Ibuprofen and cymbalta
Cymbalta side effects and how to avoid them
Most Cymbalta side effects are temporary, lasting only a day or two, but some side effects can last for weeks
Cymbalta side effects | Serious side effects | Suicide | Serotonin syndrome | Angle-closure glaucoma | How long do side effects last? | Warnings | Interactions | How to avoid side effects
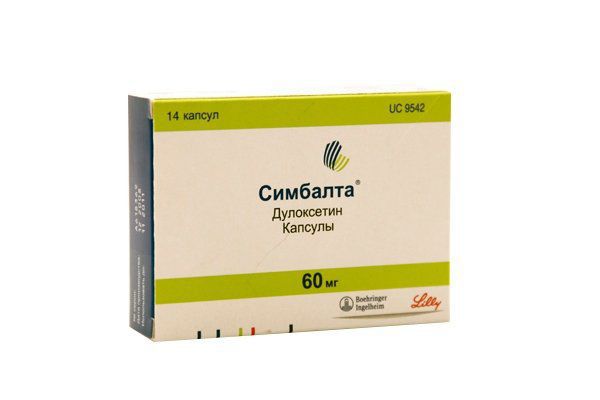
Cymbalta is a brand-name prescription antidepressant used for the treatment of major depressive disorder (MDD), generalized anxiety disorder, as well as to treat pain due to fibromyalgia, diabetic peripheral neuropathy (nerve pain due to diabetes), and chronic musculoskeletal pain such as back pain or osteoarthritis.
Duloxetine hydrochloride, the active ingredient in Cymbalta, belongs to a class of drugs called selective serotonin-norepinephrine reuptake inhibitors (SNRIs). Duloxetine raises the levels of two chemicals, serotonin, and norepinephrine, that are responsible for transmitting signals across nerves in the brain, allowing for better mood regulation.
While effective, Cymbalta may cause problems due to side effects, pre-existing conditions, or drug interactions.
RELATED: What is Cymbalta?
Common side effects of Cymbalta
The most common side effects of Cymbalta include:
- Nausea
- Headache
- Weight loss
- Dry mouth and mouth pain
- Abdominal pain
- Drowsiness
- Insomnia
- Constipation
- Fatigue
- Muscle pain
- Sexual dysfunction
- Blurred vision
- Back pain
- Yawning
- Stomach upset
- Elevated blood pressure (hypertension)
- Elevated liver enzymes
- Heart racing
- Tremor
- Anxiety
- Sweating
Serious side effects of Cymbalta
The most serious side effects of Cymbalta include:
- Suicidal thoughts and behaviors
- Worsening of depression
- Activation of mania or hypomania
- Serotonin syndrome
- Angle-closure glaucoma
- Seizures
- Low blood sodium (hyponatremia)
- Liver poisoning and liver failure
- Drug-induced movement problems (extrapyramidal effects)
- Dangerously high blood pressure
- Heart problems
- Heart attack
- Withdrawal symptoms
- Orthostatic hypotension (sudden drop in blood pressure when standing), fainting, and falling
- Severe allergic reactions or severe skin reactions
- Bleeding
- Inability to urinate
Cymbalta and suicide
Cymbalta and similar antidepressants all contain a black box warning about suicidality and worsening of depression in people diagnosed with major depressive disorder. These side effects are most common in children, teens, and young adults younger than the age of 24. For younger patients, the overall incidence of suicidal ideation (thinking about suicide) when taking Cymbalta is between 0.1% and 1%. That is high enough that caregivers should carefully monitor children and young adults taking Cymbalta for signs of suicidality such as
These side effects are most common in children, teens, and young adults younger than the age of 24. For younger patients, the overall incidence of suicidal ideation (thinking about suicide) when taking Cymbalta is between 0.1% and 1%. That is high enough that caregivers should carefully monitor children and young adults taking Cymbalta for signs of suicidality such as
- Attempts to commit suicide
- Thoughts about suicide or dying
- Acting on dangerous impulses
- Being aggressive, violent, or angry
- New or worsening depression or anxiety
- Panic attacks
- Feeling agitated, restless, or irritable
- Trouble sleeping
- A sudden increase in activity or talking
- Other unusual behaviors
Cymbalta and serotonin syndrome
Although relatively rare, serotonin syndrome is a risk when one or more drugs like Cymbalta are combined. Cymbalta and several other types of drugs work by raising serotonin in the brain. Taking one of these drugs by itself is usually not a problem. When combined, however, serotonin-raising drugs can overload the brain with serotonin causing mild to severe symptoms. The most severe cases will require hospitalization. Get medical attention if any signs of serotonin syndrome are noticed, including:
Cymbalta and several other types of drugs work by raising serotonin in the brain. Taking one of these drugs by itself is usually not a problem. When combined, however, serotonin-raising drugs can overload the brain with serotonin causing mild to severe symptoms. The most severe cases will require hospitalization. Get medical attention if any signs of serotonin syndrome are noticed, including:
- Changes in mental state such as agitation, confusion, hallucinations, or coma
- Movement problems such as loss of coordination, tremors, twitching, rigid muscles, or seizures
- Sweating, fever, or flushing
- Racing heartbeat
- Blood pressure changes
- Nausea, vomiting, or diarrhea
Cymbalta and angle-closure glaucoma
Angle-closure glaucoma happens when a narrow opening (angle) between the iris and cornea closes. This opening drains fluid from the eye, so when it closes, fluid builds up rapidly in the eye, and the increase in fluid pressure can lead to blindness if untreated. People with “narrow angles” are most vulnerable to angle-closure glaucoma. Cymbalta dilates the pupils, raising the risk of angle closure. Immediately stop taking Cymbalta and see a medical professional at any sign of angle-closure glaucoma such as:
People with “narrow angles” are most vulnerable to angle-closure glaucoma. Cymbalta dilates the pupils, raising the risk of angle closure. Immediately stop taking Cymbalta and see a medical professional at any sign of angle-closure glaucoma such as:
- Eye pain
- Changes in vision
- Swelling or redness in or around the eye
How long do side effects last?
Most common side effects of Cymbalta are temporary. Some will get better as the body adjusts to the drug or the underlying depression or anxiety improves. Other common side effects will improve about one or two days after the last dose is taken. A few common side effects, like weight loss, may take a few weeks to return to normal.
Serious side effects may take longer to resolve even after the Cymbalta has been stopped. Serotonin syndrome requires that Cymbalta be completely stopped and takes about two to three days to get better, but the most severe cases may take weeks to get better. Low blood sodium will also require Cymbalta to be stopped and may require up to two weeks of medical treatment. The most severe cases will require hospitalization. Angle-closure glaucoma or a heart attack can both have lifelong complications.
Low blood sodium will also require Cymbalta to be stopped and may require up to two weeks of medical treatment. The most severe cases will require hospitalization. Angle-closure glaucoma or a heart attack can both have lifelong complications.
Cymbalta contraindications & warnings
Cymbalta is a highly effective drug but may cause problems, particularly in people with certain pre-existing medical conditions.
Abuse and dependence
There is currently no evidence that Cymbalta can lead to abuse or dependence, but the U.S. Food and Drug Administration (FDA) does urge that healthcare providers watch for signs of misuse or diversion when prescribing Cymbalta to people with a history of drug abuse.
Overdose
An overdose of Cymbalta can be very serious and even fatal. If an overdose is suspected, seek emergency medical treatment. The most common symptoms of duloxetine overdose are:
- Sleepiness
- Seizures
- Serotonin syndrome
- Fainting
- Racing heartbeat
- Low or high blood pressure
- Vomiting
- Coma
Restrictions
Some pre-existing conditions may increase the risks of taking Cymbalta. Some people may not be able to take Cymbalta at all, while others may require dose adjustments or careful monitoring for adverse effects.
Some people may not be able to take Cymbalta at all, while others may require dose adjustments or careful monitoring for adverse effects.
- CONTRAINDICATIONS: People who are allergic to duloxetine, have severe kidney disease, severe liver disease, cirrhosis of the liver, uncontrolled closed-angle glaucoma, or an alcohol abuse problem will not be given Cymbalta.
- Suicide: People younger than the age of 25 can be given Cymbalta, but should be carefully monitored by caregivers or healthcare professionals for signs of worsening depression or suicidality, particularly in the first months of treatment.
- Bipolar disorder: Cymbalta can activate mania or hypomania in people with bipolar disorder or a history of mania, so changes in mental status and behavior need to be watched carefully.
