Mood stabilizer for bipolar disorder
Bipolar disorder - Diagnosis and treatment
Diagnosis
To determine if you have bipolar disorder, your evaluation may include:
- Physical exam. Your doctor may do a physical exam and lab tests to identify any medical problems that could be causing your symptoms.
- Psychiatric assessment. Your doctor may refer you to a psychiatrist, who will talk to you about your thoughts, feelings and behavior patterns. You may also fill out a psychological self-assessment or questionnaire. With your permission, family members or close friends may be asked to provide information about your symptoms.
- Mood charting. You may be asked to keep a daily record of your moods, sleep patterns or other factors that could help with diagnosis and finding the right treatment.
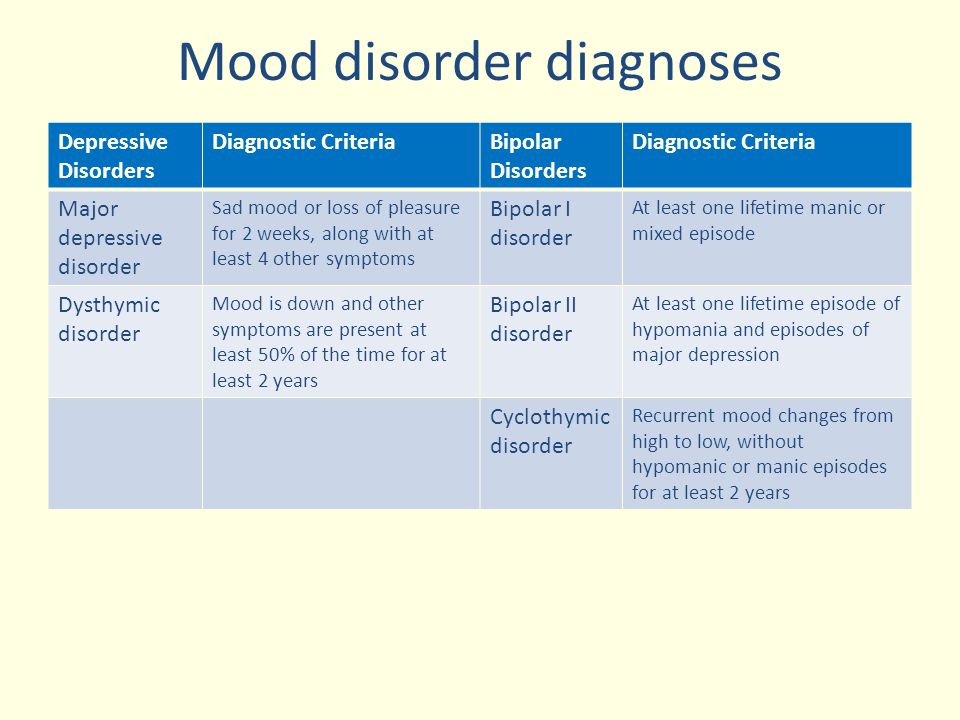
- Criteria for bipolar disorder. Your psychiatrist may compare your symptoms with the criteria for bipolar and related disorders in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
Diagnosis in children
Although diagnosis of children and teenagers with bipolar disorder includes the same criteria that are used for adults, symptoms in children and teens often have different patterns and may not fit neatly into the diagnostic categories.
Also, children who have bipolar disorder are frequently also diagnosed with other mental health conditions such as attention-deficit/hyperactivity disorder (ADHD) or behavior problems, which can make diagnosis more complicated. Referral to a child psychiatrist with experience in bipolar disorder is recommended.
Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your bipolar disorder-related health concerns Start Here
More Information
- Bipolar disorder care at Mayo Clinic
- Bipolar in children
- Urinalysis
Treatment
Treatment is best guided by a medical doctor who specializes in diagnosing and treating mental health conditions (psychiatrist) who is skilled in treating bipolar and related disorders.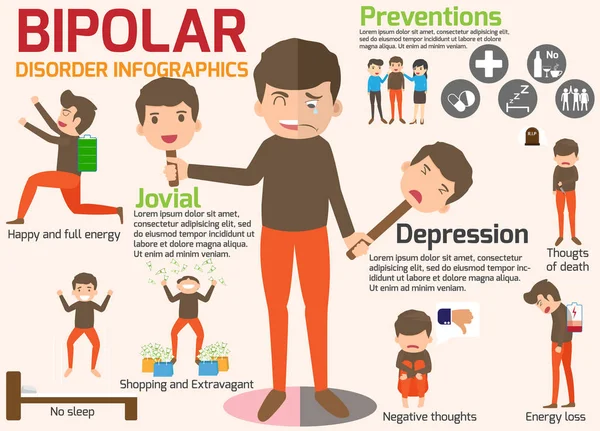 You may have a treatment team that also includes a psychologist, social worker and psychiatric nurse.
You may have a treatment team that also includes a psychologist, social worker and psychiatric nurse.
Bipolar disorder is a lifelong condition. Treatment is directed at managing symptoms. Depending on your needs, treatment may include:
- Medications. Often, you'll need to start taking medications to balance your moods right away.
- Continued treatment. Bipolar disorder requires lifelong treatment with medications, even during periods when you feel better. People who skip maintenance treatment are at high risk of a relapse of symptoms or having minor mood changes turn into full-blown mania or depression.
- Day treatment programs. Your doctor may recommend a day treatment program. These programs provide the support and counseling you need while you get symptoms under control.
-
Substance abuse treatment. If you have problems with alcohol or drugs, you'll also need substance abuse treatment.
 Otherwise, it can be very difficult to manage bipolar disorder.
Otherwise, it can be very difficult to manage bipolar disorder. - Hospitalization. Your doctor may recommend hospitalization if you're behaving dangerously, you feel suicidal or you become detached from reality (psychotic). Getting psychiatric treatment at a hospital can help keep you calm and safe and stabilize your mood, whether you're having a manic or major depressive episode.
The primary treatments for bipolar disorder include medications and psychological counseling (psychotherapy) to control symptoms, and also may include education and support groups.
Medications
A number of medications are used to treat bipolar disorder. The types and doses of medications prescribed are based on your particular symptoms.
Medications may include:
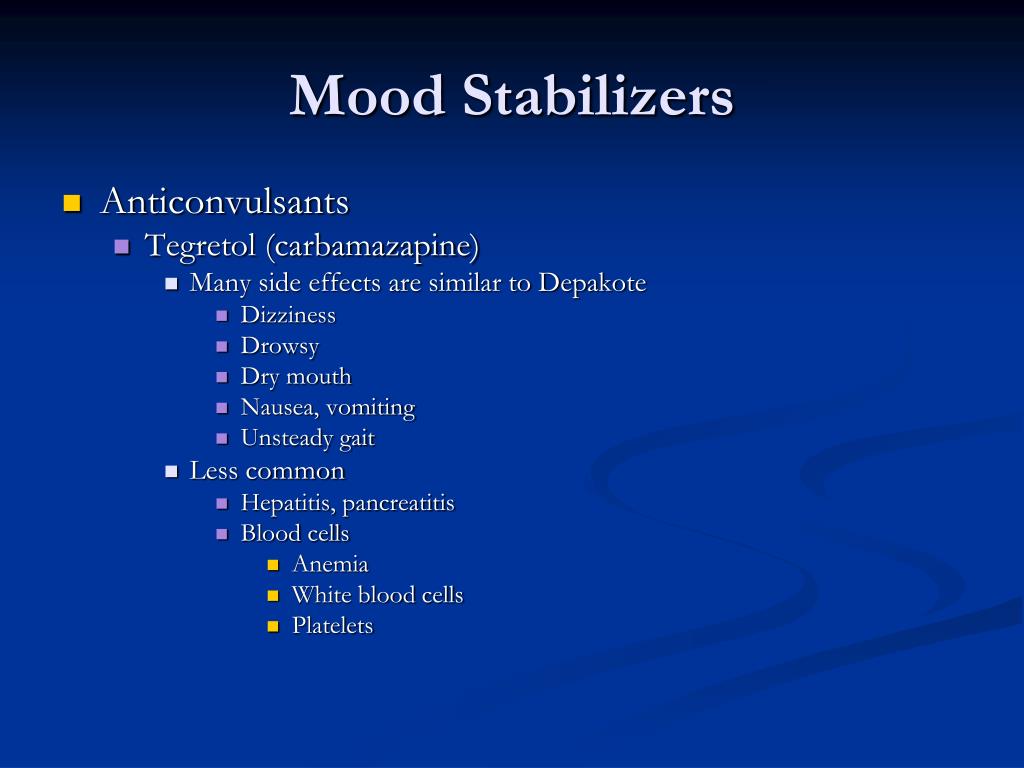
- Mood stabilizers. You'll typically need mood-stabilizing medication to control manic or hypomanic episodes. Examples of mood stabilizers include lithium (Lithobid), valproic acid (Depakene), divalproex sodium (Depakote), carbamazepine (Tegretol, Equetro, others) and lamotrigine (Lamictal).
