Autism being overdiagnosed
Autism Overdiagnosed
Share on PinterestResearchers say changing criteria has resulted in more people being diagnosed with autism. Getty Images- Researchers say the changing criteria for autism may be resulting in an overdiagnosis of the condition.
- Some experts, however, say that better diagnostic methods are simply recognizing autism in more individuals and at an earlier age.
- Earlier diagnosis allows medical professionals to begin treatments for autism at a younger age.
Autism isn’t what it used to be.
A new study finds that, over time, the differences between individuals diagnosed with autism and those who don’t have autism have decreased.
The researchers say that could mean that more people with less profound symptoms are being diagnosed with the condition.
“The autism category has considerably overextended,” with prevalence rates now 15 times greater than they were a half-century ago, said Laurent Mottron, MD, PhD, DEA, a study author and professor in the department of psychiatry at the University of Montreal, and the chair on cognitive neuroscience in autism.
“Most neurogenetic and child psychiatry disorders that have only a loose resemblance with autism can now be labeled autistic,” he said.
For instance, Mottron said, “you could not [have] ADHD and [autism] before 2013. Now you can.”
He added, while “this is justified in some cases that have both presentations,” it also gives doctors the ability to label someone as having autism who just has “pure” ADHD with “a heavy impact on socialization.”
The findings from the study published in the journal JAMA Psychiatry could indicate that autism is being overdiagnosed.
Or, it could mean that early detection has led to more awareness of the many manifestations of autism, with symptoms ranging from mild to profound.
Either way, “Possible changes in the definition of autism from a narrowly defined and homogenous population toward an inclusive and heterogeneous population may reduce our capacity to build mechanistic models of the condition,” the study concludes.
In other words, the broader definition may make it more challenging to model how the autistic brain works, said Mottron.
He contends that the implications of a broader definition may include loss of specialized knowledge and clinical experience around other conditions now considered forms of autism.
It could also increase strain on available autism services.
Other experts don’t dispute that medical professionals are casting a wider net in diagnosing autism.
But they put a more benign spin on the implications.
“As a clinical psychologist I am less concerned with the narrowing gap and attribute that more to research and awareness associated with the disorder,” Ashley Baker, PsyD, owner of Pavilion Psychological Services in Cummings, Georgia, told Healthline.
“[Healthcare workers] have worked tirelessly to educate communities and parents about early warning signs,” she added. “This leads to early intervention and diagnosis.”
Thomas Frazier, PhD, the chief science officer at Autism Speaks, told Healthline: “Autism is not being overdiagnosed.”
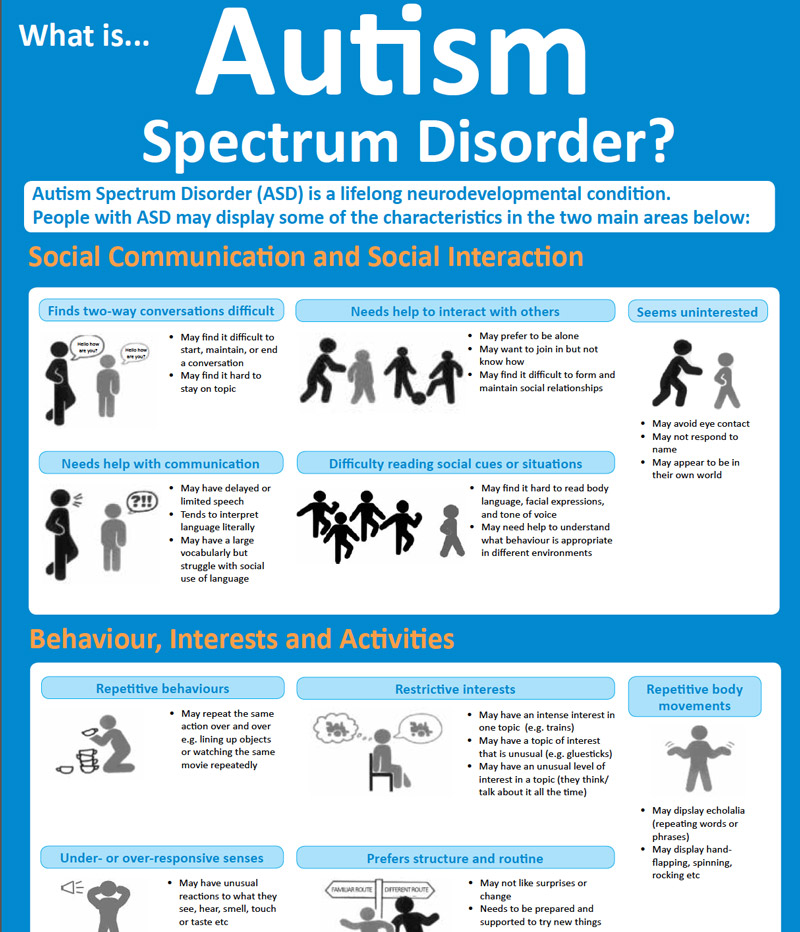
“The core features of autism — social communication and inflexible, repetitive behavior — have remained the same since the beginning,” said Frazier.
He noted that any time a condition has milder cases identified it can cause the difference in the factors that cause the ailment to get smaller.
“It does not mean that the condition is overdiagnosed,” Frazier said. “It just means we are recognizing milder manifestations that still are associated with significant functional challenges.”
Frazier said that recent changes in the diagnostic criteria for autism have been a factor in increasing autism diagnoses.
However, he added, “Rather than diluting the definition of autism, it appropriately reclassified three distinct conditions that share a unique mix of primary symptoms, allowing us to better understand the underlying processes that are involved in these areas.”
“What is most important to understand is that, with more people getting an appropriate diagnosis earlier in life, more people with autism are getting the care and support they need to be successful,” said Frazier.
The studies examined in the meta-anaylsis led by Mottron were published between 1966 and 2019.
During that period, autism prevalence has increased from under 0.05 percent at age 8 in the United States to 1.47 percent, with a lifetime prevalence rate now estimated at more than 2 percent.
Autism was initially identified as a childhood disorder in the 1940s. The diagnostic criteria for autism have been changed several times over the decades.
In 2013, the latest revision of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-5) expanded the definition of autism.
It combined the previously separate diagnoses of autistic disorder, Asperger syndrome, childhood disintegrative disorder, and pervasive developmental disorder-not otherwise specified (PDD-NOS) under the now familiar umbrella of “autism spectrum disorder.”
“People who are diagnosed with autism spectrum disorder still have symptoms and challenges associated with classic autism,” Rebecca Sachs, PhD, a licensed psychologist who specializes in counseling patients with autism, obsessive-compulsive disorder, and anxiety disorders, told Healthline.
Sachs compares the growing diversity of autism diagnoses to those of ADHD, another disorder whose diagnostic criteria have evolved as knowledge and the research base of the condition has expanded.
Yagnesh Vadgama, vice president of Clinical Care Services — Autism at Magellan Health, told Healthline that it’s important to try to understand why autism diagnoses have increased over time while also recognizing that the condition tends to be underdiagnosed in some populations, such as females, minority groups, and lower-income families.
On the one hand, he said, “we’re not seeing enough of the full evaluation” of autism as defined in the DSM-5.
On the other, “Certain populations may be overdiagnosed,” said Vadgama, pointing to a 2016 University of Washington study published in the journal Autism, where a reanalysis of previously diagnosed autism patients determined that about 9 percent shouldn’t have been classified as autistic.
“We need reevaluations in a given time frame,” he said.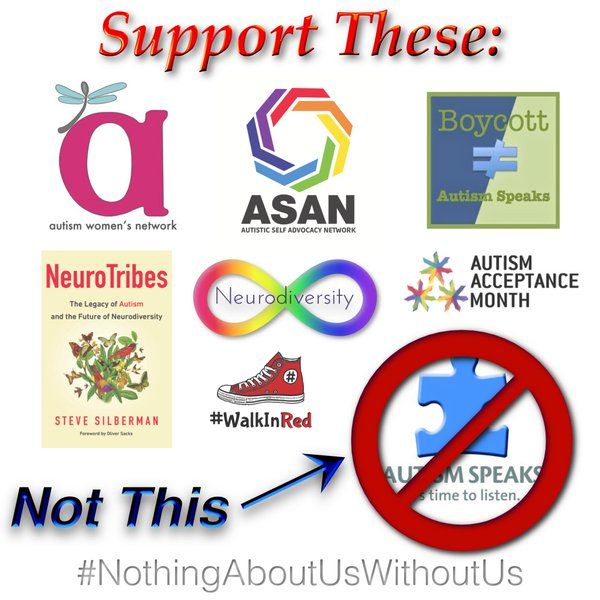 “Patients should be reevaluated more frequently than they are now.”
“Patients should be reevaluated more frequently than they are now.”
Is Autism Overdiagnosed? - Autism Parenting Magazine
When researching whether autism is overdiagnosed, Google’s related search suggested, “Why is everyone autistic now?” Is autism on the rise and affecting individuals in record numbers, or is there a problem with diagnostic criteria resulting in an ever widening spectrum where normal behavior is pathologized…
Could I be on the spectrum? Maybe you entertained this thought while those around you speculated about traits of neurodiversity in visionaries like Mark Zuckerberg and Bill Gates. We like to think of ourselves as at least a little exceptional, our hidden genius just misunderstood.