- Seizure disorders: Cymbalta lowers the seizure threshold, so people with seizure disorders will need to monitor themselves carefully.
- Heart and blood vessel problems: The effects of Cymbalta on patients with cardiovascular disease, cerebrovascular disease, and high blood pressure will need to be closely monitored.
- Low blood volume: Cymbalta can cause severe low sodium in people with low blood volume or who are dehydrated. The elderly are one group at risk for blood volume depletion. These patients will need to be monitored for side effects and may need frequent blood tests.
- Uncorrected narrow angles: People with uncorrected narrow angles are at risk for angle-closure glaucoma, a serious side effect of Cymbalta. Narrow angles can be surgically corrected before Cymbalta treatment. If not, patients need to watch for symptoms of increased eye pressure while taking Cymbalta and get immediate medical attention at any sign of elevated ocular pressure.
- Bleeding problems: Cymbalta interferes with the body’s ability to form blood clots, so it can cause bleeding episodes in people with bleeding disorders or taking blood-thinning drugs. Regular blood tests may be required while taking Cymbalta.
- Diabetes: Cymbalta affects the body’s ability to control blood sugar, so people with diabetes may require regular blood glucose testing and dose adjustments of their diabetes medications.

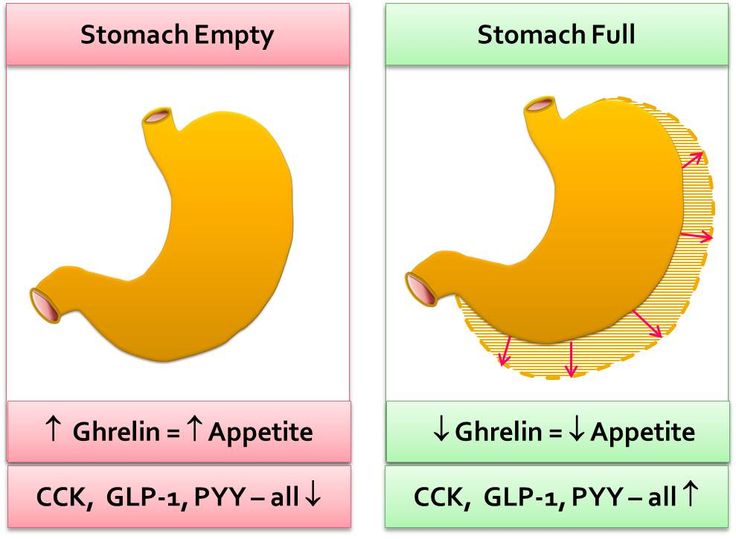
- Delayed stomach emptying: Cymbalta may be less effective in people with gastric motility problems. If the Cymbalta delayed-release capsule stays in the stomach too long, the acid may change the duloxetine into an inert substance with no beneficial effects. Healthcare providers will need to monitor the medicine’s effectiveness in these people.
- Pregnancy and nursing
Based on animal research, duloxetine is considered to be low risk for harming the fetus or mother during the first two trimesters. When duloxetine is taken in the last trimester, however, there is an increased risk of the mother experiencing postpartum hemorrhage or the baby being born with withdrawal symptoms that can require lengthy hospitalization, tube feeding, and breathing support.
Duloxetine is present in breast milk, but women can take Cymbalta while breastfeeding. They will be asked to watch the nursing baby for any effects of Cymbalta such as sedation, poor feeding, or poor weight gain.
Children
Cymbalta is FDA approved for use in children as young as 7 years of age for generalized anxiety disorder and in children as young as 13 for juvenile fibromyalgia syndrome. Children taking Cymbalta, however, are at an increased risk of worsening depression and suicidal thoughts. Caregivers are warned to monitor any child taking Cymbalta for unusual behavior changes, mood changes, or suicidality. Duloxetine may also affect children’s growth, so healthcare providers will regularly check weight and height when giving children Cymbalta.
Seniors
Seniors can safely and effectively take Cymbalta at standard adult doses. Elderly patients are, however, at a higher risk of low sodium, so healthcare providers will monitor side effects, blood pressure, and blood volume carefully. Older patients are also at a higher risk for falls, and duloxetine may increase the risk of falls and injuries. Seniors should tell the healthcare provider about any side effects of duloxetine that can cause falls such as orthostatic hypotension, fainting, or dizziness.
