Grief and loss groups
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.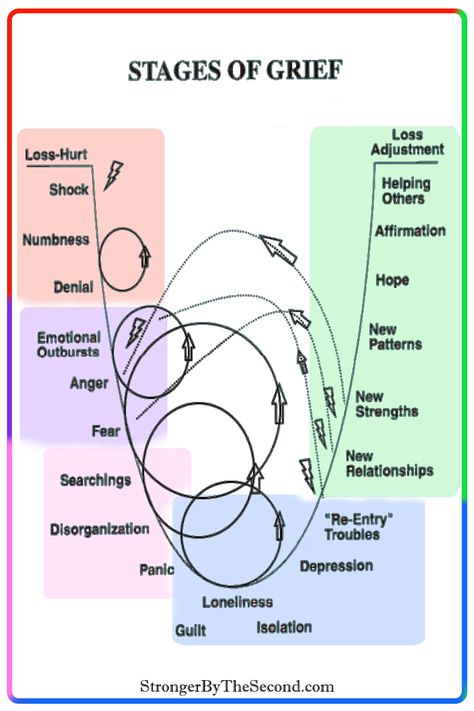
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. SAMHSA’s 2020 National Survey on Drug Use and Health reports that approximately 19.3 million people aged 18 or older had a substance use disorder in the past year.
Alcohol
Data:
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.
 6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- The 2019 National Survey on Drug Use and Health reports that 139.7 million Americans age 12 or older were past month alcohol users, 65.8 million people were binge drinkers in the past month, and 16 million were heavy drinkers in the past month
- About 2.3 million adolescents aged 12 to 17 in 2019 drank alcohol in the past month, and 1.2 million of these adolescents binge drank in that period (2019 NSDUH)
- Approximately 14.5 million people age 12 or older had an alcohol use disorder (2019 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired.
 The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.
 3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Data from the 2019 NSDUH reports that 58.1 million people were current (i.e., past month) tobacco users. Specifically, 45.9 million people aged 12 or older in 2019 were past month cigarette smokers (2019 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey.
 Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018 - E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year.
 Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH) - An estimated 745,000 people had used heroin in the past year, based on 2019 NSDUH data
- In 2019, there were 10.1 million people age 12 or older who misused opioids in the past year. The vast majority of people misused prescription pain relievers (2019 NSDUH)
- An estimated 1.6 million people aged 12 or older had an opioid use disorder based on 2019 NSDUH data
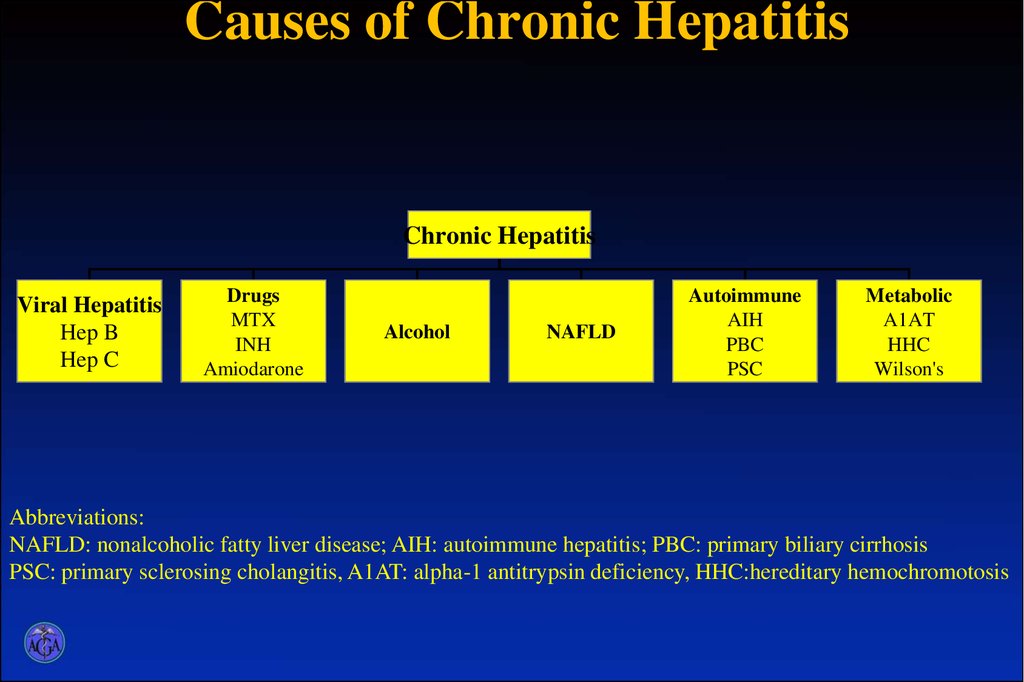
- Opioid use, specifically injection drug use, is a risk factor for contracting HIV, Hepatitis B, and Hepatitis C. The CDC reports that people who inject drugs accounted for 9 percent of HIV diagnoses in the United States in 2016
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.
 5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH) - 2019 NSDUH data indicates that 48.2 million Americans aged 12 or older, 17.5 percent of the population, used marijuana in the past year
- Approximately 4.8 million people aged 12 or older in 2019 had a marijuana use disorder in the past year (2019 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 04/27/2022
Groups at risk of severe grief:
-
elderly people experiencing the loss of a loved one a person feel more isolated and in need of sympathy;
-
children, who have lost loved ones, vulnerable and more aware of death than adults think about it:
-
before 2 years old children can not be aware because someone in the family has died. But they very concerned about it.
-
AT aged 3 to 5 years, children do not consider death is an irreversible phenomenon and they think that the deceased will return.
-
Between At 6 and 9 years of age, children gradually begin realize the inevitability of death, and their thoughts may be related to haunted.
-
Teenagers emotionally vulnerable and suffering loss especially hard.
