Excessive sensitivity to stimuli
Hyperesthesia: Causes, Symptoms, and Treatment
Hyperesthesia refers to increased sensitivity of any of your senses, such as sight, sound, touch, and smell. It can affect just one or all of the senses.
Often, the heightening of an individual sense is referred to by a separate name. For example, increased sensitivity to touch is called tactile sensitivity, and increased sensitivity to sound is called auditory sensitivity.
The term also refers to increased pain sensations. According to the International Association for the Study of Pain, hyperesthesia includes two different subcategories of enhanced pain sensation:
- Hyperalgesia. A stimulus triggers increased or extreme sensitivity to pain.
- Allodynia. A stimulus that is not usually painful suddenly triggers pain.
We explain how hyperesthesia shows itself, why it happens, and how to manage it.
The symptoms of hyperesthesia vary between people. They depend on which senses are affected and how severely:
- Some people with touch sensitivity can experience severe pain when a stimulus triggers their nerves.
- People with auditory sensitivity can hear painfully loud noises when none have occurred in the environment.
- Those with smell sensitivity often report a wide range of smells without the presence of a stimulus.
Some people will experience a combination of these symptoms. Severe hyperesthesia can also affect the nervous system, which might lead to nerve inflammation and seizures.
Neuropathic pain is a common underlying cause of hyperesthesia, but many diseases or lesions of the nervous system can lead to this type of pain.
Associated health conditions and stimuli include (but are not limited to):
- systemic diseases like diabetes, nutritional deficiencies, and hypothyroidism
- infectious diseases, such as HIV, herpes, hepatitis C, and varicella
- toxic causes, including alcohol, certain chemotherapy drugs, and immunosuppressants
- mechanical causes, such as physical trauma, complex regional pain syndrome, nerve root compression, and phantom limb pain after an amputation
- hereditary causes like Charcot-Marie-Tooth disease
Risk factors
Children with autism, obsessive-compulsive disorder (OCD), and attention deficit hyperactivity disorder (ADHD) are more likely to develop hyperesthesia.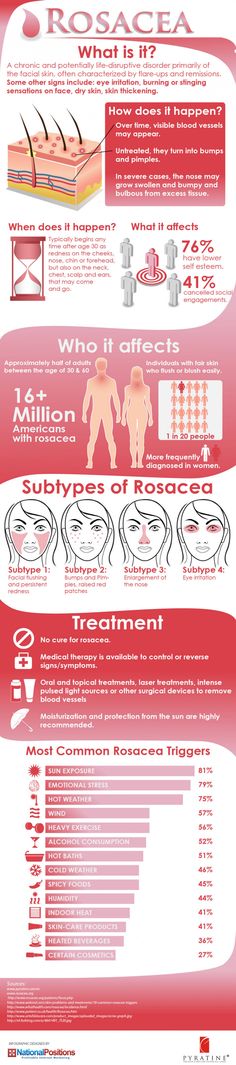
Many people in menopause also report a particular type of hyperesthesia called formication, in which they experience sensations on the skin such as tingling, crawling, or itching.
The treatment for hyperesthesia centers around addressing the underlying cause. If you experience hyperesthesia due to diabetic neuropathy, keeping your blood glucose under control can help keep the problem from getting worse.
If a vitamin B12 deficiency is causing the hyperesthesia, a physician might prescribe B12 supplements. After treating the underlying condition or removing the triggering stimulus, most people will find that the symptoms of hyperesthesia resolve.
If there’s an underlying problem in the brain or spinal cord, your doctor will assess and treat this accordingly.
Managing the effects of episodes
Some conditions linked to neuropathy, like diabetes, are chronic. It’s important to find methods of reducing the physical and emotional sensations around hypersensitivity.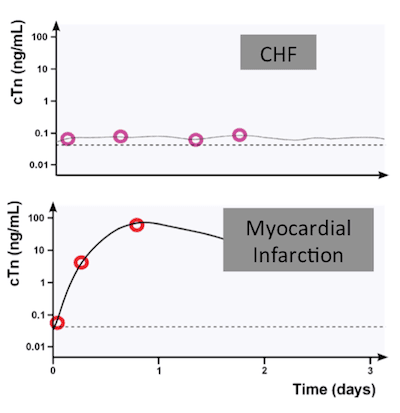
What you can do
It’s important to remember that the condition is usually manageable. Making certain lifestyle changes can ease your symptoms considerably. You may want to try to:
- Reduce your caffeine and alcohol intake, or eliminate them completely.
- Eat a well-balanced, nutritious diet.
- Train yourself to stay calm during flares of hypersensitivity by regularly practicing yoga or meditation.
What your doctor can do
Some medical interventions might also help, including:
- Physical therapy. This can help people who experience increased pain as a result of their hyperesthesia regain mobility and improve their quality of life.
- Cognitive behavioral therapy (CBT). CBT can be effective in reducing the unpleasant responses caused by any stimulus.
- Antiepileptic drugs, including gabapentinoids. People experiencing seizures can take anticonvulsant medications to reduce the frequency and severity of their seizures.
 These medications can also help reduce hyperesthesia pain in people who don’t experience seizures.
These medications can also help reduce hyperesthesia pain in people who don’t experience seizures. - Anxiolytic medications. People can take anxiety-reducing medication if they are experiencing fear and anxiety around their condition. Hyperesthesia can be debilitating and affect your ability to be around the many stimuli of daily life. This can have a negative effect on your mental health.
- Antidepressant medications. Antidepressants can help reduce neuropathic pain as well as depression.
A 2020 review suggests a diet with plenty of flavonoids might help people reduce the effects of neuropathy. Flavonoids are compounds in plants that provide antioxidants, which help counter the harmful effects of damaging free radical molecules around your body.
However, the review largely used studies that tested the effects of flavonoids in a lab and on animals, rather than in humans. The review also focused only on peripheral neuropathy, but other types like central neuropathy might work differently.![]()
So, it’s difficult to say that the findings can carry over to humans or all types of neuropathy, but they are promising.
What to do during an episode of hyperesthesia
In the moment, hyperesthesia can feel overwhelming and never-ending.
If you’re experiencing an episode of hyperesthesia, lie down in a dark room that’s as free from stimuli as possible. This can help the symptoms pass more quickly.
Try to remain calm and practice some deep breathing exercises.
Your outlook for hyperesthesia will depend on the underlying cause. Supplementing a B12 deficiency can clear up hyperesthesia symptoms entirely. For neurodiverse people, managing overstimulation will likely be a lifelong health goal.
Hyperesthesia can be unsettling and may cause pain, fear, and anxiety in those who live with it.
Hyperesthesia can exist on its own or as a symptom of another related health condition. Whichever applies to you, your doctors will try to diagnose the root cause so it can be treated effectively.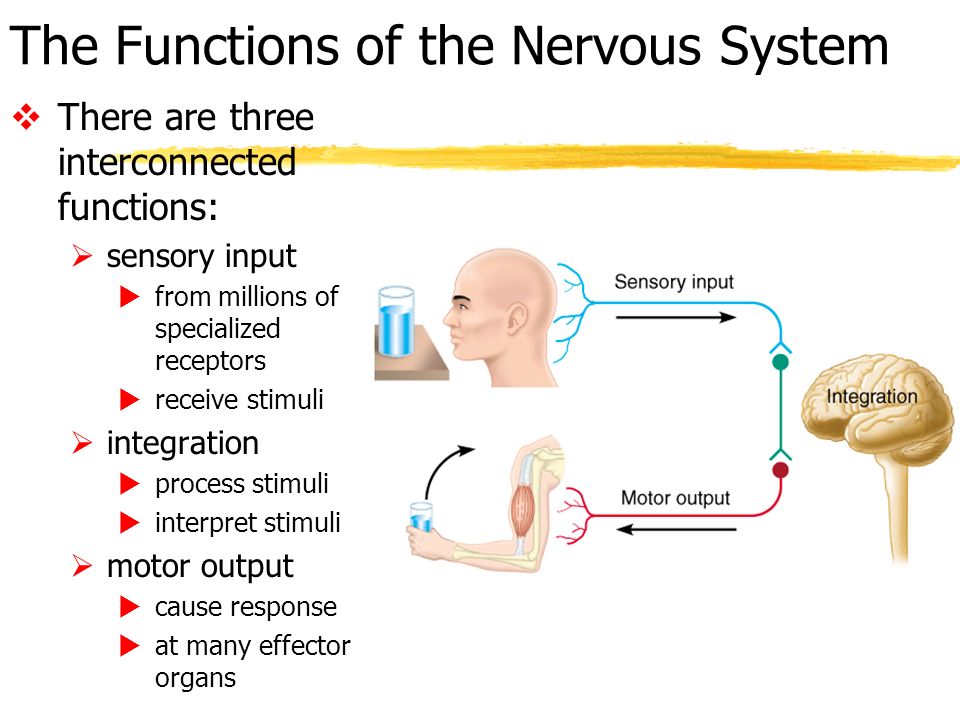
Hyperesthesia - StatPearls - NCBI Bookshelf
Continuing Education Activity
Hyperesthesia occurs as a symptom of neuropathic pain and can be present in any disease process that affects the somatosensory nervous system. Treatment involves treating underlying conditions and symptomatic support. A multidisciplinary approach that is able to provide timely diagnosis and treatment, has the best outcomes. This activity outlines the evaluation and management of hyperesthesia and reviews the role of the interprofessional team in evaluating and treating patients with this condition.
