Depression gut health
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid.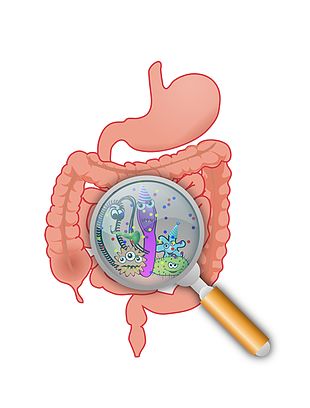 If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.
-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly.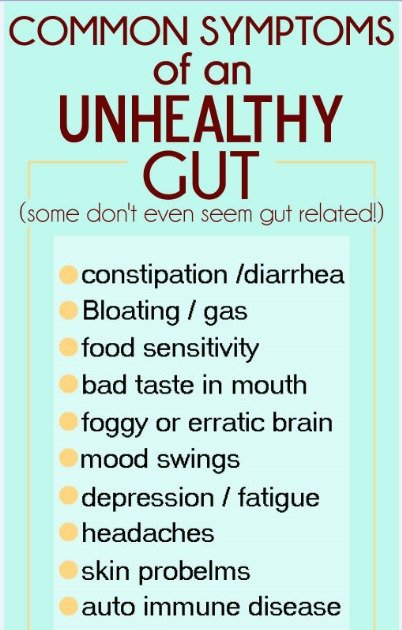 Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
How does the microbiota fight stress and depression?
Learn how gut bacteria, stress, depression and anxiety are linked, and what foods help improve mental health.
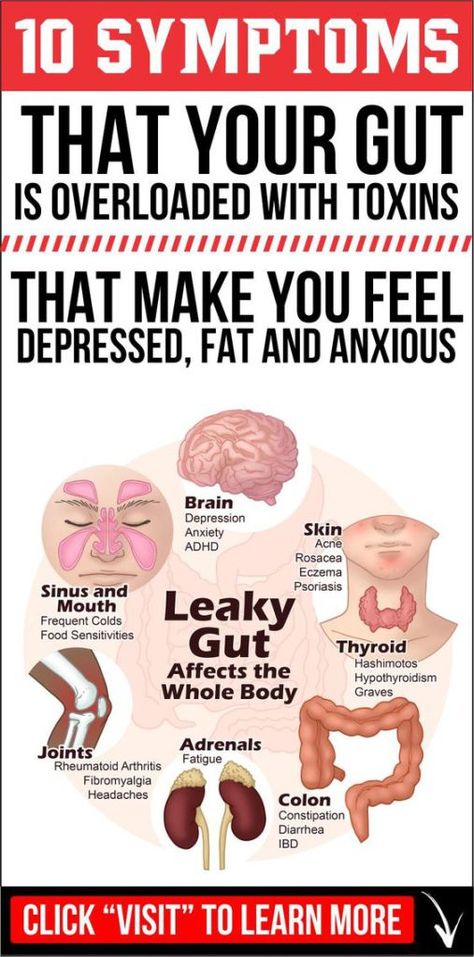
No one will be surprised that dysbacteriosis or imbalance of the microbiota affects mood: it is difficult to be cheerful and cheerful, experiencing digestive problems and discomfort. But scientists have shown that in addition to mood, the activity of intestinal bacteria affects the level of anxiety and susceptibility to stress. A balanced microflora helps the psyche to cope with this.![]()
Contents
- 1. Gut-brain connection
- 2. Stress, microbiota and depression
- 3. Depression and Anxiety Diet
- 4. Note
Gut-brain connection
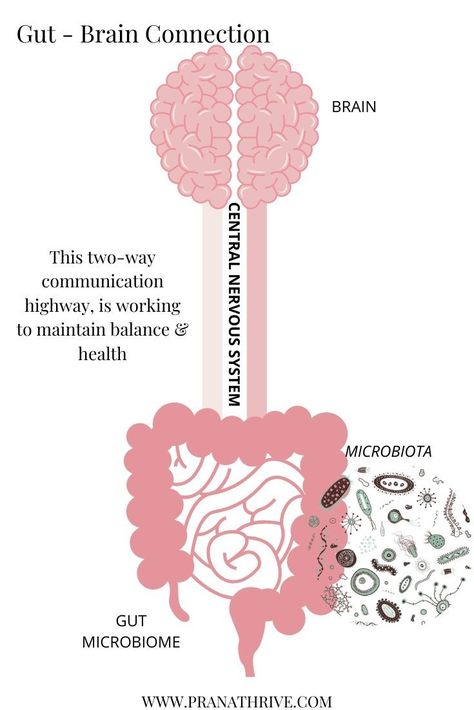
The vagus nerve, the main element of the autonomic nervous system, which regulates the functioning of internal organs, connects the intestine to the brain. Thanks to this system, we breathe, swallow and digest food without thinking. The vagus nerve helps move food through the gastrointestinal tract, stimulates the production of digestive enzymes, and lets us know how full we are. And this nerve also helps the brain monitor whether everything is in order with the intestines.