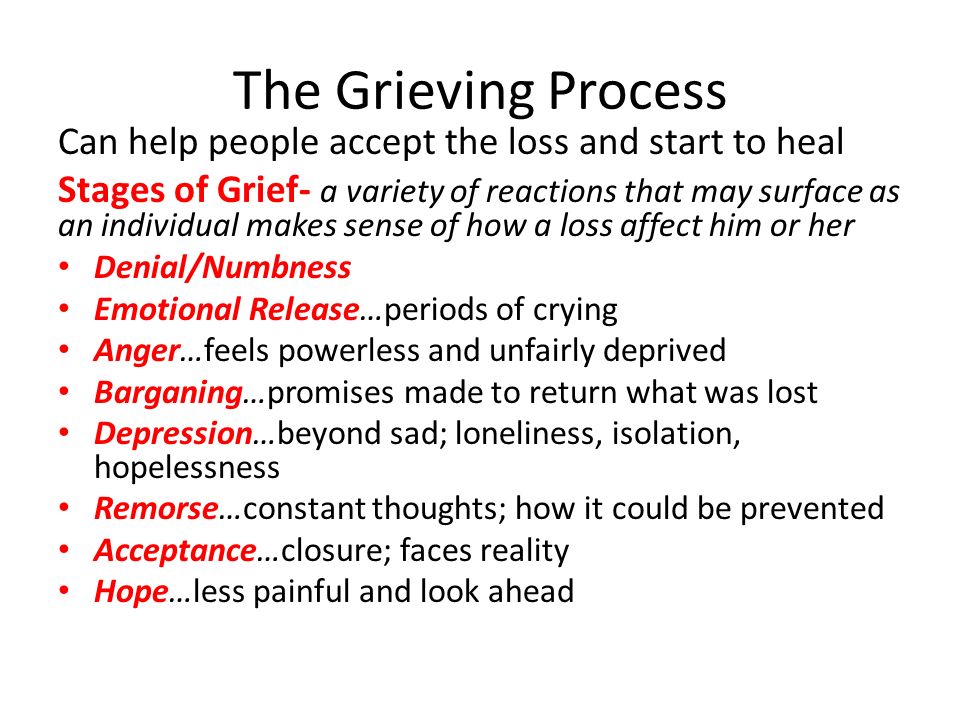
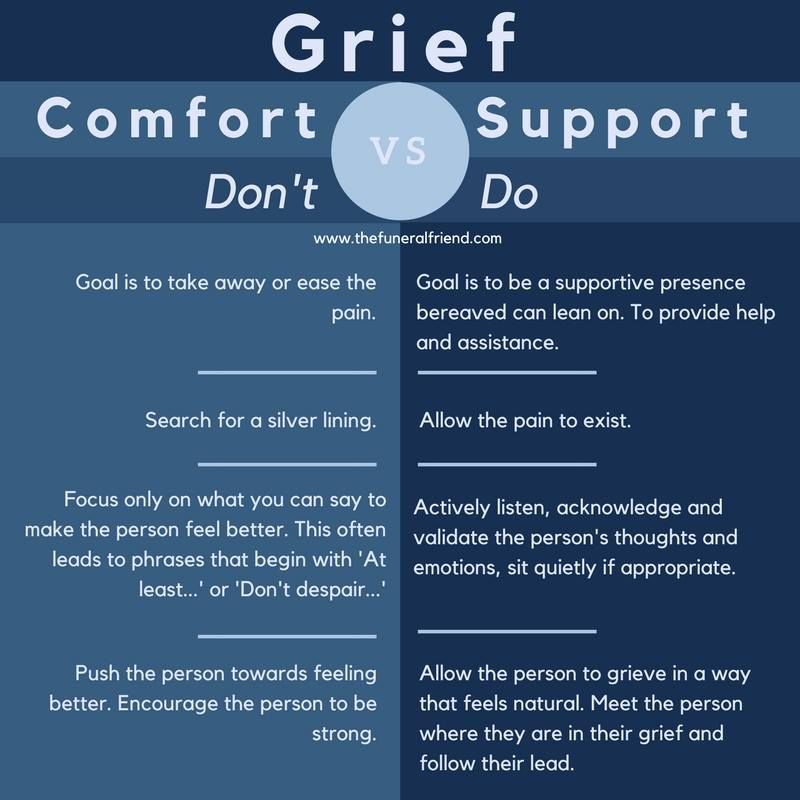
Knowledge stages of grief experienced by relatives deceased are necessary in order to avoid misunderstandings about mournful, quick-tempered judgment about his experiences at the moment. Supporting the grieving promote a healthy process experiences of sadness. The thought that something can be done and exists the end of experiences, is strong the antidote to the helplessness that the mourner experiences. Many relatives remain full feeling
guilt: "If only I had done it, he wouldn't died". We need to help them express discuss their feelings. It is known that some are especially vulnerable during worries about the loss of loved ones. Therefore, there is a risk that they will grieve too emotionally.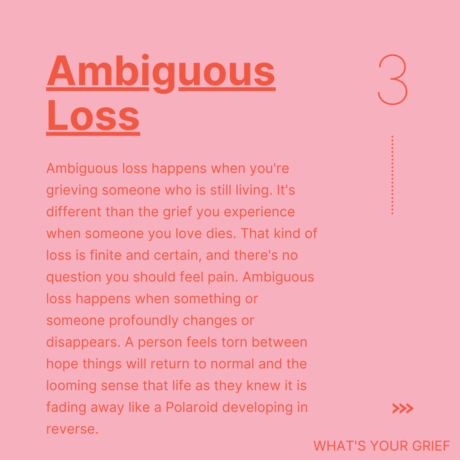 it can be unusually strong reactions and continue for more than 2 years.
it can be unusually strong reactions and continue for more than 2 years.
-
Features of communication and psychological assistance to a doomed person, his family and friends. Caring for a doomed person in a hospital and at home.
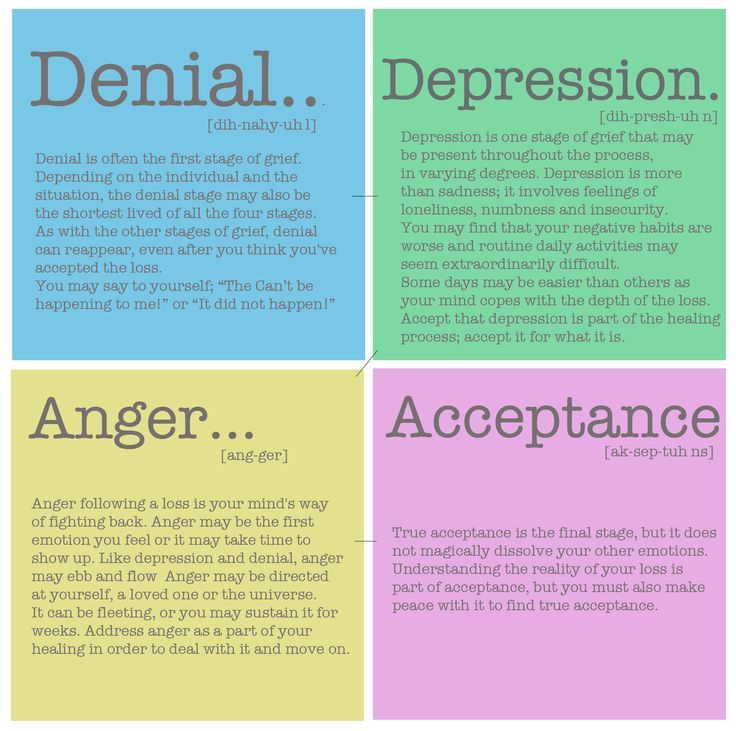
Highly it is important to recognize at what stage it is sick at the moment to render appropriate assistance to him.