Objectives:
Summarize the etiology of hyperesthesia.
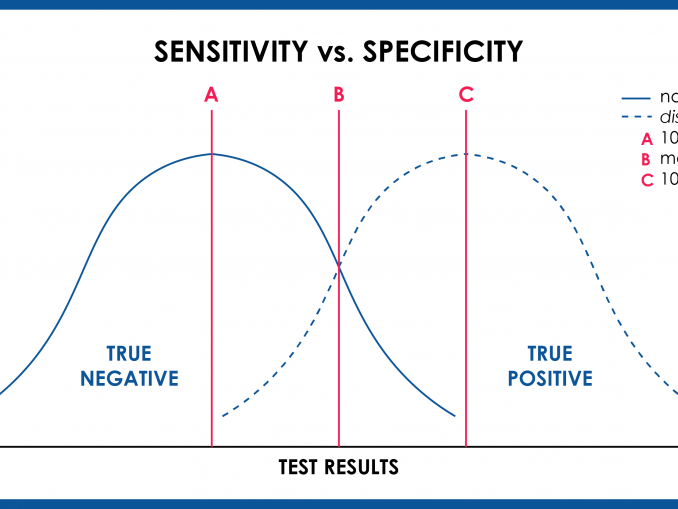
Identify which studies are appropriate to make a diagnosis of hyperesthesia.
Outline the treatment strategy of hyperesthesia/neuropathic pain.
Access free multiple choice questions on this topic.
Introduction
The International Association for the Study of Pain defines hyperesthesia as “increased sensitivity to stimulation, excluding the special senses,” which “may refer to various modes of cutaneous sensibility including touch and thermal sensation without pain, as well as to pain.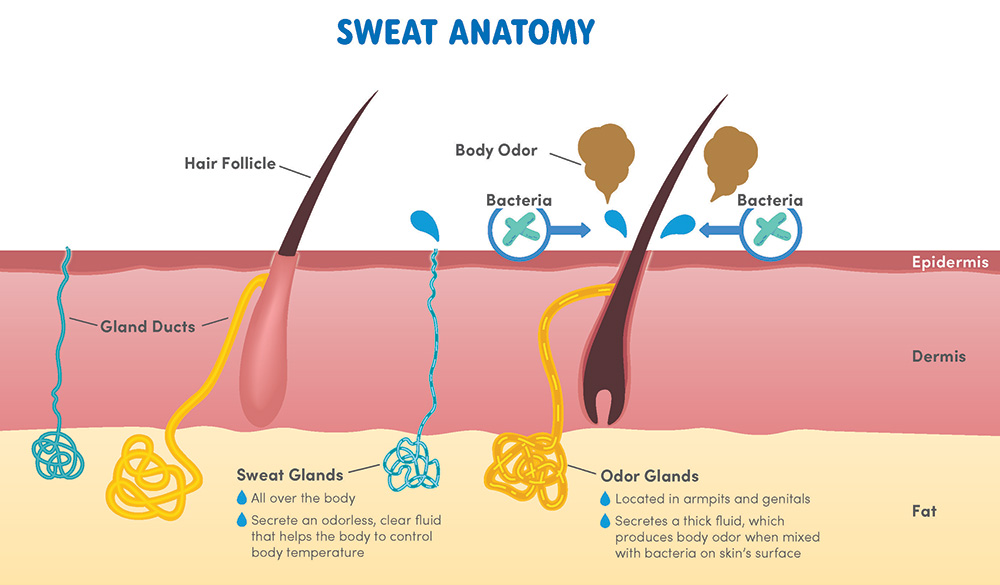 ” While hyperesthesia can be used to describe any increased sensitivity to a stimulus, it is commonly used to describe a painful sensation from a stimulus.
” While hyperesthesia can be used to describe any increased sensitivity to a stimulus, it is commonly used to describe a painful sensation from a stimulus.
Hyperesthesia is a common symptom of neuropathic pain. Neuropathic pain is defined by the International Association for the Study of Pain as “pain caused by a lesion or disease of the somatosensory system.” The neuropathic pain phenotype contains a spectrum of symptoms that can be roughly categorized into positive and negative symptoms. Hyperesthesia is a positive symptom of neuropathic pain. Positive symptoms are categorized as stimulus-dependent pain, stimulus-independent pain, and paresthesias.[1] Neuropathic pain affects about 7-8% of the general population.[2][3]
In this article, hyperesthesia will be defined as an increased cutaneous sensitivity manifesting as stimulus-dependent neuropathic pain. The most common hyperesthesias are allodynia and hyperalgesia. Allodynia is a pain caused by a stimulus that usually does not elicit a painful response (i.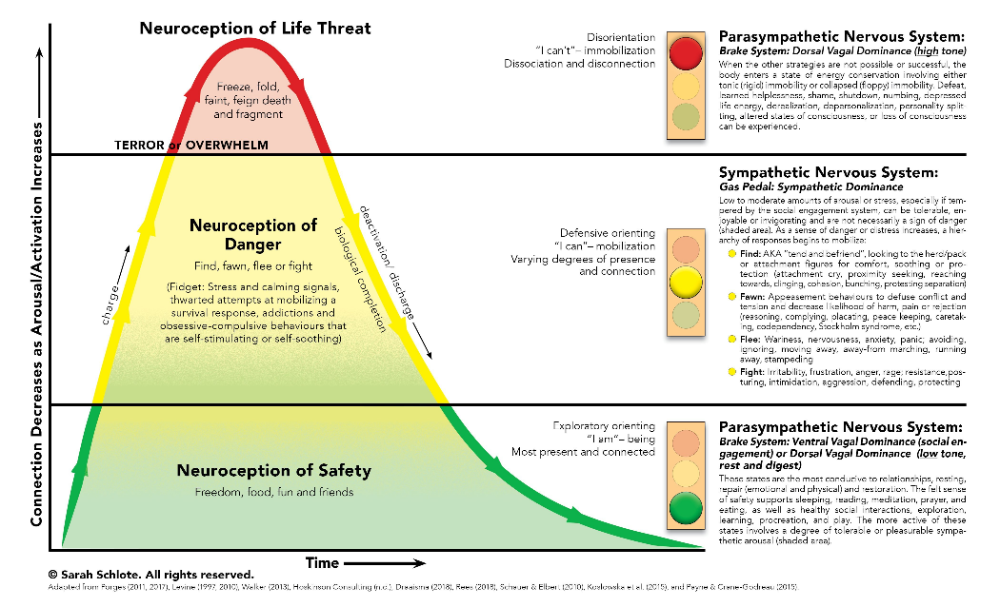 e., pain on light touch). Hyperalgesia is an exaggerated pain response to a stimulus that usually causes pain (i.e., out of proportion pain from a pinprick). While most neuropathic pain symptoms are contained within the dermatomal distribution of the affected nerve, hyperesthesia has been known to extend beyond the affected nerve’s distribution. This can sometimes obscure the correct diagnosis and lead to the inappropriate diagnosis of a psychosomatic disorder.[4]
e., pain on light touch). Hyperalgesia is an exaggerated pain response to a stimulus that usually causes pain (i.e., out of proportion pain from a pinprick). While most neuropathic pain symptoms are contained within the dermatomal distribution of the affected nerve, hyperesthesia has been known to extend beyond the affected nerve’s distribution. This can sometimes obscure the correct diagnosis and lead to the inappropriate diagnosis of a psychosomatic disorder.[4]
A detailed history and a thorough physical examination should be sufficient to identify the underlying etiology. Routine laboratories should be ordered as part of the workup. Special laboratory, diagnostic, and imaging tests may have to be ordered to make a definitive diagnosis of the etiology. Treatable and reversible etiologies should be promptly treated. The mainstay of treatment is symptomatic relief via pharmacological, non-pharmacological, and interventional therapies. Symptoms are typically challenging to eliminate, and patients will most likely continue to experience persistent symptoms. A multidisciplinary team approach has been shown to provide the most effective and lasting results.
A multidisciplinary team approach has been shown to provide the most effective and lasting results.
Etiology
Neuropathic pain symptoms, including hyperesthesia, develop secondarily to a disease or a lesion of the nervous system that results in abnormal functioning of the somatosensory system. The etiology of hyperesthesia can be categorized anatomically or etiologically. Anatomically speaking, the source can be either central or peripheral.
Peripheral
Systemic disease: diabetes mellitus (DM), nutritional deficiency, hypothyroidism, vasculitis, sarcoidosis, carcinoma/paraneoplastic, Guillain-Barre syndrome/acute inflammatory demyelinating polyneuropathy, chronic demyelinating inflammatory neuropathies, monoclonal gammopathy (amyloidosis, multiple myeloma, plasmacytoma, monoclonal gammopathy of undetermined significance), porphyria, Sjogren’s syndrome, and critical illness.
Infectious: human immunodeficiency viruses (HIV), human T-cell lymphotropic virus, herpes simplex virus, varicella-zoster virus, Ebstein-Barr virus, West Nile virus, hepatitis C virus, rabies virus, cytomegalovirus, diphtheria, Campylobacter jejuni, Mycobacterium tuberculosis, Mycobacterium leprae, Brucella spp.