Online quizzes and pop psychology fuel us to read more into our garden variety social awkwardness and intense interests. Quirky behavior, slightly south of the social norm may be enough for a diagnosis on the spectrum—even if it’s on the periphery where mild, or borderline autism is found.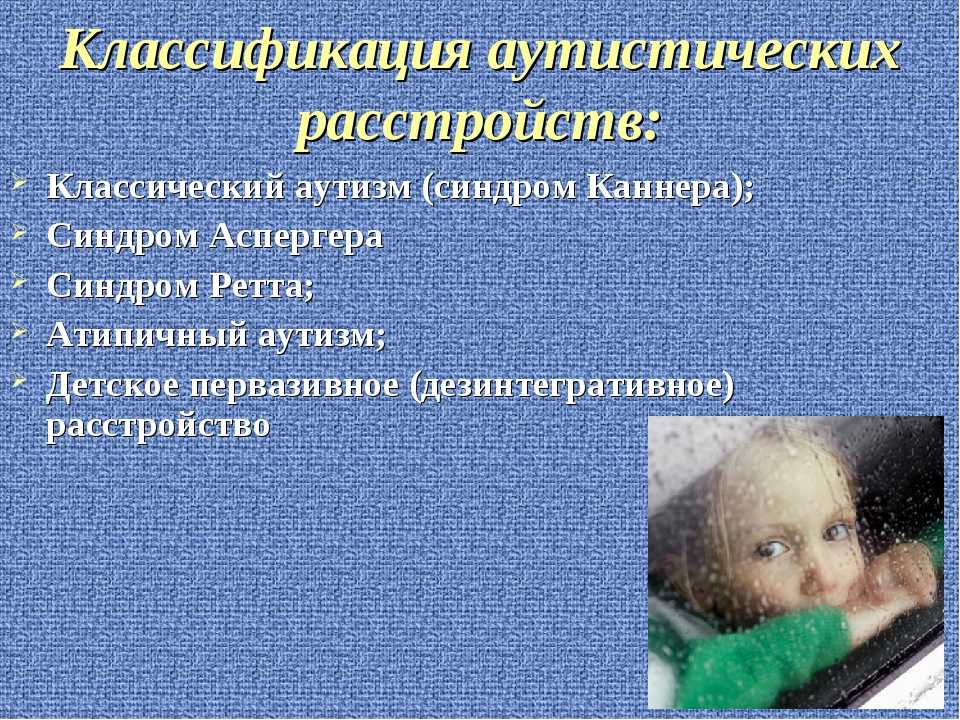
Google schooled society in pseudoscience so, sometimes, we self-diagnose and borrow symptoms from medical conditions. We speak about neurodiversity and our differently wired brains, we use attention deficit hyperactivity disorder (ADHD) as a synonym for creativity, and we identify with gifted Aspies. While this chatter may contribute to destigmatizing some conditions, it could be responsible for diluting the seriousness of a true neurodevelopmental disorder like autism—to the point where an article about surging rates of autism in Silicon Valley was titled The Geek Syndrome (Wired Magazine, 2001).
Media and cultural shifts are not the only elements influencing the possible overdiagnosis of autism. Parents sometimes accept an autism diagnosis even though they know their child is more likely to have sensory processing disorder or some other condition. Autism is a recognized medical condition and a diagnosis means treatment can be obtained, and perhaps more importantly reimbursed. There are many other factors contributing to the perceived or real overdiagnosis of autism, but before getting to those, I want to know if autism is actually being overdiagnosed.
There are many other factors contributing to the perceived or real overdiagnosis of autism, but before getting to those, I want to know if autism is actually being overdiagnosed.
Prevalence of autism rising
In 1943 Leo Kanner introduced the world to the term “infantile autism”—the first systematic description of the condition (Kanner, 1943). The term autism, however, was coined long before this, by German psychiatrist Eugen Bleuler, to describe characteristics of (a subset of) adult schizophrenia.
The 1960s marked a dark period in autism’s history where the condition was mostly blamed on mothers not loving their kids enough. Fortunately science prevailed, and in the late 1970s a revolutionary twin study (Folstein & Rutter, 1977) highlighted the genetic component of autism. Estimates of autism prevalence in the 1960s and 1970s averaged around 1 in 4 000 children (Lotter, 1967).
Compare that to the current CDC figures which tell us that around 1 in 54 children are on the spectrum. Does this sharp rise in prevalence indicate overdiagnosis of autism spectrum disorder (ASD)? Maybe, but other factors influencing diagnosis should also be considered; factors like the context in which children were diagnosed and their surrounding circumstances at the time.
Does this sharp rise in prevalence indicate overdiagnosis of autism spectrum disorder (ASD)? Maybe, but other factors influencing diagnosis should also be considered; factors like the context in which children were diagnosed and their surrounding circumstances at the time.
Autism was thought to be the result of an unloving mother or aloof parenting style. The now discredited “refrigerator mom” theory was popularized by influential academics like Bruno Bettelheim and caused much anguish to mothers who were held responsible for their child’s condition.
Stepping back into the 60s, how would a so-called “refrigerator mom” have dealt with diagnosis and treatment? Perhaps seeking a diagnosis was a shameful business best avoided.
Autism may be overdiagnosed when you look at just how sharply the prevalence rate increased in the last few years, but maybe a dramatic contextual shift also means it’s much easier for parents to seek out a diagnosis and treatment.
Neurodiversity is becoming more acceptable—in fact desirable—as different ways of thinking are celebrated. As autism education and advocacy evolve, parents fortunately no longer suffer under vile burdens of shame and blame. But has diagnostic criteria for autism also evolved and become inclusive of “normal” behavior—possibly leading to overdiagnosis?
As autism education and advocacy evolve, parents fortunately no longer suffer under vile burdens of shame and blame. But has diagnostic criteria for autism also evolved and become inclusive of “normal” behavior—possibly leading to overdiagnosis?
Diagnostic criteria, the evolution
Many researchers believe the rising prevalence of autism is only a reflection of evolving diagnostic criteria and changes in reporting practices. Others believe the frequency of autism occuring is increasing because of a combination of factors like overdiagnosis, increased awareness, an expanding definition of autism, and more controversial reasoning like associations between autism spectrum disorder and increasing nutritional risk factors (Neggers, 2014).
Danish study
A Danish study (Hansen et al., 2015) titled Explaining the increase in the prevalence of autism spectrum disorders: the proportion attributable to changes in reporting practices attributed almost two thirds of the increase in autistic Danish children to how autism is diagnosed and tracked.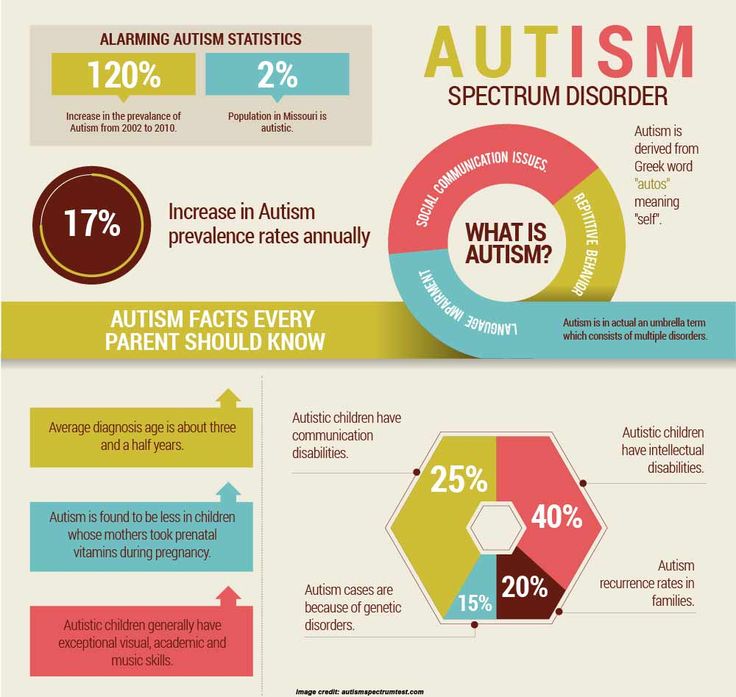
Does this mean we are not really seeing an “autism epidemic”, but rather more children are being diagnosed and that is why the prevalence rates keep increasing? More global studies are needed before definite conclusions can be reached but the influence of changing diagnostic criteria and reporting practices cannot be denied.
In the above mentioned study (Hansen et al., 2015) around 60%, or almost two thirds, of the increase, in those affected, is attributed to changing diagnostic criteria and reporting practices, but what accounts for the other 40%? Seems like the jury is still out on that matter, but perhaps this is where overdiagnosis plays a minor part.
A broadening spectrum
At first autism was regarded as a type of childhood schizophrenia, from there it was considered a condition resulting from aloof or loveless parenting. As more was discovered about the condition, research directed it to be viewed as a developmental disorder.
