Can mental illness develop later in life
Mental illness - Symptoms and causes
Overview
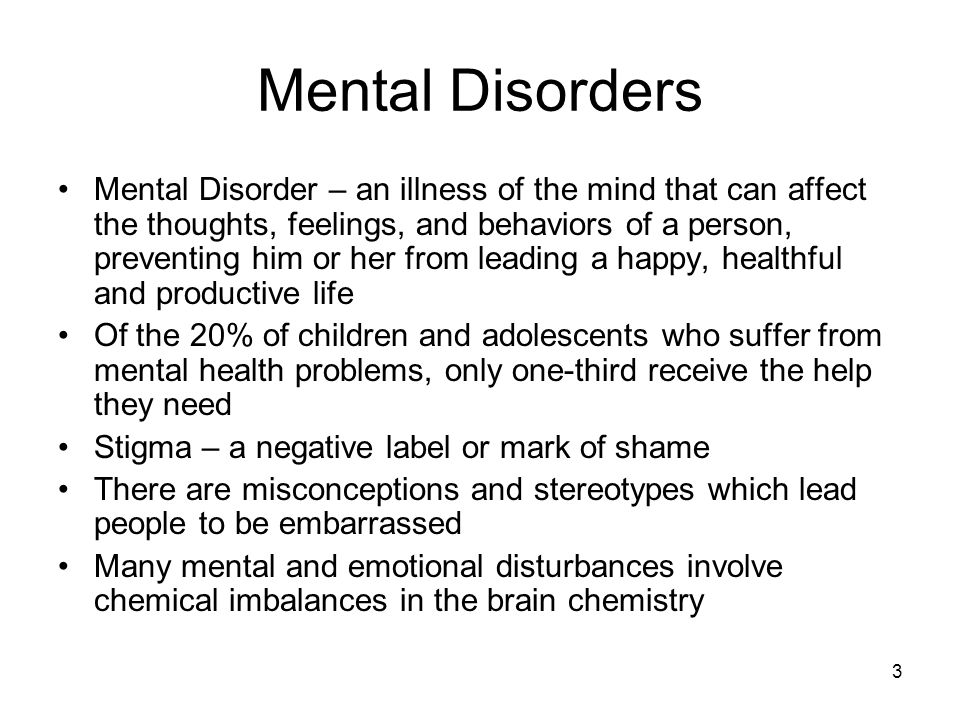
Mental illness, also called mental health disorders, refers to a wide range of mental health conditions — disorders that affect your mood, thinking and behavior. Examples of mental illness include depression, anxiety disorders, schizophrenia, eating disorders and addictive behaviors.
Many people have mental health concerns from time to time. But a mental health concern becomes a mental illness when ongoing signs and symptoms cause frequent stress and affect your ability to function.
A mental illness can make you miserable and can cause problems in your daily life, such as at school or work or in relationships. In most cases, symptoms can be managed with a combination of medications and talk therapy (psychotherapy).
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
Signs and symptoms of mental illness can vary, depending on the disorder, circumstances and other factors. Mental illness symptoms can affect emotions, thoughts and behaviors.
Examples of signs and symptoms include:
- Feeling sad or down
- Confused thinking or reduced ability to concentrate
- Excessive fears or worries, or extreme feelings of guilt
- Extreme mood changes of highs and lows
- Withdrawal from friends and activities
- Significant tiredness, low energy or problems sleeping
- Detachment from reality (delusions), paranoia or hallucinations
- Inability to cope with daily problems or stress
- Trouble understanding and relating to situations and to people
- Problems with alcohol or drug use
- Major changes in eating habits
- Sex drive changes
- Excessive anger, hostility or violence
- Suicidal thinking
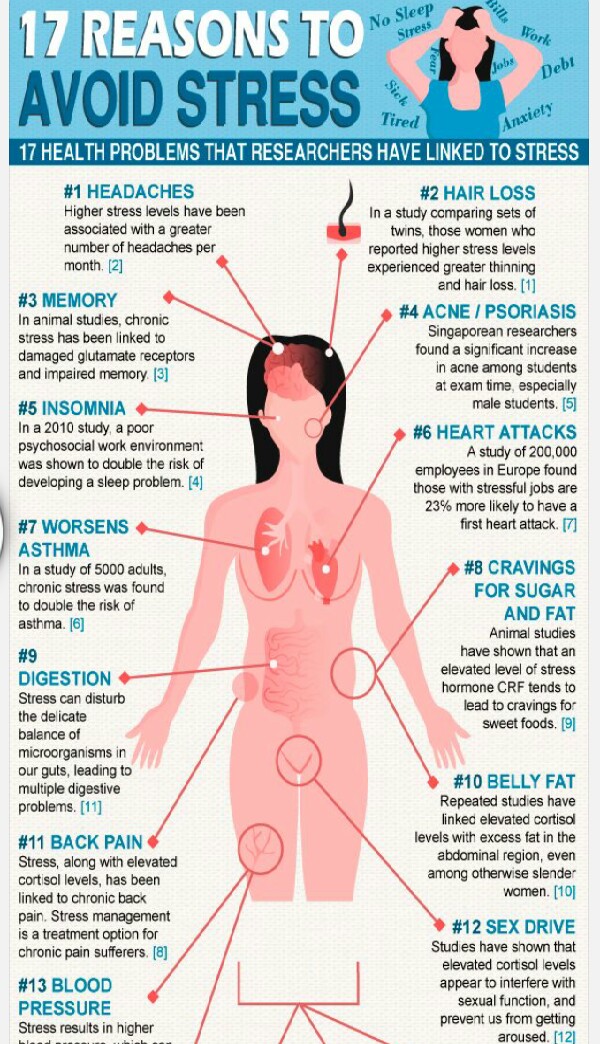
Sometimes symptoms of a mental health disorder appear as physical problems, such as stomach pain, back pain, headaches, or other unexplained aches and pains.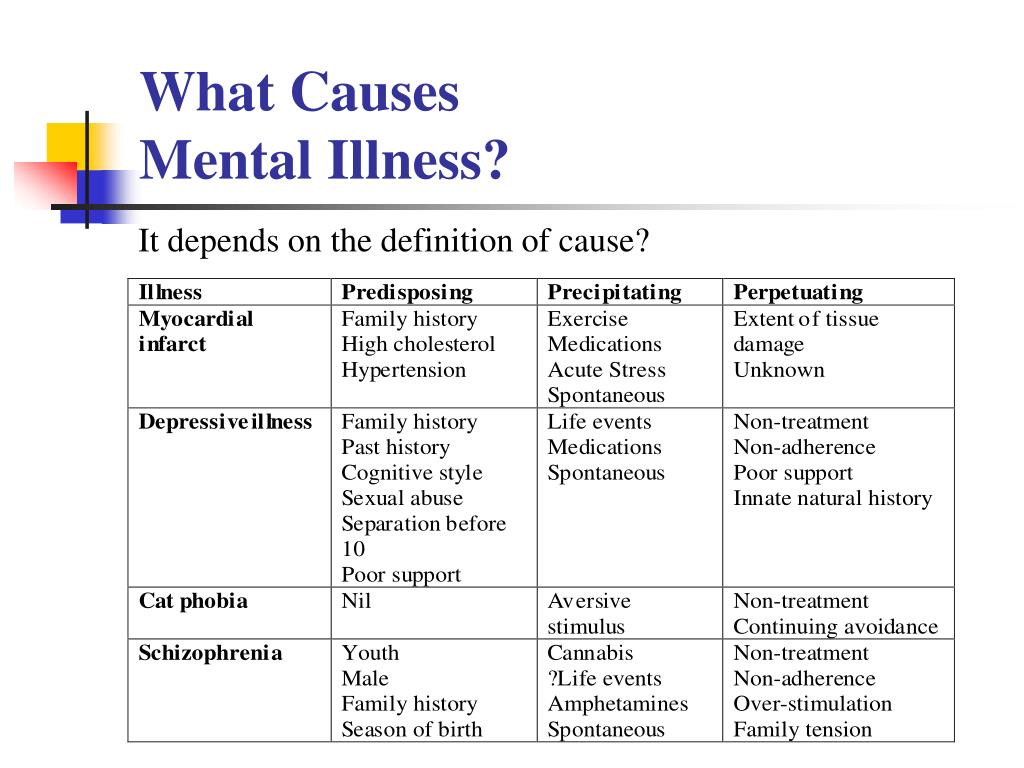
When to see a doctor
If you have any signs or symptoms of a mental illness, see your primary care provider or a mental health professional. Most mental illnesses don't improve on their own, and if untreated, a mental illness may get worse over time and cause serious problems.