 , Clostridium botulinum, and Borrelia burgdorferi.[5]
, Clostridium botulinum, and Borrelia burgdorferi.[5]Toxic:
Drugs: isoniazid, chemotherapeutics (vinca-alkaloids, taxanes, platinum compounds), statins, amiodarone, antimicrobials (isoniazid, linezolid, and metronidazole), and immunosuppressants (tumor necrosis factor inhibitors, leflunomide, and nucleoside analog reverse-transcriptase inhibitors).[6]
Other toxins: ethanol and heavy metals
Mechanical: trauma, compressive mononeuropathies, complex regional pain syndrome type, post-amputation pain/phantom limb pain, trigeminal neuralgia, post-mastectomy pain syndrome, failed back surgery syndrome, and radiculopathies (nerve root compression)
Hereditary: Charcot-Marie-Tooth disease and metachromatic leukodystrophy
Central
Systemic disease: B12 myelopathy, multiple sclerosis, spinal cord stroke, brain stroke/central post-stroke pain syndrome(CPSP), opioid-induced hyperalgesia, and infectious (Herpes simplex virus, myelitis, encephalitis)
Mechanical: spinal cord injury, tumor compression (brain and spinal cord), syringomyelia, and myelopathy[1][7][8][9]
Epidemiology
Epidemiological studies of hyperesthesia are technically challenging to perform. Barriers to performing accurate epidemiological studies include the vast amount of conditions that can cause hyperesthesia and the subjective nature of hyperesthesia. Two epidemiological studies that focused on the prevalence of chronic pain with neuropathic pain features estimated that the prevalence of neuropathic pain among the general population to be 7% to 8%.[2][3]
Barriers to performing accurate epidemiological studies include the vast amount of conditions that can cause hyperesthesia and the subjective nature of hyperesthesia. Two epidemiological studies that focused on the prevalence of chronic pain with neuropathic pain features estimated that the prevalence of neuropathic pain among the general population to be 7% to 8%.[2][3]
One study that used a questionnaire to assess sensory symptoms in patients with painful diabetic neuropathy (PDN) and postherpetic neuralgia (PHN) found that allodynia was present in about 50% of the PHN patients. That study contained 1600 patients with PDN, of which 18% reported pain to light touch, and 14% reported occasional pain with heat or cold.[10] Another study performed quantitative sensory testing of 1236 patients with diagnosed neuropathic pain. The study used both mechanical and thermal stimuli. Their results showed that 20% of patients had brush-provoked allodynia. The study also found that mechanical hyperalgesias (pinprick 29% and blunt pressure 36%) occurred more often than thermal hyperalgesias (hot 24% and cold 19%). [11]
[11]
Pathophysiology
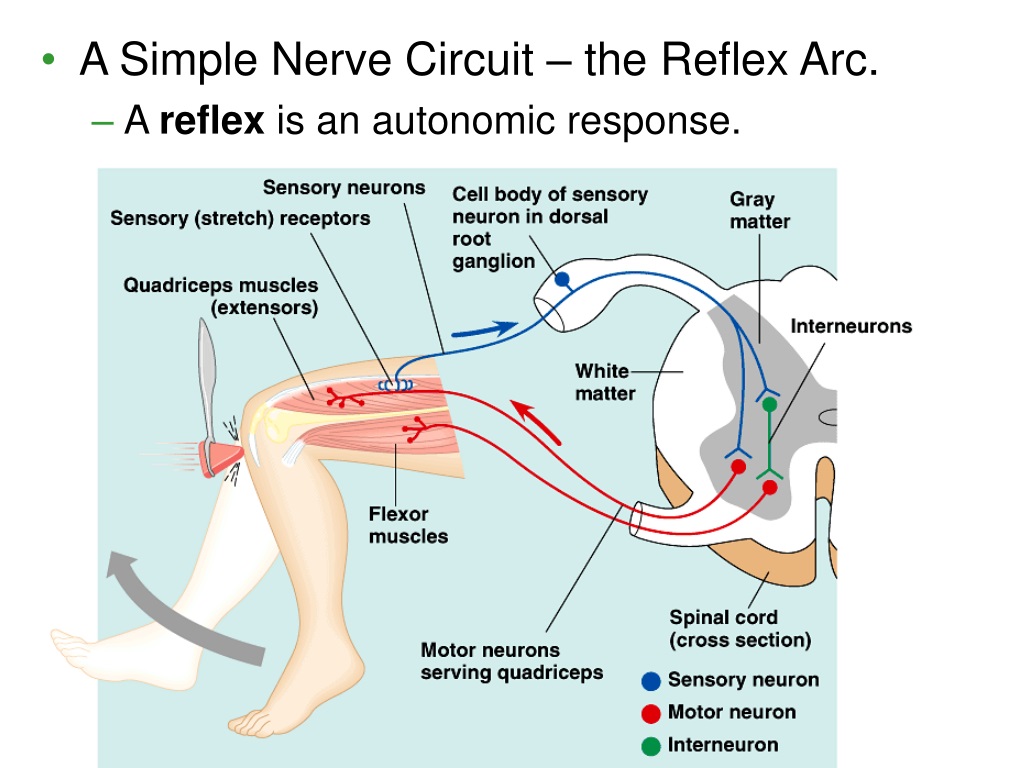
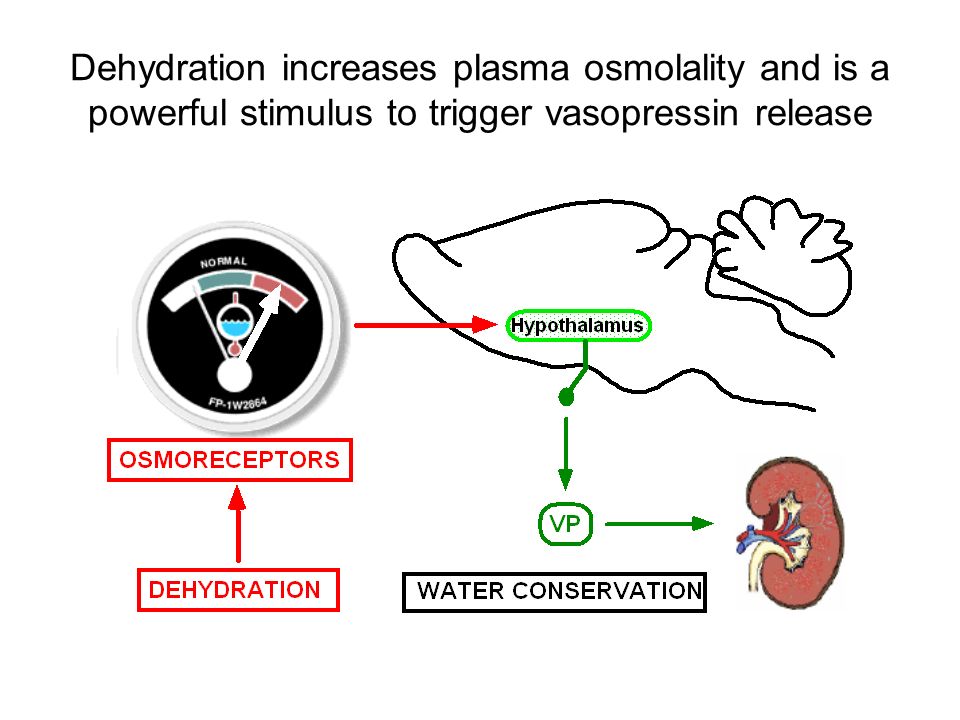
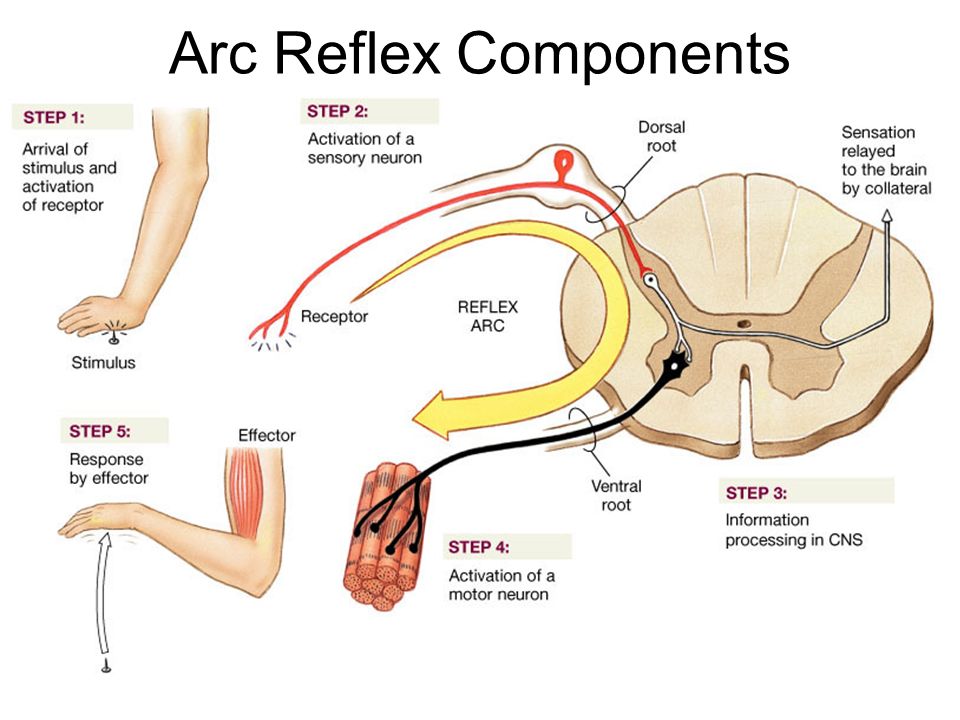
The pathophysiology of neuropathic pain has been extensively studied, and several important mechanisms have been identified. Some of the identified mechanisms provide clear explanations for the development of hyperesthesias.[7] The mechanisms that lead to the development of hyperesthesia are central sensitization of the somatosensory system, peripheral sensitization of the somatosensory system, and dysfunction of endogenous pain inhibition. It is believed that mechanical hyperesthesia(e.g., light pinprick and light manual pressure) and mechanical allodynia (i.e., stroking the skin with a brush) is due to the sensitization of the somatosensory system (i.e., peripheral sensitization and central sensitization) and dysfunction of endogenous pain inhibition.[12] Cold hyperesthesias are believed to be due to either peripheral sensitization or central disinhibition. Heat hyperesthesias are believed to be due to peripheral sensitization of nerve fibers.[13]
Central sensitization is defined as an increase in the synaptic efficacy and excitability of nociceptive pathways in the central nervous system (CNS).