Cymbalta interactions
Some drug interactions can cause problems. In particular, Cymbalta is never combined with the antipsychotic medication thioridazine because of the risk for serious side effects. Cymbalta is also never given with monoamine oxidase inhibitors (MAOIs), a small class of drugs that includes
- Phenelzine, isocarboxazid, tranylcypromine (antidepressants)
- Linezolid (an antibiotic)
- Rasagiline, selegiline, and safinamide (anti-Parkinson’s agents)
- Methylene blue injections (a dye used when taking X-rays or other medical images).
MAO inhibitors have to be discontinued for at least 14 days before Cymbalta can be taken. Discontinuation of Cymbalta has to occur at least five days before taking an MAO inhibitor.
Some drug interactions can cause serotonin syndrome, a potentially serious side effect caused by too much serotonin in the brain. Drugs that raise serotonin in the brain are generally avoided or used cautiously with Cymbalta. These include
These include
- Antidepressants
- Selective serotonin reuptake inhibitors (SSRIs)
- Antipsychotics
- Anxiety medications such as buspirone
- Triptans (migraine medications)
- Bipolar medications such as lithium
- Opioids
- Amphetamines
- Anti-nausea drugs
- Seizure medications
- Some common over-the-counter herbal or dietary supplements such as St. John’s wort or tryptophan.
Duloxetine can cause bleeding problems because it disrupts the blood clotting process. Bleeding episodes, then, could be a problem when Cymbalta is combined with over-the-counter or prescription drugs that also interfere with blood clotting, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and blood-thinners.
Finally, some drugs interfere with the body’s metabolism of duloxetine, raising the risk of adverse effects. Some of these drugs are well-known, like Prozac (fluoxetine), Paxil (paroxetine), fluvoxamine, ciprofloxacin, cimetidine, and quinidine, but healthcare providers and pharmacists are familiar with all of them. They will warn and advise you if you’re taking any of these drugs while taking Cymbalta.
Some of these drugs are well-known, like Prozac (fluoxetine), Paxil (paroxetine), fluvoxamine, ciprofloxacin, cimetidine, and quinidine, but healthcare providers and pharmacists are familiar with all of them. They will warn and advise you if you’re taking any of these drugs while taking Cymbalta.
How to avoid Cymbalta side effects
1. Take Cymbalta as directed
Take Cymbalta exactly as prescribed by the healthcare provider. The usual dose is 60 mg taken once daily. If a dose is missed, take it as soon as it’s remembered. If it’s nearly time to take the next dose, skip the missed dose and take the next dose as scheduled.
2. Read the medication guide
Cymbalta comes with a medication guide outlining how to take the medication, what side effects to monitor, and how to handle problems. Read this guide thoroughly. If it’s missing, a pharmacist can provide a copy.
3. Tell the doctor about all medical conditions
The best way to prevent adverse effects is to make sure the prescribing healthcare provider has your complete medical history.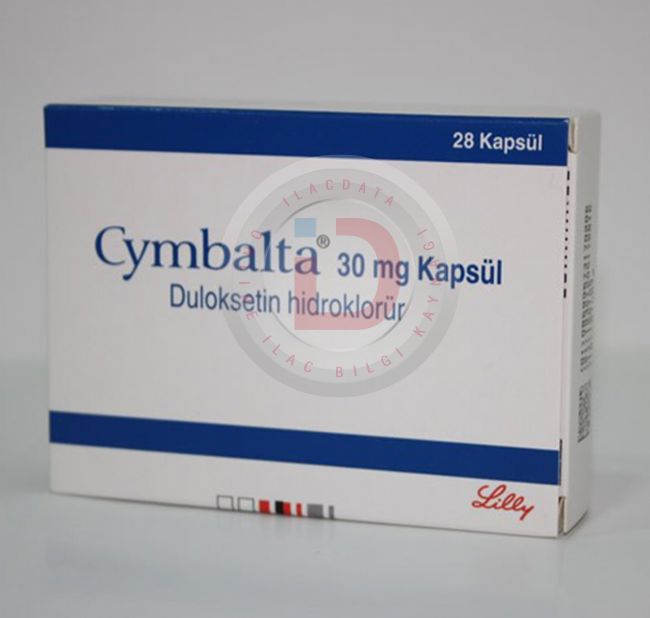 They especially need to know about:
They especially need to know about:
- Heart problems
- High blood pressure
- Diabetes
- Liver problems
- Kidney problems
- Glaucoma
- A history of seizures
- Mania or bipolar disorder
- Bleeding problems
- Pregnancy or pregnancy plans
- Breastfeeding or breastfeeding plans
4. Tell the doctor about all medications being taken
Drugs are also important, so tell the prescribing healthcare professional about all over-the-counter and prescription drugs being taken, particularly:
- MAO inhibitors
- Medicines that treat mood, anxiety, psychosis, bipolar disorder, or other mental illnesses
- Migraine medications called triptans
- Opioids (especially tramadol or fentanyl)
- Amphetamines
- The antibiotics ciprofloxacin or enoxacin
- Heart rate medications
- Blood thinners such as warfarin
- NSAIDs such as aspirin, ibuprofen, or naproxen,
- Over-the-counter supplements such as St.