Today we know so much more about the condition, and yet much of the knowledge showed just how much we still need to learn. Most experts do agree, however, that autism is a complex neurodevelopmental condition with a spectrum nature. Many feel this broad and slightly vague description of autism may be a factor in overdiagnosis—if a spectrum condition is broad enough eventually anyone could find themselves on it.
Most experts do agree, however, that autism is a complex neurodevelopmental condition with a spectrum nature. Many feel this broad and slightly vague description of autism may be a factor in overdiagnosis—if a spectrum condition is broad enough eventually anyone could find themselves on it.
This creates much controversy in the autism community. For individuals who face daily battles because of their symptoms, a glib reference to being on the spectrum is offensive. Parents who lose themselves in the constant care of a high needs child feel understandable frustration when Hollywood egos proclaim they may be on the spectrum despite their highly publicized social life.
As a parent it is difficult not to get swept up in media hype. You read about autism prevalence sky rocketing, the media increasingly refers to an “autism epidemic”. The message of early diagnosis and intervention being key becomes part of the parental subconscious. You start paying more attention to your child’s eye contact, any repetitive behavior becomes a red flag, and if their first words are lagging the diagnosis suddenly seems obvious.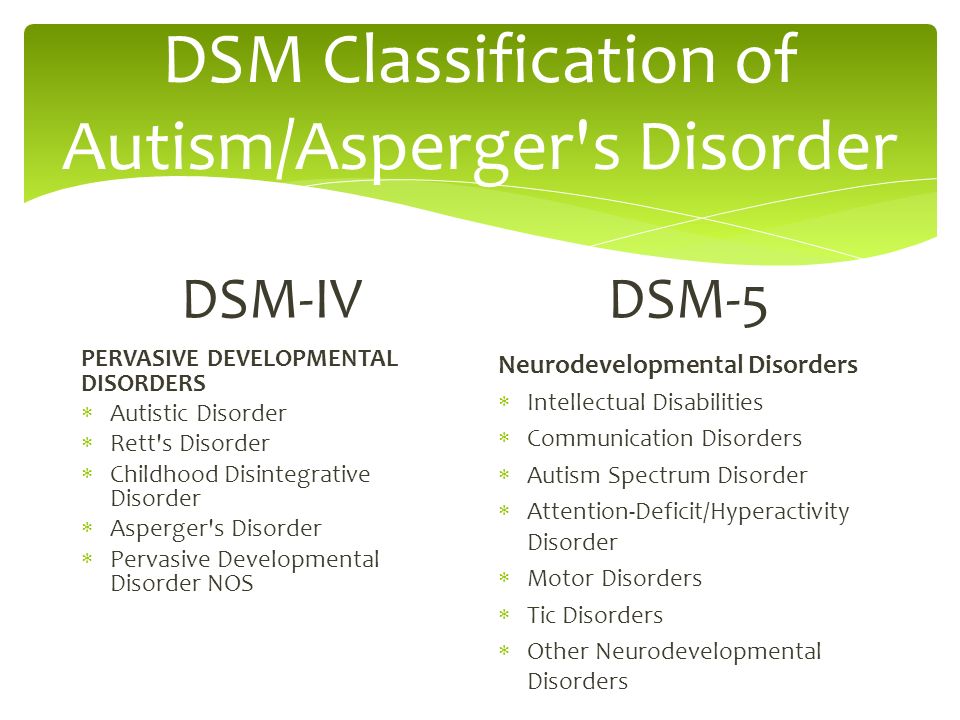
DSM-5 Autism Umbrella
To avoid overdiagnosis should autism spectrum disorder have a strict, narrowly defined diagnostic criteria? The Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM–5; American Psychiatric Association, 2013) is the latest version of the influential manual used by psychiatrists and other doctors to diagnose mental conditions. The fifth edition consolidated previous separate categories under the umbrella term of autism spectrum disorder.
The decision to do away with these previous categories like aspergers syndrome was not well received by all. The DSM-5’s umbrella term for autism created much controversy among researchers and medical experts. Some felt the new autism category is too broad, while others thought the diagnostic criteria would leave kids who desperately need intervention to fall through the cracks.
When reading all sides of the argument, it seems like precise diagnostic criteria for autism will always be a bit of a gamble.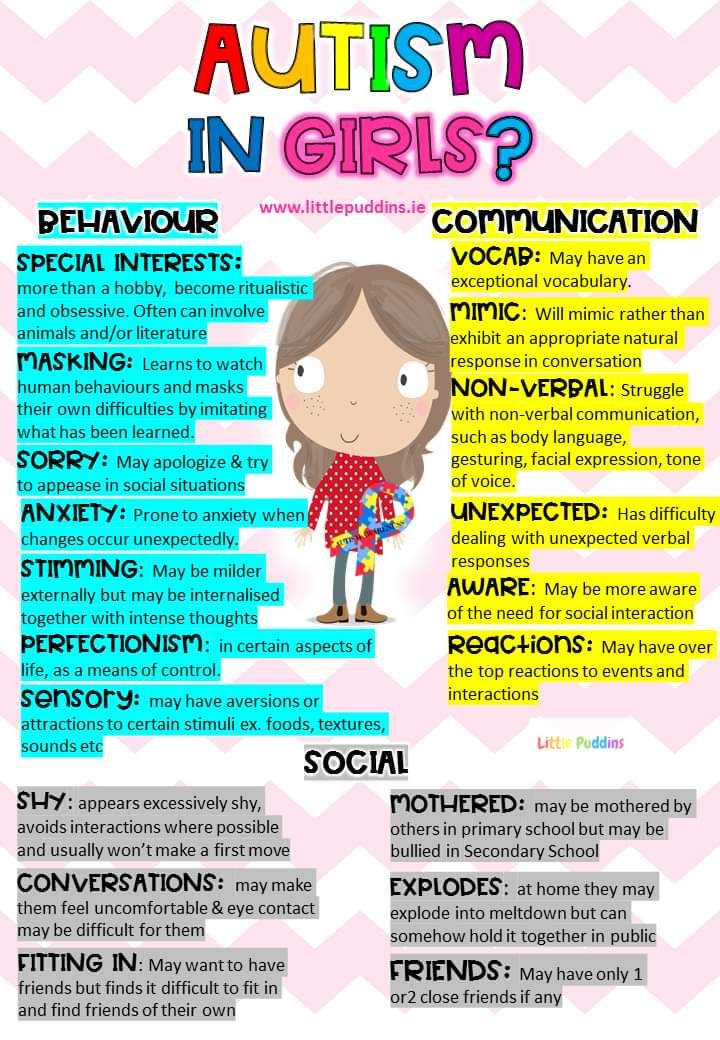 Narrow the criteria too much and those on the threshold, or individuals with atypical presentation, may be deprived of a diagnosis and therapy. Broaden the diagnosis to be more inclusive and suddenly the spectrum caters to all.
Narrow the criteria too much and those on the threshold, or individuals with atypical presentation, may be deprived of a diagnosis and therapy. Broaden the diagnosis to be more inclusive and suddenly the spectrum caters to all.
The spectrum nature of autism does make diagnosis tricky and plays a part in overdiagnosis. Even doctors admit to struggling with the boundaries of autism, When a disorder or condition occurs on a spectrum the threshold could become murky. Doctors may notice the obvious needs of a child, depriving them of a diagnosis may seem cruel, especially when a child does seem “almost autistic”.
Don't miss out on our special offer.
Click
here to find out more
Statistics
So what does research say, is autism actually overdiagnosed? Recent studies do seem to point to an overdiagnosis of the condition. Not only is autism being overdiagnosed but research also suggests that the difference between those with autism and those without the condition are shrinking (Rødgaard, 2019).
Does it matter? If an extra 10% of kids are being diagnosed with autism are the implications serious enough to warrant a revision of diagnostic criteria? Mothers struggling to get resources for their children who require significant support answer with a resounding yes.
Autism, the gateway
Others feel it perfectly okay to use autism as a gateway to getting children the services and resources they need. The former head of the US National Institute of Mental Health, Judy Rapaport famously said: “I’ll call a kid a zebra if it will get him the educational services I think he needs.”
The intention behind constructing an umbrella term to cover autism spectrum disorder was probably not to create enough shade to cover every difficult-to-diagnose childhood disorder. But if your child will only get the necessary interventions with a recognized diagnosis like autism, parents are likely to steer the diagnosis in this direction.
Resource allocation is not the only contentious issue linked to overdiagnosis; inflated prevalence rates also lead to false perceptions with far reaching implications. When parents hear autism is affecting more and more children every year, they want a culprit. Some tangible risk to remove from their lives. This atmosphere creates the perfect breeding ground for fear mongering about vaccinations, toxic diets and parenting mistakes.
When parents hear autism is affecting more and more children every year, they want a culprit. Some tangible risk to remove from their lives. This atmosphere creates the perfect breeding ground for fear mongering about vaccinations, toxic diets and parenting mistakes.
Redefining autism
If we could zone in on a more precise autism definition, or if our understanding of the condition was complete, would overdiagnosis still occur? Some individuals on the spectrum feel the misdiagnosis and overdiagnosis is part of a bigger problem—we still don’t know what autism really is. Austistic individuals should contribute to redefining autism, a definition constructed from the inside will have a significant impact on better diagnoses.
