Hot flash when i wake up
Cause of Your Morning Wake-Up Heat Wave in Menopause
“Do you know why, when I immediately wake-up, I get a heat surge through my body?” she asked.
The question immediately took me back in time. A few years ago, when in my early 50s, I experienced the same phenomenon. Even though I’m in post-menopause now, I still have the odd ‘heat surge on waking-up’ moment. When this happens, I now understand why, so I lie quietly take some deep, slow breaths to calm my respiratory rate and heart rate, before getting up to start my day.
I first heard about cortisol and a phenomenon known as the Cortisol Awakening Response (CAR) when I was studying sport and exercise science and overtrained athletes. I never imagined that I would be going back to studying it during my menopause transition, many, many years later.
The cortisol awakening response is the acute increase of the cortisol level in the 30-45 minutes after awakening. CAR is believed to act as a “boosting” mechanism, to aid in physiologically preparing one for waking up and getting on with the tasks of our day and the morning heat surge you may be feeling, could be because you aren’t sleeping or your blood pressure and resting heart rate are elevated.
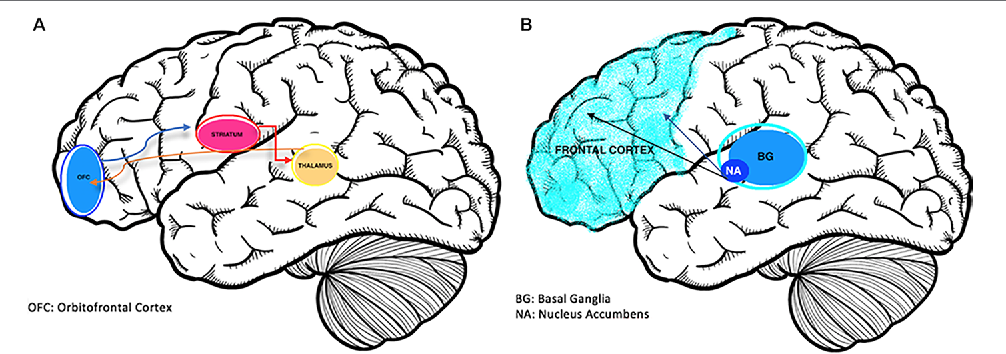
Because the cortisol-awakening-response is driven by your nerves and hormones (neuro-endocrine system), any irregularities depend on how balanced your hypothalamus, pituitary gland and adrenal glands are.
The connection that these three organs have is known as the Hypothalamus-Pituitary-Adrenal Axis (HPA axis) and the working of this axis is considered to be influenced by, and sensitive to, a host of psychological conditions and stressors. All of which affect your cortisol levels throughout the day.
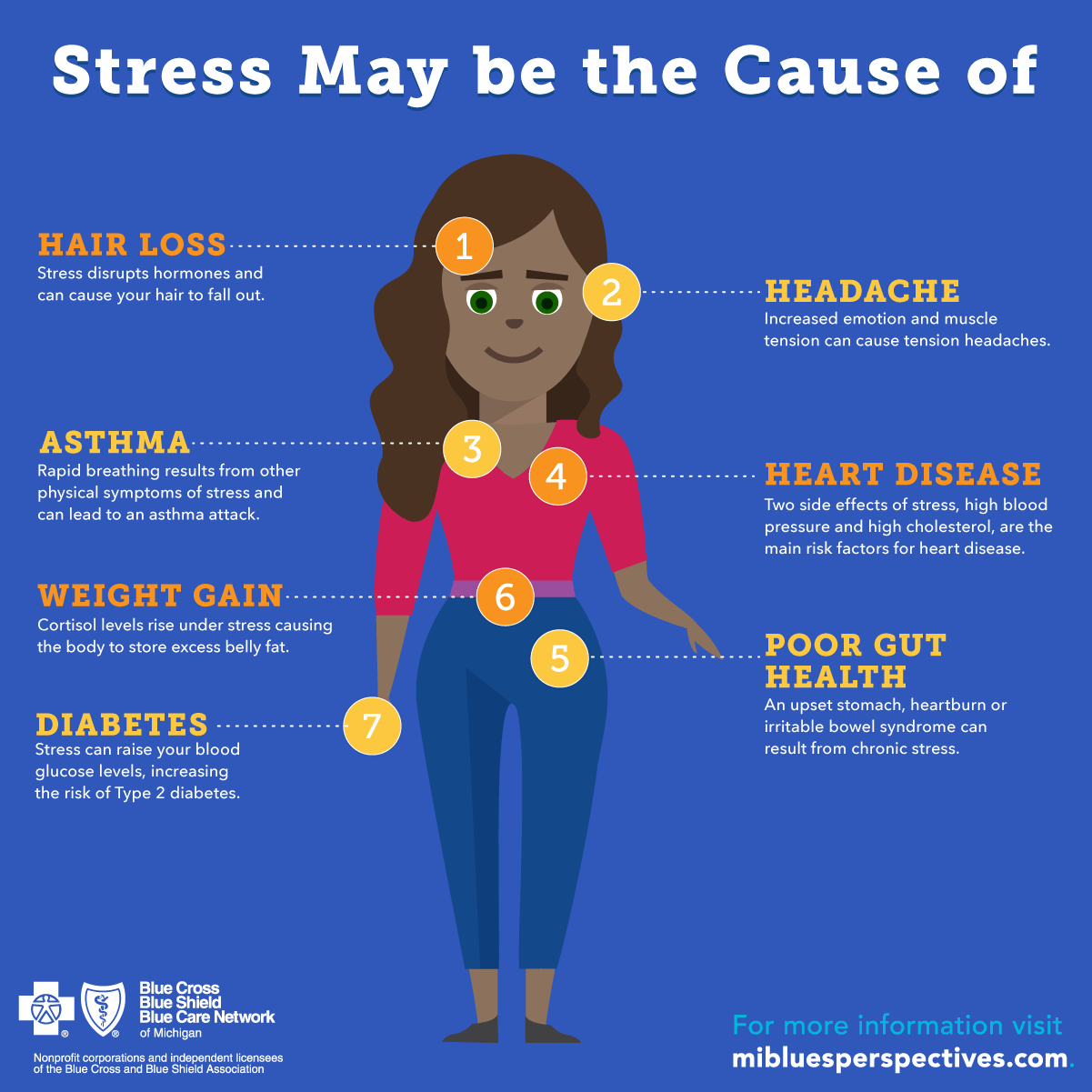
Workplace and personal stress, over-exercising, insomnia, too much fasting and of course, the hormonal changes that we undergo in menopause, all affect your HPA-axis function, which in turn affects your cortisol response. Learn more here about the sign of menopause.