For some patients the first stage is shock and is protective. At there is a conflict between desire to know the truth and the desire to escape anxiety. Once the patient is aware the reality of what is happening, its denial is replaced by anger. hard for him There are stages of denial and anger. A patient irritable, demanding and become obnoxious if the anger is tolerated for family or medical staff.
Sometimes the patient is trying to make a deal with with yourself and with others, and win additional time for life. When is the meaning of the disease fully realized, there comes a stage depression.
signs depression:
-
permanent Bad mood;
-
the loss interest in the environment;
-
feeling guilt and own inferiority;
-
hopelessness and despair;
-
attempts suicide or persistent thoughts of suicide.
emotionally - the psychological state of the patient at the fifth stage undergoes fundamental changes. Man prepares himself to death and accepting it as a fact. In this stages of intensive spiritual work - repentance, assessment of one's life and that measure good and evil, which you can evaluate your lived life. The patient starts experience a state of peace and tranquility.
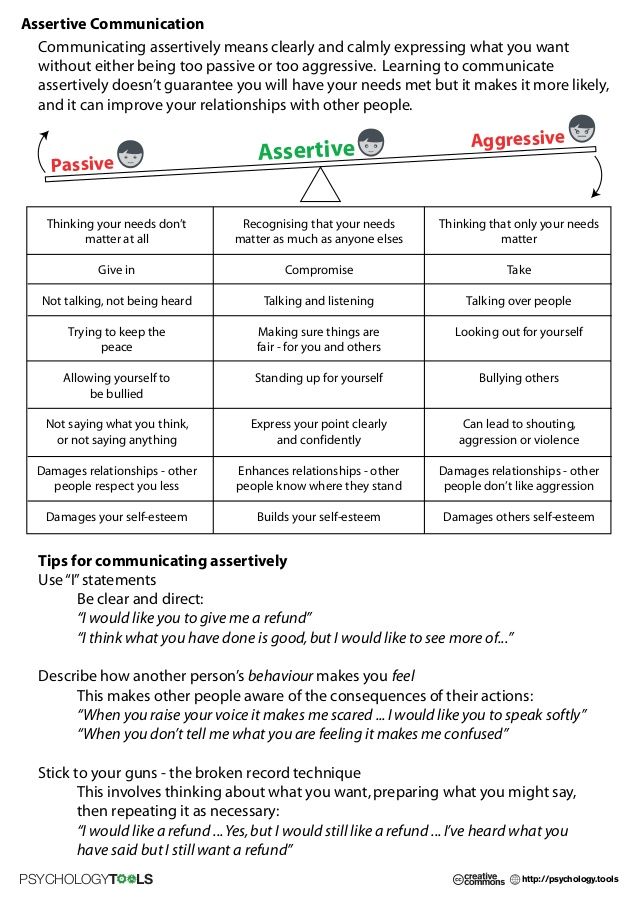
To communicate with terminally ill people, a skill is needed, which, although not without difficulties can be learned. For this you need to know yourself, the patient and his family, as well as their attitude and approach to this problem. The ability to communicate is required from a person to be honest, respect feelings others and have the ability to compassion. This skill turns on the tongue gestures, spoken language, trust, which is established between you and interlocutor. Clark (1981) described several types of needs patients and their families in communication:
This skill turns on the tongue gestures, spoken language, trust, which is established between you and interlocutor. Clark (1981) described several types of needs patients and their families in communication:
-
need in communication between people;
-
in information;
-
in council;
-
in consolation;
-
in discussion of treatment and prognosis;
-
in conversation about feelings and professional psychological support.
Remember! Relationships between a nurse and a doomed patient based on trust. Therefore not cheat patients.
Tem however, do not provide modified information and
avoid thoughtless candor. Mostly patients want to know as much as possible about your condition. However, be prepared stop if the patient gives you understand that
he got enough information.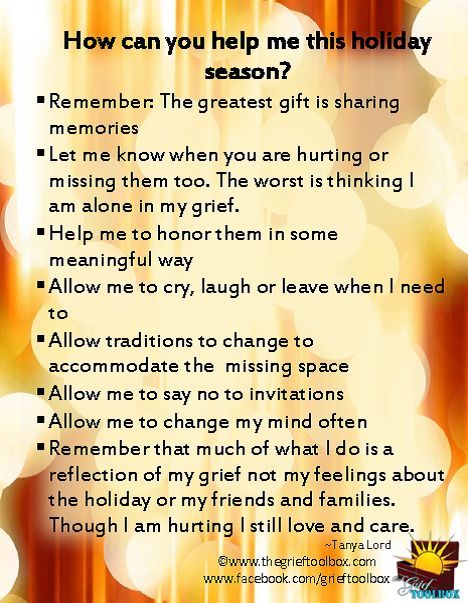
-
Highlight time for a leisurely conversation.
-
sit down and let the patient know what you have time for him.
-
try to keep your eyes on the same level co gaze patient.
-
Highly it is important to speak in private.
-
Important encourage the patient to continue the conversation, showing interest with a nod head or phrase
-
"Yes, I understand".