Another area that needs to be addressed with urgency is a separate medical diagnosis for sensory processing disorder (SPD). The fact that many medical professionals refuse to believe in the legitimacy of this condition means parents feel pressured into accepting an autism diagnosis for their children—to receive treatment, services and interventions.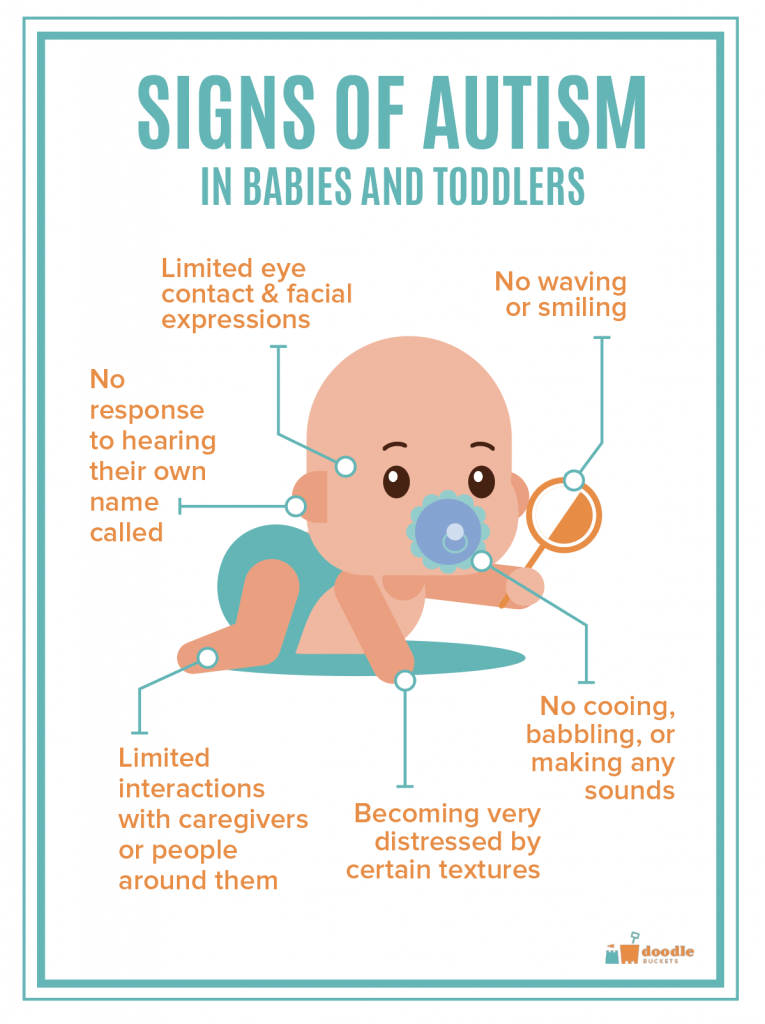 It will be difficult to determine, but interesting to note the overdiagnosis of autism because of conditions like SPD.
It will be difficult to determine, but interesting to note the overdiagnosis of autism because of conditions like SPD.
Not overly concerned
Reading about autism overdiagnosis, it becomes obvious that many medical experts are not too worried about it. They seem to accept that a child who needs help will sometimes receive the correct intervention, under a not quite right diagnosis. Maybe autism is being overdiagnosed, but hopefully the estimated 10% who fall into this overdiagnosis category are getting the right intervention under the wrong label.
References:
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Folstein, S., & Rutter, M. (1977). Infantile autism: a genetic study of 21 twin pairs. Journal of child psychology and psychiatry, and allied disciplines, 18(4), 297–321. https://doi.org/10.1111/j.1469-7610. 1977.tb00443.x
1977.tb00443.x
Kanner, L. (1943). Autistic disturbances of affective contact. Nervous Child, 2, 217–250.
Lotter, V. (1967) Epidemiology of autistic conditions in young children. Soc Psychiatry 1, 163–173. https://doi.org/10.1007/BF00578950.
Neggers Y. H. (2014). Increasing prevalence, changes in diagnostic criteria, and nutritional risk factors for autism spectrum disorders. ISRN nutrition, 2014, 514026. https://doi.org/10.1155/2014/514026.
Rødgaard, E. M., Jensen, K., Vergnes, J. N., Soulières, I., & Mottron, L. (2019). Temporal Changes in Effect Sizes of Studies Comparing Individuals With and Without Autism: A Meta-analysis. JAMA psychiatry, 76(11), 1124–1132. https://doi.org/10.1001/jamapsychiatry.2019.1956.
There is no autism epidemic, there is overdiagnosis - Trinity variant - Nauka
Olga Orlova Childhood autism was first described in detail in 1943 by Leo Kanner, one of the founders of child psychiatry. And for a long time the number of children with such a diagnosis turned out to be stable.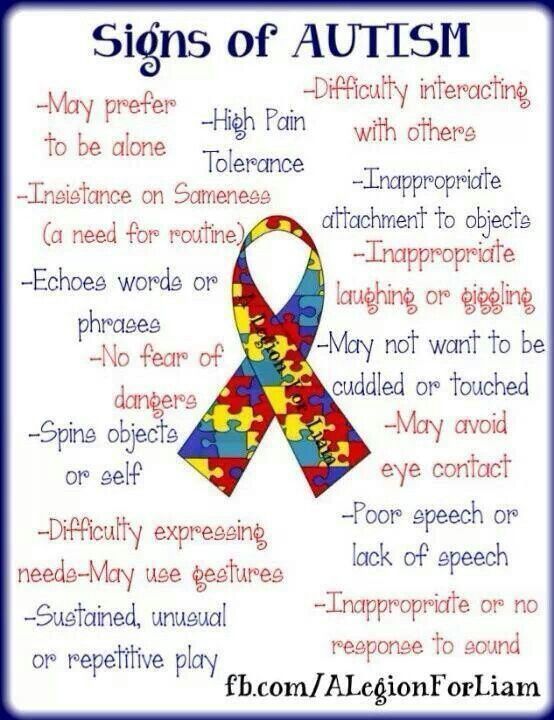 And suddenly, at the end of the 20th century, the percentage of autistic children began to grow. What is the reason?
And suddenly, at the end of the 20th century, the percentage of autistic children began to grow. What is the reason?
About this Olga Orlova , host of the Hamburg Account program on Russian Public Television, spoke with Igor Makarov , Head of the Department of Child Psychiatry, National Medical Research Center for Psychiatry and Neurology. V. M. Bekhtereva.
Igor Vladimirovich Makarov was born in 1969 in Leningrad. In 1992 he graduated from the Leningrad Pediatric Medical Institute, after which he worked at the Department of Psychiatry at his university. In 1996, he received a PhD in Psychiatry. From 19From 1999 to 2004, he worked as a deputy chief physician at the St. Petersburg Center for Rehabilitation Treatment "Children's Psychiatry". Since 2002 - Associate Professor and then Professor of the Department of Psychiatry and Narcology of the North-Western State Medical University.
I. I. Mechnikov. Since 2004, he has been the head of the Department of Child Psychiatry at the National Medical Research Center for Psychiatry and Neurology named after N.N. V. M. Bekhtereva. In 2005 he defended his doctoral thesis in psychiatry on the topic "Psychotic disorders in children: epidemiological, clinical and socio-organizational aspects". Since 2012, he has been the chief freelance child psychiatrist of the Ministry of Health in the Northwestern Federal District. Author/co-author of more than 10 monographs, textbooks and manuals in the field of child and adolescent psychiatry.
— Igor Vladimirovich, the topic of our conversation is autism and autistic diseases, mainly in children. Please tell us why the number of children with this diagnosis has been growing lately both in Russia and abroad. This is evidenced by both statistics and personal experience. As far as I can see, more and more families are facing this problem around. ..
..
— Neither I nor a number of my colleagues agree with this point of view. The number of autists has always been estimated as follows: from 4 to 8 per 10 thousand children. Somewhere early to mid 19In the 1980s, some foreign authors, primarily American ones, began to consider this problem more broadly. They began to talk not only about childhood autism, but also, for example, about the autism continuum. Then they decided to replace the word “continuum” with the word “spectrum” (presumably borrowed from physics) and they began to talk about the fact that there are autism spectrum disorders. And the expansion of diagnostics went like an avalanche. In my opinion, there is no increase in the prevalence of childhood autism and there is no, as is sometimes even said, a blazing epidemic of childhood autism. There is an epidemic of overdiagnosis. Many children with mental retardation, with mental retardation, with delays in speech development fell into the category of autists. A number of other mentally ill patients. But they began to put not even autism, but these notorious autism spectrum disorders.
A number of other mentally ill patients. But they began to put not even autism, but these notorious autism spectrum disorders.
Autism, according to the classical definition, is divided into the Kanner type, Asperger's and the so-called organic. Everything that does not apply to them is an expansion diagnostics.
You know, one of my teachers spoke on this topic something like this: “ What radioactive or chemical cloud does the Earth have to go through in order for the number of autistic children to increase so much? Even if this happened, it would not be children's autism that would increase, but other so-called organic mental disorders, not autism ".