Cortisol is widely recognized as one of our stress hormones. This hormone has a diurnal (day-night) pattern and works in with our sleep hormone called melatonin. Cortisol levels are generally high in the morning and low at night, unless there are disruptions to its normal fluctuations throughout the day, such as when we are busy, exhausted or stressed.
The body makes cortisol in our adrenal glands, and in the context of athletes, cortisol works with other adrenal hormones and the liver, to help release the glucose stored in the liver for exercise performance. During exercise, these storage forms of glucose need to be continually released and turned over.
Hence, cortisol concentrations also increase during exercise. This powerful hormone also helps to free proteins from the muscle, to be used in the liver for the production and use of more glucose. This is why, for endurance athletes especially, they tend to not have the size of muscles that bodybuilders have. Increased exposure to cortisol increases muscle breakdown or catabolism. It’s the same for women doing lots of high-intensity exercise and not sleeping – the greater the exercise intensity, the higher the levels of cortisol.
As I’m always saying to women who come onto the MyMT™ programmes, ‘without proper recovery, intense exercise can lead to elevated levels of cortisol in the bloodstream and heightened symptoms of physical stress, even when exercise is not being performed. Such as first thing in the morning. For women in menopause, this elevated cortisol, can give them a hot flush on awakening.
Such as first thing in the morning. For women in menopause, this elevated cortisol, can give them a hot flush on awakening.
For female athletes, the elevated cortisol can cause heart rate to be elevated in the morning too. There’s a reason numerous athletes wear heart rate devices – not only is this to monitor the intensity of their training, but it’s also to monitor morning heart rate.
Elevated heart rate and /or elevated cortisol go hand in hand – add on dehydration, inflammation, low blood glucose, and low iron levels, then in female athletes, elevated cortisol awakening response occurs.
But what if you aren’t an exerciser and you are waking up to hot flushes?
