Having obsessive thoughts
When Unwanted Thoughts or Repetitive Behaviors Take Over
People who are distressed by recurring, unwanted, and uncontrollable thoughts or who feel driven to repeat specific behaviors may have obsessive-compulsive disorder (OCD). The thoughts and behaviors that characterize OCD can interfere with daily life, but treatment can help people manage their symptoms.
What is OCD?
OCD is a common, long-lasting disorder characterized by uncontrollable, recurring thoughts (obsessions) that can lead people to engage in repetitive behaviors (compulsions).
Although everyone worries or feels the need to double-check things on occasion, the symptoms associated with OCD are severe and persistent. These symptoms can cause distress and lead to behaviors that interfere with day-to-day activities. People with OCD may feel the urge to check things repeatedly or perform routines for more than an hour each day as a way of achieving temporary relief from anxiety.
If OCD symptoms are not treated, these behaviors can disrupt work, school, and personal relationships and can cause feelings of distress.
OCD symptoms tend to emerge in childhood, around age 10, or in young adulthood, around age 20 to 21, and they often appear earlier in boys than in girls. Most people are diagnosed with OCD by the time they reach young adulthood.
What are the signs and symptoms of OCD?
People with OCD may have obsessions, compulsions, or both.
Obsessions are repeated thoughts, urges, or mental images that cause anxiety. Common obsessions include:
- Fear of germs or contamination
- Fear of forgetting, losing, or misplacing something
- Fear of losing control over one’s behavior
- Aggressive thoughts toward others or oneself
- Unwanted, forbidden, or taboo thoughts involving sex, religion, or harm
- Desire to have things symmetrical or in perfect order
Compulsions are repetitive behaviors that a person feels the urge to do in response to an obsessive thought. Common compulsions include:
Common compulsions include:
- Excessive cleaning or handwashing
- Ordering or arranging items in a particular, precise way
- Repeatedly checking things, such as that the door is locked or the oven is off
- Compulsive counting
How do I know if it’s OCD?
Not all rituals or habits are compulsions. Everyone double-checks things sometimes. In general, people with OCD:
- Can't control their obsessive thoughts or compulsive behaviors, even when they recognize those thoughts or behaviors as excessive
- Spend at least 1 hour a day on these obsessive thoughts or compulsive behaviors
- Don’t get pleasure when performing compulsive behaviors or rituals, but may feel brief relief from the anxiety brought on by obsessive thoughts
- Experience significant problems in daily life due to these thoughts or behaviors
Some individuals with OCD also have a tic disorder. Motor tics are sudden, brief, repetitive movements, such as eye blinking and other eye movements, facial grimacing, shoulder shrugging, and head or shoulder jerking. Common vocal tics include repetitive throat-clearing, sniffing, or grunting sounds. It is common for people with OCD also to have a diagnosed mood disorder or anxiety disorder.
Common vocal tics include repetitive throat-clearing, sniffing, or grunting sounds. It is common for people with OCD also to have a diagnosed mood disorder or anxiety disorder.
Symptoms of OCD may come and go, ease over time, or worsen. People with OCD may try to help themselves by avoiding situations that trigger their obsessions, or they may use alcohol or drugs to calm themselves. Although most adults with OCD recognize that their compulsive behaviors don’t make sense, some adults and most children may not realize that their behavior is out of the ordinary. Parents or teachers typically recognize OCD symptoms in children.
If you think you or your child may have OCD, talk to a health care provider about the possible symptoms. If left untreated, OCD can interfere in all aspects of life.
What causes OCD?
The exact causes of OCD aren’t known; however, a variety of factors are associated with an increased chance of developing the disorder.
Genetics is one factor associated with OCD. Studies have shown that having a first-degree relative (parent, sibling, or child) with OCD is associated with an increased chance of developing the disorder. Scientists have not identified any one gene or set of genes that definitively lead to OCD, but studies exploring the connection between genetics and OCD are ongoing.
In addition to genetics, other biological factors may play a role. Brain imaging studies have shown that people with OCD often have differences in the frontal cortex and subcortical structures of the brain, areas of the brain that underlie the ability to control behavior and emotional responses. Researchers also have found that several brain areas, brain networks, and biological processes play a key role in obsessive thoughts, compulsive behavior, and associated fear and anxiety. Research is underway to better understand the connection between OCD symptoms and parts of the brain.
Some studies have reported an association between childhood trauma and obsessive-compulsive symptoms. More research is needed to understand this relationship.
More research is needed to understand this relationship.