- Antipsychotics. If symptoms of depression or mania persist in spite of treatment with other medications, adding an antipsychotic drug such as olanzapine (Zyprexa), risperidone (Risperdal), quetiapine (Seroquel), aripiprazole (Abilify), ziprasidone (Geodon), lurasidone (Latuda) or asenapine (Saphris) may help. Your doctor may prescribe some of these medications alone or along with a mood stabilizer.
- Antidepressants. Your doctor may add an antidepressant to help manage depression. Because an antidepressant can sometimes trigger a manic episode, it's usually prescribed along with a mood stabilizer or antipsychotic.
- Antidepressant-antipsychotic. The medication Symbyax combines the antidepressant fluoxetine and the antipsychotic olanzapine. It works as a depression treatment and a mood stabilizer.
- Anti-anxiety medications. Benzodiazepines may help with anxiety and improve sleep, but are usually used on a short-term basis.
Finding the right medication
Finding the right medication or medications for you will likely take some trial and error. If one doesn't work well for you, there are several others to try.
This process requires patience, as some medications need weeks to months to take full effect. Generally only one medication is changed at a time so that your doctor can identify which medications work to relieve your symptoms with the least bothersome side effects. Medications also may need to be adjusted as your symptoms change.
Side effects
Mild side effects often improve as you find the right medications and doses that work for you, and your body adjusts to the medications. Talk to your doctor or mental health professional if you have bothersome side effects.
Don't make changes or stop taking your medications. If you stop your medication, you may experience withdrawal effects or your symptoms may worsen or return. You may become very depressed, feel suicidal, or go into a manic or hypomanic episode. If you think you need to make a change, call your doctor.
If you think you need to make a change, call your doctor.
Medications and pregnancy
A number of medications for bipolar disorder can be associated with birth defects and can pass through breast milk to your baby. Certain medications, such as valproic acid and divalproex sodium, should not be used during pregnancy. Also, birth control medications may lose effectiveness when taken along with certain bipolar disorder medications.
Discuss treatment options with your doctor before you become pregnant, if possible. If you're taking medication to treat your bipolar disorder and think you may be pregnant, talk to your doctor right away.
Psychotherapy
Psychotherapy is a vital part of bipolar disorder treatment and can be provided in individual, family or group settings. Several types of therapy may be helpful. These include:
- Interpersonal and social rhythm therapy (IPSRT). IPSRT focuses on the stabilization of daily rhythms, such as sleeping, waking and mealtimes.
 A consistent routine allows for better mood management. People with bipolar disorder may benefit from establishing a daily routine for sleep, diet and exercise.
A consistent routine allows for better mood management. People with bipolar disorder may benefit from establishing a daily routine for sleep, diet and exercise. - Cognitive behavioral therapy (CBT). The focus is identifying unhealthy, negative beliefs and behaviors and replacing them with healthy, positive ones. CBT can help identify what triggers your bipolar episodes. You also learn effective strategies to manage stress and to cope with upsetting situations.
- Psychoeducation. Learning about bipolar disorder (psychoeducation) can help you and your loved ones understand the condition. Knowing what's going on can help you get the best support, identify issues, make a plan to prevent relapse and stick with treatment.
- Family-focused therapy. Family support and communication can help you stick with your treatment plan and help you and your loved ones recognize and manage warning signs of mood swings.
Other treatment options
Depending on your needs, other treatments may be added to your depression therapy.
During electroconvulsive therapy (ECT), electrical currents are passed through the brain, intentionally triggering a brief seizure. ECT seems to cause changes in brain chemistry that can reverse symptoms of certain mental illnesses. ECT may be an option for bipolar treatment if you don't get better with medications, can't take antidepressants for health reasons such as pregnancy or are at high risk of suicide.
Transcranial magnetic stimulation (TMS) is being investigated as an option for those who haven't responded to antidepressants.
Treatment in children and teenagers
Treatments for children and teenagers are generally decided on a case-by-case basis, depending on symptoms, medication side effects and other factors. Generally, treatment includes:
- Medications. Children and teens with bipolar disorder are often prescribed the same types of medications as those used in adults. There's less research on the safety and effectiveness of bipolar medications in children than in adults, so treatment decisions are often based on adult research.
- Psychotherapy. Initial and long-term therapy can help keep symptoms from returning. Psychotherapy can help children and teens manage their routines, develop coping skills, address learning difficulties, resolve social problems, and help strengthen family bonds and communication. And, if needed, it can help treat substance abuse problems common in older children and teens with bipolar disorder.
- Psychoeducation. Psychoeducation can include learning the symptoms of bipolar disorder and how they differ from behavior related to your child's developmental age, the situation and appropriate cultural behavior. Understanding about bipolar disorder can also help you support your child.
- Support. Working with teachers and school counselors and encouraging support from family and friends can help identify services and encourage success.
More Information
- Bipolar disorder care at Mayo Clinic
- Bipolar medications and weight gain
- Bipolar treatment: I vs.
 II
II - Cognitive behavioral therapy
- Electroconvulsive therapy (ECT)
- Family therapy
- Psychotherapy
- Transcranial magnetic stimulation
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices.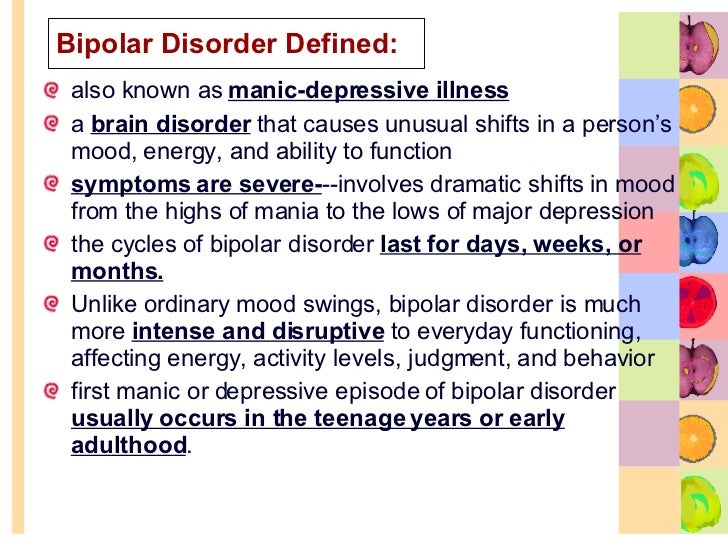 You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
You'll probably need to make lifestyle changes to stop cycles of behavior that worsen your bipolar disorder. Here are some steps to take:
- Quit drinking or using recreational drugs. One of the biggest concerns with bipolar disorder is the negative consequences of risk-taking behavior and drug or alcohol abuse. Get help if you have trouble quitting on your own.
- Form healthy relationships. Surround yourself with people who are a positive influence. Friends and family members can provide support and help you watch for warning signs of mood shifts.
- Create a healthy routine.
 Having a regular routine for sleeping, eating and physical activity can help balance your moods. Check with your doctor before starting any exercise program. Eat a healthy diet. If you take lithium, talk with your doctor about appropriate fluid and salt intake. If you have trouble sleeping, talk to your doctor or mental health professional about what you can do.
Having a regular routine for sleeping, eating and physical activity can help balance your moods. Check with your doctor before starting any exercise program. Eat a healthy diet. If you take lithium, talk with your doctor about appropriate fluid and salt intake. If you have trouble sleeping, talk to your doctor or mental health professional about what you can do. - Check first before taking other medications. Call the doctor who's treating you for bipolar disorder before you take medications prescribed by another doctor or any over-the-counter supplements or medications. Sometimes other medications trigger episodes of depression or mania or may interfere with medications you're taking for bipolar disorder.
- Consider keeping a mood chart. Keeping a record of your daily moods, treatments, sleep, activities and feelings may help identify triggers, effective treatment options and when treatment needs to be adjusted.
Alternative medicine
There isn't much research on alternative or complementary medicine — sometimes called integrative medicine — and bipolar disorder.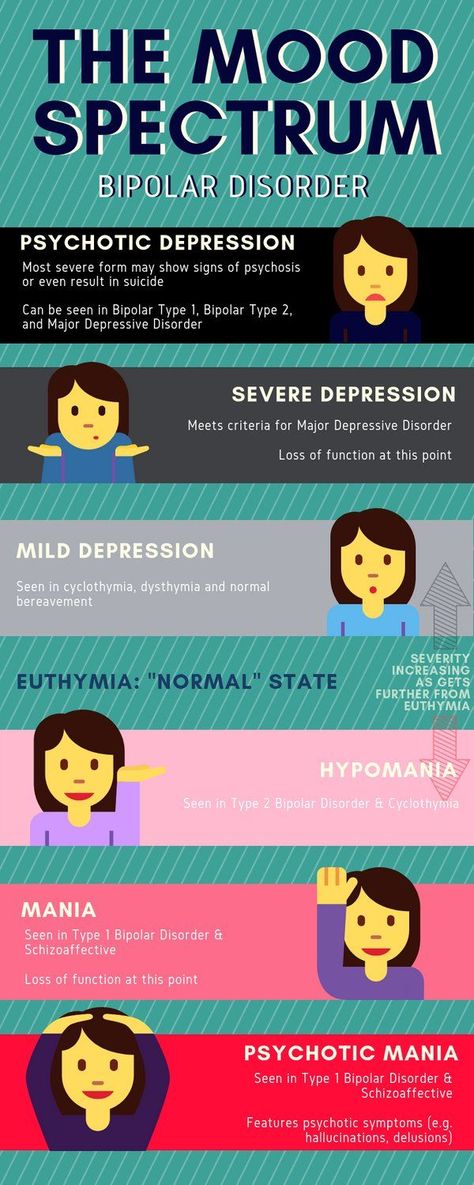 Most of the studies are on major depression, so it isn't clear how these nontraditional approaches work for bipolar disorder.