There’s another factor to consider when it comes to cortisol awakening response and hot flushes. Whilst research doesn’t support morning hot flushes being caused by Cortisol Awakening Response [CAR], what the research does indicate is that higher heart rate, anticipated stress and insomnia overnight can contribute to an elevated Cortisol Awakening Response, there is something else that is specific to women in menopause – and that is our changing and ageing blood vessels. I have talked about arterial or vascular stiffness in numerous blogs as well as in my Masterclass on Menopause, which is now online for you.
I have talked about arterial or vascular stiffness in numerous blogs as well as in my Masterclass on Menopause, which is now online for you.
Because menopause is the gateway to our biological ageing, numerous changes are occurring around our body. This includes changes to our blood vessels and other organs. In an age whereby media and pharmaceutical companies focus on marketing botox and other external products to promote anti-ageing, the salient point of our internal cellular ageing gets forgotten.
When menopause arrives, there are numerous structural changes that occur in our body, not just changes to our oestrogen and progesterone levels. Because hormones travel in the blood, they contact virtually all body tissues, however, most of them have targeted actions specific to the different hormone receptors. Which is where our blood vessels come in and the relationship to elevated blood pressure, elevated heart rate and an elevated cortisol awakening response.
This is an important point for all women, not only those who are regular exercisers. As we lose oestrogen, our blood vessels are ageing and this leads to vascular or arterial stiffness. The loss of elasticity in blood vessels and lymphatic vessels, means that we may feel more bloated, our legs may feel heavy, restless and aching (especially for exercisers) and our blood pressure and heat regulation may get out of balance too.
As we lose oestrogen, our blood vessels are ageing and this leads to vascular or arterial stiffness. The loss of elasticity in blood vessels and lymphatic vessels, means that we may feel more bloated, our legs may feel heavy, restless and aching (especially for exercisers) and our blood pressure and heat regulation may get out of balance too.
When we have busy, active lives, the vascular stiffness leaves us feeling exhausted. It can also leave us with an elevated morning heart rate – just like overtrained female athletes … or women not sleeping and feeling a bit burnt out with all that’s going on in their lives. This alone disrupts hormone regulation in the body and the reason for this is because the hypothalamic-pituitary-axis (HPA-axis) which regulates our stress response and the adaptation to stress in our lives, fails to do its job properly.
This is why feelings of overwhelm, high cortisol levels, insomnia and burnout, all mess up this lovely HPA-axis – especially during our menopause transition.
Some of you with overwhelming symptoms, may have had your hair, saliva or urine tested by Naturopaths for cortisol levels. Disruptions in HPA-axis functioning, due to chronic stress, are usually examined by investigating the level and course of cortisol during the day and the cortisol awakening response.
This CAR biomarker has shown to be independent of the general cortisol level in the body and thus provides relevant information on HPA-axis functioning (Schmidt-Reinwald et al., 1999).
Understanding why many of you may be feeling the heat on waking up is important. Not only because it helps you to put in place strategies to turn this around, but also to reassure yourself that it’s not just menopause, but related to the other changes going on around your body as part of ageing, such as inflammatory changes in your blood vessels.
That’s why calming strategies are helpful, such as doing some slow breathing which helps to reduce your heart rate; cutting back on high intensity activity if you aren’t sleepine well, because this increases inflammation and working in with your circadian rhythm and the natural ebb and flow of your cortisol levels throughout the day and evening. In a normal cycle, cortisol should be high in the morning (but not too high) and over the course of the day, it should be lowering as you head towards evening. So, evening is the time of day to put your stress away and allow your body and brain to rest and recover.
In a normal cycle, cortisol should be high in the morning (but not too high) and over the course of the day, it should be lowering as you head towards evening. So, evening is the time of day to put your stress away and allow your body and brain to rest and recover.
If you are struggling with your symptoms or menopause weight gain, then I hope you can join me on my 12 week progammes sometime. You can read about how they work HERE.
Dr Wendy Sweet, MyMT Founder/ Member: Australasian Society of Lifestyle Medicine.
References:
Anderson, T., Wideman, L. Exercise and the Cortisol Awakening Response: A Systematic Review. Sports Med – Open 3, 37 (2017). https://doi.org/10.1186/s40798-017-0102-3
Langelaan, Saar & Schaufeli, Wilmar & Rhenen, Willem & Doornen, Lorenz. (2006). Do burned-out and work-engaged employees differ in the functioning of the hypothalamic-pituitary-adrenal axis?. Scandinavian journal of work, environment & health. 32. 339-48. 10.5271/sjweh.1029.
