Helping depressed spouse
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers. The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
- Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.
 4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk.
 They Hear You.
They Hear You. - Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
- Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses.
 The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States - The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month. The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
- Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.
 4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH) - Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 01/05/2023
Depressed partner support
11/22/2019
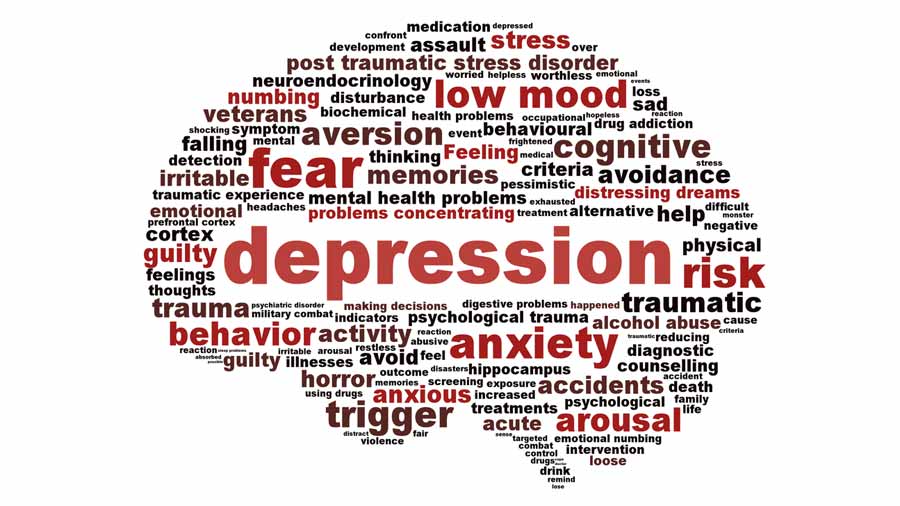
Depression is one of the most common mental disorders, affecting more than 350 million people of all age groups.
Every year about 150 million people in the world lose their ability to work due to depression
The support of family and friends is essential in the treatment of mental disorders. However, depression can negatively impact relationships and leave loved ones feeling helpless, frustrated, or afraid.
However, depression can negatively impact relationships and leave loved ones feeling helpless, frustrated, or afraid.
There are ways people can support a partner with depression on their journey to recovery.
Questions to ask about symptoms
To understand the severity of a person's depression, it is helpful to study how these symptoms affect their life.
Asking about symptoms also shows a person that his partner is interested in his feelings and experiences.
Useful questions to ask include:
- Can you help me understand how you feel?
- What activities do you find enjoyable right now?
- Do you enjoy spending time with other people?
- What's wrong with your energy?
- Do you sleep more or less than usual?
- Do you eat more or less than usual?
- Can you focus on things right now?
- Do you have thoughts of death or suicide?
Questions to avoid
Avoid asking questions that seem judgmental or that place blame on the person with depression.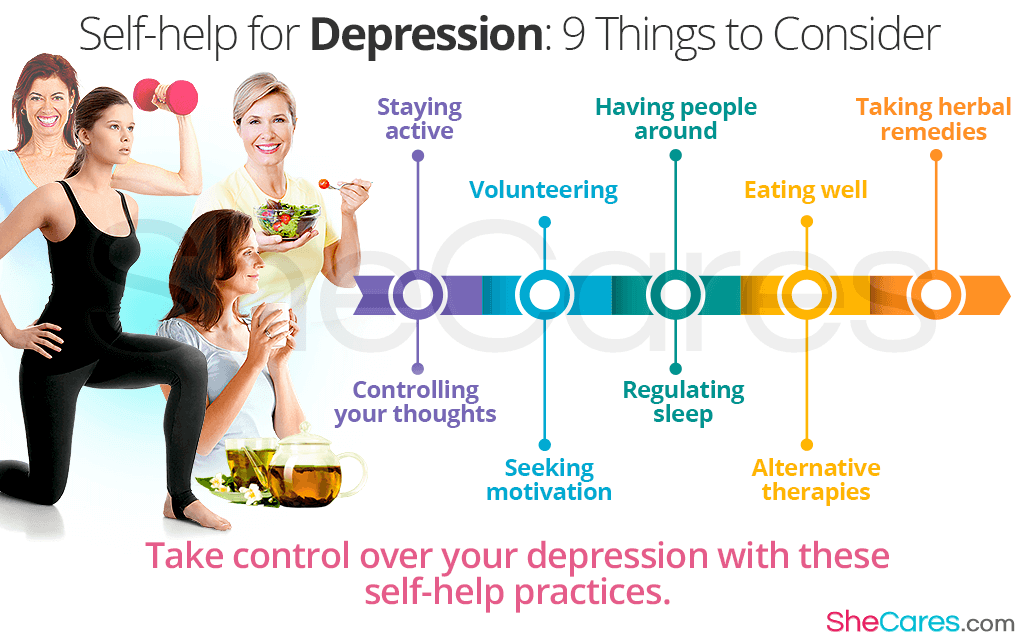 They may already be blaming themselves for their symptoms and need support rather than further judgment.