In addition to communicating via the vagus nerve, the microbiota can influence the brain through the bloodstream. For example, fatty acids produced by gut bacteria stimulate the production of serotonin. It is a neurotransmitter that keeps you in a good mood.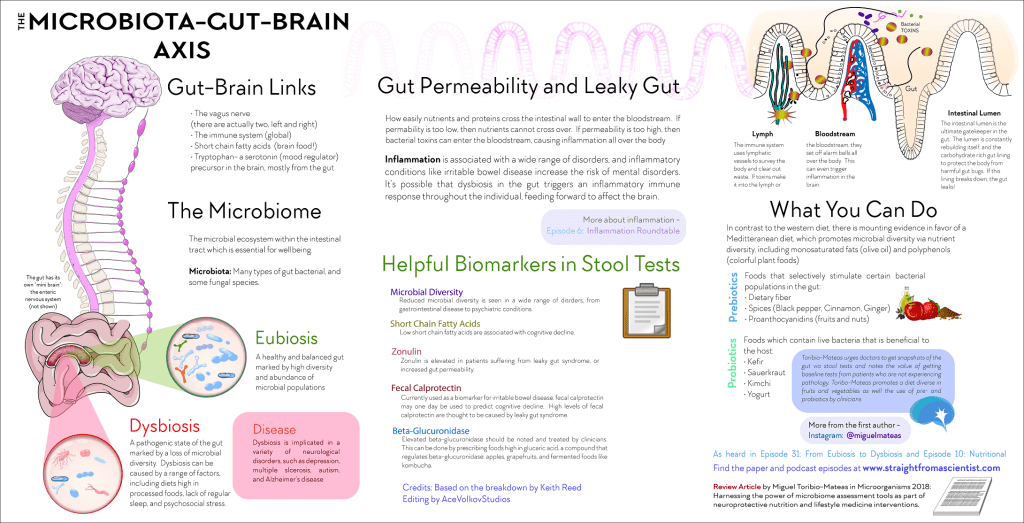 And some probiotic bacteria produce their own stress-relieving neurotransmitter gamma-aminoacetic acid (GABA).
And some probiotic bacteria produce their own stress-relieving neurotransmitter gamma-aminoacetic acid (GABA).
Stress, microbiota and depression
Stress causes the release of the hormone cortisol and increases intestinal permeability. Because of this, endotoxins, which are formed during the breakdown of bacteria, can enter the bloodstream and trigger an immune response. Inflammation begins, and the nervous system reacts to it, including a change in mood. This can lead to symptoms of depression and anxiety.
Scientists have found that persistent inflammation often accompanies depression and anxiety, and taking anti-inflammatory drugs relieves these symptoms.
In addition, the mental state affects the composition of the microbiota and can cause dysbacteriosis. For example, studies show that patients with depression become significantly more bacteria from the genera Bacteroidetes , Protobacteria and Actinobacteria , but members of the genus Faecalibacterium , on the contrary, they have little, and the less, the more serious the symptoms.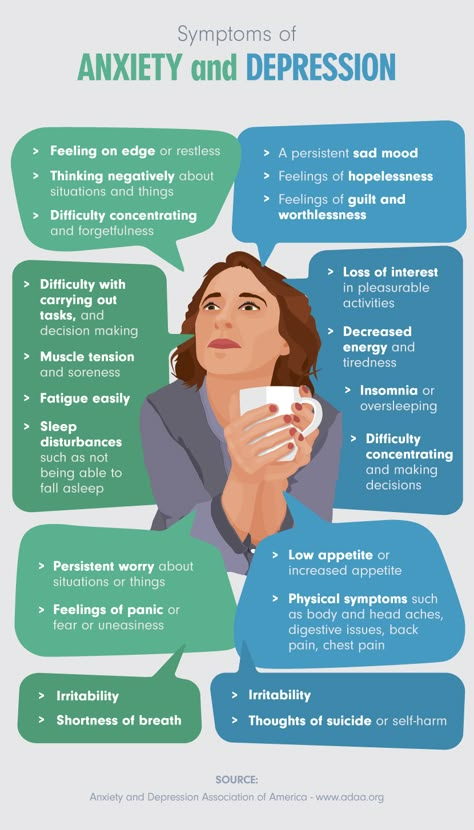
Dysbacteriosis, in turn, weakens the protective function of the intestinal mucosa and provokes inflammation. And this only exacerbates the mental state.