When people suffer, they strive for informal communication, in contrast to the state when they are calm and in control. Remember that when talking to a patient it is very important to have optimal physical space between you. The patient will feel uncomfortable if you are away from it too close. If it's far away, it will be additional barrier to communication. A lot depends on the response. the patient and his family to communicate with you.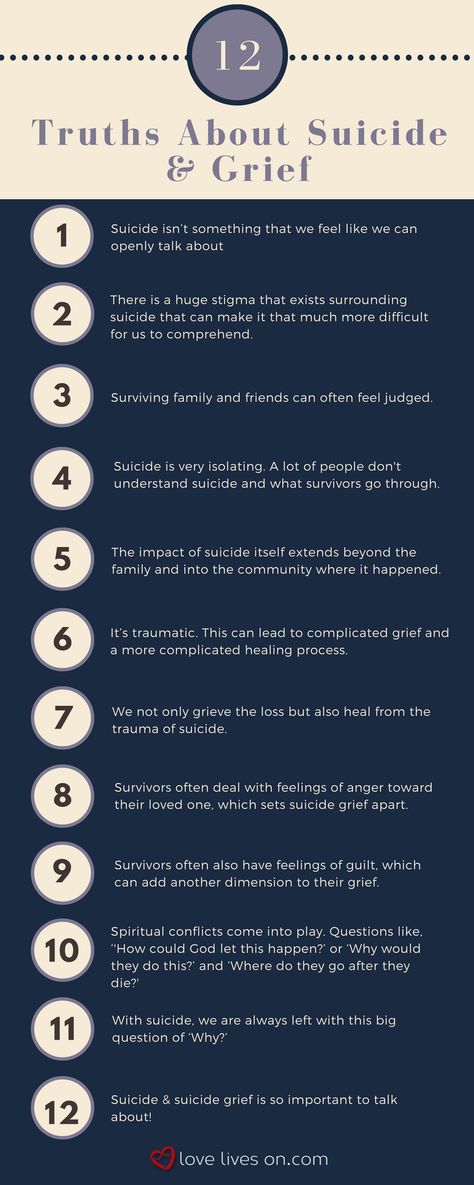 It shows how you influence patient, and how he might respond to your relationships. May occur discord in communication due to what was said the nurse is incomprehensible to the patient, so avoid medical vocabulary. Get ready for religious and philosophical conversations, dialogues with the patient about justice, about the meaning of life, about good and evil. The whole difficulty in such a situation is that philosophical Judgment is first and foremost important here. not by themselves, but as a means of consolation, reconciliation of the doomed man with your destiny. Dying patients are very acutely feel the insincerity of the interlocutor, sensitive to the smallest manifestations of indifference. Therefore, when communication with them is very important to maintain benevolence, mercy and professionalism regardless of personal problems and circumstances.
It shows how you influence patient, and how he might respond to your relationships. May occur discord in communication due to what was said the nurse is incomprehensible to the patient, so avoid medical vocabulary. Get ready for religious and philosophical conversations, dialogues with the patient about justice, about the meaning of life, about good and evil. The whole difficulty in such a situation is that philosophical Judgment is first and foremost important here. not by themselves, but as a means of consolation, reconciliation of the doomed man with your destiny. Dying patients are very acutely feel the insincerity of the interlocutor, sensitive to the smallest manifestations of indifference. Therefore, when communication with them is very important to maintain benevolence, mercy and professionalism regardless of personal problems and circumstances.
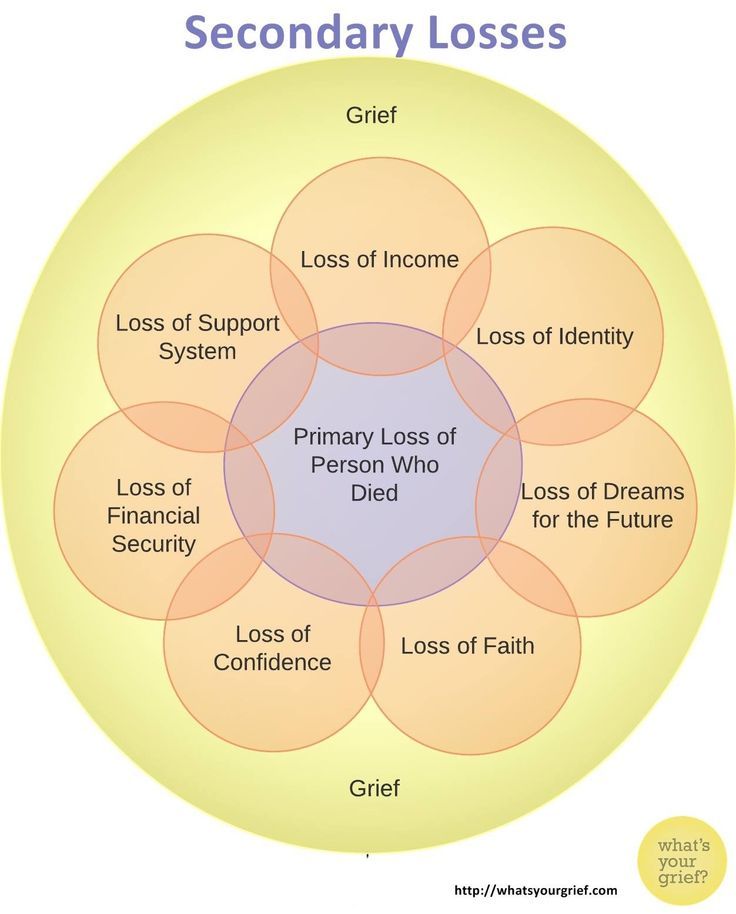
Death is often a severe shock to relatives, and therefore to them in such cases should be treated with particular care and attention, provide them with psychological support.
How behave at the bedside of the dying, as well as what can you talk to him about pay visits to the patient - this should teach the relatives of the doomed nurse.
If a dying patient in hospital due to the gravity of his condition, relatives can be involved in caring for him, teaching them the elements of care. They can, for example, to feed the patient, correct bed, hold some hygiene Events.
To the patient did not feel alone and abandoned, they can sit next to each other, holding his hand, touching his shoulder, hair, or read a book to him.
incurable illness, death of a loved one is big for his family psychological trauma. They can tired, they may develop irritation, depression, anger attitude towards the dying. Rendering psychological assistance to the family of the dying man is
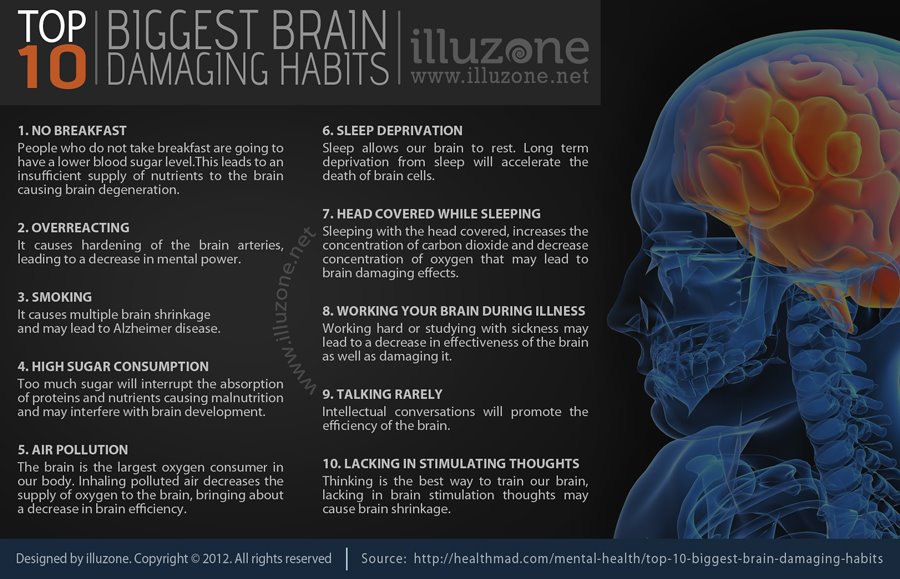
important part of the work of a nurse, which can support families after his death. Family Experiencing Death native, close person also passes grief stages. Grief of loss can overshadow remaining to live for the rest of their lives. The consequences may affect their mental balance and undermine health. It's impossible to hide from grief it must be accepted and deeply experienced; loss must be perceived not only mind, but also heart. Without such a complete grief will last and can lead to chronic depression, loss of the joy of life and even any desire to live. Dealing with grief does a person who can remember the deceased without emotional pain and save living feelings for others.