Most of the studies are on major depression, so it isn't clear how these nontraditional approaches work for bipolar disorder.
If you choose to use alternative or complementary medicine in addition to your physician-recommended treatment, take some precautions first:
- Don't stop taking your prescribed medications or skip therapy sessions. Alternative or complementary medicine is not a substitute for regular medical care when it comes to treating bipolar disorder.
- Be honest with your doctors and mental health professionals. Tell them exactly which alternative or complementary treatments you use or would like to try.
- Be aware of potential dangers. Alternative and complementary products aren't regulated the way prescription drugs are. Just because it's natural doesn't mean it's safe. Before using alternative or complementary medicine, talk to your doctor about the risks, including possible serious interactions with medications.

Coping and support
Coping with bipolar disorder can be challenging. Here are some strategies that can help:
- Learn about bipolar disorder. Education about your condition can empower you and motivate you to stick to your treatment plan and recognize mood changes. Help educate your family and friends about what you're going through.
- Stay focused on your goals. Learning to manage bipolar disorder can take time. Stay motivated by keeping your goals in mind and reminding yourself that you can work to repair damaged relationships and other problems caused by your mood swings.
- Join a support group. Support groups for people with bipolar disorder can help you connect to others facing similar challenges and share experiences.
- Find healthy outlets. Explore healthy ways to channel your energy, such as hobbies, exercise and recreational activities.
- Learn ways to relax and manage stress.
 Yoga, tai chi, massage, meditation or other relaxation techniques can be helpful.
Yoga, tai chi, massage, meditation or other relaxation techniques can be helpful.
Preparing for your appointment
You may start by seeing your primary care doctor or a psychiatrist. You may want to take a family member or friend along to your appointment, if possible, for support and to help remember information.
What you can do
Before your appointment, make a list of:
- Any symptoms you've had, including any that may seem unrelated to the reason for the appointment
- Key personal information, including any major stresses or recent life changes
- All medications, vitamins, herbs or other supplements you're taking, and the dosages
- Questions to ask your doctor
Some questions to ask your doctor may include:
- Do I have bipolar disorder?
- Are there any other possible causes for my symptoms?
- What kinds of tests will I need?
- What treatments are available? Which do you recommend for me?
- What side effects are possible with that treatment?
- What are the alternatives to the primary approach that you're suggesting?
- I have these other health conditions.
 How can I best manage these conditions together?
How can I best manage these conditions together? - Should I see a psychiatrist or other mental health professional?
- Is there a generic alternative to the medicine you're prescribing?
- Are there any brochures or other printed material that I can have?
- What websites do you recommend?
Don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your doctor will likely ask you a number of questions. Be ready to answer them to reserve time to go over any points you want to focus on. Your doctor may ask:
- When did you or your loved ones first begin noticing your symptoms?
- How frequently do your moods change?
- Do you ever have suicidal thoughts when you're feeling down?
- Do your symptoms interfere with your daily life or relationships?
- Do you have any blood relatives with bipolar disorder or depression?
- What other mental or physical health conditions do you have?
- Do you drink alcohol, smoke cigarettes or use recreational drugs?
- How much do you sleep at night? Does it change over time?
- Do you go through periods when you take risks that you wouldn't normally take, such as unsafe sex or unwise, spontaneous financial decisions?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
By Mayo Clinic Staff
Related
Associated Procedures
News from Mayo Clinic
Products & Services
Mood Stabilizers as a Treatment for Bipolar Mania
Written by WebMD Editorial Contributors
In this Article
- Which Bipolar Medicine Is Best?
- What Is Mood-Stabilizing Medication?
- Other Mood-Stabilizing Medicines
- Medicines for Bipolar Depression
- Will the Medicine Work for Me?
- Medication Tips
- Side Effects of Bipolar Drugs
- Stick to Your Treatment
If you have bipolar disorder, the right medications can be like a pair of eyeglasses.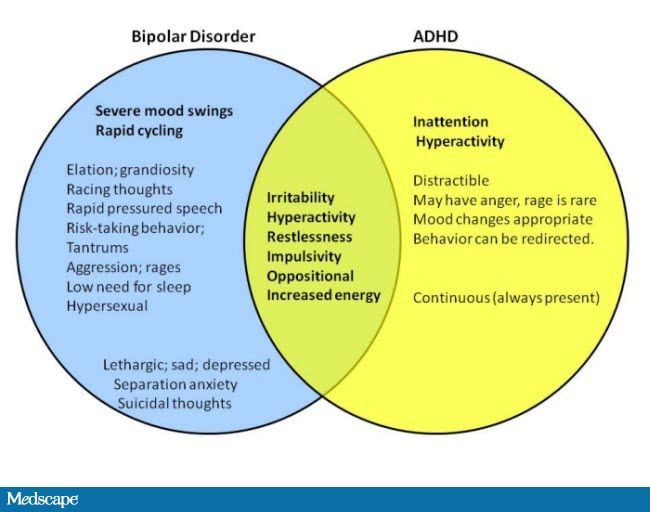 Bipolar disorder distorts your view of yourself and the world, but the medications can help you to see things clearly again.
Bipolar disorder distorts your view of yourself and the world, but the medications can help you to see things clearly again.
Medications are an essential part of a treatment plan. They won’t cure you, but they will help you keep your moods in balance so you can do the things you need and want to do.
Which Bipolar Medicine Is Best?
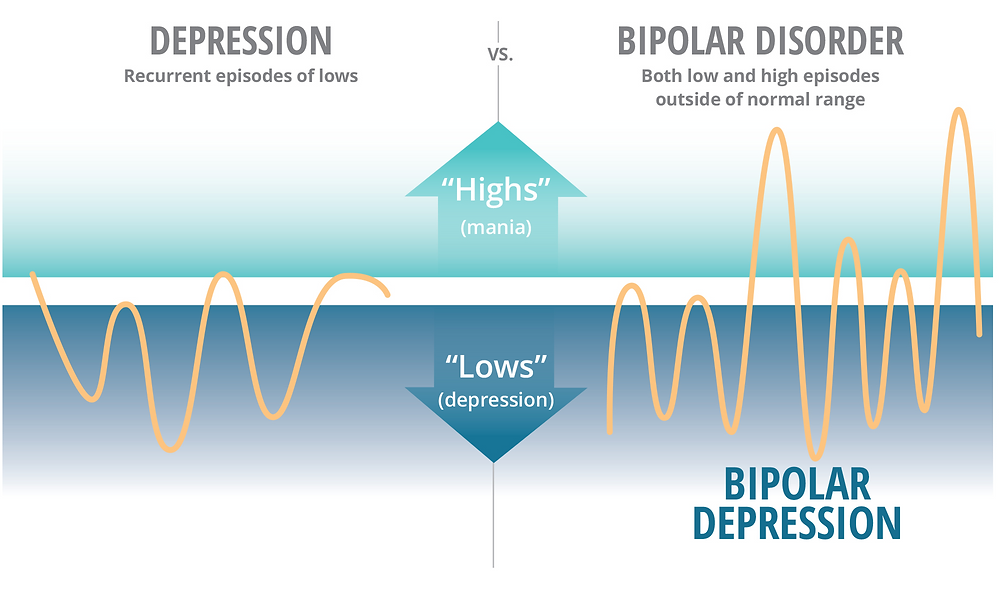
Doctors use many types of drugs to treat bipolar disorder. Some fight the extreme highs of mania and others treat the lows of depression. You might take one drug at a time or a few at the same time.
The best bipolar medicine is the one that works best for you. Work with your doctor to decide on the medication plan that helps you the most.
You may keep taking these medications for years or decades, even if it’s been a long time since your last manic or depressive episode. This is called maintenance therapy and helps prevent recurrence of symptoms.
What Is Mood-Stabilizing Medication?