32. 339-48. 10.5271/sjweh.1029.
Nijm, J. & Jonasson, Lena. (2008). Inflammation and cortisol response in coronary artery disease. Annals of Medicine, 41. 224-33. 10.1080/07853890802508934.
Woods N., Mitchell E., & Smith-DiJulio K. (2009). Cortisol levels during the menopausal transition and early postmenopause: observations from the Seattle Midlife Women’s Health Study. Menopause, 16: 708-718
How To Reduce Hot Flashes at Night – Cleveland Clinic Health Essentials
You wake up in a pool of sweat, feeling like the heat somehow got cranked up to 100 degrees. Alas, the problem isn’t the furnace but your internal thermostat.
Surely you’re too young for hot flashes, right? Right?! Maybe not.
Most people who menstruate start having symptoms of perimenopause in their 40s. Those symptoms include irregular periods, vaginal dryness and, yes, hot flashes. As many as 3 in 4 women have hot flashes in the years leading up to menopause.
Women’s health specialist Pelin Batur, MD, shares tips for surviving these nocturnal trips to the tropics.
Why do you get hot flashes at night?
Scientists don’t know the exact reason women have hot flashes, but it’s likely related to hormone levels. When you enter menopause, your body starts producing less estrogen (a hormone).
What is clear, though, is that hot flashes can be really, really unpleasant. You might feel like you’ve been swallowed by a heatwave, and you may sweat, turn red and feel your heart race. And while they’re an unwelcome experience any time of day, hot flashes can be especially troubling at night, when they mess with your sleep.
“If you’re not getting a good night’s sleep because of night sweats, then they become more than just a nuisance,” Dr. Batur says. “Really, it’s a quality of life issue.”
Advertising Policy
Nighttime hot flashes can cause you to wake up drenched in sweat. The hot flashes typically last only a few minutes, and they can also be followed by a bout of chills. By the time the whole ordeal is over, you may be wide awake and uncomfortable — not to mention soaking wet and kinda grossed out.
How to deal with or stop hot flashes
Menopause-related hot flashes and night sweats aren’t dangerous. But if they’re interfering with your slumber or otherwise making you miserable, help is available.
“I think of it as a three-pronged approach: natural approaches, nonhormonal medicine approaches and hormonal approaches,” Dr. Batur says. She shares tricks and tips to keep hot flashes to a minimum.
1. Find (and avoid) your triggers
Certain foods or environmental triggers can spark a hot flash. “There are some data that increased intake of sugar, stress and caffeine may be contributors,” Dr. Batur notes. Other common triggers include eating spicy foods, exercising in a hot environment or taking hot baths.
Spend a few days tracking your hot flashes and what you did in the hours leading up to them. You might find that spicy meals or flannel pajamas are a recipe for night sweats.
2. Decrease your stress
Easier said than done, sure, but reducing your stress levels and practicing overall mindfulness can do wonders for your health in general — and it may lessen hot flashes, too.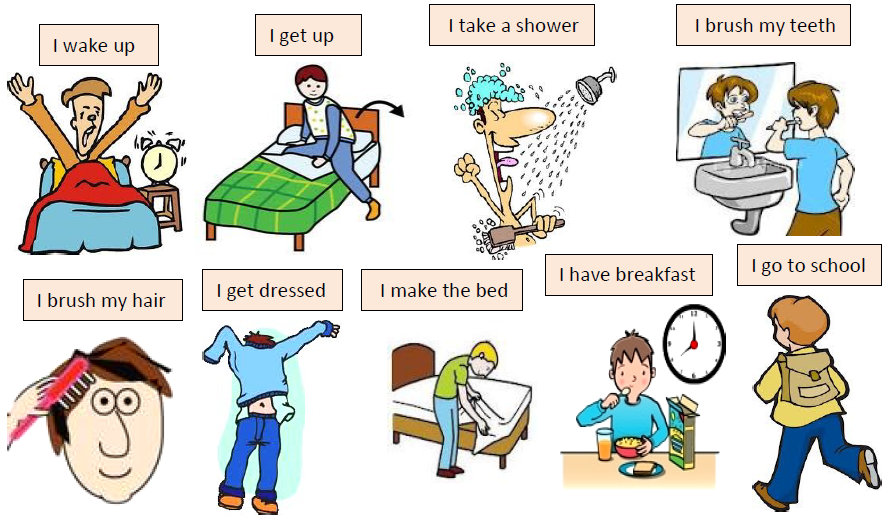
Advertising Policy
“The data for all of this is weak, but certainly it makes sense to try to minimize your stress, practice mindfulness and do some deep breathing,” Dr. Batur advises.