Children who develop a sudden onset or worsening of OCD symptoms after a streptococcal infection may be diagnosed with a condition called Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS).
How is OCD treated?
The first step is to talk with your health care provider about your symptoms. Asking questions and providing information to your health care provider can improve your care.
Your health care provider will perform a physical exam and ask you about your health history to make sure that your symptoms are not caused by other illnesses or conditions. Your health care provider may refer you to a mental health professional, such as a psychiatrist, psychologist, social worker, or counselor, for further evaluation or treatment.
Treatment for OCD typically includes specific types of psychotherapy (such as cognitive behavioral therapy), medication, or a combination of the two. A mental health professional can talk about the benefits and risks associated with different treatment options and help identify the best treatment for you. Sometimes people with OCD also have other mental illnesses, such as anxiety, depression, and body dysmorphic disorder, a disorder in which someone mistakenly believes that a part of their body is abnormal. It is important to consider these other disorders when making decisions about treatment.
A mental health professional can talk about the benefits and risks associated with different treatment options and help identify the best treatment for you. Sometimes people with OCD also have other mental illnesses, such as anxiety, depression, and body dysmorphic disorder, a disorder in which someone mistakenly believes that a part of their body is abnormal. It is important to consider these other disorders when making decisions about treatment.
It is important to follow your treatment plan because both psychotherapy and medication can take some time to work. Although there is no cure for OCD, current treatments help many people with the disorder manage their symptoms, engage in day-to-day activities, and lead full, active lives.
For tips on how to talk to your health care provider about your mental health and get the most out of your visit, read the National Institute of Mental Health (NIMH) fact sheet, Taking Control of Your Mental Health: Tips for Talking With Your Health Care Provider.
Psychotherapy
Psychotherapy can be an effective treatment for adults and children with OCD. Research shows that certain types of psychotherapy, including cognitive behavioral therapy (CBT) and other related therapies (such as habit reversal training), can be as effective as medication for many people. For others, psychotherapy may be most effective when used in combination with medication.
Research shows that a specific type of CBT called Exposure and Response Prevention (ERP) is effective for reducing compulsive behaviors, even for people who did not respond well to medication. With ERP, people spend time in a situation that triggers their compulsion (such as touching dirty objects) and they are prevented from engaging in their typical compulsion (such as handwashing). Although this approach may cause feelings of anxiety at first, compulsions decrease for most people as they continue treatment.
Children with OCD may need additional help from family members and health care providers when it comes to recognizing and managing their OCD symptoms. Mental health professionals can work with young patients to identify strategies for managing stress and increasing support so that the children are able to manage their OCD symptoms at school and at home.
Mental health professionals can work with young patients to identify strategies for managing stress and increasing support so that the children are able to manage their OCD symptoms at school and at home.
Medication
Your health care provider may prescribe medication to help treat OCD. Serotonin reuptake inhibitors (SRIs) are the most common type of medication prescribed for the treatment of OCD.
SRIs, including selective serotonin reuptake inhibitors (SSRIs), are often used to treat depression, and they also are helpful for treating symptoms of OCD. With SRI treatment, it may take up to 8 to 12 weeks before symptoms begin to improve, and treatment for OCD may require higher SRI doses than are typically used in treating depression. For some people, these medications may cause side effects such as headaches, nausea, or difficulty sleeping.
People respond to medication in different ways, but most people with OCD find that medication, often in combination with psychotherapy, can help them manage their symptoms.
Your health care provider can adjust medication doses over time to minimize any side effects or withdrawal symptoms. Do not stop taking your medication without talking to your health care provider first. Your health care provider will work with you to monitor your health and can adjust the treatment plan in a safe and effective way.
The most up-to-date information on medications, side effects, and warnings is available on the U.S. Food and Drug Administration (FDA) website.
Other Treatments
In 2018, FDA approved the use of transcranial magnetic stimulation (TMS), most commonly used in treating depression, as an add-on treatment for adults with OCD. You can learn more about brain stimulation therapies, including TMS, on the NIMH website.
Beyond Treatment: Things You Can Do
There are several important things you can do to manage stress and anxiety associated with OCD.
- Create a consistent sleep schedule.
- Make regular exercise a part of your routine.

- Eat a healthy, balanced diet.
- Seek support from trusted family and friends.
Where can I go for help?
If you’re not sure where to get help, your health care provider is a good place to start. Your health care provider can refer you to a qualified mental health professional, such as a psychiatrist or psychologist, who has experience treating OCD and can evaluate your symptoms.