Diet against depression and anxiety
You can restore the balance of the microbiota and restore a good mood if you adjust the diet. Pro- and prebiotics help restore the ratio of bacterial species and reduce the permeability of the intestinal mucosa. Studies show that such foods improve the body's response to stress and reduce inflammation, and anxiety levels and symptoms of depression decrease along with it.
Eat more plant-based foods
Good gut bacteria love natural, plant-based foods that are high in fiber. When you eat prebiotics: fruits and vegetables, nuts, whole grains, or legumes, bacteria produce butyric acid. It is an essential short chain fatty acid that supports intestinal health. It helps prevent inflammation, which means avoiding digestive problems and maintaining a good mood.
In dysbacteriosis, gut bacteria lack the beneficial nutrients to produce butyric acid and support immunity. But diet can restore a healthy balance. For example, if you eat more plant foods or prebiotics, the good bacteria can get enough nutrition. They contain fibers that serve as a source of essential fatty acids for bacteria.
But diet can restore a healthy balance. For example, if you eat more plant foods or prebiotics, the good bacteria can get enough nutrition. They contain fibers that serve as a source of essential fatty acids for bacteria.
List of foods rich in prebiotics:
| Prebiotic dietary fiber | Resistant starches | Polyphenols |
|---|---|---|
| Garlic | Legumes | Bow |
| Bow | Seeds | Apples |
| Berries | Cereals | Tea |
| Jerusalem artichoke | Chilled after cooking potatoes | Cocoa |
| Mushrooms | Green bananas | Red wine |
| Rye | Plantain (vegetable banana) | Red fruits |
| Barley | Corn | Soybeans |
Add probiotics to your diet
Probiotic bacteria have a beneficial effect on health, including mental health.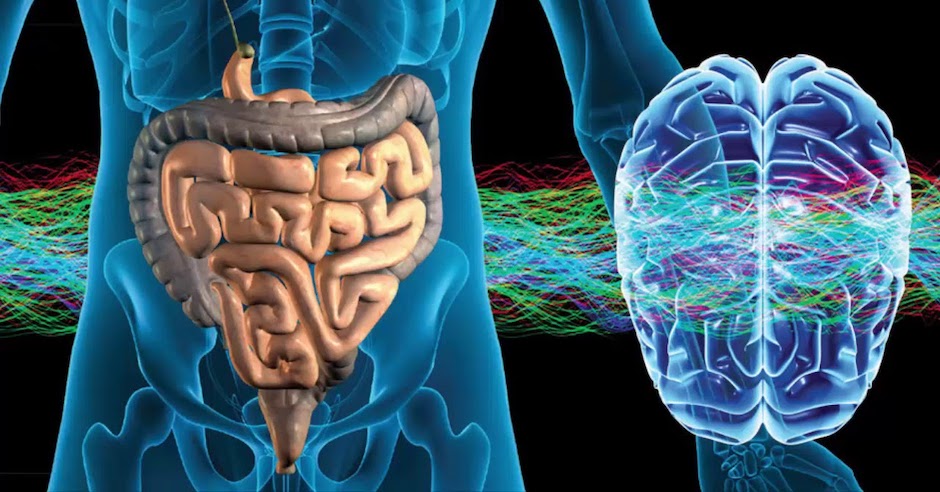 These include bifidobacteria, lactobacilli and lactococci. In the intestines, they are already there, but their share can be increased by supplements and fermented milk products.
These include bifidobacteria, lactobacilli and lactococci. In the intestines, they are already there, but their share can be increased by supplements and fermented milk products.
Probiotics maintain a healthy microbiota balance and prevent dysbiosis. Studies show that certain strains of lactobacilli increase resistance to stress and anxiety, and taking probiotics may improve symptoms of depression.
Sign up for a free email course from the Atlas team "How to be happy and productive despite stress." It talks about how to deal with stress scientifically and worry less about its consequences.