Mood stabilizers are medicines that treat and prevent highs (mania) and lows (depression).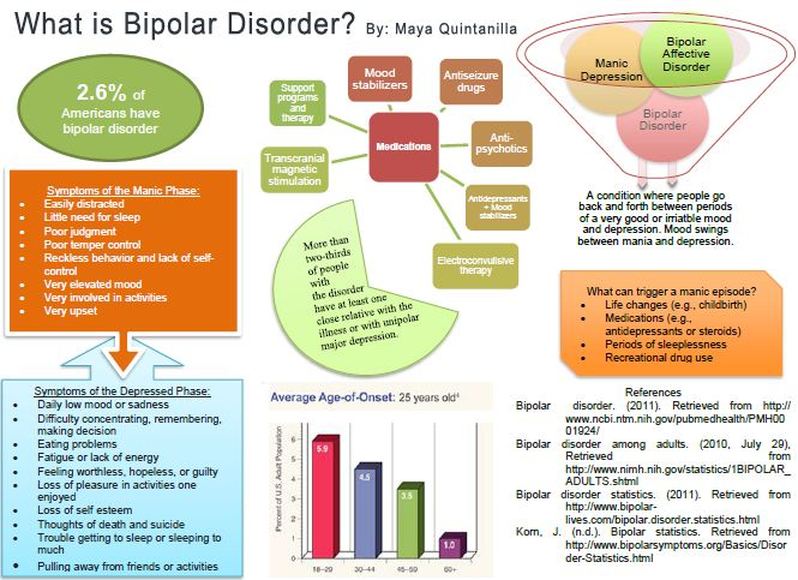 They also help to keep your moods from interfering with work, school, or your social life.
They also help to keep your moods from interfering with work, school, or your social life.
Examples include:
- Carbamazepine (Carbatrol, Epitol, Equetro, Tegretol)
- Divalproex sodium (Depakote)
- Lamotrigine (Lamictal)
- Lithium
- Valproic acid (Depakene)
Some of these drugs are known as anticonvulsants, which are also used to treat seizure disorders, including carbamazepine, lamotrigine, and valproic acid.
Not all of these drugs have the same effects, though. Some (such as lithium) are better at treating mania. Others (such as lamotrigine) may be more useful for depression.
Keep in mind that the term "mood stabilizer" can be misleading. If you take one, your mood can still change during the day. These medicines treat full episodes of mania or depression that last for several days or weeks at a time.
Other Mood-Stabilizing Medicines
Drugs called antipsychotic medications are also common in bipolar treatment plans.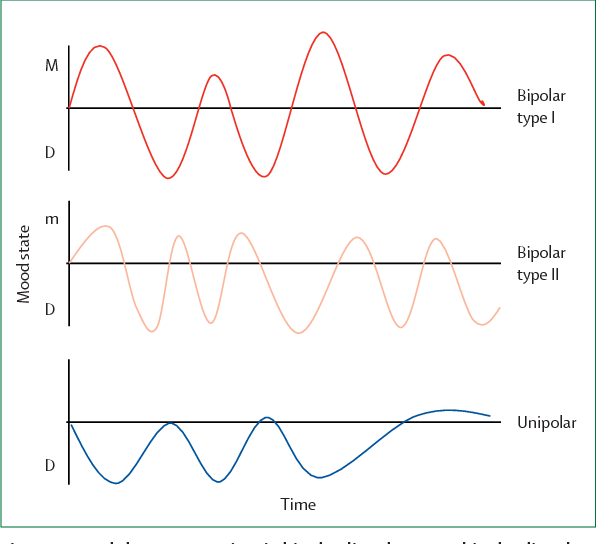 You can take them alone or with mood stabilizers to help with symptoms of mania. These drugs include:
You can take them alone or with mood stabilizers to help with symptoms of mania. These drugs include:
- Haloperidol (Haldol)
- Loxapine (Loxitane) or loxapine inhaled (Adasuve)
Today, doctors may prescribe newer antipsychotic drugs, including:
- Aripiprazole (Abilify)
- Asenapine (Saphris)
- Cariprazine (Vraylar)
- Lumateperone (Caplyta)
- Lurasidone (Latuda)
- Olanzapine (Zyprexa)
- Olanzapine/samidorphan (Lybalvi)
- Quetiapine fumarate (Seroquel)
- Risperidone (Risperdal)
- Ziprasidone (Geodon)
Medicines for Bipolar Depression
Most of the time, doctors will start bipolar disorder treatment by prescribing a mood-stabilizing drug like lithium. But the FDA has approved some medicines for bipolar depression, too:
- Fluoxetine combined with olanzapine (Symbyax)
- lumateperone (Caplyta)
- Lurasidone (Latuda). You might take it alone or with lithium or valproic acid.
- Quetiapine fumarate (Seroquel)
For some people, traditional antidepressants may trigger a manic episode. Because of this risk, your doctor should keep track of you closely if you take one.
Will the Medicine Work for Me?
Your doctor can’t predict how well a particular bipolar medication will work for you. You may need to try several different kinds and different doses to figure out the right approach. And that can take time.
It can be frustrating, but don't give up. Eventually, you and your doctor should be able to find a prescription that works for you.
Medication Tips
If you have bipolar disorder, taking your medication should be part of your routine. Take it at the same time every day. It's easier to remember if you do it along with another daily activity, like brushing your teeth, eating breakfast, or getting into bed. A weekly pillbox can help you see if you've missed a dose.
Be sure to talk to your pharmacist or doctor about the best time of day to take your bipolar medications.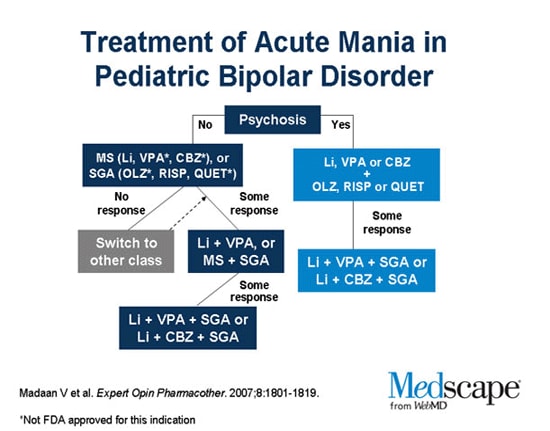 Some are best if you take them in the morning or at bedtime and others with meals or after meals.
Some are best if you take them in the morning or at bedtime and others with meals or after meals.
Make sure you know what to do if you accidentally miss a dose. Ask your doctor. Don't assume that doubling up is a good idea.
Side Effects of Bipolar Drugs
Like any drug, bipolar medicines can cause some side effects. They vary depending on which medications you use. These side effects can include:
- Nausea
- Tremors
- Hair loss
- Sexual problems
- Weight gain
- Liver damage
- Kidney damage
- Diarrhea
- Belly pain
- Skin reaction
Some medications can affect how well your liver works or the amount of white blood cells or platelets you have. You may need regular tests to make sure that you're staying healthy. The antipsychotic drug ziprasidone (Geodon) is linked to a rare but serious skin reaction called DRESS syndrome (drug reaction with eosinophilia and systemic symptoms).
Many side effects will go away after a few weeks of treatment.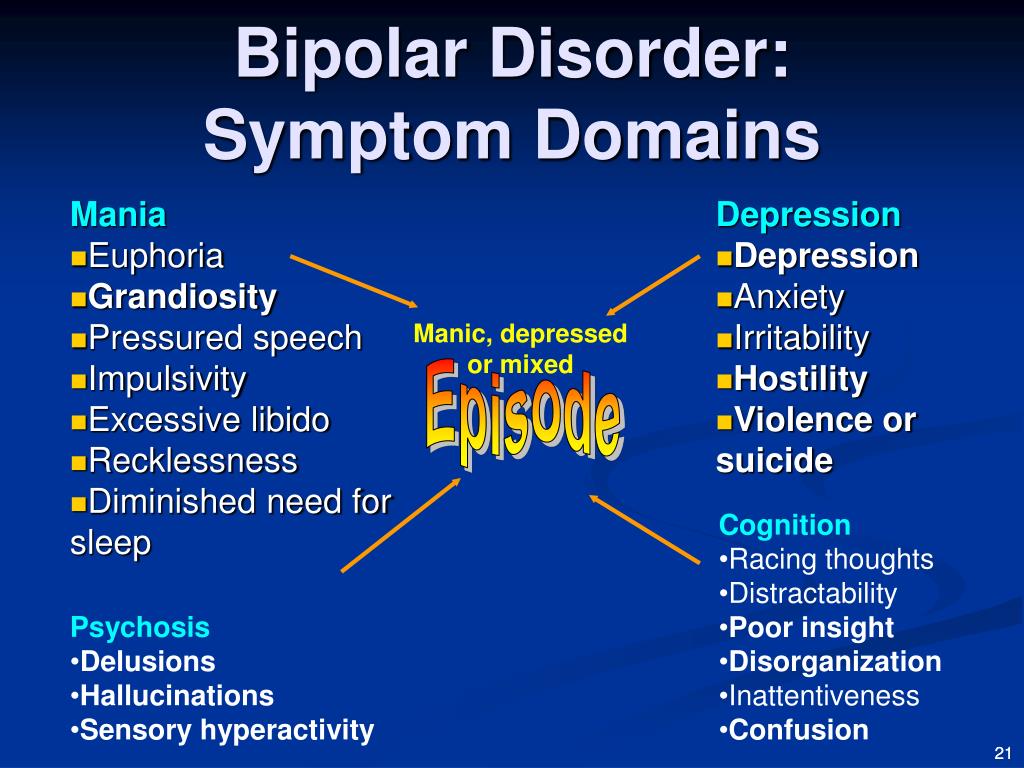 If you still feel bad after that, see your doctor. Don't assume you have to just live with the side effects. Your doctor may be able to change your dose, give you another medicine to control the side effects, or try a different medication altogether.