You can learn more about getting help and finding a health care provider on NIMH's Help for Mental Illnesses webpage. The Substance Abuse and Mental Health Services Administration (SAMHSA) has an online tool to help you find mental health services in your area.
I know someone who is in crisis. What do I do?
If you or someone you know is having thoughts about wanting to die or is thinking about hurting themselves or someone else, get help quickly.
- Do not leave a person who is in crisis alone.

- Call 911 or go to the nearest hospital emergency room.
- Call the toll-free National Suicide Prevention Lifeline at 1-800-273-TALK (8255). You also can text the Crisis Text Line (text HELLO to 741741) or use the Lifeline Chat on the National Suicide Prevention Lifeline website. These services are confidential, free, and available 24/7.
Participating in Clinical Research
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you. For more information, visit NIMH’s clinical trials webpage.
Reprints
This publication is in the public domain and may be reproduced or copied without permission from NIMH. Citation of NIMH as a source is appreciated. To learn more about using NIMH publications, please contact the NIMH Information Resource Center at 1-866‑615‑6464, email [email protected], or refer to our reprint guidelines.
For More Information
MedlinePlus (National Library of Medicine) (En español)
ClinicalTrials.gov (En español)
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
National Institutes of Health
NIH Publication No. 20-MH-4676
Revised 2020
Obsessive-compulsive disorder (OCD) - Symptoms and causes
Overview
Obsessive-compulsive disorder (OCD) features a pattern of unwanted thoughts and fears (obsessions) that lead you to do repetitive behaviors (compulsions). These obsessions and compulsions interfere with daily activities and cause significant distress.
You may try to ignore or stop your obsessions, but that only increases your distress and anxiety. Ultimately, you feel driven to perform compulsive acts to try to ease your stress. Despite efforts to ignore or get rid of bothersome thoughts or urges, they keep coming back. This leads to more ritualistic behavior — the vicious cycle of OCD.
OCD often centers around certain themes — for example, an excessive fear of getting contaminated by germs. To ease your contamination fears, you may compulsively wash your hands until they're sore and chapped.
If you have OCD, you may be ashamed and embarrassed about the condition, but treatment can be effective.
Symptoms
Obsessive-compulsive disorder usually includes both obsessions and compulsions. But it's also possible to have only obsession symptoms or only compulsion symptoms. You may or may not realize that your obsessions and compulsions are excessive or unreasonable, but they take up a great deal of time and interfere with your daily routine and social, school or work functioning.
You may or may not realize that your obsessions and compulsions are excessive or unreasonable, but they take up a great deal of time and interfere with your daily routine and social, school or work functioning.
Obsession symptoms
OCD obsessions are repeated, persistent and unwanted thoughts, urges or images that are intrusive and cause distress or anxiety. You might try to ignore them or get rid of them by performing a compulsive behavior or ritual. These obsessions typically intrude when you're trying to think of or do other things.
Obsessions often have themes to them, such as:
- Fear of contamination or dirt
- Doubting and having difficulty tolerating uncertainty
- Needing things orderly and symmetrical
- Aggressive or horrific thoughts about losing control and harming yourself or others
- Unwanted thoughts, including aggression, or sexual or religious subjects
Examples of obsession signs and symptoms include:
- Fear of being contaminated by touching objects others have touched
- Doubts that you've locked the door or turned off the stove
- Intense stress when objects aren't orderly or facing a certain way
- Images of driving your car into a crowd of people
- Thoughts about shouting obscenities or acting inappropriately in public
- Unpleasant sexual images
- Avoidance of situations that can trigger obsessions, such as shaking hands
Compulsion symptoms
OCD compulsions are repetitive behaviors that you feel driven to perform. These repetitive behaviors or mental acts are meant to reduce anxiety related to your obsessions or prevent something bad from happening. However, engaging in the compulsions brings no pleasure and may offer only a temporary relief from anxiety.
These repetitive behaviors or mental acts are meant to reduce anxiety related to your obsessions or prevent something bad from happening. However, engaging in the compulsions brings no pleasure and may offer only a temporary relief from anxiety.
You may make up rules or rituals to follow that help control your anxiety when you're having obsessive thoughts. These compulsions are excessive and often are not realistically related to the problem they're intended to fix.