— What caused the overdiagnosis?
- The first factor: this diagnosis was made not only by psychiatrists, despite the fact that the diagnosis is psychiatric. And both national and international classifications of mental illness recognize this. But, alas, I can state with regret: neurologists began to make this diagnosis.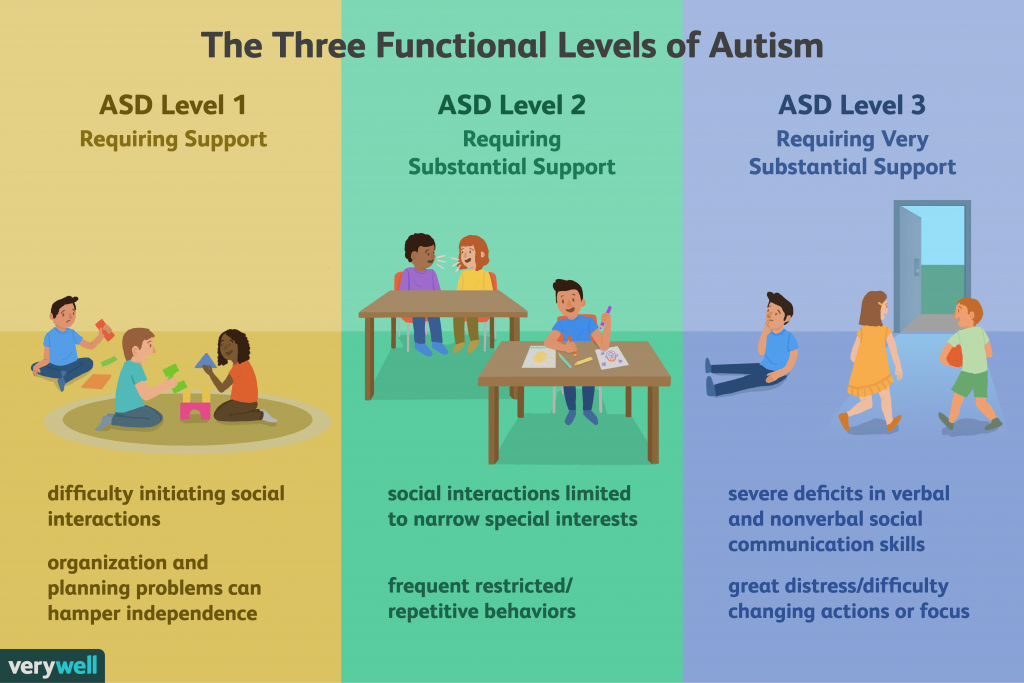 With all due respect to neurologists, they are not psychiatrists. In addition, pediatricians and, moreover, psychologists, speech therapists, defectologists. In my practice, there were cases when nannies in kindergarten told parents: “We authoritatively declare to you: your child has an autism spectrum disorder.” Needless to say, non-specialists cannot have in-depth knowledge of psychiatry. Here, imagine. I work as a child psychiatrist. I have chosen this profession. I would like to hope that she chose me and reciprocates me. But I am less interested in problems, for example, neurology, endocrinology. I don't even try to make endocrinological or neurological diagnoses. If a specialist in his field, but not a psychiatrist, makes these diagnoses, is he apparently not interested in his specialty? Is he really not satisfied with the boundaries of the specialty? This surprises me.
With all due respect to neurologists, they are not psychiatrists. In addition, pediatricians and, moreover, psychologists, speech therapists, defectologists. In my practice, there were cases when nannies in kindergarten told parents: “We authoritatively declare to you: your child has an autism spectrum disorder.” Needless to say, non-specialists cannot have in-depth knowledge of psychiatry. Here, imagine. I work as a child psychiatrist. I have chosen this profession. I would like to hope that she chose me and reciprocates me. But I am less interested in problems, for example, neurology, endocrinology. I don't even try to make endocrinological or neurological diagnoses. If a specialist in his field, but not a psychiatrist, makes these diagnoses, is he apparently not interested in his specialty? Is he really not satisfied with the boundaries of the specialty? This surprises me.
Second moment. Some child psychiatrists also began to make this diagnosis more actively. In my opinion, these are problems of education in the field of child and adolescent psychiatry.
There are other factors. It got ridiculous. In one of the regions of the North-West of Russia, the governor proposes to introduce the position of chief specialist in childhood autism. Because figures about the growing prevalence of this disease reach him. But, in my opinion, the number of autists from 4 to 8 per 10 thousand of the child population remains the same.
Imagine a situation. The patient came to an appointment with an obstetrician-gynecologist. And he says to her: "You, my dear, have such a conclusion: the spectrum of pregnancy." “Doctor, please. So pregnancy or pregnancy spectrum? - “Well, my dear ... Why is that so? You have a spectrum." - "Doctor, explain." “You have a manifestation of the pregnancy spectrum. Spectrum is yours." Do you think such a patient will go to another specialist? There are reasons to think that it will. It's the same with autism. He either is, or he is not. There is no such thing as an autism spectrum diagnosis.
By the way, if you look at the International Classification of Diseases adopted in Europe (ICD) or the classification adopted in North America (DSM), there is no diagnosis of autism spectrum disorder.
- Let's talk about cases where autism definitely exists. What do modern scientists know about the causes of this disease? First of all, what is the genetic component in such a diagnosis?
- Indeed, in a number of types of autism - both Kanner and Asperger's types - it must be assumed that genetic determinism works. Unfortunately, there are no global findings that would provide answers to questions about the origin of autism.
- So there is no clear answer yet?
— No. It must be assumed that primary failures are also possible. Everything is in order in the family, but initially this child had a failure, and he can pass this heredity to his children.
We do not know the mechanisms of inheritance. Here, I think, in the coming years, geneticists have something to work on. But even if we know the cause of the disease, we do not have a time machine to go back and fix everything. Therefore, the psychiatrist works with the disease itself. But any clinician, not only a psychiatrist, can say this about himself. And part of autism is not due to genetics, but to the so-called organic brain lesions.
But any clinician, not only a psychiatrist, can say this about himself. And part of autism is not due to genetics, but to the so-called organic brain lesions.
— What is this?
— Fetal hypoxia. Sometimes these are intrauterine infections. This is a lesion of the fetal brain, still intrauterine. Affecting factors during pregnancy. There is no mention of a genetic defect. But most autism does seem to be genetic. However, we cannot predict anything. If there is a child with childhood autism in the family (let's say with Kanner's autism), it is impossible to say for sure whether the next child will have autism, whether there will be transmission of autism in a generation or in two generations. To date, there are no answers to these questions.
- Due to the fact that autism is becoming a kind of social problem, quite a lot of myths and rumors arise around this disease. It is claimed that autism can develop in children who were born as a result of artificial insemination (the so-called IVF).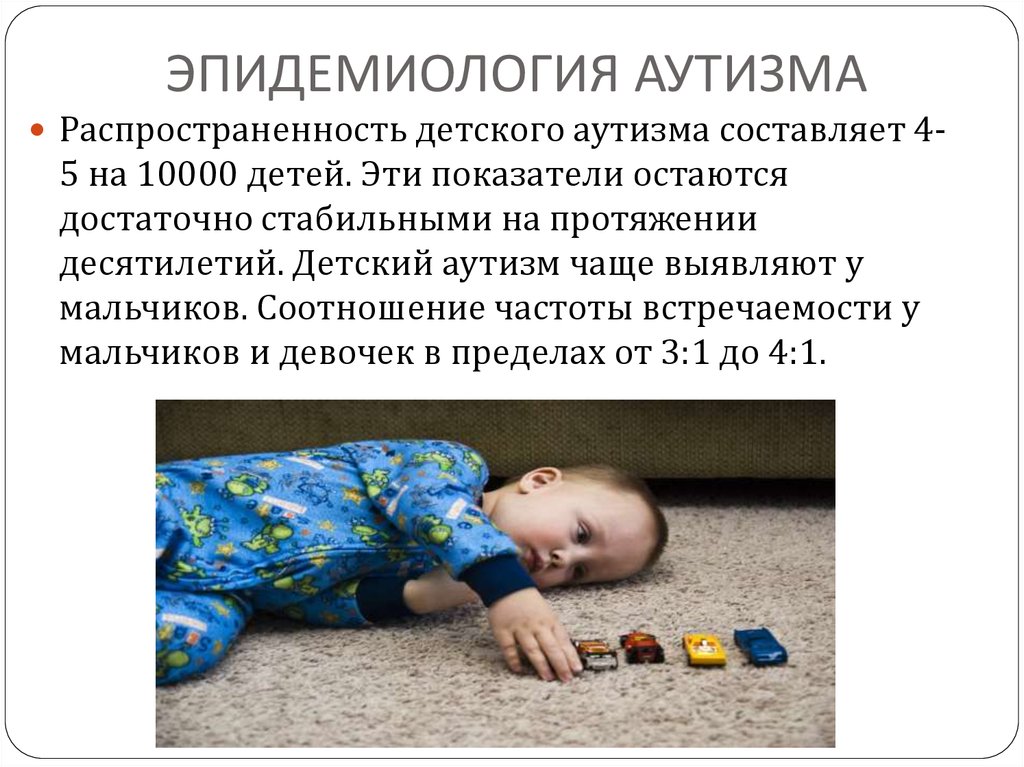 This is true?