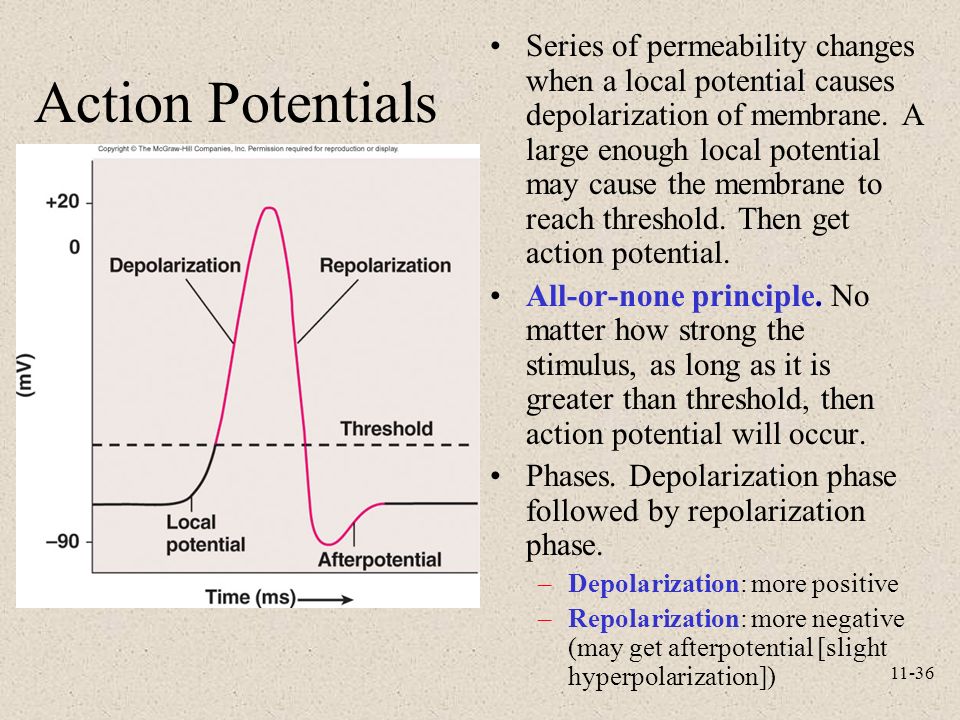 Through this mechanism, pain signals entering the CNS are amplified. The process by which the central sensitization of the somatosensory system occurs is not well understood. One proposed mechanism suggests that A-beta touch cells undergo phenotypic changes, which then express increased levels of neuropeptides and increased activity of amino acid transmission.[12][13]
Through this mechanism, pain signals entering the CNS are amplified. The process by which the central sensitization of the somatosensory system occurs is not well understood. One proposed mechanism suggests that A-beta touch cells undergo phenotypic changes, which then express increased levels of neuropeptides and increased activity of amino acid transmission.[12][13] Peripheral sensitization most often occurs after peripheral nerve inflammation and leads to a reduced threshold for activation and hyperexcitability of primary afferent neurons. This is believed to occur due to post-translational changes, trafficking, and expression of the transient receptor potential cation channel subfamily V member 1 (TRPV1) that arise after nerve damage. After these changes, peripheral nerves are more sensitive to mechanical and thermal stimuli.[13]
Dysfunction of endogenous pain inhibition most likely occurs due to reduced GABA and glycine inhibition of second-order neurons leading to a net excitation of these neurons.
 [14]
[14]
History and Physical
History: A thorough history should be performed, as this should be sufficient to make a diagnosis of hyperesthesia.
Past medical history (diabetes mellitis, stroke, fractures, irritable bowel syndrome)
Psychiatric history (mood disorders)
Medications (use of neurotoxic drugs)
Surgery
Family history
Sexual history
Substance abuse (alcohol or opioid)
Functional history: A functional history that examines the effect of the patient’s symptoms on their ability to function should be performed. It should focus on any impairments to the patient’s activities of daily living, instrumental activities of daily living, ambulatory status (use of assistive devices), work, or sleep.[4]
History of presenting illness: The examiner should gather a thorough description of the patient’s pain symptoms.
 The description of the patient’s symptoms should include all of the following components.
The description of the patient’s symptoms should include all of the following components. Location
Intensity (0-10 rating scale)
Quality (burning, cold, hot, or allodynia) Pain descriptors such as burning, tingling, or shooting are the most characteristic of neuropathic pain syndrome and have a high likelihood of being present along with hyperesthesia.[7]
Onset (did the symptoms occur after an inciting event)
Temporal variation: At what time of the day is the pain worse? (neuropathic pain tends to be worse towards the end of the day) Has the pain progressively worsened over some time?
Radiation (does the pain have axial origin)
Positional variation (i.e., is the pain worse in the lower pack or the thigh)
Aggravating/alleviating factors
Attempted treatments (neuropathic pain symptoms are typically non-responsive to acetaminophen or nonsteroidal anti-inflammatory drugs)
Frequency
Associated symptoms (loss of range of motion, skin or hair changes, muscle spasms, muscle weakness, changes in sensation, redness, or swelling)
Physical exam: A complete neurological exam should be performed in addition to a general focused physical exam.
Cranial nerve testing (CNS lesions may have cranial nerve involvement)
Manual motor testing (weakness may be present in both peripheral and central etiologies, and any weakness should be differentiated as either real weakness or antalgic weakness)
Deep tendon reflexes (may be brisk in central etiologies and diminished in peripheral etiologies)
Sensory testing
Light touch (allodynia)
Pinprick (hyperalgesia)
Vibration and proprioception
Temperature (ice and hot packs for possible thermal allodynia)
Straight leg test or slump test (radiculopathy)
Tinel’s sign (peripheral nerve entrapment)
Myofascial trigger points
For complex regional pain syndrome (CRPS), a skin examination should be performed focusing on cutaneous temperature discrepancies, color changes, hidrosis, scars in a dermatomal distribution, and hair changes.
Evaluation
The first step should be to determine whether the etiology is peripheral or central. It is essential to accurately diagnose the cause of hyperesthesia to provide treatment of any treatable underlying cause.
Laboratory tests:
Routine: Should be considered as part of a standard workup of peripheral hyperesthesia
Complete blood count
Comprehensive metabolic panel
Fasting blood glucose
Erythrocyte sedimentation rate
Thyroids stimulating hormone
Vitamine B12
If indicated, based on clinical suspicion:
Hemoglobin A1c (HbA1c)
HIV antibodies
Liver panel
Lyme antibodies
Rapid plasma reagin (RPR), venereal disease research laboratory (VDRL)
Urinalysis
Urine protein electrophoresis
Serum protein electrophoresis
Angiotensin-converting enzyme levels
Antinuclear antibody (ANA) test
Perinuclear anti-neutrophil cytoplasmic antibodies (P-ANCA) test
Antineutrophil cytoplasmic antibodies (C-ANCA) test
Tests for rare conditions
Paraneoplastic panel
Antimyelin associated glycoprotein
Antiganglioside antibodies
Salivary flow rate
Cerebrospinal fluid analysis
Genetic testing
Imaging: imaging is typically not needed to diagnose hyperesthesia, but it helps diagnose specific conditions.
Computed tomographic scan and magnetic resonance imaging (nerve root compression, herniated disc, myelopathy, tumor in the brain or spinal cord)
Triple phase bone scan (can be used to support a diagnosis of CRPS)[7]
Special Tests:
Electrodiagnostics: electromyography and nerve conduction studies (only tests large fibers)
Punch skin biopsy (identifies small-fiber neuropathy)[7]
Treatment / Management
Treatment of hyperesthesia and other neuropathic pain symptoms is challenging but is best achieved by using a multidisciplinary team approach that can focus on treating underlying causes, administer pharmacotherapy, apply interventional therapy, address functional impairments, and provide mental health services if needed.[7][9] Realistic goals for hyperesthesia should be established early on. Any comorbidities such as mood disorders or sleep disturbances should be addressed promptly. Patients typically require close follow-up to monitor response to therapy and continued evaluation of the underlying cause.