Grief of loss can overshadow remaining to live for the rest of their lives. The consequences may affect their mental balance and undermine health. It's impossible to hide from grief it must be accepted and deeply experienced; loss must be perceived not only mind, but also heart. Without such a complete grief will last and can lead to chronic depression, loss of the joy of life and even any desire to live. Dealing with grief does a person who can remember the deceased without emotional pain and save living feelings for others.
German experience - Pro Palliative
Contents
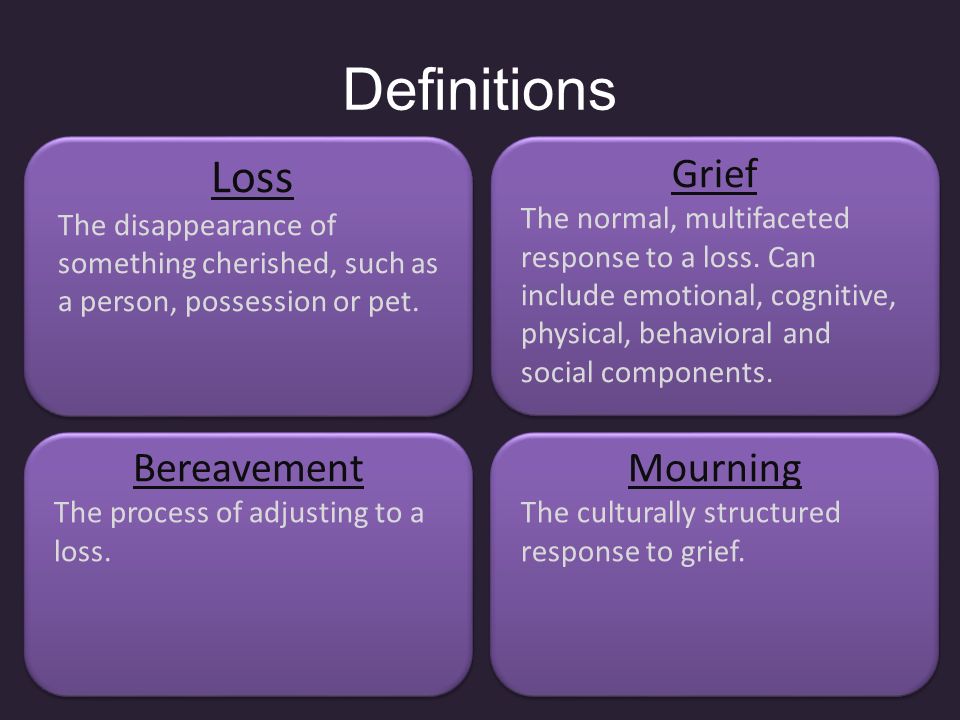
What is mourning?
Lock time
Janus time
Labyrinth phase
Rainbow phase
Recall the situation when someone close to your friend, acquaintance or colleague died. Who among us has not been confused? How to comfort? The phrase "Hold on!", help in organizing the funeral, money? And then what? Distract? Leave alone?
The grief of losing a loved one is constantly faced by palliative care professionals and ordinary people. To support a relative of a deceased patient, you need to know how to do it correctly. We offer you to get acquainted with the practice of such support, which is used in the German "Long-term Care Center Ludwig-Steil-Hoff". This was told at the Summit of Nurses in Moscow by Katya Petker, a senior nurse, head of one of the Center's hospitals.
To support a relative of a deceased patient, you need to know how to do it correctly. We offer you to get acquainted with the practice of such support, which is used in the German "Long-term Care Center Ludwig-Steil-Hoff". This was told at the Summit of Nurses in Moscow by Katya Petker, a senior nurse, head of one of the Center's hospitals.
In Germany, each clinic has the right to freely choose the concept of mourning, or the concept of bereavement, according to which it will work with relatives, accompany them after the death of a loved one. There are several of these concepts, and there is no “obligation” which one to follow.
After our patient dies - it doesn't matter if he was in our hospital or was at home and we observed him - we do not leave his relatives, we do not leave them alone in trouble, but we try to accompany them. And for the past five years we have been working in accordance with the concept of experiencing loss according to Schmieding (the creator of the model is Ruthmaraika Schmieding, a German teacher: having lost a person close to her, she began to study the processes that happen to people during this period), which describes what a person experiences at every stage of his mourning.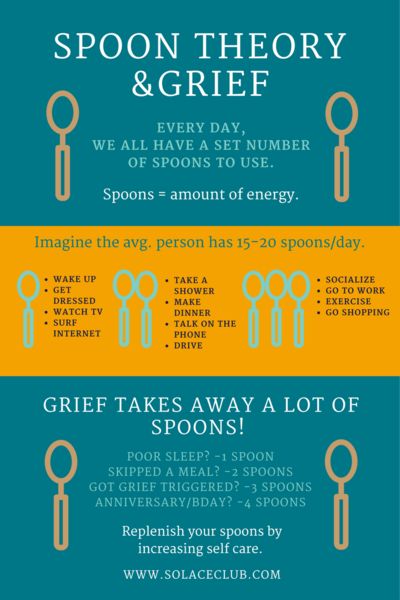
What is mourning?
People cannot stand the pain of others About what can be done for a person who has lost a loved one. Personal experience.
Mourning is an external form of expression of sadness or grief due to the loss of a loved one. This concept is also used when it comes to the death of a public figure, a major statesman, the tragic death of a large number of people. But, of course, we most acutely experience the death of a loved one.
I would like to introduce you to the mourning model for Schmieding. Why is it so important to know her? This knowledge will help both the relatives of the deceased and the staff of the medical institution.
Without knowing anything about the stages of mourning, about how a person reacts to loss and what phases he goes through in his grief, sometimes you might think that he is pretending that his reactions are feigned.