This is true?
- I saw a couple of posts on this subject. To date, there is no conclusive evidence to support this assertion.
- Another popular opinion. There is an anti-vaccine movement. In particular, they spread the horror story that autism is one of the consequences of mass vaccination of the population.
— Yes, similar opinions have been expressed in Israel and in a number of other countries. To date, again, there are no convincing facts confirming this. The problem is different. And I understand the concerns of parents. In a number of cases, when a child receives a vaccine, especially some types of complex vaccinations, in the first year of life or shortly after a year, he has a throwback in the development of the psyche, he has what some child psychiatrists used to call mental retardation. Is the vaccine causing this? No way. But it can be a trigger. And this is not due to the vaccination itself, but to the fact that the child was not fully examined before vaccination.
We know perfectly well (this is in all instructions of the Ministry of Health) that the child must be absolutely healthy. But let's imagine a common practice. What happens before vaccination? With a spatula they will look into the child's mouth - and that's it. But in fact, ideally, you need a complete immunological status of the child, a pediatric examination, a complete neurological status, and the absence of any acute respiratory and other diseases. In this case, the child is vaccinated, and in this case the consequences are reduced to the very, very minimum. There is no need to say that vaccinations do not give complications. All over the world it is stated.
If a child is vaccinated against the background of some disease… I can't say what mechanisms work, but in a number of cases the child develops some disorders of mental development. Not autistic manifestations, but rather a lag in mental development.
I really hope that it will be possible to conduct a large cohort study, not only psycho-neurological, but also together with fellow immunologists, infectious disease specialists. It would be interesting. This problem cannot be glossed over. She is now polarized. Some say: it is massive. Others say: do not invent. Vaccinations are the greatest achievement of mankind. You need to calmly, from the standpoint of the same evidence-based medicine, conduct an examination and figure it out.
It would be interesting. This problem cannot be glossed over. She is now polarized. Some say: it is massive. Others say: do not invent. Vaccinations are the greatest achievement of mankind. You need to calmly, from the standpoint of the same evidence-based medicine, conduct an examination and figure it out.
— There is such a social problem: almost any child with deviant behavior is trying to be immediately diagnosed with autism. To what extent is this specific to Russia?
- This problem is specific, in my opinion, not only for Russia. Before talking about deviant behavior, I want to talk about the difference in approaches to the same schizophrenia. In the 1970s, a study was conducted in the Soviet Union: they counted the number of patients with schizophrenia in clinics in Leningrad and in clinics in Moscow. In Moscow clinics, it turned out to be almost twice as much. What is it connected with? What, Muscovites are more likely to get schizophrenia? No.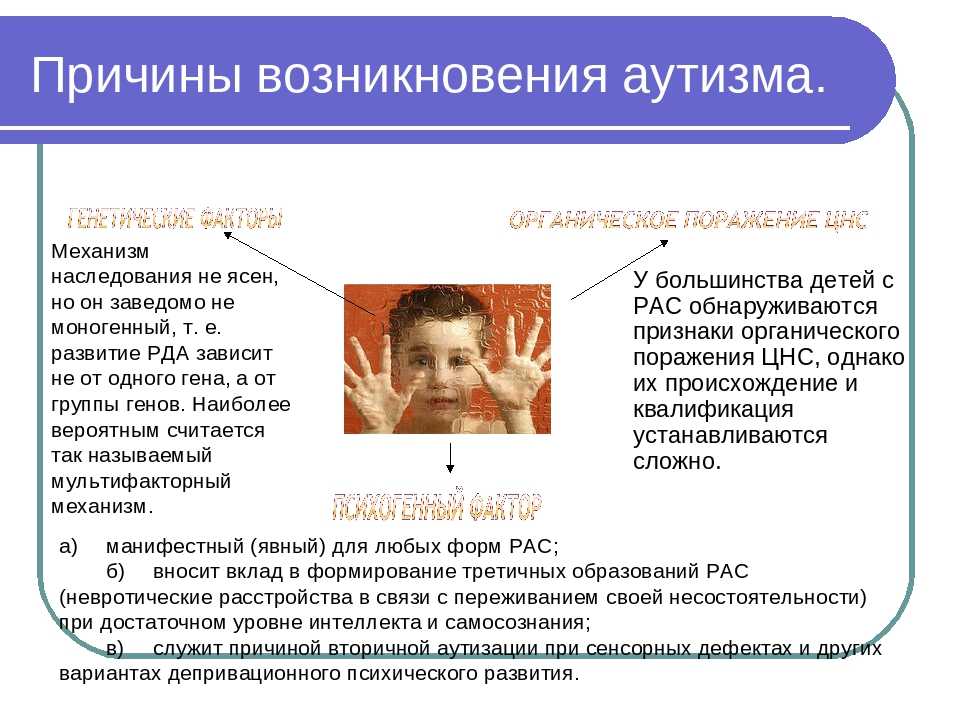 Moscow psychiatrists often put it. Leningrad psychiatrists put it less frequently. But some other diagnoses were made more often. Therefore, this is the difference of schools, the difference of approaches. It manifests itself in both child and adult psychiatry.
Moscow psychiatrists often put it. Leningrad psychiatrists put it less frequently. But some other diagnoses were made more often. Therefore, this is the difference of schools, the difference of approaches. It manifests itself in both child and adult psychiatry.
With regard to behavioral disorders, the issue is very, very complex. Look, if an adult begins, say, to steal, to reach into the pockets of other people - in transport, in a trolleybus, in a tram - it is difficult to imagine that he will be sent to a psychiatrist under generally equal conditions.
- He will be sent to the police.
- He will probably be recognized as a thief and go through the stage. The same is true if someone fights, hooligans, beats another person. Under generally equal conditions, he will be sent to law enforcement agencies. But in children's practice, this is not always the case. If a child starts stealing or becomes aggressive enough, they may be referred to a psychiatric hospital.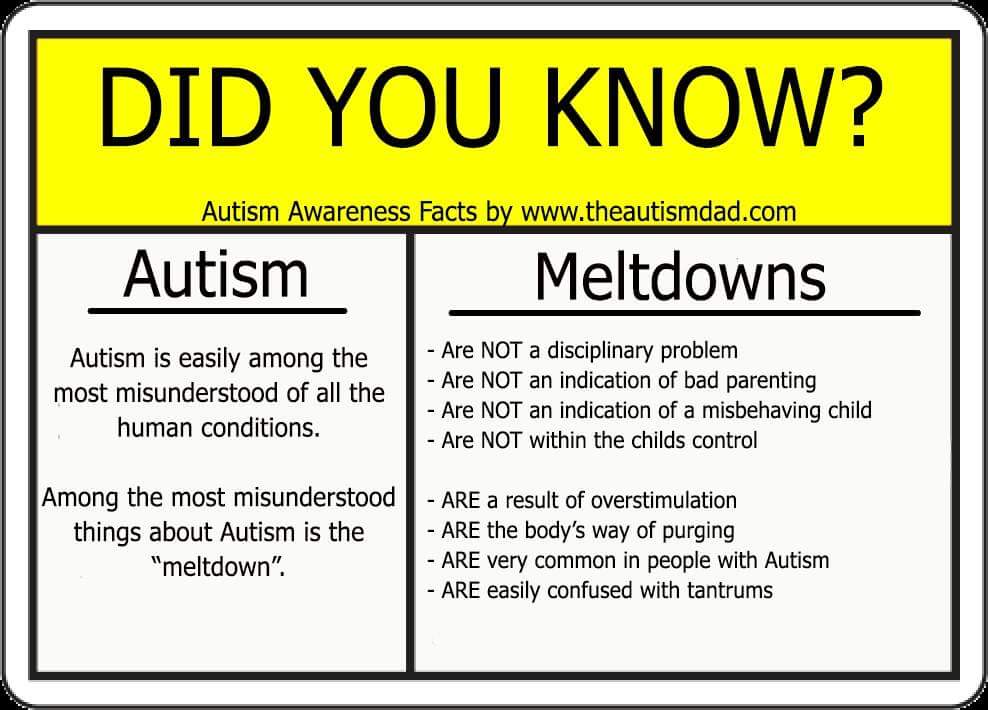 This occurs in a number of children in orphanages and boarding schools, or in children living in families.
This occurs in a number of children in orphanages and boarding schools, or in children living in families.
You see, stealing from a child does not in itself mean mental illness. In this regard, I am confused by the classification of diseases of the tenth revision (ICD-10) currently in force in Europe and in our country. There are diagnoses of the so-called socialized and unsocialized conduct disorder.
— Is the ICD an international classification of diseases?
— Exactly. And when I read the comments on these diagnoses, for example, socialized conduct disorder may include "stealing in terms of gang membership." How do you like it? And in the unsocialized - "stealing alone." Of course, behavioral disorders in children and adolescents, and even in adulthood, can be in the structure of a number of diseases. Nobody disputes this, and one must agree with this. And such people are observed in the hospital or on an outpatient basis.
