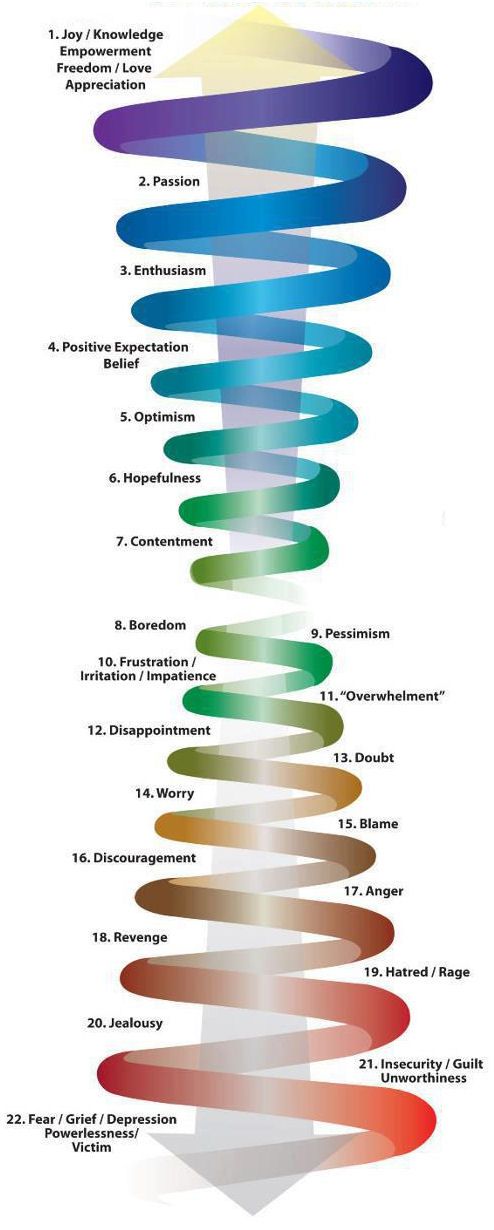
Downward spiral depression
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers. The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
- Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.
 4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk.
 They Hear You.
They Hear You. - Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
- Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses.
 The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States - The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month. The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
- Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.
 4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH) - Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medications for Substance Use Disorders
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 03/22/2023
Spiral dressing
superimposed on the limbs and trunk, when required close more in length than in the previous case, damage. Starts with the imposition of a circular dressings, preferably away from the area damage. Two options are known spiral bandage. The first is spiral bandage without kinks (Fig. 18) is applied on cylindrical parts of the body (thoracic cage, shoulder, hip). Some evasion from a geometrically correct shape cylinder is compensated for due to the elasticity of the bandage. Second option - spiral bandage with kinks (Fig. 19) superimposed on cone-shaped parts of the body (limbs), especially on forearm and lower leg.
Second option - spiral bandage with kinks (Fig. 19) superimposed on cone-shaped parts of the body (limbs), especially on forearm and lower leg.
Fig.17 Circular dressing
Fig.18 Fig.19 Dense Spiral Ascending (a) and descending (b) bandage without kinks folded spiral bandages
Tours spiral bandages lie unevenly, one edge of the bandage crashes, on the other slack remains. In order for this was not, the bandage is overturned. After spending spiral tour, the head of the bandage is overturned so that its front side becomes inside out, next round ends tipping the bandage in the opposite direction etc. Places of bends of the bandage should be in a straight line. Every subsequent round of bandage for 1/2 or 2/3 closes the previous round.
Creeping bandage
Applies for fixing a large length dressing material on the top and lower limbs. creeping bandage is not the main one, but only preliminary before application spiral or some other bandage. The imposition of a creeping bandage eliminates the need for an assistant prevent dressing contamination material in the process of applying a bandage, contributes to better adaptation dressing material. Begin with circular bandage in the area wrist joint or in the area ankles followed by rapid displacement in the proximal direction. Between individual tours remain free a space approximately equal to the width bandage (Fig. 33)
The imposition of a creeping bandage eliminates the need for an assistant prevent dressing contamination material in the process of applying a bandage, contributes to better adaptation dressing material. Begin with circular bandage in the area wrist joint or in the area ankles followed by rapid displacement in the proximal direction. Between individual tours remain free a space approximately equal to the width bandage (Fig. 33)
Turtle headband
superimposed in the elbow, knee and ankle joints. Exists in in the form of two variants: divergent and converging bandages. When damaged directly in the area of the elbow fold, a converging bandage is more advantageous, with damage in the distal parts shoulder - divergent. The first one starts with the imposition of two circular bandages, located above and below the joint, followed by bandaging convergent type (Fig. 34).
Fig.34 Converging Turtle Headband
divergent tortoiseshell bandage starts with overlay circular bandage directly on the joint area, then produce divergent bandaging (Fig. 35).