It can be difficult to understand what is happening to him, where he has certain emotional manifestations, and how to help him.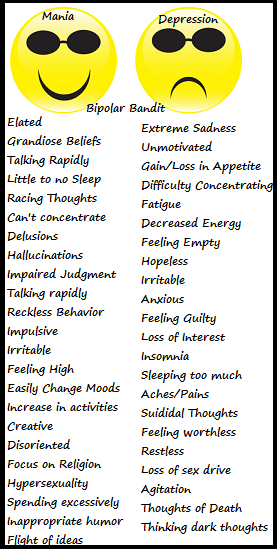 And this model just gives an understanding of how a person experiences his loss. This helps to support a suffering relative so that he can get back on his feet and move on in life. The ultimate goal of this model is to help the relative find resources and opportunities that will give him the strength to live on after the loss.
And this model just gives an understanding of how a person experiences his loss. This helps to support a suffering relative so that he can get back on his feet and move on in life. The ultimate goal of this model is to help the relative find resources and opportunities that will give him the strength to live on after the loss.
“Hold on”, “I understand you”, “The time has come” – how not to comfort Crisis psychologist, psychologist at the Children’s Hospice “House with a Lighthouse” Larisa Pyzhyanova – about typical phrases of consolation and about what is really behind they cost
This model considers not only the emotional side of experiencing the death of a loved one. Mourning affects all areas of life - on the psyche, on spiritual aspects, on consciousness, cognitive functions, on the social side, so we consider a person in the complex of his manifestations.
Looking at mourning in general, there are four phases of pain:
- “Time of locks”;
- Janus Time;
- Maze Time;
- Rainbow Time.
The difficulty lies in the fact that mourning, mourning is not a linear process: these phases can be repeated, come back, and many times. You have probably heard about the stages of accepting death according to Elisabeth Kübler-Ross? She distinguishes five phases: denial, anger, bargaining, depression, acceptance. These stages are intertwined, can alternate, repeat, which is why it is so difficult to be close to a worried person: today he is calm, peaceful, tomorrow he again rushes about, gets angry, the day after tomorrow he has depression, apathy.
It's the same here: all these stages are shifting, so it can be very difficult to understand a person who is in mourning, in mourning, it is very difficult to support and accompany him.
Lock time
This is the shortest of the four periods, it lasts from the death of a loved one until his funeral. And this is the only phase of the four that does not repeat, so it is very important to take into account the cultural and religious needs of a person at this moment.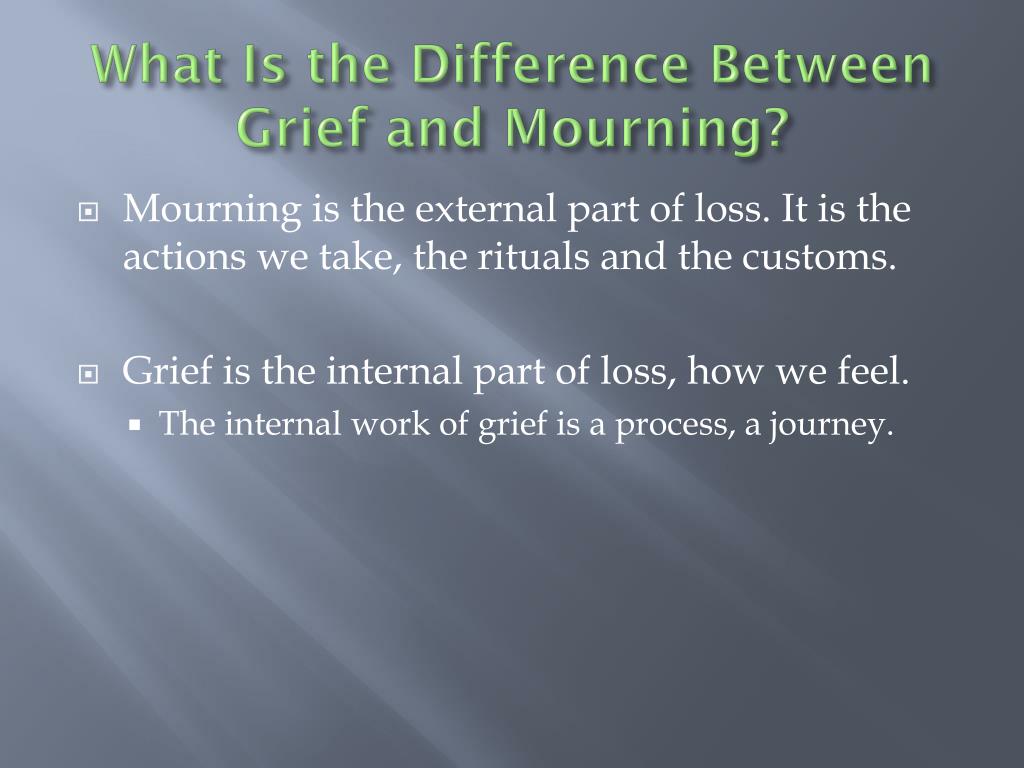
Of course, a lot depends on whether the death was sudden, say, as a result of an accident, or expected, after a long illness. Naturally, sudden death is much more difficult, more painful, and the process of mourning is delayed.
In general, this phase can be characterized by the following metaphor: the ship needs to be controlled, and a “gateway guard” is needed, who opens the lock so that the ship moves from one basin to another, that is, ensures the transition from one state to another. Otherwise, grief can overflow.
I imagine this situation as follows: a person died, and while he was ill, he was lying in our institution, he was the captain of the ship. This person is gone, which means that now someone else must become the captain of this ship, and this other must lead the ship until the funeral takes place. What does it mean? First of all, he must be a Man with a capital letter: be able to listen, keep silent where necessary, support, come, shake hands, just sit next to him.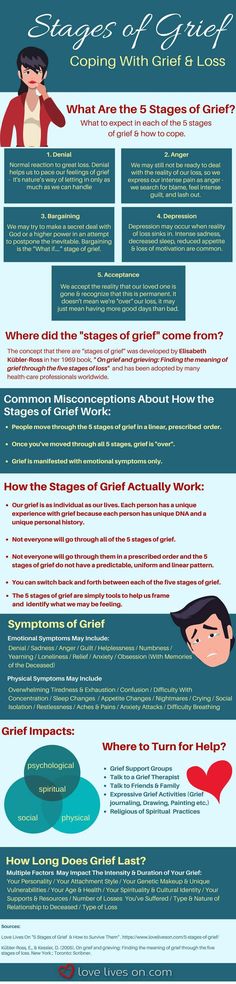 Such actions alleviate grief, partially relieve its emotional severity.
Such actions alleviate grief, partially relieve its emotional severity.
Of course, the maintainer needs to be attentive and infinitely patient in order to be able to listen to the same stories over and over again. Each of us, I'm sure who went through this phase, noticed that a person who has lost a loved one is able to tell the same story ten times, connected with the deceased, constantly returning to it. In the end, the listener begins to think: “Yes, I don’t want to listen to this for the eleventh time!”.