If you have suicidal thoughts
Suicidal thoughts and behavior are common with some mental illnesses. If you think you may hurt yourself or attempt suicide, get help right away:
- Call 911 or your local emergency number immediately.
- Call your mental health specialist.
- Call a suicide hotline number. In the U.S., call the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255) or use its webchat on suicidepreventionlifeline.org/chat.
- Seek help from your primary care provider.
- Reach out to a close friend or loved one.
- Contact a minister, spiritual leader or someone else in your faith community.
Suicidal thinking doesn't get better on its own — so get help.
Helping a loved one
If your loved one shows signs of mental illness, have an open and honest discussion with him or her about your concerns. You may not be able to force someone to get professional care, but you can offer encouragement and support. You can also help your loved one find a qualified mental health professional and make an appointment. You may even be able to go along to the appointment.
If your loved one has done self-harm or is considering doing so, take the person to the hospital or call for emergency help.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
Mental illnesses, in general, are thought to be caused by a variety of genetic and environmental factors:
- Inherited traits. Mental illness is more common in people whose blood relatives also have a mental illness. Certain genes may increase your risk of developing a mental illness, and your life situation may trigger it.
- Environmental exposures before birth.
 Exposure to environmental stressors, inflammatory conditions, toxins, alcohol or drugs while in the womb can sometimes be linked to mental illness.
Exposure to environmental stressors, inflammatory conditions, toxins, alcohol or drugs while in the womb can sometimes be linked to mental illness. - Brain chemistry. Neurotransmitters are naturally occurring brain chemicals that carry signals to other parts of your brain and body. When the neural networks involving these chemicals are impaired, the function of nerve receptors and nerve systems change, leading to depression and other emotional disorders.
