include type 2 diabetes and milder forms of insulin resistance, obesity, high blood pressure, dyslipidemia, and high levels of inflammatory markers such as C-reactive protein (CRP).
Diagnostics
An accurate clinical diagnosis of Alzheimer's disease is based on the clinical presentation, using a variety of tests and procedures to rule out other causes of dementia. The doctor evaluates the person's personal and family medical history, and conducts neuropsychological tests to measure memory, language skills, and other cognitive functions.
Imaging tools such as computed tomography (CT) and magnetic resonance imaging (MRI) are often used to look for signs of trauma, tumors, and stroke, as well as brain atrophy seen as the disease progresses.
Unfortunately, there are no laboratory tests to diagnose Alzheimer's disease during life. The only accurate tool to confirm the presence of the disease is a histological examination of a part of the brain after death. Pathologists describe senile plaques and neurofibrillary tangles characteristic of Alzheimer's disease. Because plaque and glomerular formation is also seen in normal aging, the sample is compared with a control sample of normal brain tissue from a person of the same age but without the disease.
New criteria and guidelines for the diagnosis of Alzheimer's disease were developed in 2011. The preclinical, subclinical and clinical stages of the disease have been identified, new criteria for dementia syndrome in Alzheimer's disease have been developed.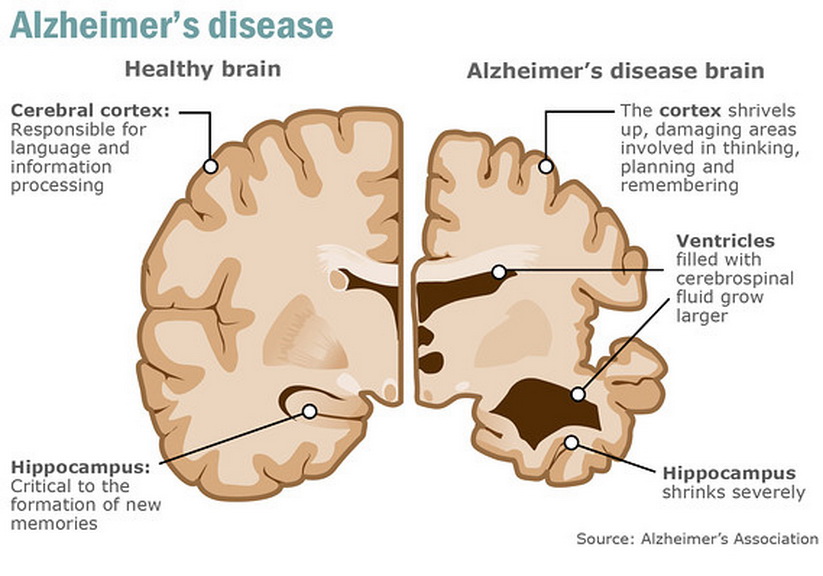
The preclinical stage of Alzheimer's disease is characterized by the absence of cognitive impairment, but amyloid bodies can be detected in the brain. The appearance of biomarkers during neuroimaging is a precursor of dementia 10–15 years before its manifestation. This stage is designed to help guide research towards early diagnosis of the condition.
Moderate cognitive impairment due to Alzheimer's disease - the presence of mild changes in memory and thinking abilities that do not interfere with daily activities.
Dementia in Alzheimer's disease. Memory, thinking, and behavioral symptoms that interfere with a person's ability to function in daily life.
The guidelines are intended to provide more information on the current understanding of Alzheimer's disease and provide a basis for future research.
Treatment
Drug therapy includes the cholinesterase inhibitor group of drugs and antiglutamatergics. Non-drug therapy is aimed at improving cognitive functions and forming neural connections: aerobic physical activity, maintaining an active social life, performing cognitive training.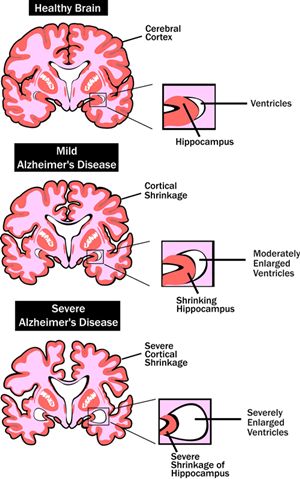
- hereditary diseases
share:
Recommended studies
62.006
Check-up "Diabetes"
can be taken at home
1 295 ₽
1 day
? *The indicated period does not include the day of taking the biomaterial
* Taking biomaterial is paid separately: 200 rub
61.613
Lipid profile, extended
available at home
available CITO
2 805 ₽
1 day
? *The indicated period does not include the day of taking the biomaterial
* Taking biomaterial is paid separately: 200 rub
14.142
C-Reactive Protein, High Sensitivity (HSCRP)
available at home
available CITO
590 ₽
9014 1 day? *The indicated period does not include the day of taking the biomaterial
* Taking biomaterial is paid separately: 200 rub
Similar articles
Aging.