For peripheral neuropathy, the most common treatable causes are diabetes mellitis, hypothyroidism, and nutritional deficiencies.[8] Other causes of hyperesthesia, such as nerve root compression or peripheral nerve entrapment, may be initially treated conservatively with symptomatic pharmacotherapeutic support, physical therapy, lifestyle modifications, and minimally invasive procedures (i.e., epidural steroid injection or peripheral nerve injection). However, if there is worsening or stagnation of function, surgery may be required.
Pharmacological treatments can be used to treat both central and peripheral causes of hyperesthesia. Of the pharmacological options available, antidepressants and antiepileptic drugs are the most widely used.[15] General guidelines for treatment are provided below; however, recommendations for the treatment of choice for specific etiologies are provided.
First-line drugs: These drugs have the most substantial evidence to support their treatment of neuropathic pain symptoms. This group contains two classes of antidepressants and one class of antiepileptic drugs.
This group contains two classes of antidepressants and one class of antiepileptic drugs.
Antidepressants: all medications in this class have the added benefit of treating comorbid mood disorders.
TCAs: Amitryptiline, imipramine, and nortriptyline
Indications: painful diabetic neuropathy (PDN), postherpetic neuralgia (PHN), central poststroke pain (CPSP)
SNRIs: duloxetine and venlafaxine
Indications: PDN, post-traumatic neuropathic pain, CRPS, radiculopathy, and central pain
Antiepileptic drugs:
Gabapentinoids: Gabapentin and pregabalin
Indications: PDN, PHN, central pain, posttraumatic neuropathic pain, CRPS, radiculopathy. Pregabalin has proven to be effective in the treatment of spinal cord injury central pain.[16][17]
Second-line treatments:
Third-line treatments:
Not all patients will respond to monotherapy; in fact, 45% of individuals with neuropathic pain are on two or more medications for their pain.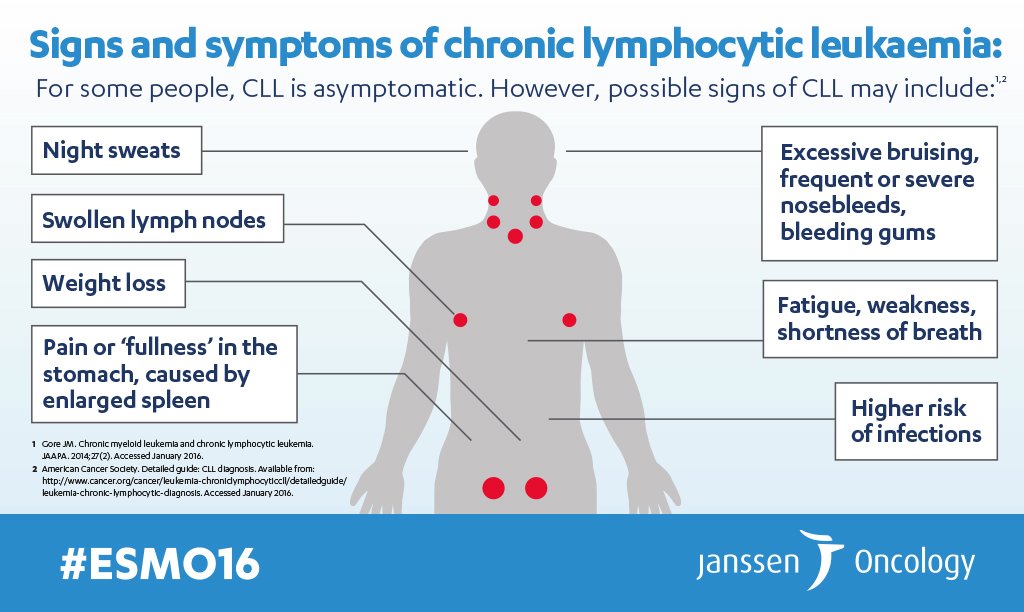 If a patient fails first-line monotherapy, they can be used in combination (i.e., gabapentinoid + TCA or SNRI).[18]
If a patient fails first-line monotherapy, they can be used in combination (i.e., gabapentinoid + TCA or SNRI).[18]
Interventional Therapies:
Epidural steroid injections: considered third-line therapy.
Sympathetic nerve block
Neurostimulation: Fourth-line treatment[18]
Spinal cord stimulation:
Motor cortex stimulation:
Transcutaneous electrical nerve stimulation (TENS)
Some interventional treatments currently being practiced lack robust trials to be recommended by the guidelines. Some of the interventions that require continued research are radiofrequency denervation of the dorsal root ganglion, adhesiolysis for FBSS, TENS, spinal cord stimulation, and motor cortex stimulation.
Differential Diagnosis
Nociceptive source of pain
Myofascial pain syndrome
Fibromyalgia
Chronic fatigue syndrome
Prognosis
It is difficult to completely eliminate hyperesthesias and other neuropathic pain symptoms.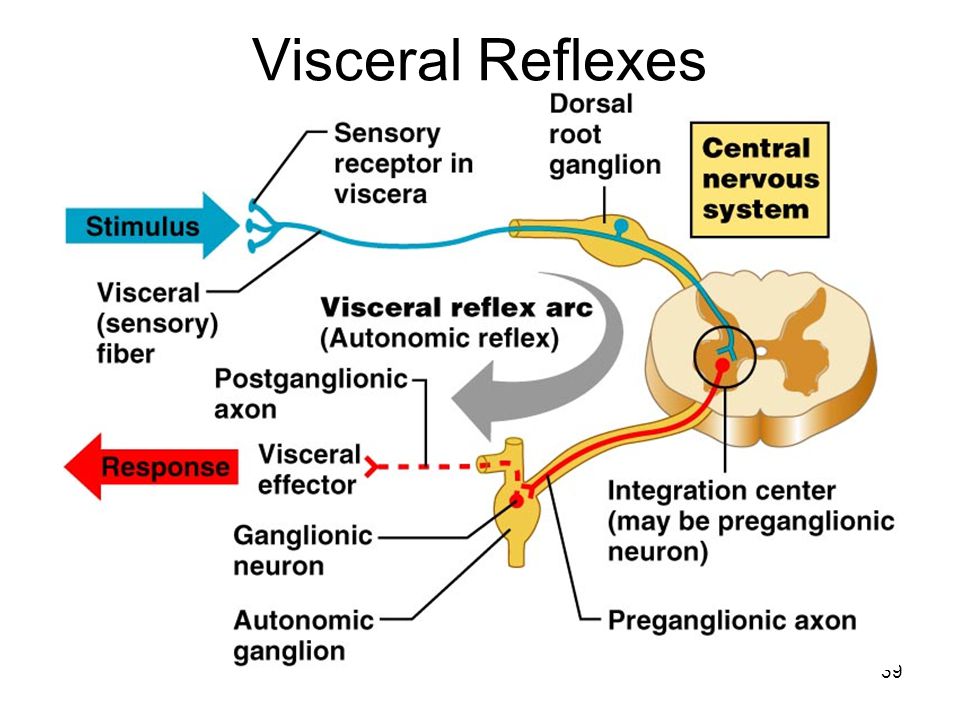 This should be explained to the patient early during the treatment course. Monotherapy should be initially started; however, 45% of the patients with neuropathic pain are on two or more medications for their pain.
This should be explained to the patient early during the treatment course. Monotherapy should be initially started; however, 45% of the patients with neuropathic pain are on two or more medications for their pain.
Complications
Complications of hyperesthesia include increased morbidity if symptoms are not controlled. The patient may also experience increased morbidity from extensive interventional procedures. Also, if the patient is started on potent opioids for treatment, the patient may become addicted.
Consultations
Consultations with the following may be required:
Pain medicine specialist
Sleep medicine professionals
Physical therapy
Occupational therapy
Psychiatrist
Psychologist
Neurologist
Neurosurgeon
Deterrence and Patient Education
Here are important points to take note of:
Managing the patient's expectations is crucial in the treatment plan.
 Hyperesthesia and other neuropathic pain symptoms are difficult to control, and complete resolution will most likely never be achieved. It is essential to discuss this with the patient early on during the treatment course.
Hyperesthesia and other neuropathic pain symptoms are difficult to control, and complete resolution will most likely never be achieved. It is essential to discuss this with the patient early on during the treatment course.Hyperesthesia and other neuropathic pain symptoms are best managed with an interdisciplinary team. This provides the best possible pain control and has the best outcomes.
Treatment should proceed in a stepwise manner.
Interventional procedures should be offered to patients who are not adequately managed with pharmacotherapy or wish to wean off high-risk medications such as opioids.
It is vital to manage comorbid conditions, such as mood disorders and sleeping difficulties.
The current treatment plan and possible treatments should be discussed with the patient regularly.
Enhancing Healthcare Team Outcomes
Early identification of hyperesthesia and other neuropathic pain symptoms is essential to start the patient on a proper treatment plan. The education of the patient early on during the treatment is necessary to establish realistic pain goals. Always treat with a multidisciplinary team approach. While the general practitioner is almost always involved in the care of patients with hyperesthesia, it is essential to consult with an interprofessional team of specialists that include pain medicine specialists, sleep medicine professionals, physical therapy, and occupational therapy. A psychiatrist and psychologist evaluations are recommended as many patients suffer from mood disorders.