They may already be blaming themselves for their symptoms and need support rather than further judgment.
It is also important not to oversimplify depression, which is a serious illness.
Examples of questions to avoid include:
- Why can't you just cheer up?
- Don't I make you happy?
- When will you feel better?
- Don't you understand that it's all in your head?
- Why do you attach such importance to this?
- Do you know that others are in a much worse situation than you?
Partner support
1. Learn about depression
Learning about depression can make it easier to support those with depression. Learning about symptoms often helps people recognize symptoms in their loved ones.
Symptoms can range from mild to severe and may change over time. However, symptoms must last at least 2 weeks before a doctor can diagnose depression.
Symptoms of depression may include:
- feelings of sadness, worthlessness or guilt
- loss of interest in previously enjoyable activities
- changes in appetite or weight
- changes in sleep habits
- fatigue and loss of energy
- difficulty concentrating or making decisions
- thoughts of death or suicide
2. Understand and acknowledge your partner's feelings
It is important to listen to a person with depression and express empathy, which is the ability to understand and share other people's feelings. One way to show empathy is to mirror what the person is saying.
For example, if he says, "I just feel like things will never get better," their partner might reflect this by saying, "that sounds like you're not hopeful for the future."
Constant attempts to cheer up a person are useless, as this devalues his condition and feelings. Phrases like “tomorrow will be better” or “try to cheer up” do not take into account the nature of the disease.
Phrases like “tomorrow will be better” or “try to cheer up” do not take into account the nature of the disease.
3. Ask your partner what they want from you
To show further understanding and support, ask the person what they need. He may need:
- medication reminders
- company when visiting a doctor or visiting therapy
- homemade dishes
- encouragement to socialize or exercise
- hug or hold the hand
- to sometimes be left alone
Useful questions to ask include:
- How can I help you?
- Would it be helpful if I...?
4. Encourage your partner to heal
Depression can cause a person to lose their motivation, which can be a barrier to seeking treatment. However, most people with depression need treatment to get better.
Those who support someone with depression can play an important role in their recovery by encouraging them to seek medical help.
To inspire a partner to seek treatment, a person can try:
- joint detection and documentation of your partner's symptoms
- expression of desire to help
- discussion of treatment options such as medication, psychotherapy, and lifestyle changes
- accompaniment to doctor appointments
5. Support your partner during recovery
Recovery from depression can sometimes be difficult. To support a partner in the recovery process:
- help them keep track of their prescriptions and medications
- do some physical exercise together
- plan and prepare healthy meals together
- try to reduce stressors at home
- make your goals small and achievable
- encourage them to socialize with other people
- plan fun activities together
- pay attention to the person's progress towards recovery
- avoid forcing treatment on the person
Let your partner know they are not alone when you say:
- I'm here for you.

- We'll deal with this together.
6. Accept that there will be bad days
People with depression have good days and bad days. To cope with bad days:
- expect them to happen
- understand that this is a normal part of depression
- don't give up love and support at this time
- take some time and do something nice, either alone or with others
- remember that not every day will be like this - there will be good days
7. Take care of yourself
When a person supports a partner with depression, it is very important to take the time to enjoy hobbies and other activities for yourself.
Caring for a partner with depression can be draining, frustrating, and intimidating.