As with obsessions, compulsions typically have themes, such as:
- Washing and cleaning
- Checking
- Counting
- Orderliness
- Following a strict routine
- Demanding reassurance
Examples of compulsion signs and symptoms include:
- Hand-washing until your skin becomes raw
- Checking doors repeatedly to make sure they're locked
- Checking the stove repeatedly to make sure it's off
- Counting in certain patterns
- Silently repeating a prayer, word or phrase
- Arranging your canned goods to face the same way
Severity varies
OCD usually begins in the teen or young adult years, but it can start in childhood. Symptoms usually begin gradually and tend to vary in severity throughout life. The types of obsessions and compulsions you experience can also change over time. Symptoms generally worsen when you experience greater stress. OCD, usually considered a lifelong disorder, can have mild to moderate symptoms or be so severe and time-consuming that it becomes disabling.
Symptoms usually begin gradually and tend to vary in severity throughout life. The types of obsessions and compulsions you experience can also change over time. Symptoms generally worsen when you experience greater stress. OCD, usually considered a lifelong disorder, can have mild to moderate symptoms or be so severe and time-consuming that it becomes disabling.
When to see a doctor
There's a difference between being a perfectionist — someone who requires flawless results or performance, for example — and having OCD. OCD thoughts aren't simply excessive worries about real problems in your life or liking to have things clean or arranged in a specific way.
If your obsessions and compulsions are affecting your quality of life, see your doctor or mental health professional.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Causes
The cause of obsessive-compulsive disorder isn't fully understood. Main theories include:
- Biology.
 OCD may be a result of changes in your body's own natural chemistry or brain functions.
OCD may be a result of changes in your body's own natural chemistry or brain functions. - Genetics. OCD may have a genetic component, but specific genes have yet to be identified.
- Learning. Obsessive fears and compulsive behaviors can be learned from watching family members or gradually learned over time.
Risk factors
Factors that may increase the risk of developing or triggering obsessive-compulsive disorder include:
- Family history. Having parents or other family members with the disorder can increase your risk of developing OCD.
- Stressful life events. If you've experienced traumatic or stressful events, your risk may increase. This reaction may, for some reason, trigger the intrusive thoughts, rituals and emotional distress characteristic of OCD.

- Other mental health disorders. OCD may be related to other mental health disorders, such as anxiety disorders, depression, substance abuse or tic disorders.
Complications
Problems resulting from obsessive-compulsive disorder may include, among others:
- Excessive time spent engaging in ritualistic behaviors
- Health issues, such as contact dermatitis from frequent hand-washing
- Difficulty attending work, school or social activities
- Troubled relationships
- Overall poor quality of life
- Suicidal thoughts and behavior
Prevention
There's no sure way to prevent obsessive-compulsive disorder. However, getting treatment as soon as possible may help prevent OCD from worsening and disrupting activities and your daily routine.
By Mayo Clinic Staff
Related
Associated Procedures
Obsessive Compulsive Disorder Treatment
Great Thought is an obsessive compulsive disorder treatment program. We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
Symptoms of obsessive-compulsive disorder
- Frightening images and drives
- Compulsive acts (rituals)
- Intrusive check of one's own actions
- Fear of trouble, pollution or infection
- Inexplicable desire to count something
- Excessive organization and pedantry
- Perfectionism in relationships, work and even leisure
- "Stuck", "looping" on one's thoughts
You feel that over time your mood becomes worse: apathy, depression, obsessions increase, and rituals begin to fill all your free time or harm your physical health.
You may have had more than one meeting with psychologists, psychotherapists and psychiatrists. You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder is a syndrome characterized by the presence of obsessive thoughts (obsessions) to which a person reacts with certain actions (compulsions). The causes of the disorder are rarely superficial. The syndrome is also accompanied by the development of obsessive memories and various pathological phobias. May be chronic, episodic or progressive.
Obsession - obsessive thought, persistent desire for something, uncontrollable and accompanied by anxiety and intense anxiety. In an attempt to cope with such thoughts, a person resorts to committing compulsions.
Compulsion - an irresistible need to perform certain actions (rituals), which can be assessed by the person himself as irrational or meaningless, and the internal need to perform them is forced and is the result of obsessive ideas.
Common examples of OCD manifestations
- An exaggerated sense of danger.
 Fear of the materiality of thoughts:
Fear of the materiality of thoughts: - "now I will lose control and hurt my loved ones"
- "something terrible is about to happen, I can feel it"
- "I shouldn't think like that, all this will come true because of me"
- Pathological fear of pollution. Thirst for Purity
- Excessive perfectionism, exaggerated responsibility - "everything must be done perfectly", "everything depends on me, mistakes are unacceptable"
How does this painful algorithm work?