Risk factors
Certain factors may increase your risk of developing a mental illness, including:
- A history of mental illness in a blood relative, such as a parent or sibling
- Stressful life situations, such as financial problems, a loved one's death or a divorce
- An ongoing (chronic) medical condition, such as diabetes
- Brain damage as a result of a serious injury (traumatic brain injury), such as a violent blow to the head
- Traumatic experiences, such as military combat or assault
- Use of alcohol or recreational drugs
- A childhood history of abuse or neglect
- Few friends or few healthy relationships
- A previous mental illness
Mental illness is common.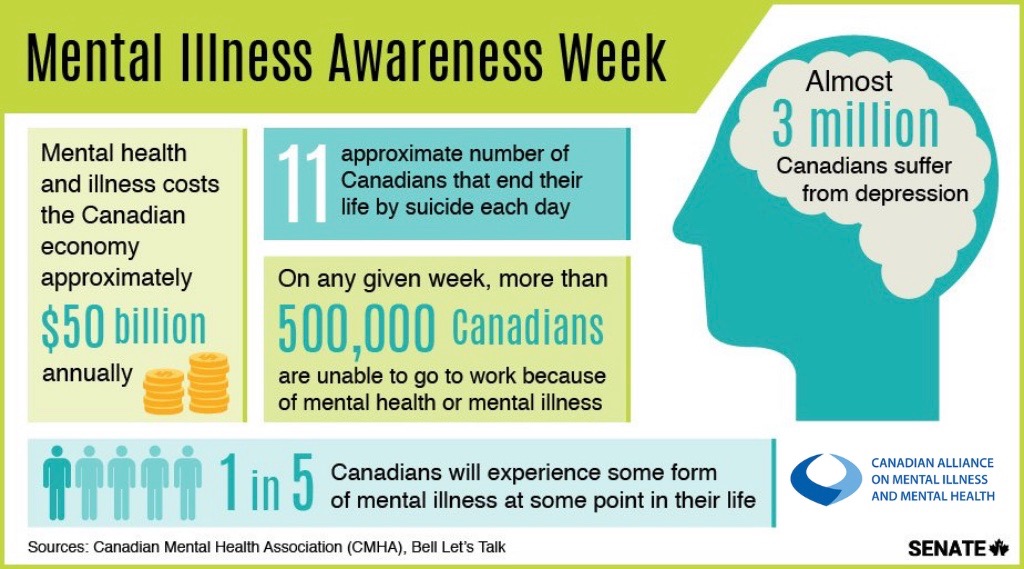 About 1 in 5 adults has a mental illness in any given year. Mental illness can begin at any age, from childhood through later adult years, but most cases begin earlier in life.
About 1 in 5 adults has a mental illness in any given year. Mental illness can begin at any age, from childhood through later adult years, but most cases begin earlier in life.
The effects of mental illness can be temporary or long lasting. You also can have more than one mental health disorder at the same time. For example, you may have depression and a substance use disorder.
Complications
Mental illness is a leading cause of disability. Untreated mental illness can cause severe emotional, behavioral and physical health problems. Complications sometimes linked to mental illness include:
- Unhappiness and decreased enjoyment of life
- Family conflicts
- Relationship difficulties
- Social isolation
- Problems with tobacco, alcohol and other drugs
- Missed work or school, or other problems related to work or school
- Legal and financial problems
- Poverty and homelessness
- Self-harm and harm to others, including suicide or homicide
- Weakened immune system, so your body has a hard time resisting infections
- Heart disease and other medical conditions
Prevention
There's no sure way to prevent mental illness.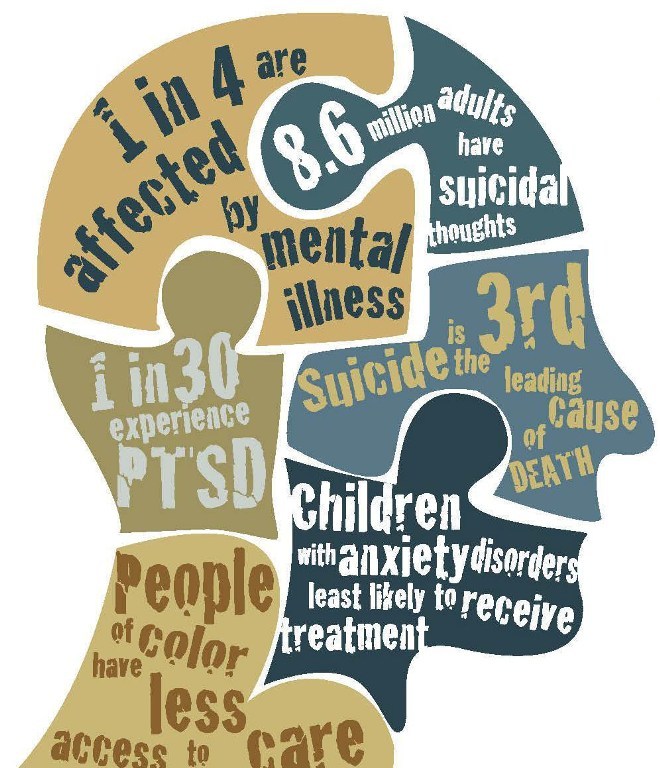 However, if you have a mental illness, taking steps to control stress, to increase your resilience and to boost low self-esteem may help keep your symptoms under control. Follow these steps:
However, if you have a mental illness, taking steps to control stress, to increase your resilience and to boost low self-esteem may help keep your symptoms under control. Follow these steps:
- Pay attention to warning signs. Work with your doctor or therapist to learn what might trigger your symptoms. Make a plan so that you know what to do if symptoms return. Contact your doctor or therapist if you notice any changes in symptoms or how you feel. Consider involving family members or friends to watch for warning signs.