Note:
The intestines and the brain are closely interconnected and influence each other. Stress and dysbacteriosis worsen mood and affect the risk of anxiety and depression. And depression, at the same time, can upset the balance of the microbiota and lead to the development of inflammation.
A diet rich in pro- and prebiotics helps reduce inflammation, rebalance the microbiota, increase resilience to stress, and ease depression and anxiety.

With the Atlas Microbiota Test, you can find out if your bacteria are in balance and what to add to your diet to better cope with stress.
Other articles on the effects of stress on health in the blog:
- How Stress Affects Digestion
- 9 Ways to Reduce Cortisol and Prevent Stress
- Ansari, F et al. The Effects of Probiotics and Prebiotics on Mental Disorders: A Review on Depression, Anxiety, Alzheimer, and Autism Spectrum Disorders, 2020
- Benakis, C et al. The Microbiome-Gut-Brain Axis in Acute and Chronic Brain Diseases, 2020* Cheung, S, G et al. Systematic Review of Gut Microbiota and Major Depression, 2019* Liu, H et al. Butyrate: A Double-Edged Sword for Health? , 2018
- Liu, L and Zhu, G. Gut-Brain Axis and Mood Disorder, 2018
- Peirce, J, M and Alviña, K. The Role of Inflammation and the Gut Microbiome in Depression and Anxiety, 2018
- Stakenborg, N et al.
 The Versatile Role of the Vagus Nerve in the Gastrointestinal Tract, 2014
The Versatile Role of the Vagus Nerve in the Gastrointestinal Tract, 2014 - Winter, G et al. Gut Microbiome and Depression: What We Know and What We Need to Know, 2018
- de Punder, K., & Pruimboom, L. Stress induces endotoxemia and low-grade inflammation by increasing barrier permeability. 2015
- Müller, N. et al. The cyclooxygenase-2 inhibitor celecoxib has therapeutic effects in major depression: Results of a double-blind, randomized, placebo controlled, add-on pilot study to reboxetine.2006
Anastasia Komarova Biologist, editor, science communication specialist
Not in the head, but in the stomach: how to eat to avoid depression
- David Robson
- BBC Future
Image copyright Getty Images
One hundred years ago, several separate studies found a link between diet and mental health.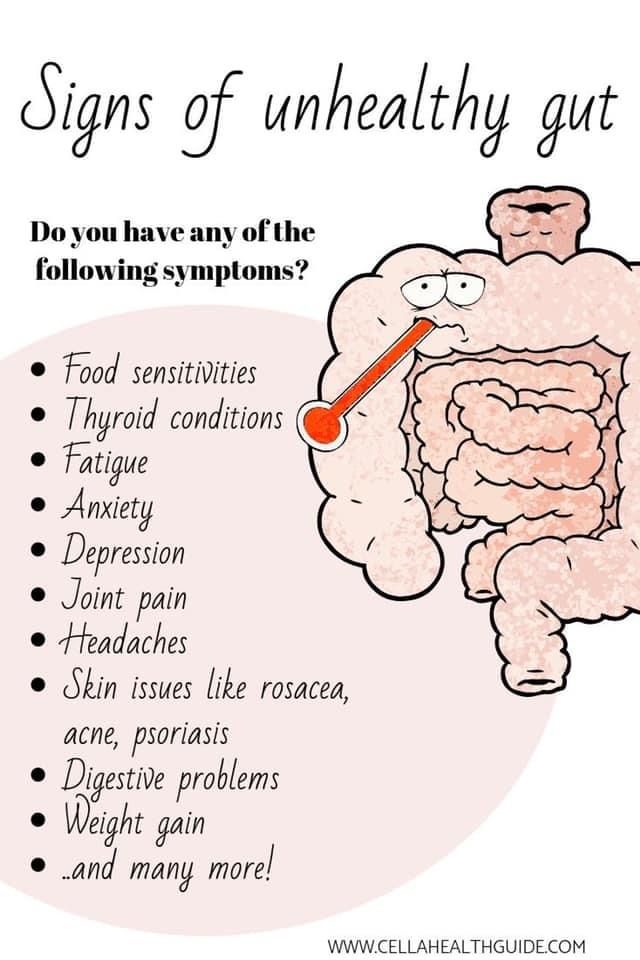 Scientists now confirm that the bacteria in our gut can affect brain function and mental health.