Most people have unwanted or obsessive thoughts quite often, but all sufferers of the disorder greatly exaggerate their importance. Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
As we noted earlier, repetitive avoidance behavior can "get stuck", "loop", that is, have a tendency to repeat. The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
If you periodically experience over the years:
- Constant or fluctuating anxiety
- The need to perform certain ritualized actions
- A persistent decline in the quality of life due to the need to avoid certain thoughts and actions, places and events
And you are also persecuted:
- Significant problems in studies and career
- Failure to establish a serious relationship
- Constant criticism and pressure from relatives
- Many senseless activities
- Excessive involvement in computer games and the Internet, alcohol
- Loneliness and isolation
We strongly recommend that you do not delay seeking help and that you complete a remedial program. Consultations and psychotherapeutic sessions according to the program are held several times a week, until the relief of severe symptoms, then the frequency of meetings with specialists is reduced to 2–3 per month.
Count on the fact that in the end we will deal with your problem together.
Treatment of obsessive-compulsive disorder in Neuro-Psi
Every day, the specialists of the NEURO-PSI clinic analyze the world practice in the field of psychiatry and psychotherapy. The goal is the impartial selection and implementation of those methods of treatment and psychological assistance, the effectiveness of which has been convincingly proven in independent studies.
We are guided by the principles of evidence-based medicine and use as a basic method of treatment a psychotherapeutic paradigm, the effectiveness of which has been widely recognized by the professional community.
1. What is the essence of the obsessive-compulsive disorder treatment program
Since obsessive thoughts, rituals and conditions are only symptoms of mental dysfunction, the root cause must be treated in order to achieve a stable result. A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
The main emphasis is on teaching the client how to properly respond to his thoughts, emotions, inner feelings and interpretation of external events.
All types of psychotherapeutic and drug treatments serve the same goal: to achieve the best result in the shortest possible time. At the same time, by coordinating the efforts of specialists in various fields, the most complete coverage of all types of mental illnesses, disorders and disorders is possible.
2. What treatments are used
- Priority:
- Cognitive-Behavioral Therapy.
- Schema Therapy.
- Reality Therapy.
- Choice Theory.
- Rational pharmacotherapy.
- Psychopharmacotherapy (if indicated)
- Biofeedback Therapy
- Rational psychocorrection of stress
- Jacobson progressive muscle relaxation.
- Traditional and modern gymnastic systems, relaxation techniques.
- Breathing techniques .
- Stress exposure.
- Self-control training.
- Lifestyle modification
- Work with bad habits.
- Diet correction.
- Professional and social adaptation.
3. How is the treatment under the program
Each treatment program at the NEURO-PSI clinic consists of four stages:
- diagnostics,
- work with disease symptoms,
- work with the causes of the disease,
- consolidation of the achieved results.
Work efficiency is increased by dividing the treatment process into a predetermined number of sessions, at convenient times and without hospitalization. This means that each program is adapted to the problem that the client has addressed.
The program method of treatment is predictable, time-limited, productive, and, most importantly, understandable for the client.
Of course, the treatment takes place in a comfortable mode without interruption from work, study or family. Specialists of various profiles will work with you (team method). This is necessary to minimize the risk of diagnostic errors that could lead to the adoption of a suboptimal treatment plan.
Specialists of various profiles will work with you (team method). This is necessary to minimize the risk of diagnostic errors that could lead to the adoption of a suboptimal treatment plan.
Improvements in well-being and mood (healing) occur in stages: after the decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future.
4. What are the results and prognosis?
Upon completion of the program, you get rid of obsessive thoughts and rituals, fear of pollution, unmotivated fears, panic attacks and multiple vegetative symptoms (sudden jumps in blood pressure, heart palpitations, dizziness, nausea).
According to statistics, the effectiveness of the methods used approaches 100% if all recommendations of specialists are followed.
Skills you acquire during the program:
- self-control and self-regulation
- constructive analysis of the state of the body
- understanding one's own mental and emotional sphere
- ability to control one's attention
- ability to act consciously in stressful situations
Significantly improves the emotional and physical condition, gains self-confidence, in the future. Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
5. Where to start taking the course
In order for you to know the treatment plan, we recommend signing up for a diagnostic (first) consultation.
treatment, causes, how to deal with obsessive thoughts
Obsessive thoughts (obsessions) are images or urges that uncontrollably, against the will of a person, invade consciousness. Attempts to get rid of these thoughts lead to outbreaks of anxiety and bring great discomfort. A person experiences constant fears and bad thoughts. If you do not seek help in time, obsessions lead to psychological exhaustion, social isolation and depression.