- Get routine medical care. Don't neglect checkups or skip visits to your primary care provider, especially if you aren't feeling well. You may have a new health problem that needs to be treated, or you may be experiencing side effects of medication.
- Get help when you need it. Mental health conditions can be harder to treat if you wait until symptoms get bad. Long-term maintenance treatment also may help prevent a relapse of symptoms.

- Take good care of yourself. Sufficient sleep, healthy eating and regular physical activity are important. Try to maintain a regular schedule. Talk to your primary care provider if you have trouble sleeping or if you have questions about diet and physical activity.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Late-life Mental Health - What is Mental Illness? - UTHealth Harris County Psychiatric Center - UT Harris County Psychiatric Center
Aging and Mental Health • Late-Life Mental Health Afflictions • Living with Late-Life Mental Illness • How Family and Friends Can Help
Having sound mental health as an adult does not make a person immune from psychiatric problems later in life. Elderly individuals can also suffer from mental illness. Fortunately, these disorders can usually be diagnosed and treated successfully; few elderly people, however, actually seek help. Many older people simply do not understand mental illnesses; some deny there is a problem; others are ashamed of their problem; yet others simply dismiss it as a result of getting older.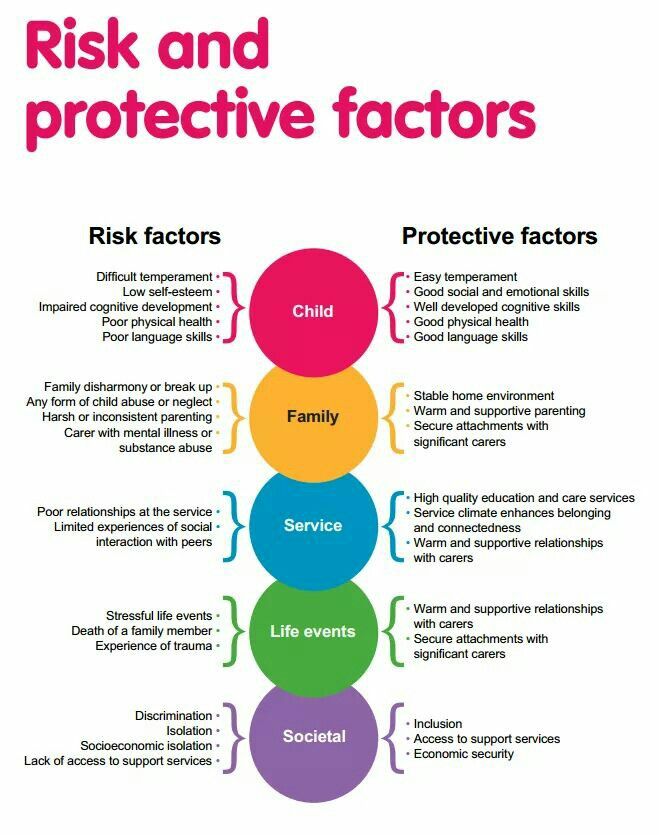 However, proper treatment and care can reduce or eliminate the symptoms, returning people to functioning, happier lives.
However, proper treatment and care can reduce or eliminate the symptoms, returning people to functioning, happier lives.
Aging and Mental Health
Aging is a complex physical, mental, social and spiritual process. It affects each individual differently. Some people remain alert and active well into their 90's. Others seem old in every way as early as their 60's. Some factors that influence the attitudes and behaviors of older people include:
*Personality
*Physical, mental and emotional health
*Intellectual functioning
*Economic and environmental limitations
*Family relationships
*Inner motivation
These factors ultimately affect an older person's overall mental health, causing or complicating one of several mental disorders.