To be heard for the tenth, eleventh, and one hundred and eleventh time is very important for a person in mourning! Thus, he, as it were, processes his grief, looking for the next step in order to move on in life.
How to help a grieving child How a child perceives death and experiences grief at different ages, why it is important to take children to funerals, and why the phrases “poor thing, you are the only one left” or “now you are the head of the house” are dangerous
This is especially characteristic of the "gateway" period.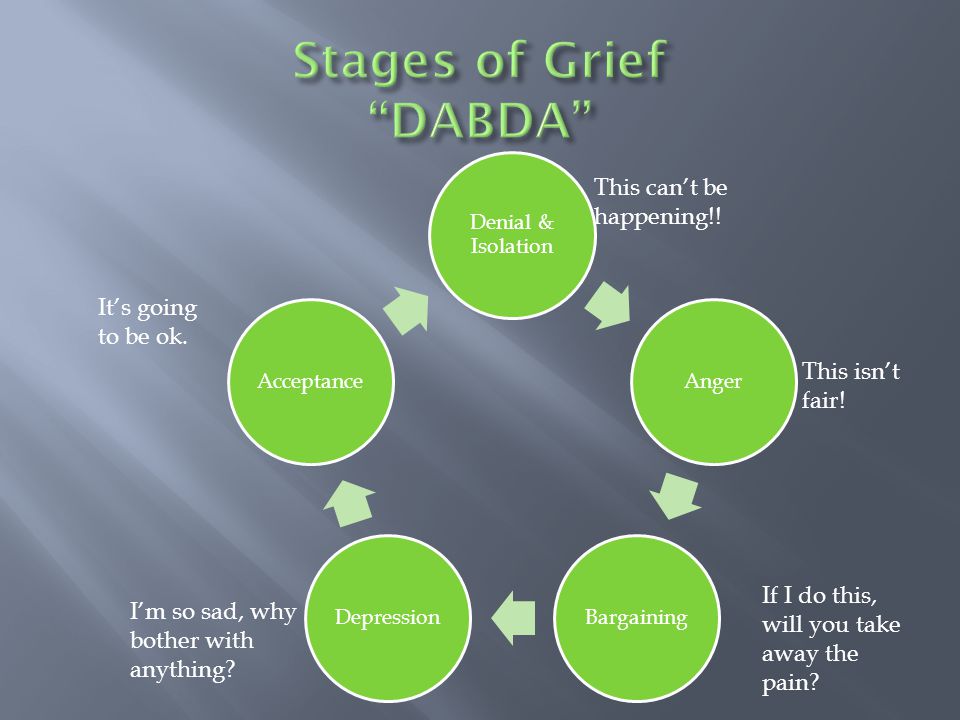
At this moment it is necessary to reach out to the mourner: visit him, listen to him, help organize a worthy funeral and commemoration. It is necessary to try to protect the sufferer during this period from some stumbling blocks, additional experiences that exacerbate suffering. A person experiencing a loss often experiences a feeling of guilt, a feeling that he didn’t do something, didn’t finish something: “If I were there then ...”, “If we organized the funeral like this ...”, - such experiences place an additional burden on the shoulders of a person in mourning, and he carries this burden further. Therefore, it is very important that everything that can be done is done to remove this burden from the shoulders of a person: you need to talk to him, support him, listen, help with the funeral, help in solving emerging problems. It is important that at this time of grief, other individual paths open up before the person so that the person takes the next step.
Janus time
The second phase of mourning is Janus time .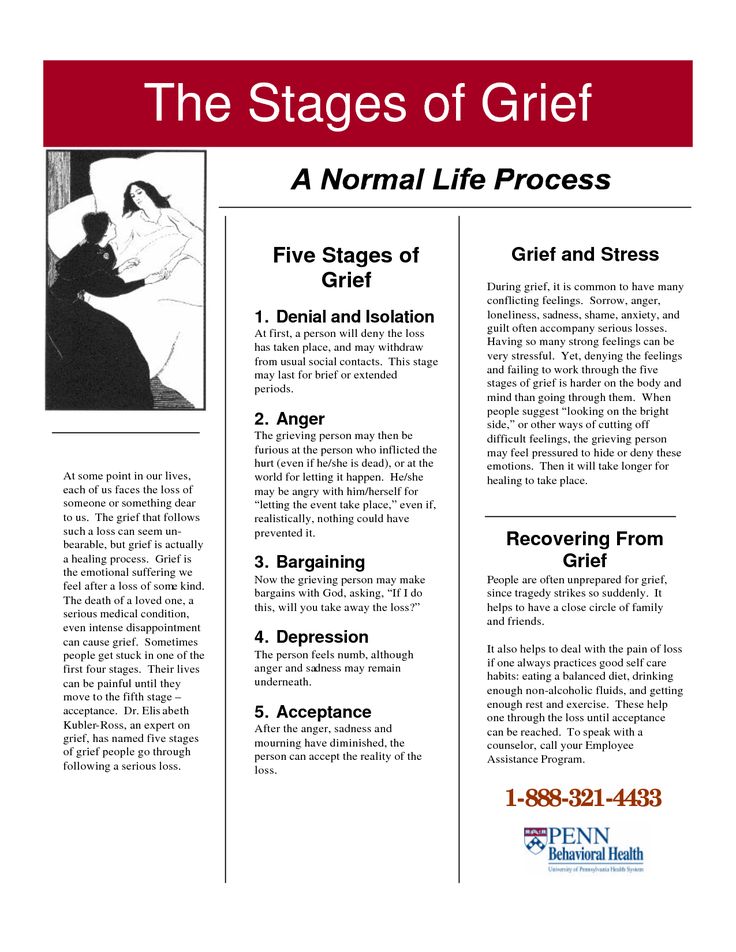 Why Janus? This is the two-faced god of time in ancient Greek mythology: one face is young, the other is the face of an old man. A person in this phase also has “two faces”: one is the one that he shows to others, to society, the second he hides, hiding what is really happening to him (for example, he comes home and cries into the pillow for a long time, or he fancies , as if he hears the voice of the deceased, but he is afraid to tell someone about it, so that he would not be considered crazy).
Why Janus? This is the two-faced god of time in ancient Greek mythology: one face is young, the other is the face of an old man. A person in this phase also has “two faces”: one is the one that he shows to others, to society, the second he hides, hiding what is really happening to him (for example, he comes home and cries into the pillow for a long time, or he fancies , as if he hears the voice of the deceased, but he is afraid to tell someone about it, so that he would not be considered crazy).