 John’s wort or tryptophan.
John’s wort or tryptophan.
5. Do not stop taking Cymbalta
Before stopping Cymbalta for whatever reason, get medical advice first. Suddenly stopping Cymbalta could cause withdrawal symptoms. To stop this drug safely, you may need to take a steadily falling dose over a couple of weeks.
6. Do not drink alcohol
Do not drink alcohol when taking Cymbalta. Not only does the combination increase the risk of side effects such as sleepiness and dizziness, but these two drugs taken together can damage the liver.
7. Be careful about driving and other risky activities
All people taking Cymbalta will be cautioned about driving, operating machinery, or other risky activities. Cymbalta can cause drowsiness, dizziness, fainting, falls, and injuries, so it’s a good idea to be very familiar with how Cymbalta affects you before engaging in risky activities.
8. Avoid NSAIDs
Avoid NSAID pain relievers such as aspirin or ibuprofen. Combining them with Cymbalta can cause stomach pain, stomach swelling, stomach bleeding, and other bleeding problems. When treating fever or minor aches and pains, acetaminophen might be a better choice.
When treating fever or minor aches and pains, acetaminophen might be a better choice.
9. Eat a healthy diet
To avoid weight loss, eat a healthy diet. A dietitian or nutritionist can help.
- Changes in sexual functioning, The Journal of Sexual Medicine
- Cymbalta, Epocrates
- Cymbalta, Prescriber’s Digital Reference
- Cymbalta delayed-release capsules prescribing information, U.S. National Library of Medicine
- Duloxetine for the treatment of generalized anxiety disorder: A review, Neuropsychiatric Disease and Treatment
- Sexual dysfunction in selective serotonin reuptake inhibitors (SSRIs), The Mental Health Clinician
Synergistic interactions between the dual serotonergic, noradrenergic reuptake inhibitor duloxetine and the non-steroidal anti-inflammatory drug ibuprofen in inflammatory pain in rodents
. 2007 Feb;11(2):208-15.
2007 Feb;11(2):208-15.
doi: 10.1016/j.ejpain.2006.02.008. Epub 2006 Mar 20.
Carrie K Jones 1 , Steven C Peters, Harlan E Shannon
Affiliations
Affiliation
- 1 Lilly Research Laboratories, Lilly Corporate Center, Eli Lilly and Company, Indianapolis, IN 46285, USA.
- PMID: 16542861
- DOI: 10.1016/j.ejpain.2006.02.008
Carrie K Jones et al. Eur J Pain. 2007 Feb.
. 2007 Feb;11(2):208-15.
2007 Feb;11(2):208-15.
doi: 10.1016/j.ejpain.2006.02.008. Epub 2006 Mar 20.
Authors
Carrie K Jones 1 , Steven C Peters, Harlan E Shannon
Affiliation
- 1 Lilly Research Laboratories, Lilly Corporate Center, Eli Lilly and Company, Indianapolis, IN 46285, USA.
- PMID: 16542861
- DOI: 10.1016/j.ejpain.2006.02.008
Abstract
Objectives: The present study was undertaken to characterize whether the pharmacologic interaction between duloxetine, a balanced serotonergic and noradrenergic reuptake inhibitor, and the non-steroidal anti-inflammatory drug ibuprofen was simply additive, less than additive, or greater than additive (i. e., synergistic) in preclinical models of visceral and inflammatory pain, specifically acetic acid-induced writhing in mice and carrageenan-induced thermal hyperalgesia and mechanical allodynia in rats.
e., synergistic) in preclinical models of visceral and inflammatory pain, specifically acetic acid-induced writhing in mice and carrageenan-induced thermal hyperalgesia and mechanical allodynia in rats.