35).
Fig.35 Divergent tortoise headband
(Octal (swirl-shaped) bandage. Overlay on the occipital region, back surface neck, chest, wrist joint, popliteal fossa, etc. Begins with a circular bandage. Followed by criss-cross tours, alternating with circular, located distally or proximal to the first circular bandages (Fig. 36).
Fig.36 Eight-shaped bandage on the ankle joint
Pituitary gland: size matters - Medical Department Severstal
Often, after an MRI (magnetic resonance imaging) examination of the brain prescribed by a neurologist, patients are referred to an endocrinologist. In what cases does this happen, for what reasons, what is the purpose of the referral? The fact is that doctors, MRI specialists, find changes in the pituitary gland.
"Conductor" of the hormonal orchestra
The brain consists of several parts responsible for specific functions: vision, thinking, memory, hearing, smell, movement in space, sleep, and so on. And these are not only neurological functions, but also endocrine ones.
And these are not only neurological functions, but also endocrine ones.
The pituitary gland - the main endocrine gland of the body, the "conductor" of the entire hormonal orchestra - is located in the lower part of the brain, in the bone niche, not far from the optic chiasm. The organ is very small, weighing only 0.7 g, but extremely important. Translated from Latin, "hypophysis" means "process".
The first description of the structure of the pituitary gland was made in 1867 by P.I. Peremezhko. In the future, many different studies are being carried out to study the anatomy and physiology of the pituitary gland, the release of hormones from it. The pituitary gland is also mentioned in the world fiction, it is enough to recall the immortal creation of Mikhail Bulgakov “Heart of a Dog”.
Anatomically, the pituitary gland consists of three lobes: anterior (adenohypophysis), posterior (neurohypophysis) and intermediate. The pituitary gland produces many different hormones necessary for the normal functioning of the human body. These are thyrotropic, adrenocorticotropic, gonadotropic, somatotropic, prolactin, vasopressin, oxytocin, and melanocyte-stimulating hormones.
These are thyrotropic, adrenocorticotropic, gonadotropic, somatotropic, prolactin, vasopressin, oxytocin, and melanocyte-stimulating hormones.
Reasons for the decrease
The pituitary gland is a very actively working organ (hormone-producing), it has a very dense blood supply, and therefore is subject to influences from inside and outside. Normally, the volume of the pituitary gland is 0.2–0.41 ml. Reducing the size of an organ is much less common than increasing it. For example, a change in the type of the syndrome of "empty Turkish saddle" is more common in patients after injuries, with frequent headaches and a drop in intracranial pressure. The pituitary gland is preserved, but it is compressed by the cerebrospinal fluid and becomes similar in shape to a crescent 1-2 mm wide, its function can be either preserved or impaired.
The size can be reduced after surgery on the pituitary gland, such cases also occur, for example, after the removal of somatotropinoma - a tumor that produces a lot of growth hormone. Hypoplasia (reduction of the pituitary gland) occurs with congenital growth hormone deficiency and short stature.
Hypoplasia (reduction of the pituitary gland) occurs with congenital growth hormone deficiency and short stature.
Next, the homogeneity of the tissue and the presence of volumetric formations are assessed: the pituitary tissue may be diffusely heterogeneous, may have pinpoint hemorrhages, contain a cyst or adenoma. Each such case is evaluated individually.