Photo: Sydney Sims / Unsplash
And in this phase, a lot depends on whether the person died suddenly, or his death was expected. If this happened suddenly, then, if possible, it is not necessary to talk about the deceased with a relative, during this period such conversations will be an additional burden, stress, and heaviness for him. The time will come, and the mourner himself will ripen for such conversations. As long as he himself does not talk about the deceased, do not provoke him to such conversations.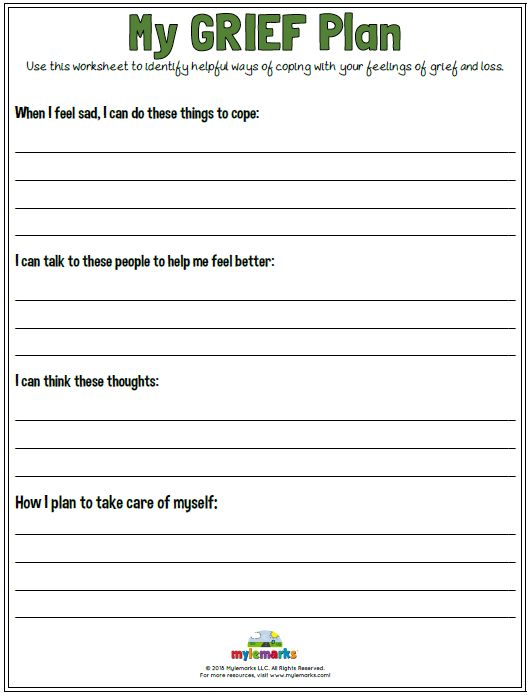 You just need to be there, to accompany, to listen, but not to speak. And if death was expected, here, on the contrary, it is very important to talk with relatives in this phase: discuss the funeral, talk about how the deceased lived, about everything connected with him. Each such conversation brings relief, strengthens a person and gives him the resources to take the next step, to find, as I always say, solid ground under his feet and move on in life.
You just need to be there, to accompany, to listen, but not to speak. And if death was expected, here, on the contrary, it is very important to talk with relatives in this phase: discuss the funeral, talk about how the deceased lived, about everything connected with him. Each such conversation brings relief, strengthens a person and gives him the resources to take the next step, to find, as I always say, solid ground under his feet and move on in life.
Society's attitude towards death. From the book “In the middle of life” Why, despite the inevitability of death, we try not to talk about it, and how this “conspiracy of silence” affects children who have lost loved ones
Here is the funeral behind: what happens next with people who experience the death of a loved one ? In the process of mourning, they begin to pay attention to dates, correlate certain days with events that took place near the deceased: they follow the calendar, remember when this person was born, at what time he got to the hospital, etc.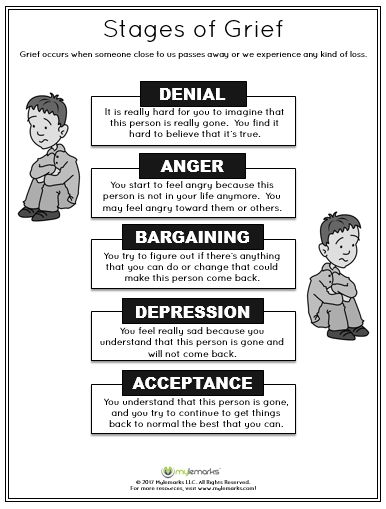 That is, they seem to relive everything that happened again.
That is, they seem to relive everything that happened again.
Bereaved people often have sleep disturbances—we all know that. This is a time of tears and doubts. The man has already spent a lot of energy on the funeral, and he understands that he has a hard way ahead. He loses his appetite, he does not sleep, he may have a feeling that he is going crazy.
My mother died in 2005. At that time, there was no such program for accompanying relatives. And after her death, after the funeral, one day I came home from work, crossed the threshold of the house and heard my mother say to me in German: “Katya, is that you?”. I answered: “Yes”, but I knew that my mother was no more.
I got scared then, I thought: “That's it, I'm going crazy”. But when I began to discuss this episode with my colleagues, it turned out that this is quite a normal phenomenon during a period when a person is in this phase of mourning: changes occur in his body, there is a feeling that time has stopped. These are all normal reactions of a grieving person. A loved one is no more, but for those who mourn, he is there. Many feel the familiar smell of the departed, hear his voice, feel his touch.
These are all normal reactions of a grieving person. A loved one is no more, but for those who mourn, he is there. Many feel the familiar smell of the departed, hear his voice, feel his touch.
Often people continue to observe all the usual family rituals, as before, when a loved one was alive - they set the table, cook food for the same number of family members as before. They, as if by inertia, still live with a deceased loved one. All these actions are reflected in the change of phases of mourning, this is part of the process, and in any case a person must be supported. Grieving people are often afraid to tell someone about what they are experiencing, but it is very important for them to speak out! Therefore, we create groups of mourning, mourning: once a month or every few months we invite relatives who have lost their loved ones to a meeting so that they can talk and get support. And if it is clear that a person has a need for psychiatric help - he has depression, suicidal thoughts - we offer help to such a relative.
Phase of the labyrinth
If guilt tears the heart apart In all the languages of the universe, so different, we are connected by one dialect - the one that sounds in our hearts as the voice of pain. When we lose loved ones...
This is the very core of mourning, when grief is processed. In principle, this stage can be represented as follows: mourning is a backpack, it is a burden on the shoulders. And with this burden, a person enters the labyrinth, steps forward along it, stumbles, wanders, returns back to the old place. He is looking for a way out, trying to get out of this phase! In the end, there is a way out, and we all know it. A person will come out of this labyrinth - and the backpack will be with him, yes, but - it is no longer as heavy as at the beginning. The one experiencing the loss has already understood, accepted that the deceased is not next to him, he understood that his life goes on, and the departed remains in his heart. By the end of this period, a person is fully aware of the reality of the loss and, with the awareness of this loss, moves on in life.
By the end of this period, a person is fully aware of the reality of the loss and, with the awareness of this loss, moves on in life.
To talk or not to talk to him during this period? Here everything is individual. Regardless of the phase, if a person accepts your help, is open to conversations, you need to support them - remember the deceased, be there. But if the mourner declines your help, you need to step aside and just watch. And be ready to help, listen when needed.
Rainbow phase
The last step is rainbow phase . Having survived, processed grief, a person moves on in life and again finds the opportunity to rejoice. This is the end of the time of sorrow, life goes on as usual, but no one is forgotten. The deceased becomes part of the new life.
But even at this stage it is possible to return back to the previous phase. Those who accompanied the mourners know that today they can laugh, and tomorrow they can cry inconsolably.