Scientists now confirm that the bacteria in our gut can affect brain function and mental health.
The patient's intestines do not seem to be the place to look for the causes of depression. But it was he who drew the attention of George Porter Phillips at the beginning of the 20th century.
While observing patients at the Bethlem Royal Hospital in London, Phillips noticed that depressed patients with melancholia often suffered from severe constipation, as well as other signs of a "general metabolic disorder" - brittle nails, dull hair, sallow complexion.
One might assume that these physiological problems are the result of depression, but Phillips thought of reverse causality. He wondered if it was possible to alleviate the mental state of the patient by solving problems with the intestines?
- Do probiotics help restore the intestinal microflora?
- How bacteria affect our mood
To find out, he put patients on a special diet.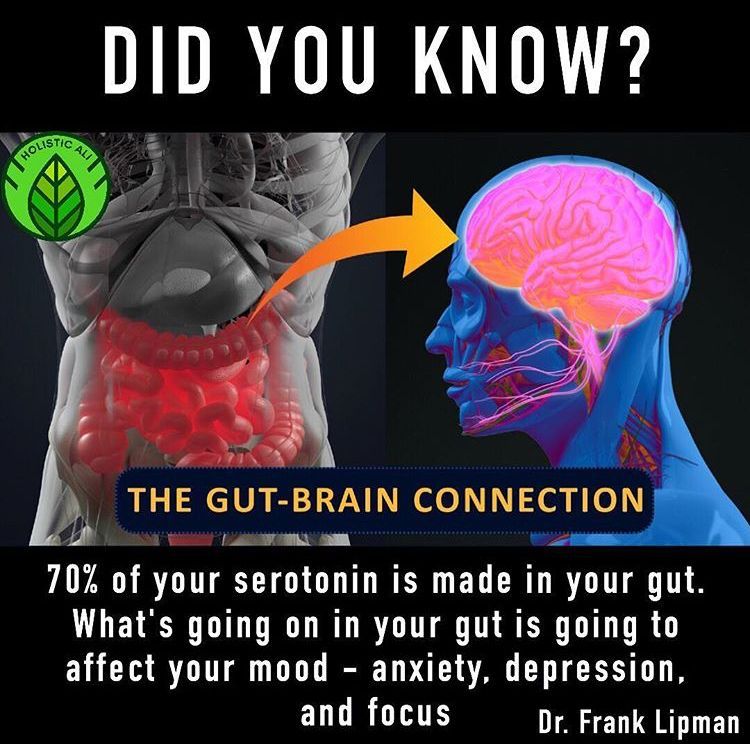 It contained no meat, only fish, as well as kefir, a fermented milk drink with lactobacilli known to improve digestion.
It contained no meat, only fish, as well as kefir, a fermented milk drink with lactobacilli known to improve digestion.
Surprisingly, it worked. Of the 18 patients that Phillips checked himself, 11 made a full recovery, while the other two showed marked improvement. This experiment is one of the first evidence that the bacteria in our gut can have a profound effect on our mental state.
There is a lot of talk about the microbiome and its role in human health today.
However, its connection with the psyche is more difficult to explain.
How can these microscopic scavengers that feed on the waste products of our digestion affect the brain?
"I'm in no way questioning the fact that microbes affect mental health," says Jane Allison Foster, laboratory director at McMaster University in Canada, whose research is leading the field.
And this means that we will be able to heal our brain through the intestines. "This area has great potential for the development of both new therapeutics and personalized medicine."
"This area has great potential for the development of both new therapeutics and personalized medicine."
However, Foster emphasizes that an unhealthy gut is only one of many possible causes of mental disorders. That is, only a fraction of patients will respond well to the new "psychobiotic" treatment.
But for those who suffer from an imbalance in the intestinal microflora, new methods can bring significant relief.
Photo credit, Unsplash
Photo caption,An early 20th century study found that kefir had a positive effect on patients with depression health was unpopular for almost the entire twentieth century.
Serious evidence for this idea began to appear only in the last two decades.
One of the most interesting modern experiments was carried out at the University of Kyushu in Japan in 2004.
- More than half your body is someone else's
A team of scientists have shown for the first time that "sterile" mice raised without contact with microbes showed fluctuations in the levels of corticosterone and ACTH, which are responsible for stress.
Scientists have suggested that the gut bacteria of healthy mice somehow affect the hormonal profile.
The researchers then seeded sterile mice with lactobacilli, which Phillips also used in his experiment.