The education of the patient early on during the treatment is necessary to establish realistic pain goals. Always treat with a multidisciplinary team approach. While the general practitioner is almost always involved in the care of patients with hyperesthesia, it is essential to consult with an interprofessional team of specialists that include pain medicine specialists, sleep medicine professionals, physical therapy, and occupational therapy. A psychiatrist and psychologist evaluations are recommended as many patients suffer from mood disorders.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Gilron I, Baron R, Jensen T. Neuropathic pain: principles of diagnosis and treatment. Mayo Clin Proc. 2015 Apr;90(4):532-45. [PubMed: 25841257]
- 2.
Bouhassira D, Lantéri-Minet M, Attal N, Laurent B, Touboul C. Prevalence of chronic pain with neuropathic characteristics in the general population.
 Pain. 2008 Jun;136(3):380-387. [PubMed: 17888574]
Pain. 2008 Jun;136(3):380-387. [PubMed: 17888574]- 3.
Torrance N, Smith BH, Bennett MI, Lee AJ. The epidemiology of chronic pain of predominantly neuropathic origin. Results from a general population survey. J Pain. 2006 Apr;7(4):281-9. [PubMed: 16618472]
- 4.
Gilron I, Watson CP, Cahill CM, Moulin DE. Neuropathic pain: a practical guide for the clinician. CMAJ. 2006 Aug 01;175(3):265-75. [PMC free article: PMC1513412] [PubMed: 16880448]
- 5.
Brizzi KT, Lyons JL. Peripheral nervous system manifestations of infectious diseases. Neurohospitalist. 2014 Oct;4(4):230-40. [PMC free article: PMC4212417] [PubMed: 25360209]
- 6.
Vilholm OJ, Christensen AA, Zedan AH, Itani M. Drug-induced peripheral neuropathy. Basic Clin Pharmacol Toxicol. 2014 Aug;115(2):185-92. [PubMed: 24786912]
- 7.
Watson JC, Dyck PJ. Peripheral Neuropathy: A Practical Approach to Diagnosis and Symptom Management. Mayo Clin Proc.
2015 Jul;90(7):940-51. [PubMed: 26141332]
- 8.
Azhary H, Farooq MU, Bhanushali M, Majid A, Kassab MY. Peripheral neuropathy: differential diagnosis and management. Am Fam Physician. 2010 Apr 01;81(7):887-92. [PubMed: 20353146]
- 9.
Zilliox LA. Neuropathic Pain. Continuum (Minneap Minn). 2017 Apr;23(2, Selected Topics in Outpatient Neurology):512-532. [PubMed: 28375916]
- 10.
Baron R, Tölle TR, Gockel U, Brosz M, Freynhagen R. A cross-sectional cohort survey in 2100 patients with painful diabetic neuropathy and postherpetic neuralgia: Differences in demographic data and sensory symptoms. Pain. 2009 Nov;146(1-2):34-40. [PubMed: 19592166]
- 11.
Johnson RW, Wasner G, Saddier P, Baron R. Herpes zoster and postherpetic neuralgia: optimizing management in the elderly patient. Drugs Aging. 2008;25(12):991-1006. [PubMed: 19021299]
- 12.
Gierthmühlen J, Baron R. Neuropathic Pain. Semin Neurol.
 2016 Oct;36(5):462-468. [PubMed: 27704502]
2016 Oct;36(5):462-468. [PubMed: 27704502]- 13.
von Hehn CA, Baron R, Woolf CJ. Deconstructing the neuropathic pain phenotype to reveal neural mechanisms. Neuron. 2012 Feb 23;73(4):638-52. [PMC free article: PMC3319438] [PubMed: 22365541]
- 14.
Jensen TS, Finnerup NB. Allodynia and hyperalgesia in neuropathic pain: clinical manifestations and mechanisms. Lancet Neurol. 2014 Sep;13(9):924-35. [PubMed: 25142459]
- 15.
Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, Gilron I, Haanpää M, Hansson P, Jensen TS, Kamerman PR, Lund K, Moore A, Raja SN, Rice AS, Rowbotham M, Sena E, Siddall P, Smith BH, Wallace M. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015 Feb;14(2):162-73. [PMC free article: PMC4493167] [PubMed: 25575710]
- 16.
Siddall PJ, Cousins MJ, Otte A, Griesing T, Chambers R, Murphy TK. Pregabalin in central neuropathic pain associated with spinal cord injury: a placebo-controlled trial.
 Neurology. 2006 Nov 28;67(10):1792-800. [PubMed: 17130411]
Neurology. 2006 Nov 28;67(10):1792-800. [PubMed: 17130411]- 17.
Cardenas DD, Nieshoff EC, Suda K, Goto S, Sanin L, Kaneko T, Sporn J, Parsons B, Soulsby M, Yang R, Whalen E, Scavone JM, Suzuki MM, Knapp LE. A randomized trial of pregabalin in patients with neuropathic pain due to spinal cord injury. Neurology. 2013 Feb 05;80(6):533-9. [PMC free article: PMC3589291] [PubMed: 23345639]
- 18.
Bates D, Schultheis BC, Hanes MC, Jolly SM, Chakravarthy KV, Deer TR, Levy RM, Hunter CW. A Comprehensive Algorithm for Management of Neuropathic Pain. Pain Med. 2019 Jun 01;20(Suppl 1):S2-S12. [PMC free article: PMC6544553] [PubMed: 31152178]
- 19.
Chou R, Loeser JD, Owens DK, Rosenquist RW, Atlas SJ, Baisden J, Carragee EJ, Grabois M, Murphy DR, Resnick DK, Stanos SP, Shaffer WO, Wall EM., American Pain Society Low Back Pain Guideline Panel. Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain: an evidence-based clinical practice guideline from the American Pain Society.
Spine (Phila Pa 1976). 2009 May 01;34(10):1066-77. [PubMed: 19363457]
- 20.
Manchikanti L, Abdi S, Atluri S, Benyamin RM, Boswell MV, Buenaventura RM, Bryce DA, Burks PA, Caraway DL, Calodney AK, Cash KA, Christo PJ, Cohen SP, Colson J, Conn A, Cordner H, Coubarous S, Datta S, Deer TR, Diwan S, Falco FJ, Fellows B, Geffert S, Grider JS, Gupta S, Hameed H, Hameed M, Hansen H, Helm S, Janata JW, Justiz R, Kaye AD, Lee M, Manchikanti KN, McManus CD, Onyewu O, Parr AT, Patel VB, Racz GB, Sehgal N, Sharma ML, Simopoulos TT, Singh V, Smith HS, Snook LT, Swicegood JR, Vallejo R, Ward SP, Wargo BW, Zhu J, Hirsch JA. An update of comprehensive evidence-based guidelines for interventional techniques in chronic spinal pain. Part II: guidance and recommendations. Pain Physician. 2013 Apr;16(2 Suppl):S49-283. [PubMed: 23615883]
- 21.
Dworkin RH, O'Connor AB, Kent J, Mackey SC, Raja SN, Stacey BR, Levy RM, Backonja M, Baron R, Harke H, Loeser JD, Treede RD, Turk DC, Wells CD.
Interventional management of neuropathic pain: NeuPSIG recommendations. Pain. 2013 Nov;154(11):2249-2261. [PMC free article: PMC4484720] [PubMed: 23748119]
- 22.
Cruccu G, Aziz TZ, Garcia-Larrea L, Hansson P, Jensen TS, Lefaucheur JP, Simpson BA, Taylor RS. EFNS guidelines on neurostimulation therapy for neuropathic pain. Eur J Neurol. 2007 Sep;14(9):952-70. [PubMed: 17718686]
Hypersensitivity of hard tissues of teeth (hyperesthesia)
Hypersensitivity of hard tissues of teeth (hyperesthesia)
the same condition, which is characterized by the sudden onset of acute, transient pain, a feeling of soreness under the influence of temperature, chemical and mechanical stimuli (provided that this pain cannot be explained by other dental diseases, for example, complications of caries - pulpitis, periodontitis).
Patients often turn to the dentist with complaints of pain that occurs after eating sour, sweet or salty foods, carbonated drinks, pain with a sharp temperature change (intake of cold and hot food and liquids), pain when brushing teeth and using hard food.
Up to 50-60% of the adult population of different countries suffer from this pathology, and it is more pronounced at the age of 30-60 years. Women suffer more than men. Most often, hypersensitivity is observed in diseases of non-carious origin (abrasion, pathological abrasion, erosion, less often with wedge-shaped defects), in which there is a significant decrease in enamel and dentin is exposed. With carious defects, as well as with initial caries, especially when it is localized in the cervical region, pain may occur, which is associated with demineralization of the enamel under the action of acids and an increase in its permeability. Hyperesthesia can also occur after the treatment of carious lesions if the filling technique and enamel etching are not followed. Hyperesthesia is noted with traumatic injuries of hard tissues of the teeth: a split, a chip, a crack, a break of the tooth crown. Enamel hypersensitivity, as a complication, can be considered after teeth whitening. This kind of pain can also occur in connection with some pathological conditions of the body (the so-called systemic or functional hyperesthesia): psychoneuroses, endocrinopathies, diseases of the gastrointestinal tract, metabolic disorders, age-related hormonal changes and disorders, infectious and other concomitant diseases.