3. Make your bed a cool zone
Do what you can to turn your bed into a sweat-free sanctuary.
- Turn your bedroom temperature down at night.
- Wear lightweight pajamas in breathable fabrics like linen and cotton.
- If possible, invest in pillows and mattress covers filled with cooling gel.
4. Start treatment
If nighttime hot flashes are keeping you from sleep, your doctor can help. Their course of action will depend on your health conditions and concerns, but options include:
- Hormone therapy.
- Prescription medications.
- Alternative therapies like cognitive behavioral therapy, hypnosis and acupuncture.
Do hot flashes stop?
Hot flashes can be a part of your life for months or even years. But if they’re getting in the way of your life, it’s time to seek treatment.
Plus, not all hot flashes are from menopause. They can also be related to thyroid disorders and other conditions or medications, so it’s especially important to get evaluated by your doctor. They’ll work with you to determine the root cause and a course of action to help improve your health and keep those sheets nice and dry.
"If you're having a severe panic attack, don't hesitate to call an ambulance"
UN experts released a report expressing fears that the COVID-19 pandemic could trigger a global mental health crisis. Isolation, fear, uncertainty and economic difficulties can provoke a state of psychological distress in a person. The fact that millions of people who had never thought about death before faced it as a real threat to themselves and their loved ones is already a complex traumatic shock in itself, experts say.
For those people who had psychological problems before self-isolation, for example, anxiety disorders, the current situation can provoke an exacerbation. One of the most common types of these disorders is panic attacks. These are bouts of sudden fear and intense anxiety for no apparent reason.
One of the most common types of these disorders is panic attacks. These are bouts of sudden fear and intense anxiety for no apparent reason.
During the COVID-19 pandemic, the frequency and intensity of these attacks may increase, and it becomes more difficult to deal with them. This is exactly what happened to 22-year-old Maria.
Mary's story
“You seem to be dying”
— I had my first panic attack at 16. I was still at school then, I remember that they took me out of class and called an ambulance, because it became very bad. It was difficult to breathe, my pulse jumped sharply, my heart began to ache and tingle in my hands.
At such moments you do not understand what is happening to you, it is wildly scary and all the time it seems that you are dying.
My family line is at risk of cardiovascular disease: my grandfather died due to heart problems, my grandmother died because her heart failed during surgery, and my father died because he had coronary heart disease. heart disease. So when I had my first panic attack, a couple of months after my father died, I then thought that I, too, would die due to cardiac arrest.
heart disease. So when I had my first panic attack, a couple of months after my father died, I then thought that I, too, would die due to cardiac arrest.
Cope with fear: four projects to help Muscovites
Read more
But the doctors, based on the results of the ECG examination, assured me that everything was fine with my heart, which led to the idea of vegetative-vascular dystonia in the West, the name "somatoform autonomic dysfunction of the nervous system" is used. - Approx. ed.) and related anxiety disorder.
Since then, I have learned to manage my panic attacks on my own. She took magnesium, valerian, corvalol, motherwort, loaded herself every day with various activities: went to school, worked, studied the Korean language and practiced samulnori (“samulnori” or “samullori” is a Korean musical performance in the traditional style, including playing the national drums tools. - Approx. ed.).
- Approx. ed.).
I thought that if I was doing something all the time and being on the move, then I simply would not have the energy for attacks. I did not consider the help of a specialist for myself, since I believed that a psychotherapist could not afford me.
After some time of self-treatment, severe attacks really stopped happening. Their intensity weakened, for almost five years, panic attacks could happen once or twice a year, because of which I stopped paying attention to the problem.
Coronavirus and isolation
With the news of the coronavirus, I began to worry again, the familiar anxiety returned. When self-isolation was finally introduced in Moscow, the attacks returned with renewed vigor.
They could happen at absolutely any moment, no matter what state I was in or what was happening around me. The attack could have been caused by some external trigger, disturbing news, but it could just as well have happened out of the blue. I tried, as before, to stop with sedatives, but they stopped helping me. Until that moment, I had never had attacks on the same day and they lasted from 15 minutes to an hour - maximum. Now they were repeated several times a day and could last up to three hours non-stop.