If you still feel bad after that, see your doctor. Don't assume you have to just live with the side effects. Your doctor may be able to change your dose, give you another medicine to control the side effects, or try a different medication altogether.
Stick to Your Treatment
Medications for bipolar disorder are powerful drugs, and you must take them exactly as your doctor recommends. Don't stop taking a medicine without your doctor's approval. It can be dangerous.
When you're feeling good, you might decide that you want to stop taking your medication. But that's a bad idea unless your doctor agrees. Treatment only during mood episodes may not be enough to prevent symptoms from coming back. In most people, maintenance treatment between mood episodes makes mania and depression happen less often and makes them less severe. If you're feeling good now, that's likely because your medication is working. So stick with it.
Bipolar Disorder Guide
- Overview
- Symptoms & Types
- Treatment & Prevention
- Living & Support
Valproate as a maintenance treatment for people with bipolar disorder after episodes of mood disorder
Bipolar disorder is a disorder that manifests itself in the form of manic and depressive states, and sometimes mixed.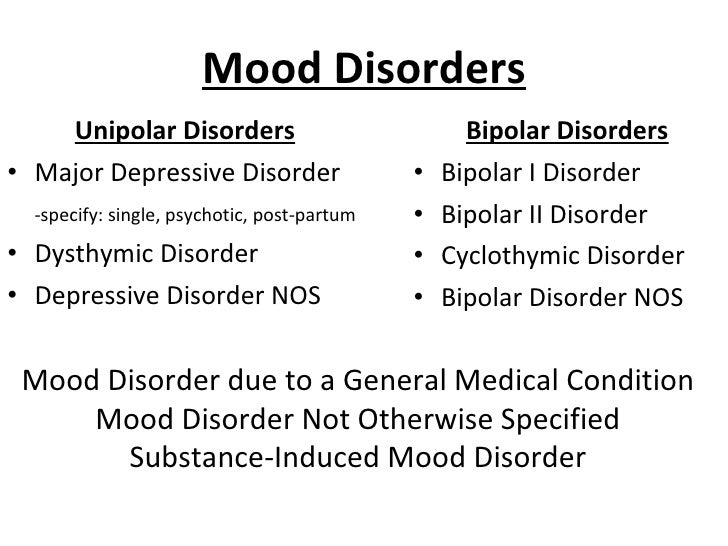 Depression is characterized by a decline in mood and energy, as well as an inability to experience joy, often in combination with other problems, such as sleep disturbance. Mania is the opposite - there is "too" a lot of energy, as well as problems with a good mood or irritability. In mixed states, the symptoms of depression and mania are combined. These episodes of mood disorder usually occur several times in a person's life, so long-term treatment (supportive care) can play a very important role in preventing relapses. Since valproate is a drug that may be useful in the treatment of the acute phase of bipolar disorder, in this review we wanted to answer the following question: is valproate useful as a maintenance agent in bipolar disorder?
Depression is characterized by a decline in mood and energy, as well as an inability to experience joy, often in combination with other problems, such as sleep disturbance. Mania is the opposite - there is "too" a lot of energy, as well as problems with a good mood or irritability. In mixed states, the symptoms of depression and mania are combined. These episodes of mood disorder usually occur several times in a person's life, so long-term treatment (supportive care) can play a very important role in preventing relapses. Since valproate is a drug that may be useful in the treatment of the acute phase of bipolar disorder, in this review we wanted to answer the following question: is valproate useful as a maintenance agent in bipolar disorder?
We searched for relevant studies (randomized controlled trials or RCTs) of long-term treatment of people with bipolar disorder with valproate or any other mood stabilizer, antipsychotic, or placebo. Three of us looked at RCTs to make sure the experiments were scientific. We extracted data from studies, put all the evidence together, and performed statistical analysis to find significant results.
We extracted data from studies, put all the evidence together, and performed statistical analysis to find significant results.
We searched up to 11 January 2013 and found six studies with 876 participants. The quality of the studies in terms of design was not very good, which means that the effects of some drugs may have been overestimated. The pooled studies suggest that valproate may help prevent the recurrence of bipolar disorder, especially depressive episodes. However, due to limited evidence, conclusions regarding valproate versus placebo and lithium (or other active agents) cannot be made with any reasonable degree of certainty. Lithium is an important drug to compare with valproate as it is known to be effective in preventing the recurrence of bipolar disorder. When we pooled the results of all studies that compared valproate with lithium, the evidence did not support superiority of valproate or lithium in terms of efficacy. People who took valproate for a long time were more likely to continue taking their prescribed medications than patients who were given lithium. Clinicians and patients should be aware of the side effects of valproate, including alopecia, tremor, and weight gain.
Clinicians and patients should be aware of the side effects of valproate, including alopecia, tremor, and weight gain.
We also found a study comparing valproate monotherapy with combination therapy (taking two drugs at the same time). This study compared people who took only lithium or valproate with those who took valproate and lithium at the same time. There is no evidence that the use of valproate and lithium, compared with lithium alone, provided greater patient adherence to the prescribed treatment.
Translation notes:
Translation: Lilianna Lenarovna Mullina. Editing: Kukushkin Mikhail Evgenievich. Project coordination for translation into Russian: Cochrane Russia - Cochrane Russia (branch of the Northern Cochrane Center on the basis of Kazan Federal University). For questions related to this translation, please contact us at: [email protected]; [email protected] by: Ekaterina Yudina
Bipolar affective disorder (BAD) - causes, symptoms, treatment
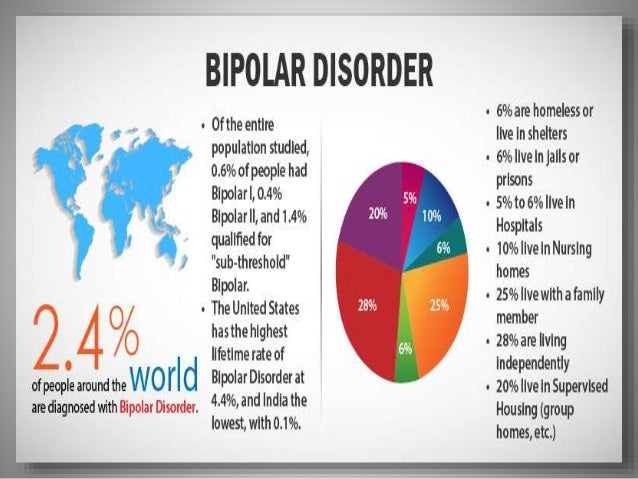
Bipolar affective disorder (BAD) is a severe mental illness characterized by mood and energy swings with recurring episodes of depression followed by episodes of mania or hypomania. BD is highly heritable. Early onset, chronic course and lack of optimal treatment make it one of the most disabling diseases. The lifetime prevalence of bipolar disorder across the spectrum is estimated at 2–4% of the general population and is the sixth leading cause of disability worldwide.
BD is highly heritable. Early onset, chronic course and lack of optimal treatment make it one of the most disabling diseases. The lifetime prevalence of bipolar disorder across the spectrum is estimated at 2–4% of the general population and is the sixth leading cause of disability worldwide.
The average age at onset of bipolar affective disorder varies. According to epidemiological studies, the peak period is 20 years. It is also reported that approximately 20% of all patients show some signs of the disease in adolescence, about 50% by 30 years and 99% by 60 years.
Overall, the data indicate that bipolar disorder is more common in women, but the disease is also widespread among men. Currently, no relationship has been found between incidence and belonging to any social class. By comparison, there is a clear downward social drift among schizophrenic patients.