Late-Life Mental Afflictions
Some common mental disorders that afflict elderly people include:
Depression
Depression is a very common mental disorder. It is often mistaken for "the blues" and therefore goes untreated.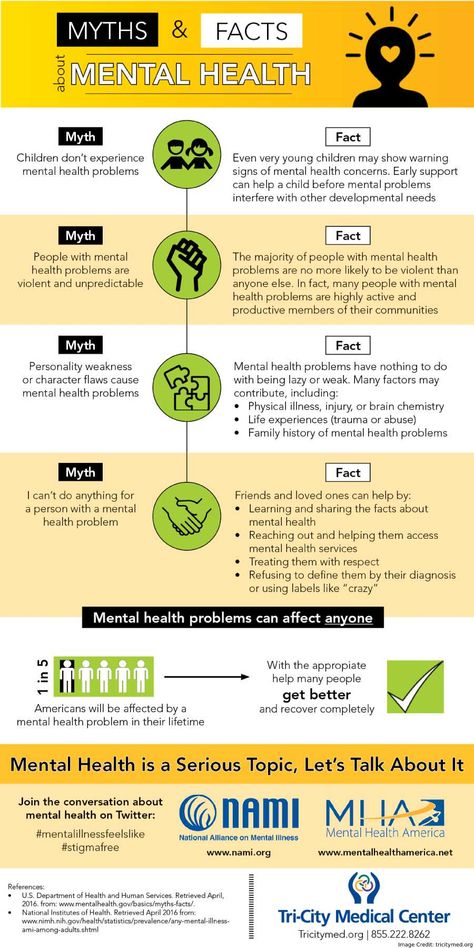 Depression is caused by a number of factors, from chemical imbalances to environmental influences. There are different forms of depression, some mild, others more severe. A person with depression will likely display one or more of the following behaviors:
Depression is caused by a number of factors, from chemical imbalances to environmental influences. There are different forms of depression, some mild, others more severe. A person with depression will likely display one or more of the following behaviors:
* Feelings of worthlessness, hopelessness, helplessness, total indifference and/or extreme guilt
* Prolonged sadness; unexplained crying spells
* Jumpiness or irritability
* Withdrawal from formerly enjoyable activities or relationships
* Inability to concentrate or remember details; indecisiveness
* Noticeable change in appetite with sudden weight loss or gain
* Changes in sleep patterns: constant fatigue, insomnia, early waking, oversleeping
* Physical ailments that cannot be explained otherwise
* Thoughts of death or suicide attempts
Dementia
Dementia is a disorder marked by memory impairment and intellectual decline and changes in comprehension and judgment, language, recognition, behavior and personality. While these symptoms are sometimes thought of as typical signs of growing old, in reality they reflect underlying illnesses. Only a small portion of the aging population, roughly 10 percent, suffers from dementia.
While these symptoms are sometimes thought of as typical signs of growing old, in reality they reflect underlying illnesses. Only a small portion of the aging population, roughly 10 percent, suffers from dementia.
Some conditions that cause dementia include: Alzheimer's disease, stroke, brain infections and tumors, Parkinson's or Huntington's disease, depression, nutritional disorders, excessive medication, and alcoholism.
Some of these conditions associated with dementia are not progressive; they can be stopped or even reversed. It is therefore important that a physician complete a thorough dementia evaluation.
Alzheimer's Disease
Alzheimer's disease, a leading cause of death in America, is a form of dementia. It is a disease that causes brain cells to die, often beginning in a part of the brain that controls memory. As it spreads, it affects a growing number of intellectual, emotional and behavioral abilities.
Alzheimer's disease usually appears slowly and gradually. The first symptoms include loss of recent, short-term memory and mild personality changes, such as mild apathy or social withdrawal. As the disease progresses, patients have trouble with abstract thinking, handling money or other personal affairs, understanding what they are reading or organizing their days. They may also become irritable, troubled and less neat in appearance. In the late stages, patients become seriously confused and disoriented, show significant personality and emotional changes, develop incontinence and ultimately become unable to care for themselves.
The first symptoms include loss of recent, short-term memory and mild personality changes, such as mild apathy or social withdrawal. As the disease progresses, patients have trouble with abstract thinking, handling money or other personal affairs, understanding what they are reading or organizing their days. They may also become irritable, troubled and less neat in appearance. In the late stages, patients become seriously confused and disoriented, show significant personality and emotional changes, develop incontinence and ultimately become unable to care for themselves.
Scientists have been unable to pinpoint the exact cause of Alzheimer's disease, but they are routinely learning more and more about this devastating illness. Although Alzheimer's itself cannot be cured, there are significant treatments to help control the symptoms.
Living with Late-Life Mental Illness
Because of late-life health conditions, elderly people are more likely to require a variety of medications.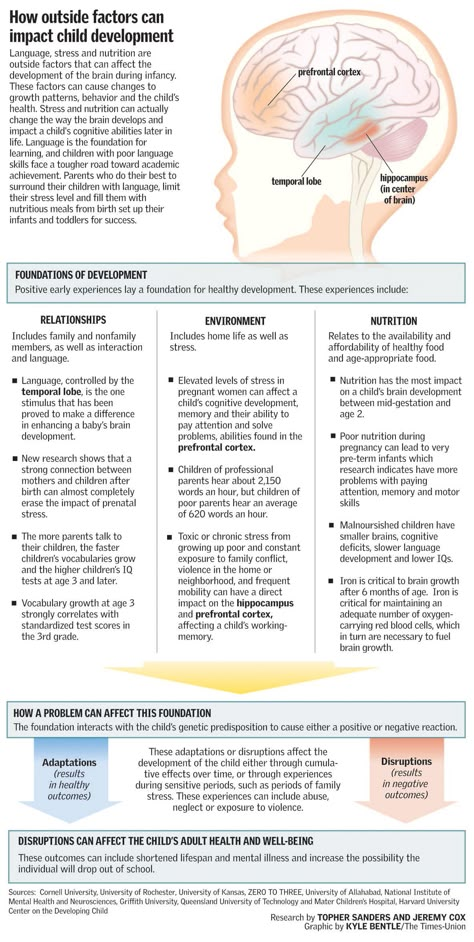 These medications can interact with each other in a negative way, sometimes compounded by alcohol use or abuse. Furthermore, the illness for which these medications are used can result in symptoms that resemble certain mental illnesses.
These medications can interact with each other in a negative way, sometimes compounded by alcohol use or abuse. Furthermore, the illness for which these medications are used can result in symptoms that resemble certain mental illnesses.
It is important that elderly people be aware of their medications and overall physical health status and work closely with their physicians to find regimens that are safe and effective.