Studies show that having a spouse with depression increases a person's risk of developing depressive symptoms. This risk is especially high when a man is supportive of a depressed woman.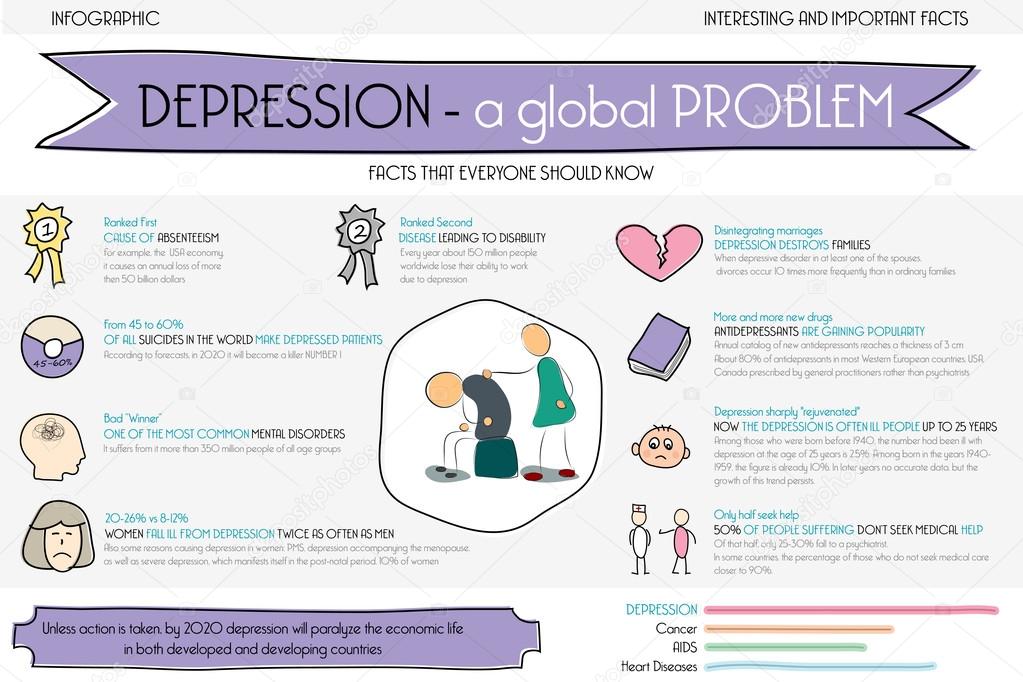
Those caring for someone with a mental illness should also take care of their own mental health. They can do it:
- trying to stay positive
- having realistic expectations about the recovery process
- knowing that they also have the right to be heard and respected
- taking time out and doing pleasurable activities and hobbies
- interacting with people other than their partner
- seeking help from friends or relatives
- doing regular exercise
- eating healthy
- trying to get more sleep and rest
- visiting a psychologist or psychological support groups
Professional support
Professional treatment is an important part of the recovery process. The first step is often to see a doctor, who can recommend treatment, psychotherapy, or both.
For particularly severe depressive symptoms or in life-threatening situations, seek emergency care.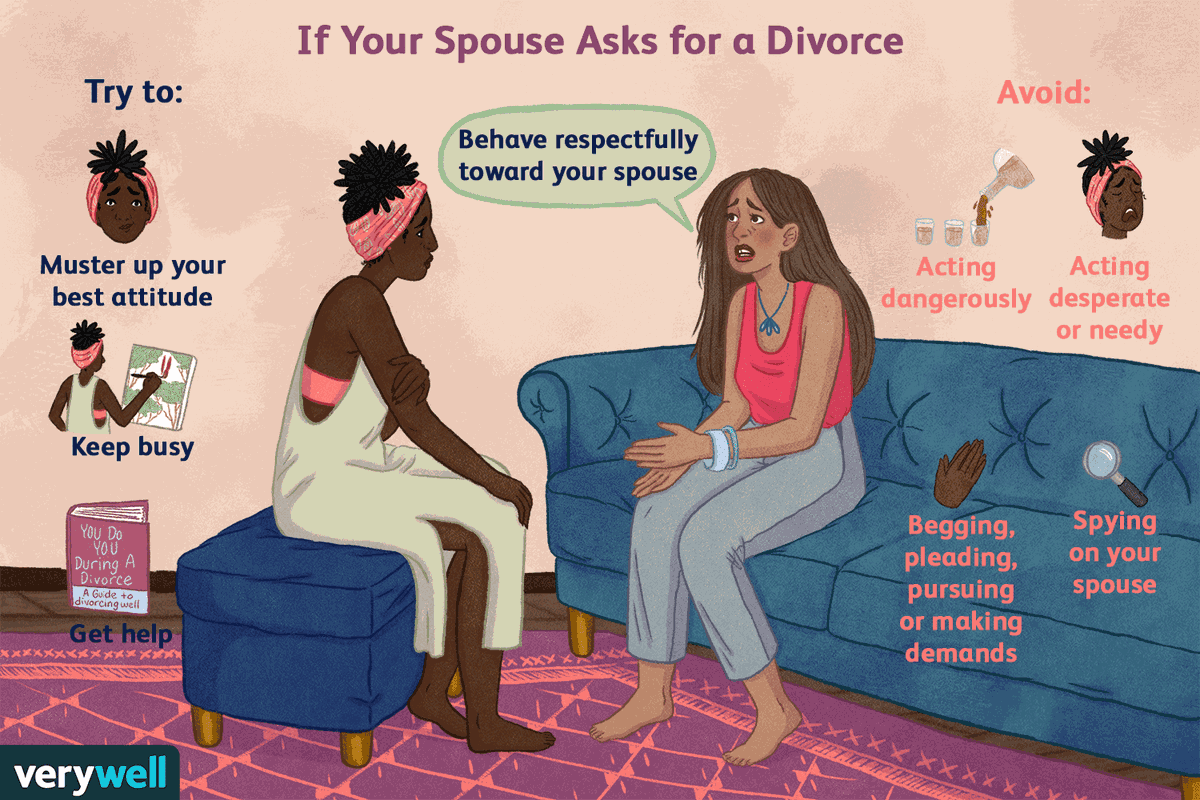
Beginning of form
People with depression may be at risk of suicide. According to the American Foundation for Suicide Prevention, more than half of those who die by suicide suffer from major depression.
Partners of those who suffer from depression should be aware of the warning signs of suicide so that they can take prompt action if necessary. Warning signs include:
- talking about death or suicide
- having a suicide plan
- preparation of means of suicide, e.g. collection of pills
- preparation for death, e.g. by making a will
- distribution of things
- farewell to family and friends
- engaging in risky or reckless behavior
- Extreme changes in mood or personality
- withdrawal from society
If a person suspects that someone is in imminent danger of suicide, they should seek emergency help.
If someone believes that a loved one is contemplating suicide but is not in immediate danger, they should contact the person's doctor and seek support from other family members or a support group.
Support for a partner with depression, both emotional and practical, can help speed up the recovery process.
CONTROL AND INSURANCE ORGANIZATIONS
LEGAL INFORMATION
INDEPENDENT QUALITY ASSESSMENT OF MED. SERVICES