Until that moment, I had never had attacks on the same day and they lasted from 15 minutes to an hour - maximum. Now they were repeated several times a day and could last up to three hours non-stop.
After such panic attacks, I was no longer able to concentrate on my studies, or even go to bed. But even if I did manage to fall asleep, panic attacks would cause me to experience sleep surges that could last all night. I woke up with a feeling of causeless fear, a pounding heart and a rapid pulse.
Photo: Flickr.com/Adam R.T. Because of the death of my father, I have a constant fear that something is wrong with my heart and I will die because of it. This thought haunts me, and with it a panic disorder. Therefore, if I feel that my pulse has risen and my arm is tingling, it gives to my chest, the tremor begins, then I kind of understand with my head that everything is physically fine with me, that this is not a heart attack, but the body is already on edge and it is not calm down. There is a feeling of being lost in space and the unreality of what is happening. It's like a vicious circle.
There is a feeling of being lost in space and the unreality of what is happening. It's like a vicious circle.
Imagine if a robber with a gun came up to you on the street and put a gun to your head. You give him everything you have, and the criminal says he won't kill you, but it definitely doesn't make it any easier - the gun is still pointed at you. This is how I feel during panic episodes.
Academic crisis
I am a third-year student of graphic design at the Institute of Economics and Culture: I am engaged in the development of corporate identity, packaging design and printing. As in many other educational institutions, our session was moved online during the quarantine, and my period of increased panic attacks had a very negative impact on my studies, although in normal times I consider myself a fairly collected and diligent student. I stopped attending video conferences because I couldn't focus on the topic of the class. She couldn't do the layout of the magazine or write a term paper, ignored the deadlines and accumulated debts.
For one of the subjects, we were given the task of making an infographic related in some way to the coronavirus outbreak. It will sound ironic, but then I chose the topic “how not to go crazy during self-isolation” with basic recommendations from WHO and Rospotrebnadzor.
It so happened that I had to contact the teacher and ask for a postponement of the deadline, because, they say, I literally went crazy in isolation and I can’t concentrate on my studies because of my condition. The most difficult thing was that, without completing some task, I felt more depressed, I could not relax, and this increased my anxiety even more.
Photo: National Cancer Institute / UnsplashWhere to find help
I live separately from my parents, with my boyfriend. Of course, I shared my anxieties with him, he himself saw everything with his own eyes, but at some point it began to seem to me that I had already exhausted him with my whining. Dima [the young man] is very understanding and caring, but I already felt uncomfortable talking about it with him, I didn’t want to dump my problems on him, so I kept everything to myself.
How to deal with anxiety and return to a safe state
Read more
Communicated on this topic with my mother, more than once. She herself has problems of a similar nature, she told me that she faced the same panic attacks in her youth. Her response to my fears and anxiety was: "Give birth, and all the sores will pass." She kind of understands my condition and supports, trying to console, but does not take seriously. It sounds more like baby talk to her.
During one particularly severe attack, I had to go to the ambulance. By that time, I had not been able to get an appointment at my clinic for more than two weeks and had been putting off going to the ambulance for a long time.
To be honest, it was embarrassing to call and complain about my panic attacks when the doctors there might be busy with people who are now dying. But I understood that I had no other choice, that I could not cope on my own.
Panic attacks won't kill you, but they will definitely make you think and feel like you're dying. And it's unbearable.
At that time, no one came to see me because I did not have a temperature or any other symptoms of coronavirus, they told me to wait for a call from the district hospital. I was first contacted by a local hospital therapist, and the next morning by a psychotherapist. The doctor said that she would call the clinic and ask me to leave a prescription for the drug in my name, which I would have to come and pick up from there, and also allowed me to call her if it got worse.
I am an anxious and impressionable person, I observe quarantine and do not go to crowded places, so going to the hospital was difficult for me in this regard. There was a queue at the entrance to the clinic, no one was allowed inside. One man complained of a cough and headache, but they refused to see him and sent him home with a prescription for antibiotics. A young man approached with a bandaged lip and hand: he got into a fight in a neighboring area and got into the police, came for a bandage and a sick leave - he was also refused admission. As it turned out, there was almost no one in the hospital that day, except for the nurses. At the post I was given a prescription, I went to the pharmacy and bought medicine.
As it turned out, there was almost no one in the hospital that day, except for the nurses. At the post I was given a prescription, I went to the pharmacy and bought medicine.