Although the mice's stress response remained above normal, it was markedly reduced compared to animals that did not have the bacteria in their bodies.
There are also some indications that depressive behavior can be transmitted from species to species - from human to mouse - through microbes in the gut.
This was proved by Chinese researchers from the city of Chongqing, who transplanted part of the microbiota of patients with major depressive disorder into sterile mice.
Of course, these are only animal experiments, but their findings are supported by epidemiological studies involving a large number of people (the results of the latter were made public on February 4, 2019).
All of these studies systematically confirm that the intestinal microflora affects the human psyche, in particular, the development of depression and anxiety.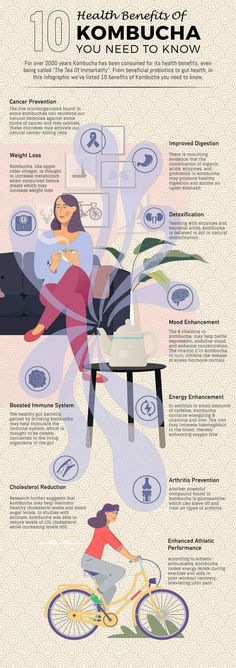
Image copyright, Getty Images
Image caption,Only two out of 10 patients get better with antidepressants
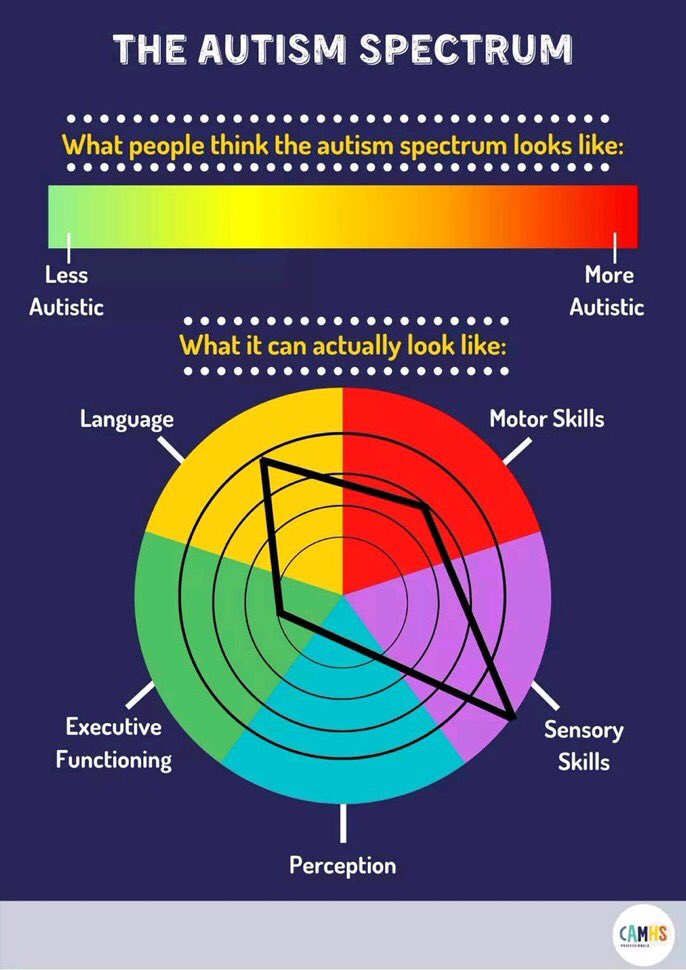
No single species of bacteria can cause this effect. The whole point, it seems, is the general ratio of different families of microbes.
The gut microbiome of depressed and anxious people is less diverse than that of people with good mental health.
Moreover, in a recent publication on the subject, researchers found an association between schizophrenia and low gut species diversity. When samples of the patients' bacteria were transplanted into sterile mice, their brains experienced shifts that are characteristic of this mental disorder.
Microbes and the brain
This connection can be formed in different ways.
Some types of bacteria protect the intestinal wall by strengthening the intestinal mucosa, which prevents contents from entering the bloodstream.
Without such a barrier, a person may suffer from the release of cytokines that cause inflammation. These proteins increase blood circulation around the source of infection and regulate the body's immune response.
This response is important in fighting infection, but cytokines also contribute to fatigue. That is why we often feel tired and depressed when we are sick. But such a state for a long time can lead to depression.