First, let's clarify that tooth enamel is an insensitive tissue. The dentin of the tooth has sensitivity, and to be more precise, the nerve structures located in the dentinal tubules react to stimuli. At the same time, the state of the enamel, changes in its physical and chemical properties (enamel loss, increase in its permeability, damage) can contribute to the emergence of sensitivity. Normally, the dentin is tightly covered by enamel, and the cement of the tooth by the gum. This protects the dentin from environmental irritants. Enamel in the cervical area is less mineralized and has a thinner thickness, so hypersensitivity is most common in these areas. The most common and strong irritant for such teeth is cold. There is a less pronounced reaction to elevated temperature.
The most common and strong irritant for such teeth is cold. There is a less pronounced reaction to elevated temperature.
Patients with sensitive teeth have problems taking care of their teeth because brushing can cause pain. This leads to a deterioration in the hygienic state of the oral cavity, excessive deposition of plaque, which in turn can cause the occurrence of multiple carious lesions, inflammation of periodontal tissues. Further, pathological changes in the periodontium lead to inflammation of the gums, resulting in increased hypersensitivity. Thus, there is a vicious circle.
More complex is the mechanism of the appearance of pain sensitivity in intact enamel, which is most often observed in general concomitant pathology of the body. In all likelihood, in some cases, there are still microcracks in the enamel, through which irritants can penetrate deep into. Not the last role in this process is played by the threshold of human pain sensitivity. If the threshold of pain sensitivity is lowered, then sensitivity to physical, chemical and mechanical stimuli increases. In this case, even those whose enamel and dentin do not have visible damage can feel pain.
If the threshold of pain sensitivity is lowered, then sensitivity to physical, chemical and mechanical stimuli increases. In this case, even those whose enamel and dentin do not have visible damage can feel pain.
Treatment of hyperesthesia
For this purpose, preparations are used that rebuild and compact the structure of dentin, form compounds that clog the dentinal tubules, as well as agents that bind to proteins of the hard tissues of the tooth and precipitate in the tubules. In this regard, the use of calcium, fluorine, strontium, citrate preparations is relevant. A sufficiently large number of methods and means have been proposed: fluoride-containing varnishes and gels, fluoride-containing toothpastes, the “deep fluoridation” method, etc. The effect of fluorides is more associated with a physical blockade of the dentinal tubules.
Another way to reduce sensitivity is to reduce the excitability of the nerve endings themselves in the dentinal tubules, and for this purpose potassium salts (nitrate, chloride) are effectively used. Means that help patients control tooth sensitivity throughout almost their entire lives are special toothpastes. The use of these pastes is mainly long-term, the indication for continued use of the paste is the patient's subjective sensations. Periodically it is recommended to replace the paste. It should be noted that desensitizing toothpastes are classified as low abrasive (dentine abrasion index - RDA is 30-50) or they can be gel. The mechanism for reducing the sensitivity of hard tissues of the teeth is carried out due to the ingredients included in the toothpaste. The most common and effective pastes on the Russian market are: Sensodine, Sensodine F, Oral-B, Elgifluor, President, Parodontol, Pardontol Sensitive, New Zhemchug with calcium glycerophosphate and others. Brushes for sensitive teeth should be soft or very soft depending on the severity of hypersensitivity manifestations, the tips of the bristles are rounded. The trimming shape of the brush field is preferably even. In the arsenal of products for the care of sensitive teeth, it is advisable to use rinses for sensitive teeth, for example, "Sensodine", containing sodium fluoride and potassium chloride, "Oral-B", containing active ingredients: sodium fluoride and potassium nitrate.
Means that help patients control tooth sensitivity throughout almost their entire lives are special toothpastes. The use of these pastes is mainly long-term, the indication for continued use of the paste is the patient's subjective sensations. Periodically it is recommended to replace the paste. It should be noted that desensitizing toothpastes are classified as low abrasive (dentine abrasion index - RDA is 30-50) or they can be gel. The mechanism for reducing the sensitivity of hard tissues of the teeth is carried out due to the ingredients included in the toothpaste. The most common and effective pastes on the Russian market are: Sensodine, Sensodine F, Oral-B, Elgifluor, President, Parodontol, Pardontol Sensitive, New Zhemchug with calcium glycerophosphate and others. Brushes for sensitive teeth should be soft or very soft depending on the severity of hypersensitivity manifestations, the tips of the bristles are rounded. The trimming shape of the brush field is preferably even. In the arsenal of products for the care of sensitive teeth, it is advisable to use rinses for sensitive teeth, for example, "Sensodine", containing sodium fluoride and potassium chloride, "Oral-B", containing active ingredients: sodium fluoride and potassium nitrate. For prevention, patients should maintain good oral hygiene, follow the correct brushing technique, use a small amount of toothpaste, brush their teeth without excessive effort and for no more than the recommended time, do not use brushes with hard bristles, use brushes with rounded ends of the bristles, immediately after when taking acidified foods and carbonated drinks, rinse your mouth with water, avoid improper use of dental floss and other means for cleaning the contact surfaces of the teeth, do not damage the gums when using brushes.
For prevention, patients should maintain good oral hygiene, follow the correct brushing technique, use a small amount of toothpaste, brush their teeth without excessive effort and for no more than the recommended time, do not use brushes with hard bristles, use brushes with rounded ends of the bristles, immediately after when taking acidified foods and carbonated drinks, rinse your mouth with water, avoid improper use of dental floss and other means for cleaning the contact surfaces of the teeth, do not damage the gums when using brushes.
Prepared by: dentist Krysalnaya N.N.
http://www.krasotaimedicina.ru/diseases/zabolevanija_stomatology/teeth_hyperesthesia
https://studfiles.net/preview/468586/
Sections:
What to do if you are too sensitive. And this is noticeable
Increased emotionality is no longer a sign of weakness - it is a feature of the psyche. The existence of highly sensitive people has been scientifically proven. In a world where more and more people cannot cope with stress, American psychologists are closely studying those who are especially prone to worry about any reason. "Lifestyle" offers to join them.
"Lifestyle" offers to join them.
If you can't stand bright lights and turmoil around you, you can't watch horror movies, and after watching the news about an earthquake or a military conflict, you start crying out of pity for the victims, you are a highly sensitive person. According to the author of the term Elaine N. Aron, there are about 20% of people like you in the world. This means that it's time to stop hiding your feelings and no longer be ashamed of crying in the movies.
In today's Western world, it's a shame to be a weakling — and that's why we have to hide our feelings, constantly keep in good shape, pretend that we can live without lunch and sleep and work 12 hours a day, otherwise our colleagues will look askance at us , and the authorities - to make jokes about us.
In our country, it is not customary to be capricious, and that is why we are forced to agree to the conditions that we have, to work in a basement or open space, under the wind of an air conditioner, under the harsh light of fluorescent lamps and under the cries of colleagues from neighboring departments.
close
100%
Are we suffering from all this? Yes, we suffer. In general, we suffer from a lot of things: we can’t stand the feeling of hunger, we can’t watch films about the war, we don’t wear woolen clothes because they prick, we tear off the tags from T-shirts because they get in the way. We cannot work when it is cold, hungry or noisy, we react sharply to criticism and take any comments personally, we catch changes in the mood of others. It remains to say who we are.
We are highly sensitive people. Do not rush to laugh and call us sissies - and not only because it is very offensive to us.
Perhaps you, too, are one fifth of the world's population, which is characterized by a particularly sensitive processing of sensory information. Then you are one of us.
Perhaps you, too, were forbidden to watch the news program as a child, because they show war and starving children in Africa? Maybe you were dying of shame when a geographer slapped you a deuce once in your life? Maybe they hated running and, in general, any form of competition, when everyone is looking at you, and you run no more than a three? Maybe at school it was a real torment for you to raise your hand in class, even if you knew exactly the right answer? Maybe. Or maybe you have other examples from your childhood that will help you to say that you were a highly sensitive child and probably grew up to be a highly sensitive adult as well.
Or maybe you have other examples from your childhood that will help you to say that you were a highly sensitive child and probably grew up to be a highly sensitive adult as well.
The term "highly sensitive person" was first used in its current sense by Dr. Elaine Aron, a scientist and author of The Highly Sensitive Person, published in the United States in 1997. The hypothesis that high sensitivity to external stimuli is a feature inherent in about 20% of the inhabitants of the Earth was put forward by a psychologist twenty years ago.
However, the real interest in this idea has awakened among the public only now, when it became clear that more and more people can not cope with stress.
And I woke up just in time: for twenty years, Dr. Aron and her colleagues have conducted many studies that helped to understand what processes occur in the brain of a highly sensitive person, and to conclude that this feature is innate: certain parts of the brain of such a person react to external stimuli sharper than other, less sensitive people.
And not only negative ones, but also positive ones too. Yes, highly sensitive people feel acute discomfort in awkward situations. But brighter experience the pleasure of contemplating objects of art and views of nature, listening to music, communicating with pleasant people.
How to know that you are a highly sensitive person
close
100%
1. You have deep feelings
One of the main characteristics of highly sensitive people is the ability to deeply feel what is happening around. They have developed intuition, which allows them to be more perceptive than their less sensitive comrades.