The most common among these MRI findings are adenomas (hormonally active formations) or incidentalomas (hormonally inactive formations). The type of formation is clarified after a hormonal examination. These tumors are always benign. Of course, dimensions are important: micro- or macroadenoma. This will determine the treatment strategy. Microadenoma has a size of up to 1 cm, macroadenoma - more than 1 cm, giant adenoma - more than 3 cm. corticotropinoma (produces ACTH - adrenocorticotropic hormone, causes Cushing's disease), tumors that produce the main sex hormones - FSH and LH (practically not found), thyrotropinoma (produces TSH and acts on the thyroid gland, is also extremely rare).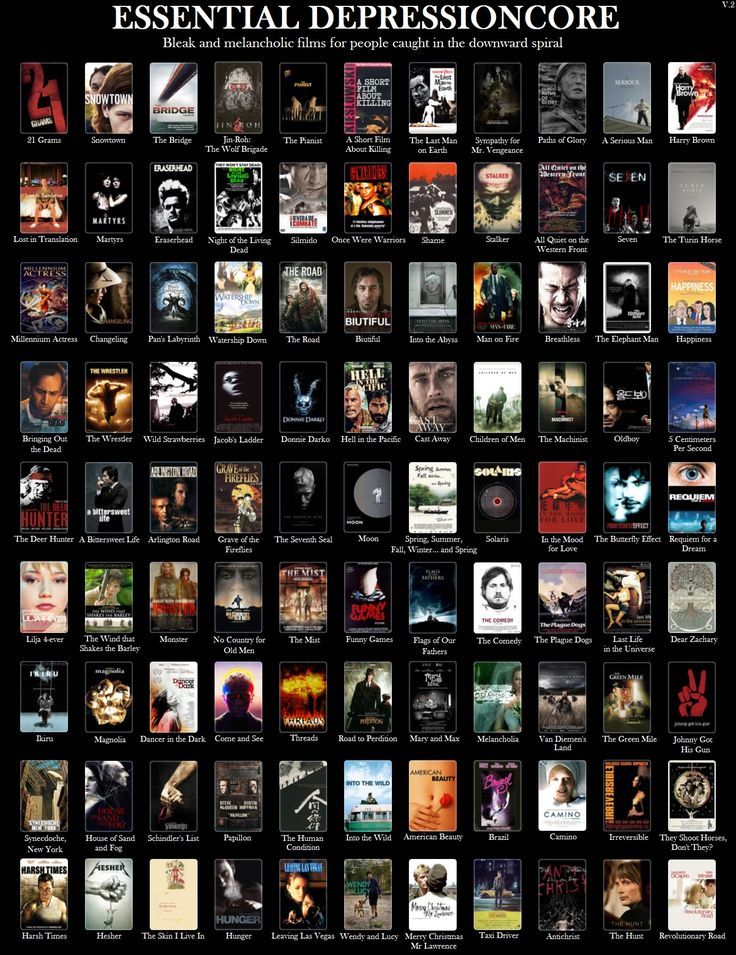
Therefore, to clarify the nature of hormone production, patients are tested for TSH, T4f, T3f, ACTH, cortisol, prolactin, FSH, LH, IGF1 and growth hormone (GH).
Clinical manifestations of the disease depend on the type of hormone produced by the tumor, but we will not dwell on this. Let me just say: since the most vulnerable part of the pituitary gland is the area responsible for the production of the main sex hormones (FSH and LH), and the tumor often compresses this area, symptoms of sexual dysfunction appear. In women, this is easier to identify, since there is a violation of the menstrual cycle.
MRI is usually done with contrast, so you can see the affected area more clearly.
Growth vector
According to the nature of growth, adenomas are divided into the following types:
supra
- asellar - growth towards the optic nerve, the most dangerous growth with a risk of visual impairment, and growth towards the third ventricle, which causes a violation of the outflow of cerebrospinal fluid, more often these are corticotropinomas and hormonally inactive tumors;
- parasellar - growth towards the temporal lobes with compression of the cranial nerves, more often these are prolactinomas and growth hormones;
- infrasellar - growth occurs in the sinus, a fairly safe growth;
- retrosellar - growth through the back of the Turkish saddle (a bony protrusion behind the pituitary gland) towards the brain stem with corresponding manifestations;
- antesellar - growth towards the nasal passages, is rare, only with very large adenomas.
Treatment of adenomas without hormonal production and with hormonal production can be both medical and surgical, radiation treatment is less commonly used, often just monitoring is carried out without serious intervention.
Different adenomas have their own characteristics. Prolactinomas often do not have cysts within the tumor and are sized like microadenomas. Somatotropinomas often have a sharply reduced tumor density signal and large sizes (macroadenomas). Giant adenomas are often hormonally inactive.
Other types of brain tumors
Craniopharyngiomas are a type of common brain tumors. A slowly growing tumor that develops from the remnants of embryonic tissue. It does not produce hormones, but it compresses the "neural pathways" from the hypothalamus to the pituitary gland. It is more common in children and causes dysplasia. In adults, it causes hypothyroidism, diabetes insipidus, menstrual disorders, male potency disorders, and obesity. The peak of the disease is 6-16 years.
The peak of the disease is 6-16 years.
Hypothalamic hamartoma is a rare tumor detected in such an endocrine disease as precocious puberty in children (PPR). Hamartomas are often small - 3–15 mm. They do not affect the surrounding tissues. In addition to signs of PPR (growth of the mammary glands, pubic hair growth at the age of 6-7 years, sometimes spotting), hamartoma is often accompanied by neurological manifestations: epileptic seizures of laughter, convulsions, disorders of thinking, memory and perseverance, emotional disorders - attention deficit, autism, syndrome Asperger's, depression, some children may have uncontrolled aggression.
Cyst of the pineal gland (pineal gland). The pineal gland is an area of the brain that produces the hormone melatonin. A cyst develops due to blockage of the excretory valve of the gland, as a result of which the secret of the gland is not excreted, but accumulates inside the cystic formation. When the gland is affected, there are often no symptoms, but in some cases there may be sleep disturbance, persistent headache, blurred vision, impaired coordination of movements, nausea and vomiting.