- What to eat for clarity of thought and good memory
Gut microflora influences how our body digests and metabolizes the precursors for the synthesis of important neurotransmitters such as serotonin and dopamine.
Gut bacteria directly influence the brain through the vagus nerve, which innervates the intestinal mucosa, which allows it to control the process of digestion.
In this way, gut microbes can send signals that affect brain activity through the vagus nerve.
"Gut bacteria can communicate in different ways with different structures in the body, including the nervous system," says Foster. "It's a very dynamic, interactive, complex space."
But this is not a one-way street, so brain activity can also affect the composition of the gut microflora. Stress increases the risk of inflammatory reactions that affect the intestinal microflora.
It's kind of a vicious circle.
New treatments
As Foster points out, the industry is growing rapidly, with both university scientists and commercial companies conducting research.
Their goal is to find new treatments for depression.
Antidepressants change the balance of brain chemicals, such as serotonin levels, but they don't work for everyone. In fact, only two out of 10 patients get better with antidepressants.
Cognitive-behavioral therapy has a good effect, but it also does not help everyone.
As a result, many people never receive effective treatment. Therefore, the connection between the brain and gut bacteria may become one of the most promising areas of research.
Image copyright, Getty Images
Image caption,When sterile mice were fed beneficial lactobacilli, they were much more stress-tolerant. In some studies, changing the diet or adding probiotics to it reduced symptoms of depression, while in other studies, such measures had an effect that was no different from the placebo effect.
Foster explains the negative result by saying that the experiments were carried out on patients whose depression had other causes. Gut bacteria can undoubtedly affect the mental state of some people, but in many cases the trigger may be completely different. Kefir is unlikely to help such patients.
To further complicate matters, each individual's microbiome is unique, so any therapy targeting the gut flora must account for these differences.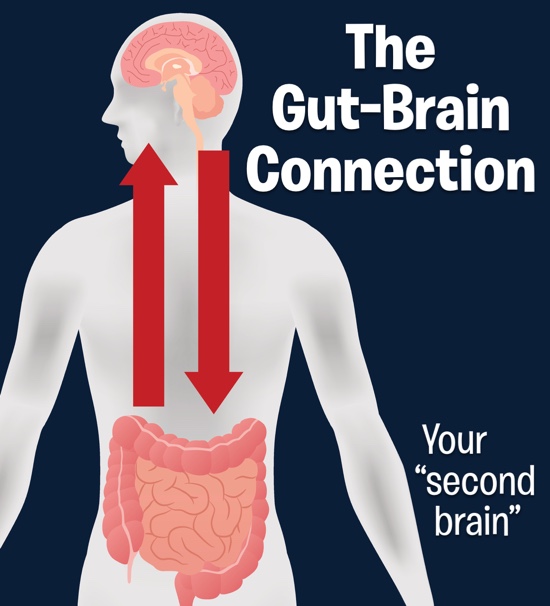
- The 100 most nutritious foods in the world. Fat is in the top ten
- How hormones, immunity, microbes and pulse affect our character
Therefore, the method of treatment must be complex and individual, the researcher believes.
"The theory of the connection between the intestines and the brain is primarily applicable in precision medicine (which takes into account the individual characteristics of the organism, and not general principles for all)."
The challenge, according to Foster, is "to identify a biotype or group of individuals with a similar microbiome that may be causing their symptoms." Before starting treatment, check, for example, the patient's tendency to inflammatory processes.
Since, unlike antidepressants, it is not about interfering with the brain, the possible side effects of such therapy will be less dangerous.
Eat like Italians
The gut-brain connection theory is further proof that a healthy, balanced diet reduces the risk of many diseases, depression in particular.
Many of these studies have focused on the so-called "Mediterranean diet" - a general term for a diet rich in vegetables, fruits, nuts, seafood, unsaturated fats and vegetable oils, and low in refined sugar, red and processed meats.
(This is, of course, a rather rough generalization, since there are significant differences in how southern Europeans eat.)
However, one Spanish study found that people who ate a traditional Mediterranean diet were half as likely to develop depression.
Image copyright, Getty Images
Image caption,A Mediterranean diet rich in fruits, vegetables, healthy oils, low in processed foods, very healthy
Scientists have shown that the Mediterranean diet increases the diversity of intestinal bacteria and reduces the possibility of other physiological changes, such as chronic inflammation, which also accompany depression.
More than a century after Phillips' experiment at Bethlem Royal Hospital, a reliable cure for depression has yet to be found.