2. You react more emotionally than others
Highly sensitive people experience more intense emotions and are often infected by the emotions of others. These are not necessarily close people, they can easily pick up a bad mood from a friend or take care of a colleague's problems. This makes them hate delivering bad news or making unpopular decisions – they worry about how others will react to it.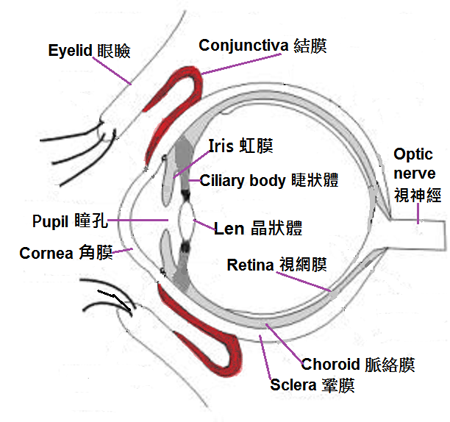
3. You are often told: “Don't take it personally.”
Sensitive people are treated differently in different cultures: if in the West emotionality is a manifestation of weakness, then in the East everything is not so simple.
Dr. Ted Zeff, author of The Highly Sensitive Person's Survival Guide, states based on his research that in India and Thailand sensitive men are very rarely teased, while in North In America, men with a fine mental organization are often the objects of ridicule.
4. You prefer to exercise alone
Highly sensitive people hate team sports, according to Dr. Zeff. And our experience confirms this: such people like cycling, swimming or walking, but playing football or basketball causes them to panic.
However, there are exceptions: if such a person is lucky with smart and understanding parents, he may not be afraid to prove himself in a team.
5. You find it difficult to make elementary decisions
Highly sensitive people are attentive to the details of the situation and the subtleties of circumstances. From this, they try to take everything into account and fall into a stupor, because there is too much of this.
From this, they try to take everything into account and fall into a stupor, because there is too much of this.
Even the task of choosing an ice cream can confuse them. However, there is good news: having once understood how to behave in a certain situation, in similar conditions in the future, such a person, without getting lost, will immediately do the right thing.
6. You get upset when you make a mistake
Mistakes upset everyone, but highly sensitive people - especially: because of annoying little things and oversights that others have forgotten to even think about, they can suffer for weeks, imagining that they still remember the mistake.
7. You are an introvert
But there are exceptions: according to Dr. Aron, 30% of highly sensitive individuals are extroverts. This happens when a person grows up in a closed environment where everything is in plain sight, in a village, a small town, a religious community or a family of a public person.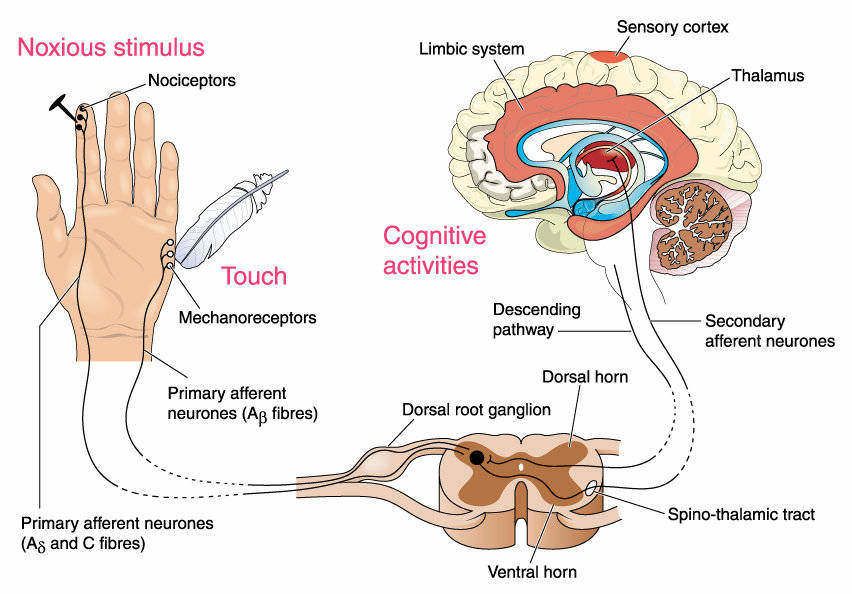
8. You know how to work in a team
Paradoxically, but true: the depth of experience makes highly sensitive people excellent employees. Only they should not take positions in which they must make final decisions: for example, if it is a doctor, he should have the opportunity to consult with colleagues before prescribing treatment.
9. You are prone to anxiety and depression
This only happens if you have suffered a lot of adversity in the past - but who among us is lucky to do without them at all? Shy people are often teased in childhood: if a highly sensitive person was not given proper support in childhood, he grows up with the feeling that the world is hostile, and only doctors and antidepressants can help here.
It is worth taking a closer look at your child: high sensitivity is often inherited.
10. You can't stand sharp sounds
Someone can't stand it when Styrofoam squeaks on glass. Someone - the sound of a perforator or drill.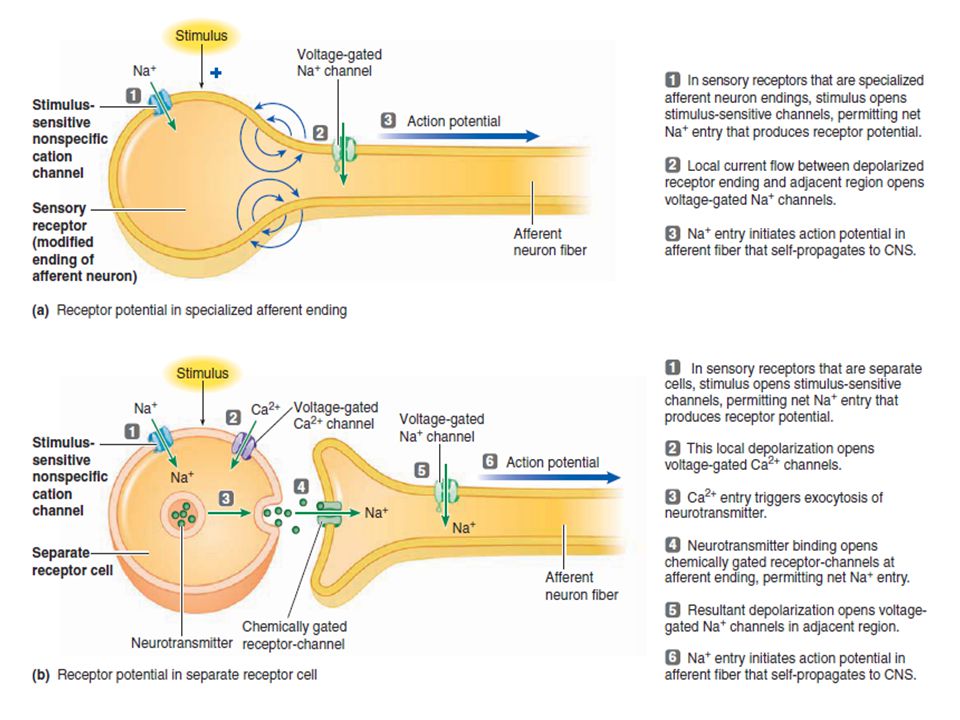 It annoys someone when others eat loudly: champing and smacking is really impossible to endure, why do people even allow themselves to eat with their mouths open ?!
It annoys someone when others eat loudly: champing and smacking is really impossible to endure, why do people even allow themselves to eat with their mouths open ?!
11. You can't see the violence on the screen
A highly sensitive person cannot watch horror films about dismemberment, disaster films about drowning dogs, and arthouse about rape. Lars von Trier, Gaspar Noe and Michael Haneke are cinematic enemies.
Salo by Pier Paolo Pasolini? Look in your VGIK, and it’s enough for us to read the plot.
But you can watch Game of Thrones by closing your eyes in certain places, because the costumes are beautiful.
12. You can cry from scratch
When such a person is offended to tears for some reason, he is really capable of bursting into tears. And, by the way, it costs him a lot of effort not to do this. A sad film (without violence), a touching commercial for a charity campaign, a story about a penguin who annually comes to the Brazilian (or Chilean?) who saved him - in general, anything can cause a surge of feelings.
13. You are very polite
Good manners are a hallmark of highly sensitive people: it is important for them not to hurt the feelings of others. They try not to inconvenience others: they regularly give up their seats on public transport, carefully place their carts in the supermarket, let people go ahead, and endlessly apologize and thank you. So sometimes it's even annoying.
14. You are sensitive to criticism
Highly sensitive people literally cannot stand criticism, taking it to heart. When their team is criticized, they take everything personally.
Because of this, they often use ridiculous defense mechanisms: they try to please everyone in advance, they criticize themselves, they avoid everything that can be a source of criticism.
Dr. Aron claims that self-defense such people use the following methods, which may seem strange to most: minimizing contact, blaming, trying to achieve too high a result, resentment, projecting, refusal to compete.
15. You can’t work in an open office
Open space is a nightmare for any office employee: noise, bright light that not everyone can stand, constant flickering, talking on the phone, arguments and extraneous smells - all this makes you a highly sensitive person's head is spinning, but it does not work out in any way. He is generally incapable of working under pressure: maybe someone needs a good kick to start working, but not for him.
close
100%
10 Rules for a Highly Sensitive Person
1. Remember that you are not alone and that what happens to you is normal.
2. Avoid people you don't like.
3. Avoid situations that make you tired.
4. Don't overload your schedule or you might fall off at the most inopportune moment.
5. Set healthy boundaries with people who use your capacity for empathy.
6. Keep a journal to help you clear your head and learn how to make decisions.
7. Enjoy good music, art, and people who support you.