Obsessive thoughts are found in many diseases: neurosis, depression, obsessive-compulsive disorder (obsessive-compulsive disorder) and even schizophrenia.
Features that distinguish obsessive thoughts syndrome:
- a person cannot influence the appearance of such thoughts, thoughts arise against desire;
- obsessive thoughts are not connected with the usual thoughts of a person - they are separate, alien images;
- the syndrome of obsessive thoughts cannot be overcome by an effort of will;
- the disorder is associated with intense anxiety, irritability;
- clarity of consciousness and critical perception of one's state are usually preserved.

The disorder is extremely difficult to bear. Usually a person realizes what obsessive thoughts mean, understands all the irrationality of the images that arise in the head, but cannot fight them. Attempts to stop the appearance of thoughts and the coercive actions associated with them are unsuccessful and lead to even greater experiences.
It is not difficult to convince people who suffer from this disorder that their obsessive thoughts have no basis. But it doesn't help to get rid of the problem. Situations repeat themselves over and over. A necessary step to get rid of painful conditions is to seek help from a specialist before complications arise.
What are obsessive thoughts
Obsessive thoughts torment a person, they are unpleasant and disturbing, you want to hide from them, run away. There are all kinds of obsessions.
Here are some examples of intrusive thoughts:
- concerns about pollution and disease;
- pathological need for order and symmetry;
- obsessive and uncontrolled account;
- obsessive thoughts about the bad: a person constantly thinks about accidents that can happen to him, to his loved ones, to his property, or even to humanity as a whole;
- groundless and unreasonable avoidance of certain actions or objects;
- thoughts of a religious, sexual, aggressive or any other orientation, which are alien to the thinking of the patient and arise against the will.

Constant intrusive thoughts cause unbearable discomfort. Of course, a person has a desire to succumb to these ideas and try to correct the situation. In this case, compulsions appear - actions that a person is forced to periodically perform, even if he does not want to, in order to control what is happening in his head. When obsessive thoughts (obsessions) and obsessive actions (compulsions) are present together, time-consuming, disruptive, and distressing, it indicates the presence of a disease such as obsessive-compulsive disorder (OCD).
A person begins to avoid cracks in the asphalt or touches every tree on the road because alien thoughts “tell” him that if he does not do this, something bad will happen.
Usually compulsions make you do something over and over again, like a ritual. By giving in to coercion, the person hopes that they can prevent or reduce the anxiety that accompanies obsessions. For example, he begins to avoid cracks in the asphalt or touches every tree on the road because alien thoughts "tell" him that if he does not do this, something bad will happen. Unfortunately, such actions do not bring relief and only get worse over time, taking the form of an endless ritual.
Unfortunately, such actions do not bring relief and only get worse over time, taking the form of an endless ritual.
In addition to OCD, there are other diseases in psychiatry that are characterized by different types of obsessive thoughts. Here is some of them:
- phobias,
- neurasthenia,
- schizophrenia.
A phobia is an anxiety disorder characterized by panic and an uncontrollable, irrational fear of certain situations or objects. Strong anxiety can arise even when thinking about a frightening situation, so the patient tries with all his might to avoid a terrible object. All terrible obsessive thoughts and anxieties are associated exclusively with this object.
There are different types of phobias. The most common:
- agoraphobia — fear of open spaces or crowded places;
- social phobia - fear of social interactions. There are other specific phobias that can relate to anything: airplanes, specific animals, the sight of blood.
A phobic disorder may include panic attacks - attacks of fear, which are accompanied by a feeling of impending death and physical sensations: retrosternal pain, interruptions in the heart, dizziness, feeling short of breath, numbness of the extremities, intestinal disorders. All this significantly limits the personal life and performance of a person.
Neurasthenia is a disorder that is associated with exhaustion of the nervous system. It happens after a long illness, physical overload, severe or prolonged stress. Characterized by persistent headache, symptoms of cardiovascular disorders, indigestion and sleep.
Intrusive delusional thoughts may be one of the manifestations of schizophrenia, but the diagnosis is made only in the presence of other signs of schizophrenia.