How Family and Friends Can Help
Reaching elder years can bring about changes - physical, mental, emotional and social - that can affect one's life. Many are not ready to accept this change, and it can therefore be a difficult experience. Family and friends can help by offering emotional support - understanding, patience, affection and encouragement.
Family and friends can also help by becoming involved in their loved one's mental and physical well-being. This may involve encouraging him or her to seek or to stay with treatment, going with the patient to the doctor, or even monitoring whether the patient is taking medication.
Caring for an elderly person can be demanding, stressful and emotionally taxing on family and friends. Many organizations are dedicated to providing support for these people as well.
Mental disorders of late age
Mental disorders of late age are diseases that occur in presenile (presenile, involutional) and senile age. Since there are large differences in the definition of the concept of "late age", in psychiatry, the involutionary period is usually understood as the age from 45 to 55 years, and patients older than 60 years are referred to the old age (V. M. Bleikher, I. V. Kruk "Explanatory Dictionary psychiatric terms", 1995), which is at odds with the WHO classification, according to which patients from 60 to 74 years old are considered elderly, and persons from 75 to 90 years old are classified as old age.
The increase in life expectancy has led to a change in the age structure of the population, manifested in an increase in the proportion of elderly and senile patients and, accordingly, elderly patients who manifest certain somatic disorders, as well as severe mental disorders.
Gerontological mental disorders:
Mental disorders of late age are usually divided into diseases of "organic" origin, which arise on the basis of a certain destructive process and lead to dementia (dementia), and "functional" (reversible and, as a rule, not leading to severe dementia) disorders.
The treatment of affective (manifested by such disorders as depression or manic states) and delusional (manifested mainly by delirium) senile psychoses does not differ from the psychopharmacotherapy of similar conditions in other mental illnesses. At the European Medical Center, we use combined treatment with antipsychotics and antidepressants - depending on the patient's condition, treatment can be started with the use of antipsychotics and, upon reaching a decrease in the patient's anxiety-delusional arousal, it is possible to add antidepressant drugs.
If a patient with affective and affective-delusional senile (senile) psychosis is insensitive to psychotropic drugs, it is possible to prescribe the so-called electroconvulsive therapy (ECT), if there are no contraindications.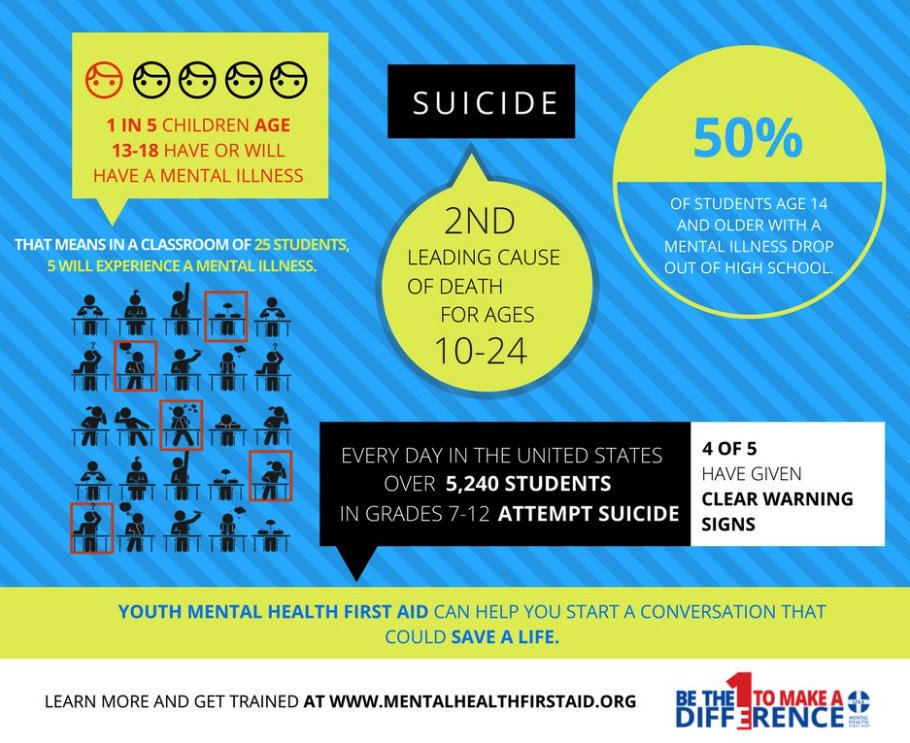 Since ECT is ineffective in delusional forms of senile psychosis, treatment with antipsychotics is used.
Since ECT is ineffective in delusional forms of senile psychosis, treatment with antipsychotics is used.
Psychopharmacological treatment of mental disorders of late age is carried out in a multidisciplinary hospital of the European Medical Center, where patients are provided with comprehensive support and treatment - a complete physical examination is carried out, round-the-clock monitoring of the patient's condition during therapy is provided and complications are prevented.