BAR types
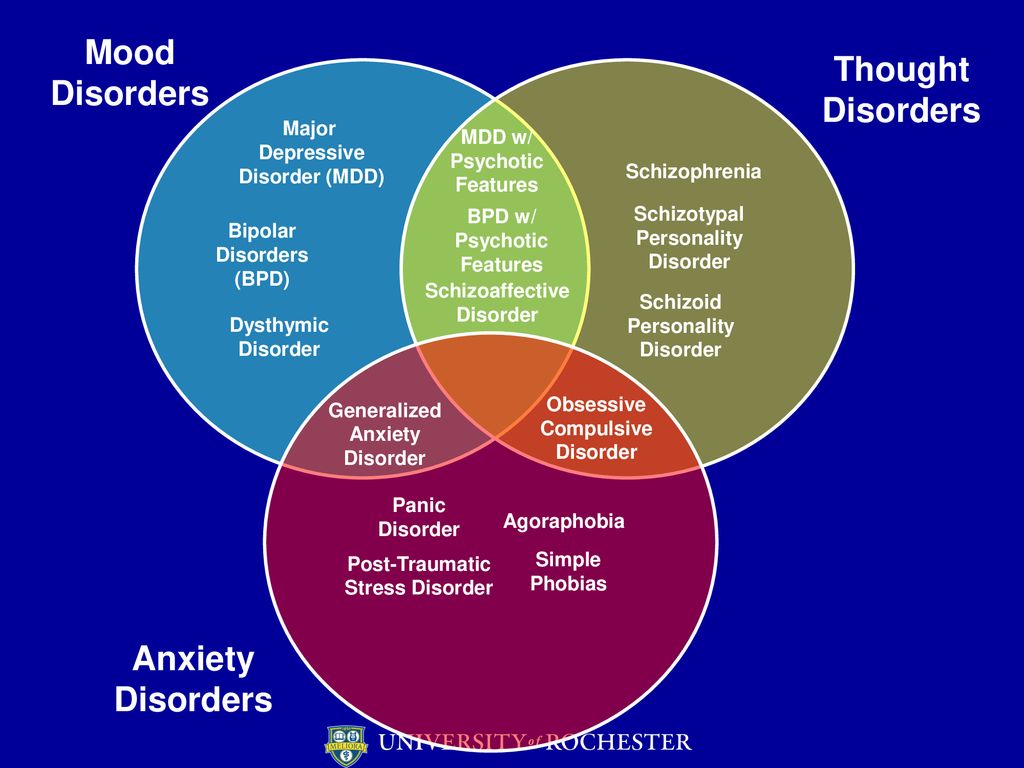
The current diagnostic classification describes two main subtypes: bipolar I disorder and bipolar II disorder, which are distinguished by the absence of full-blown manic episodes in type II bipolar disorder. Type I bipolar disorder can be diagnosed on the basis of a single manic episode, but depressive episodes occur in most cases. Type II bipolar disorder is diagnosed if at least one hypomanic and one depressive episode has occurred. Hypomanic episodes are, by definition, clinically less severe than manic episodes, potentially of shorter duration, not markedly impaired in social or occupational functioning, and do not require hospitalization; the appearance of any psychotic symptoms qualifies the episode as manic.
Type I bipolar disorder can be diagnosed on the basis of a single manic episode, but depressive episodes occur in most cases. Type II bipolar disorder is diagnosed if at least one hypomanic and one depressive episode has occurred. Hypomanic episodes are, by definition, clinically less severe than manic episodes, potentially of shorter duration, not markedly impaired in social or occupational functioning, and do not require hospitalization; the appearance of any psychotic symptoms qualifies the episode as manic.
Causes of bipolar disorder
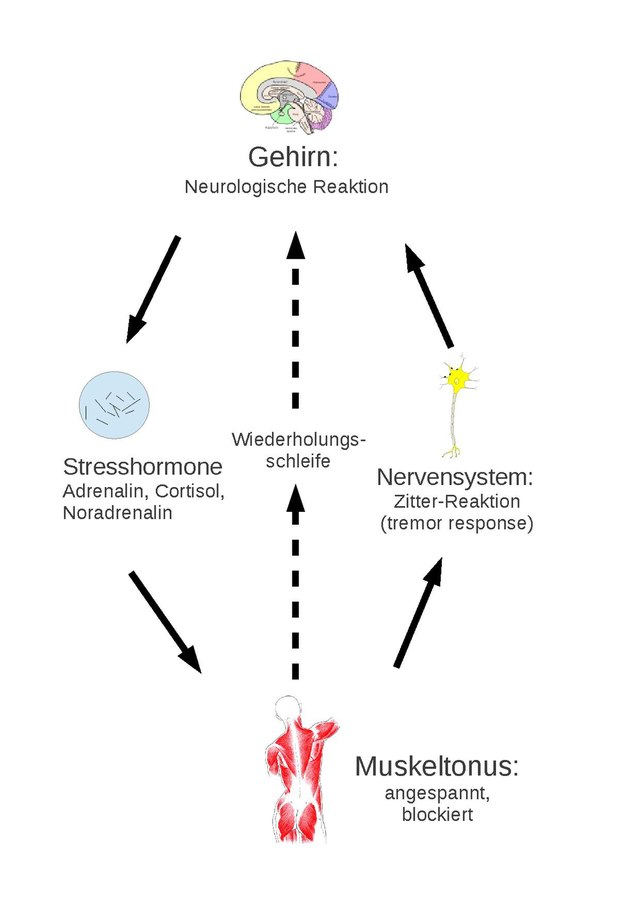
The mechanisms of the development of the disease are complex, multifaceted and not fully established. Among them, there are genetic predisposition, disturbances in the metabolism of neurotransmitters at the level of the brain, endocrine causes, environmental factors, and others.
Psychiatric genetic research has led to the understanding that bipolar affective disorder and its associated diagnoses undoubtedly have a genetic basis, however, they are not caused by a single abnormal gene, but rather have a highly polygenic structure that is not specific to a particular diagnosis. Large pedigree studies show that BAD accumulates in families. The relative risk for immediate family members of patients with bipolar affective disorder is ~7–10%. It is also known that bipolar I disorder tends to aggregate more in families than bipolar type Ⅱ disorder. BAD runs in families with related diagnoses such as major depressive disorder and schizophrenia. At the same time, schizophrenia is more often associated with BAD type Ⅰ compared to BAD type Ⅱ, and major depressive disorder is clearly not combined with a specific BAD subtype.
Large pedigree studies show that BAD accumulates in families. The relative risk for immediate family members of patients with bipolar affective disorder is ~7–10%. It is also known that bipolar I disorder tends to aggregate more in families than bipolar type Ⅱ disorder. BAD runs in families with related diagnoses such as major depressive disorder and schizophrenia. At the same time, schizophrenia is more often associated with BAD type Ⅰ compared to BAD type Ⅱ, and major depressive disorder is clearly not combined with a specific BAD subtype.
In the 1960s, the instrumental possibilities for conducting experiments with brain samples expanded. It became realistic to evaluate their response to the introduction of certain drugs. The results of such experiments, combined with clinical observations, have generated many hypotheses about a single neurotransmitter responsible for the development of a particular mental illness. The catecholamine theory of the occurrence of bipolar affective disorder is popular.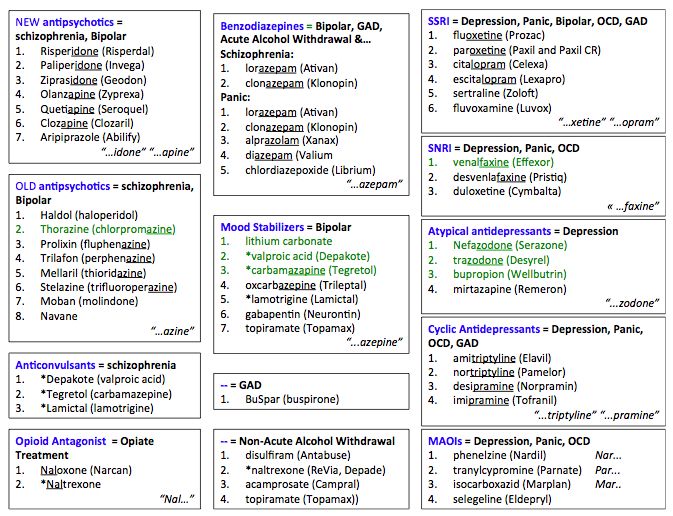 Its central principle is that the two clinical poles of bipolar disorder - mania and depression - arise as a result of functional changes in the activity of catecholamines, while low activity causes a depressive state, and high activity causes a manic state. There is currently strong evidence that the clinical symptoms of BAD can be mimicked and alleviated by pharmacological modulation of the catecholamine system, but there is no direct evidence that the catecholamine system is involved in the pathogenesis of BAD. The same conclusion has been drawn from contemporary evaluations of other influential hypotheses, such as the dopamine hypothesis of schizophrenia.
Its central principle is that the two clinical poles of bipolar disorder - mania and depression - arise as a result of functional changes in the activity of catecholamines, while low activity causes a depressive state, and high activity causes a manic state. There is currently strong evidence that the clinical symptoms of BAD can be mimicked and alleviated by pharmacological modulation of the catecholamine system, but there is no direct evidence that the catecholamine system is involved in the pathogenesis of BAD. The same conclusion has been drawn from contemporary evaluations of other influential hypotheses, such as the dopamine hypothesis of schizophrenia.