But if we are not talking about a mental illness, then just theft itself should not be assessed as a behavioral deviation. This is probably a deviation from the generally accepted norms of behavior of most of society. But, you see, if theft is assessed as a psychiatric pathology, then maybe when people don't dress like everyone else, don't think like the majority, or vote differently, they also need psychiatric diagnoses? There should not be panpsychiatrization of everything. The psychiatrist has "his" diseases. If this is a person who loves his specialty, he loves these nosological forms, deals with them, this is enough for him. He should not go into a mental, psychiatric norm.
This is probably a deviation from the generally accepted norms of behavior of most of society. But, you see, if theft is assessed as a psychiatric pathology, then maybe when people don't dress like everyone else, don't think like the majority, or vote differently, they also need psychiatric diagnoses? There should not be panpsychiatrization of everything. The psychiatrist has "his" diseases. If this is a person who loves his specialty, he loves these nosological forms, deals with them, this is enough for him. He should not go into a mental, psychiatric norm.
So I'll be honest. I don't know what to do in some cases. When a child living, for example, in an orphanage or a boarding school runs away from there, starts stealing, he is often sent to a psychiatric hospital.
— This problem of overdiagnosis again emerges because there is no social solution…
— Quite right. I don't see how to solve this issue.
- It turns out some kind of archaism, punitive psychiatry, which we seem to have already experienced. Not?
Not?
- This is an archaic method, perhaps. But this is the only method that is used almost all over the world. I will return to the fact that this is an international classification of diseases. Therefore, what does the so-called punitive psychiatry of the Soviet period have to do with it? Punitive psychiatry did not originate with us. You can recall the work "One Flew Over the Cuckoo's Nest" and a number of others. Probably, in this way society wants to protect itself from those who are not very desirable in this society. But, in my opinion, this should not always be done by the hands of psychiatrists. Psychiatrists can only help the patient and protect society if the patient is mentally ill. In all other cases, this problem should be solved by lawyers, psychologists, philosophers, if you like, social services, sociology as a whole as a science, but not psychiatry. Psychiatry is a humanistic specialty. It was created as a humanistic one. Not at all as a punitive specialty. And in fact, psychiatry often stands guard over the interests of the patient himself, and his relatives and friends. Who, besides a psychiatrist, remains on the other side of the barricades with a patient? Sometimes it happens that there is no one else.
And in fact, psychiatry often stands guard over the interests of the patient himself, and his relatives and friends. Who, besides a psychiatrist, remains on the other side of the barricades with a patient? Sometimes it happens that there is no one else.
- Who do you think is the most talented portrayer of autism in fiction or film?
Dustin Hoffman in "Rain Man" (1988)- Of course, traditionally everyone remembers the film "Rain Man" with Dustin Hoffman.
— What kind of autism is this?
- To do this, I would like to get an answer to the question: was the intellect of this patient preserved or not? After all, the film specifically does not show, to the smallest detail, what kind of intelligence the character has. If it is Kanner's autism, there, unfortunately, in most cases, such patients have reduced intellectual abilities.
When it is Asperger's autism, then, on the contrary, the intellect is completely preserved.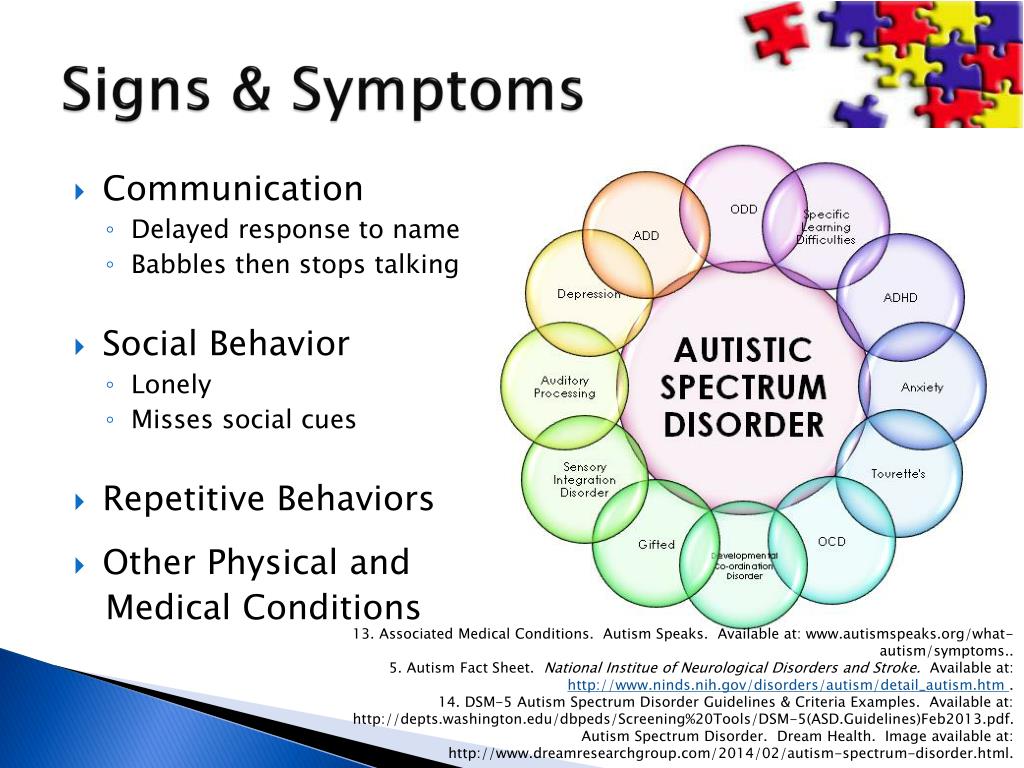 There are very highly intelligent patients with Asperger's Syndrome. I can say one thing: Dustin Hoffman played well. And, indeed, he, presumably, prepared theoretically. He probably had the opportunity to communicate with people with autism in practice.
There are very highly intelligent patients with Asperger's Syndrome. I can say one thing: Dustin Hoffman played well. And, indeed, he, presumably, prepared theoretically. He probably had the opportunity to communicate with people with autism in practice.
- And the last question. If you take medical professionals in any other field, over the past 50 years they have received unique tools related to technological development. Urologists, ophthalmologists, cardiologists - they have ultrasound, robots. What do you get from technological progress?
— You know, there are specialties that develop faster, and there are specialties that develop more slowly due to both objective and, first of all, but sometimes also subjective reasons. Take at least this situation: you can take an intravital biopsy in case of kidney disease. And what about the brain? This is impossible.
- It turns out that, again, this problem of overdiagnosis, on the one hand, is caused by an unresolved social complex, and on the other hand, psychiatry in this sense simply does not receive the tools that physicians in other areas receive. And you are the most unlucky?
And you are the most unlucky?
— No. I wouldn't say so. You know, in psychiatry the situation is such that no CT scan, no electroencephalograph, no other additional, auxiliary (whatever you want to call them) methods can replace a doctor's head. Psychiatric diagnostics is, first of all, the ability to understand the patient, to properly conduct a conversation with him, to speak correctly and correctly with his relatives, friends, and sometimes with other people. This is patient observation. Without this, no CT scan or MRI will allow a diagnosis to be made.
It is very common to see parents with a mentally ill child at the reception, who bring the results of a large number of examinations. It's just War and Peace. Four volumes, five volumes, huge volumes. And for diagnosis, many examinations are simply not needed. Psychiatry is still a subjective view of one or another specialist. Hence the difference in schools.
In fact, of course, psychiatry is also moving in line with evidence-based medicine. But, on the other hand, we cannot entrust psychiatric diagnostics only to a computer or sort everything out by points and by shelves. Sometimes it is impossible to express qualitative phenomenological psychiatric phenomena by quantitative methods and indicate everything in points.
But, on the other hand, we cannot entrust psychiatric diagnostics only to a computer or sort everything out by points and by shelves. Sometimes it is impossible to express qualitative phenomenological psychiatric phenomena by quantitative methods and indicate everything in points.
You will rate patients with delusions in points, relatively speaking, you will say: “This one has 70 points, the delirium is not severe, and that one has 80 points, the delusion is very severe.” But the one with 70 points committed much more dangerous acts and ended up in compulsory treatment, and the one with 80 is relatively fine. This is very conditional.
First of all, a psychiatrist must be a thinking person. Perhaps this applies not only to psychiatrists. In my opinion, and highly cultured. At one time, Professor Samuil Mnukhin, the founder of the Leningrad School of Child Psychiatrists, when recruiting interns and clinical residents for his department, did not ask about psychiatry (one of his students and my teacher told me about this). He asked whether they had read Bunin's Dark Alleys, whether they had read Kuprin and other classics of domestic and foreign literature. He believed that without this, a psychiatrist would never become a highly qualified specialist. And if the candidate for interns or residents did not know this, he refused to accept him for training, for work.
He asked whether they had read Bunin's Dark Alleys, whether they had read Kuprin and other classics of domestic and foreign literature. He believed that without this, a psychiatrist would never become a highly qualified specialist. And if the candidate for interns or residents did not know this, he refused to accept him for training, for work.