Methods: In the writhing test, male CF-1 mice were injected intraperitoneally with 0.55% acetic acid and 5 min later the number of writhes was counted over a 5-min period. In the carrageenan models, male Sprague-Dawley rats were injected with a 1.5% carrageenan solution into the ventral surface of the hind paw; hypersensitivity to thermal and mechanical stimuli was subsequently evaluated 2h post-carrageenan.
Results: Vehicle or a dose of duloxetine alone (1-100 mg/kg), ibuprofen alone (10-300 mg/kg), or duloxetine and ibuprofen in combination in a dose-ratio of 1:10 duloxetine:ibuprofen were orally administered 30 or 60 min before testing. Isobolographic analysis of the effects of duloxetine in combination with ibuprofen revealed a significant synergistic (greater than additive) interaction between duloxetine and ibuprofen both for reducing acetic acid-induced writhing and carrageenan-induced thermal hyperalgesia, but were additive for reversing mechanical allodynia.
Isobolographic analysis of the effects of duloxetine in combination with ibuprofen revealed a significant synergistic (greater than additive) interaction between duloxetine and ibuprofen both for reducing acetic acid-induced writhing and carrageenan-induced thermal hyperalgesia, but were additive for reversing mechanical allodynia.
Conclusions: Our data indicate that duloxetine and ibuprofen have synergistic efficacy in a visceral and an inflammatory pain model in rodents, and suggest that duloxetine and ibuprofen in combination may provide a useful approach to the clinical treatment of persistent pain, particularly inflammation-related pain.
Similar articles
-
Efficacy of duloxetine, a potent and balanced serotonergic and noradrenergic reuptake inhibitor, in inflammatory and acute pain models in rodents.

Jones CK, Peters SC, Shannon HE. Jones CK, et al. J Pharmacol Exp Ther. 2005 Feb;312(2):726-32. doi: 10.1124/jpet.104.075960. Epub 2004 Oct 19. J Pharmacol Exp Ther. 2005. PMID: 15494550
-
Analgesic effects of serotonergic, noradrenergic or dual reuptake inhibitors in the carrageenan test in rats: evidence for synergism between serotonergic and noradrenergic reuptake inhibition.
Jones CK, Eastwood BJ, Need AB, Shannon HE. Jones CK, et al. Neuropharmacology. 2006 Dec;51(7-8):1172-80. doi: 10.1016/j.neuropharm.2006.08.005. Epub 2006 Oct 11. Neuropharmacology. 2006. PMID: 17045620
-
Nefopam and ketoprofen synergy in rodent models of antinociception.
Girard P, Verniers D, Coppé MC, Pansart Y, Gillardin JM.
 Girard P, et al. Eur J Pharmacol. 2008 Apr 28;584(2-3):263-71. doi: 10.1016/j.ejphar.2008.02.012. Epub 2008 Feb 14. Eur J Pharmacol. 2008. PMID: 18316069
Girard P, et al. Eur J Pharmacol. 2008 Apr 28;584(2-3):263-71. doi: 10.1016/j.ejphar.2008.02.012. Epub 2008 Feb 14. Eur J Pharmacol. 2008. PMID: 18316069 -
Central antinociceptive effects of non-steroidal anti-inflammatory drugs and paracetamol. Experimental studies in the rat.
Björkman R. Björkman R. Acta Anaesthesiol Scand Suppl. 1995;103:1-44. Acta Anaesthesiol Scand Suppl. 1995. PMID: 7725891 Review.
-
Serotonin and noradrenaline reuptake inhibitors in animal models of pain.
Mochizucki D. Mochizucki D. Hum Psychopharmacol. 2004 Oct;19 Suppl 1:S15-9. doi: 10.1002/hup.620. Hum Psychopharmacol. 2004. PMID: 15378668 Review.
See all similar articles
Cited by
-
Apical periodontitis-induced mechanical allodynia: A mouse model to study infection-induced chronic pain conditions.