The influence of environmental factors is not studied as widely as the influence of genes. However, some reviews show the role of childhood adversity in the development of bipolar disorder, as well as the role of perinatal complications, maternal influenza infection during pregnancy, exposure to maternal smoking in utero, older paternal age at conception, and others.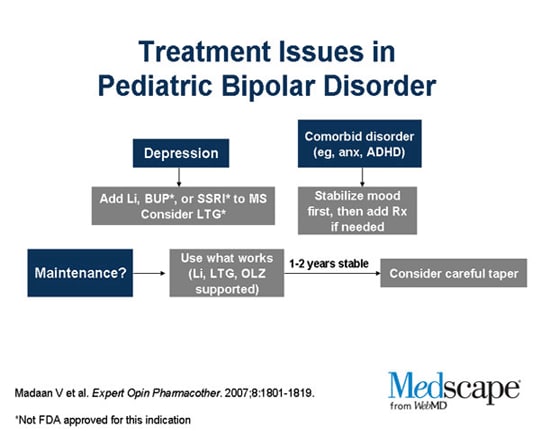
Although stressful life events in and of themselves are not considered a cause of bipolar disorder, they can be a trigger for relapse.
Clinical picture
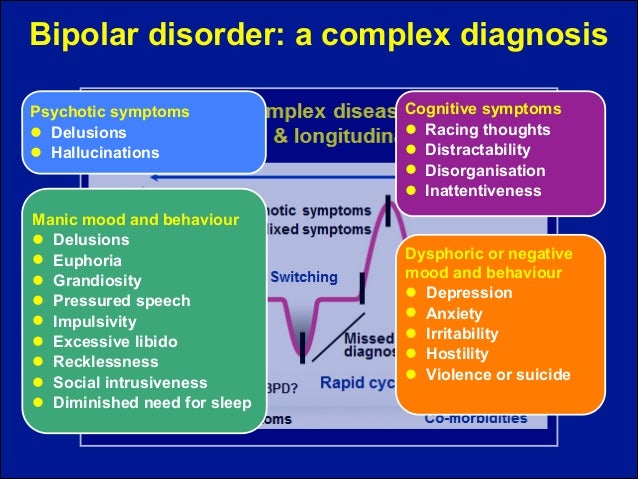
Bipolar affective disorder refers to mood disorders. It manifests itself in different types of episodes - manic, depressive, mixed, which can be expressed in mild, moderate and severe degrees.
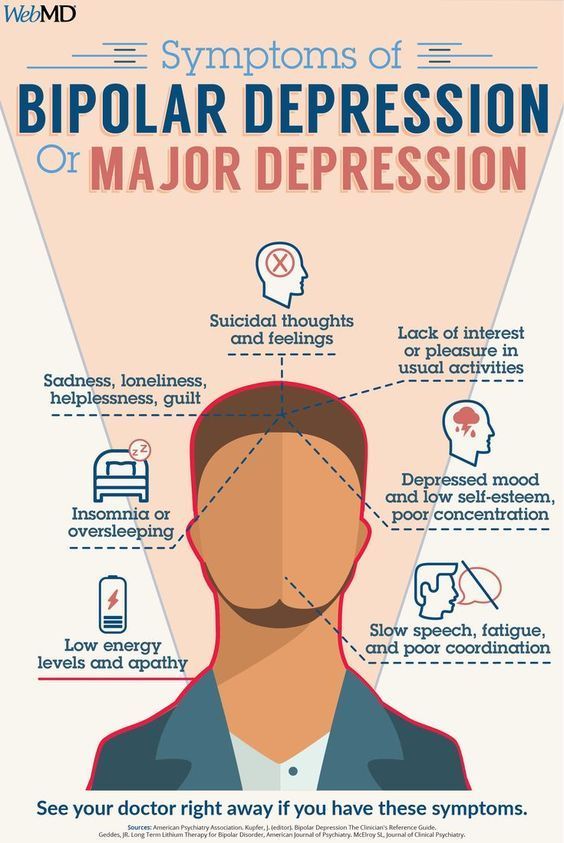
In the case of a depressive syndrome, this can range from subclinical depression to a severe condition that patients perceive as the worst thing that happened in their life. The addition of psychotic symptoms to a severe depressive episode is also likely. These may be delusional ideas of sinfulness, imminent poverty and other misfortunes, for which, according to the patient, he himself is responsible. Auditory hallucinations insult and humiliate, accuse a person, and olfactory hallucinations are most often represented by the smell of sewage. The patient perceives his life as a series of tragic mistakes. Psychomotor retardation can develop up to stupor. Severe depression at least deprives a person of the opportunity to work and maintain social relationships, and in the worst case can lead to suicide.
Psychomotor retardation can develop up to stupor. Severe depression at least deprives a person of the opportunity to work and maintain social relationships, and in the worst case can lead to suicide.
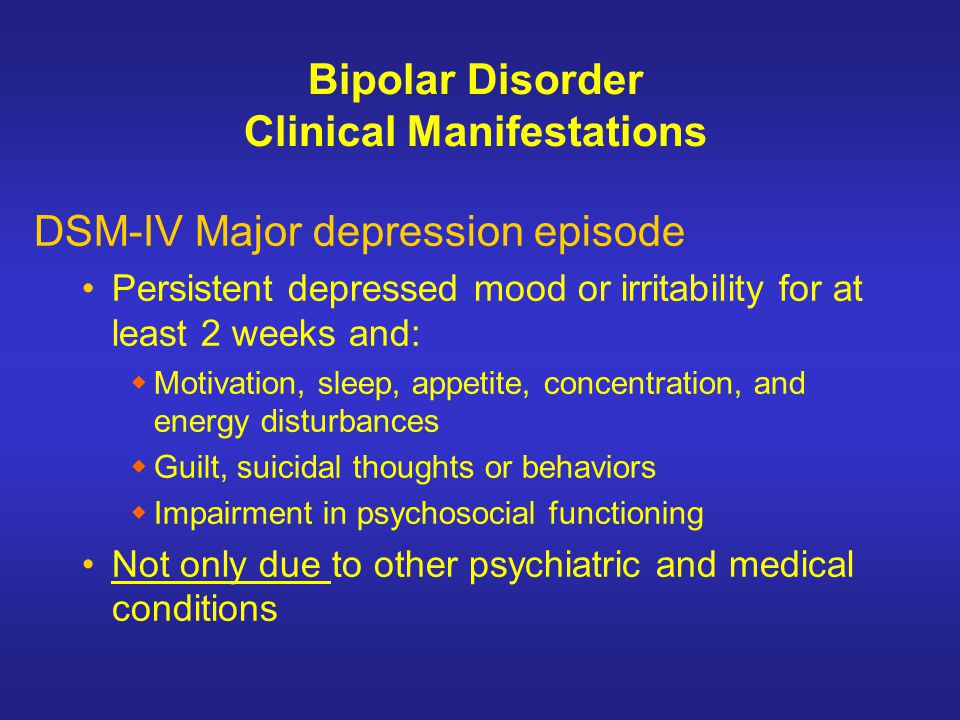
Patients with a mild or even moderate depressive episode certainly experience a reluctance to engage in daily activities, but they usually do not stop functioning fully. They have a significant decrease in mood, loss of interest in the surrounding reality, anhedonia - an inability to enjoy, they feel weak, fatigued. Other symptoms include a decrease in the ability to concentrate, low self-esteem, ideas of one's own insignificance, gloomy ideas about the future, sleep disturbances, and a decrease in appetite.
For a definite diagnosis of depression in bipolar affective disorder, the duration of an episode must be at least two weeks.
Manic syndrome can also be expressed in varying degrees: from hypomania to severe mania with psychotic symptoms.
During the period of hypomania, patients are more socially adapted than in mania.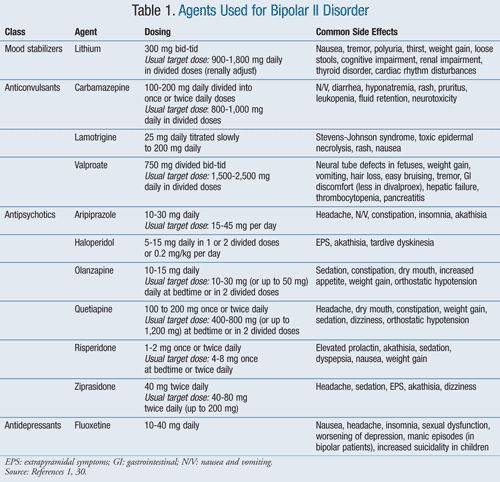 However, in both cases, an important detail is missing - criticism of one's own condition, awareness of oneself as sick.
However, in both cases, an important detail is missing - criticism of one's own condition, awareness of oneself as sick.
The manic stage of bipolar disorder is subjectively more pleasant than the depressive stage. Classical mania, the so-called "jolly mania", is characterized by a typical triad of symptoms: increased mood, ideational-psychic excitement, desire for activity. Patients are in a great mood, they love the whole world, they love themselves. They do not have the slightest doubt in their own abilities, in their own genius, and in addition they have a large supply of energy: many sacrifice sleep for the sake of activity, sleep an hour a day, while not feeling overwhelmed. A person in mania has a false sense of being productive, but new ideas come to him so quickly that old ones remain unfulfilled.