Igor Makarov
Interviewed by Olga Orlova
Video recording of the conversation, see otr-online.ru/programmi/gamburgskii-schet/otkritiya-bozona-higgsadlya-72946.html
epidemic: why there are more and more children with autism
EducationHealth
- Photo
- Getty Images
Psychiatrists have known the diagnosis of autism for almost 80 years. In 1943, Leo Kanner described the behavior of 11 children, noting the "red flags of autism" - unusual manifestations in behavior, which are still the first attention of doctors today.
There were no methods for the rehabilitation of such children at that time. however, one of the guys later graduated from college, and three more got qualified jobs.
Compared with the beginning of the last century, today specialists have seriously advanced in the study of this disease and have learned how to socialize people with autism. Today it is believed that more than 20% of these patients can live a full life.
This is on one side. On the other hand, there are more and more children with such a diagnosis in developed countries.
And now, some people are already talking about the epidemic of autism, while others brush aside that it is necessary to examine children less and educate them more, and everything will be fine. Like, they grew up without any diagnostics, and there were no such diagnoses.
Where is the truth, Parents.ru asked psychophysiologist Victoria Efimova.
Organizer of the general educational forum “Child Brain Plasticity 2021”, psychophysiologist and head of the Prognoz Clinic
Red Flags
“Is there an autism epidemic or not? There is no answer to this question, because it is not yet known what autism is.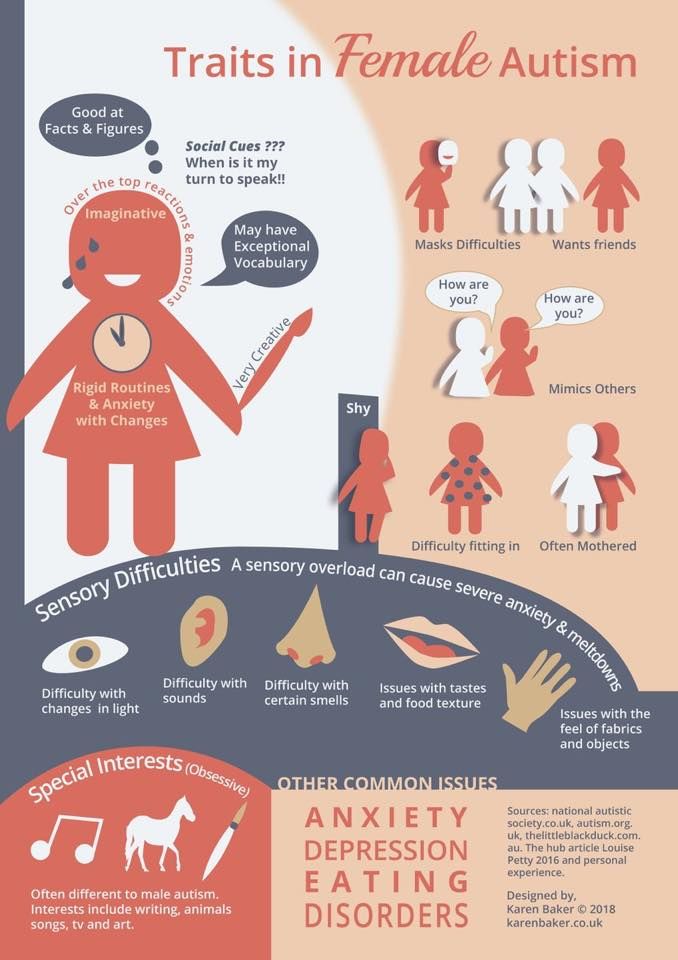 It is not clear whether this is a single disorder or a whole complex of dysfunctions that manifest themselves in a similar way in behavior. In fact, children with autism are completely different from each other. Each one is unique. And although huge amounts of money are being spent on scientific research on autism around the world, there is still no clear result: it is not known why it occurs.
It is not clear whether this is a single disorder or a whole complex of dysfunctions that manifest themselves in a similar way in behavior. In fact, children with autism are completely different from each other. Each one is unique. And although huge amounts of money are being spent on scientific research on autism around the world, there is still no clear result: it is not known why it occurs.
In addition, there is no analysis, type of diagnosis or test that would unequivocally confirm or not confirm the presence of autism in a patient,” says our expert.
Victoria explains: the doctor makes a diagnosis based on observation of the child's behavior. So, foreign experts use standardized questionnaires: they need to note whether any of the listed points has a child. These manifestations are called "red flags". If there are many, the child may receive a diagnosis.
“But many of these characteristics may well be found in children without autism,” the psychophysiologist warns against hasty conclusions. - For example, if a child has a speech delay or sensory integration disorder. If this is autism, then there should be a lot of “red flags”, and this behavior will be more than once or twice. And it is stable to manifest itself in different situations.
- For example, if a child has a speech delay or sensory integration disorder. If this is autism, then there should be a lot of “red flags”, and this behavior will be more than once or twice. And it is stable to manifest itself in different situations.
Autism red flags
-
Stereotyped movements (arm shaking, rotating in place, etc.).
-
Difficulties in interacting with other people.
-
Avoid eye-to-eye contact.
-
Unusual attachment to objects.
-
Delayed speech development.
-
Repetition of other people's phrases.
-
Craving for order and uniformity.
-
Reduced sensitivity to pain.
-
Increased response to sounds (or no response).
-
Hypersensitivity to touch or search for touch.
-
No sense of danger.
-
Difficulties in expressing your needs.
-
Inappropriate laughter.

“For Russian parents, autism is a tragedy”
Ideally, before making a diagnosis, the child is observed for a long time, perhaps even several weeks. They look at how he behaves in different conditions, how he perceives different people. How behavior at home will be different from behavior in the doctor's office. How will he behave in the same situation in front of his parents or specialists.
An ideal that is still unattainable in our country.
“Our children often receive a diagnosis after a 10-minute consultation with a psychiatrist,” Viktoria Yefimova complains. - For some doctors, it is enough to see the “wings” (when a child shakes his palms in front of his face) to make his verdict.
Since there is no objective diagnosis of autism, there is too much room for a doctor to express his subjective opinion.”
Here you have overdiagnosis: so that later they would not blame that the doctor overlooked, and, conversely, the denial of the disease. Many doctors still believe that autism does not exist. A child with strange behavior will at best be labeled “mentally retarded”, at worst, diagnosed with schizophrenia.
Many doctors still believe that autism does not exist. A child with strange behavior will at best be labeled “mentally retarded”, at worst, diagnosed with schizophrenia.
- Photo
- Getty Images
But doctors are not the only ones who sin with denial. Even more often, relatives of a small patient do not want to believe in the diagnosis - most often it is they who need the help of a psychotherapist in order to "accept" the child's illness and live on.
“According to my observations, in Europe and the United States, parents are calmer about the fact that a child has received a diagnosis of autism than in our country,” says Victoria Yefimova. “They know that the state will financially and socially support the child throughout his life. For parents in Russia, this is a tragedy. Because the development of social services that should help such families is still in its early stages.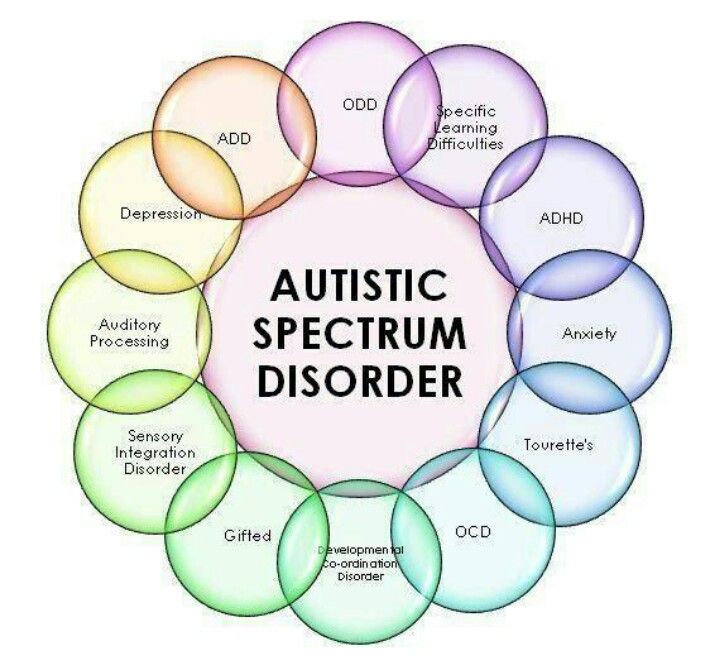 ”
”
The first "bells"
A rare doctor will talk about childhood autism before the baby is 3 years old. Yes, and at this age, perhaps, initially they will look for other diseases.
But attentive parents will notice oddities much earlier: after all, autism is a violation of the body at all levels. These are neurological dysfunctions, and immunity disorders, and malfunction of the gastrointestinal tract, and problems at the cellular level.
Signs of the disease always appear in the first years of life. And therefore, most likely, at first, adults will write off the condition of the crumbs for anything, but not for this autism.
“For example, a baby may not suck well at the breast, he will have problems with swallowing,” says the psychophysiologist. “Also, many notice problems with sleep, persistent constipation or diarrhea.”
And here it is very important to find a specialist as soon as possible, who will collect all these "bells" together and make the correct diagnosis.