Mohaved SB, Shilpa G, Li Q, Austah O, Bendele M, Brock R, Ruparel NB. Mohaved SB, et al. Mol Pain. 2020 Jan-Dec;16:1744806919900725. doi: 10.1177/1744806919900725. Mol Pain. 2020. PMID: 31902318 Free PMC article.
-
Antinociceptive Effects of the Serotonin and Noradrenaline Reuptake Inhibitors Milnacipran and Duloxetine on Vincristine-Induced Neuropathic Pain Model in Mice.
Katsuyama S, Aso H, Otowa A, Yagi T, Kishikawa Y, Komatsu T, Sakurada T, Nakamura H. Katsuyama S, et al. ISRN Pain. 2014 Feb 23;2014:915464. doi: 10.1155/2014/915464. eCollection 2014. ISRN Pain. 2014. PMID: 27335884 Free PMC article.
-
An overview of clinical pharmacology of Ibuprofen.
Bushra R, Aslam N. Bushra R, et al.
 Oman Med J. 2010 Jul;25(3):155-1661. doi: 10.5001/omj.2010.49. Oman Med J. 2010. PMID: 22043330 Free PMC article.
Oman Med J. 2010 Jul;25(3):155-1661. doi: 10.5001/omj.2010.49. Oman Med J. 2010. PMID: 22043330 Free PMC article.
Publication types
MeSH terms
Substances
Interaction between Ibuprofen-chemopharm and Simbalta when used simultaneously
Interacts with
- Simbalta
- serotonin reuptake, antidepressant, antidepressants, other antidepressants
Concomitant use with serotonin reuptake inhibitors (cyhalopram. fluoxetine, paroxetine, sertraline) will increase the risk of serious gastrointestinal bleeding. Cefamandol, cefaperazone, cefotetan, valnrosal acid, plicamycin increase the incidence of hyioprothrombinemia.
Cefamandol, cefaperazone, cefotetan, valnrosal acid, plicamycin increase the incidence of hyioprothrombinemia.
Microsomal oxidation inducers (phenytoin, ethanol, barbiturates, rifampicin, phenylbutazone, tricyclic antidepressants) increase the production of hydroxylated active metabolites, increasing the risk of developing severe geiatotoxic intoxications.
Old age, chronic heart failure, arterial hypertension, ischemic heart disease, cerebrovascular disease, dyslipidemia/hymerlipidemia, diabetes mellitus, peripheral arterial disease, smoking, frequent alcohol consumption, liver cirrhosis with portal hypertension, hepatic and/or renal failure with clearance creatinine less than 60 ml/min, nephrotic syndrome, hyperbilirubinemia, peptic ulcer of the stomach and duodenum (history), the presence of Helicobactor pylori infection, gastritis, enteritis, colitis, blood diseases of unknown etiology (leukopenia and anemia), long-term use of NSAIDs, severe somatic diseases, simultaneous administration of oral glucocorticosteroids (GCS) (including prednisone), anticoagulants (including warfarin), antiplatelet agents (including acetylsalicylic acid, clopidogrel), selective serotonin reuptake inhibitors (including h. citalopram, fluoxetine, paroxetine, sertraline), pregnancy (I and II trimesters), lactation period.
citalopram, fluoxetine, paroxetine, sertraline), pregnancy (I and II trimesters), lactation period.
Do not use two or more non-steroidal anti-inflammatory drugs at the same time, as the risk of side effects increases. When used together, ibuprofen reduces the antiaggregatory and anti-inflammatory properties of acetylsalicylic acid. When used together with thrombolytic drugs (streptokinase, alteplase, urokinase), the possibility of bleeding increases. Ibuprofen enhances the properties of antiplatelet agents, indirect anticoagulants, fibrinolytics. The combined use of ibuprofen and inducers of microsomal oxidation (ethanol {alcohol, vodka}, phenytoin, barbiturates, phenylbutazone, rifampicin, tricyclic antidepressants) increases the risk of developing severe hepatotoxic events. Inhibitors of microsomal oxidation reduce the possibility of hepatotoxicity. Colestyramine and antacids reduce the absorption of ibuprofen. Caffeine increases the analgesic effect of ibuprofen. Cefoperazone, cefamandol, valproic acid, cefotetan increase the incidence of hypoprothrombinemia.