Parkinson's disease is a degenerative-atrophic disease of the brain that manifests itself at a later age and is often accompanied by mental disorders. The most effective treatment for movement disorders currently used to treat Parkinson's disease is L-DOPA, but the drug has side effects (approximately 50% of patients may experience mental disorders such as confusion, psychomotor agitation with anxiety, agitation, drowsiness, increased depression ). The appointment of L-DOPA follows after a thorough assessment of the mental state of the patient and treatment begins with small doses, which are gradually increased.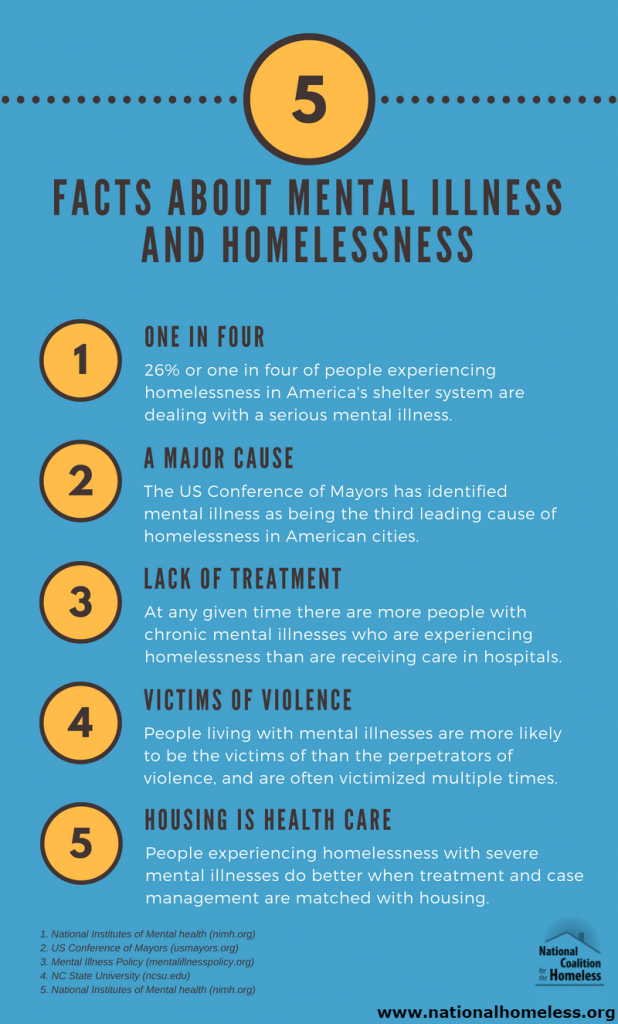 If psychotic disorders occur, along with a gradual decrease in doses of antiparkinsonian drugs (up to temporary cancellation) and detoxification therapy, it is possible to prescribe small doses of psychotropic drugs.
If psychotic disorders occur, along with a gradual decrease in doses of antiparkinsonian drugs (up to temporary cancellation) and detoxification therapy, it is possible to prescribe small doses of psychotropic drugs.
Alzheimer's disease - an atrophic brain disease that manifests itself mainly in presenile age, which leads to dementia and is accompanied by disorders of higher nervous activity. The prognosis of this disease is unfavorable, and today there are no proven effective methods of its treatment. In the later stages of the process, patients, as a rule, need to be hospitalized in psychiatric hospitals or placed in neuropsychiatric boarding schools.
Senile dementia is the most characteristic mental illness of senile age with a progressive breakdown of mental activity, culminating in most cases in total dementia (decrease in all intellectual functions). Some foreign psychiatrists consider senile dementia, a kind of completion of the physiological process of aging of the brain, inevitable in old age. With physiological aging, there is also a decrease in the level of mental activity, reminiscent of the initial symptoms of senile dementia. Proper care and symptomatic therapy are important for the fate of such patients - at the initial stage of the disease, patients are recommended to be left in their usual home environment (if their condition allows). Transfer to an unusual (including hospital) environment can cause an aggravation of the course of the disease. Patients are hospitalized only for special indications (helplessness, lack of care, danger to themselves and others).
With physiological aging, there is also a decrease in the level of mental activity, reminiscent of the initial symptoms of senile dementia. Proper care and symptomatic therapy are important for the fate of such patients - at the initial stage of the disease, patients are recommended to be left in their usual home environment (if their condition allows). Transfer to an unusual (including hospital) environment can cause an aggravation of the course of the disease. Patients are hospitalized only for special indications (helplessness, lack of care, danger to themselves and others).
There are no convincing data indicating the effectiveness of the treatment of senile dementia with nootropic drugs, and therefore such therapy can be recommended only in the initial stages of the disease, as well as in the combination of senile dementia with cerebral atherosclerosis. Psychotropic drugs in very small doses are indicated only when the patient is very agitated, persistent insomnia or psychotic disorders.
What mental illnesses are inherited - Atlant, medical center
Are mental illnesses hereditary? This question worries many parents. After all, it is very scary to “reward” your child with a mental disorder.
How mental illnesses are transmitted
The fact that mental illness can be inherited has been noticed for a long time. Today, geneticists confirm: indeed, mental disorders are more likely to appear in a child in a family where a relative suffered from a similar illness. And the reason for this are violations in the structure of genes.
There is such a thing as the coefficient of hereditary risk. The higher this coefficient, the higher the likelihood that the child will inherit the disease of relatives.