The danger lies in the many rash actions performed by a person on the rise. To give away property, to collect loans, to have questionable sexual contacts, leaving the family and children - a patient with bipolar affective disorder is capable of all this, and he will later have to regret all this.
In addition to classical mania, angry, dysphoric mania also takes place in the structure of the disease. The patient becomes irritable and aggressive beyond measure, especially towards those who do not support his ideas.
The mixed episode combines seemingly incompatible manifestations: melancholy with significant motor arousal, excellent mood simultaneously with stupor, many ideas in parallel with suicidal thoughts. A person is extremely emotionally unstable, which may be a harbinger of an unfavorable outcome of the course of BAD.
The German psychiatrist Emil Kraepelin noted as early as the 19th century that states of manic arousal can vary greatly in duration from weeks to months, and that more severe forms of mania with marked arousal and psychotic features tend to have relatively long episodes. He also believed that melancholic (depressive) states are usually longer than manic episodes, can sometimes persist for years, and tend to become more pronounced than mania at older ages.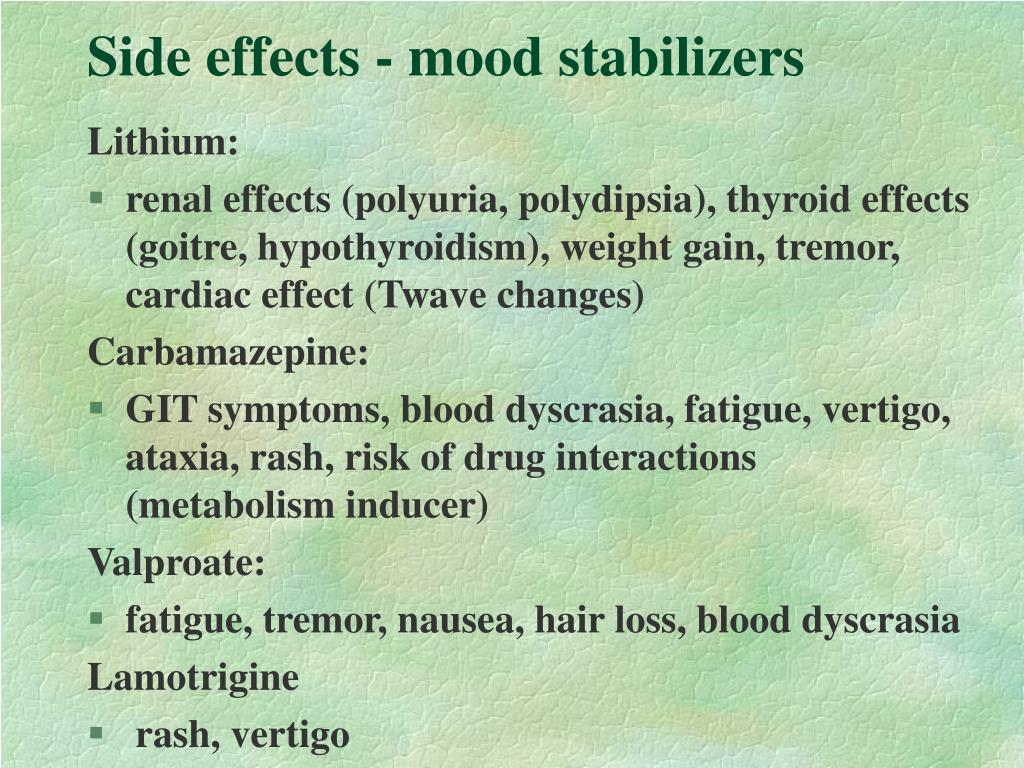 Modern research confirms these ancient ideas.
Modern research confirms these ancient ideas.
Diagnosis
Bipolar disorder of both types (BAD type Ⅰ and BAD type Ⅱ) is difficult to accurately diagnose in clinical practice, especially in the early stages. Only 20% of patients with bipolar disorder who have had a depressive episode are diagnosed within the first year after seeking treatment, and the average delay between onset and diagnosis is 5–10 years. The main reason for the difficulty in diagnosis is to differentiate bipolar type I or II disorder from unipolar depression, a disease characterized by recurrent depressive episodes, especially in patients who present directly during a depressive episode and in those who do not have a clear history. mania or hypomania. Unipolar depression has been reported to be a common misdiagnosis in patients with bipolar disorder, especially in bipolar II disorder, since patients with this disorder, by definition, never experience major manic episodes.
In recent years, the diagnostic criteria for bipolar disorder have been revised to address this problem to include both mood changes and activity or energy changes. New rating scales for self-administration and clinical use have been developed to help improve the early detection of clinical signs suggestive of a diagnosis of bipolar disorder in people with a history of depressive episodes.
New rating scales for self-administration and clinical use have been developed to help improve the early detection of clinical signs suggestive of a diagnosis of bipolar disorder in people with a history of depressive episodes.
As with most mental illnesses, physicians are forced to focus only on a carefully collected history and observation of the clinical picture, due to the lack of laboratory or instrumental studies that could help establish the diagnosis of bipolar disorder. It requires an analysis of subjective - collected from the words of the patient, as well as objective - collected from the words of the immediate environment, anamnestic data, isolating information about affective episodes, the nature, duration and severity of their course.
Features of the course of BAD in women
There is not much difference between the sexes in lifetime prevalence of bipolar affective disorder. However, there are several clinical characteristics that distinguish men and women with bipolar disorder.
Women have a later age of onset than men. They are more likely to debut during the fifth decade. Women with bipolar disorder are more likely to experience an episode of depression followed by mania, while men with bipolar disorder are either as likely or more likely to experience episodes of mania followed by depression.
A bimodal peak in psychiatric hospitalizations in spring and autumn is observed in women with bipolar disorder compared to a unimodal peak in men in the spring.
Some studies have shown gender differences in the long-term outcome of bipolar disorder. Women face significantly greater disruption to social/recreational and family life. This, apparently, is due to their irritability, increased self-confidence, talkativeness, windiness and excessive financial extravagance, since such behavior on the part of a woman is more condemned in society than on the part of a man.
Women are hospitalized much more often than men because they feel worse and tend to seek medical attention more often.
Complications
The most formidable complication of the disease, of course, is the possible suicide of the patient. The determination of suicidal risk is carried out at the very first diagnostic stage of the examination. It includes clarification of anamnestic data related to previous suicide attempts (if any), as well as an assessment of risk factors. There are special questionnaires that can help with this, for example, the Columbia Suicidal Intention Severity Scale.
Loss of connection with reality during the period of mania, in turn, can also lead to a person causing harm of varying degrees of severity to both himself and others.
BAD treatment
Medical therapy
Due to advances in research on pharmacological and psychosocial treatments for bipolar disorder, recommendations for the treatment of the disorder are frequently revised.
According to recent data, there are several types of treatment for acute mania: mood stabilizers (such as lithium and valproic acid) are widely used in combination with atypical antipsychotics (quetiapine, olanzapine, aripiprazole, risperidone, asenapine, paliperidone, and cariprazine). Typical neuroleptics are also effective in mania, although there is a risk of it switching to depression.
Typical neuroleptics are also effective in mania, although there is a risk of it switching to depression.
On the other hand, treatment options for acute bipolar depression are relatively limited. There is evidence supporting the efficacy of quetiapine and olanzapine, as well as the combination of olanzapine and fluoxetine, an antidepressant from the group of selective serotonin reuptake inhibitors. In the depressive phase, it is also possible to prescribe lithium.
Widely available and common tricyclic antidepressants can cause rapid episode cycling and manic reversal, so they should not be used in bipolar disorder, even when combined with mood stabilizers.
Ketamine, which has a rapid antidepressant effect on treatment-resistant depression, can also be used to treat bipolar depression.
Neuromodulation
Electroconvulsive therapy finds its use in therapeutically resistant depression in bipolar disorder.
Transcranial magnetic stimulation is effective in unipolar depression and mania, but its effectiveness in bipolar depression has not yet been proven.
Other drugs and supplements
Some research suggests a possible beneficial effect of N-acetylcysteine, an antioxidant, on bipolar depression and ramelteon, a melatonin agonist, on mood stability. A meta-analysis found that omega-3 fatty acids are effective for bipolar depression but not for mania. Clinical trials of nutritional supplements that improve mitochondrial function are currently ongoing.
Psychosocial treatments
In the treatment of bipolar disorder, pharmacological and psychosocial approaches must work closely together.
With regard to psychosocial treatment, psychoeducation is paramount and should be carried out for all patients, as this significantly reduces the number of relapses.
Various types of psychotherapy are used in the treatment of bipolar disorder: interpersonal and social rhythm therapy (IPSRT) - a modified version of interpersonal therapy specifically designed for the treatment of bipolar disorder, family therapy, cognitive behavioral therapy (CBT).