The drug turned out to be a powerful tranquilizer, and it also happened to be my first treatment and prescription drug experience. At first, it was scary to take the pills because of the long list of side effects, but at the same time, I thought that it couldn’t be worse than what I had already gone through, and I took a chance. I was lucky, tranquilizers really helped. Of course, they must be taken strictly under the supervision of a doctor and according to the recommendations. The psychotherapist who advised me prescribed a course of two weeks, three tablets a day, and then advised me to look at the condition: if it gets worse, then take it again in the same way. At the moment, I have stopped taking it and I feel much better: at night I can finally sleep, and during the day, as before, I can calmly study. For the entire course of taking the attack happened only once, at an early stage.
For the entire course of taking the attack happened only once, at an early stage.
What's next
I realize that I have started my problem a lot, so I plan to start complex treatment when the pandemic ends and it becomes possible to safely visit medical institutions. Take a course of psychotherapy, work through the trauma associated with the death of his father, and take specially selected medications. Although I think panic attacks will stay with me forever, my main goal is to reduce their number and intensity.
I’m skeptical about the lifting of quarantine in Moscow: on the one hand, like everyone else, I’m tired of sitting at home, I’m worried about my parents: they didn’t receive income at the time of quarantine, since my stepfather works in a restaurant (temporarily closed), and my mother quit from his previous place of work just before the start of self-isolation.
On the other hand, the epidemiological situation still does not inspire confidence in me, given the increase in cases and the fact that from the moment of the appearance of each new infected person, quarantine, in fact, moves forward two weeks. Most likely, I will rarely, but I will leave the house in gloves and a mask, with an antiseptic in service. Of course, I will continue to avoid large crowds and try to keep my distance from people in public places and transport.
Most likely, I will rarely, but I will leave the house in gloves and a mask, with an antiseptic in service. Of course, I will continue to avoid large crowds and try to keep my distance from people in public places and transport.
When seizures last as long and painfully as I have, such a situation is very exhausting, reduces the quality of life and motivation, depressive states may appear.
What would I advise, based on my experience, right now, in a pandemic: if you have really severe seizures, none of the known methods help, then you can call an ambulance, and then they will tell you what to do and where address.
And then it needs to be treated. I still can't afford the services of a private psychotherapist, but having tried free medical care in action, I think it's worth starting with this treatment option. It’s just that until you try, nothing will change: yes, panic attacks can go away on their own, but then they will definitely return. This is what I found out from my own experience.
This is what I found out from my own experience.
Psychotherapist's comment
Elena Romanchenko , practicing psychologist, author and host of training programs on working with shock and developmental traumas:
— When a traumatic experience occurs, a person loses contact with reality and, falling into the funnel of trauma, begins to lead as if the trauma is happening in real time. And the task of psychotherapy is to pull a person out of this state, to enable him to see and feel that everything has already happened and passed. In the current conditions of the global crisis and pandemic, there is an unrelenting sense of long-term anxiety in us. The nervous system begins to perceive the state as a constant threat to life, and since the body and psyche are in a chronic expectation of danger, the suppressed traumatic reactions are triggered instantly. Here in the work of the psychotherapist it is important to use resources and techniques that will help the client control what he can cope with, as well as in a healthy way to adapt to what is happening.
Practical tips for dealing with anxiety and preventing panic attacks
- Communication with loved ones. Talk to family members and friends about how you feel. Explore your emotions and try to understand them. This will help you avoid getting caught up in the negative thinking that comes with isolation and fear.
- Breathing exercises. There are many instructions and video tutorials on the Internet that can help with the first symptoms of a panic attack, anxiety and restlessness. If you feel the onset of panic, use the breathing techniques that suit you until all signs of an attack disappear. For prevention: focus on deep slow breathing in the stomach in the morning and in the evening for 10 minutes.
- Outdoor walks. While in isolation, many people experience stress, symptoms of claustrophobia and agoraphobia, in a sense forget about the existence of the world outside the apartment, which creates a certain pressure and a favorable environment for panic.
 We remind you that from June 9, self-isolation was canceled in the capital: Muscovites can freely go outside, take walks and visit public places. Despite the lifting of restrictions, it is necessary to remember to maintain social distance and use personal protective equipment when leaving the house.