The disease has three forms-stages that develop one after another. In the hypersthenic form, emotional lability, irritability and intolerance are observed.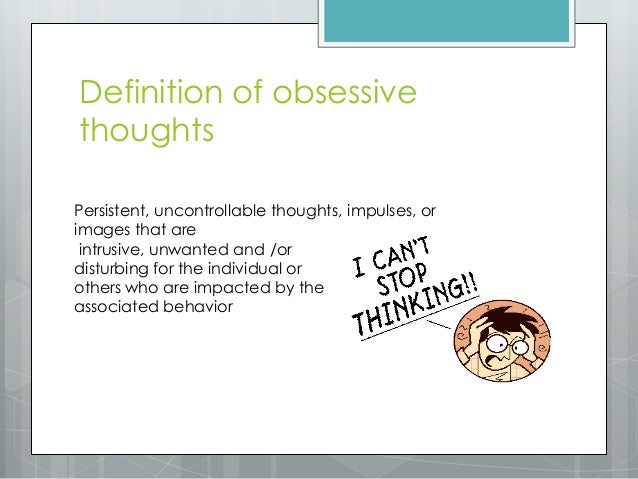 In the second phase, which is called "irritable weakness", aggression and irritation are quickly replaced by emotional exhaustion and impotence. In the third, hyposthenic form, the patient arrives in a state of constant fatigue and bad mood. He focuses on his inner feelings, which depresses him even more. This phase is characterized by obsessive thoughts of a hypochondriacal nature.
In the second phase, which is called "irritable weakness", aggression and irritation are quickly replaced by emotional exhaustion and impotence. In the third, hyposthenic form, the patient arrives in a state of constant fatigue and bad mood. He focuses on his inner feelings, which depresses him even more. This phase is characterized by obsessive thoughts of a hypochondriacal nature.
Schizophrenia is a complex polymorphic mental illness characterized by a fundamental impairment of perception and the breakdown of thought processes. The clinical picture is varied and depends on the form of the disease: hallucinations, delusions, loss of natural mental functions, personality distortion, and much more.
A sick person who suffers from this disease needs full treatment from a psychiatrist. Intrusive delusional thoughts may be one of the manifestations of schizophrenia, but the diagnosis is made only in the presence of other signs that are specific, diagnostically significant criteria for this disorder.
Causes of obsessive thoughts
The occurrence of obsessions is directly related to the underlying disease. For treatment to be effective, an accurate diagnosis is essential. It is not always possible to accurately answer the question of where obsessive thoughts come from. Factors that contribute to the occurrence of this disorder have been identified:
- genetic predisposition;
- impaired brain function due to organic or biochemical causes, including imbalance of neurotransmitters;
- mental trauma and stress;
- personality traits: people with sensitive and labile temperament;
- The presence of somatic and infectious diseases, disability, pregnancy are predisposing causes of obsessive thoughts.
There are many disorders in which this syndrome occurs, so the diagnosis should be carried out by a highly qualified psychiatrist who can understand the intricacies of the clinical picture and understand why obsessive thoughts arise.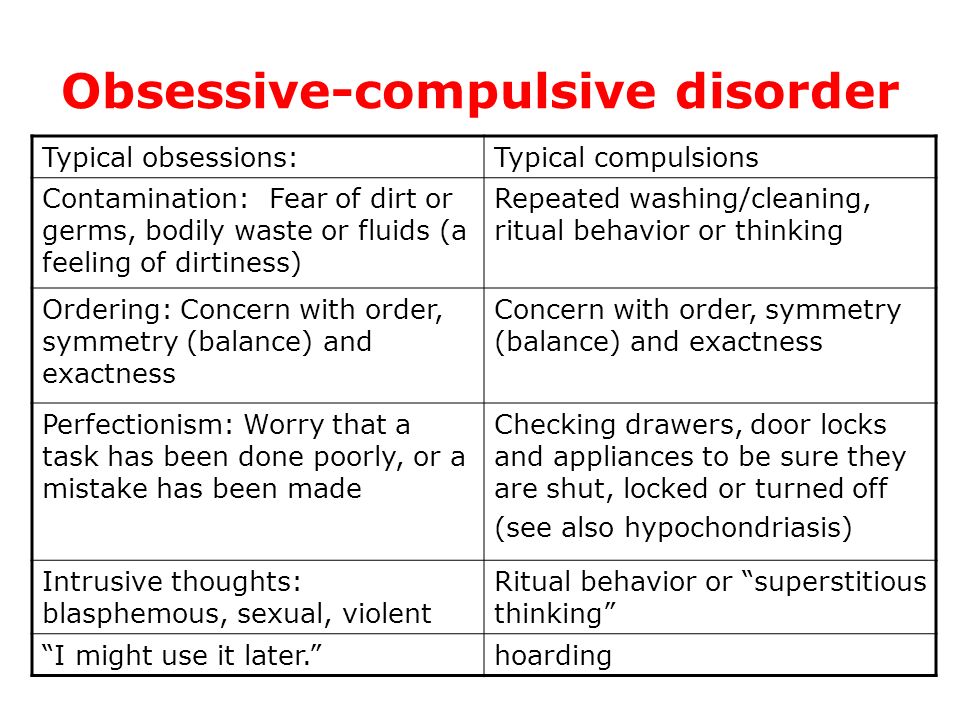 When conducting diagnostics, the following methods are used:
When conducting diagnostics, the following methods are used:
- Psychiatric examination: a specialist will collect an anamnesis, understand the clinical manifestations and personal characteristics of each patient.