ANTI-CORRUPTION
PRICE LIST FOR PAID SERVICES
VACANCIES
How to help a loved one get out of depression
August 4, 2015 Adviсe
When in a loving couple one of the partners gets depressed, it's hard for both. Sad days come, each of which brings new grief and may be the last for this relationship. But if you stop blaming your partner for a depressed mood and try to help, then depression will recede, and your union will only strengthen.
The word "depression" has been stuck in my teeth lately. It is used everywhere. They denote a protracted bad mood, it is used in jokes and memes. In fact, when true depression comes to your loved one, for some reason it becomes not at all funny, but rather sad and even scary.
You see the changes that happen to your partner: nothing pleases or surprises him, he can lie in bed all day, he is not interested in your conversations and attempts to entertain him. And you are simply torn apart by the influx of thoughts and emotions. Are you the cause of the depression? Maybe the relationship is over? How long will this continue and how can you help?
Depression is a dark experience for a couple. But you can pass it successfully. In this article, we will talk about how to help a partner and save your union. We're touching on the delicate topic of mental health, so you should understand that you don't have to blindly follow all the recommendations. Think about which ones and how you can use them for your couple.
Don't take the symptoms of depression personally
Most of the symptoms of depression make your couple the antithesis of a happy union. A person in depression has a distorted perception of reality: even positive and joyful moments appear to him, if not in black, then definitely in gray.
Of course he doesn't want to go out, go on dates, talk for hours and have sex. But these are generally accepted indicators of a good relationship. It is unlikely that one of your friends says: “We have such a wonderful couple! My beloved comes home in the evening, stares silently at the iPad for three hours, and then goes to bed without saying a word!”
Therefore, having noticed changes in your partner's behavior, you make the only correct conclusion, as it seems to you: he has lost all interest in you. Your friends will actively confirm this guess if you describe the situation to them.