We remind you that from June 9, self-isolation was canceled in the capital: Muscovites can freely go outside, take walks and visit public places. Despite the lifting of restrictions, it is necessary to remember to maintain social distance and use personal protective equipment when leaving the house. - Psychological help online. A free consultation with a psychologist can be obtained at the Moscow Psychological Assistance Service. Chat with a psychologist in an online chat, ask a question in a webinar format, or sign up for an individual Skype consultation. You can clarify detailed information on the website of the MSPP and by calling a single reference number: +7 (499) 173-09-09.
Subscribe to telegram channel ASI .
Flashes in the eyes - causes and treatment and treatment in Moscow
Contents
- Causes
- Treatment
Flashes of light in the eyes are an imaginary sensation in which it seems to a person that he sees luminous images of various shapes (lightning bolts, spots, balls of various colors).
This is a symptom characteristic of some diseases and conditions of the eye, but sometimes it can accompany general pathological conditions of the body. Very often the appearance of flashes is combined with the appearance of flying flies before the eyes. As a rule, this occurs when there is a violation in the retina of the eye.
Causes
In different cases, flashes in the eyes can be both a completely harmless manifestation of ordinary eye fatigue, and an indicator of serious problems requiring immediate medical attention. Experts refer to the reasons for their occurrence:
Posterior vitreous detachment . The gel-like substance that fills the central part of the eyeball and attaches to the retina is called the vitreous humor. With age, it begins to shrink and gradually flake off from its original place. At attachment points, the vitreous body pulls the retina, which causes flashes of light in the eyes. This symptom occurs when moving the eyes, is not dangerous and does not require special treatment. However, posterior vitreous detachment is a diagnosis that requires dynamic monitoring by an ophthalmologist. Indeed, a harmless manifestation sometimes masks a more formidable condition - retinal detachment, which, without timely medical care, can lead to irreversible blindness.
However, posterior vitreous detachment is a diagnosis that requires dynamic monitoring by an ophthalmologist. Indeed, a harmless manifestation sometimes masks a more formidable condition - retinal detachment, which, without timely medical care, can lead to irreversible blindness.
Retinal detachments and tears . In some cases, flashes of light before the eyes indicate the onset of retinal detachment. It is especially worth alerting if these symptoms occur after serious physical exertion or severe stress. With retinal detachment or ruptures, flashes of light, as a rule, are accompanied by the appearance of a veil in front of the eye against the background of a sharp decrease in vision. Retinal detachment requires urgent intervention of specialists and hospitalization of the patient.
Migraine . Visual symptoms often precede headache attacks in patients with migraine. At the same time, flashes of light can look like bright zigzag lines, geometric patterns or myriads of sparkles. They usually appear along the periphery of the visual fields, on one or both eyes. True, light flashes of light can occur in the eyes and outside of a headache attack. This condition is called ocular migraine. It should be treated by a neurologist.
They usually appear along the periphery of the visual fields, on one or both eyes. True, light flashes of light can occur in the eyes and outside of a headache attack. This condition is called ocular migraine. It should be treated by a neurologist.
Vascular diseases. These include hypertension, diabetes mellitus, etc. Often, with common chronic vascular pathologies, people note the periodic appearance of flashes in front of their eyes in the dark or with their eyes closed. This is due to short-term spasms in the vessels and a violation of the blood flow in the retinal tissue.
Tumors in the occipital lobe of the brain . In this case, flashes of light are permanent, have a different color and shape.
Inflammatory processes of the retina and choroid. Eye diseases such as retinitis and choroiditis may be accompanied by flashes of light in front of the eyes. However, with them, there are additional symptoms that point specifically to inflammation, despite the fact that both diseases are painless: this is blurred vision and blurred visible objects.
Eye or head injuries. In this case, flashes before the eyes are felt at the moment of impact - injury.
Toxic effects on the body . For example, an overdose of certain medicinal substances or narcotic drugs often leads to flashes of light in front of the eyes.
Treatment
Usually, flashes of light in the eyes, as a symptom, occur once, no longer recurring. True, in the case of posterior vitreous detachment, flashes of light in the eyes may disturb the patient at different intervals, but they do not pose a threat and do not require special treatment. In other cases, to fix the problem, it is necessary to undergo diagnostics and find out the cause of its occurrence. For example, with inflammation of the retina and choroid, flashes in the eyes completely disappear after treatment by an ophthalmologist.
Although it is very often not an ophthalmologist who treats flashes in the eyes after an examination, but a neurologist, endocrinologist or therapist.