- Pathopsychological study: an effective and comfortable technique that, with the help of special experiments, surveys and observations, allows you to conduct a qualitative analysis of mental disorders and understand why obsessive thoughts come.
- Laboratory and instrumental examination: modern diagnostic tests, such as Neurotest and Neurophysiological test system, allow assessing the severity of pathological processes and making an accurate differential diagnosis. Functional methods will help to exclude organic pathology.
How to deal with intrusive thoughts
Mental illnesses that underlie the syndrome in question are a reason to immediately consult a psychiatrist. The symptoms vary greatly, and it is not always easy to notice the distinctive features.-4828.jpg) Therefore, it is necessary to address the question of what to do with obsessive thoughts to an experienced specialist.
Therefore, it is necessary to address the question of what to do with obsessive thoughts to an experienced specialist.
It happens that a person is afraid to seek help or tries to independently find a way to cope with obsessive thoughts that are so annoying. One of the most common decisions is the use of alcohol and drugs. If a person manages to be distracted, the illusion may be created for a short time that the problem has disappeared. In fact, the situation is only getting worse. You should not try to "kill" intrusive thoughts in this way, because it is likely that obsessions will only intensify when intoxicated.
Talk to someone you trust, such as your parents or friends. A great option is to go to group therapy, in a society of people with similar problems. This will allow you to share experiences and get support.
The consequences of drinking alcohol can be unpredictable. Even if there is a brief relief, thoughts will still arise again, and with even greater force. As a result, new health problems are added, dependence on alcohol or drugs develops, and the disorder worsens. With neurosis of obsessive thoughts, only a specialist will tell you how to get rid of or alleviate the condition.
As a result, new health problems are added, dependence on alcohol or drugs develops, and the disorder worsens. With neurosis of obsessive thoughts, only a specialist will tell you how to get rid of or alleviate the condition.
In addition to the stages of treatment that the doctor will select for you, you need to remember about self-control, rehabilitation and prevention. Here are a few tips beyond basic treatment to help you deal with intrusive thoughts:
- Learn more about your disorder. Learning about your condition will help you quickly accept the problem, calm down and motivate you to better adhere to the treatment plan.
- Talk to someone you trust, such as your parents or friends. A great option is to go to group therapy, in a society of people with similar problems. This will allow you to share experiences and get support.
- Normalization of lifestyle: proper sleep, diet, avoidance of alcohol and strong psychotropic substances, moderate physical activity.

- Do not give up your normal activities. Build a career, study, devote time to your favorite hobby. Spend time with family and friends. Don't let illness interfere with your life.
- Avoid Stress: The idea that a strong outburst of emotions will make the fight against obsessive thoughts more effective is false. It will be possible to be distracted only for a short time, but then the nervous system will become even more vulnerable.
Treatment of obsessive thoughts
With the help of modern medicine, it is possible to mitigate the intensity of manifestations, and often completely get rid of obsessions and compulsions.
For obsessive thoughts syndrome, treatment is most effective when combined with psychotherapy and medication. In some cases, one thing is enough. A competent specialist will select an individual program, which will depend on the clinical picture and the severity of the condition.
For obsessive thoughts, treatment may consist of psychotherapy and pharmacotherapy.
Psychotherapy allows you to fully analyze the situation and work out behavioral, psychological and social problems. Communication with a highly qualified psychotherapist teaches you how to manage symptoms, overcome fears and protect yourself from stress. The arsenal of a modern specialist includes cognitive behavioral therapy, hypno-suggestive techniques, auto-training and other effective approaches. Psychotherapy for obsessive thoughts is a key treatment that will help you understand the problem and deal with it.
Pharmacotherapy. Modern medicines help to correct neurotic symptoms, relieve fear and anxiety, and keep mood under control. Mild antidepressants, antipsychotics and tranquilizers are used.
Fortunately, modern psychiatry knows how to cure obsessive thoughts, reduce or completely eliminate symptoms. Thanks to effective treatment and rehabilitation provided by a competent specialist, patients return to an active life without fears and restrictions.