The danger of depression is also in its invisibility. If a person has a broken leg, he also cannot walk and have a lot of sex, but everyone can see why - here is the cast. We cannot point a finger at the internal state, therefore we explain external changes for ourselves in the most common and simple way: love has passed. This conviction is further strengthened if you see that with other people your partner continues to behave as before, and alone with you - it deflates like a balloon. Literally, Darling's blog claims it's actually good:
Literally, Darling
blog
We almost always take the constant bad mood of a loved one at our own expense. You begin to feel that you are the cause of the oppressed state. A depressed person cannot behave as usual, and even more so with loved ones who know him thoroughly. While among strangers, he can pretend for a short time that everything is in order.
Naturally, it hurts you to see how your partner behaves quite normally with others and completely changes around you. But, surprisingly, this is a good sign. This means that he completely trusts you, loves you and allows himself to reveal what is really in his soul. If he sometimes tries to push you away, do not be offended, move away, but stay close.
Depression can affect a person for many reasons: illness or death of loved ones, one's own poor health, problems at work, difficulties with relatives or friends. But its symptoms will affect you first of all: he will suddenly become bored talking to you, he will not want to go somewhere or even watch TV shows in the evening.
If you can't get rid of the idea that your partner just doesn't want to be with you, ask them directly. And when he answers that it's not about you, accept this answer, calm down and start solving the problem of his poor moral health together.
Develop a depression recovery plan together
Don't take depression symptoms personally, but don't ignore them either. Yes, your partner is not showing any romantic feelings right now, but he will still be hurt if you dismiss his condition. If your loved one is sick or injured, you do not blame him, but take care of him and help him recover. Do the same with depression.
In fact, for someone who is trying to cope with a depressed state of mind, relationships are a huge help. But only if you are moving in the same direction and acting together: you need to understand your partner and take practical steps together. The Anxiety and Depression Association of America offers a variety of techniques to deal with depression: studying your condition, setting goals, recording results. However, the best method of treatment is joint work with a loving person.
American Depression Association
Mental health professionals are increasingly recommending couples and family treatment programs. After training with a doctor, a partner or family member can help the patient at home, that is, provide round-the-clock therapy for him. The "house doctor" should be near the patient in situations that exacerbate anxiety and bad mood, and support him by reducing anxiety.
Your partner may not want to be treated. In this case, you can not press on him and rush him. You can support, but not force. You can try to start by looking for a good doctor together or reading articles about treatment. The main thing for the two of you is to understand that you are together and you are moving in the same direction.
If your efforts are frustrated by your partner's stubbornness, if he rejects your support and is sure that he does not need help, then decide for yourself whether you want to continue in this relationship and wait for positive changes, or do you not have the strength for this? But do not be a tractor for your partner, he must only understand and accept that he needs help.
Give your partner some space.
Treatment for depression will always be a mess. It's like letting your cat stomp on paint and then run across a white sheet. It seems that your treatment plan has been worked out in detail, goals have been set, everything is neatly recorded in a journal of observations, and you are cheerfully moving along the right path.
But one morning the patient wakes up and feels hopeless... Everything is bad, so much hard work has been done, but nothing helps, the soul is still empty and terribly depressing. It would be better now to curl up in a ball of sadness and renounce the whole world.
This happens, and it is natural. But at these moments you want to either give your patient a good kick so that he stops sour, or completely abandon the treatment, because it does not bear fruit. Take your time, one bad day is not the end of the world. Although your love will not be the main cure for depression, it is still important for the patient, says psychotherapist Rita de Maria.
Rita de Maria
psychotherapist
Your partner needs your love, your presence, your warmth. It won't stop depression, just as it won't, for example, lower blood sugar or relieve arthritis pain. And yet, your feelings can change the “broken” processes in your partner’s head, revive his positive thoughts and raise his self-esteem during this difficult period.
Depression radically changes the habitual life. What made you happy ceases to make you happy; what fascinated or interested now does not evoke even a drop of emotions. The presence next to someone who accepts this state without judgment or resentment is very supportive and even inspiring.
Set limits to save yourself
It's always hard to keep a depressed person going. Sometimes the overexertion will reach proportions that will endanger your own mental health. There is no need for sacrifices like: “I will do everything so that my loved one is healthy.” When helping a partner, set clear boundaries for your presence, do not completely dissolve in his state. Leave time for your hobbies, meetings with friends, and just to be alone.
Sure you want to help. But you don’t need to subordinate your life to your partner’s depression, for this you will pay with the stability of your morale. You may even refuse to be your loved one's "home therapist" if you feel that this is too much for you.
![]()