Only some mental illnesses are directly related to breakdowns in the genes, for example, Huntington's chorea, the hereditary risk coefficient of which is 5000. For comparison, for such a mental illness as schizophrenia, it is 9.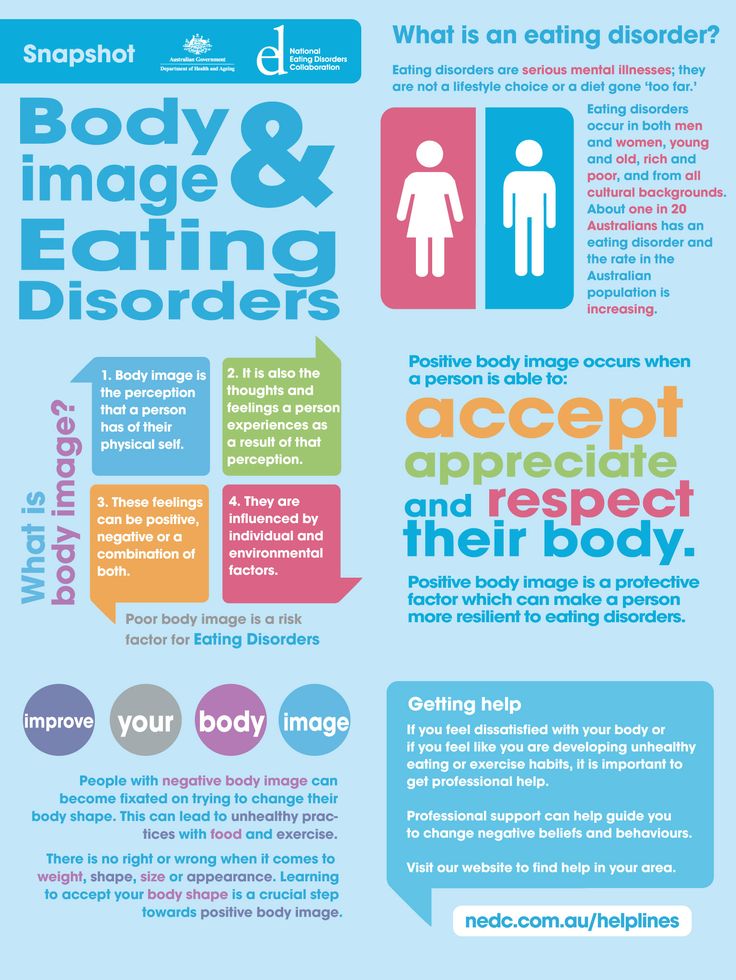
How does the degree of relationship affect hereditary diseases?
The risk of developing a mental illness depends on the degree of relationship with a sick family member and on the number of sick relatives.
The highest probability of transmission of the disease in identical twins, followed by 1st degree relationship (parents, children, brothers, sisters). In 2nd degree relatives, the risk is significantly reduced
So, with schizophrenia, which is present in the mother and father, the probability of its occurrence in children is 46%, if one parent is sick - about 13%, if the grandfather or grandmother is sick - 5%.
Which mental illnesses are most often inherited
1. Disorders of the mental development of children
- Attention deficit hyperactivity disorder (ADHD) is manifested by impulsivity, difficulty concentrating, increased physical activity. Often this disorder is combined with depression, behavioral disorders.
- Dyslexia - the inability to read, compare what is written with speech in some cases is hereditary.
- Autism is a severe mental disorder, which is expressed in violation of social adaptation. An autistic child is closed, he does not want to communicate with the outside world, he exists in his personal space. He does not tolerate any change, he has his own rituals, which he strictly observes. He constantly repeats stereotypical movements (rocking, bouncing) or the same phrases.
Autism is usually diagnosed in the first three years of a child's life.
It is believed that the role of heredity in the occurrence of this disease is great.
2. Schizophrenia
This is a mental illness, which is characterized by disturbances in thinking, perception of the world, inappropriate behavior and an abnormal reaction to stimuli. The disease may be accompanied by agitation, delusions, hallucinations. Patients are prone to depression and suicidal.
As a rule, the onset of the disease falls on the age of 20-22 to 30 years.
Heredity plays a significant role in the occurrence of this disease, but other factors are no less important: complications during gestation, difficult childbirth in the mother, infections, difficult psycho-emotional situations, and even birth in winter.
3. Affective bipolar disorder
Otherwise, this mental illness is called manic-depressive psychosis. It proceeds with an alternation of phases: depression and excitement, sometimes with aggression. There may be gaps between these phases.
4. Alzheimer's disease
This disease develops after the age of 65 and is expressed first in forgetfulness, difficulty concentrating. Then there is confusion, loss of orientation in space. Irritability, unmotivated aggression appear, speech is disturbed. Dementia develops.
Rarely enough, the disease begins earlier, and here the hereditary factor, the pathological gene, plays a significant role.
Other hereditary mental illnesses:
- epilepsy;
- psychopathy;
- alcohol dependence;
- dementia;
- Down syndrome;
- Huntington's chorea;
- "cat cry" syndrome;
- Klinefelter's syndrome.
All of these mental illnesses can be inherited. At the same time, they can appear in a family where no one has suffered from such disorders. True, the risk of disease in this case is less, but it exists. So, you can get schizophrenia in a completely “healthy” family with a probability of 1%.
If there is a risk
Many people are afraid of passing on hereditary diseases to their children (even if distant relatives suffered from them), especially mental disorders, and therefore prefer not to have a child. Is such an approach correct?
A hereditary disease does not mean at all that a child will definitely have it. Yes, there is such a risk, but it is also present in children from "hereditarily safe" families.